Abstract
BACKGROUND:
The purpose of the current study is to examine the association between non-exercise estimated cardiorespiratory fitness and incident hypertension by gender.
METHODS:
A total of 5513 participants (4403 men and 1110 women) free of hypertension from the Aerobics Center Longitudinal Study, were followed for incident hypertension, which was determined as resting systolic or diastolic blood pressure at least 130/80 mm Hg or physician diagnosis. Non-exercise estimated cardiorespiratory fitness was estimated in METs (metabolic equivalent) with sex-specific algorithms which was developed by Jackson. Age, body mass index, waist circumference, and resting heart rate were used as continuous variable whereas being physical active and current smoking were dichotomous variable. Multivariable Cox regression models were used to examine the association between cardiorespiratory fitness and risk of developing hypertension. Hazard ratios (HRs) and 95% confidence intervals (CIs) were reported as an index of strength of association.
RESULTS:
During an average follow up of 5 years, 61.7% men and 39.5% women developed hypertension. In men, the upper and middle tertiles of cardiorespiratory fitness had 22% (95% CI 0.71–0.86) and 10% (95% CI 0.82–0.99) lower risk of developing hypertension compared to those in the lower tertile, respectively. In women, the upper and middle tertiles of cardiorespiratory fitness had 30% (95% CI 0.55–0.88) and 6% (95% CI 0.74–1.18) lower risk of developing hypertension. Each one-MET increment was associated with an 10% lower risk of incident hypertension in the overall sample.
CONCLUSION:
Cardiorespiratory fitness estimated using a non-exercise algorithm is inversely associated with risk of developing hypertension in men and women.
Keywords: fitness, hypertension, cohort study
INTRODUCTION
Primary hypertension prevention remains a global public health challenge; 116 million (47%) Americans live with hypertension which make it a primary or contributing cause for nearly half a million deaths in the United States annually1, and worldwide the prevalence of hypertension is projected to increase around 60% by 20252. Existing data from large perspective studies such as the Aerobics Center Longitudinal Study (ACLS), Coronary Artery Risk Development in Young Adults (CARDIA) study, and others demonstrate that cardiorespiratory fitness, an objective indicator of recent habitual physical activity, is inversely associated with the development of hypertension3–5.
Cardiorespiratory fitness is a strong predictor of cardiovascular morbidity and mortality6–8 and has been shown to improve classification and discrimination of cardiovascular disease events beyond conventional risk factors9,10. The voluminous evidence provides scientific rationale for the statement released from the AHA proposing that cardiorespiratory fitness be considered a clinical vital sign11. However, access to cardiorespiratory fitness is limited, primarily due to the cost and burden of exercise testing12 and accordingly it is not included in common risk algorithms. Non-exercise algorithms that estimate cardiorespiratory fitness using readily available clinical and self-reported variables, have been proposed as a promising alternative that overcomes the practical issues of directly measured cardiorespiratory fitness in healthcare settings9,13–15. Recent studies have documented significant associations between estimated cardiorespiratory fitness algorithms and a variety of outcomes, such as fatal and non-fatal cardiovascular disease events and all-cause mortality9,13,16, showing relative risk reductions comparable to directly measured cardiorespiratory fitness. No existing study has associated non-exercise estimated cardiorespiratory fitness with incident hypertension and therefore, the purpose of the current study is to examine the relationship between non-exercise estimated cardiorespiratory fitness and incident hypertension in an ACLS cohort of men and women. The non-exercise estimated cardiorespiratory fitness formula utilized readily available data from patients’ health records and could be a valid alternative in risk assessment of hypertension. We also chose to conduct sex-specific analyses due to the significant interaction between non-exercise estimated cardiorespiratory fitness and sex (P for interaction < 0.0001).
METHODS
Study design and participants
We analyzed data from the ACLS of men and women who have been examined at the Cooper Clinic in Dallas, TX. The ACLS is a longitudinal observational study where patients visited the clinic for periodic preventive medical examinations and for counseling regarding health and lifestyle habits including, but not limited to exercise, nutrition, and stress management between 1979 and 20054,17. Patients came from all 50 states; were unpaid volunteers sent by their physicians or employers or were self-referred. At the time of their clinic examination, the ACLS was described to patients who then provided written informed consent for enrollment in the follow-up study. The Cooper Institute Institutional Review Board annually reviewed and approved the study protocol.
