Abstract
Objective
To identify and synthesize original research on contraceptive user values, preferences, views, and concerns about specific family planning methods, as well as perspectives from health workers.
Study design
We conducted a systematic review of global contraceptive user values and preferences. We searched 10 electronic databases for qualitative and quantitative studies published from 2005 to 2020 and extracted data in duplicate using standard forms.
Results
Overall, 423 original research articles from 93 countries among various groups of end-users and health workers in all 6 World Health Organization regions and all 4 World Bank income classification categories met inclusion criteria. Of these, 250 (59%) articles were from high-income countries, mostly from the United States of America (n = 139), the United Kingdom (n = 29), and Australia (n = 23). Quantitative methods were used in 269 articles, most often cross-sectional surveys (n = 190). Qualitative interviews were used in 116 articles and focus group discussions in 69 articles. The most commonly reported themes included side effects, effectiveness, and ease/frequency/duration of use. Interference in sex and partner relations, menstrual effects, reversibility, counseling/interactions with health workers, cost/availability, autonomy, and discreet use were also important. Users generally reported satisfaction with (and more accurate knowledge about) the methods they were using.
Conclusions
Contraceptive users have diverse values and preferences, although there is consistency in core themes across settings. Despite the large body of literature identified and relevance to person-centered care, varied reporting of findings limited robust synthesis and quantification of the review results.
Keywords: Contraception, Health worker preferences, Patient preferences, Systematic review
1. Introduction
Understanding the values and preferences of contraceptive users is an important component of good healthcare practice at clinical, community, and health system levels, and can ultimately support contraceptive users in identifying and using a method that suits their needs and enables them to meet their family planning goals. Choice—or rather, optimizing choice—is a fundamental principle that guides efforts to strengthen the quality of family planning and contraceptive services [1]. At the clinical level, health workers will be better equipped to work with clients to meet each individual's reproductive health needs if they have an understanding of user values and preferences. Community-level support for contraceptive use, which may include awareness and access through local health workers and pharmacists, media campaigns, and large-scale training and information activities, will benefit from greater understanding of the range of values and preferences. At the health system level, service providers will be better able to respond to unmet need for family planning and empower individuals to access and use preferred contraceptive methods if they are attuned to what end-users value and prefer.
The World Health Organization (WHO) Medical Eligibility Criteria for Contraceptive Use [2] and Selected Practice Recommendations for Contraceptive Use [3] guidelines present information on the safety of various contraceptive methods in the context of specific health conditions and personal characteristics, and how to safely and effectively use a particular method once a person is deemed medically eligible. WHO's guideline development process [4], considers the values and preferences of end-users of contraception and health workers—the individuals and populations affected by the intervention—within the review and development of these guidelines. To inform updated versions of these guidelines, we conducted a systematic review using systematic search, screening, and data abstraction methods to examine values and preferences for all of the contraceptive methods covered. In this manuscript, we present our overall findings from the global review [5,6]. Additional papers in this series detail values and preferences for specific populations of contraceptive end-users and health workers [7–11].
2. Methods
We conducted this review according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [12]. We previously published a detailed description of the methods for the review [6].
Briefly, we searched 10 electronic databases (PubMed, PsycINFO, Sociological Abstracts, CINAHL, Scopus, LILACS, WHO Global Health Libraries, Ovid Global Health, Embase, and POPLINE), secondary-searched several relevant review articles [[13], [14], [15], [16]–17], and asked experts in the field to identify articles published in a peer-reviewed journal between January 1, 2005 and July 27, 2020. Articles had to present primary data (qualitative or quantitative) on contraceptive clients’ or health workers’ values, preferences, views, or concerns regarding the contraceptive methods considered within the WHO's Medical Eligibility Criteria for Contraceptive Use and Selected Practice Recommendations for Contraceptive Use guidelines. To keep the review as broad as possible, we set no restrictions based on language of publication, country/setting, or study design. We searched using key terms for contraception and contraceptive methods, values and preferences, and elimination of irrelevant studies (such as animal studies) and adapted terms for each of the 10 databases.
We first conducted title/abstract screening, then secondary screening in duplicate with discrepancies resolved by discussion and consensus. Inclusion in the global review was determined after full-text review in duplicate. We abstracted data using standardized forms developed specifically for this project, gathering information on: citation, location, target population, study design, sample size, key quantitative or qualitative results, and study rigor (using the Evidence Project Risk of Bias tool [18] for quantitative findings and the Critical Appraisal Skills Programme qualitative research checklist [19] for qualitative findings). We iteratively coded themes that encapsulated values and preferences of end-users and health workers, and we ranked themes by frequency of mention. We summarized coded results narratively to capture main findings related to values and preferences. Due to the large number of included articles, we generally do not include citations to individual articles in the results presented below; instead, we only cite specific papers when providing illustrative quotes or statistics.
3. Results
3.1. Search results
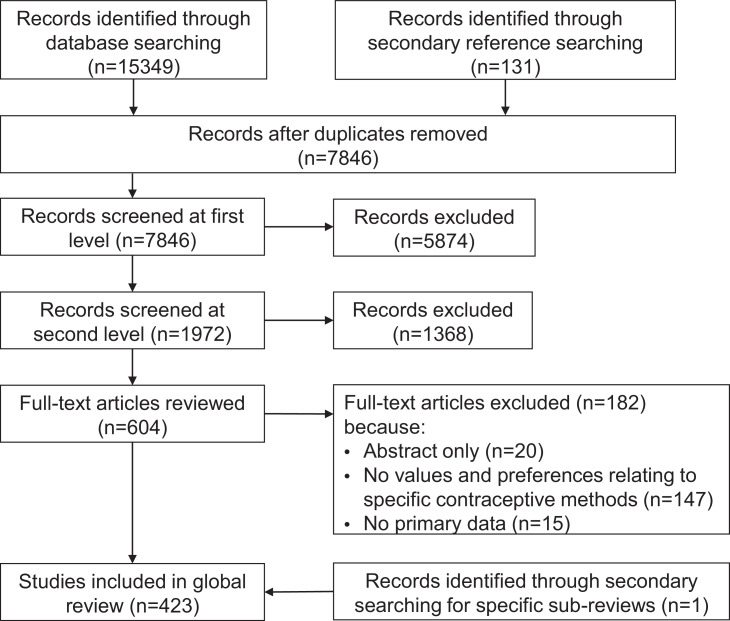
We identified 15,349 potential articles through our search process and an additional 131 through secondary reference searching of included articles, relevant reviews, and specific population subanalyses (Fig. 1). After removing duplicates, we screened the titles/abstracts of 7846 articles and reviewed the full text of 604 articles. Ultimately, 423 articles reporting data from 412 studies met our inclusion criteria. Below, we present an overview of findings from this global review.
Fig. 1.
PRISMA flowchart presenting the search and screening process for the contraceptive values and preferences global review 2005-2020.
3.2. General characteristics of included studies
Summary characteristics of the included articles are provided in the study description table, organized by geographic WHO region (Tables 1A–1F). The Contraceptive Health Research of Informed Choice Experience (CHOICE) study, a large European multicountry study, was reported in 10 articles [[20], [21], [22], [23], [24], [25], [26], [27], [28], [29]–29], and the Contraceptive CHOICE study on long-acting reversible contraceptive (LARC) methods in Missouri, the United States of America (USA), was reported in 4 articles [[30], [31], [32]–33]. The 410 studies (reported in 423 articles) included 463,048 participants; individual study sample sizes ranged from 10 (a qualitative study on intrauterine devices (IUDs) in the United Kingdom [34]) to 70,016 (a cross-sectional analysis of a national household survey in India [35]).
Table 1B.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO Eastern Mediterranean Region 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Abu Hashim 2012 | 10.1016/j.contraception.2011.07.012 | Egypt: Mansoura | Menstrual Issues | Quantitative |
| Jamali 2014 | 10.4103/2231-4040.143025 | Iran | General (female) | Quantitative |
| Kariman 2014 ARABIC | sid.ir/en/Journal/ViewPaper.aspx?ID=364280 | Iran: Zahedan | General (female) | Quantitative |
| Rahmanpour 2010 | PMID: 21381574 | Iran: Zanjan | Postpartum | Quantitative |
| Rahnama 2010 | 10.1186/1471-2458-10-779 | Iran: Tehran | General (female) | Quantitative |
| Shirvani 2008 FARSI | hayat.tums.ac.ir/browse.php?a_id=169 | Iran: Ghaemshahr | General (female) | Quantitative |
| Baram 2020 | 10.1080/13625187.2019.1699048 | Israel | General (female) | Quantitative |
| Romer 2009 | 10.3109/13625180903203154 | Multicountry: Austria; Bulgaria; Estonia; France; Germany; Hungary; Ireland; Italy; Jordan; Latvia; Lebanon; Lithuania; Malta; Netherlands; Poland; Russia; Spain; Ukraine | General (female) | Quantitative |
| Xu 2014 | 10.1016/j.fertnstert.2011.08.019 | Multicountry: China, Taiwan, Hong Kong, Indonesia, Malaysia, Pakistan, South Korea, Thailand | Menstrual Issues | Quantitative |
| Lendvay 2014 | 10.1016/j.contraception.2013.11.002 | Multicountry: Kenya: Nairobi; Pakistan: Sindh, Punjab | General (female) | Quantitative |
| Azmat 2012 | ecommons.aku.edu/cgi/viewcontent.cgi? article=1895&context=pakistan_fhs_mc_chs_chs | Pakistan: Punjab, Sindh | General (mixed gender) | Qualitative |
| Naqaish 2012 | PMID: 23855088 | Pakistan: Islamabad | General (female), Menstrual Issues | Quantitative |
| Nishtar 2013 | 10.5539/gjhs.v5n2p84 | Pakistan: Kirachi: Nasir Colony and Chakra Goth | Young people (mixed gender), Vasectomies | Qualitative |
| Karim 2015 | 10.12669/pjms.316.8127 | Saudi Arabia: Riyadh | General (female) | Quantitative |
Table 1C.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO European Region 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Bodner 2011 | 10.1007/s00404-010-1368-6 | Austria: multiple sites | Young people (female), General (female) | Quantitative |
| Egarter 2012 | 10.1016/j.rbmo.2011.12.003 | Austria: multiple sites | General (female) | Quantitative |
| Stoegerer-Hecher 2012 | 10.3109/09513590.2011.588751 | Austria | General (female) | Quantitative |
| Merckx 2011 | 10.3109/13625187.2011.625882 | Belgium | General (female) | Quantitative |
| Benčić 2014 CROATIAN | PMID: 26285466 | Croatia: Zaprešić | General (female) | Quantitative |
| Fait 2011a | 10.2478/s11536-011-0062-9 | Czech Republic | General (female) | Quantitative |
| Kikalova 2014 CZECH | N/A | Czech Republic: Olomouc, Palacky University | Young people (mixed gender) | Quantitative |
| Tiihonen 2008 | 10.2165/1312067-200801030-00004 | Finland | General (female) | Quantitative |
| Amouroux 2018 | 10.1371/journal.pone.0195824 | France | General (male), Providers | Quantitative |
| Jost 2014 FRENCH | 10.1016/j.gyobfe.2014.04.008 | France | General (female) | Quantitative |
| Brucker 2008 | 10.1080/13625180701577122 | Germany | General (female) | Quantitative |
| Oppelt 2017 | 10.1007/s00404-017-4373-1 | Germany | General (female), Providers | Quantitative |
| Schramm 2007 | 10.1016/j.contraception.2007.03.014 | Germany | General (female) | Quantitative |
| Buhling 2014 | 10.3109/13625187.2014.945164 | Germany | Providers | Quantitative |
| Tsikouras 2014 | 10.1007/s00404-014-3181-0 | Greece | Previously had abortions | Quantitative |
| Sweeney 2015 | 10.1371/journal.pone.0144074 | Ireland: Galway | General (female), Providers | Qualitative |
