Abstract
Background:
The growing nurse practitioner (NP) workforce plays a critical role in primary care delivery in the United States. However, better recruitment and retention of the robust NP workforce in underserved areas are needed; evidence to inform such effort is limited.
Purpose:
This scoping review aimed to examine the findings, scope, and knowledge gaps of available literature on factors associated with NP recruitment and retention in underserved areas.
Methods:
This review was guided by Joanna Briggs’ Scoping Review Methodology and PRISMA-SCR reporting standards. Literature search for peer-reviewed and gray literature was conducted in six databases.
Findings:
A total of 22 studies met inclusion criteria. Factors associated with NP recruitment and retention in underserved areas were mapped into five themes, including factors related to: the individual NP, NP education programs/financial aid, organizations employing NPs, the communities NPs work in, and autonomous practice. Majority of the included studies were published before 2010; few used rigorous study designs and analysis methods; and few exclusively studied NPs and unique challenges facing the NP workforce.
Discussion and Conclusion:
Available studies show that NP recruitment and retention can be addressed by various stakeholders (e.g., educators, policy makers); however, up-to-date, methodologically rigorous, and NP-focused studies are needed.
Keywords: Nurse practitioner, scoping review, recruitment, retention, workforce, underserved population, underserved area
Primary care, a critical sector of the United States healthcare system, improves health outcomes and reduces mortality across the lifespan (National Academy of Medicine, 2021; Starfield et al., 2005). Despite its merits, the nation continues to struggle with inadequate primary care access and persistent workforce shortages. These issues may be aggravated as the 65 and older population increases (Dall et al., 2020) and efforts to increase healthcare access, such as the executive order to strengthen Medicaid and the Affordable Care Act (Exec. Order No. 14009, 2021), expand healthcare coverage among Americans.
The healthcare workforce shortage is worse in certain geographic areas, and may be attributed to maldistribution, where providers are concentrated in metropolitan areas and insufficient in rural and/or low-income areas (Naylor et al., 2019). The consequences of this maldistribution are especially concerning as individuals in these underserved communities have poorer health and may need more healthcare services to maintain their health. For example, rural residents are more likely to be older, obese, low-income, and use tobacco compared to residents in metropolitan areas (Meit et al., 2014; US Department of Agriculture, 2021).
The growing nurse practitioner (NP) workforce is a solution to meeting the nation’s primary care demands and increasing access to care. The NP workforce grew by 109% from 2010–2017 (Auerbach et al., 2020), and is projected to continue growing at 6.8% annually (Auerbach et al., 2018). NPs provide cost-efficient and high-quality care with comparable or better outcomes than physician care (Muench et al., 2019; Swan et al., 2015). Compared to physicians, NPs are also more likely to work in underserved areas and care for vulnerable populations, including rural, non-white, and Medicare-Medicaid dual-eligible patients (Buerhaus et al., 2018; DesRoches et al., 2013). While physician supply has decreased in rural and low-income areas, the supply of actively practicing NPs has grown (Xue et al., 2019).
Despite their propensity for working with underserved populations, the NP workforce is also experiencing a degree of maldistribution. Although the NP workforce has and will continue to grow, the robust NP supply is not well-reflected in underserved areas. For example, in a sample of rural health clinics, half of the clinics reported difficulty recruiting NPs (Wright et al., 2015). Nationwide, 50% of community health centers—safety net institutions caring for underserved populations—reported at least one NP position vacancy, with an average of five months to fill a vacancy (National Association of Community Health Centers, 2016). More primary care NP graduates have chosen to work in private practices compared to community health or federally qualified health centers (Faraz & Salsberg, 2019).
By ensuring that the robust NP workforce is well-distributed to areas with the most need, NPs’ impact in increasing primary care access and reducing health disparities can be maximized. To develop strategies to improve NP distribution, it is important to first understand what factors help to recruit and retain NPs in underserved areas. This knowledge, however, is limited. Majority of studies on clinician recruitment and retention in underserved areas focus on physicians and physician assistants (Goodfellow et al., 2016; MacQueen et al., 2018; Rabinowitz et al., 2000; Smith et al., 2012; Walker et al., 2010; Yuen & Lessard, 2018). While these studies produce critical insights, they cannot be fully utilized to inform recruitment and retention strategies for NPs as NPs have unique professional attributes, such as state-level scope of practice policies that determine NPs’ ability to independently deliver care to patients (American Association of Nurse Practioners, 2021).
Currently, no synthesis of evidence on recruitment and retention of NPs in underserved areas exist, and little is known about the content, scope, and gaps of this literature. Thus, we conducted a scoping review. Scoping reviews are ideal to provide an overview of extant knowledge, especially for an unexplored body of literature (Munn et al., 2018; Peters et al., 2015, 2020; Pollock et al., 2021). More specifically, the purpose of this scoping review is to 1) map factors associated with NP recruitment and retention in underserved areas from available literature; 2) examine the characteristics and scope of current literature (e.g., study designs, populations studied); and 3) assess gaps and discuss implications for future studies.
Method
We followed the Joanna Brigg’s scoping review framework (Peters et al., 2015) and results are reported according to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews) reporting guidelines (Tricco et al., 2018) (see supplementary materials for PRISMA-ScR reporting checklist). The Population-Concept-Context framework (Peters et al., 2015) was used to inform the inclusion criteria and search strategies for studies (Table 1). An a priori protocol was developed and uploaded to Open Science Framework website (Kueakomoldej, 2021). Unlike systematic reviews which focus on appraisal and synthesis of findings for targeted research questions, scoping reviews prioritize breadth in their inclusion criteria to fully understand the range of evidence available (Peters et al., 2015, 2020). Studies are included regardless of quality, and appraisal of individual studies are usually not completed with scoping reviews (Peters et al., 2015).
Table 1.
Population-Concept-Context Framework
| Criteria | Concept | Search terms |
|---|---|---|
| Population | Nurse practitioner | Nurse practitioner, NP, advanced practice nurse, APN |
|
| ||
| Concept | Recruitment and retention | Recruitment, retention, stay, practice, staffing, turnover, quit, relocate, remain, retain |
|
| ||
| Context | Underserved areas | Underserved, health professional shortage area (HPSA), rural, rural health clinics, indian, tribal, federally qualified health centers, community health centers, remote |
| Primary care | Primary care, family practice, general practice | |
Note. Population-Concept-Context Framework from Peters et al. (2015)
Eligibility Criteria
Studies were included in this review if they examined factors associated with recruitment and/or retention of primary care NPs in underserved areas. Informed by recruitment and retention studies in extant literature, recruitment was defined as attracting or placing NPs in positions in underserved areas (MacQueen et al., 2018; Walker et al., 2010); retention was defined as keeping NPs in positions in underserved areas (Rabinowitz et al., 2001). Recruitment and retention can be measured by either objective measures (e.g., retention rate, employment time) or subjective report (e.g., practice location decision, intent to stay in underserved area). NPs studied must provide direct patient care in the primary care setting; studies examining NPs in acute care settings, education, or non-patient facing roles were excluded.
