Abstract
Introduction:
Obesity prevalence among children and adolescents has risen sharply, yet there is a limited understanding of the age-specific dynamics of obesity as there is no single nationally representative cohort following children into young adulthood. Investigators constructed a pooled data set of 5 nationally representative panels and modeled age-specific obesity incidence from childhood into young adulthood.
Methods:
This longitudinal prospective follow-up used 718,560 person-years of observation in a pooled data set of 5 high-quality nationally representative panels— National Longitudinal Survey of Youth 1979 and 1997, National Longitudinal Study of Adolescent Health, and Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 and 2011—constructed by the authors covering 1980–2016. Differences in obesity incidence across birth cohorts and disparities in obesity incidence by sex and race/ethnicity (non-Hispanic Black, Hispanic, and non-Hispanic White) were tested in multivariate models. Data were analyzed from September 2018 to October 2021.
Results:
Obesity incidence increased by approximately 6% for each 1 year of age (hazard ratio=1.06, 95% CI=1.05, 1.07); however, incidence was non-linear, exhibiting an inverted U-shaped pattern before age 15 years and then rising from adolescence through age 30 years. Obesity incidence more than doubled between the cohorts born in 1957–1965 and those born in 1974–1985 during adolescence. There was no significant change among those born in 1991–1994 and 2003–2006 up to age 15 years. Compared with non-Hispanic White children, non-Hispanic Black and Hispanic children had higher obesity incidence in all study cohorts. The magnitude of these disparities on the relative scale remained stable throughout the study period.
Conclusions:
Although many children become obese prior to age 10 years, obesity incidence rises from about age 15 years into early adulthood, suggesting that interventions are required at multiple developmental stages.
INTRODUCTION
Obesity levels have increased rapidly among U.S. children.1–4 Between 1988–1994 and 2015–2018, the percentage of American children with obesity aged 2–18 years approximately doubled.5,6 Obesity during childhood and adolescence is associated with a wide range of illnesses, negative social consequences, and poor academic performance.7–15 Children and adolescents with obesity have a high likelihood of remaining obese long term,16–21 what is termed “entrenched obesity,”21 elevating the risk of chronic disease and mortality.22–26 Thus, prevention of obesity before it develops has been a foremost public health priority.
Obesity prevalence, which is commonly reported to monitor obesity levels, does not provide information on the actual ages of obesity onset, where prevention efforts could be tailored. Rather, it offers a snapshot of existing obesity at specific ages or periods. Alternatively, the age-specific obesity incidence identifies the age-based risks of becoming obese, thereby informing developmentally appropriate interventions to prevent or at least delay obesity onset. For instance, if the preschool years hold the highest risk, investments should be disproportionately targeted to families with children in this age group; if incidence is highest upon school entry or thereafter, school-based interventions could be preferable.
Studies measuring obesity incidence among U.S. children are few and have been restricted in the ages and birth cohorts examined.27–32 In a review, Cheung et al.32 counted only 3 studies of childhood obesity incidence among 19 that relied on nationally representative data. The average follow-up length was 2.0 years. There exists minimal information on how the age-specific incidence of obesity changes throughout childhood and adolescence within a birth cohort, and to what extent age-specific incidence is changing across birth cohorts including changes by sex and race/ethnicity.
A limiting factor has been the lack of a nationally representative panel following children from an early age into adulthood. To provide a comprehensive evaluation, 5 national longitudinal (panel) studies of U.S. children, adolescents, and young adults were examined. Collectively, cohorts born during 1957–2007 at ages 4–30 years were included, although not all birth cohorts were observed at all ages. Changes in the age-specific incidence of obesity within birth cohorts as they aged and differences in incidence across non-overlapping birth cohorts at specific ages were investigated where the data permitted. Differences by sex and race/ethnicity were also examined.
METHODS
Study Sample
Data were from 5 national panel studies: National Longitudinal Survey of Youth 1979 (NLSY79) and 1997 (NLSY97), National Longitudinal Study of Adolescent Health (ADDTH), Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 (ECLS-K:1998) and 2011 (ECLS-K:2011). These data sets have been described previously.33–40 The NLSY79 baseline wave was a stratified multistage cluster sample (n=6,111) of U.S. non-institutionalized civilians aged 14–21 years in 1979 (cohorts born during 1957–1965). It collected data annually during 1979–1994 and biennially thereafter.38 Weight and height data were available from 1981 onward. The baseline wave of NLSY1997 was a stratified multistage cluster sample (n=8,984) of youth aged 12–18 years in 1997 (cohorts born during 1979–1985).34,39 NLSY1997 was conducted annually during 1997–2011 and biennially thereafter. The baseline wave was a stratified cluster sample (n=20,745) of adolescents aged 11–21 in the 1994–1995 school year (cohorts born during 1974–1984). Follow-up waves were in 1996, 2001, and 2007.35,40 The baseline waves of ECLS-K:1998 (n=21,409) and ECLS-K:2011 (n=18,174) were stratified multistage cluster samples of American children aged 3–7 years (birth cohorts 1991–1994 and 2003–2006, respectively).37 The percentage of respondents participating in ≥1 follow-up wave was: 88.74% for ADDTH, 85.02% for NLSY79, 73.28% for NLSY97, 82.84% for ECLS-K: 1998, and 82.60% for ECLS-K:2011.
