Abstract
The current cross-sectional study aimed to extend the literature on childhood adversity by examining the unique associations between potentially traumatic events (PTEs) and a range of mental health concerns, including domain-specific versus comorbid concerns. Participants were 11,877 preadolescents (47.8% female, 15.0% Black, 20.3% Hispanic/Latinx, Mage = 9.5 years) taking part in the Adolescent Brain and Cognitive Development (ABCD) Study®. The Kiddie Schedule for Affective Disorders and Schizophrenia was used to measure PTEs and caregiver- and child-reported mental health concerns. Adjusted odds ratios (aORs) were used for the outcomes of interest. Overall, PTEs were consistently associated with increased odds of experiencing comorbid posttraumatic stress disorder (PTSD), internalizing disorders, and externalizing disorders, significant AORs = 1.34–4.30, after accounting for children’s experiences of other PTEs and polyvictimization. In contrast, PTEs were generally not associated with meeting the criteria for diagnoses within only one domain (i.e., internalizing-only or externalizing-only diagnoses). We also found PTEs to be differentially related to the various mental health outcomes. In particular, witnessing domestic violence was consistently associated with children’s psychopathology. Other PTEs, such as witnessing community violence, were not associated with children’s psychopathology in the final model. Associations between PTEs and mental health concerns did not differ as a function of sex. Overall, the results support the notion that PTEs are associated with comorbid concerns rather than individual disorders. These findings have important implications for the screening of PTEs, continued research on the conceptualization of traumatic stress, and the importance of accounting for comorbidities across mental health domains.
Potentially traumatic events (PTEs) are experiences with a high likelihood of harm, including actual or threatened death, serious injury, or sexual violence (American Psychiatric Association [APA], 2013). A majority of individuals in the United States will experience at least one PTE by the end of adolescence (McLaughlin et al., 2013). The biopsychosocial sequelae that follow PTE exposure are heterogeneous, including impairments in attachment, behavioral regulation, attention, and emotional and social information processing (D’Andrea et al., 2012; McLaughlin et al., 2020). Consistent with the theory of multifinality (Cicchetti, 1993), PTEs are associated with a range of mental health concerns, including posttraumatic stress disorder (PTSD), anxiety, depression, impairments in attention, and conduct problems (Alisic et al., 2014; Copeland et al., 2007; Crum et al., 2018; Greeson et al., 2014; Layne et al., 2014).
Although there is strong support for associations between PTEs and multiple forms of psychopathology, researchers continue to examine mental health concerns separately. This is a limitation of prior work given evidence that associations between risk factors and psychopathology are attenuated after accounting for comorbid symptoms (Brislin et al., 2021; Keyes et al., 2012). More specifically, prior work has shown that after removing the shared variance between internalizing and externalizing symptoms, domain-specific factors, such as experiencing internalizing-only or externalizing-only symptoms, are no longer associated with childhood maltreatment (Keyes et al., 2012) or family and school risk factors (Brislin et al., 2021). Gaining a better understanding of the associations between PTEs and domain-specific versus comorbid concerns has important implications for the screening of psychopathology and conceptualization of traumatic stress.
Prior work has also highlighted the importance of examining the unique versus cumulative risk of PTE exposure on adjustment. For example, multiple studies have found graded dose-response associations between PTE scores and psychopathology among children and adolescents (Copeland et al., 2007; Finkelhor et al., 2007; Greeson et al., 2014; Layne et al., 2014) such that as the number of PTEs increased, so did the prevalence rates of anxiety, depression, and behavioral disorders. Notably, when taking polyvictimization into account, defined as exposure to PTEs across multiple domains, the influence of individual PTEs on traumatic stress symptoms was found to be greatly reduced and, at times, eliminated among a population-based sample of children and adolescents (Finkelhor et al., 2007). These findings suggest that experiencing multiple types of events may be a more salient risk factor for mental health concerns compared with experiencing any specific event.
Nonetheless, cumulative scores have significant limitations. For example, they do little to shed light on whether certain PTEs are uniquely associated with specific mental health concerns. Turner and colleagues (2020) found that PTEs categorized by victimization (i.e., peer victimization, physical assault, and community violence) were more strongly associated with symptoms of PTSD than nonvictimization adversities. McLaughlin and colleagues (2012) found that abuse and maladaptive family functioning were the strongest predictors of the onset of psychiatric disorders. However, it remains unclear whether certain PTEs are more strongly associated with domain-specific versus comorbid concerns.
The current study had three primary aims. First, we aimed to extend upon past PTE studies (e.g., Carliner et al., 2017; Copeland et al., 2007; Finkelhor et al., 2007; Greeson et al., 2014; Layne et al., 2014) by providing prevalence rates of and associations between PTEs and mental health concerns using data from the large Adolescent Brain Cognitive Development (ABCD) Study cohort of 11,878 children. Although there has been a push to address comorbid symptoms through higher-order and bifactor analyses (i.e., the “p factor”; Smith et al., 2020), clinicians still rely heavily on the Diagnostic and Statistical Manual of Mental Disorders (fifth ed.; DSM-5) for identifying and treating mental health problems. This continued reliance on the DSM underscores the importance of examining psychopathology using diagnostic criteria and clinical cutoff thresholds. Therefore, we used the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-5; Kaufman et al., 1997; Townsend et al., 2020) to assess caregiver and youth reports of anxiety, depression, and suicidality, as well as caregiver reports of PTSD, attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and conduct disorder (CD). Notably, however, clinicians were not consulted within the ABCD Study, and, thus, formal diagnoses were not provided. We hypothesized that higher cumulative PTE scores would be associated with higher odds of meeting the criteria for each of the mental health concerns.
Second, we examined whether the associations between PTEs and lifetime psychopathology differed after accounting for comorbidities across three caregiver-reported domains: PTSD, internalizing disorders (i.e., anxiety, depression, suicidality), and externalizing disorders (i.e., ADHD, ODD, CD). Based on prior literature (Brislin et al., 2021; Keyes et al., 2012), we hypothesized that PTEs would be more strongly associated with comorbid psychopathology that spanned the three domains compared with the associations between PTEs and each specific domain that removed shared variance: PTSD-only, internalizing-only, and externalizing-only symptoms.
Third, we examined the associations between individual PTEs and mental health concerns both before and after controlling for the other PTEs and polyvictimization. Based on prior literature (Finkelhor et al., 2007), we hypothesized that associations between individual PTEs and psychopathology would be attenuated after accounting for the other PTEs and polyvictimization. We also hypothesized that, compared with noninterpersonal PTEs (e.g., medical events, disasters), interpersonal violence (e.g., abuse, assault, domestic and community violence) would be more likely to remain associated with psychopathology across both caregiver and child reporters, after controlling for polyvictimization. Finally, we examined whether these relations differed for boys and girls, which we considered to be an exploratory aim.
METHOD
Participants and procedure
The current cross-sectional study was conducted through secondary analyses using baseline cross-sectional data from the ABCD Study (Data Release 3.0) from the National Institute of Mental Health data archive. See Supplementary Table 1 for details regarding which ABCD Study variables were used. The 21 ABCD Study sites targeted representation from approximately 20% of all 9- and 10-year-olds in the United States. The ABCD Study approximates the American Community Survey’s estimates for preadolescents’ demographic characteristics, including sex, race, ethnicity, and household size (see Garavan et al., 2018, and Heeringa & Berglund, 2020, for exceptions, including higher household incomes). All procedures were approved at each site’s institutional research ethics board (i.e., institutional review board [IRB]) or through reliance from the Central IRB at the University of California at San Diego. Sites also complied with their respective states’ mandated reporting requirements for suspected abuse and neglect. Written informed child assents and parental permissions were obtained from all youth and caregivers. More detailed information regarding the design and the recruitment process can be found in Garavan et al. (2018).
The mean participant age was 9.5 years, and the sample was 47.8% female. Based on the caregivers’ reports, most of the youth were White (52.0%), but other racial/ethnic groups were also represented (i.e., 15.0% Black; 2.1% Asian; 20.3% Hispanic or Latinx; and 10.5% “other” race, which included multiracial youth). Family demographic characteristics were also diverse. With regard to educational attainment, 5.1% percent of the caregivers reported leaving school without a degree, 12.1% reported a high school degree or equivalent, 16.4% reported some college, 41.0% reported having attained an associate’s or bachelor’s degree, and one quarter of the caregivers (25.2%) reported having received a graduate degree. Over two thirds of caregivers (67.3%) reported currently being married. Across the sample, caregiver-reported combined household income was negatively skewed, with 19.3% reporting below $35,000 (USD), 20.5% reporting $35,000–$74,999, 13.2% reporting $75,000–$99,999, and 38.4% reporting $100,000 or more; 8.6% of caregivers did not report on their income.