In our review, underserved areas refer to settings frequently faced with primary care provider shortages, more specifically: a) settings with Health Professional Shortage Area (HPSA) status—a federal designation identifying areas, populations, or facilities with health professional shortages (Health Resources and Services Administration, 2021); b) rural areas including rural health clinics; and c) health centers caring for underserved populations, such as federally qualified and community health centers. To best understand the scope of extant literature, we did not restrict our search by timeframe. Also, studies did not need to exclusively focus on NPs (e.g., NPs may be studied collectively with other providers).
Relevant peer-reviewed quantitative, qualitative, and mixed method studies were considered for inclusion. Gray literature was also included to maximize breadth of search and understanding of the literature body. Gray literature had to report empirical data (e.g., dissertation, program reports and evaluations) to be considered; editorials and expert opinions were excluded. Only U.S. studies were included due to vast regulatory and cultural differences between NPs in different countries (Pulcini et al., 2010; Sheer & Wong, 2008).
Information Sources and Search Strategy
After search strategy consultation with a library informationist, a comprehensive literature search was completed in six databases: PubMed, Embase, Scopus, CINAHL, PsycINFO, and ProQuest (see complete search strategy in supplementary materials). Gray literature hand search, using a combination of terms in Table 1, was completed in Google, Google Scholar, Agency for Healthcare and Research Quality (AHRQ) website, EvidenceNOW, and relevant NP association websites such as American Association of Nurse Practitioners (www.AANP.com). Included studies’ reference lists were also searched for additional studies. Results were imported into Covidence, a review management program (Veritas Health Innovation, n.d.), for screening and data management.
Study Selection and Data Extraction
Literature search retrieved 2351 articles. After duplicate removal, 1185 abstracts were screened, and then, 45 full-text articles were assessed for eligibility. Seven additional studies were found from reference lists of eligible studies and gray literature search (see Figure 1 for PRISMA diagram). Studies were independently screened by SK and AM; discrepancies were discussed and conflicts were resolved with a third author (ET). A total of three meetings were held to discuss conflicts. Data were independently extracted by SK and ET using a standardized form. After all studies were extracted, data were reviewed and conflicts were resolved with discussion by the two authors. A third author (LP) was available for any unresolved conflicts.
Figure 1.
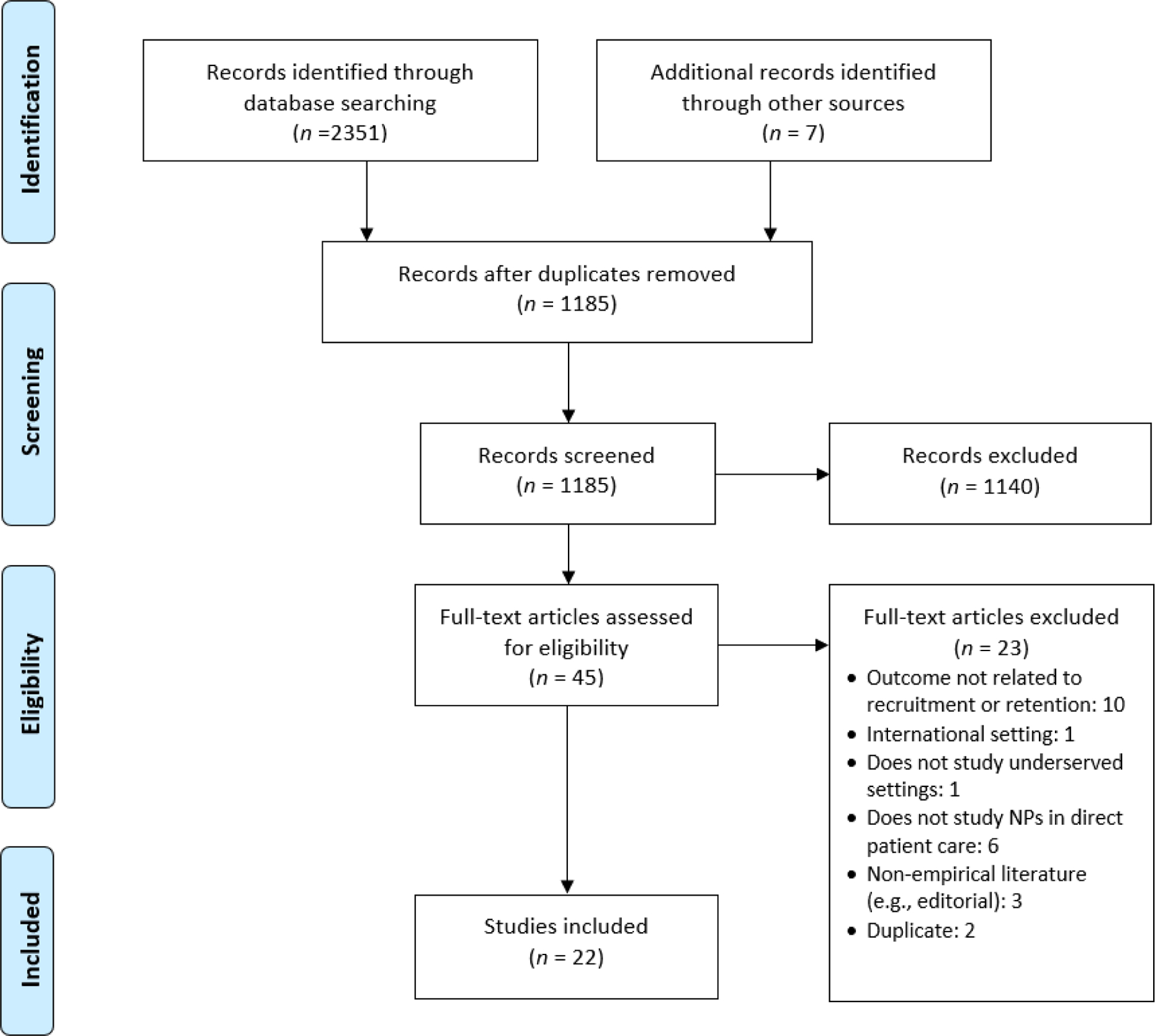
PRISMA Diagram
The data extraction form included author information, year published, study design, analysis method, purpose, study sample, setting, measure of recruitment/retention, and key findings. Factors found to influence NP recruitment and retention in underserved areas were grouped together into common themes by the researchers. The findings were then discussed narratively in the Results section, tabulated in Table 2, and visually mapped in Figure 2. In this review, clinicians refer to study samples that included healthcare professionals beyond NPs (e.g., physicians, physician assistants, nurses).
Table 2.