All data sets were probability samples designed to be nationally representative at the time of enrollment and will be representative for later years except for subsequent immigration or emigration. One exception: Because the ECLS-K studies are school-based samples, the 4 year olds in ECLS-K were representative of 4-year-olds in school (kindergarten or higher), which would not be representative of all 4-year-olds in the U.S. at the time, as most children do not start kindergarten until age 5 years. These children were included in the study because of interest in making inference about children at as young an age as possible.
Appendix Figure 1 shows the years and ages contained in the pooled data set. A total of 64,772 unique respondents aged 4–24 years at the initial wave of their respective study were included. Respondents were followed for a total of 718,560 person-years.
Measures
Height and weight were measured in ECLS-K: 1999, ECLS-K:2011, and the follow-up waves of ADDTH and self-reported in NLSY79, NLSY97, and the baseline wave of ADDTH. These data were adjusted in 3 ways. First, outliers were identified and removed using Cook’s distance (575 outliers were detected). Second, self-reported values were corrected for measurement error. Third, missing values were imputed and years where there was no survey were conducted were interpolated.
Self-reported weight and height data were corrected using correction factors obtained from an analysis of the 1999–2016 National Health and Nutrition Examination Survey, which contains both self-reported and clinically measured height and weight for a subsample. Calibration models in the National Health and Nutrition Examination Survey were fitted predicting measured weight and height (separately) as a function of self-reported height and weight by sex and race/ethnicity among those aged 16–30 years.41 Further details are in Appendix 2.
In the NLSY79, height was asked in 1981–1982, 1985, and 2006–2016 (biennially). Height was imputed using a linear interpolation for waves in which height was not collected. NLSY97 did not ask about height in the last 2 waves (2013 and 2015) and height was set in those waves to a value equal to the 2011 wave when all respondents were aged ≥25 years. Using sequential imputation, BMI (kg/m2) was imputed for all survey waves in instances when weight or height were missing or were eliminated owing to being an outlier (collectively, 6.7% of person-year observations). Finally, BMI was linearly interpolated in all non-survey years to complete the person-year cells of the data.
Obesity for respondents aged <17 years was defined as BMI ≥95th percentile of the sex-specific BMI-for-age growth charts from the Centers for Disease Control and Prevention.42 Obesity for those aged ≥17 years was defined as a BMI ≥30 kg/m2. Appendix 3 summarizes the thresholds by age.
The main outcome was obesity incidence defined as follows. A transition from a non-obese to obese state was counted as an incident event if the respondent remained obese for 2 adjacent waves in order to reduce the influence of random fluctuations across the BMI threshold. That is, a respondent was considered to experience an incident event at time t if they were not obese at time t – 1 and obese at both times t and t + 1. In approximately 30% of instances in which there was a non-obese to obese transition from t − 1 to t, obesity was not observed in t+1. Recurrent incident events for the same individual were permitted. Eight percent of individuals experiencing 1 incident event experienced a subsequent event.
Models were adjusted for age, sex (female/male), and race/ethnicity (non-Hispanic White [henceforth, White], non-Hispanic Black [Black], Hispanic). Because not all surveys separated Whites from other non-Black races, for the purposes of data harmonization other non-Black races were combined into the White category in instances in which they were separated.
Statistical Analysis
First, obesity incidence by age and birth cohort was graphed based on a discrete-time semi-parametric survival analyses fitted using complementary log-log binary regressions.43 A flexible parameterization of age was used by employing penalized cubic splines with ridge regularization and k = 10 knots.
Second, complementary log-log regression models were employed to identify the hazard ratios (HRs) associated with age, sex, race/ethnicity, and study. These models are akin to estimating age/cohort models and identify patterns by age and birth cohort. In Model 1, female and male participants were combined and birth cohort, sex, and race/ethnicity were included as control variables. Models 2 (female) and 3 (male) were sex-stratified versions of Model 1. Model 4 (female and male participants combined) was an interactive model, which included 2-way interactions between birth cohort and age, birth cohort and sex, and birth cohort and race/ethnicity. Model 4 provides tests of whether the HRs associated with age, sex, and race/ethnicity have changed over birth cohorts.
All estimates, including HR model parameter estimates, were weighted using weights supplied in each study. Variance estimates accounted for survey weights, clustering, and stratification.44 Baseline sample weights provided in each data set were used. The ADDTH and NLSY97 data sets had overlapping age by cohort data for certain age cohorts between 1997 and 2007; sampling weights in these 2 combined data sets were down weighted by the fraction of the total unweighted sample size in order to avoid “double counting” of population estimates.45 All analyses were performed in R, version 3.6.3.
RESULTS
Unweighted descriptive characteristics are shown in Table 1. At initial wave, 49.40% were female, 16.86% were Black, and 18.62% were Hispanic. Mean BMI was 19.58 kg/m2 and 11.63% were obese at the initial wave.
Table 1.