Measures
Demographic characteristics
Covariates included child age, race, ethnicity, and sex assigned at birth, as well as caregiver educational attainment, total household income, and parental marital status (i.e., married or not).
Caregiver mental health
Caregiver mental health problems were self-reported using the Achenbach Adult Self Report Questionnaire (ASR; Achenbach, 2017). The ASR comprises 120 problem items, each of which is scored on a scale of 0–2, and includes eight syndrome subscales: Anxious/Depressed, Withdrawn, Attention Problems, Aggressive Behavior, Rule-Breaking Behavior, and Intrusion. In the current study, we used a total raw score, which ranged from 0 to 154 (M = 21.14, SD = 17.96). Internal consistency of the ASR was acceptable (α = .68).
PTEs
PTEs included items from the self-administered, caregiver-reported computerized KSADS-5 PTSD module (Kaufman et al., 1997; Townsend et al., 2020). Items were coded as 1 if caregivers responded “yes” to an item and as 0 if caregivers denied that their child had ever experienced that event. Due to low prevalence rates and covariance coverage, we collapsed the 17 PTEs into seven categories: (a) accidents requiring medical attention, (b) natural disasters, (c) witnessing community violence, (d) witnessing domestic violence, (e) physical victimization, (f) sexual trauma, and (g) sudden death of a loved one. Total PTE scores were also calculated by summing the number of individual PTEs reported. Based on the low prevalence rates for more than three PTEs, we collapsed PTE cumulative scores into the following four categories: exposure to zero PTEs, one PTE, two PTEs, and three or more PTEs. Additionally, polyvictimization was separately coded as 1 if a child had experienced two or more lifetime PTEs and as 0 if they had experienced one or no lifetime PTEs.
Child mental health outcomes
Caregiver report.
Caregivers reported on current and past episodes of mood, anxiety, and disruptive behavioral disorders and symptoms during the administration of the computerized KSADS-5 (Kaufman et al., 1997; Townsend et al., 2020). Diagnoses generated from the computerized version demonstrated good convergent validity against established clinical rating scales (Townsend et al., 2020). Binary items were created for a lifetime mental health diagnosis (i.e., presently or in the past). Within the current study, we examined lifetime symptoms of anxiety; depression; suicidality; including suicidal ideation, intent, or attempts; PTSD; ADHD; ODD; and CD. To examine comorbidities, internalizing domains included anxiety, depression, and suicidality, whereas externalizing domains included ADHD, ODD, and CD. PTSD was considered its own domain.
Child report.
Children were also administered portions of the computerized KSADS-5 (Kaufman et al., 1997; Townsend et al., 2020). We used child reports of lifetime depression, anxiety, and suicidality. Within the ABCD Study, children did not report on their symptoms of PTSD, ADHD, ODD, or CD at baseline.
Data analysis
All analyses were conducted using Mplus (Version 8.6; Muthén & Muthén, 2017). For the multivariate models, full information maximum likelihood estimation and Monte Carlo integration were used to address missing data and numerical integration. Missing data on the mental health concerns ranged from 0.6% to 1.4% of the total sample, with 2.7% of the sample missing information on PTE exposure. We assumed that the data were missing at random (MAR) conditional on the other predictors in the models (i.e., sex, age, race, ethnicity, caregiver education, household income, caregiver marital status, and caregiver’s own mental health concerns) and the residuals of the other mental health concerns, which were covaried across outcomes. However, we acknowledge that we cannot exclude the possibility that data were missing not at random (MNAR), as it is likely that some individuals refused to answer questions about PTEs and mental health concerns specifically due to their experiences with PTEs and mental health concerns. Stratification and clustering variables were used to account for the nesting of participants among the 21 sites and within families.
To address our first study aim, multiple group models were used to examine nonadjusted prevalence rates of caregiver- and child-reported mental health concerns across caregiver-reported PTE scores. For our second and third research aims, we used multivariate logistic regressions. See Supplementary Table 2 for the final Mplus model. Adjusted odds ratios (aORs) were used as our main effect size for these analyses. An adjusted odds ratio above 1.0 indicated that experiencing a particular PTE was associated with a higher likelihood of experiencing the mental health concern compared to youth who had not experienced that PTE. An adjusted odds ratio below 1 indicated that, compared to non-PTE exposed youth, experiencing a particular PTE was associated with a reduced likelihood of experiencing the mental health concern. Furthermore, we provided probabilities at times; for instance, an adjusted odds ratio of 1.0 indicated a 50% probability of meeting the criteria for a mental health concern based on experiencing a particular PTE (i.e., no better than chance). In contrast, an adjusted odds ratio of 2.0 indicated a 67% probability and 4.0 indicated an 80% probability based on experiencing a particular PTE, after controlling for covariates. Given the large number of regression coefficients, we used a Benjamini–Hochberg–adjusted p value of .025 or less to limit the family-wise Type 1 error rate across all logistic regression analyses (Benjamini & Hochberg, 1995). We used a Wald test within an unconstrained multiple group model to test whether the adjusted odds ratios in the final model differed across sex.
RESULTS
Prevalence rates
Lifetime prevalence rates of PTEs and mental health concerns are reported in Table 1. Overall, 62.5% of caregivers reported that their child had not experienced any PTEs, one quarter (25.4%) reported one PTE, 7.1% reported two PTEs, and 2.4% reported three or more PTEs across the seven PTE domains. Almost half of all caregivers (40.8%) reported that their child had experienced clinically significant internalizing concerns, including anxiety, depression, or suicidality, compared with only 14.2% of youth self-reports. A little over one quarter (27.4%) of caregivers reported externalizing concerns, including ADHD, ODD, or CD. Whereas only 4.6% of caregivers reported that their child had experienced PTSD, 91.5% of those caregivers also reported clinically significant internalizing or externalizing concerns, and 62.1% of caregivers who reported PTSD reported clinically significant symptoms of both internalizing and externalizing concerns. Given the low prevalence rates of PTSD-only symptoms (i.e., 0.4% of the entire sample), no further analyses were conducted using the PTSD-only domain.
TABLE 1.
Unadjusted prevalence rates of caregiver-reported potentially traumatic events (PTEs) and mental health concerns
| PTE | n | % |
|---|---|---|
|
|
||
| Unexpected death of a loved one | 2,782 | 24.1 |
| Witnessed domestic violence | 934 | 8.1 |
| Accident requiring medical treatment | 865 | 7.5 |
| Natural disaster that caused damage or injury | 508 | 4.4 |
| Sexual trauma (abuse or assault) | 230 | 2.0 |
| Victimization (physical abuse, assault, or threats to kill) | 209 | 1.8 |
| Witnessed community violence (shootings, stabbing, terrorism, or war) | 150 | 1.3 |
| PTE cumulative score | ||
| 0 | 7,418 | 62.5 |
| 1 | 3,014 | 25.4 |
| 2 | 844 | 7.1 |
| 3 or more | 284 | 2.4 |
| Mental health concerns: Caregiver report | ||
| Anxiety | 4,326 | 36.4 |
| Depression | 741 | 6.2 |
| Suicidality | 897 | 7.6 |
| Any internalizing concern | 4,849 | 40.8 |
| Internalizing concerns only | 2,629 | 22.1 |
| ADHD | 2,550 | 21.5 |
| ODD | 1,667 | 14.0 |
| CD | 375 | 3.2 |
| Any externalizing concern | 3,255 | 27.4 |
| Externalizing concerns only | 1,127 | 9.5 |
| Internalizing + externalizing | 2,093 | 17.6 |
| PTSD | 551 | 4.6 |
| PTSD only | 47 | 0.4 |
| PTSD + internalizing | 469 | 3.9 |
| PTSD + externalizing | 377 | 3.2 |
| PTSD + internalizing + externalizing | 342 | 2.9 |
| Mental health concerns: Youth report | ||
| Anxiety | 387 | 3.3 |
| Depression | 597 | 5.0 |
| Suicidality | 1,040 | 8.8 |
| Any internalizing concern | 1,683 | 14.2 |
Note. Prevalence rates do not add up to 100% due to missingness. PTSD = posttraumatic stress disorder; ADHD = attention-deficit hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder.