Summary of Reviewed Articles
| Author (year) | Study design | Analysis method | Purpose of study | Sample and setting | Measure of recruitment and/or retention | Key findings associated with recruitment and/or retention |
|---|---|---|---|---|---|---|
| Andrus & Fenley (1976) | Program Report/Evaluation | Descriptive statistics | Describe and evaluate a rural NP training program | 10 NP graduates from rural California counties at UC Davis NP training program, evaluated years 1970–1976 | Practice in rural area |
|
| Aysola et al. (2015) | Cross-sectional | Multivariable analysis | Evaluate the effectiveness of 1) health professional training program, 2) area health education center program, and 3) career ladder program on provider recruitment and retention | 391 CHCs (employing NPs) in the United States | Practice-reported difficulty in primary care provider recruitment and retention |
|
| Bailey (1997) | Mixed Methods | Quant: Multivariable analysis Qual: Inductive analysis |
Assess the characteristics of communities that maintain access to care and the characteristics of NPs and PAs that practice in these communities | 500 community residents, 11 NPs and 19 Pas from frontier communities in Colorado, Montana, North Dakota, South Dakota, Utah, and Wyoming | NP/PAs practiced for three or more years in a frontier community vs left before three years |
|
| Daniels et al. (2007) | Longitudinal cohort | Multivariable analysis | Examine factors associated with recruitment and retention of health care professional graduates | 765 health professional program graduates from University of New Mexico (incl. MDs, NPs, PAs,) | Whether participant’ s first employment is rural or moved to rural if previously urban, and whether rural participant stayed rural |
|
| Doyle et al. (2017) | Retrospective cohort | Descriptive statistics | Assess the effectiveness of the Advanced Nursing Education Expansion (ANEE) program. | 26 ANEE program grantees and 172 NP graduates | Practice location after graduation |
|
| Edwards et al. (2006) | Cross-sectional | Descriptive statistics | Examine the effect of East Tennessee State University’s Title VII & VIII programs to promote interest in rural/underserved practices | 371 family medicine and 342 NP program graduates from East Tennessee State University | Practice location of graduates |
|
| Flinter (2011) | Program Report/Evaluation | Descriptive statistics | Describe and evaluate an NP residency program in a FQHC | 16 NP residents at an FQHC in Connecticut | Practice in FQHC after graduation |
|
| Fowkes et al. (1994) | Mixed methods | Quant: Descriptive statistics and bivariate analysis Qual: No information provided |
Describe and evaluate the effectiveness of training programs in preparing graduates for practice in underserved areas | 51 NP, PA, and nurse midwife training programs in the US that prepare graduates for practice in underserved areas (43 PA, NP, and CNM graduates interviewed) | Quant: Program success defined as >60% of graduates in primary care and >25% in HPSA practices; towns with <10,000 population, or >60% serving in other underserved areas. Qual: Decision to practice in underserved area |
|
| Gilman (2013) | Program Report/Evaluation | Descriptive statistics | Examine what draws health professionals to working in Delaware, what factors attract them to Delaware’s underserved areas, and what factors retain those who participate in obligatory health care recruitment programs | 38 healthcare professionals (including MDs, NPs, PAs) in Delaware who participated in obligatory health care recruitment programs (NHSC, Delaware state loan repayment program, J1 visa) | Whether participant stays or relocates after end of obligatory service |
|
| Hafferty & Goldberg (1986) | Cross-sectional | Multivariable analysis | Examine how different training pathways place NPs and PAs in targeted areas | 210 NP and PA students from the Primary Care Associate Program created to train primary care NPs and PAs for underserved areas in California | Working within the area that NPs or PAs resided in before entering the program |
|
| Holland et al. (2019) | Program Report/Evaluation | Descriptive statistics | Describe and evaluate the Rural Primary Care Scholars Initiative curriculum to prepare NPs for rural practice in Alabama | 47 NP program graduates from the Rural Primary Care Scholars Initiative in rural Alabama | Employment as NPs in rural Alabama |
|
| Kippenbrock (2004) | Cross-sectional | Descriptive statistics | Examine factors associated with NP employment in rural areas | 121 NPs in rural Arkansas | Selection of employment in rural area |
|
| Li et al. (1995) | Qualitative, focus groups | Thematic analysis | To understand the rationale behind career choices for healthcare providers who work with underserved populations | 24 providers (MDs, NPs, PAs and dentist) in Salt Lake City, Utah | Decision to work with underserved populations |
|
| Lindsay (2007) | Qualitative, semi-structured interviews | Thematic analysis | Explore experience of NPs and PAs by gender and geographic area | 55 NPs, PAs, and nurse anesthetists in New York and Pennsylvania | Decision to work in current location (rural vs urban) |
|
| Negrusa et al. (2014) | Program Report/Evaluation | Multivariable analysis | Examine NHSC clinicians’ retention in high-need areas after completion of their program, and characteristics contributing to retention | 1st dataset: 8,973 NHSC participants; over 1 million non-NHSC providers 2nd dataset: 18,500 NHSC participants including MDs, NPs, PAs, social workers, dentists | Serving in the same HPSA and same county or another HPSA in a different county after completion of NHSC program |
|
| Pathman, Fannell et. al (2012) | Program Report/Evaluation | Multivariable analysis | Examine practice, clinician, and experience factors associated with clinicians’ intention to remain at retention program sites | 996 clinicians from NHSC and other similar state-run clinician retention programs, including MDs, NPs, PAs | Anticipated intention to remain at service site for 1, 2, 3, and up to 10 years after end of service term |
|
| Pathman, Konrad et al. (2012) | Program Report/Evaluation | Multivariable analysis | Assess short, medium, and long term retention rates and factors associated with retention for NHSC clinicians | 2,731 NHSC clinicians and alumni including MDs, NPs, PAs, dentists, etc. | Remaining in NHSC practice after completion of program or leaving but working in other underserved practices |
|
| Ryan et al. (1986) | Program Report/Evaluation | Descriptive statistics | Describe and evaluate Georgia Southern College’s program to prepare NP students for rural practice | 28 NP graduates from Georgia Southern College’s rural NP program | Employment in rural area |
|
| Scarbrough et al. (2016) | Cross-sectional | Descriptive statistics and bivariate analysis | Assess NHSC clinicians’ preference for retention strategies | 66 NHSC clinicians in Texas | Preference for retention strategies by NHSC clinicians |
|
| Sinclair-Lian et al. (2008) | Cross-sectional | Descriptive statistics and bivariate analysis | Examine the association between membership in a PBRN and clinician employment time | 95 clinicians (incl. MDs, NPs, PAs) in New Mexico | Quantitative: Mean employment time in underserved practices |
|
| Spetz et al. (2017) | Cross-sectional | Descriptive statistics and bivariate analysis | Compare urban and rural primary care NPs and examine factors that may influence their supply in rural regions | 13,000 NPs from the 2012 National Sample Survey of Nurse Practitioners | Plan to leave position within 1–2 years |
|
| Sullivan et al. (1978) | Cross-sectional | Descriptive statistics and bivariate analysis | Examine the characteristic of rural NPs, their practice characteristics, motivation to practice in rural areas, and satisfaction with the NP role | 525 NP graduates across the U.S. | Selection of rural practice setting |
|
Note. NP = nurse practitioner; MD = physician; PA = physician assistant; CHC = community health center; NHSC = National Health Service Corp; SOP = scope of practice; FQHC = federally qualified health center; HPSA = Health Professional Shortage Area; PBRN = practice-based research network.