| Shilo 2015 | 10.1111/jsm.12940 | Israel | Young people (mixed gender) | Quantitative |
| Cagnacci 2018 | 10.1080/13625187.2018.1541080 | Italy | General (female) | Quantitative |
| Crosignani 2009 | 10.1186/1472-6874-9-18 | Italy: multiple sites | General (female) | Quantitative |
| Di Giacomo 2013 | 10.1111/jocn.12432 | Italy | Postpartum | Quantitative |
| Franchini 2017 | 10.1016/j.jmig.2017.02.004 | Italy | Other special medical conditions | Quantitative |
| Gambera 2015 | 10.1186/s12905-015-0226-x | Italy | General (female) | Quantitative |
| Sabatini 2006 | 10.1016/j.contraception.2006.03.022 | Italy: Bari | General (female) | Quantitative |
| Tafuri 2010 | 10.3109/13625180903427683 | Italy: Apulia | General (mixed gender) | Quantitative |
| Vercellini 2010 | 10.1016/j.fertnstert.2009.01.071 | Italy: Milan | Other special medical conditions, Menstrual Issues | Quantitative |
| Zeqiri 2009 | PMID: 20380116 | Kosovo: Kosova | General (female) | Quantitative |
| Čepuliene 2012 | PMID: 23128463 | Lithuania | General (female) | Quantitative |
| Crosby 2013 | 10.1258/ijsa.2008.008120 | Multicountry (online): mostly USA; Australia; Canada; New Zealand; United Kingdom; Western Europe | General (mixed gender) | Quantitative |
| Gemzell-Danielsson 2017 | 10.1111/j.1600-0412.2011.01180.x | Multicountry: Argentina; Canada; Chile; Finland; France; Hungary; Mexico; Netherlands; Norway; Sweden; USA | General (female) | Quantitative |
| Gemzell-Danielsson 2012 | 10.1016/j.contraception.2012.06.002 | Multicountry: Australia, Brazil, Canada, France, Germany, Korea, Mexico, Spain, Sweden, United Kingdom | Providers | Quantitative |
| Hooper 2010 | 10.2165/11538900-000000000-00000 | Multicountry: Australia; Brazil; France; Germany; Italy; Russia; Spain; United Kingdom; USA | General (female) | Quantitative |
| Apter 2016 | 10.1016/j.fertnstert.2016.02.036 | Multicountry: Australia; Finland; France; Norway; Sweden; United Kingdom | General (female) | Quantitative |
| Schultz-Zehden 2006 | 10.2165/00024677-200605040-00006 | Multicountry: Austria; Belgium; Czech Republic; Denmark; Finland; France; Germany; Hungary; Iceland; Netherlands; Norway; Slovakia; Spain; Sweden; United Kingdom | General (female) | Quantitative |
| Bitzer 2012 | 10.1080/13625180902968856 | Multicountry: Austria; Belgium; Czech Republic; Israel; Netherlands; Poland; St Petersburg/Moscow in Russia; Slovakia; Sweden; Switzerland; Ukraine | General (female) | Quantitative |
| Bitzer 2013 | 10.3109/13625187.2011.637586 | Multicountry: Austria; Belgium; Czech Republic; Israel; Netherlands; Poland; St Petersburg/Moscow in Russia; Slovakia; Sweden; Switzerland; Ukraine | General (female) | Quantitative |
| Egarter 2013 | 10.1186/1472-6874-13-9 | Multicountry: Austria; Belgium; Czech Republic; Israel; Netherlands; Poland; St Petersburg/Moscow in Russia; Slovakia; Sweden; Switzerland; Ukraine | General (female) | Quantitative |
| Ahrendt 2006 | 10.1016/j.contraception.2006.07.004 | Multicountry: Austria; Belgium; Denmark; France; Germany; Italy; Norway; Spain; Sweden; Switzerland | General (female) | Quantitative |
| Urdl 2005 | 10.1016/j.ejogrb.2005.01.021 | Multicountry: Austria; Belgium; Finland; France; Germany; Hungary; Netherlands; Poland; South Africa; Switzerland | General (female) | Quantitative |
| Nappi 2016 | 10.3109/13625187.2016.1154144 | Multicountry: Austria; Belgium; France; Italy; Poland; Spain | General (female) | Quantitative |
| Borgatta 2016 | 10.1080/13625187.2016.1212987 | Multicountry: Austria; Belgium; Germany; USA | General (female) | Quantitative |
| Romer 2009 | 10.3109/13625180903203154 | Multicountry: Austria; Bulgaria; Estonia; France; Germany; Hungary; Ireland; Italy; Jordan; Latvia; Lebanon; Lithuania; Malta; Netherlands; Poland; Russia; Spain; Ukraine | General (female) | Quantitative |
| Jakimiuk 2011 | 10.3109/09513590.2010.538095 | Multicountry: Belgium; Bulgaria; France; Ireland; Italy; Poland; Romania; Russia | General (female) | Quantitative |
| Short 2009 | 10.2165/00044011-200929030-00002 | Multicountry: Belgium; Czech Republic; Estonia; France; Germany; Hungary; Latvia; Lithuania; Malta; Slovakia; Slovenia; Spain | General (female) | Quantitative |
| Mansour 2014 | 10.2147/IJWH.S59059 | Multicountry: Brazil; France; Germany; Italy; USA | General (female) | Quantitative |
| Fait 2018 | 10.7573/dic.212510 | Multicountry: Czech Republic; Poland; Romania; Russia; Slovakia | General (female) | Quantitative |
| Fait 2011b CZECH | PMID: 21838148 | Multicountry: Czech Republic; Slovakia | General (female) | Quantitative |
| Fait 2011c CZECH | PMID: 21649999 | Multicountry: Czech Republic; Slovakia | General (female) | Quantitative |
| Heikinheimo 2014 | 10.1093/humrep/deu063 | Multicountry: Finland; France; Ireland; Sweden | General (female) | Quantitative |
| Wiegratz 2010 | 10.3109/13625187.2010.518708 | Multicountry: Germany; Austria | Providers | Quantitative |
| Lopez-del Burgo 2013 | 10.1111/jocn.12180 | Multicountry: Germany; France; Sweden; Romania; United Kingdom | General (female) | Quantitative |
| Haimovich 2009 | 10.1080/13625180902741436 | Multicountry: Germany; France; United Kingdom; Spain; Italy; Russian Federation; Estonia; Latvia; Lithuania; Austria; Czech Republic; Denmark; Norway; Sweden | general (female), Young people (female) | Quantitative |
| Festin 2016 | 10.1093/humrep/dev341 | Multicountry: Thailand, Brazil, Singapore, Hungary | General (female) | Quantitative |
| Loeber 2017 | 10.1080/13625187.2017.1283399 | Netherlands | Previously had abortions | Mixed methods |
| Roumen 2006 | 10.1080/13625180500389547 | Netherlands | General (female) | Quantitative |
| Banas 2014 | 10.3109/01443615.2013.817982 | Poland | General (female), Other special medical conditions | Quantitative |
| Zgliczynska 2019 | 10.3390/ijerph16152723 | Poland (online) | General (female) | Quantitative |
| Bombas 2012 | 10.3109/13625187.2011.631622 | Portugual: multiple sites | Providers | Quantitative |
| Costa 2011 | 10.3109/13625187.2011.608441 | Portugual: multiple sites | General (female) | Quantitative |
| Larivaara 2010 | 10.1080/09581590903436895 | Russia: St. Petersburg | Providers | Qualitative |
| Lete 2007 | 10.3109/13625187.2016.1174206 | Spain: multiple sites | General (female) | Quantitative |
| Lete 2008 | 10.1016/j.contraception.2007.11.009 | Spain: multiple sites | General (female) | Quantitative |
| Lete 2016 | 10.1016/j.contraception.2007.04.014 | Spain | General (mixed gender) | Quantitative |
| Gemzell-Danielsson 2011 | 10.1016/j.ejogrb.2016.11.022 | Sweden: multiple sites | General (female) | Quantitative |
| Kilander 2017 | 10.1080/13625187.2016.1238892 | Sweden | Providers | Qualitative |
| Bitzer 2009 | 10.3109/13625187.2013.819077 | Switzerland: Basel, Bern, Zurich | Providers | Quantitative |
| Merki-Feld 2007 | 10.3109/13625187.2011.630114 | Switzerland | General (female), Young people (female) | Quantitative |
| Merki-Feld 2010 | 10.3109/13625187.2010.524717 | Switzerland: Zurich | General (female) | Quantitative |
| Merki-Feld 2012 | 10.3109/13625187.2014.907398 | Switzerland: multiple sites | General (female) | Quantitative |
| Merki-Feld 2014 | 10.1080/13625180701440180 | Switzerland: Zurich | General (female), Young people (female), Menstrual Issues | Quantitative |
| Asker 2006 | 10.1783/147118906776276170 | United Kingdom: England: Birmingham | General (female) | Qualitative |
| Altiparmak 2006 TURKISH | N/A | Turkey: Manisa | General (female) | Quantitative |
| Ciftcioglu 2009 | 10.1111/j.1365-2648.2009.05024.x | Turkey | General (female) | Quantitative |
| Eskicioglu 2017 | 10.12891/ceog3291.2017 | Turkey | Other special medical conditions | Quantitative |
| Kahramanoglu 2017 | 10.5603/GP.a2017.0115 | Turkey: Istanbul | General (female) | Quantitative |
| Kursun 2014 | 10.3109/13625187.2014.890181 | Turkey | General (female) | Quantitative |
| Ortayli 2005 | 10.1016/s0968-8080(05)25175-3 | Turkey | General (male) | Qualitative |
| Ozturk Inal 2017 | 10.4274/jtgga.2016.0180 | Turkey: Meram | General (female) | Quantitative |
| Yanikkerem 2006 | 10.1016/j.midw.2005.04.001 | Turkey: Manisa | General (female) | Quantitative |
| Bracken 2014 | 10.3109/13625187.2014.917623 | United Kingdom | General (female) | Quantitative |
| Cheung 2005 | 10.1016/j.contraception.2004.12.010 | United Kingdom: England: London | Young people (female), Special social conditions | Qualitative |
| Free 2005 | 10.1080/08870440412331337110 | United Kingdom | Young people (female) | Qualitative |
| Glasier 2008 | 10.1783/147118908786000497 | United Kingdom: Scotland: Edinburgh, Glasgow | General (female), Young people (female) | Qualitative |
| Heller 2017 | 10.1111/aogs.13178 | United Kingdom: Scotland: Edinburgh and surrounding area | Other special medical conditions, Pregnant | Quantitative |
| Hoggart 2013 | 10.1016/s0968-8080(13)41688-9 | United Kingdom: England: London | Young people (female), Providers | Qualitative |
| Kane 2009 | PMID: 19416603 | United Kingdom: England: Lincolnshire | General (female), Young people (female) | Mixed methods |
| Lakha 2005 | 10.1016/j.contraception.2004.12.002 | United Kingdom: Scotland: Edinburgh | General (female) | Quantitative |
| Lowe 2019 | 10.1080/13625187.2019.1675624 | United Kingdom: England: Birmingham, Solihull | General (female) | Mixed methods |
| Moses 2010 | 10.3109/13625180903414483 | United Kingdom: England: Leicestershire and Rutland | Vasectomies | Quantitative |
| Newton 2014 | 10.1136/jfprhc-2014-100956 | United Kingdom: England: London | Young people (female) | Qualitative |
| Okpo 2014 | 10.1016/j.puhe.2014.08.012 | United Kingdom: Scotland | Young people (female), Special social conditions | Qualitative |
| Rosales 2012 | 10.3109/01443615.2011.638998 | United Kingdom | General (female), Previously had abortions | Quantitative |
| Say 2009 | 10.1783/147118909787931780 | United Kingdom: England: Newcastle upon Tyne | Young people (female) | Mixed methods |
| Seston 2007 | 10.1007/s11096-006-9068-9 | United Kingdom: England: North West | General (female) | Quantitative |
| Stephenson 2013 | 10.1016/j.contraception.2013.03.014 | United Kingdom | General (female) | Quantitative |
| Umranikar 2008 | ijsw.tiss.edu/greenstone/collect/ijsw/index/assoc/HASH0182/026f5b23.dir/doc.pdf | United Kingdom: England: Southamptom | General (female) | Quantitative |
| Verran 2015 | 10.1136/jfprhc-2013-100764 | United Kingdom: England: West Midlands | General (female), Special social conditions | Qualitative |
| Walker 2012 | 10.1016/j.jadohealth.2018.10.291 | United Kingdom | General (mixed gender) | qualitative |
| Wellings 2007 | 10.1016/j.contraception.2007.05.085 | United Kingdom | Providers, General (mixed gender) | quantitative |
| Williamson 2009 | 10.1783/147118909788708174 | United Kingdom: Scotland | Young people (female) | qualitative |
Table 1D.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO Region of the Americas 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Alves 2008 Portuguese | 10.1590/s0034-71672008000100002 | Brazil: Sao Paulo | Young people (mixed gender) | Quantitative |
| Fernandes 2006 Portuguese | old.scielo.br/scielo.php?pid=S0104-42302006000500019&script=sci_abstract&tlng=en | Brazil: Sao Paulo: Campinas | Other special medical conditions | Quantitative |
| Ferreira 2014 | 10.1016/j.contraception.2013.09.012 | Brazil: Sao Paulo: Campinas | General (female) | Quantitative |
| Gurgel Cosme de Nascimento 2017 Portuguese | 10.15446/rsap.v19n1.44544 | Brazil: Caraubas: West Potiguar | General (mixed gender) | Quantitative |
| Heilborn 2009 | 10.1590/S0102-311X2009001400009 | Brazil: Rio de Janeiro State | General (female) | Qualitative |
| Hoga 2013 | 10.1016/j.srhc.2013.04.001 | Brazil: Sao Paolo | General (male), Special social conditions | Qualitative |