Association between cumulative PTE scores and psychopathology
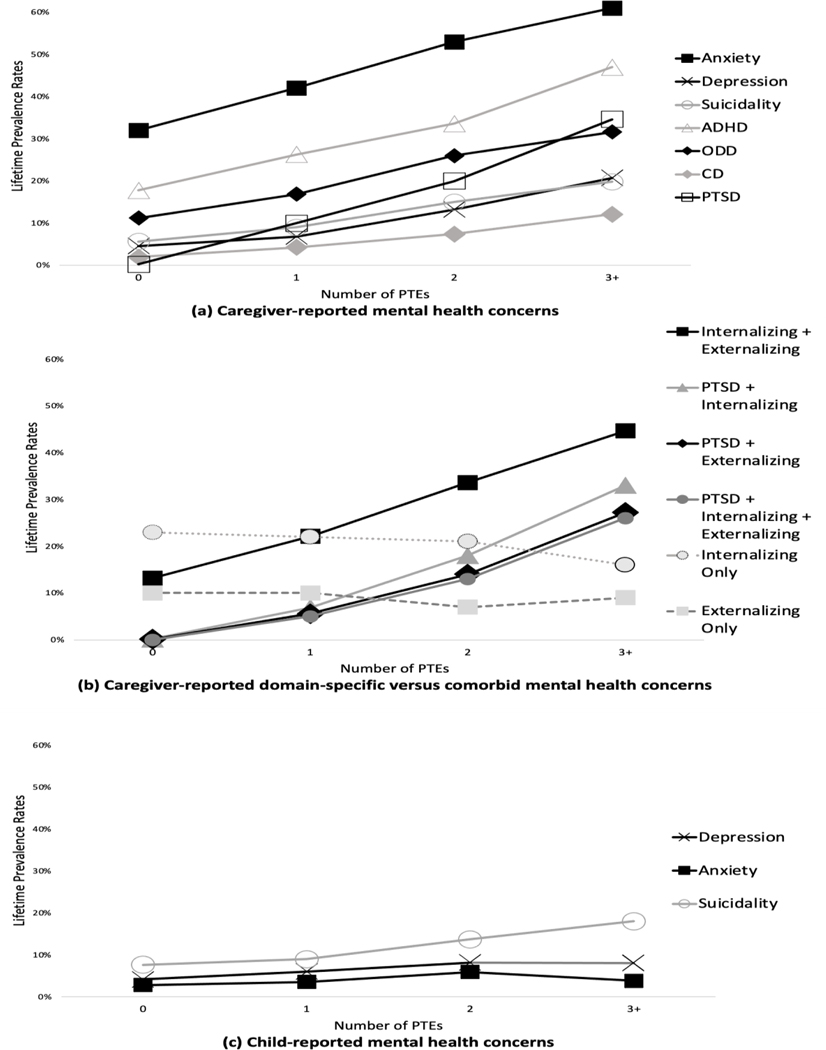
Our first hypothesis, that higher cumulative PTE scores would be associated with higher odds of meeting the criteria for each of the mental health concerns, was partially supported. We found a graded dose-response association between the number of PTEs experienced and higher frequencies of children’s caregiver-reported mental health concerns (Table 2; Figure 1, Panel A). Across PTE scores, caregivers endorsed high rates of anxiety disorders (32.1%–61.3%) and ADHD (17.8%–46.8%). Caregiver-reported depression and suicidality rates increased at similar rates, and both were higher among children with higher PTE frequencies. Over one third (35.1%) of the children with caregiver reports of three or more PTEs met the criteria for PTSD. We also found a graded dose-response relation between the number of PTEs and caregiver-reported ODD and CD, albeit at lower prevalence rates than ADHD.
Table 2.
Unadjusted prevalence rates of mental health concerns, by potentially traumatic event (PTE) exposure
| Variable | 0 PTEs (n = 7,418) | 1 PTE (n = 3,014) | 2 PTEs (n = 844) | ≥3 PTEs (n = 284) |
|---|---|---|---|---|
|
|
||||
| Caregiver-reported concerns | % 95% CI | % 95% CI | % 95% CI | % 95% CI |
|
|
||||
| Anxiety | 32.1 [31.0, 33.2] | 42.3 [40.4, 44.1] | 52.7 [49.2, 56.2] | 61.3 [55.5, 67.2] |
| Depression | 4.6 [4.1, 5.0] | 6.9 [6.0, 7.8] | 13.4 [11.0, 15.8] | 21.3 [16.4, 26.2] |
| Suicidality | 5.8 [5.3, 6.4] | 8.7 [7.7, 9.7] | 15.2 [12.7, 17.7] | 19.5 [14.8, 24.2] |
| Internalizing concerns only | 22.8 [21.8, 23.7] | 22.2 [20.6, 23.7] | 21.3 [18.5, 24.0] | 15.6 [11.3, 19.9] |
| ADHD | 17.8 [16.9, 18.7] | 26.4 [24.8, 28.0] | 33.8 [30.6, 37.1] | 46.8 [40.8, 52.8] |
| ODD | 11.2 [10.5, 12.0] | 16.9 15.5, 18.3] | 25.7 [22.6, 28.7] | 31.9 [26.5, 37.3] |
| CD | 1.9 [1.6, 2.3] | 4.4 [3.6, 5.1] | 7.5 [5.7, 9.3] | 12.1 [8.3, 15.8] |
| Externalizing concerns only | 9.8 [9.1, 10.5] | 10.0 [9.0, 11.1] | 7.1 [5.4, 8.9] | 9.2 [5.8, 12.6] |
| PTSD | 0.2 [0.1, 0.4] | 8.8 [7.7, 9.8] | 19.8 [17.1, 22.6] | 35.1 [29.4, 40.8] |
| Caregiver-reported comorbidities | ||||
| Internalizing + externalizing | 13.2 [12.4, 14.0] | 22.4 [20.8, 23.9] | 34.1 [30.8, 37.3] | 45.4 [39.5, 51.3] |
| PTSD + internalizing | 0.2 [0.1, 0.3] | 7.0 [6.1, 8.0] | 17.5 [14.8, 20.1] | 33.0 [27.4, 38.6] |
| PTSD + externalizing | 0.1 [0.1, 0.2] | 5.7 [4.9, 6.5] | 13.9 [11.5, 16.3] | 27.3 [22.0, 32.6] |
| PTSD + internalizing + externalizing | 0.1 [0.1, 0.2] | 4.9 [4.1, 5.6] | 13.1 [10.8, 15.4] | 26.2 [21.0, 31.5] |
| Child-reported concerns | ||||
| Anxiety | 2.8 [2.4, 3.2] | 3.6 [2.9, 4.2] | 5.9 [4.3, 7.6] | 3.5 [1.4, 5.7] |
| Depression | 4.2 [3.7, 4.6] | 6.1 [5.2, 6.9] | 7.8 [6.0, 9.6] | 7.8 [4.7, 10.9] |
| Suicidality | 8.0 [7.4, 8.6] | 8.6 [7.6, 9.6] | 14.3 [11.8, 16.7] | 18.0 [13.6, 22.4] |
Note. The number of participants ranged from 11,512 to 11,537 due to missingness on the variables. PTSD = posttraumatic stress disorder; ADHD = attention-deficit hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder.
Figure 1.
Unadjusted prevalence rates of mental health concerns, by potentially traumatic event (PTE) exposure
Note. PTSD = posttraumatic stress disorder; ADHD = attention-deficit hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder.
We also examined domain-specific versus comorbid concerns across PTE scores (Table 2; Figure 1, Panel B). Caregiver-reported comorbid mental health concerns were higher among children with higher PTE frequencies, with the highest rates of comorbid internalizing and externalizing concerns (i.e., 45.4% for three or more PTEs). Prevalence rates were relatively similar for youth with caregiver-reported comorbid PTSD and internalizing concerns, comorbid PTSD and externalizing concerns, and comorbidities across all three domains (26.2%–33.0% for three or more PTEs). However, meeting the criteria for only internalizing or only externalizing concerns did not fluctuate substantially as PTE exposure increased, with higher rates occurring among youth without any caregiver-reported PTEs.
Compared to the caregiver reports, children reported lower rates of depression and anxiety but similar rates of suicidality across PTE scores (Table 2; Figure 1, Panel C). Notably, 18.0% of youth who had experienced three or more PTEs reported lifetime suicidal ideation. However, in contrast to our hypothesis, prevalence rates among child-reported mental health concerns were less variable across PTE scores than those from the caregiver reports, particularly child-reported anxiety and depression.