Figure 2.
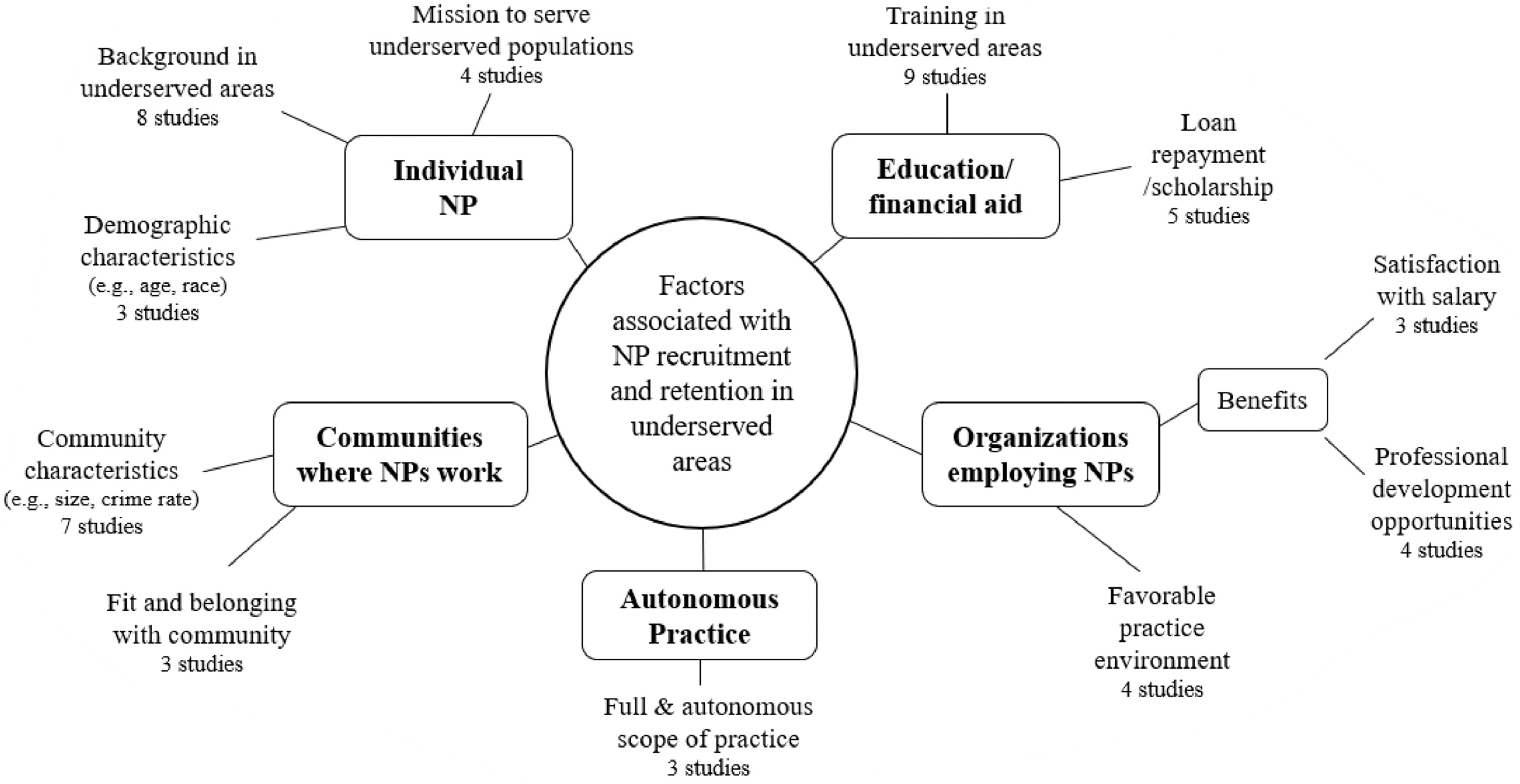
Map of Factors Associated with NP Recruitment and Retention in Underserved Areas
Note. NP = nurse practitioner.
Results
Description and Scope of Included Studies
A total of 22 articles were included in this review. Out of these 22 studies, nine were gray literature (Andrus & Fenley, 1976; Bailey, 1997; Flinter, 2011; Gilman, 2013; Holland et al., 2019; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Ryan et al., 1986) and 13 remaining were peer-reviewed articles. Of the peer-reviewed articles, ten studies were quantitative, two were qualitative, and one was mixed methods. The majority of quantitative studies were cross-sectional (8/10) and two were cohort studies (Daniels et al., 2007; Doyle et al., 2017). Publication date ranged from 1976–2019; most (12/22) of the studies were published before 2010, only one study was published within the past three years (Holland et al., 2019). Majority of the studies inclusively examined recruitment and retention of different healthcare professions (e.g., NPs, physicians, and physician assistants were studied together). Only eight out of the 22 included studies examined recruitment and retention of NPs exclusively (Andrus & Fenley, 1976; Doyle et al., 2017; Flinter, 2011; Holland et al., 2019; Kippenbrock et al., 2004; Ryan et al., 1986; Spetz et al., 2017; Sullivan et al., 1978).
Overview of Findings
Factors associated with NP recruitment and retention in underserved areas were mapped into five themes, including factors related to the individual NP, NP education programs and financial aid, organizations employing NPs, the communities NPs work in, and NPs’ autonomous practice. Studies most frequently focused on NP training (9 studies) and background (8 studies) in underserved areas.
Factors Related to the Individual Nurse Practitioner
A total of 10 studies demonstrated associations between working in underserved areas and clinicians’ individual factors—including background, demographic characteristics, and personal mission to serve (Andrus & Fenley, 1976; Daniels et al., 2007; Fowkes et al., 1994; Hafferty & Goldberg, 1986; Li et al., 1995; Lindsay, 2007; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Ryan et al., 1986). Eight studies found that clinicians who grew up in rural or underserved areas were more likely to practice and stay in such areas (Andrus & Fenley, 1976; Daniels et al., 2007; Fowkes et al., 1994; Hafferty & Goldberg, 1986; Lindsay, 2007; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Ryan et al., 1986). Three studies found that demographic characteristics including older age, whether one has children, and White race were associated with retention in underserved areas (Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012).
Four studies found associations between clinicians’ personal mission to serve underserved populations and their recruitment/retention in underserved areas (Daniels et al., 2007; Li et al., 1995; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012). Researchers discovered themes of moral conviction and strong sense of service when exploring why clinicians chose to work with underserved populations (Li et al., 1995). Daniels et al. also found that clinicians’ mission to serve significantly influenced their decision to choose rural areas as their first practice location (OR = 1.7; CI 95% [1.0, 2.7]) (Daniels et al., 2007).