| Machado 2013 | 10.3109/09513590.2013.808325 | Brazil | General (female) | Quantitative |
| Marchi 2008 | 10.1111/j.1466-7657.2007.00572.x | Brazil: Sao Paulo: Campinas | Vasectomies | Qualitative |
| Scavuzzi 2016 | 10.1055/s-0036-1580709 | Brazil: Pernambuco | General (female), Nulliparous | Quantitative |
| Telles Dias 2006 | 10.1007/s10461-006-9139-x | Brazil: Belem, Salvador, Sao Jose do Rio Preto, Rio de Janeiro, Porto Alegre, Itajai | General (mixed gender), Special social conditions, PLHIV | Mixed methods |
| Choi 2010 | 10.1016/s1701-2163(16)34571-6 | Canada: British Columbia | Providers | Quantitative |
| Nguyen 2011 | 10.1016/j.contraception.2017.01.002 | Canada: Ontario: Kingston (online) | General (mixed gender) | Quantitative |
| Skakoon-Sparling 2019 | 10.1080/00224499.2019.1579888 | Canada: Ontario | General (mixed gender) | Quantitative |
| Toma 2012 | 10.1016/j.jpag.2006.05.005 | Canada | Young people (female) | Quantitative |
| Wiebe 2006 | 10.1016/j.contraception.2006.02.001 | Canada: Vancouver | General (female) | Qualitative |
| Wiebe 2010 | 10.1016/S1701-2163(16)34477-2 | Canada: British Columbia | Nulliparous | Mixed methods |
| Wiebe 2012 | PMID: 23152475 | Canada: British Columbia | Providers | Mixed methods |
| Weisberg 2005b | 10.3109/13625187.2013.853034 | Canada | General (female) | Quantitative |
| Gomez Sanchez 2015 Spanish | 10.1007/s10995-017-2297-9 | Colombia | General (female) | Quantitative |
| Pomales 2013 | 10.1111/maq.12014 | Costa Rica: San Jose | General (male), Vasectomies | Qualitative |
| van Dijk 2013 | 10.1016/j.jana.2012.10.007 | Dominican Republic: Santiago, Puerto Plata | Special social conditions, General (mixed gender) | Qualitative |
| Cremer 2011 | 10.1089/jwh.2010.2264 | El Salvador: La Paz, San Vicente, Cuscatlan, Cabanas | General (female), Special social conditions | Quantitative |
| Cravioto 2014 | 10.1016/j.contraception.2014.04.001 | Mexico | Other special medical conditions | Quantitative |
| Juarez 2011 | 10.1080/17441692.2011.581674 | Mexico: Mexico City: Gustavo A. Madera, Iztapalapa | General (mixed gender) | Qualitative |
| Crosby 2013 | 10.1258/ijsa.2008.008120 | Multicountry (online): mostly USA; Australia; Canada; New Zealand; United Kingdom; Western Europe | General (mixed gender) | Quantitative |
| Crosby 2008 | 10.1007/s10935-013-0294-3 | Multicountry (online): mostly USA; Canada | General (mixed gender) | Quantitative |
| Gemzell-Danielsson 2017 | 10.1111/j.1600-0412.2011.01180.x | Multicountry: Argentina; Canada; Chile; Finland; France; Hungary; Mexico; Netherlands; Norway; Sweden; USA | General (female) | Quantitative |
| Gemzell-Danielsson 2012 | 10.1016/j.contraception.2012.06.002 | Multicountry: Australia, Brazil, Canada, France, Germany, Korea, Mexico, Spain, Sweden, United Kingdom | Providers | Quantitative |
| Hooper 2010 | 10.2165/11538900-000000000-00000 | Multicountry: Australia; Brazil; France; Germany; Italy; Russia; Spain; United Kingdom; USA | General (female) | Quantitative |
| Borgatta 2016 | 10.1080/13625187.2016.1212987 | Multicountry: Austria; Belgium; Germany; USA | General (female) | Quantitative |
| Yam 2007 | 10.1363/ifpp.33.160.07 | Multicountry: Barbados; Jamaica: Kingston metro area | Providers | Quantitative |
| Todd 2011 | 10.1007/s10461-010-9848-z | Multicountry: Brazil: Rio de Janiero; Kenya: Kericho; South Africa: Soweto | PLHIV | Qualitative |
| Mansour 2014 | 10.2147/IJWH.S59059 | Multicountry: Brazil; France; Germany; Italy; USA | General (female) | Quantitative |
| Coffey 2006 | 10.1016/j.contraception.2005.10.017 | Multicountry: Mexico: Cuernavaca; South Africa: Durban; Thailand: Khon Kaen | General (mixed gender) | Quantitative |
| Mack 2010 | 10.1363/3614910 | Multicountry: Nicaragua: Managua; El Salvador: San Salvador and San Miguel | Special social conditions, Providers | Mixed methods |
| Festin 2016 | 10.1093/humrep/dev341 | Multicountry: Thailand, Brazil, Singapore, Hungary | General (female) | Quantitative |
| Cartwright 2020 | 10.12688/gatesopenres.13045.2 | Multicountry: unspecified | Young people (mixed gender), Special social conditions | Mixed methods |
| Yarris 2016 | 10.1080/17441692.2016.1168468 | Nicaragua: Matagalpa | General (female) | Qualitative |
| Jennings 2011 | 10.1016/j.contraception.2010.11.011 | Peru: Lima, Piura | General (female), Providers | Quantitative |
| Ortiz-Gonzalez 2014 | PMID: 25244880 | Puerto Rico: San Juan | Young people (female), Pregnant | Quantitative |
| Agénor 2020 | 10.1363/psrh.12128 | USA: MA: Boston | Young people (male), Special social conditions | Qualitative |
| Akers 2010 | 10.1089/jwh.2009.1735 | USA: PA: Pittsburgh | Providers | Qualitative |
| Amico 2016 | 10.1016/j.contraception.2016.04.012 | USA: NY: NYC: Bronx | General (female) | Qualitative |
| Anderson 2014 | 10.1363/46e1814 | USA: CA: San Francisco | General (female) | Qualitative |
| Arteaga 2016 | 10.1080/00224499.2015.1079296 | USA: CA: San Francisco Bay Area | Young people (female) | Qualitative |
| Bachorik 2015 | 10.1016/j.jpag.2014.08.002 | USA: NY: New York City | Young people (female) | Quantitative |
| Baldwin 2016 | 10.1016/j.contraception.2015.12.006 | USA: OR | Postpartum | Quantitative |
| Benfield 2018 | 10.1016/j.contraception.2018.01.017 | USA: NY | Providers | Quantitative |
| Best 2014 | 10.1363/46E0114 | USA: IN: Indianapolis | Young people (female) | Quantitative |
| Borrero 2009 | 10.1007/s11606-008-0887-3 | USA: PA: Pittsburgh | General (female), Other special medical conditions | Qualitative |
| Callegari 2017 | 10.1016/j.ajog.2016.12.178 | USA | General (female), Special social conditions | Quantitative |
| Campo 2010 | 10.1080/03630242.2010.480909 | USA: (unspecified) rural midwestern state | General (female) | Qualitative |
| Carr 2018 | 10.1016/j.contraception.2017.10.008 | USA: NM | Pregnant, Postpartum, Special social conditions | Mixed methods |
| Chapa 2012 | 10.2147/PPA.S30247 | USA: TX: Dallas | General (female), Other special medical conditions | Quantitative |
| Coleman-Minahan 2019 | 10.1016/j.contraception.2019.08.011 | USA: TX | General (female), Special social conditions, Postpartum | Quantitative |
| Corbett 2006 | 10.1111/j.1745-7599.2006.00114.x | USA: (unspecified) southern coastal city | Young people (mixed gender) | Quantitative |
| Creinin 2008 | 10.1097/01.AOG.0000298338.58511.d1 | USA: multiple sites (Boston, New York, Norfolk, Baltimore, Portland, Los Angeles, Chicago, Philadelphia, Pittsburg, Madison) | General (female) | Quantitative |
| Dehlendorf 2010 | 10.1016/j.pec.2010.06.021 | USA: CA: San Francisco | Previously had abortions | Quantitative |
| Dehlendorf 2013 | 10.1016/j.contraception.2012.10.012 | USA: CA: San Francisco | General (female) | Qualitative |
| DeMaria 2019 | 10.1186/s12905-019-0827-x | USA: (unspecified) southeastern coastal region | General (female) | Mixed methods |
| DeSisto 2018 | 10.1186/s40834-018-0073-x | USA: GA | Postpartum, Special social conditions | Mixed methods |
| Diedrich 2015 | 10.1016/j.ajog.2014.07.025 | USA: MO: St. Louis | General (female) | Quantitative |
| Donnelly 2014 | 10.1016/j.contraception.2014.04.012 | USA: ME, NH, VT | General (female), Providers | Quantitative |
| Downey 2017 | 10.1016/j.whi.2017.03.004 | USA: CA: San Francisco Bay Area | Young people (female) | Qualitative |
| Edelman 2007 | 10.1016/j.contraception.2007.02.005 | USA: OR: Portland; GA: Atlanta | General (female) | Quantitative |
| Epstein 2008 | 10.1016/j.jadohealth.2007.12.007 | USA: CA: San Francisco | Young people (female), Special social conditions | Qualitative |
| Espey 2014 | 10.1016/j.ajog.2013.11.018 | USA: NM: Albuquerque | Nulliparous | Quantitative |
| Fan 2016 | 10.1007/s10508-016-0816-1 | USA: PA: Pittsburgh | General (female) | Mixed methods |
| Fennell 2014 | 10.1016/j.contraception.2013.11.012 | USA: CT, MA, NC, NJ, RI, VA | General (female) | Qualitative |
| Fleming 2010 | 10.1016/j.contraception.2010.02.020 | USA: CA | Young people (female) | Quantitative |
| Foster 2014 | 10.1016/j.contraception.2014.01.025 | USA: multiple sites (St. Louis, New York, San Francisco, Philadelphia, Salt Lake City) | General (female) | Quantitative |
| Friedman 2015 | 10.1016/j.jpag.2014.02.015 | USA: NY: New York City | Young people (female) | Quantitative |
| Frost 2008 | 10.1363/4009408 | USA | General (female) | Quantitative |
| Galloway 2017 | 10.1016/j.jadohealth.2016.12.006 | USA: SC: Spartanburg, Horry | Young people (mixed gender), Nulliparous | Qualitative |
| Garbers 2013 | 10.1089/jwh.2013.4247 | USA: NY: New York City | General (female) | Quantitative |
| Gilliam 2009 | 10.1016/j.jpag.2008.05.008 | USA: IL: Chicago | Young people (female) | Qualitative |
| Gollub 2015 | 10.1080/13691058.2015.1005672 | USA | General (female) | Mixed methods |
| Gomez 2014 | 10.1363/46e2014 | USA | General (female) | Quantitative |
| Gomez 2015 | 10.1016/j.whi.2015.03.011 | USA | General (mixed gender) | Quantitative |
| Gomez 2017 | 10.1016/j.whi.2015.03.011 | USA | General (female) | Qualitative |
| Goyal 2017 | 10.1097/AOG.0000000000001926 | USA: TX | Women seeking abortion services | Quantitative |
| Gubrium 2011 | 10.1007/s13178-011-0055-0 | USA: MA: 3 cities in western region | General (female) | Qualitative |
| Hall 2016a | 10.1016/j.contraception.2016.02.007 | USA | General (female), Young people (female) | Quantitative |
| Hall 2016b | 10.1136/jfprhc-2014-101046 | USA: NY: Ithaca | General (female), Young people (female) | Quantitative |
| He 2016 | 10.1089/jwh.2016.5807 | USA | General (female) | Quantitative |
| Hensel 2012 | 10.1111/j.1743-6109.2012.02700.x | USA | General (male) | Quantitative |
| Higgins 2008 | 10.1363/psrh.12025 | USA: GA: Atlanta | General (mixed gender) | Qualitative |
| Higgins 2015 | 10.1111/jsm.12375 | USA | General (female) | Qualitative |
| Higgins 2017 | 10.1363/47e4515 | USA: WI: Dane County | General (female) | Qualitative |
| Hodgson 2013 | 10.1016/j.contraception.2012.10.011 | USA: CT: New Haven | General (female), Special social conditions | Qualitative |
| Holt 2006 | 10.1089/jwh.2006.15.281 | USA: CA: Northern region | General (mixed gender) | Qualitative |
| Hoopes 2015 | 10.1016/j.jpag.2015.09.011 | USA: WA | Young people (female) | Qualitative |
| Hoopes 2018 | 10.1016/j.jpag.2017.11.008 10.1016/j.jpag.2017.11.008. Epub 2017 Dec 1. | USA: CO | General (female) | Quantitative |
| Howard 2013 | 10.1016/j.jpag.2013.07.013 | USA: MO: Kansas City | Postpartum, Young people (female) | Quantitative |
| Hubacher 2015b | 10.1016/j.contraception.2014.11.006 | USA: NC | General (female) | Quantitative |
| Hubacher 2017 | 10.1016/j.ajog.2016.08.033 | USA: NC | General (female) | Quantitative |
| Jackson 2016 | 10.1016/j.contraception.2015.12.010 | USA | General (female), Women seeking abortion services | Quantitative |
| Kaller 2020 | 10.1186/s12905-020-0886-z | USA: CA: San Francisco | Women seeking emergency contraception, Young people (female) | Qualitative |
| Kavanaugh 2013 | 10.1016/j.jpag.2012.10.006 | USA | Young people (female), Providers | Qualitative |
| Kimport 2017 | 10.1016/j.contraception.2016.10.009 | USA: CA: San Francisco Bay Area | General (female) | Qualitative |
| Lamvu 2006 | 10.1016/j.contraception.2005.10.007 | USA | General (female) | Quantitative |
| Latka 2008 | 10.1521/aeap.2008.20.2.160 | USA: NY: New York City | Young people (mixed gender) | Qualitative |
| Lehan Mackin 2015 | 10.1177/0193945914551005 | USA | General (female) | Quantitative |
| Lessard 2012 | 10.1363/4419412 | USA: multiple sites (St. Louis, Chicago, Little Rock, Seattle, Philadelphia, Oakland) | Women seeking abortion services | Quantitative |
| Levy 2014 | 10.1016/j.whi.2014.10.001 | USA: CA: 6 San Francisco Bay Area clinics | General (female), Providers | Qualitative |