Unweighted Descriptive Statistics of the Pooled Data (n=64,772)
| Characteristic | Pooled | NLSY79 | ADDTH | NLSY97 | ECLS-K:1998 | ECLS-K:2011 |
|---|---|---|---|---|---|---|
| Birth cohorts, range | 1957–2006 | 1957–1965 | 1974–1984 | 1979–1985 | 1991–1994 | 2003–2006 |
| Sample size (% of pooled sample) | 64,772 (100) | 5,849 (9.03) | 18,414 (28.43) | 8,528 (13.17) | 18,995 (29.33) | 12,986 (20.05) |
| Study years, range | 1981–2016 | 1981–1994 | 1995–2007 | 1997–2014 | 1998–2007 | 2010–2016 |
| Number of waves | 43 | 10 | 4 | 16 | 6 | 7 |
| Mean follow-up, years | 8.74 | 9.22 | 10.65 | 14.00 | 6.50 | 5.66 |
| Characteristics at Initial Wave | ||||||
| Age range, years | 4–24 | 16–24 | 11–21 | 12–18 | 4–7 | 4–7 |
| Mean age (SD) | 10.66 (5.73) | 19.51 (2.24) | 15.7 (1.74) | 14.38 (1.49) | 5.14 (0.41) | 5.13 (0.41) |
| Mean BMI (SD) | 19.58 (4.82) | 23.02 (3.65) | 22.95 (4.77) | 22.09 (4.67) | 16.27 (2.19) | 16.43 (2.20) |
| Percentage obese (SD) | 11.63 (32.06) | 5.40 (22.61) | 12.12 (32.63) | 11.73 (32.17) | 11.56 (31.97) | 13.79 (34.48) |
| Percentage female | 49.40 | 50.95 | 50.41 | 47.97 | 49.03 | 48.75 |
| Percentage male | 50.60 | 49.05 | 49.59 | 52.03 | 50.97 | 51.25 |
| Percentage White | 64.52 | 80.63 | 61.57 | 53.90 | 67.12 | 64.60 |
| Percentage Black | 16.86 | 12.24 | 21.48 | 20.19 | 14.96 | 13.00 |
| Percentage Hispanic | 18.62 | 7.13 | 16.95 | 25.90 | 17.93 | 22.40 |
Note: Total of 718,560 person-years of data. Racial categories Whites and Black are non-Hispanics.
NLSY, National Longitudinal Survey of Youth 1979 and 1997; ADDTH, National Longitudinal Study of Adolescent Health; ECLS, Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 and 2011.
Figure 1 shows obesity incidence expressed as a percentage by age and study based on the semi-parametric model. Before age 15 years, incidence followed an inverted U-shape with peak incidence at approximately age 9 years in the ECLS cohorts (those born in 1991–1994 and 2003–2006). The pattern suggests decreasing incidence in early adolescence and then rising incidence from approximately age 15 years into early adulthood. In the NLSY97 (born 1979–1985) and ADDTH (1974–1984), obesity incidence approximately tripled from 2% at age 15 years to 5%–6% by age 30 years. For the earlier NSLY79 cohort (born 1979–1985), incidence also increased with age, although the level of incidence was considerably lower than in the NLSY97 (born 1979–1985) and ADDTH (1974–1984) cohorts.
Figure 1.
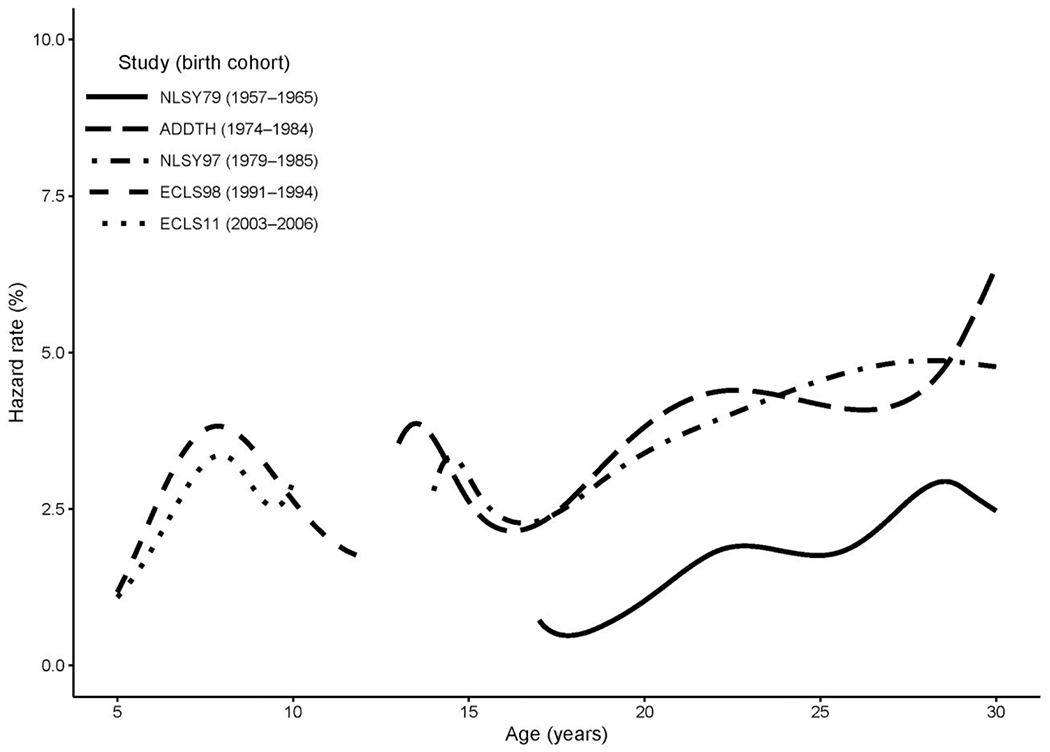
Hazard of incident obesity expressed as a percentage by birth cohort and age.