Associations between psychopathology and individual versus cumulative exposure to PTEs
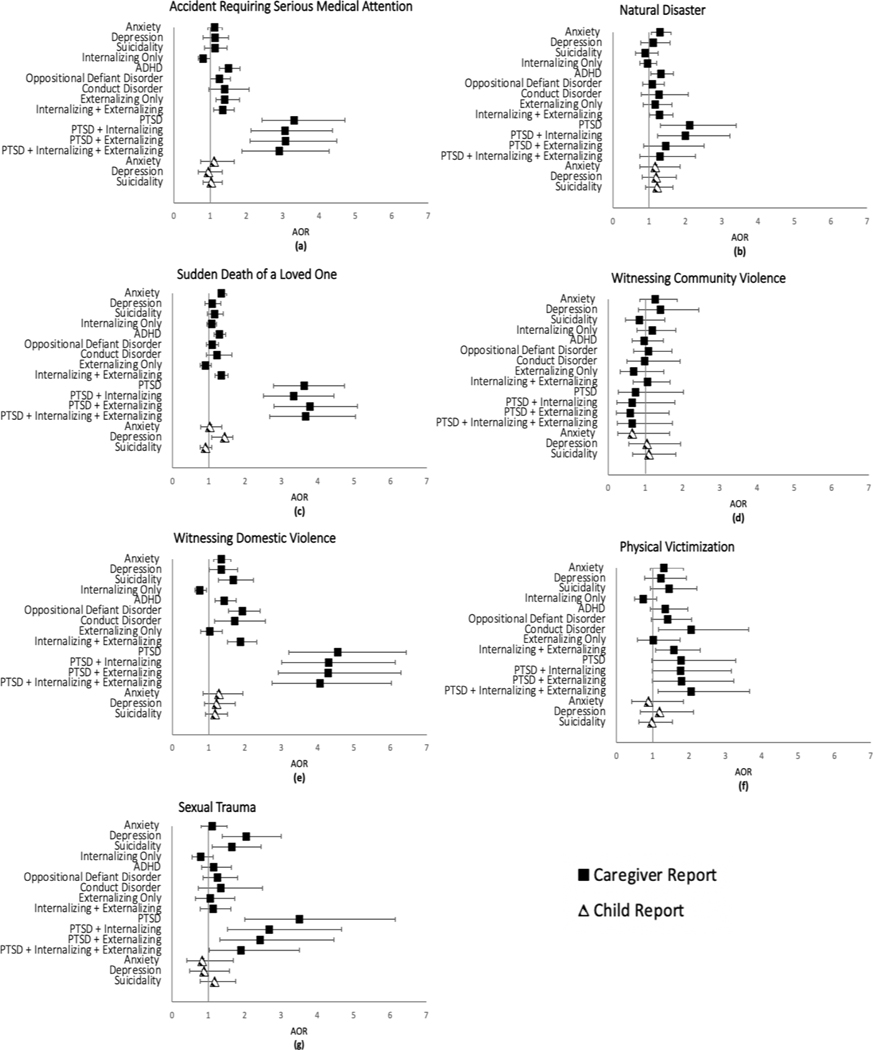
To address our second and third research aims, caregiver- and child-reported mental health concerns were regressed on each of the PTEs individually across seven individual models and on the PTEs simultaneously along with polyvictimization status (i.e., the full model). All models included sex, age, race, ethnicity, caregiver educational attainment, total household income, caregiver marital status, and caregivers’ own mental health concerns as covariates. Because numerical integration was required to address missing predictor variable data, absolute fit statistics were not provided in the Mplus output. However, relative fit indices (i.e., Akaike information criterion, Bayesian information criterion, sample-size adjusted Bayesian information criterion) are reported in Table 3. Tables 4–6 provide adjusted odds ratios and 95% confidence intervals for caregiver-reported mental health concerns, and Table 7 provides adjusted odds ratios and 95% confidence intervals for child-reported mental health concerns. Results for the full model are graphically depicted in Figure 2. Graphical depiction of the individual models that did not control for the other PTEs can be found within the Supplementary Materials.
Table 3.
Relative fit indices
| Model | Free parameters | Log-likelihood | AIC | BIC | SABIC |
|---|---|---|---|---|---|
|
|
|||||
| Individual modelsa | |||||
| Accident | 269 | − 176,231.93 | 353,001.85 | 354,987.73 | 354,132.88 |
| Natural disaster | 269 | −173,559.47 | 347,656.93 | 349,642.81 | 348,787.96 |
| Death | 269 | −181,505.67 | 363,549.33 | 365,535.21 | 364,680.36 |
| Community violence | 269 | −166,683.59 | 333,905.17 | 335,891.05 | 335,036.20 |
| Domestic violence | 269 | −175,919.25 | 352,376.51 | 354,362.38 | 353,507.53 |
| Victimization | 269 | −168,459.98 | 337,457.95 | 339,443.83 | 338,588.98 |
| Sexual trauma | 269 | −168,992.81 | 338,523.62 | 340,509.50 | 339,654.65 |
| Full modelb | 493 | −153,644.82 | 308,275.64 | 311,915.19 | 310,348.49 |
| Multiple group model, by sex | 764 | −153,062.13 | 307,652.26 | 313,292.45 | 310,864.55 |
Note. N = 11,877.
Seven separate models were estimated.
One model was estimated. AIC = Akaike information criterion; BIC = Bayesian information criterion; SABIC = sample-size adjusted Bayesian information criterion.
TABLE 4.
Associations between potentially traumatic events (PTEs) and caregiver-reported internalizing disorders and posttraumatic stress disorder (PTSD)
| Caregiver-reported MH concerns | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| PTE | Anxiety | Depression | Suicidality | Internalizing Only | PTSD | |||||
|
|
||||||||||
| Individual modelsa | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
|
|
||||||||||
| Accident | 1.28** | [1.10, 1.49] | 1.50** | [1.17, 1.93] | 1.40** | [1.11, 1.76] | 0.81* | [0.67, 0.97] | 4.28*** | [3.40, 5.37] |
| Natural disaster | 1.48*** | [1.23, 1.79] | 1.53** | [1.12, 2.08] | 1.15 | [0.84, 1.57] | 0.93 | [0.74, 1.16] | 3.37*** | [2.51, 4.52] |
| Death | 1.43*** | [1.30, 1.57] | 1.34** | [1.13, 1.59] | 1.35*** | [1.16, 1.58] | 1.05 | [0.94, 1.17] | 4.32*** | [3.58, 5.22] |
| Community violence | 1.82** | [1.27, 2.61] | 2.49*** | [1.54, 4.02] | 1.57 | [0.95, 2.59] | 1.01 | [0.68, 1.50] | 3.79*** | [2.39, 6.02] |
| Domestic violence | 1.56*** | [1.34, 1.81] | 1.87*** | [1.49, 2.34] | 2.16*** | [1.74, 2.68] | 0.75** | [0.62, 0.90] | 5.94*** | [4.79, 7.37] |
| Victimization | 1.76*** | [1.28, 2.42] | 2.26*** | [1.52, 3.37] | 2.33*** | [1.63, 3.33] | 0.66c | [0.45, 0.95] | 4.94*** | [3.33, 7.31] |
| Sexual trauma | 1.45* | [1.08, 1.95] | 3.02*** | [2.14, 4.27] | 2.39*** | [1.67, 3.42] | 0.72 | [0.51, 1.02] | 6.79*** | [4.83, 9.55] |
| Full modelb | ||||||||||
| Accidents | 1.12 | [0.95, 1.34] | 1.13 | [0.86, 1.50] | 1.13 | [0.87, 1.47] | 0.81c | [0.66, 1.00] | 3.31*** | [2.32, 4.71] |
| Natural disaster | 1.30* | [1.06, 1.60] | 1.11 | [0.77, 1.58] | 0.89 | [0.63, 1.25] | 0.95 | [0.74, 1.21] | 2.11** | [1.31, 3.39] |
| Death | 1.34*** | [1.20, 1.49] | 1.09 | [0.89, 1.33] | 1.16 | [0.96, 1.39] | 1.08 | [0.95, 1.21] | 3.63*** | [2.78, 4.73] |
| Community violence | 1.26 | [0.85, 1.86] | 1.41 | [0.81, 2.44] | 0.84 | [0.47, 1.52] | 1.18 | [0.77, 1.82] | 0.74 | [0.27, 2.02] |
| Domestic violence | 1.35** | [1.13, 1.61] | 1.35c | [1.02, 1.79] | 1.68*** | [1.27, 2.23] | 0.76* | [0.62, 0.94] | 4.55*** | [3.21, 6.44] |
| Victimization | 1.30 | [0.93, 1.84] | 1.22 | [0.78, 1.93] | 1.45 | [0.94, 2.22] | 0.74 | [0.50, 1.10] | 1.78 | [0.97, 3.28] |
| Sexual trauma | 1.11 | [0.80, 1.52] | 2.04*** | [1.38, 3.01] | 1.65* | [1.11, 2.45] | 0.79 | [0.55, 1.13] | 3.50*** | [2.00, 6.14] |
| Polyvictimization | 1.07 | [0.86, 1.33] | 1.39 | [0.98, 1.98] | 1.31 | [0.93, 1.85] | 1.03 | [0.80, 1.34] | 0.82 | [0.50, 1.33] |
| Caregiver MH | 1.03*** | [1.03, 1.03] | 1.03*** | [1.02, 1.03] | 1.03*** | [1.02, 1.03] | 1.01*** | [1.00, 1.01] | 1.02*** | [1.02, 1.03] |
| R 2 | .10*** | .11*** | .12*** | .02*** | .29*** | |||||
Note. N = 11,877. MH = mental health; aOR = adjusted odds ratio.