| Lewis 2012 | 10.1016/j.jpag.2012.08.003 | USA: IL: Chicago | postpartum, Young people (female) | Qualitative |
| Madden 2010 | 10.1016/j.contraception.2009.08.002 | USA: IL | Providers | Quantitative |
| Madden 2015 | 10.1016/j.ajog.2015.01.051 | USA | General (female) | Quantitative |
| Mantell 2011 | 10.1521/aeap.2011.23.1.65 | USA: NY: New York City | Providers | Qualitative |
| Marshall 2016 | 10.1363/48e10116 | USA | General (female) | Quantitative |
| Marshall 2017 | 10.1016/j.contraception.2017.10.004 | USA: CA: Oakland | General (female) | Qualitative |
| McLean 2017 | 10.1016/j.contraception.2016.08.010 | USA: CA: San Francisco Bay Area | General (female), Providers | Mixed methods |
| McNicholas 2012 | 10.1016/j.whi.2012.04.008 | USA: (unspecified) urban site | Women seeking abortion services | Quantitative |
| Melo 2015 | 10.1016/j.jpag.2014.08.001 | USA: CO | Young people (female) | Qualitative |
| Melton 2012 | 10.1363/4402212 | USA: UT: Salt Lake City | Women seeking emergency contraception | Quantitative |
| Merkatz 2014 | 10.1016/j.contraception.2014.05.015 | USA: MO: St. Louis | General (female) | Quantitative |
| Michaels 2018 | N/A | USA: IA | Women seeking abortion services | Quantitative |
| Miller 2011 | 10.1016/j.contraception.2010.06.005 | USA: PA | Young people (mixed gender) | Quantitative |
| Minnis 2014 | 10.1363/46e1414 | USA: CA: San Francisco | Young people (female) | Mixed methods |
| Modesto 2014 | 10.1093/humrep/deu089 | USA: CA: San Francisco | General (female) | Quantitative |
| Munsell 2009 | print.ispub.com/api/0/ispub-article/9991 | USA: TX: Galveston | Providers | Quantitative |
| Nelson 2017 | 10.1016/j.contraception.2017.09.010 | USA | General (female) | Quantitative |
| Nettleman 2007 | 10.1016/j.jmwh.2006.10.019 | USA | General (female), Special social conditions | Qualitative |
| Nguyen 2017 | 10.1016/j.jpag.2011.06.002 | USA | Providers | Quantitative |
| Paul 2020 | 10.1016/j.ajog.2019.11.1266 | USA: (unspecified) mid-west region | General (female) | Quantitative |
| Payne 2016 | 10.1111/jmwh.12425 | USA: (unspecified) southeastern | General (female) | Qualitative |
| Peipert 2011 | 10.1097/AOG.0b013e31821188ad | USA: MO: St. Louis | General (female), Special social conditions | Quantitative |
| Philliber 2014 | 10.1016/j.whi.2014.06.001 | USA: CO, IA | Providers | Quantitative |
| Potter 2014a | 10.1097/aog.0000000000002136 | USA: NY: school- based health centers (SBHCs) and community health center | Young people (female) | Qualitative |
| Potter 2014b | 10.1016/j.contraception.2014.06.039 | USA: TX: El Paso, Austin | Postpartum | Quantitative |
| Potter 2017 | 10.1016/j.contraception.2014.01.011 | USA: TX: Odessa, Austin, Edinburg, Dallas, Houston, El Paso | Postpartum | Quantitative |
| Powell-Dunford 2011 | 10.1016/j.whi.2010.08.006 | USA | General (female), Special social conditions | Quantitative |
| Raifman 2018 | 10.1016/j.whi.2017.07.006 | USA: MI, MO, NJ, UT | general (female) | Quantitative |
| Rey 2020 | 10.1016/j.contraception.2020.01.010 | USA: VT | General (female), PWID | Quantitative |
| Rocca 2007 | 10.1016/j.ajog.2006.08.024 | USA: CA: San Francisco Bay Area | Young people (female) | Quantitative |
| Roe 2016 | 10.1016/j.rmed.2016.10.012 | USA: PA (online) | Other special medical conditions | Quantitative |
| Rubin 2010 | 10.1016/j.jpag.2015.09.001 | USA: NY: NYC: Bronx | General (female) | Qualitative |
| Rubin 2015 | 10.1089/jwh.2009.1549 | USA: NY: NYC: Bronx | Young people (female) | Qualitative |
| Sanders 2014 | 10.1371/journal.pone.0199724 | USA | Young people (male) | Quantitative |
| Sanders 2018 | 10.1007/s10461-013-0422-3 | USA: UT: Salt Lake City | General (female) | Quantitative |
| Sangi-Haghpeykar 2006 | 10.1016/j.contraception.2006.02.010 | USA: TX: Houston | General (female), Previously had abortions | Quantitative |
| Sangraula 2017 | 10.1016/j.jpag.2016.11.004 | USA: NY: NYC: Uptown Manhattan, Lower Bronx | Young people (female) | Qualitative |
| Sastre 2015 | 10.1080/13691058.2014.989266 | USA: FL: Miami-Dade County | General (mixed gender), Special social conditions | Qualitative |
| Shih 2013 | 10.1177/1557988312465888 | USA: CA: San Francisco | General (mixed gender), Vasectomies | Qualitative |
| Sittig 2020 | 10.1016/j.whi.2019.11.003 | USA: PA (online) | General (female), Special social conditions | Quantitative |
| Spies 2010 | 10.1016/j.whi.2010.07.005 | USA | Young people (female), General (female) | Qualitative |
| Stanek 2009 | 10.1016/j.contraception.2008.09.003 | USA: OR | Women seeking abortion services | Quantitative |
| Stanwood 2009 | 10.1016/j.contraception.2005.05.020 | USA | General (female) | Quantitative |
| Stein 2020 | 10.1016/j.jpag.2020.01.004 | USA: NY: NYC: Bronx | Young people (female) | Quantitative |
| Stewart 2007 | 10.1016/j.jpag.2007.06.001 | USA: CA: San Francisco | Young people (female), Special social conditions | Quantitative |
| Straten 2016 | 10.1007/s10461-016-1299-8 | USA | General (female) | Quantitative |
| Sulak 2006 | 10.1016/j.contraception.2005.07.001 | USA | Providers | Quantitative |
| Sundstrom 2015 | 10.1080/10410236.2016.1172294 | USA: SC: Charleston | General (female) | Qualitative |
| Sundstrom 2016 | 10.1080/10810730.2015.1018650 | USA | Young people (female) | Qualitative |
| Tanner 2008 | 10.1016/j.jadohealth.2008.02.017 | USA: IN: Indianapolis | Young people (female) | Quantitative |
| Teal 2012 | 10.1016/j.contraception.2011.07.001 | USA: CO | Young people (female) | Quantitative |
| Terrell 2011 | 10.1016/j.jpag.2011.02.003 | USA: IN: Indianapolis | Young people (female) | Quantitative |
| Thorburn 2006 | 10.1300/J013v44n01_02 | USA: CA | Young people (female) | Quantitative |
| Tung 2012 | 10.1080/07448481.2012.663839 | USA | General (mixed gender) | Quantitative |
| Turok 2016 | 10.1016/j.contraception.2016.01.009 | USA: UT: Salt Lake City | Women seeking emergency contraception | Quantitative |
| Tyler 2012 | 10.1097/AOG.0b013e31824aca39 | USA: multiple sites | Providers | Quantitative |
| Venkat 2008 | 10.1007/s10900-008-9100-1 | USA: NY: NYC | General (female), Special social conditions | Quantitative |
| von Sadovszky 2008 | 10.1016/j.whi.2008.01.004 | USA | General (female), Special social conditions | Quantitative |
| Walker 2019 | 10.1080/03630242.2012.728190 | USA: CA: Northern region | Young people (female) | Quantitative |
| Werth 2015 | 10.1016/j.ajog.2014.09.003 | USA: MO: St. Louis | General (female) | Quantitative |
| Weston 2012 | 10.1016/j.ajog.2011.06.094 | USA: IL: Chicago | Young people (female), Postpartum | Qualitative |
| Whitaker 2008 | 10.1016/j.contraception.2008.04.119 | USA: PA: Pittsburgh | Young people (female) | Quantitative |
| White 2013 | 10.1016/j.whi.2013.05.001 | USA: TX: El Paso | General (female) | Qualitative |
| Whittaker 2010 | 10.1363/4210210 | USA: PA: Philadelphia | Young people (mixed gender) | Qualitative |
| Woo 2015 | 10.1016/j.contraception.2015.09.007 | USA: MD: Baltimore | General (female) | Quantitative |
| Xu 2011 | 10.2147/ijwh.s57470 | USA | General (female) | Quantitative |
| Yee 2010 | 10.1016/j.jadohealth.2010.03.014 | USA: IL: Chicago | Young people (female), Postpartum | mixed methods |
Table 1E.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO South-East Asia Region 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Zafar 2006 | 10.1111/j.1447-0578.2006.00132.x | Bangladesh: Tangail District: Kalihati sub-district | General (female) | Qualitative |
| Ahuja 2019 | 10.4103/jfmpc.jfmpc_676_19 | India : Patiala, Punjab Province | Young people (female) | Quantitative |
| Das 2015 | 10.1071/SH15045 | India: Delhi | General (female), Special social conditions | Qualitative |
| Hall 2008 | 10.1136/jfprhc-2014-101046 | India: Maharashtra | General (female) | Qualitative |
| Jain 2016 | 10.7860/JCDR/2016/16545.7516 | India: New Delhi | Menstrual Issues | Quantitative |
| Khokhar 2005 | moam.info/determinants-of-acceptance-of-no-scalpel-vasectomy-medind_59d916e41723dd4e6be7785f.html | India: New Delhi | Vasectomies | Quantitative |
| Meenakshi 2020 | 10.4103/jfmpc.jfmpc_1012_19 | India: Jodhpur, Rajasthan | Providers | Quantitative |
| Neeti 2010 | nihfw.org/Publications/pdf/HPPI_33(1),2010.pdf | India: Delhi: Central district | general (female) | Qualitative |
| Patra 2015 | 10.1108/ijhrh-06-2014-0010 | India | General (female) | Quantitative |
| Rizwan 2014 | 10.7860/jcdr/2014/8278.4714 | India: northern | General (male), Special social conditions | Quantitative |
| Sharma 2018 | pesquisa.bvsalud.org/portal/resource/pt/sea-185340 | India: east Delhi | General (female) | Quantitative |
| Sherpa 2013 | PMID: 24971113 | India: Karnataka: Udupi District: Moodu Alevoor village | General (female) | Quantitative |
| Sood 2015 | ijmch.org/home/indian-journal-of-maternal-and-child-health-volume-17-april—december-2015 | India: Punjab, Amritsar | General (female) | Quantitative |
| Thulaseedharan 2018 | 10.2147/oajc.s152178 | India: Trivandrum district, Kerala | General (female) | Quantitative |
| Valsangkar 2012 | 10.4103/0970-1591.102704 | India: Karimnagar district, Andhra Pradesh | General (mixed gender) | Quantitative |
| Spagnoletti 2019 | 10.1080/17441730.2019.1578532 | Indonesia: Yogyakarta | General (female) | Qualitative |
| Titaley 2017 | 10.1016/j.midw.2017.07.014 | Indonesia: East Java, Nusa Tenggara Barat Provinces | Providers | Qualitative |
| Brunie 2019 | 10.1371/journal.pone.0216797 | Multicountry: India: New Dehli; Nigeria: Ibadan | General (female), Providers | Qualitative |
| Cartwright 2020 | 10.12688/gatesopenres.13045.2 | Multicountry: unspecified | Young people (mixed gender), Special social conditions | Mixed methods |
| Coffey 2006 | 10.1016/j.contraception.2005.10.017 | Multicountry: Mexico: Cuernavaca; South Africa: Durban; Thailand: Khon Kaen | General (mixed gender) | Quantitative |
| Cover 2013 | 10.1016/j.contraception.2016.10.007 | Multicountry: India: Lucknow, Uttar Pradesh; Uganda: Kampala | General (mixed gender) | Qualitative |
| Festin 2016 | 10.1093/humrep/dev341 | Multicountry: Thailand, Brazil, Singapore, Hungary | General (female) | Quantitative |
| Hooper 2010 | 10.2165/11538900-000000000-00000 | Multicountry: Australia; Brazil; France; Germany; Italy; Russia; Spain; United Kingdom; USA | General (female) | Quantitative |
| Machiyama 2018 | 10.1186/s12978-018-0514-7 | Multicountry: Kenya: Nairobi, Homa Bay; Bangladesh: Matlab | General (female), Special social conditions | Quantitative |
| Xu 2014 | 10.1016/j.fertnstert.2011.08.019 | Multicountry: China, Taiwan, Hong Kong, Indonesia, Malaysia, Pakistan, South Korea, Thailand | Menstrual Issues | Quantitative |
| Sapkota 2016 | 10.3389/fpubh.2016.00122 | Nepal: Kapibastu | General (female), General (male) | Mixed methods |
| Shrestha 2014 | 10.3126/kumj.v12i3.13718 | Nepal: Kathmandu: Dhulikhel | General (mixed gender), Postpartum | Quantitative |
| Santibenchakul 2016 | 10.5372/1905-7415.1003.485 | Thailand: Bangkok | General (female) | Quantitative |
Table 1A.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO African Region 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Schaan 2014 | 10.2989/16085906.2014.952654 | Botswana | PLHIV | Quantitative |
| Ajong 2018 | 10.1371/journal.pone.0202967 | Cameroon: Biyem-Assi | General (female) | Quantitative |
| Thomson 2012 | 10.1186/1471-2458-12-959 | Democratic Republic of the Congo: Idjwi Island | General (female) | Mixed methods |
| Alene 2018 | 10.1186/s12905-018-0608-y | Ethiopia: Amhara | PLHIV | Quantitative |
| Asfaw 2014 | 10.1186/1471-2458-14-566 | Ethiopia: Addis Ababa | PLHIV | Quantitative |
| Belda 2017 | 10.1186/s12913-017-2115-5 | Ethiopia: Oromia Regional State, Bale Eco-Region | General (female) | Quantitative |
| Both 2015 | 10.1016/j.rhm.2015.06.005 | Ethiopia: Addis Ababa | General (female) | Mixed methods |