NLSY, National Longitudinal Survey of Youth 1979 and 1997; ADDTH, National Longitudinal Study of Adolescent Health; ECLS, Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 and 2011.
Table 2 shows HRs of incident obesity. On average, incidence increased 6.00% (HR=1.060, 95% CI=1.061, 1.067) for each additional year of age and female participants had 9.9% (HR=1.099, 95% CI=1.047, 1.155) higher incidence compared with male participants (p<0.001) (Model 1). Blacks (HR=1.459, p<0.001) and Hispanics (HR=1.485, p<0.001) had a higher incidence compared with Whites (Model 1). Among the study cohorts covering adolescence and young adulthood (NLSY79, ADDTH, NLSY97), those in NLSY97 (born 1979–1985) and ADDTH (born 1974–1984) had significantly (p<0.001) higher obesity incidence (HR=2.256 and HR=2.185, respectively) compared with the NLSY79 cohort (born: 1957–1967). Among the younger-aged study cohorts (ECLS-K:1998, ECLS-K:2011), those in ECLS-K:2011 (born 2003–2006) had slightly lower incidence compared with those in ECLS-K: 1998, but this comparison was not statistically significant at the p=0.05 level (HR=0.985, p=0.712). Patterns for each sex (Models 2 and 3) did not differ markedly from each other.
Tahle 2.
Hazard Ratios (HRs) of Incident Obesity Using the Pooled Data (n=64,772)
| Characteristic | Total Model 1 HR (95% CI) |
Male Model 2 HR (95% CI) |
Female Model 3 HR (95% CI) |
|---|---|---|---|
| Age | 1.060 (1.054, 1.067) | 1.061 (1.051, 1.070) | 1.060 (1.051, 1.069) |
| Sex | |||
| Male | 1.000 | 1.000 | 1.000 |
| Female | 1.099 (1.047,1.155) | – | – |
| Birth cohort (birth year) | |||
| NLSY79 (1957–1967) | 1.000 | 1.000 | 1.000 |
| ADDTH (1974–1984) | 2.256 (2.074, 2.455) | 2.359 (2.076, 2.680) | 2.174 (1.943, 2.431) |
| NLSY97 (1979–1985) | 2.185 (2.002, 2.384) | 2.366 (2.077, 2.696) | 2.039 (1.813, 2.295) |
| ECLS-K:1998 (1991–1994) | 3.459 (3.045, 3.928) | 4.381 (3.633, 5.283) | 2.738 (2.300, 3.261) |
| ECLS-K:2011 (2003–2006) | 3.405 (2.957, 3.921) | 4.437 (3.615, 5.446) | 2.592 (2.130, 3.154) |
| Race | |||
| White | 1.000 | 1.000 | 1.000 |
| Black | 1.459 (1.370, 1.553) | 1.218 (1.109, 1.337) | 1.711 (1.572, 1.863) |
| Hispanic | 1.485 (1.398, 1.577) | 1.370 (1.257, 1.494) | 1.611 (1.480, 1.753) |
| Intercept | 0.012 (0.011, 0.013) | 0.011 (0.010, 0.013) | 0.013 (0.012, 0.015) |
Note: Age has been centered at its grand mean. Racial categories Whites and Black are non-Hispanics. Total of 718,560 person-years of data.
NLSY, National Longitudinal Survey of Youth 1979 and 1997; ADDTH, National Longitudinal Study of Adolescent Health; ECLS, Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 and 2011.
To evaluate changes over the studies, Table 3 shows study-specific HRs for age, sex, and race/ethnicity. Male and female cohorts were combined. Comparisons of similar-aged cohorts were investigated: ECLS-K: 1998 and ECLS-K:2011 for respondents aged <15 years and NLSY79, NLSY97, and ADDTH for adolescents and young adults. Comparing birth cohorts at similar ages, there were no statistically significant (p=0.05 threshold) differences in the female-to-male ratio over the cohorts (e.g., the 95% CIs for the HRs for female overlapped among NSLY79, NLSY97, and ADDHLTH as well as between ECLS98 and ECLS11). Blacks and Hispanics had higher incidence relative to Whites in all cohorts. There was no indication of widening race/ethnic disparities in the HRs over the study cohorts at younger (ECLS-K: 1998, ECLS-K:2011) or older ages (NLSY79, ADDTH, NLSY97).
Table 3.