All participants included in this study were free of hypertension during the first examination and were followed for incident hypertension (primary outcome) from the follow up examinations. The frequency of these examinations ranged from 2 to 29. The mean (interquartile range) interval between two adjunct examinations was 2.1 (1.0 to 2.2) years with a minimum of 5 months. We included all participants who had complete data to calculate the non-exercise estimated cardiorespiratory fitness. We then excluded individuals who met the following criteria: myocardial infarction (n=50), stroke (n=4), cancer (n=157), body mass index (BMI)<18.5 (n=100), age<20 or age>90 (n=53). Among the eligible participants, 5513 individuals who had at least two follow-up visits in order to identify incident hypertension, and therefore became the final analytical sample for the current study. A flow chart was developed to further illustrate the selection of the study sample (Figure 1).
Figure 1.
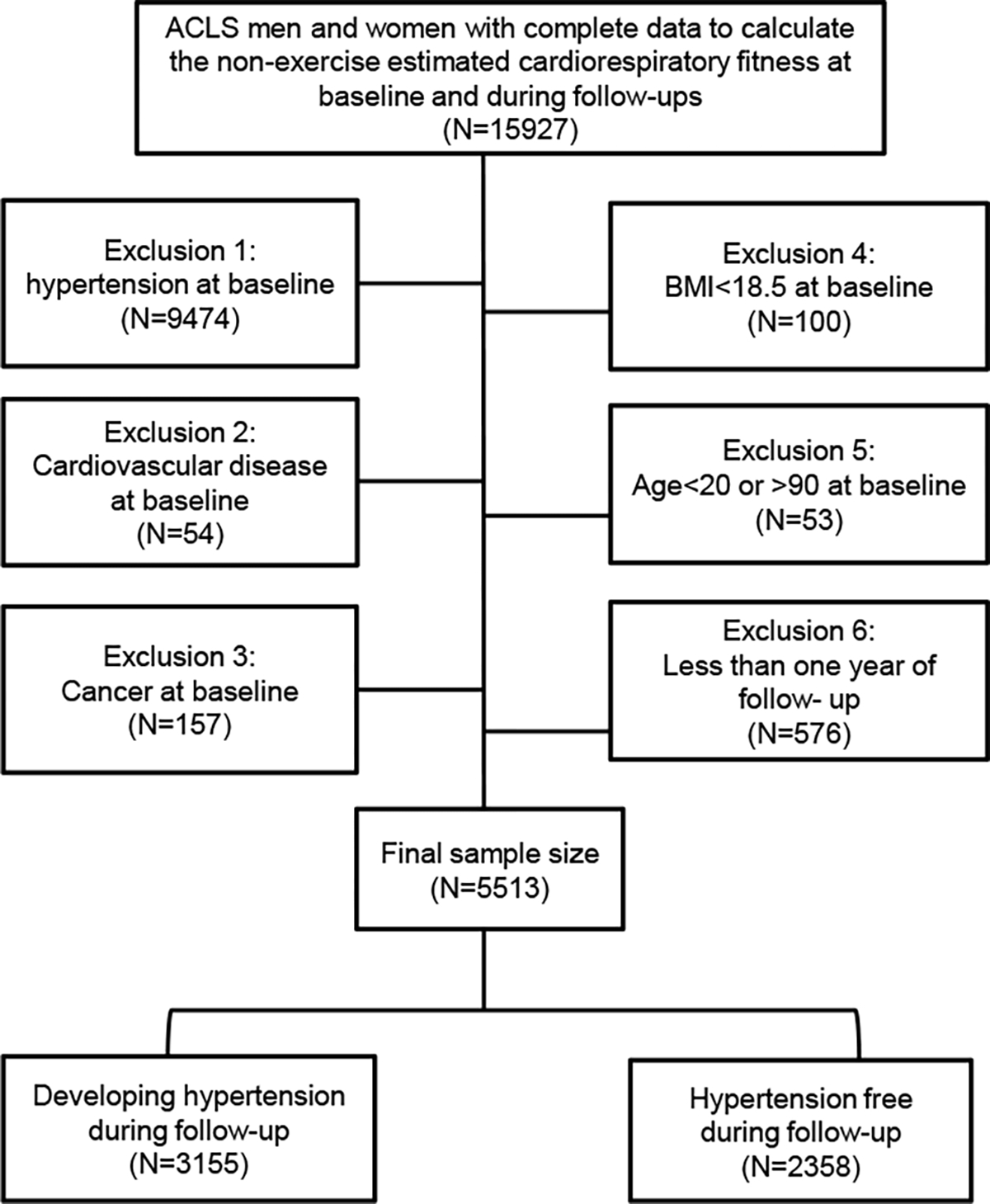
Study flow and Aerobics Center Longitudinal Study (ACLS) inclusion criteria depicting final sample size and incident hypertension frequency. BMI, body mass index.