| Davidson 2016 | 10.1007/s10995-016-2018-9 | Ethiopia | General (mixed gender), Special social conditions | Qualitative |
| Endriyas 2018 | 10.1186/s12884-018-1731-3 | Ethiopia: Southern Nations, Nationalities and People's Region | General (female), Providers | Mixed methods |
| Gebremariam 2014 | 10.1155/2014/878639 | Ethiopia: Tigray: Adigrat Town, Tigray | General (mixed gender), Providers | Qualitative |
| Keith 2014 | 10.1016/j.contraception.2013.12.010 | Ethiopia: Oromia Region (rural and peri-urban) | General (female), Providers | Qualitative |
| Tsehaye 2011 | 10.1155/2013/317609 | Ethiopia: Tigray Region: Shire Indaselassie Town | General (female) | Quantitative |
| Weldegerima 2008 | 10.1016/j.sapharm.2007.10.001 | Ethiopia: Fogera District: Woreta | General (female) | Quantitative |
| Adu 2018 | 10.4314/gmj.v52i4.3 | Ghana: Central Region | General (female) | Quantitative |
| Agyei-Baffour 2015 | 10.1186/s12978-015-0022-y | Ghana: Kumasi | General (male) | Mixed methods |
| Krakowiak-Redd 2011 | PMID: 22574499 | Ghana: Kumasi | General (female) | Quantitative |
| L'Engle 2011 | 10.1136/jfprhc-2011-0077 | Ghana: Accra | Women seeking emergency contraception | Qualitative |
| Opare-Addo 2011 | PMID: 21987939 | Ghana: Kumasi | General (female) | Quantitative |
| Osei 2014 | 10.1363/4013514 | Ghana: Accra | General (mixed gender), Previously had abortions | Qualitative |
| Rominski 2017 | 10.9745/GHSP-D-16-00281 | Ghana: Kumasi, Accra | General (female) | Quantitative |
| Staveteig 2017 | 10.1371/journal.pone.0182076 | Ghana: greater Accra | General (female) | Mixed methods |
| Teye 2013 | PMID: 24069752 | Ghana: Asuogyaman District | General (female) | Mixed methods |
| van der Geugten 2017 | 10.1007/s12119-017-9432-z | Ghana: Bolgatanga municipality | Young people (mixed gender), General (mixed gender) | Qualitative |
| Hubacher 2013 | 10.1016/j.contraception.2013.03.001 | Kenya: Nairobi | Postpartum | Quantitative |
| Hubacher 2015a | 10.1016/j.contraception.2015.01.009 | Kenya: Nairobi | Postpartum | Quantitative |
| Keesara 2017 | 10.1080/13691058.2017.1340669 | Kenya: Nairobi | Postpartum | Qualitative |
| Mayhew 2017 | http://dx.doi.org/10.1186/s12889-017-4514-2 | Kenya | PLHIV | Mixed methods |
| Ndegwa 2014 | PMID: 26859013 | Kenya: Embu | Pregnant | Quantitative |
| Newmann 2013 | 10.1155/2013/915923 | Kenya: Nyanza Province: Migori, Rongo, Siba districts: government-run HIV care and treatment clinics and patient support centers | Providers, PLHIV | Mixed methods |
| Odwe 2020 | 10.1016/j.conx.2020.100030 | Kenya: Homa Bay County | General (female), Special social conditions | Quantitative |
| Patel 2014 | 10.1089/apc.2014.0046 | Kenya: Nyanza Province: Kisumu East, Nyatike, Rongo, and Suba districts | PLHIV, General (male) | Qualitative |
| Roxby 2016 | 10.1136/jfprhc-2015-101233 | Kenya: Nairobi | General (mixed gender), PLHIV, Pregnant | Qualitative |
| Ruminjo 2005 | 10.1016/j.contraception.2005.04.001 | Kenya: Nairobi, Riruta, Thika | General (female) | Quantitative |
| Shabiby 2015 | 10.1186/s12905-015-0222-1 | Kenya: Naivasha (rural), Mbagathi (urban) districts | PLHIV, Postpartum, General (female) | Quantitative |
| Shapley-Quinn 2019 | 10.2147/IJWH.S185712 | Kenya: Kisuma; South Africa: Soshanguve | General (female) | Qualitative |
| RamaRao 2018 | 10.1111/sifp.12046 | Kenya, Nigeria, Senegal | Postpartum | Mixed methods |
| Chipeta 2010 | 10.4314/mmj.v22i2.58790 | Malawi: Mangochi district: Lungwena, Makanjira | General (mixed gender), Young people (mixed gender) | Qualitative |
| Haddad 2013 | 10.1016/j.contraception.2013.08.006 | Malawi: Lilongwe | PLHIV | Quantitative |
| Haddad 2014 | 10.1016/j.ijgo.2014.03.026 | Malawi: Lilongwe | PLHIV | Quantitative |
| O'Shea 2015 | 10.1080/09540121.2014.972323 | Malawi: Lilongwe | General (female), PLHIV, Postpartum | Quantitative |
| Brunie 2019 | 10.1371/journal.pone.0216797 | Multicountry: India: New Dehli; Nigeria: Ibadan | General (female), Providers | Qualitative |
| Burke 2014a | 10.1016/j.contraception.2014.01.009 | Multicountry: Senegal: Mbour, Thies, and Tivaouane; Uganda: Mubende, Nakasongola | Providers | Qualitative |
| Burke 2014b | 10.1016/j.contraception.2014.01.022 | Multicountry: Senegal; Uganda | General (female) | Quantitative |
| Callahan 2019 | 10.1371/journal.pone.0217333 | Multicountry: Burkina Faso; Uganda | General (female), General (male), Providers | Mixed methods |
| Cartwright 2020 | 10.12688/gatesopenres.13045.2 | Multicountry: unspecified | Young people (mixed gender), Special social conditions | Mixed methods |
| Chin-Quee 2014 | 10.1136/jfprhc-2013-100687 | Multicountry: Kenya: Nairobi; Nigeria: Lagos | General (female) | Quantitative |
| Coffey 2006 | 10.1016/j.contraception.2005.10.017 | Multicountry: Mexico: Cuernavaca; South Africa: Durban; Thailand: Khon Kaen | General (mixed gender) | Quantitative |
| Cover 2013 | 10.1016/j.contraception.2016.10.007 | Multicountry: India: Lucknow, Uttar Pradesh; Uganda: Kampala | General (mixed gender) | Qualitative |
| Lendvay 2014 | 10.1016/j.contraception.2013.11.002 | Multicountry: Kenya: Nairobi; Pakistan: Sindh, Punjab | General (female) | Quantitative |
| Machiyama 2018 | 10.1186/s12978-018-0514-7 | Multicountry: Kenya: Nairobi, Homa Bay; Bangladesh: Matlab | General (female), Special social conditions | Quantitative |
| Montgomery 2010a | 10.1007/s10461-009-9609-z | Multicountry: South Africa: Durban, Soweto; Zimbabwe: near Harare | General (female) | Quantitative |
| Nel 2016 | 10.1371/journal.pone.0147743 | Multicountry: Kenya; Malawi; South Africa; Tanzania | General (female) | Quantitative |
| Todd 2011 | 10.1007/s10461-010-9848-z | Multicountry: Brazil: Rio de Janiero; Kenya: Kericho; South Africa: Soweto | PLHIV | Qualitative |
| Tolley 2014 | 10.9745/GHSP-D-13-00147 | Multicountry: Kenya (peri-urban and urban sites); Rwanda (rural, peri-urban, and urban sites) | General (female), Providers | Qualitative |
| Urdl 2005 | 10.1016/j.ejogrb.2005.01.021 | Multicountry: Austria; Belgium; Finland; France; Germany; Hungary; Netherlands; Poland; South Africa; Switzerland | General (female) | Quantitative |
| Woodsong 2014 | 10.1111/1471-0528.12875 | Multicountry: Malawi: Lilongwe; Zimbabwe: Harare | General (mixed gender), Providers | Qualitative |
| Mayaki 2014 | 10.1080/02646838.2014.888545 | Niger | General (female) | Quantitative |
| Aisien 2010 | PMID: 20857796 | Nigeria: Edo State: Benin-City | General (female) | Quantitative |
| Egede 2015 | 10.2147/PPA.S72952 | Nigeria: Ebonyi State: Abakaliki | General (female) | Quantitative |
| Ezugwu 2019 | 10.1002/ijgo.13027 | Nigeria: Enugu | Postpartum | Quantitative |
| Iyoke 2014 | 10.2147/PPA.S67585 | Nigeria: Enugu | General (mixed gender) | Quantitative |
| Lanre-Babalola 2015 | proquest.com/scholarly-journals/dynamics-knowledge-use-preference-birth-control/docview/1709681040/se-2?accountid=11752 | Nigeria: Ibadan | General (female) | Quantitative |
| Okunlola 2006 | 10.1080/01443610600613516 | Nigeria: Ibadan | General (female), Young people (female) | Quantitative |
| Olajide 2014 | PMID: 25022145 | Nigeria: Osun State; primary and secondary schools | Young people (mixed gender), Other special medical conditions | Quantitative |
| Orji 2005 | 10.1080/13625180500331259 | Nigeria: Southwest | Young people (mixed gender) | Quantitative |
| Sodje 2016 | 10.1016/j.ijgo.2016.05.005 | Nigeria: Edo, Delta, Anambra, Ebonyi, Abia states | Postpartum | Quantitative |
| Sunmola 2005 | 10.1080/09540120412331319732 | Nigeria: Ibadan | Young people (mixed gender) | Quantitative |
| Ujuju 2011 | 10.1111/j.1466-7657.2011.00900.x | Nigeria: Katsina state: Rimi, Katsina, Kaita; Enugu state: Nkanu West, Enugu East, Igbo-Etiti | Providers, General (mixed gender) | Qualitative |
| Kestelyn 2018 | 10.1371/journal.pone.0199096 | Rwanda: Kigali | General (female) | Mixed methods |
| Shattuck 2014 | 10.1016/j.contraception.2014.02.003 | Rwanda | General (mixed gender), Vasectomies | Quantitative |
| Leye 2015 FRENCH | PMID: 26164961 | Senegal: Diourbel region: Mbacke district | General (female) | Mixed methods |
| Crede 2012 | 10.1186/1471-2458-12-197 | South Africa: Cape Town: Khaylitsha and Mitchell's Plain | Postpartum, PLHIV | Quantitative |
| de Bruin 2017 | 10.1080/09540121.2017.1327647 | South Africa | Young people (mixed gender) | Qualitative |
| Harries 2019 | 10.1186/s12978-019-0830-6 | South Africa: Western Cape | General (female) | Qualitative |
| Joanis 2011 | 10.1016/j.contraception.2010.08.002 | South Africa: Durban | General (female) | Quantitative |
| Laher 2009 | 10.1007/s10461-009-9544-z | South Africa: Soweto | PLHIV | Qualitative |
| Mahlalela 2016 | 10.11564/30-2-873 | South Africa: Durban | general (female) | Qualitative |
| Morroni 2006 | 10.1016/j.contraception.2006.01.005 | South Africa: Western Cape Province | General (female) | Quantitative |
| Ndinda 2017 | 10.3390/ijerph14040353 | South Africa: Kwa-Zulu-natal (rural) | General (mixed gender) | Qualitative |
| Schwartz 2016 | 10.1177/0956462415604091 | South Africa: Johannesburg | General (mixed gender), PLHIV | Qualitative |
| Smit 2006 | 10.1016/j.contraception.2005.10.019 | South Africa: KwaZulu-Natal: Durban | General (female), Special social conditions | Quantitative |
| Mathenjwa 2012 | 10.3109/13625187.2012.694147 | Swaziland: Lavusima | special social conditions | Qualitative |
| Ziyane 2006 | 10.4102/hsag.v11i1.213 | Swaziland | Young people (mixed gender) | Qualitative |
| Bunce 2007 | 10.1363/3301307 | Tanzania: Kigoma Region | Vasectomies, General (mixed gender) | Qualitative |
| Cooper 2019 | 10.1111/mcn.12735 | Tanzania: Mara, Kagera | General (mixed gender), Postpartum, Providers | Qualitative |
| Rusibamayila 2016 | 10.1080/13691058.2016.1187768 | Tanzania: Kilombero District | General (mixed gender), Providers | Qualitative |
| Sato 2020 | 10.1080/26410397.2020.1723321 | Tanzania: Arusha Region | General (female) | Quantitative |
| Sheff 2019 | 10.1186/s12978-019-0836-0 | Tanzania: Kilombero, Rufiji, and Ulanga | General (mixed gender) | Qualitative |
| Akol 2014 | 10.9745/ghsp-d-14-00085 | Uganda: multiple sites | Providers, General (mixed gender) | Quantitative |
| Byamugisha 2010 | 10.3109/00016341003611220 | Uganda: Kampala | Women seeking emergency contraception | Quantitative |
| Cover 2017 | 10.1363/3919513 | Uganda: Gulu district, Mubende | General (female) | Quantitative |
| Higgins 2014 | 10.2105/AJPH.2007.115790 | Uganda: Rakai District | Young people (mixed gender) | Qualitative |
| Kabagenyi 2016 | 10.11604/pamj.2016.25.78.6613 | Uganda: Mpigi, Bugiri (rural) | General (mixed gender) | Qualitative |
| Kakaire 2016 | 10.3109/13625187.2016.1146249 | Uganda: Kampala | PLHIV | Quantitative |
| Lester 2015 | 10.1016/j.contraception.2014.12.002. Epub 2014 Dec 12.; ID: 106 | Uganda: Kampala | Pregnant | Quantitative |
| Mbonye 2012 | 10.1258/ijsa.2009.009357 | Uganda: Central region (rural, semi-urban, and urban) | PLHIV, General (mixed gender) | Mixed methods |
| Nattabi 2011 | 10.1186/1752-1505-5-18 | Uganda: Gulu health facilities | Special social conditions, PLHIV | Mixed methods |
| Paul 2016 | 10.3402/gha.v9.30283 | Uganda: Central region (rural, semi-urban, and urban) | Providers | Qualitative |
| Polis 2014 | 10.1016/j.contraception.2013.11.008 | Uganda: Rakai | PLHIV | Quantitative |
| Wanyenze 2013 | 10.1186/1471-2458-13-98 | Uganda: Kampala | PLHIV | Qualitative |
| Montgomery 2010b | 10.1186/1758-2652-13-30 | Zimbabwe: Epworth | General (female) | Quantitative |
| van der Straten 2010 | 10.1783/147118910790290966 | Zimbabwe: Harare | Young people (female) | Mixed methods |
| van der Straten 2012 | 10.1007/s10461-012-0256-4 | Zimbabwe: Harare: peri-urban township | General (female) | Mixed methods |
Table 1F.