Factors Related to Nurse Practitioner Education Programs and Financial Aid
A total of 13 studies examined the association between education-related factors and recruitment and retention of NPs and other clinicians in underserved areas (Andrus & Fenley, 1976; Daniels et al., 2007; Doyle et al., 2017; Edwards et al., 2006; Flinter, 2011; Fowkes et al., 1994; Hafferty & Goldberg, 1986; Holland et al., 2019; Kippenbrock et al., 2004; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Ryan et al., 1986). Nine studies showed that programs that emphasized training and curriculum in underserved areas had high success in deploying their graduates to, and keeping them in, underserved areas (Andrus & Fenley, 1976; Daniels et al., 2007; Doyle et al., 2017; Edwards et al., 2006; Flinter, 2011; Fowkes et al., 1994; Hafferty & Goldberg, 1986; Holland et al., 2019; Ryan et al., 1986). Participants with clinical or practicum experiences in rural areas had 2.7 times higher odds of choosing rural versus urban as their first practice location (OR = 2.7; CI 95% [1.6, 4.8]) (Daniels et al., 2007). In fact, when training location was examined with other variables (e.g., age, sex, marital status), only training location significantly predicted practice in underserved areas while other variables did not (Hafferty & Goldberg, 1986).
Five studies examined the impact of educational financial aid (i.e., loan repayment, scholarship) on clinician recruitment and retention (Daniels et al., 2007; Kippenbrock et al., 2004; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012). In Daniels et al., clinicians reported that financial aid obligations influenced their decision to work in rural practices (OR = 1.9; 95% CI [1.3, 2.9]) (Daniels et al., 2007). However, financial aid may not be the dominant factor attracting clinicians to underserved settings. In a study of rural Arkansas NPs, only 37% of NPs reported that they chose to practice in rural areas because of loan repayment obligation (Kippenbrock et al., 2004). Another study surveyed clinicians in the National Health Service Corps (NHSC), a scholarship and loan repayment program for clinicians working in underserved areas (Health Resources and Services Administration, 2020). The researchers found that NHSC clinicians who were motivated to practice in underserved areas due to financial support were less likely to anticipate staying in their service sites over time (Pathman, Fannell, et al., 2012).
Factors Related to the Organization Employing Nurse Practitioners
A total of six studies (Aysola et al., 2015; Gilman, 2013; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Scarbrough et al., 2016; Sinclair-Lian et al., 2008) examined the associations between clinician recruitment and retention in underserved areas and organizational factors. Organizational factors included attributes of the healthcare organizations employing clinicians (e.g., practice environment) and benefits offered by the organization (e.g., availability of professional development program, salary).
Issues related to practice environment—including good relationships with administration, job recognition, and adequate and competent support staff—influenced clinicians’ retention in underserved areas in four studies (Gilman, 2013; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Scarbrough et al., 2016). Three studies found that satisfaction with salary influenced clinicians’ retention in underserved communities (Gilman, 2013; Pathman, Fannell, et al., 2012; Scarbrough et al., 2016). Organization-based professional development programs, such as career-ladder incentives and research partnerships (Aysola et al., 2015; Sinclair-Lian et al., 2008), also increased clinician recruitment and retention in underserved areas. Community health centers with career ladder programs reported less difficulty in recruiting (17.6% vs 10.6%, p = .01) and retaining (39.4% vs 21.2%, p = .0001) clinicians compared to health centers without such programs (Aysola et al., 2015). Clinicians also reported that availability of professional development opportunities significantly influenced their intention to stay in their jobs (Gilman, 2013; Scarbrough et al., 2016).
Factors Related to Communities where Nurse Practitioners Work
A total of eight studies found associations between community factors and clinicians’ recruitment/retention in underserved areas (Bailey, 1997; Daniels et al., 2007; Gilman, 2013; Lindsay, 2007; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Spetz et al., 2017). Community characteristics—including size, crime rate, cost of living, rurality, and income level—impacted clinicians’ decision to work and stay in underserved areas in seven studies (Bailey, 1997; Daniels et al., 2007; Gilman, 2013; Negrusa et al., 2014; Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Spetz et al., 2017). Clinicians working in rural communities had higher retention compared to those in urban communities (Pathman, Fannell, et al., 2012; Pathman, Konrad, et al., 2012; Spetz et al., 2017). However, findings conflicted for community income level and clinician retention: One study found that communities with higher per-capita income were associated with increased NP and physician assistant retention (Bailey, 1997), while another study found that communities that are poorer and less educated had higher clinician retention (Negrusa et al., 2014). Three studies also reported that clinicians practiced and stayed in underserved areas because of their fit, belonging, and relationship with the communities they work with (Gilman, 2013; Lindsay, 2007; Pathman, Fannell, et al., 2012).
Factors Related to Nurse Practitioners’ Autonomous Practice
In three studies, clinicians reported that autonomous and full scope of practice were associated with their decision to practice and stay in underserved areas (Lindsay, 2007; Pathman, Konrad, et al., 2012; Sullivan et al., 1978). Participants from the study by Lindsay (2007) reported preferring rural areas because of the higher “depth and breadth” to practice (p.74), ability to make independent decisions, and expansion of skills when faced with a wide variety of patient conditions. NHSC clinicians reported that being able to work to their fullest scope of practice influenced their decision to stay in underserved areas after their contract ended (Pathman, Konrad, et al., 2012).
Discussion
Our scoping review aimed to map, scope, and assess gaps in the literature of factors influencing recruitment and retention of NPs in underserved areas. This review included a total of 22 studies. Factors influencing NP recruitment and retention in underserved areas were mapped into five themes relating to: 1) the individual NP (e.g., background in underserved areas); 2) NP education programs and financial aid (e.g., training in underserved areas, loan repayment); 3) organizations employing NPs (e.g., practice environment, salary); 4) the communities NPs work in (e.g., community characteristics); and 5) autonomous practice (e.g., full scope of practice). This map of studies demonstrates that factors influencing NP recruitment and retention in underserved areas are broad and multileveled, from individual factors to community characteristics. NP recruitment and retention efforts may be initiated by stakeholders at various levels, including educators, practice administrators, and legislators. For example, educators can increase selection of students from underserved backgrounds and design curriculum focused on underserved populations. Practice administrators can implement professional development programs and ensure positive work environments. Legislators can support full scope of practice to attract NPs to underserved areas.
Scope of the literature was assessed in regard to study design, publication date, analysis method, and populations studied. We found that this literature is outdated, lacks robust study designs, and few studies focus exclusively on NPs—these characteristics are also gaps of the extant literature. The majority of the studies were conducted before 2010; outdated studies do not consider the implications of recent changes affecting healthcare workforces (e.g., the Affordable Care Act, recent expansions of scope of practice regulations). In addition, many studies are cross-sectional and provide only descriptive results. Also, of the 22 included studies, only eight studies have NP-only samples. Studies frequently surveyed NPs along with other clinicians, neglecting an NP-predominant perspective (i.e., the NP viewpoint may be lost when they are studied with other healthcare professionals). Although our map of studies demonstrates the breadth of factors influencing NP recruitment and retention in underserved areas, current and NP-focused studies with strong designs are needed to expand the literature and produce more compelling evidence.