Seven separate models were estimated.
One model was estimated. Each model also included sex, age, race, ethnicity, caregiver education, household income, caregiver marital status, and caregivers’ own mental health concerns.
Denotes p < .05, but the coefficient did not meet the significance threshold based on the Benjamini–Hochberg procedure.
p < .025.
p < .01.
p < .001.
TABLE 6.
Associations between potentially traumatic events (PTEs) and caregiver-reported comorbid child mental health concerns
| PTE model | Caregiver-reported comorbid MH concerns | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Internalizing + externalizing | PTSD + internalizing | PTSD + externalizing | PTSD + internalizing + externalizing | |||||
|
| ||||||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
|
| ||||||||
| Individual modelsa | ||||||||
| Accident | 1.61*** | [1.35, 1.91] | 4.34*** | [3.41, 5.53] | 4.27*** | [3.29, 5.54] | 4.30*** | [3.27, 5.64] |
| Natural disaster | 1.56*** | [1.25, 1.95] | 3.44*** | [2.50, 4.72] | 2.75*** | [1.92, 3.94] | 2.65*** | [1.81, 3.88] |
| Death | 1.50*** | [1.33, 1.68] | 4.34*** | [3.53, 5.33] | 4.76*** | [3.79, 5.97] | 4.89*** | [3.84, 6.23] |
| Community violence | 1.89** | [1.27, 2.81] | 3.62*** | [2.20, 5.95] | 3.33*** | [1.98, 5.61] | 3.54*** | [2.06, 6.06] |
| Domestic violence | 2.25*** | [1.89, 2.67] | 6.16*** | [4.88, 7.77] | 6.09*** | [4.73, 7.86] | 6.29*** | [4.81, 8.21] |
| Victimization | 2.45*** | [1.76, 3.42] | 5.02*** | [3.36, 7.50] | 4.72*** | [3.13, 7.13] | 5.29*** | [3.47, 8.07] |
| Sexual trauma | 1.12** | [1.25, 2.36] | 5.96*** | [4.17, 8.50] | 5.37*** | [3.61, 7.98] | 4.75*** | [3.14, 7.18] |
| Full modelb | ||||||||
| Accidents | 1.35** | [1.10, 1.66] | 3.06*** | [2.15, 4.37] | 3.08*** | [2.11, 4.49] | 2.90*** | [1.97, 4.27] |
| Natural Disaster | 1.29c | [1.01, 1.65] | 1.99** | [1.23, 3.22] | 1.46 | [0.85, 2.51] | 1.30 | [0.75, 2.27] |
| Death | 1.34*** | [1.17, 1.53] | 3.34*** | [2.51, 4.44] | 3.78*** | [2.80, 5.09] | 3.67*** | [2.68, 5.04] |
| Community violence | 1.06 | [0.67, 1.66] | 0.65 | [0.23, 1.79] | 0.60 | [0.22, 1.64] | 0.65 | [0.25, 1.73] |
| Domestic violence | 1.88*** | [1.52, 2.32] | 4.30*** | [3.01, 6.14] | 4.29*** | [2.92, 6.29] | 4.07*** | [2.75, 6.03] |
| victimization | 1.58* | [1.08, 2.31] | 1.77 | [0.99, 3.17] | 1.79 | [0.99, 3.23] | 2.05* | [1.15, 3.66] |
| Sexual trauma | 1.13 | [0.78, 1.62] | 2.68** | [1.53, 4.67] | 2.43** | [1.32, 4.46] | 1.90c | [1.03, 3.51] |
| Polyvictimization | 1.09 | [0.84, 1.42] | 1.01 | [0.62, 1.64] | 0.97 | [0.58, 1.61] | 1.14 | [0.68, 1.91] |
| Caregiver MH | 1.04*** | [1.03, 1.04] | 1.03*** | [1.02, 1.03] | 1.03*** | [1.02, 1.03] | 1.03*** | [1.03, 1.04] |
| R 2 | .18*** | .31*** | .31*** | .32*** | ||||
Note. N = 11,877. PTSD = posttraumatic stress disorder; aOR = adjusted odds ratio; MH = mental health.
Seven models were estimated.
One model was estimated. Each model also included sex, age, race, ethnicity, caregiver education, household income, caregiver marital status, and caregivers’ own mental health concerns.
Denotes p < .05, but the coefficient did not meet the significance threshold based on the Benjamini–Hochberg procedure.
p < .025.
p < .01.
p < .001.
Table 7.
Associations between potentially traumatic events (PTEs) and child-reported mental health concerns
| Child-reported mental health concerns | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| PTE model | Anxiety | Depression | Suicidality | |||
|
| ||||||
| Individual modelsa | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
|
|
||||||
| Accident | 1.29 | [0.91, 1.82] | 1.04 | [0.77, 1.41] | 1.30* | [1.04, 1.61] |
| Natural disaster | 1.34 | [0.87, 2.07] | 1.27 | [0.89, 1.83 | 1.51** | [1.14, 2.00] |
| Death | 1.16 | [0.91, 1.46] | 1.38** | [1.15, 1.66] | 1.08 | [0.93, 1.26] |
| Community violence | 0.83 | [0.34, 2.05] | 1.28 | [0.72, 2.27] | 1.58 | [0.99, 2.52] |
| Domestic violence | 1.47* | [1.05, 2.05] | 1.32 | [1.00, 1.74] | 1.50*** | [1.22, 1.86] |
| Victimization | 1.09 | [0.55, 2.18] | 1.33 | [0.81, 2.20] | 1.49c | [1.01, 2.19] |
| Sexual trauma | 1.01 | [0.51, 2.00] | 1.04 | [0.60, 1.79] | 1.59* | [1.10, 2.32] |
| Full modelb | ||||||
| Accidents | 1.11 | [0.74, 1.66] | 0.95 | [0.68, 1.34] | 1.03 | [0.81, 1.33] |
| Natural disaster | 1.17 | [0.75, 1.84] | 1.19 | [0.81, 1.75] | 1.22 | [0.90, 1.65] |
| Death | 1.03 | [0.78, 1.36] | 1.43** | [1.08, 1.66] | 0.91 | [0.76, 1.08] |
| Community violence | 0.65 | [0.26, 1.65] | 1.04 | [0.56, 1.94] | 1.10 | [0.66, 1.82] |
| Domestic violence | 1.28 | [0.85, 1.94] | 1.22 | [0.88, 1.73] | 1.18 | [0.91, 1.52] |
| Victimization | 0.88 | [0.42, 1.85] | 1.18 | [0.66, 2.12] | 0.98 | [0.62, 1.54] |
| Sexual trauma | 0.83 | [0.41, 1.69] | 0.88 | [0.49, 1.58] | 1.17 | [0.78, 1.75] |
| Polyvictimization | 1.34 | [0.79, 2.28] | 1.01 | [0.67, 1.52] | 1.54** | [1.12, 2.12] |
| Caregiver mental health | 1.01** | [1.00, 1.01] | 1.01*** | [1.00, 1.01] | 1.01*** | [1.01, 1.02] |
| R 2 | .03*** | .04*** | .04*** | |||
Note. N = 11,877. aOR = adjusted odds ratio.
Seven models were estimated.
One model was estimated. Each model also included sex, age, race, ethnicity, caregiver education, total household income, caregiver marital status, and caregivers’ own mental health concerns.