Summary characteristics of articles included in the contraceptive values and preferences global systematic review which were conducted in countries in the WHO Western Pacific Region 2005-2020
| Author year | DOI | Location | Population | Study design |
|---|---|---|---|---|
| Bateson 2016 | 10.1111/ajo.12534 | Australia: New South Wales: Queensland | General (female) | Quantitative |
| Dixon 2014 | 10.3109/13625187.2014.919380 | Australia | General (female) | Qualitative |
| Garrett 2015 | 10.1186/s12905-015-0227-9 | Australia | Young people (female), Providers | Qualitative |
| Inoue 2017 | 10.1136/jfprhc-2014-101132 | Australia: New South Wales | General (female) | Qualitative |
| Kelly 2016 | 10.1136/jfprhc-2015-101356 | Australia: New South Wales: Sydney | Providers | Qualitative |
| Knox 2012 | 10.1016/j.socscimed.2012.12.025 | Australia | General (female), Providers | Quantitative |
| Knox 2013 | 10.2165/11598040-000000000-00000 | Australia | General (female) | Quantitative |
| Larkins 2007 | 10.5694/j.1326-5377.2007.tb01025.x | Australia: New South Wales: Queensland | Young people (mixed gender), Special social conditions | Quantitative |
| Mills 2006 | 10.1080/07399330600629468 | Australia | General (female) | Qualitative |
| Olsen 2014 | 10.1186/1472-6874-14-5 | Australia | PWID | Qualitative |
| Ong 2013 | 10.1363/4507413 | Australia: Victoria | General (female) | Quantitative |
| Philipson 2011 | 10.1089/jwh.2010.2455 | Australia | General (female) | Quantitative |
| Russo 2020 | 10.1080/13691058.2019.1643498 | Australia: Victoria: Melbourne | Special social conditions, General (mixed gender) | Qualitative |
| Watts 2014 | 10.1093/jrs/feu040 | Australia: Victoria: Melbourne | Providers, Young people (female), Pregnant | Qualitative |
| Weisberg 2005a | 10.1016/s1701-2163(16)30462-5 | Australia: New South Wales: Queensland; South Australia | General (female) | Quantitative |
| Weisberg 2013 | 10.3109/13625187.2013.777830 | Australia | General (female), providers | Quantitative |
| Weisberg 2014 | PMID: 16113711 | Australia: New South Wales | General (female) | Quantitative |
| Wigginton 2016 | 10.1136/jfprhc-2015-101184 | Australia | Young people (female) | Qualitative |
| Wong 2009 | 10.1016/j.contraception.2009.03.021 | Australia: Victoria | General (female) | Quantitative |
| Thyda 2015 | 10.1097/QAI.0000000000000635 | Cambodia: Chhouk Sar | PLHIV | Quantitative |
| Hou 2010 | 10.1016/j.ijgo.2009.09.020 | China: Guandong Province: Enping City | Special social conditions | Quantitative |
| Nian 2010 | PMID: 21073077 | China: Sichuan Province | Providers, General (mixed gender), Vasectomies | Qualitative |
| Cartwright 2020 | 10.12688/gatesopenres.13045.2 | Multicountry: unspecified | Young people (mixed gender), Special social conditions | Mixed methods |
| Crosby 2013 | 10.1258/ijsa.2008.008120 | Multicountry (online): mostly USA; Australia; Canada; New Zealand; United Kingdom; Western Europe | General (mixed gender) | Quantitative |
| Festin 2016 | 10.1093/humrep/dev341 | Multicountry: Thailand, Brazil, Singapore, Hungary | General (female) | Quantitative |
| Gemzell-Danielsson 2012 | 10.1016/j.contraception.2012.06.002 | Multicountry: Australia, Brazil, Canada, France, Germany, Korea, Mexico, Spain, Sweden, United Kingdom | Providers | Quantitative |
| Xu 2014 | 10.1016/j.fertnstert.2011.08.019 | Multicountry: China, Taiwan, Hong Kong, Indonesia, Malaysia, Pakistan, South Korea, Thailand | Menstrual Issues | Quantitative |
| Roke 2016 | 10.1071/HC15040 | New Zealand | General (female) | Quantitative |
| Rose 2011 | 10.1089/jwh.2010.2658 | New Zealand: Wellington | Women seeking abortion services, Young people (female) | Qualitative |
| Terry 2011 | 10.1177/0959353511419814 | New Zealand | Vasectomies | Qualitative |
| Gupta 2017 | 10.1111/ajo.12596 | Papua New Guinea: Madang Island, Milne Bay (mainland) | General (female) | Quantitative |
| Lee 2019 | 10.5468/ogs.2019.62.3.173 | South Korea | Providers | Quantitative |
| Park 2011 | 10.2147/IJWH.S26620 | Vietnam: Thai Nguyen, Khanh Hoa, Vinh Long provinces | General (female) | Quantitative |
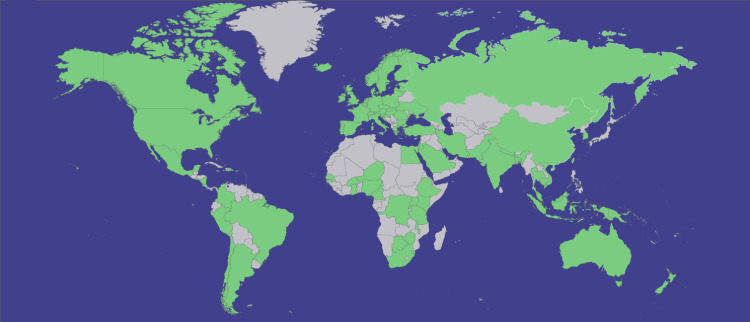
Studies were conducted in 93 countries (Fig. 2). Fifty-one articles reported data from multiple countries, mostly in Europe; 10 articles were from the 11-country European CHOICE study. All 6 WHO regions1 were represented: the African Region (AFRO) (n = 103), the Region of the Americas (PAHO) (n = 172), the South-East Asia Region (SEARO) (n = 27), the European Region (EURO) (n = 99), the Eastern Mediterranean Region (EMRO) (n = 14), and the Western Pacific Region (WPRO) (n = 34). A plurality of articles reported studies that took place in the USA (n = 139), followed by the United Kingdom (n = 29) and Australia (n = 23). Most articles reported studies that were primarily conducted in high-income countries (n = 250), but studies were also conducted in upper-middle (n = 67), lower-middle (n = 78), and low- (n = 44) income countries as classified by the World Bank. (Note: numbers do not add to 423 because of studies taking place in multiple countries.)
Fig. 2.
Countries where studies presenting primary data on contraceptive values and preferences were conducted. Sources were published between January 2005 and July 2020. Green indicates data available; gray, data not identified.
While most articles presented quantitative findings (269/423, 63%), 121 (29%) used qualitative methods, and 34 (8%) used mixed- or multimethods. A range of study designs and methods were used: the most common quantitative design was cross-sectional surveys (n = 190), followed by qualitative in-depth interviews (n = 116) and focus group discussions (n = 69); however, prospective cohort studies, randomized trials, and other observational designs were also represented. The mixed/multimethods studies generally involved a cross-sectional quantitative survey with additional qualitative analysis of open-ended survey responses or additional data collection from focus group discussions or in-depth interviews.
3.3. Risk of bias varied by study design.
We generally found that studies involving qualitative analyses presented the 9 rigor domains assessed by the Critical Appraisal Skills Programme qualitative checklist. Cross-sectional studies generally did not include comparison groups (22%); of those which did, only a few compared across sociodemographic characteristics (16%) or outcomes (5%). Studies employing quantitative analyses sometimes followed participants over time (36%), used a control or comparison group (39%), or compared outcomes pre- and postexposure to a contraceptive method (19%). Quantitative studies rarely randomly selected participants for assessment (15%) or randomly allocated participants to the intervention or control arm (if applicable) (14%). Of quantitative studies that followed participants over time (n = 90), 55 (61%) had a follow-up rate of 80% or more. Of quantitative studies including a control or comparison group (n = 106), 35 (33%) compared groups across sociodemographic characteristics and 6 (5%) compared groups on outcome measures at baseline.
The articles explored the values and preferences of contraceptive users in the general female population (n = 220), general male population (n = 10), general population (not disaggregating between male and female participants) (n = 44), women with specific reproductive health experiences (n = 52), adolescents and young adults (n = 76), people living with HIV (n = 22), sex workers (n = 6), transmasculine individuals (n = 1), people who inject drugs (n = 2), and those living in humanitarian contexts (n = 4), as well as perspectives of health workers (n = 53) (Table 2). (Note: numbers do not add to 423 because some articles included perspectives from multiple population groups.) Separate systematic reviews examining the values and preferences of women with specific reproductive health experiences (i.e., pregnant, postpartum, seeking emergency contraception, or seeking abortion) [9], adolescents and young adults [7], people living with HIV [10], other end-users in specific circumstances (i.e., sex workers, transmasculine individuals, people who inject drugs, and those living in humanitarian contexts) [8], and health workers [11] are published in this same journal issue.
Table 2.
Number of articles included in the contraceptive values and preferences global systematic review that provide data on different populations 2005-2020
| Population category | Number of articlesa (% out of 423 total included articles) |
|---|---|
| General population | |
| Female contraceptive users | 220 (52%) |
| Male contraceptive users | 10 (2.4%) |
| Both male and female (not disaggregated by gender) | 44 (10.4%) |
| Women with specific reproductive health experiences | |
| Women who are nulliparous | 4 (0.9%) |
| Women who are pregnant | 7 (1.7%) |
| Postpartum women | 23 (5.4%) |
| Women seeking abortion services | 7 (1.7%) |
| Women seeking emergency contraception | 5 (1.2%) |
| Women who previously had abortion(s) | 6 (1.4%) |
| Adolescents and young adults | |
| Female young people | 55 (13%) |
| Male young people | 2 (0.5%) |
| Both male and female (not disaggregated by gender) | 19 (4.5%) |
| People in specific social conditions or humanitarian settings | |
| People living with HIV | 22 (5.2%) |
| Sex workers | 6 (1.4%) |
| Transmasculine individuals | 1 (0.2%) |
| People who inject drugs | 2 (0.5%) |
| Those living in humanitarian contexts | 4 (0.9%) |
| Health workers | 53 (12.5%) |
Studies that reported any findings on contraceptive values and preferences for this specific population group. Note that studies often reported data for multiple population groups, so percentages do not add up to 100.
Included articles mentioned end-users' and health workers’ values and preferences related to all of the methods covered by WHO's guidelines, including male condoms (n = 161), female condoms (n = 41), oral contraceptive pills, i.e., combined oral contraceptive pills (n = 204) and progestogen-only pills (POP) (n = 105), intrauterine devices (IUD) or hormone-releasing intrauterine systems (IUS) (n = 221), implants (n = 139), injectable contraceptives (n = 140), diaphragm (n = 37), vaginal ring (n = 82), transdermal patch (n = 74), male sterilization or vasectomy (n = 39), female sterilization or tubal ligation (n = 72), fertility awareness-based methods (e.g., rhythm method, calendar method) (n = 64), emergency contraception (n = 42), withdrawal (n = 67), and other contraceptive methods, including abstinence, lactational amenorrhea method, and other (often unspecified) traditional methods (n = 42).
3.4. Commonly reported values among contraceptive users
Contraceptive users across geographic regions and population subgroups consistently prioritized several thematic issues (Table 3). Overall, people wanted choice: they desired a range of options from which to choose, especially since different people preferred different methods at different times for different reasons.
Table 3.
Common themes related to values and preferences, listed in order of frequency, described by articles included in the contraceptive values and preferences global systematic review 2005-2020
| Values and preferences themes | Number of articles (% out of 423 total included articles) |
|---|---|
| Side effects and safety | 246 (58.2%) |
| Method effectiveness/reliability | 191 (45.2%) |
| Ease, duration, or frequency of use | 179 (42.3%) |
| Noninterference in sex and partner relations | 141 (33.3%) |
| Effects on menstruation | 83 (19.6%) |
| Cost/affordability | 71 (16.8%) |
| Control and autonomy | 67 (15.8%) |
| Private, discreet, or covert use | 50 (11.8%) |
Side effects and safety was the most commonly reported issue (mentioned in 246 articles) when considering contraceptive methods. Contraceptive users and health workers were concerned about pain. They desired minimal side effects or adverse events (relating to changes in libido, bleeding, menstrual cycles, acne, weight gain, etc.); if these were unavoidable, they wanted to be able to anticipate, manage, and tolerate side effects. Women often asked how commonly used contraceptive methods were, and how safe or healthy they were.
Method effectiveness and reliability were the next most commonly reported (mentioned in 191 articles), especially for preventing pregnancy (e.g., “security in not getting pregnant” [36], “having had a false alarm [about pregnancy] in the past” [37]), but also for providing dual protection against HIV and other STIs [38]. Women in some studies expressed interest in contraceptive methods that were effective, despite experiencing uncomfortable side effects like vomiting or diarrhea. Participants expressed varying acceptability levels for percent efficacy—or conversely, varying tolerance levels for likelihood of contraceptive failure.
Ease and duration/frequency of use (mentioned in 179 articles) was also very important. Many people desired contraceptive methods that were comfortable or convenient to use. Conversely, others expressed fears of the contraceptive method “falling off” [39] or forgetting to use or administer it. One hundred forty-four articles mentioned accessibility as a factor in their contraceptive preference, considering logistical issues in getting advice on, obtaining, maintaining, or changing contraceptive methods. Reversibility was very important to current and hypothetical contraceptive users (mentioned in 73 articles), both in terms of duration of contraceptive effectiveness and frequency of use (whether taken once a day, administered weekly or monthly or longer, or a permanent contraceptive method) and how difficult it was to start, switch, or stop the contraceptive method (e.g., stop taking a daily oral contraceptive pill versus getting an IUD removed). Women preferred choosing a method that “they are in control of stopping” [40]. For many women, it was important that they be able to resume fertility immediately after discontinuation or at least that using a contraceptive method for a period of time would not “affect the ability to have children in the future” [41].
A contraceptive method's noninterference in sex and partner relations was valued as well, mentioned in 141 articles. Contraceptive users often reported considering whether they or their partner(s) could feel the contraceptive method/device during intercourse, and how the contraceptive method affected the spontaneity, pleasure, and frequency of sex. Partner's influence towards women's contraceptive choice was also highlighted, where oftentimes “[m]en's disapproval over contraceptive use restricted preferences for women” [42], particularly in low- and middle-income countries regarding “non-natural” or hormonal contraceptives. Even in the USA, though, young women mentioned using withdrawal because of their male partners, though it “did not align with their own contraceptive desires,” since using a condom would imply lack of trust or relationship intimacy and they were embarrassed about using withdrawal as a contraceptive method [43].
Women were concerned about the impact of hormonal contraceptives on menstruation (mentioned in 83 articles), whether they desired regular menstrual cycles (to alleviate dysmenorrhea) or amenorrhea (to stop menstrual bleeding altogether for a specified time) or pain relief during menses; for example, a multimethod study in the US found contraceptive choice linked to menstrual control, suppression, and symptoms [44]. Some preferred “natural” or “nonartificial” nonhormonal methods in order to retain menstruation as a tangible symbol of health and fertility [45].
Cost—the financial burden to pay for the contraceptive method itself and the services of a health worker, in addition to time and transport/distance—was important to users (reported in 71 articles). Two-thirds of the mentions of cost/affordability/accessibility appeared in articles originating from the USA and other high-income countries, with two-thirds of such articles (29/45, 64%) discussing LARCs. However, among articles that ranked the contraceptive attributes that end-users considered important, cost/affordability usually ranked below effectiveness and side effects.
In 67 articles, people expressed the desire to have a sense of control and autonomy over contraceptive decision-making or usage. For example, one article noted that users wanted to make the choice of birth control method that was “right for them when given the proper information and options” [36]. In choosing a contraceptive method, women also considered whether they needed a health worker to insert/remove or administer the method or if they could self-administer—and what training or education was needed prior to use (e.g., demonstration, training, supervision, product storage, waste management).
Fifty articles highlighted that women also wanted the ability to use a contraceptive method discreetly, privately, or covertly, without others—whether partners, family members, or community members—being able to discern which, if any, contraceptive method they were using. This is particularly significant for contraceptive methods that may be easily observable by others (e.g., patches, sub-dermal implants), for which contraceptive visibility could jeopardize the end-user's physical safety in some extreme cases [46].
Contraceptive values and preferences varied across the 6 WHO regions. Across the 3 regions in which included articles were most commonly conducted (AFRO, EURO, and PAHO), clients most typically reported side effects to be the most important issue when deciding which contraceptive method to use. The least commonly reported feature was cost/access in AFRO, privacy/discretion/covert use in PAHO, and control/autonomy in EURO. In AFRO, EURO, and PAHO, the most preferred options of contraceptive methods were the injection, pill, and IUD. The least preferred choice in PAHO and EURO was male sterilization, while the patch was least preferred in AFRO.