Having an underserved background (i.e., growing up in underserved areas) and educational training focused on underserved communities were factors most often associated with NP recruitment and retention in underserved areas. These findings are consistent with literature demonstrating that among other primary care providers (i.e., physicians and physician assistants), underserved background and training also predict whether these providers practice in underserved areas (Goodfellow et al., 2016; MacQueen et al., 2018; Rabinowitz et al., 2000; Smith et al., 2012; Walker et al., 2010; Yuen & Lessard, 2018). We also found that autonomous and fuller scope of practice influenced NPs’ decision to work and stay working in underserved areas, corroborating with Xue and colleagues’ findings that states with less restrictive scope of practice regulations have increased NP number (Xue et al., 2016).
Our review found that the general practice environment (e.g., good administration, adequate support staff) was associated with recruitment and retention of clinicians in underserved areas. However, included studies did not specifically examine the practice environment of NPs in underserved areas. The NP practice environment contains distinct aspects unique to the profession, such as visibility and acceptance of the NP role (Poghosyan et al., 2017). Studying NP practice environment and understanding its effect specifically on NP recruitment and retention can help administrators create modifiable, organization-level strategies tailored for their practices. Other issues distinct to the NP profession may also affect NPs’ recruitment and retention to underserved areas, such as equitable reimbursement rates. Medicaid reimbursement for NP services ranges from 75–100% of the physician rate (Kaiser Family Foundation, n.d.), yet, NPs have higher odds of working in states that reimburse NPs at 100% of the physician rate (Barnes et al., 2017). Future studies examining these NP-unique issues will help to deepen our knowledge to improve NP recruitment and retention in underserved areas.
Our findings also raise considerations for current policies. As underserved background is frequently associated with underserved practice, certain policies may have implications on recruitment and retention of NPs in underserved areas. One example is the DNP degree requirement for NP practice. In 2004, the American Association of Colleges of Nursing recommended the doctoral-level DNP degree as the standard educational preparation for advanced practice nurses in place of masters-level MSN degrees (American Associations of Colleges of Nursing, 2004). Despite the benefits, DNP programs are more cost and time intensive compared to MSN programs (McCauley et al., 2020), and may be prohibitive for prospective NP students from underserved backgrounds. As NPs from underserved backgrounds are more likely to work in underserved areas, the DNP degree requirement may impact the number of future NPs working in underserved communities.
The influence of clinicians’ education and training on practice in underserved areas has been well-acknowledged by policymakers; several policies and grants exist to increase clinician training and number in underserved settings. One prominent example for NPs is the Advanced Nursing Education Workforce (ANEW) grant, awarded to schools to prepare NPs for practice in underserved communities (Health Resources & Services Administration, n.d.). Grants such as ANEW, however, may reach only a select number of schools and students. NP education leaders and researchers should consider the impact of prioritizing underserved population-focused curriculum throughout NP programs nationally, which may increase the number of NPs working in underserved areas.
Limitations
Our review has limitations. To prioritize breadth in our inclusion criteria, we included studies that examined recruitment and retention of NPs along with other clinicians; thus, our map of findings may not accurately reflect the NP perspective or viewpoint. Second, the decision to exclude international studies was due to regulatory differences governing NP practice in different countries—insights from other countries may have been overlooked due to this exclusion. Lastly, critical appraisal of included studies was not conducted. Although not required in the scoping review methodology, lack of quality appraisal may limit comprehensive understanding of the literature body’s quality (e.g., bias, reliability, validity of studies). Also, due to lack of quality appraisal, the synthesis of findings in this scoping review should not be used to inform practice changes but rather to inform further research and investigation efforts (Munn et al., 2018; Peters et al., 2020). However, this approach is consistent with the methodology of scoping reviews (Peters et al., 2020; Pollock et al., 2021).
Conclusion
The factors influencing NP recruitment and retention in underserved areas are broad and multileveled; several avenues exist for educators, practice administrators, and policymakers to address this issue. However, literature in this area is developing and there is a lack of current, robust, and NP-focused studies. Future studies closing these gaps can provide strong evidence to improve NP distribution in underserved areas, maximize the robust NP supply, and optimize NPs’ contribution to equalizing primary care access and mitigating health disparities.
Supplementary Material
Acknowledgement
The authors would like to acknowledge John Usseglio and Ellie Kim for their assistance with this manuscript. The authors also thank the peer-reviewers for their time and comments.
Declaration of Competing Interest
SK is supported by NIH-NINR CER2 T32NR014205 training grant.
CRediT Statement
| Author | Tasks |
|---|---|
| S. Kueakomoldej | Conceptualization, analysis, writing-original draft |
| E. Turi | Analysis, writing-original draft, writing-reviewing and editing |
| A. McMenamin | Analysis, writing-original draft, writing-reviewing and editing |
| Y. Xue | Writing-reviewing and editing |
| L. Poghosyan | Writing-reviewing and editing |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Supakorn Kueakomoldej, Columbia University School of Nursing.
Eleanor Turi, Columbia University School of Nursing.
Amy McMenamin, Columbia University School of Nursing.
Ying Xue, Loretta C. Ford Endowed Professorship in Primary Care Nursing, University of Rochester, Rochester, NY.
Lusine Poghosyan, Columbia University School of Nursing and Professor of Health Policy and Management, Department of Health Policy and Management, Mailman School of Public Health, Columbia University, New York, NY.