Hazard Ratios (HRs) From Models Including Interactions Between Study Cohort and Age, Sex, and Raee/Ethnicity Using the Pooled Data (n=64,772)
| Characteristic | Total Model 4 HR (95% CI) |
|---|---|
| Age | |
| NLSY79 (1957–1967) | 1.112 (1.089, 1.137) |
| ADDTH (1974–1984) | 1.050 (1.040, 1.061) |
| NLSY97 (1979–1985) | 1.058 (1.049, 1.067) |
| ECLS-K:1998 (1991–1994) | 0.985 (0.968, 1.002) |
| ECLS-K:2011(2003–2006) | 1.166 (1.122, 1.212) |
| Sex | |
| Female (ref: males) | |
| NLSY79 (1957–1967) | 1.257 (1.079, 1.464) |
| ADDTH (1974–1984) | 1.169 (1.083, 1.262) |
| NLSY97 (1979–1985) | 1.096 (1.004, 1.196) |
| ECLS-K:1998 (1991–1994) | 0.809 (0.734, 0.892) |
| ECLS-K:2011(2003–2006) | 0.760 (0.664, 0.870) |
| Race/ethnicity | |
| NH Blacks (ref: NH Whites) | |
| NLSY79 (1957–1967) | 1.631 (1.339, 1.986) |
| ADDTH (1974–1984) | 1.445 (1.321, 1.581) |
| NLSY97 (1979–1985) | 1.367 (1.227, 1.524) |
| ECLS-K:1998 (1991–1994) | 1.532 (1.338, 1.755) |
| ECLS-K:2011(2003–2006) | 1.374 (1.118, 1.688) |
| Hispanics (ref: NH Whites) | |
| NLSY79 (1957–1967) | 1.670 (1.287, 2.168) |
| ADDTH (1974–1984) | 1.261 (1.129, 1.410) |
| NLSY97 (1979–1985) | 1.564 (1.418, 1.724) |
| ECLS-K:1998 (1991–1994) | 1.499 (1.332, 1.687) |
| ECLS-K:2011(2003–2006) | 1.750 (1.509, 2.028) |
Note: Model controls for main effects of study cohort, age sex, race/ethnicity. Total of 718,560 person-years of data.
NLSY, National Longitudinal Survey of Youth 1979 and 1997; ADDTH, National Longitudinal Study of Adolescent Health; ECLS, Early Childhood Longitudinal Study-Kindergarten cohorts of 1998 and 2011.
DISCUSSION
Three key findings emerged. First, obesity incidence changes in a highly non-linear pattern by age, increasing from age 4 years, peaking at around age 9 years, and subsequently declining until adolescence, after which it rises into young adulthood. Second, among adolescents, obesity incidence more than doubled between the cohorts born in 1957–1965 and those born in 1974–1985. By contrast, there were no significant changes in incidence among those born in 1991–1994 and 2003–2006 aged <15 years. Third, Blacks and Hispanics, relative to Whites, had higher obesity incidence at all ages with no appreciable changes in the disparities on the relative scale.
Van Cleave et al.28 analyzed the NLSY-Child Cohort of 1980–1988, reporting an incidence of 1.7% for children aged 4.5–10.5 years in the U.S. Using the same data, Strauss and Knight31 reported an incidence rate of 1.3%. For children aged 4–8 years, an incidence rate of 1.4% was observed in 1999 and 1.0% in 2011. One study reported an adjusted incidence rate of 6.4% for Americans aged 18–29 years, but that study was based on an indirect assessment of incidence from the cross-sectional 2019 Behavioral Risk Factors Surveillance System.46 The estimates in this age range from the ADDTH and NLSY97 ranged from approximately 2.5% to 6%. Cunningham and colleagues27 reported that incidence decreased from 5.4% during kindergarten (age 5–6 years) to 1.7% between fifth and eighth grade (age 9–14 years). However, Cunningham et al. investigated the first onset of obesity in children, whereas this study allowed for recurrence of incidence. Eight percent of individuals experiencing an incident event had a recurrent event.
The shape of the incidence pattern observed here is likely a function of many social and biological processes occurring across developmental stages. These estimates suggest that incidence rises through the early schooling years. Datar and colleagues,47 using the ECLS-K:1998, found that the largest weight gain during the elementary school years was between the first and third grade and this was most pronounced among Hispanics. Although Datar et al., like this study, did not examine the reasons for this growth, the pattern suggests that school-based exposures such as changes in dietary patterns due to the influence of other children or being outside of the home for extended periods, combined with insufficient physical activity throughout the school day, may be contributing factors. After early childhood, the second increase in incidence by age began in early adolescence and persisted into early adulthood. This rise may be precipitated in part to the onset of puberty, which is associated with weight gain especially among girls,48 and reinforced by poor diet throughout the teenage and young adulthood years. The persistent disparities by race/ethnicity are furthermore a function of many interacting social and behavioral factors. The role of early-life factors in contributing to the higher levels of childhood obesity among non-Hispanic Blacks and Hispanics has received considerable attention,49,50 particularly the roles of maternal depression, early introduction of solid foods, and low levels of breastfeeding. Structural factors such as neighborhood environment, food deserts, and racism are also thought to be important contributors.51,52
Using cross-sectional data, Ogden and colleagues5 documented obesity prevalence trends by age groups between 1999–2000 and 2017–2018, finding no significant trend in obesity across cohorts during early childhood (age 2–5 years), but moderate increases between ages 6 and 8 years (15.8% to 19.3%) and more substantial ones in adolescence (16.0% to 20.9%). Consistent with these snapshots, the findings in this study suggest little change in incidence between cohorts born in the early 1990s and those born in the early 2000s between ages 4 and 7 years. There were sizeable increases between the 1957–1965 birth cohort and those born in the 1970s and first half of the 1980s.