Denotes p < .05, but the coefficient did not meet the significance threshold based on the Benjamini–Hochberg procedure.
p < .025.
p < .01.
p < .001
Figure 2.
Adjusted odds ratios (aORs) and 95% confidence intervals of mental health concerns, by potentially traumatic event (PTE) exposure
Note. All analyses controlled for demographic characteristics, other PTE exposure, and polyvictimization. PTSD = posttraumatic stress disorder; ADHD = attention-deficit/hyperactivity disorder.
Accidents requiring serious medical attention
Experiencing a serious accident was associated with increased odds of meeting all seven caregiver-reported mental health concerns, as well as comorbidities between internalizing disorders, externalizing disorders, and PTSD (Tables 4–6); in contrast, this PTE exposure was associated with decreased odds of only meeting the criteria for caregiver-reported internalizing disorders. After including the other six PTEs and polyvictimization in the model, experiencing an accident remained associated with increased odds of meeting the criteria for caregiver-reported ADHD, PTSD, and comorbidities across the three domains and was now also associated with externalizing-only disorders (57.4%–76.8% probability; Figure 2, Panel A). Experiencing a serious accident was associated with increased odds of child-reported suicidality within the individual model but not after accounting for the other PTEs and polyvictimization (Table 7; Figure 2, Panel A).
Natural disasters
Being caught in a natural disaster was associated with increased odds of meeting the criteria for caregiver-reported anxiety, depression, PTSD, ADHD, and comorbidities across the three mental health domains (Tables 4–6). After controlling for the other six PTEs and polyvictimization, experiencing a natural disaster remained associated with increased odds of meeting the criteria for anxiety, PTSD, ADHD, and comorbid PTSD and internalizing disorders (56.5%–67.8% probability; Figure 2, Panel B). Experiencing a natural disaster was associated with increased odds of child-reported suicidality within the model that examined experiencing a disaster individually but not after accounting for the other PTEs and polyvictimization (Table 7; Figure 2, Panel B).
Sudden death of a loved one
Learning about the sudden death of a loved one was associated with increased odds of meeting the criteria for each of the seven individual caregiver-reported mental health concerns as well as comorbidities across the three domains (Tables 4–6). However, exposure to this PTE was associated with decreased odds of only meeting the criteria for externalizing disorders. After controlling for the other PTEs and polyvictimization, the sudden death of a loved one remained associated with caregiver-reported anxiety; PTSD; ADHD; and comorbidities between PTSD, internalizing disorders, and externalizing disorders (56.3%–79.1% probability; Figure 2, Panel C). The sudden death of a loved one was associated with child-reported depression in both models that examined the death of a loved one individually and after accounting for the other PTEs and polyvictimization (58.8% probability; Table 7; Figure 2, Panel C).
Witnessing community violence
Prior to controlling for the other PTEs, witnessing community violence was associated with caregiver-reported anxiety, depression, PTSD, ODD, and comorbidities across the three mental health domains (Tables 4–6). However, after accounting for the other six PTEs and polyvictimization, it did not uniquely predict any caregiver- or child-reported mental health concerns (Tables 4–7; Figure 2, Panel D).
Witnessing domestic violence
Before controlling for the other PTEs, witnessing domestic violence was associated with higher odds of meeting the clinical criteria for each of the individual caregiver-reported mental health concerns as well as comorbidities across the three domains. However, witnessing domestic violence was associated with decreased odds of only meeting the criteria for internalizing disorders (Tables 4–6). Within the full model, witnessing domestic violence remained significantly associated with each of the caregiver-reported mental health concerns except depression (43.2% probability for internalizing-only concerns and between 57.4%–82.0% for all other significant associations; Figure 2, Panel E). Witnessing domestic violence was also associated with child-reported anxiety and suicidality; however, no associations remained after accounting for the other PTEs and polyvictimization (Table 7; Figure 2, Panel E).
Physical victimization
Physical victimization was associated with increased odds of meeting the criteria for each of the seven caregiver-reported mental health concerns as well as comorbidities across the three domains (Tables 4–6). After controlling for other PTEs and polyvictimization, physical victimization remained associated with CD; comorbid internalizing and externalizing disorders; and comorbid PTSD, internalizing disorders, and externalizing disorders (61.2%–67.2% probability; Figure 2, Panel F). No associations were found between physical victimization and child-reported mental health concerns in either model (Table 7; Figure 2, Panel F).
Sexual trauma
Sexual trauma was associated with increased odds of meeting the criteria for each of the seven caregiver-reported mental health concerns as well as comorbidities across the three domains (Tables 4–6). After controlling for the other PTEs and polyvictimization, sexual trauma remained significantly associated with caregiver-reported depression; SI; PTSD; and comorbid PTSD, internalizing disorders, and externalizing disorders (62.3%–77.8% probability; Figure 2, Panel G). Sexual trauma was also associated with increased odds of child-reported suicidality; however, this did not remain significant when accounting for the other PTEs and polyvictimization (Table 7; Figure 2, Panel G).
Sex differences
Within the final model, the magnitude of the associations between PTEs, polyvictimization, and mental health concerns did not significantly differ across sex, Wald χ2(128, N = 11,878) = 142.831, p = .175.
DISCUSSION
Using the large ABCD Study sample of over 11,000 9–10-year-olds, the current cross-sectional study aimed to extend the literature on childhood adversity by examining the associations between PTEs and domain-specific versus comorbid mental health concerns. Consistent with prior studies (Copeland et al., 2007; Greeson et al., 2014; Layne et al., 2014), we found support for our first hypothesis such that PTE cumulative scores were significantly associated with a broad range of mental health concerns within childhood, with particularly high rates of comorbid PTSD, internalizing disorders, and externalizing disorders based on caregiver-reports. Notably, however, youth reported lower prevalence rates of internalizing concerns, and fewer associations were found between PTEs and child-reported concerns. We also found differential associations between individual PTEs and each of the mental health concerns after controlling for other PTEs and polyvictimization, which did not differ across sex. Overall, the current findings support the theory of multifinality of trauma exposure, which asserts that similar stressful events can lead to a diverse range of outcomes (Cicchetti, 1993; McLaughlin et al., 2020).
The caregiver-reported PTE prevalence rates were much lower than prior studies’ estimates of PTEs. Two thirds of caregivers reported that their child had not experienced any of the PTEs included in the current study. Some discrepancies with prior studies are expected given that most have examined prevalence rates within adolescence rather than childhood (Copeland et al., 2007; McLaughlin et al., 2013). However, prevalence rates found within the current study are much lower than rates from the National Survey of Children’s Exposure to Violence (NatSCEV; Finkelhor et al., 2015). For example, Finkelhor and colleagues found that 47% of caregivers reported that their 6–9-year-olds had experienced a physical assault within the last year. Within the ABCD Study, only 1.8% of caregivers reported any type of lifetime physical victimization. This may be due to differences in the severity of victimization queried. It is also possible that assessment modality played a role in caregivers’ forthcomingness, as the NatSCEV conducted interviews via a brief (i.e., approximately 60 min) telephone call, whereas families within the ABCD Study committed to an in-person, day-long assessment at baseline. The underrepresentation of lower-income households within the ABCD Study (Garavan et al., 2018) may also partially explain the lower prevalence rates of PTEs. Future work using the ABCD Study sample should examine whether PTE prevalence rates increase over time, as many PTEs tend to peak during adolescence (Finkelhor et al., 2007).
We found full support for our second hypothesis, which is consistent with transdiagnostic approaches to childhood trauma (McLaughlin et al., 2020). PTEs were not significantly associated with increased odds of internalizing-only or externalizing-only domains but rather associated with comorbidities across PTSD, internalizing disorders, and externalizing disorders. That is, associations between PTEs and internalizing and externalizing disorders were inflated when we did not account for the shared variance across disorder categories. For example, although witnessing domestic violence was associated with increased odds of experiencing anxiety, youth were not at increased risk of experiencing anxiety alone but rather at increased risk of experiencing anxiety along with PTSD or externalizing symptoms. These findings make it difficult to compare our results with prior studies, as very few studies have examined the associations between PTEs and domain-specific versus comorbid mental health concerns.