Contraceptive values and preferences also varied by country income level as classified by the World Bank. Across all income levels, side effects followed by effectiveness, ease of use, and duration were the most commonly reported issues considered by clients when deciding what contraceptive method to use. In high- and upper-middle-income countries, privacy/discretion/covert use was the least commonly reported factor, while control/autonomy was the least commonly reported factor in low- and lower-middle income countries. Where studies reported rankings of contraceptive methods, the most preferred contraceptive choice was IUDs in high-income countries, male condoms in upper-middle-income countries, the combined oral contraceptive pill in lower-middle-income countries, and injectable contraceptives in low-income countries, while the least preferred contraceptive method was male sterilization in high-income countries and the patch in lower-middle and low-income countries.
3.5. Preferences for specific contraceptive methods
Preferences for specific contraceptive methods varied by country and population subgroup. Preferences depended on people's knowledge of contraceptive methods—both knowledge of what options are available, and general awareness of how those methods work.
Oral contraceptive pills and male condoms are 2 of the predominant methods globally, according to an international cross-sectional survey on women’s attitudes regarding hormonal contraception [47]. Oral contraceptive pills accounted for around half of all contraceptive users and were typically the first mode of contraception ever used by women. Condoms and withdrawal (coitus interruptus) were often used alongside or as backup for other contraceptive methods at various times throughout the life course, especially for those who had had bad experiences with other contraceptive methods. Use of these methods was frequently dependent on perceived relationship commitment and stability. Use of emergency contraception correlated strongly with the individual user's (or health worker's) view of when life begins.
Study participants often contrasted modern (hormonal) with traditional (“natural,” often barrier) contraceptive methods. Women in some studies described distrust in hormonal contraception and wanting to “take a break” or “detox” [48] from their contraceptive method. When considering intrauterine contraception or vaginal rings, many expressed negative feelings, concerns, fears, or discomfort with having “something in [my] body” [49], the notion or sensation of a “foreign body” or “foreign object” [50], or having something potentially “get lost inside of me” [51]. Among quantitative studies, between 22% [50] and 53% [52] of participants reported these types of IUD-related concerns.
Most contraceptive users wanted a contraceptive method that fit into their lifestyle, and that was supported by their culture, religious beliefs, government, and community norms. Many people used familiarity to choose a contraceptive method, asking questions like, “Do I know anyone else who uses it?” [27]. In choosing a method, people often used the process of elimination, determining what contraceptive methods they did not want to use based on their own past personal experiences or “the stories of close friends or family, whose experiences were often valued as if they were a women's own” [53]. However, once a contraceptive method was chosen, people tended to have high satisfaction with (ranging from 42.5% among women experiencing idiopathic menstrual bleeding after a 3-month trial using combined oral contraceptive pills [54] to 100% among 24–45-year-old women using the implant [55], with a majority of quantitative studies measuring satisfaction, likelihood of recommendation to others, or desire to continue reporting in the 80%–95% range) what they chose.
3.6. Role of counseling in contraceptive choice
Counseling plays an important role in the selection of contraceptive method. Seventy-four of the included articles mentioned the impact of counseling or interactions with health workers on contraceptive choice. Several studies showed that counseling can cause a substantial percentage (33%–50%) of women to change their contraceptive method selection and that it can enable undecided women to make a selection. Research has particularly focused on the effect of counseling in moving women from an intention to use oral contraceptive pills to trying another method, such as the patch or ring [20,21,56].
Ten articles came from one large multicountry study: the Contraceptive Health Research Of Informed Choice Experience (CHOICE) study [20–29]. The CHOICE study was conducted between 2009 and 2010 among 18,787 women in 11 countries: Austria, Belgium, the Czech Republic, Slovakia, the Netherlands, Poland, Russia, Sweden, Switzerland, Ukraine, and Israel. Women who expressed an interest in combined hormonal contraceptives were recruited into the study and asked about their contraceptive preferences. Health workers then used standardized approaches to counsel women on the pill, the patch, and the ring. Women's final contraceptive selection was recorded along with their reasons for this preference and their perceptions of the attributes of each method. Participants described a wide range of preferences for contraceptive method and rationale, with the greatest variability explained by country of residence, followed by health workers’ gender, age, and more frequently recommended method [20]. Preference choice was also associated with the woman's age, educational level, prior unintended pregnancy experience, relationship status, and last contraceptive method. Prior to entering the study, women reported using combined oral contraceptive pills (42%), condoms (25%), and natural family planning (6%); 10% were not using any contraceptive measures [21]. At the start of the study, before receiving counseling, women's contraceptive intentions leaned toward the pill (52%), with only 5% intending to use the patch and 8% the ring; 10% wanted to use another method, and 26% were undecided. Nearly half of the counseled women selected a contraceptive choice different from the method they originally intended to use [20]. After counseling, women chose the pill slightly less (51%) and were more likely to select alternative methods like the patch (8%) and the ring (30%), though the distribution varied by country [21].
Among women choosing between the pill, patch, and ring in the European CHOICE study [23,25,26], intensive counseling significantly decreased the proportion of undecided women and significantly increased the proportion of women choosing the ring (from less than 10% pre-counseling to 23.8%–42.6% postcounseling, p < 0.001) though pill and patch intention/usage remained fairly consistent (around 50% and less than 10% respectively). Women who stayed with oral contraceptive pills cited ease of use and familiarity as their primary reasons, while women who switched to the patch and ring cited reasons like ease of use, decreased frequency of use (and thus less opportunity to forget, i.e., lower probability of omission), and effectiveness when experiencing vomiting/diarrhea/illness. Other than the European CHOICE study, several other papers provided information on the value and role of counseling [[56], [57], [58], [59], [60], [61]–62].
Contraceptive users typically felt they should make the final decision about which contraceptive method they should use but appreciated health worker recommendations and assistance in determining the best method. They preferred caring, less formal relationships with their health workers and prioritized access to comprehensive information, including about alternative methods and side effects, presented both verbally (e.g., face-to-face) and in writing (e.g., internet, books, pamphlets). Before counseling, users were often dissatisfied with the information they had received about family planning methods and less than half reported a high level of confidence in their knowledge of the risks, benefits, and side effects, Clients preferred health workers who engaged with them in “an interactive, appropriately targeted manner” [63], taking into account contextual factors that could influence method choice and giving messages that included personal decision-making language (informative but not commanding). Younger women were more accepting of medical opinion, while older women rejected medical interference in contraceptive decisions and could be quite critical of medical practitioners and their practices. Training and counseling were also important to address users' reservations and concerns. For methods that are new to a user, clients reported that it was helpful to receive practical guidance and support from health workers. For example, adolescents at a family planning clinic in the USA were given demonstrations using sample vaginal rings and diagrams of the vagina; the first time they used the ring, they self-inserted at the clinic, sometimes with the health worker's help, and thereafter at home [64].
4. Discussion
In this global review, we found a large literature documenting diverse values and preferences about contraceptive methods. Across 423 articles from 93 countries in all regions of the world, we found that values centered on themes of choice, ease of use, side effects, and effectiveness. Many users also considered factors such as cost, availability, interference in sex and partner relations, the effect of hormonal contraceptives on menstruation, and interactions with health workers as aspects they valued in their decisions. Preferences for specific contraceptive methods varied between individual women, as well as across settings, geographic regions, cultures, population subgroups, and which options were considered or available. Users generally reported satisfaction with (and more accurate knowledge about) the methods they were using.
Family planning counseling can play an important role in clients' choice of contraceptive method. Contraceptive users were generally open to discussion about options, risks and benefits, timing, and side effects, though they usually wanted to personally make their own decision with input from health workers and from their partner(s), family, and community. Health workers require training to be able to provide complete, accurate information and provision of all potential method choices to their clients.
Studies were diverse across populations, geographic settings, contraceptive methods, and study designs. The majority of studies were conducted among adult or adolescent women in the general population. Fewer studies were conducted among women with specific demographic, health, or social considerations. While there were a small number of studies among men, most focused on male-controlled methods of contraception rather than covering contraceptive methods more broadly. This perhaps does not reflect the full potential for male involvement in family planning programs as clients, supportive partners, and agents of change [65]. While studies most commonly came from the USA, Europe, and Australia, there was representation from all regions of the world. However, the diversity of populations and specific contraceptive methods covered prevented us from being able to make definitive comparisons of values and preferences across regions. We identified articles on all 26 contraceptive methods covered by the WHO guidelines, and articles covered a range of appropriate quantitative and qualitative study designs. In these regards, we found few obvious gaps in the literature. We also conducted more focused reviews to delve into the values and preferences of several populations of interest [7–11], using subsets of articles identified in this global review.
Our review has some limitations. While we attempted to conduct a comprehensive search, there was some inherent subjectivity in determining what counted as a study of values and preferences, and we thus may have missed some articles that should have been included. For example, we included only one article on values and preferences of transgender people; however, a recent review also examines perspectives of this population in more detail [66]. We also encountered significant challenges synthesizing such a complex topic at the global level. Regardless of study design, the investigators of specific studies often framed their questions around a limited number of values and preferences, so the themes we discuss in this review (presented by frequency of mention in the 423 included articles) may in part reflect the values and preferences most commonly queried, and some studies explored only a very select set of values/preferences. Our findings are ultimately limited by what was presented in the included articles. Finally, quality of the included studies varied (e.g., some studies had very small sample sizes, and others had nonrepresentative samples, limiting generalizability), and our overall findings are only as strong as the studies on which they are based.
Family planning programs around the world share the goals of improving access to effective contraceptive methods and supporting the reproductive rights of women and men. WHO human rights guidelines recommend ensuring accessibility, acceptability, meaningful participation, and informed decision-making in the provision of contraceptive information and services [67]. Understanding values and preferences that end-users and health workers hold towards different contraceptive methods will help to inform the development of such rights-based, person-centered services that support contraceptive users and their partners in making decisions that are right for them.
In summary, contraceptive users value having a range of contraceptive methods from which to choose and prefer methods that are efficacious, easy to use, and have few side effects. Users desire control over the final choice of which contraceptive method to use, with the guidance of health workers who explore their values and preferences. They want comprehensive information about available methods and side effects. This review uncovered wide variability in values and preferences within and across studies. Context and available options shape people's values and preferences, emphasizing the need for high-quality counseling
Data request
An online repository of data abstracted from included articles is provided in the Appendix. For specific full-text articles or additional information, please contact the corresponding author.
Acknowledgments
We would like to thank the 2014 WHO Medical Eligibility Criteria for Contraceptive Use Guidelines Development Group and 2016 WHO Technical Consultation on Hormonal Contraception and HIV Group for their inputs. We also thank the Johns Hopkins Bloomberg School of Public Health and School of Medicine graduate students, staff, and faculty (Melissa Alamo, Afia Amoah, Anne Burke, Anita Dam, Priyanka Das, Amalia Debrosse, Avani Duggaraju, Nicole Garbarino, Laura Graf, Belinda Jivapong, Huneid Kautsar, Jingjia (Cynthia) Li, Jessica Lin, Shea Littlepage, Jaime Marquis, Habibat Oguntade, Shristi Pandey, Kate Perepezko, Molly Petersen, Caitlin Quinn, Tasfia Rahman, Kathleen Ridgeway, Eric Rodriguez, Joseph (Gregory) Rosen, Haneefa Saleem, Komal Soin, and Jeslyn Tengkawan) and colleagues from the United States Centers of Disease Control and Prevention Division of Reproductive Health (Kate Curtis, Isabel Morgan, and Angeline Ti), World Health Organization (Antonella Lavelanet) and elsewhere (Christina Ge, Rachel Logan, and Jessika Ralph) who contributed to the searching, screening, and data abstraction process.
Footnotes
Declaration of competing interest: None.
Funding: This manuscript was developed with the support of the UNDP-UNFPA-UNICEF-WHO-World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), a cosponsored program executed by the World Health Organization (WHO). This manuscript is made possible by the generous support of the American people through the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) through an interagency agreement with the United States Agency for International Development (USAID), cooperative agreement #No. AID-OAA-A-15-00045. The contents of this paper are the sole responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
The World Health Organization comprises of 150 country offices and other offices around the world serving 194 Member States across six regional offices, https://www.who.int/about/structure.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.contraception.2022.04.011.
Appendix. Supplementary materials
References
- 1.Altshuler AL, Gaffield ME, Kiarie JN. The WHO's medical eligibility criteria for contraceptive use: 20 years of global guidance. Curr Opin Obstet Gynecol. 2015;27:451–459. doi: 10.1097/GCO.0000000000000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO . 5th ed. World Health Organization; Geneva, Switzerland: 2015. Medical eligibility criteria for contraceptive use.https://www.who.int/reproductivehealth/publications/family_planning/MEC-5/en/ Available at. [PubMed] [Google Scholar]
- 3.WHO . 3rd ed. World Health Organization; Geneva, Switzerland: 2016. Selected practice recommendations for contraceptive use.https://www.who.int/reproductivehealth/publications/family_planning/SPR-3/en/ Available at. [PubMed] [Google Scholar]
- 4.WHO . 2nd ed. World Health Organization; Geneva, Switzerland: 2014. WHO handbook for guideline development. [Google Scholar]
- 5.Gaffield ME, Kiarie J. Setting global standards: The paramount importance of considering contraceptive values and preferences of clients and providers. Contraception. 2022;111:1–2. doi: 10.1016/j.contraception.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kennedy CE, Yeh PT, Gaffield ME. Contraception values and preferences: protocol and methods for a global systematic review. Contraception. 2020;101:69–73. doi: 10.1016/j.contraception.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 7.Ti A, Soin K, Rahman T, Dam A, Yeh PT. Contraceptive values and preferences of adolescents and young adults: a systematic review. Contraception. 2022;111:22–31. doi: 10.1016/j.contraception.2021.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Lavelanet AF, Ralph JA, Ti A, Duggaraju A, Yeh PT. A systematic review exploring the contraception values and preferences of sex workers, transmasculine individuals, people who inject drugs, and those living in humanitarian contexts. Contraception. 2022;111:32–38. doi: 10.1016/j.contraception.2021.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dam A, Yeh PT, Burke AE, Kennedy CE. Contraceptive values and preferences of pregnant women, postpartum women, women seeking emergency contraceptives, and women seeking abortion services: a systematic review. Contraception. 2022;111:39–48. doi: 10.1016/j.contraception.2021.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Saleem HT, Rosen JG, Quinn C, Duggaraju A, Kennedy CE. Contraception values and preferences of people living with HIV: a systematic review. Contraception. 2022;111:49–61. doi: 10.1016/j.contraception.2021.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soin KS, Yeh PT, Ge C, Gaffield ME, Kennedy CE. Healthcare workers’ values and preferences regarding contraceptive methods globally: a systematic review. Contraception. 2022;111:62–71. doi: 10.1016/j.contraception.2022.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 13.Bitzer J, Simon JA. Current issues and available options in combined hormonal contraception. Contraception. 2011;84:342–356. doi: 10.1016/j.contraception.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 14.Coombe J, Harris ML, Loxton D. What qualities of long-acting reversible contraception do women perceive as desirable or undesirable? A systematic review. Sex Health. 2016 doi: 10.1071/SH15189. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JA, Smith NK. The sexual acceptability of contraception: reviewing the literature and building a new concept. J Sex Res. 2016;53:417–456. doi: 10.1080/00224499.2015.1134425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roumen FJ, Mishell DR., Jr. The contraceptive vaginal ring, NuvaRing((R)), a decade after its introduction. Eur J Contracept Reprod Health Care. 2012;17:415–427. doi: 10.3109/13625187.2012.713535. [DOI] [PubMed] [Google Scholar]
- 17.Woodsong C, Holt JD. Acceptability and preferences for vaginal dosage forms intended for prevention of HIV or HIV and pregnancy. Adv Drug Deliv Rev. 2015;92:146–154. doi: 10.1016/j.addr.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Kennedy CE, Fonner VA, Armstrong KA, Denison JA, Yeh PT, O'Reilly KR, et al. The Evidence Project risk of bias tool: assessing study rigor for both randomized and non-randomized intervention studies. Syst Rev. 2019;8:3. doi: 10.1186/s13643-018-0925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Critical Appraisal Skills Programme. CASP qualitative research checklist [online]. 2017. accessed December 21, 2017. Available at: http://docs.wixstatic.com/ugd/dded87_25658615020e427da194a325e7773d42.pdf.