Earlier work has shown that Black and Hispanic adolescents, compared with White adolescents, have higher incidence of transitioning to obesity and lower incidence of transitioning from being obese to non-obese.27,31,53–56 The findings in this study indicate that, on the relative scale, there has been no widening in racial/ethnic disparities in incidence. With increasing obesity levels, however, stable relative differences over time translate into wider absolute differences over time and are therefore consistent with widening absolute racial/ethnic differences in obesity prevalence documented by Ogden et al.47 Hispanic and non-Hispanic Black children represent a growing percentage of all children, and if current patterns persist into the future, a larger share of American children may become obese.
Limitations
This study had limitations. No single study covered the entire analyzed age range. Data on earlier cohorts at younger ages or more recent cohorts at older ages were not available. Though all data sets were nationally representative of the U.S. population of a given cohort at the time of enrollment (with the exception of those aged 4 years in the ECLS-K data sets), there is no attempt to refresh a given panel with immigrants. Given relatively low immigration rates for non-Hispanic Whites, there should be little impact on representativeness of later waves of this group. For non-Hispanic Blacks and Hispanics, this exclusion may be of bigger concern. The share of the U.S. Black population that is foreign-born has increased appreciably since the 1980s. In 2017, among non-Hispanic Black children aged <18 years, 3% were foreign-born.57 Among Hispanic children aged <18 years, 11% were foreign-born in 2017. Foreign-born children generally have lower obesity prevalence compared with native-born children58 and therefore the estimates of obesity incidence for the Hispanic population and to a lesser extent for the non-Hispanic Black population may be an underestimate.
CONCLUSIONS
Although it is encouraging that the growth in obesity incidence over birth cohorts has appeared to slow, a high proportion of children still become obese prior to their adolescence in recent cohorts. Moreover, incidence rises nearly linearly between ages 15 and 30 years—a span of 15 years—suggesting that successful preventive efforts targeting adolescents and young adults can have a sizeable impact on overall obesity prevalence. Proximally, high caloric intake, consumption of foods with poor nutritional value, and inadequate physical activity are all likely contributors. However, intervening on a broad set of “distal” determinants such as school policies (e.g., promotion of healthy foods/beverages, increasing physical activity) and structural factors (e.g., improving access to maternal/infant care, improving neighborhood environments, reducing discrimination) are critical.59,60 Relatedly, given persistent inequality in obesity incidence by sex and race/ethnicity (and the shifting racial/ethnic composition across cohorts), this study further highlights the continued need for culturally tailored programs for particularly vulnerable populations in this regard, including girls, Hispanics, and Blacks. A priority for future research is to understand how obesity dynamics may be mediated by other factors, such as SES and contextual environments.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank all the researchers and staff who have been involved in collecting the data used in this study. We would also like to thank the editor and 3 reviewers for their careful review and helpful suggestions.
This research was funded by the National Institute of Diabetes and Digestive and Kidney Diseases, grant number R01DK115937. Riosmena also benefited from administrative, research, and computing support through the University of Colorado Population Center funded by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of NIH (P2CHD066613).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All authors declare that there is no conflict of interest, financial or otherwise.
CRediT author statement
Ali Rafei: Conceptualization, Methodology, Software, Formal analysis, Data Curation, Writing - Original Draft, Visualization
Michael R. Elliott: Conceptualization, Methodology, Resources, Writing - Review & Editing, Supervision, Funding acquisition
Rebecca Jones: Writing - Review & Editing
Fernando Riosmena: Writing - Review & Editing
Solveig A. Cunningham: Conceptualization, Resources, Writing - Review & Editing, Supervision, Funding acquisition
Neil K. Mehta: Conceptualization, Methodology, Resources, Writing - Review & Editing, Supervision, Funding acquisition
REFERENCES
- 1.Reither EN, Hauser RM, Yang Y. Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States. Soc Sci Med. 2009;69(10):1439–1448. 10.1016/j.socscimed.2009.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dobson A, Hockey R, Chan H-W, Mishra G. Flexible age-period-cohort modelling illustrated using obesity prevalence data. BMC Med Res Methodol. 2020;20:16. 10.1186/s12874-020-0904-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An R, Xiang X. Age–period–cohort analyses of obesity prevalence in US adults. Public Health. 2016;141:163–169. 10.1016/j.puhe.2016.09.021. [DOI] [PubMed] [Google Scholar]
- 4.Keyes KM, Utz RL, Robinson W, Li G. What is a cohort effect? Comparison of three statistical methods for modeling cohort effects in obesity prevalence in the United States, 1971–2006. Soc Sci Med. 2010;70(7):1100–1108. 10.1016/j.socscimed.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogden CL, Fryar CD, Martin CB, et al. Trends in obesity prevalence by race and Hispanic origin—1999–2000 to 2017–2018. JAMA. 2020;324(12):1208–1210. 10.1001/jama.2020.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Amutha A, Mohan V. Diabetes complications in childhood and adolescent onset type 2 diabetes—a review. J Diabetes Complications. 2016;30(5):951–957. 10.1016/j.jdiacomp.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 8.Nowicki P, Kemppainen J, Maskill L, Cassidy J. The role of obesity in pediatric orthopedics. J Am Acad Orthop Surg Glob Res Rev. 2019;3(5):e036. 