The high prevalence rates of caregiver-reported ADHD, ODD, and CD among PTE-exposed youth found within the current study are consistent with prior studies that have examined associations between PTEs and disruptive behavior disorders (Carliner et al., 2017; McLaughlin et al., 2013). These findings highlight the importance of screening for PTEs when presenting problems include inattention, hyperactivity, and oppositionality. Symptoms of avoidance, intrusion, and hyperarousal associated with PTSD could mirror symptoms of ADHD or ODD (e.g., distractibility, hyperactivity, irritability, and impulsivity) and lead to misdiagnosis (Symanski et al., 2011). Some researchers have advocated for the use of diagnoses that better capture the heterogeneity of trauma-related symptoms, such as developmental trauma disorder (DTD; van Der Kolk et al., 2019). The ongoing, longitudinal nature of the ABCD Study provides optimal future opportunities to examine DTD as a diagnosis that better captures comorbidities among children exposed to familial stress. Another possible explanation is that PTSD and ADHD share common risk factors, such as parental ADHD symptoms (e.g., impulsivity, inattention), that increase a child’s risk for developing ADHD and experiencing a PTE through separate biological and environmental mechanisms. Alternatively, prior longitudinal work has found that ODD and CD increase youths’ risk for later exposure to interpersonal violence (Carliner et al., 2017), suggesting bidirectional risk as opposed to misdiagnosis. Further work capturing the age of onset of PTEs and related symptoms could shed light on some of these alternative hypotheses.
Our third research aim focused on differential associations between psychopathology and individual PTEs versus polyvictimization. Consistent with prior work (Finkelhor et al., 2007), associations were attenuated and often no longer significant after accounting for the other PTEs and polyvictimization. This underscores the importance of examining multiple PTEs simultaneously and the need to assess for exposure to PTEs across multiple domains. However, we only found partial support for our fourth hypothesis. We predicted that, compared to noninterpersonal PTEs, interpersonal violence would remain associated with psychopathology across both caregiver and child reporters. First, very few PTEs were associated with child-reported symptoms in either model. After accounting for the other PTEs, experiencing the death of a loved one remained significantly associated with child-reported depression. These results suggest that the death of a loved one may be one of the most salient risk factors for depression among PTE-exposed youth. Nonetheless, this is a somewhat speculative assertion, as the DSM-5 (APA, 2013) cautions clinicians to differentiate between normal grieving and symptoms of depression, and a clinician’s expertise was not used within the ABCD Study. In contrast to depression, no PTE remained significantly associated with child-reported anxiety or suicidality; however, polyvictimization was associated with an increased risk of child-reported suicidality, which was the largest odds ratio across all child-reported concerns. Therefore, the cumulative effects of experiencing stressful events may be more influential on youths’ risk for suicidal ideation than any particular event. Given that youth only reported on their internalizing symptoms, future work is needed to determine whether associations between PTEs and child-reported concerns would be attenuated after accounting for comorbidities with PTSD and externalizing symptoms.
Regarding caregiver-reported mental health concerns, community violence was the only PTE that did not remain significantly associated with a mental health concern after accounting for the other PTEs and polyvictimization. Therefore, although some PTEs are considered more severe than others (e.g., witnessing community violence vs. experiencing a natural disaster), they may be less salient risk factors for maladjustment when accounting for exposure to other PTEs. In addition, the results indicated that all other PTEs were associated with at least one of the four comorbid domain combinations. Thus, many PTEs were associated with comorbid psychopathology regardless of subjective severity.
Associations between PTEs and psychopathology were largest for witnessing domestic violence. For example, among youth exposed to domestic violence, the probability of experiencing comorbid mental health concerns ranged from 65% to 81%. These findings are consistent with prior research indicating that domestic violence has a complex and enduring impact on child development (Noble-Carr et al., 2020). Within the current study, we also found caregiver mental health to be a significant predictor of every caregiver- and child-reported mental health concern, albeit at very low effect sizes, even when controlling for each of the PTEs and polyvictimization. Thus, screening for family violence and parental psychopathology and providing referrals for outside treatment may augment pediatric clinical care as well as provide benefits to other members of the household (e.g., siblings).
Several limitations in the current study warrant discussion. First, the cross-sectional nature of the study prevents us from implying causation between PTEs and mental health concerns. Exposure to PTEs has been found to be higher among adolescents with preexisting disruptive disorders (Carliner et al., 2017; McLaughlin et al., 2013). Thus, our current findings do not preclude the possibility that mental health concerns increased the risk of exposure to PTEs or, more likely, that bidirectional relations between PTEs and these mental health outcomes exist. The current study also focused exclusively on PTEs used to diagnose PTSD—that is, PTEs that are linked to threatened or actual death, injury, or sexual violence. There has been an increasing call for the expansion of what is deemed traumatic given links between other nonviolent life stressors (e.g., suboptimal housing, parental job loss, food insecurity) and PTSD (Thompson et al., 2020). Our findings were also based primarily on caregiver reports, which may have led to measurement bias and low PTE prevalence rates. This may be most evident in the large confidence intervals across adjusted odds ratios. Replication of the current findings is needed using youth-reported PTEs, which is tentatively planned for either the sixth or seventh follow-up wave of the ABCD Study. In addition, PTEs were measured using manifest variables rather than latent constructs based on multiple items, which could have reduced the reliability of our results.
This study extends PTE findings downward to 9- and 10-year-olds as captured primarily using caregiver reports of internalizing and externalizing problems collected during the large ABCD Study. Overall, these findings highlight the importance of differentiating between domain-specific and comorbid mental health concerns. The present findings have important implications for the screening of PTEs and mental health concerns beyond PTSD as well as for continued research on the conceptualization of traumatic stress. The ABCD Study also offers a unique opportunity to prospectively study the evolution of trauma-associated behavioral health concerns and many other biological measures (e.g., brain structure or function) over time in future work.
Supplementary Material
TABLE 5.
Associations between potentially traumatic events (PTEs) and caregiver-reported externalizing disorders
| Caregiver-reported MH concerns | ||||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| PTE model | ADHD | ODD | CD | Externalizing Only | ||||
|
| ||||||||
| Individual modelsa | aOR | 95% CI | aAOR | 95% CI | aOR | 95% CI | aOR | 95% CI |
|
|
||||||||
| Accident | 1.61*** | [1.36, 1.90] | 1.44*** | [1.19, 1.74] | 1.62** | [1.18, 2.24] | 1.15 | [0.91, 1.45] |
| Natural disaster | 1.46*** | [1.18, 1.80] | 1.29+ | [1.01, 1.64] | 1.56c | [1.02, 2.39] | 0.97 | [0.71, 1.32] |
| Death | 1.35*** | [1.21, 1.51] | 1.23** | [1.08, 1.39] | 1.38** | [1.10, 1.74] | 0.81** | [0.69, 0.95] |
| Community violence | 1.42 | [0.98, 2.07] | 1.75** | [1.18, 2.61] | 1.80c | [1.01, 3.19] | 0.54 | [0.26, 1.13] |
| Domestic violence | 1.56*** | [1.31, 1.84] | 2.23*** | [1.87, 2.67] | 2.04*** | [1.52, 2.75] | 0.81 | [0.63, 1.04] |
| Victimization | 1.72** | [1.24, 2.39] | 2.18*** | [1.57, 3.04] | 2.88*** | [1.80, 4.61] | 0.74 | [0.45, 1.24] |
| Sexual trauma | 1.45* | [1.06, 1.99] | 1.78** | [1.28, 2.47] | 2.04** | [1.20, 3.47] | 0.82 | [0.51, 1.32] |
| Full modela | ||||||||
| Accidents | 1.50*** | [1.24, 1.82] | 1.25+ | [1.00, 1.56] | 1.40 | [0.95, 2.07] | 1.40** | [1.09, 1.81] |
| Natural disaster | 1.32* | [1.05, 1.67] | 1.08 | [0.82, 1.42] | 1.27 | [0.78, 2.07] | 1.17 | [0.84, 1.63] |
| Death | 1.29*** | [1.14, 1.46] | 1.09 | [0.94, 1.26] | 1.23 | [0.93, 1.63] | 0.91 | [0.77, 1.07] |
| Community violence | 0.97 | [0.64, 1.48] | 1.08 | [0.68, 1.71] | 0.98 | [0.50, 1.93] | 0.69 | [0.32, 1.49] |
| Domestic violence | 1.43** | [1.17, 1.76] | 1.93*** | [1.54, 2.41] | 1.72** | [1.16, 2.56] | 1.03 | [0.78, 1.37] |
| Victimization | 1.35 | [0.93, 1.96] | 1.41 | [0.96, 2.07] | 2.05* | [1.16, 3.64] | 1.01 | [0.58, 1.75] |
| Sexual trauma | 1.15 | [0.81, 1.63] | 1.25 | [0.86, 1.80] | 1.35 | [0.73, 2.49] | 1.05 | [0.64, 1.72] |
| Polyvictimization | 0.93 | [0.73, 1.19] | 1.11 | [0.84, 1.47] | 0.96 | [0.59, 1.56] | 0.62* | [0.43, 0.89] |
| Caregiver MH | 1.03*** | [1.03, 1.03] | 1.03*** | [1.03, 1.03] | 1.03*** | [1.02, 1.03] | 1.01*** | [1.00, 1.01] |
| R 2 | .15*** | .14*** | .19*** | .06*** | ||||
Note. N = 11,877. ADHD = attention/deficit-hyperactivity disorder; ODD = oppositional defiant disorder; CD = conduct disorder; MH = mental health; aOR = adjusted odds ratio.