- 20.Bitzer J, Cupanik V, Fait T, Gemzell-Danielsson K, Grob P, Oddens BJ, et al. Factors influencing women's selection of combined hormonal contraceptive methods after counselling in 11 countries: results from a subanalysis of the CHOICE study. Eur J Contracept Reprod Health Care. 2013;18:372–380. doi: 10.3109/13625187.2013.819077. [DOI] [PubMed] [Google Scholar]
- 21.Bitzer J, Gemzell-Danielsson K, Roumen F, Marintcheva-Petrova M, van Bakel B, Oddens BJ. The CHOICE study: effect of counselling on the selection of combined hormonal contraceptive methods in 11 countries. Eur J Contracept Reprod Health Care. 2012;17:65–78. doi: 10.3109/13625187.2011.637586. [DOI] [PubMed] [Google Scholar]
- 22.Egarter C, Frey Tirri B, Bitzer J, Kaminskyy V, Oddens BJ, Prilepskaya V, et al. Women's perceptions and reasons for choosing the pill, patch, or ring in the CHOICE study: a cross-sectional survey of contraceptive method selection after counseling. BMC Women's Health. 2013;13:9. doi: 10.1186/1472-6874-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Egarter C, Grimm C, Nouri K, Ahrendt HJ, Bitzer J, Cermak C. Contraceptive counselling and factors affecting women's contraceptive choices: results of the CHOICE study in Austria. Reprod Biomed Online. 2012;24:692–697. doi: 10.1016/j.rbmo.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 24.Fait T. Predictors of combined hormone contraception choice between Czech and Slovak women. J Ev Purkyne. 2011;76:190–193. Ceska gynekologie /Ceska lekarska spolecnost. [PubMed] [Google Scholar]
- 25.Fait T. Combined hormone contraceptive choice experience in Czech Republic. Cent Eur J Med. 2011;6:582–587. [Google Scholar]
- 26.Fait T, Apetauer I. Importance of the consultation for combined hormonal contraception's choice–results of CHOICE project in Czech and Slovak Republic. J Ev Purkyne. 2011;76:140–144. Ceska gynekologie /Ceska lekarska spolecnost. [PubMed] [Google Scholar]
- 27.Gemzell-Danielsson K, Thunell L, Lindeberg M, Tyden T, Marintcheva-Petrova M, Oddens BJ. Comprehensive counseling about combined hormonal contraceptives changes the choice of contraceptive methods: results of the CHOICE program in Sweden. Acta Obstet Gynecol Scand. 2011;90:869–877. doi: 10.1111/j.1600-0412.2011.01180.x. [DOI] [PubMed] [Google Scholar]
- 28.Merckx M, Donders GG, Grandjean P, Van de Sande T, Weyers S. Does structured counselling influence combined hormonal contraceptive choice? Eur J Contracept Reprod Health Care. 2011;16:418–429. doi: 10.3109/13625187.2011.625882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merki-Feld GS, Gruber IM. Intention to use a combined contraceptive method and decision after counselling in Switzerland–Swiss data from the European CHOICE study. Eur J Contracept Reprod Health Care. 2012;17:119–127. doi: 10.3109/13625187.2011.630114. [DOI] [PubMed] [Google Scholar]
- 30.Peipert JF, Zhao Q, Allsworth JE, Petrosky E, Madden T, Eisenberg D, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Werth SR, Secura GM, Broughton HO, Jones ME, Dickey V, Peipert JF. Contraceptive continuation in Hispanic women. Am J Obstet Gynecol. 2015;212:312. doi: 10.1016/j.ajog.2014.09.003. e1-8. [DOI] [PubMed] [Google Scholar]
- 32.Madden T, Secura GM, Nease R, Politi M, Peipert JF. The role of contraceptive attributes in women's contraceptive decision making. Am J Obstet Gynecol. 2015;213:46. doi: 10.1016/j.ajog.2015.01.051. e1-e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paul R, Huysman BC, Maddipati R, Madden T. Familiarity and acceptability of long-acting reversible contraception and contraceptive choice. Am J Obstet Gynecol. 2020;222:S884. doi: 10.1016/j.ajog.2019.11.1266. e1-S.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asker C, Stokes-Lampard H, Beavan J, Wilson S. What is it about intrauterine devices that women find unacceptable? Factors that make women non-users: a qualitative study. J Fam Plann Reprod Health Care. 2006;32:89–94. doi: 10.1783/147118906776276170. [DOI] [PubMed] [Google Scholar]
- 35.Patra S, Singh RK. Addressing unmet need and religious barrier towards the use of family planning method among Muslim women in India. Int J Human Rights Healthcare. 2015;8:22–35. [Google Scholar]
- 36.Sangraula M, Garbers S, Garth J, Shakibnia EB, Timmons S, Gold MA. Integrating long-acting reversible contraception services into New York City school-based health centers: quality improvement to ensure provision of youth-friendly services. J Pediatr Adolesc Gynecol. 2017;30:376–382. doi: 10.1016/j.jpag.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 37.Lehan Mackin M, Clark MK, McCarthy AM, Farris K. Knowledge and use of emergency contraception in college women. West J Nurs Res. 2015;37:462–480. doi: 10.1177/0193945914551005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laher F, Todd CS, Stibich MA, Phofa R, Behane X, Mohapi L, et al. A qualitative assessment of decisions affecting contraceptive utilization and fertility intentions among HIV-positive women in Soweto, South Africa. AIDS Behav. 2009;13:47–54. doi: 10.1007/s10461-009-9544-z. [DOI] [PubMed] [Google Scholar]
- 39.von Sadovszky V, Ryan-Wenger N, Germann S, Evans M, Fortney C. Army women's reasons for condom use and nonuse. Womens Health Issues. 2008;18:174–180. doi: 10.1016/j.whi.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 40.Rey CN, Badger GJ, Melbostad HS, Wachtel D, Sigmon SC, MacAfee LK, et al. Perceptions of long-acting reversible contraception among women receiving medication for opioid use disorder in Vermont. Contraception. 2020;101:333–337. doi: 10.1016/j.contraception.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whitaker AK, Johnson LM, Harwood B, Chiappetta L, Creinin MD, Gold MA. Adolescent and young adult women's knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78:211–217. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]
- 42.Yarris KE, Dent NJ. Gender, inequality and Depo-provera: constraints on reproductive choice in Nicaragua. Glob Public Health. 2017;12:449–468. doi: 10.1080/17441692.2016.1168468. [DOI] [PubMed] [Google Scholar]
- 43.Arteaga S, Gomez AM. “That a method of birth control?” A qualitative exploration of young women's use of withdrawal. J Sex Res. 2016;53:626–632. doi: 10.1080/00224499.2015.1079296. [DOI] [PubMed] [Google Scholar]
- 44.DeMaria AL, Sundstrom B, Meier S, Wiseley A. The myth of menstruation: how menstrual regulation and suppression impact contraceptive choice. BMC Women's Health. 2019;19:125. doi: 10.1186/s12905-019-0827-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Payne JB, Sundstrom B, DeMaria AL. A qualitative study of young women's beliefs about intrauterine devices: fear of infertility. J Midwifery Women's Health. 2016;61:482–488. doi: 10.1111/jmwh.12425. [DOI] [PubMed] [Google Scholar]
- 46.Harries J, Constant D, Wright V, Morroni C, Müller A, Colvin CJ. A multidimensional approach to inform family planning needs, preferences and behaviours amongst women in South Africa through body mapping. Reprod Health. 2019;16:159. doi: 10.1186/s12978-019-0830-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mansour D. International survey to assess women's attitudes regarding choice of daily versus nondaily female hormonal contraception. Int J Women's Health. 2014;6:367–375. doi: 10.2147/IJWH.S59059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wigginton B, Harris ML, Loxton D, Lucke JC. A qualitative analysis of women's explanations for changing contraception: the importance of non-contraceptive effects. J Fam Plan Reprod Health Care. 2016;42:256–262. doi: 10.1136/jfprhc-2015-101184. [DOI] [PubMed] [Google Scholar]
- 49.Rubin SE, Winrob I. Urban female family medicine patients' perceptions about intrauterine contraception. J Womens Health. 2010;19:735–740. doi: 10.1089/jwh.2009.1549. [DOI] [PubMed] [Google Scholar]
- 50.Zeqiri F, Pacarada M, Zeqiri V, Bojaxhiu M, Pllana T. Analysis of contraception using IUDs in Kosova. Med Arhiv. 2009;63:342. [PubMed] [Google Scholar]
- 51.Terrell LR, Tanner AE, Hensel DJ, Blythe MJ, Fortenberry JD. Acceptability of the vaginal contraceptive ring among adolescent women. J Pediatr Adolesc Gynecol. 2011;24:204–210. doi: 10.1016/j.jpag.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 52.Hooper DJ. Attitudes, awareness, compliance and preferences among hormonal contraception users: a global, cross-sectional, self-administered, online survey. Clin Drug Investig. 2010;30:749–763. doi: 10.2165/11538900-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 53.Yee L, Simon M. The role of the social network in contraceptive decision-making among young, African American and Latina women. J Adolesc Health. 2010;47:374–380. doi: 10.1016/j.jadohealth.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abu-Hashim H, Alsherbini W, Bazeed M. Contraceptive vaginal ring treatment of heavy menstrual bleeding: a randomized controlled trial with norethisterone. Contraception. 2012;85:246–252. doi: 10.1016/j.contraception.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 55.Aisien AO, Enosolease ME. Safety, efficacy and acceptability of Implanon a single rod implantable contraceptive (etonogestrel) in University of Benin Teaching Hospital. Niger J Clin Pract. 2010;13:331–335. [PubMed] [Google Scholar]
- 56.Costa AR, Palma F, Sa JL, Vicente L, Bombas T, Nogueira AM, et al. Impact of a women's counselling programme on combined hormonal contraception in Portugal–the IMAGINE Study. Eur J Contracept Reprod Health Care. 2011;16:409–417. doi: 10.3109/13625187.2011.608441. [DOI] [PubMed] [Google Scholar]
- 57.Dehlendorf C, Levy K, Kelley A, Grumbach K, Steinauer J. Women's preferences for contraceptive counseling and decision making. Contraception. 2013;88:250–256. doi: 10.1016/j.contraception.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mills A, Barclay L. None of them were satisfactory: women's experiences with contraception. Health Care Women Int. 2006;27:379–398. doi: 10.1080/07399330600629468. [DOI] [PubMed] [Google Scholar]
- 59.Wong RC, Bell RJ, Thunuguntla K, McNamee K, Vollenhoven B. Implanon users are less likely to be satisfied with their contraception after 6 months than IUD users. Contraception. 2009;80:452–456. doi: 10.1016/j.contraception.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 60.Khokhar A, Sachdeva TR, Talwar R, Singh S, Rasania SK. Determinants of acceptance of no-scalpel vasectomy among men attending the NSV clinic in a public sector hospital of Delhi. Health Popul Perspect Issues. 2005;28:197–204. [Google Scholar]
- 61.Philipson S, Wakefield CE, Kasparian NA. Women's knowledge, beliefs, and information needs in relation to the risks and benefits associated with use of the oral contraceptive pill. J Women's Health. 2011;20:635–642. doi: 10.1089/jwh.2010.2455. (15409996) [DOI] [PubMed] [Google Scholar]
- 62.Gambera A, Corda F, Papa R, Bastianelli C, Bucciantini S, Dessole S, et al. Observational, prospective, multicentre study to evaluate the effects of counselling on the choice of combined hormonal contraceptives in Italy–the ECOS (Educational COunselling effectS) study. BMC Women's Health. 2015;15:69. doi: 10.1186/s12905-015-0226-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Minnis AM, Mavedzenge SN, Luecke E, Dehlendorf C. Provider counseling to young women seeking family planning services. Perspect Sex Reprod Health. 2014;46:223–231. doi: 10.1363/46e1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Epstein LB, Sokal-Gutierrez K, Ivey SL, Raine T, Auerswald C. Adolescent experiences with the vaginal ring. J Adolesc Health. 2008;43:64–70. doi: 10.1016/j.jadohealth.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Adamou BM, Iskarpatyoti BS, Agala CB, Mejia C. Exploring gaps in monitoring and evaluation of male engagement in family planning. Gates Open Res. 2019;3:1114. doi: 10.12688/gatesopenres.12927.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bonnington A, Dianat S, Kerns J, Hastings J, Hawkins M, De Haan G, et al. Society of family planning clinical recommendations: contraceptive counseling for transgender and gender diverse people who were female sex assigned at birth. Contraception. 2020;102:70–82. doi: 10.1016/j.contraception.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 67.WHO . World Health Organization; Geneva, Switzerland: 2014. Ensuring human rights in the provision of contraceptive information and services: guidance and recommendations.https://www.who.int/reproductivehealth/publications/family_planning/human-rights-contraception/en Available at. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.