10.5435/jaaosglobal-d-19-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Black MH, Zhou H, Takayanagi M, Jacobsen SJ, Koebnick C. Increased asthma risk and asthma-related health care complications associated with childhood obesity. Am J Epidemiol. 2013;178(7):1120–1128. 10.1093/aje/kwt093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arens R, Muzumdar H. Childhood obesity and obstructive sleep apnea syndrome. J Appl Physiol. 2010;108(2):436–444. 10.1152/japplphysiol.00689.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibson-Smith D, Halldorsson TI, Bot M, et al. Childhood overweight and obesity and the risk of depression across the lifespan. BMC Pediatr. 2020;20:25. 10.1186/s12887-020-1930-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindberg L, Hagman E, Danielsson P, Marcus C, Persson M. Anxiety and depression in children and adolescents with obesity: a nationwide study in Sweden. BMC Med. 2020;18:30. 10.1186/s12916-020-1498-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rankin J, Matthews L, Cobley S, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health, Med Ther. 2016;7:125–146. 10.2147/ahmt.sl01631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187–192. 10.4103/2249-4863.154628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blanco M, Solano S, Alcántara A, Parks M, Román F, Sepúlveda A. Psychological well-being and weight-related teasing in childhood obesity: a case–control study. Eat Weight Disord. 2020;25(3):751–759. 10.1007/s40519-019-00683-y. [DOI] [PubMed] [Google Scholar]
- 16.Simmonds M, Llewellyn A, Owen C, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107. 10.1111/obr.12334. [DOI] [PubMed] [Google Scholar]
- 17.Ng CD, Cunningham SA. In, out, and fluctuating: obesity from adolescence to adulthood. Ann Epidemiol. 2020;41:14–20. 10.1016/j.annepidem.2019.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Power C, Lake JK, Cole TJ. Measurement and long-term health risks of child and adolescent fatness. Int J Obes. 1997;21(7):507–526. 10.1038/sj.ijo.0800454. [DOI] [PubMed] [Google Scholar]
- 19.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22(2):167–177. 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 20.Srinivasan SR, Bao W, Wattigney WA, Berenson GS. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart Study. Metabolism. 1996;45(2):235–240. 10.1016/s0026-0495(96)90060-8. [DOI] [PubMed] [Google Scholar]
- 21.Cunningham SA, Datar A, Narayan KMV, Kramer MR. Entrenched obesity in childhood: findings from a national cohort study. Ann Epidemiol. 2017;27(7):435–441. 10.1016/j.annepidem.2017.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89(3):309–319. 10.1016/j.diabres.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 23.Abdullah A, Stoelwinder J, Shortreed S, et al. The duration of obesity and the risk of type 2 diabetes. Public Health Nutr. 2011;14(1):119–126. 10.1017/s1368980010001813. [DOI] [PubMed] [Google Scholar]
- 24.Mehta NK, Stenholm S, Elo I, Aromaa A, Heliövaara M, Koskinen S. Weight histories and mortality among Finnish adults: the role of duration and peak body mass indix. Epidemiology. 2014;25(5):707–710. 10.1097/ede.0000000000000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Preston SH, Mehta NK, Stokes A. Modeling obesity histories in cohort analyses of health and mortality. Epidemiology. 2013;24(1):158–166. 10.1097/ede.0b013e3182770217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2016;17(1):56–67. 10.1111/obr.12316. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham SA, Kramer MR, Narayan K. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370(5):403–411. 10.1056/nejmoa1309753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. JAMA. 2010;303(7):623–630. 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- 29.Stevens J, Murray DM, Baggett CD, et al. Objectively assessed associations between physical activity and body composition in middle-school girls: the Trial of Activity for Adolescent Girls. Am J Epidemiol. 2007;166(11):1298–1305. 10.1093/aje/kwm202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson DR, Obarzanek E, Franko DL, et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2007;150(1):18–25. 10.1016/j.jpeds.2006.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103(6):e85. 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 32.Cheung PC, Cunningham SA, Narayan KV, Kramer MR. Childhood obesity incidence in the United States: a systematic review. Child Obes. 2016;12(1):1–11. 10.1089/chi.2015.0Q55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rothstein DS, Carr D, Cooksey E. Cohort profile: the national longitudinal survey of youth 1979 (NLSY79). Int J Epidemiol. 2019;48(1):22–22e. 10.1093/ije/dyy133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moore W, Pedlow S, Krishnamurty P, Wolter K, Chicago I. National longitudinal survey of youth 1997 (NLSY97). National Opinion Research Center, Chicago, IL. 2000;254. [Google Scholar]
- 35.Harris KM, Halpern CT, Whitsel EA, et al. Cohort profile: The National Longitudinal Study of Adolescent to Adult Health (ADDTH). Int J Epidemiol. 2019;48(5):1415–1415k. 10.1093/ije/dyz115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tourangeau K, Nord C, Lê T, Sorongon AG, Najarian M. Early Childhood Longitudinal Study, Kindergarten Class of 1998-99 (ECLS-K): Combined User’s Manual for the ECLS-K Eighth-Grade and K-8 Full Sample Data Files and Electronic Codebooks. NCES 2009-004. National Center for Education Statistics. 2009. [Google Scholar]
- 37.Tourangeau K, Nord C, Lê T, et al. Early Childhood Longitudinal Study, Kindergarten Class of 2010-11 (ECLS-K: 2011). User’s Manual for the ECLS-K: 2011 Kindergarten Data File and Electronic Codebook, Public Version. NCES 2015-074. National Center for Education Statistics. Published 2015. [Google Scholar]
- 38.U.S. Bureau of Labor Statistics. National longitudinal survey of youth 1979 cohort, 1981–2016 (rounds 3–27). Center for Human Resource Research; 2019. [Google Scholar]
- 39.U.S. Bureau of Labor Statistics. National longitudinal survey of youth 1997 cohort, 1997–2015 (rounds 1–23). Center for Human Resource Research; 2019. [Google Scholar]
- 40.Harris KM, Halpern CT, Whitsel E, et al. The national longitudinal study of adolescent to adult health: study design. http://www.cpc.unc.edu/projects/addhealth/design. Published 2003. Accessed January 27, 2022.