References
- American Association of Nurse Practioners. (2021). State practice environment. https://www.aanp.org/advocacy/state/state-practice-environment
- American Associations of Colleges of Nursing. (2004). AACN position statement on the practice doctorate in nursing. https://www.aacnnursing.org/DNP/Position-Statement
- Andrus LH, & Fenley MD (1976). Evolution of a family nurse practitioner program to improve primary care distribution. Journal of Medical Education, 51, 317–324. [DOI] [PubMed] [Google Scholar]
- Auerbach DI, Buerhaus PI, & Staiger DO (2020). Implications of the rapid growth of the nurse practitioner workforce in the US. Health Affairs, 39(2), 273–279. 10.1377/hlthaff.2019.00686 [DOI] [PubMed] [Google Scholar]
- Auerbach DI, Staiger DO, & Buerhaus PI (2018). Growing ranks of advanced practice clinicians: Implications for the physician workforce. New England Journal of Medicine, 378(25), 2358–2360. 10.1056/NEJMp1801869 [DOI] [PubMed] [Google Scholar]
- Aysola J, Groves D, & Hicks LS (2015). Health center professional programs and primary care workforce. J Fam Med Community Health, 2(8), 1–11. 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey BE (1997). Vast territory surrounded by vast terrority: A development and maintainance theory of access to primary health care on the frontier [Doctoral dissertation, University of Colorado at Denver]. UMI. [Google Scholar]
- Barnes H, Maier CB, Sarik DA, Germack HD, Linda H, & McHugh MD (2017). Effect of regulation and payment policies on nurse practitioners’ clinical practices. Medical Care Research and Review, 74(4), 431–451. 10.1177/1077558716649109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buerhaus P, Perloff J, Clarke S, O’Reilly-Jacob M, Zolotusky G, & DesRoches CM (2018). Quality of primary care provided to Medicare beneficiaries by nurse practitioners and physicians. Medical Care, 56(6). 10.1097/MLR.0000000000000908 [DOI] [PubMed] [Google Scholar]
- Dall T, Reynolds R, Chakrabarti R, Jones K, & Iacobucci W (2020). The complexities of physician supply and demand: Projections from 2013 to 2025. Association of American Medical Colleges. https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf [Google Scholar]
- Daniels ZM, Vanleit BJ, Skipper BJ, Sanders ML, & Rhyne RL (2007). Factors in recruiting and retaining health professionals for rural practice. Journal of Rural Health, 23(1), 62–71. 10.1111/j.1748-0361.2006.00069.x [DOI] [PubMed] [Google Scholar]
- DesRoches CM, Gaudet J, Perloff J, Donelan K, Iezzoni LI, & Buerhaus P (2013). Using Medicare data to assess nurse practitioner-provided care. Nursing Outlook, 61, 400–407. 10.1016/j.outlook.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Doyle JM, Zangaro GA, Howie BA, & Bigley MB (2017). Retrospective evaluation of the Advanced Nursing Education Expansion Program. Journal for Nurse Practitioners, 13(7), 488–495. 10.1016/j.nurpra.2017.04.019 [DOI] [Google Scholar]
- Edwards JB, Wilson J, L., Behringer BA, Smith PL, Ferguson KP, Blackwelder RB, Florence JA, Bennard B, & Tudiver F (2006). Practice locations of graduates of family physician residency and nurse practitioner programs: Considerations within the context of institutional culture and curricular innovation through Titles VII and VIII. The Journal of Rural Health, 22(1), 69–77. 10.1080/14739879.2015.1128684 [DOI] [PubMed] [Google Scholar]
- Exec. Order No. 14009, 86 Fed. Reg. 7793 (Jan 28, 2021).
- Faraz A, & Salsberg E (2019). From education to practice: What we can learn about the workforce from a survey of new nurse practitioners. Journal of the American Association of Nurse Practitioners, 31(8), 454–461. 10.1097/JXX.0000000000000226 [DOI] [PubMed] [Google Scholar]
- Flinter M (2011). From new nurse practitioner to primary care provider: Bridging the transition through FQHC-based residency training. Online Journal of Issues in Nursing, 17(1), 1–11. 10.3912/OJIN.Vol17No01PPT04 [DOI] [PubMed] [Google Scholar]
- Fowkes VK, Gamel NN, Wilson SR, & Garcia RD (1994). Effectiveness of educational strategies preparing physician assistants, nurse practitioners, and certified nurse-midwives for underserved areas. Public Health Reports, 109(5), 673–682. [PMC free article] [PubMed] [Google Scholar]
- Gilman L (2013). Recruitment and retention in designated shortage areas: The effectiveness of obligatory health care recruitment programs in the recruitment and retention of health care service providers in Delaware. Delaware Health and Social Services. https://pdfs.semanticscholar.org/ce99/c922b31381d63311724ff2978b6e210b2fb5.pdf [Google Scholar]
- Goodfellow A, Ulloa JG, Dowling PT, Talamantes E, Chheda S, Bone C, & Moreno G (2016). Predictors of primary care physician practice location in underserved urban and rural areas in the United States: A systematic literature review. Academic Medicine, 91(9), 1313–1321. 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafferty FW, & Goldberg HI (1986). Educational strategies for targeted retention of nonphysician health care providers. Health Services Research, 21(1), 107–124. [PMC free article] [PubMed] [Google Scholar]
- Health Resources & Services Administration. (n.d.). Advanced nursing education workforce (ANEW). https://www.hrsa.gov/grants/find-funding/hrsa-19-003
- Health Resources and Services Administration. (2021, February). What is a health professional shortage area (HPSA)? https://bhw.hrsa.gov/workforce-shortage-areas/shortage-designation#hpsas
- Health Resources and Services Administration. (2020). About NHSC. https://nhsc.hrsa.gov/about-us
- Holland A, Selleck C, Deupree J, Hodges A, Shirey M, Blakely K, Plane LC, & Harper DC (2019). A curriculum to expand rural health care access. Journal for Nurse Practitioners, 15, e69–e72. 10.1016/j.nurpra.2018.12.021 [DOI] [Google Scholar]
- Kaiser Family Foundation. (n.d.). Medicaid benefits:Nurse practitioner services. https://www.kff.org/medicaid/state-indicator/nurse-practitioner-services/
- Kippenbrock T, Stacy A, & Gilbert-Palmer D (2004). Educational strategies to enhance placement and retention of nurse practitioners in rural Arkansas. Journal of the American Academy of Nurse Practitioners, 16(3), 139–143. 10.1111/j.1745-7599.2004.tb00385.x [DOI] [PubMed] [Google Scholar]
- Kueakomoldej S (2021). Recruitment and retention of primary care nurse practitioners in underserved areas: A scoping review protocol (No. 12761885). OSF. https://osf.io/7zj38/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li LB, Williams SD, & Scammon DL (1995). Practicing with the urban underserved: A qualitative analysis of motivations, incentives, and disincentives. Archives of Family Medicine, 4, 124–133. 10.1001/archfami.4.2.124 [DOI] [PubMed] [Google Scholar]
- Lindsay S (2007). Gender differences in rural and urban practice location among mid-level health care providers. Journal of Rural Health, 23(1), 72–76. 10.1111/j.1748-0361.2006.00070.x [DOI] [PubMed] [Google Scholar]
- MacQueen IT, Maggard-Gibbons M, Capra G, Raaen L, Ulloa JG, Shekelle PG, Miake-Lye I, Beroes JM, & Hempel S (2018). Recruiting rural healthcare providers today: A systematic review of training program success and determinants of geographic choices. Journal of General Internal Medicine, 33(2), 191–199. 10.1007/s11606-017-4210-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCauley LA, Broome ME, Frazier L, Hayes R, Kurth A, Musil CM, Norman LD, Rideout KH, & Villarruel AM (2020). Doctor of nursing practice (DNP) degree in the United States: Reflecting, readjusting, and getting back on track. Nursing Outlook, 68, 494–503. 10.1016/j.outlook.2020.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meit M, Knudson A, Gilbert T, Yu AT-C, Tanenbaum E, Ormson E, TenBroeck S, Bayne A, & Popat S (2014). The 2014 update of the rural-urban chartbook. Rural Health Research and Policy Centers. http://www.ruralhealthresearch.org/. [Google Scholar]