Seven separate models were estimated.
One model was estimated. Each model also included sex, age, race, ethnicity, caregiver education, household income, caregiver marital status, and caregivers’ own mental health concerns.
Denotes p < .05, but the coefficient did not meet the significance threshold based on the Benjamini–Hochberg procedure.
p < .025.
p < .01.
p < .001.
Acknowledgments
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children aged 9–10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health (NIH) and additional federal partners (U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147). A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in the analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from https://doi.org/10.15154/1519007. Digital object identifiers can be found at https://nda.nih.gov/study.html?id=634. Erin L. Thompson’s work was supported by the National Institute on Drug Abuse (T32 5T32DA043449-02; PI: William E. Pelham).
Footnotes
The authors have no conflicts of interest to disclose.
Open Practices Statement
The study reported in this article was not formally preregistered. Deidentified data along with a codebook are posted at https://doi.org/10.15154/1519007. Data analysis scripts are included in the Supplemental Online Material associated with this article.
REFERENCES
- Achenbach TM, Ivanova MY, & Rescorla LA (2017). Empirically based assessment and taxonomy of psychopathology for ages 1½–90+ years: Developmental, multi-informant, and multicultural findings. Comprehensive Psychiatry, 79, 4–18. 10.1016/j.comppsych.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, & Smid GE (2014). Rates of post-psychological distress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry: The Journal of Mental Science, 204(5), 335–340. 10.1192/bjp.bp.113.131227 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. [Google Scholar]
- Benjamini Y, & Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57(1), 289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Brislin S, Martz ME, Joshi S, Duval ER, Gard AM, Clark DA, Hyde L, Hicks B, Taxali A, Angstadt M, Rutherford S, Heitzeg MM, & Sripada C. (2020). Differentiated nomological networks of internalizing, externalizing, and the general factor of psychopathology (“p factor”) in emerging adolescence in the ABCD study. Psychological Medicine. Advance online publication. 10.1017/S0033291720005103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H, Gary D, McLaughlin KA, & Keyes KM (2017). Trauma exposure and externalizing disorders in adolescents: Results from the National Comorbidity Survey Adolescent Supplement. Journal of the American Academy of Child & Adolescent Psychiatry, 56(9), 755–764. 10.1016/j.jaac.2017.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D. (1993). Developmental psychopathology: Reactions, reflections, projections. Developmental Review, 13(4), 471–502. 10.1006/drev.1993.1021 [DOI] [Google Scholar]
- Copeland WE, Keeler G, Angold A, & Costello EJ (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577–584. 10.1001/archpsyc.64.5.577 [DOI] [PubMed] [Google Scholar]
- Crum KI, Cornacchio D, Coxe S, Greif Green J, & Comer JS (2017). Conduct problems among Boston-area youth following the 2013 Marathon bombing: The moderating role of prior violent crime exposure. Journal of Clinical Child & Adolescent Psychology, 46(3), 343–352. 10.1080/15374416.2015.1077450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Andrea W, Ford J, Stolbach B, Spinazzola J, & Van Der Kolk BA (2012). Understanding interpersonal trauma in children: Why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry, 82(2), 187–200. 10.1111/j.1939-0025.2012.01154.x [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007). Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect, 31(1), 7–26. 10.1016/j.chiabu.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the National Survey of Children’s Exposure to Violence. JAMA Pediatrics, 169(8), 746–754. 10.1001/jamapediatrics.2015.0676 [DOI] [PubMed] [Google Scholar]
- Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, Jernigan T, Potter A, Thompson W, Zahs D. (2018). Recruiting the ABCD Sample: Design considerations and procedures. Developmental Cognitive Neuroscience, 32, 16–22. 10.1016/j.dcn.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greeson JK, Briggs EC, Layne CM, Belcher HM, Ostrowski SA, Kim S, Lee RC, Vivrette RL, Pynoos RS, & Fairbank JA (2014). Traumatic childhood experiences in the 21st century: Broadening and building on the ACE studies with data from the National Child Traumatic Stress Network. Journal of Interpersonal Violence, 29(3), 536–556. 10.1177/0886260513505217 [DOI] [PubMed] [Google Scholar]
- Heeringa SG, & Berglund PA (2020). A guide for population-based analysis of the Adolescent Brain Cognitive Development (ABCD) Study baseline data. BioRxiv, 1–36. 10.1101/2020.02.10.942011 [DOI] [Google Scholar]
- Kaufman J, Birmaher B, & Brent D. (1997). Kiddie Schedule for Affective Disorders and Schizophrenia. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 545–553. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Keyes KM, Eaton NR, Krueger RF, McLaughlin KA, Wall MM, Grant BF, & Hasin DS (2012). Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry: The Journal of Mental Science, 200(2), 107–115. 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layne CM, Greeson JKP, Ostrowski SA, Kim S, Reading S, Vivrette RL, Briggs EC, Fairbank JA, & Pynoos RS (2014). Cumulative trauma exposure and high-risk behavior in adolescence: Findings from the National Child Traumatic Stress Network Core Data Set. Psychological Trauma: Theory, Research, Practice, and Policy, 6(Suppl 1), S40–S49. 10.1037/a0037799 [DOI] [Google Scholar]
- McLaughlin KA, Colich NL, Rodman AM, & Weissman DG (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Medicine, 18(1). 10.1186/s12916-020-01561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky A, & Kessler RC (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of adolescents. Archives of General Psychiatry 69, 1151–1160. 10.1001/archgenpsychiatry.2011.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 52(8), 815–830. 10.1016/j.jaac.2013.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. [Google Scholar]
- Noble-Carr D, Moore T, & McArthur M. (2020). Children’s experiences and needs in relation to domestic and family violence: Findings from a meta-synthesis. Child & Family Social Work, 25(1), 182–191. 10.1111/cfs.12645 [DOI] [Google Scholar]
- Smith GT, Atkinson EA, Davis HA, Riley EN, & Oltmanns JR (2020). The general factor of psychopathology. Annual Review of Clinical Psychology, 16(1), 75–98. 10.1146/annurev-clinpsy-071119-115848 [DOI] [PubMed] [Google Scholar]
- Szymanski K, Sapanski L, & Conway F. (2011). Trauma and ADHD—Association or diagnostic confusion? A clinical perspective. Journal of Infant, Child, and Adolescent Psychotherapy, 10(1), 51–59. 10.1080/15289168.2011.575704 [DOI] [Google Scholar]
- Thompson EL, Coleman JN, O’Connor KE, Farrell AD, & Sullivan TN (2020). Exposure to violence and nonviolent life stressors and their relations to trauma-related distress and problem behaviors among urban early adolescents. Psychology of Violence, 10(5), 509–519. 10.1037/vio0000264 [DOI] [Google Scholar]
- Townsend L, Kobak K, Kearney C, Milham M, Andreotti C, Escalera J, Alexander L, Gill MK, Birmaher B, Sylvester R, Rice D, Deep A, & Kaufman J. (2020). Development of three web-based computerized versions of the Kiddie Schedule for Affective Disorders and Schizophrenia Child Psychiatric Diagnostic Interview: Preliminary validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 59(2), 309–325. 10.1016/j.jaac.2019.05.009 [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Mitchell KJ, Jones LM, & Henly M. (2020). Strengthening the predictive power of screening for adverse childhood experiences (ACEs) in younger and older children. Child Abuse & Neglect, 107, 104522. 10.1016/j.chiabu.2020.104522 [DOI] [PubMed] [Google Scholar]
- van Der Kolk B, Ford JD, & Spinazzola J. (2019). Comorbidity of developmental trauma disorder (DTD) and post-traumatic stress disorder: Findings from the DTD field trial. European Journal of Psychotraumatology, 10((1), 1–13. 10.1080/20008198.2018.1562841 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.