- 41.Patel SA, Winkel M, Ali MK, Narayan KV, Mehta NK. Cardiovascular mortality associated with 5 leading risk factors: national and state preventable fractions estimated from survey data. Ann Intern Med. 2015;163(4):245–253. 10.7326/m14-1753. [DOI] [PubMed] [Google Scholar]
- 42.Kuczmarski RJ. CDC growth charts: United States. HHS, Centers for Disease Control and Prevention, National Center for Health Statistics; 2000. [Google Scholar]
- 43.Allison PD. Discrete-time methods for the analysis of event histories. SociolMethodol. 1982;13:61–98. [Google Scholar]
- 44.Binder DA. On the variances of asymptotically normal estimators from complex surveys. Int Stat Rev. 1983;51(3):279–292. 10.2307/1402588. [DOI] [Google Scholar]
- 45.Korn EL, Graubard BI. Analysis of health surveys. Vol 323. John Wiley & Sons; 2011. [Google Scholar]
- 46.Pan L, Freedman DS, Gillespie C, Park S, Sherry B. Incidences of obesity and extreme obesity among US adults: findings from the 2009 Behavioral Risk Factor Surveillance System. Popul Health Metr. 2011;9(1):56. 10.1186/1478-7954-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Datar A, Shier V, Sturm R. Changes in body mass during elementary and middle school in a national cohort of kindergarteners. Pediatrics. 2011;128(6):e141l–e1417. 10.1542/peds.2011-0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jasik CB, Lustig RH. Adolescent obesity and puberty: the “perfect storm”. Ann N Y Acad Sci. 2008;1135(1):265–279. 10.1196/annals.1429.009. [DOI] [PubMed] [Google Scholar]
- 49.Kumanyika SK. Environmental influences on childhood obesity: ethnic and cultural influences in context. Physiol Behav. 2008;94(1):61–70. 10.1016/j.physbeh.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 50.Isong IA, Rao SR, Bind MA, Avendaño M, Kawachi I, Richmond TK. Racial and ethnic disparities in early childhood obesity. Pediatrics. 2018;141(1):e20170865. 10.1542/peds.2017-0865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sharifi M, Sequist TD, Rifas-Shiman SL, et al. The role of neighborhood characteristics and the built environment in understanding racial/ethnic disparities in childhood obesity. Prev Med. 2016;91:103–109. 10.1016/j.ypmed.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Caprio S, Daniels SR, Drewnowski A, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment. Diabetes Care. 2008;31(11):2211–2221. 10.2337/dc08-9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huh D, Stice E, Shaw H, Boutelle K. Female overweight and obesity in adolescence: developmental trends and ethnic differences in prevalence, incidence, and remission. J Youth Adolesc. 2012;41(1):76–85. 10.1007/s10964-011-9664-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim J, Must A, Fitzmaurice GM, et al. Incidence and remission rates of overweight among children aged 5 to 13 years in a district-wide school surveillance system. Am J Public Health. 2005;95(9):1588–1594. 10.2105/ajph.2004.054015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rendall MS, Weden MM, Fernandes M, Vaynman I. Hispanic and black US children’s paths to high adolescent obesity prevalence. Pediatr Obes. 2012;7(6):423–435. 10.1111/j.2047-6310.2012.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nntr. 2004;80(3):569–575. 10.1093/ajcn/80.3.569. [DOI] [PubMed] [Google Scholar]
- 57.Child Trends. Immigrant children. https://www.childtrends.org/indicators/immigrant-children. Published 2018. Accessed November, 2018.
- 58.Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009;34(4):271–281. 10.1007/s10900-009-9148-6. [DOI] [PubMed] [Google Scholar]
- 59.Lambrinou CP, Androutsos O, Karaglani E, et al. Effective strategies for childhood obesity prevention via school based, family involved interventions: a critical review for the development of the Feel4Diabetes-study school based component. BMC Endocr Disord. 2020;20(2):52. 10.1186/s12902-020-0526-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA Pediatr. 2013;167(8):731–738. 10.1001/jamapediatrics.2013.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