- Muench U, Guo C, Thomas C, & Perloff J (2019). Medication adherence, costs, and ER visits of nurse practitioner and primary care physician patients: Evidence from three cohorts of Medicare beneficiaries. Health Services Research, 54, 187–197. 10.1111/1475-6773.13059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, & Aromataris E (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18, 1–7. 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academy of Medicine. (2021). Implementing high-quality primary care: Rebuilding the foundation of health care. The National Academies Press. 10.17226/25983 [DOI] [PubMed] [Google Scholar]
- National Association of Community Health Centers. (2016). Staffing the safety net: Building the primary care workforce at America’s health center. https://www.nachc.org/wp-content/uploads/2015/10/NACHC_Workforce_Report_2016.pdf
- Naylor KB, Tootoo J, Yakusheva O, Shipman SA, Bynum JPW, & Davis MA (2019). Geographic variation in spatial accessibility of U.S. healthcare providers. PLoS ONE, 14(4). 10.1371/journal.pone.0215016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negrusa S, Ghosh P, & Warner JT (2014). Provider retention in high need areas. https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//97216/NHSC%20Final%20Report%20508%20compliance%20July_21_2015.pdf
- Pathman DE, Fannell J, Konrad TR, Pierson S, Toblin M, & Jonsson M (2012). Findings of the first year retention survey of the multi-state/ NHSC retention collaborative. https://chcworkforce.org/sites/default/files/Findings%20of%20Multi-State%20NHSC%20Collaborative.pdf
- Pathman DE, Konrad TR, Schwartz R, Meltzer A, Goodman C, & Kumar J (2012). Evaluating retention in BCRS programs: Final report. https://www.shepscenter.unc.edu/wp-content/uploads/2017/08/Evaluating-Retention-in-BCRS-Programs-Final-Report_Pathman_5-4-12-1.pdf
- Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, & Soares CB (2015). Guidance for conducting systematic scoping reviews. International Journal of Evidence-Based Healthcare, 13(3), 141–146. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, & Khalil H (2020). Chapter 11: Scoping reviews. In Aromataris E & Munn Z (Eds.), JBI manual for evidence synthesis (2020 version, pp.406–444). JBI. 10.46658/JBIMES-20-01 [DOI] [Google Scholar]
- Poghosyan L, Chaplin WF, & Shaffer JA (2017). Validation of Nurse Practitioner Primary Care Organizational Climate Questionnaire: A new tool to study nurse practitioner practice settings. Journal of Nursing Measurement, 25(1), 142–155. [DOI] [PubMed] [Google Scholar]
- Pollock D, Davies EL, Peters MDJ, Tricco AC, Alexander L, McInerney P, Godfrey CM, Khalil H, & Munn Z (2021). Undertaking a scoping review: A practical guide for nursing and midwifery students, clinicians, researchers, and academics. Journal of Advanced Nursing, 77, 2102–2113. 10.1111/jan.14743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulcini J, Jelic M, Gul R, & Loke AY (2010). An international survey on advanced practice nursing education, practice, and regulation. Journal of Nursing Scholarship, 42(1), 31–39. 10.1111/j.1547-5069.2009.01322.x [DOI] [PubMed] [Google Scholar]
- Rabinowitz HK, Diamond JJ, Markham FW, & Paynter NP (2001). Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA, 286(9), 1041–1048. 10.1001/jama.286.9.1041 [DOI] [PubMed] [Google Scholar]
- Rabinowitz HK, Diamond JJ, Veloski JJ, & Gayle JA (2000). The impact of multiple predictors on generalist physicians’ care of underserved populations. American Journal of Public Health, 90(8), 1225–1228. 10.2105/AJPH.90.8.1225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan R, Hanson CM, Hodnicki D, & Dorroh MW (1986). Education of health care providers for the rural setting: A family nurse practitioner demonstration program. The Journal of Rural Health, 2(1), 7–22. 10.1111/j.1748-0361.1986.tb00132.x [DOI] [PubMed] [Google Scholar]
- Scarbrough AW, Moore M, Shelton SR, & Knox RJ (2016). Improving primary care retention in medically underserved areas. Health Care Manager, 35(4), 368–372. 10.1097/HCM.0000000000000137 [DOI] [PubMed] [Google Scholar]
- Sheer B, & Wong FKY (2008). The development of advanced nursing practice globally. Journal of Nursing Scholarship, 40(3), 204–211. 10.1111/j.1547-5069.2008.00242.x [DOI] [PubMed] [Google Scholar]
- Sinclair-Lian N, Rhyne RL, Alexander SH, & Williams RL (2008). Practice-based research network membership is associated with retention of clinicians in underserved communities: A research involving outpatient settings network (RIOS Net) study. Journal of the American Board of Family Medicine, 21(4), 353–355. 10.3122/jabfm.2008.04.080022 [DOI] [PubMed] [Google Scholar]
- Smith B, Muma RD, Burks L, & Lavoie MM (2012). Factors that influence physician assistant choice of practice location. Journal of the American Academy of Physician Assistants, 25(3), 46–51. 10.1097/01720610-201203000-00010 [DOI] [PubMed] [Google Scholar]
- Spetz J, Skillman SM, & Andrilla CHA (2017). Nurse practitioner autonomy and satisfaction in rural settings. Medical Care Research and Review, 74(2), 227–235. 10.1177/1077558716629584 [DOI] [PubMed] [Google Scholar]
- Starfield B, Shi L, & Macinko J (2005). Contribution of primary care to health systems and health. Milbank Quarterly, 83(3), 457–502. 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan JA, Dachelet CZ, Sultz HA, & Henry M (1978). The rural nurse practitioner: a challenge and a response. American Journal of Public Health, 68(10), 972–976. 10.2105/AJPH.68.10.972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan M, Ferguson S, Chang A, Larson E, & Smaldone A (2015). Quality of primary care by advanced practice nurses: A systematic review. International Journal for Quality in Health Care, 27(5), 396–404. 10.1093/intqhc/mzv054 [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, … Straus SE (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- US Department of Agriculture, Economic Research Service. (2021). Rural poverty & well-being. https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/
- Veritas Health Innovation. (n.d.). Covidence systematic review software. www.covidence.org
- Walker KO, Ryan G, Ramey R, Nunez FL, Beltran R, Splawn RG, & Brown AF (2010). Recruiting and retaining primary care physicians in urban underserved communities: The importance of having a mission to serve. American Journal of Public Health, 100(11), 2168–2175. 10.2105/AJPH.2009.181669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright B, Damiano PC, & Bentler SE (2015). Implementation of the affordable care act and rural health clinic capacity in Iowa. Journal of Primary Care and Community Health, 6(1), 61–65. 10.1177/2150131914542613 [DOI] [PubMed] [Google Scholar]
- Xue Y, Smith JA, & Spetz J (2019). Primary care nurse practitioners and physicians in low-income and rural areas, 2010–2016. JAMA, 321(1), 102–105. 10.1001/jama.2018.17944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue Y, Ye Z, Brewer C, & Spetz J (2016). Impact of state nurse practitioner scope-of-practice regulation on health care delivery: Systematic review. Nursing Outlook, 64, 71–85. 10.1016/j.outlook.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Yuen CX, & Lessard D (2018). Filling the gaps: Predicting physician assistant students’ interest in practicing in medically underserved areas. Journal of Physician Assistant Education, 29(4), 220–225. 10.1097/JPA.0000000000000219 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