Assessment of non-exercise estimated cardiorespiratory fitness
Non-exercise cardiorespiratory fitness at baseline was estimated in METs (3.5 mL O2·kg−1·min−1) with the following sex-specific algorithms:14
Cardiorespiratory fitness in men (METs) =21.2870 + (0.1654*age) − (0.0023*age2) − (0.2318*BMI) − (0.0337*waist circumference) − (0.0390*resting heart rate) + (0.6351*physically active) − (0.4263*current smoker)
Cardiorespiratory fitness in women (METs) =14.7873 + (0.1159*age) − (0.0017*age2) − (0.1534*BMI) − (0.0085*waist circumference) − (0.0364*resting heart rate) + (0.5987*physically active) − (0.2994*current smoker)
Age, BMI, waist circumference, and resting heart rate are entered as continuous variables, whereas being physically active and being a current smoker are dichotomous variables with a value of 1 when present and 0 when absent.
BMI was calculated from measured height and weight in accordance with standard procedures during participants’ clinical visit. Waist circumference was measured level with the umbilicus. Resting heart rate was determined with the participants recumbent after 5-minute rest before the test and was obtained from the resting ECG. Physical activity was assessed with a five-level physical activity index 14,18 based on a formerly validated questionnaire19. Physically active was defined as walking or jogging 10 miles or more per week that was equal to the PA index levels 3 and 4; inactive was defined as walking or jogging less than 10 miles per week, participating in some other regular physical activity such as bicycling, swimming, racquet sports, and other strenuous sports, but not walking or jogging, or no regular activity that was equal to the physical activity index levels 0 to 2. Participants also reported their smoking status (never smoked, former smokers, or current smokers). Once the algorithms were implemented, participants’ METs value were calculated as a continuous variable. We then classified all participants into lower, middle, and upper tertiles of estimated cardiorespiratory fitness groups based on age-specific (20–30, 40–49, 50–59, or ≥60 years) thirds of the estimated METs distribution and separated by sex. The thresholds that defined the three fitness categories were presented in Table 1.
TABLE 1.
The thresholds of the three fitness categories in men and women.
| Age Groups |
||||
|---|---|---|---|---|
| 20–30 year | 40–49 year | 50–59 year | ≥60 year | |
|
| ||||
| Non-exercise estimated cardiorespiratory fitness in METs in men | ||||
| T1 (Lower third) | ≤ 13.38 | ≤13.10 | ≤12.47 | ≤11.38 |
| T2 (Middle third) | 13.38–14.31 | 13.10–14.01 | 12.47–13.36 | 11.38–12.46 |
| T3 (Upper third) | >14.31 | >14.01 | >13.36 | >12.46 |
| Non-exercise estimated cardiorespiratory fitness in METs in women | ||||
| T1 (Lower third) | ≤ 10.84 | ≤10.59 | ≤9.90 | ≤9.23 |
| T2 (Middle third) | 10.84–11.44 | 10.59–11.13 | 9.90–10.62 | 9.23–9.91 |
| T3 (Upper third) | >11.44 | >11.13 | >10.62 | >9.91 |
Identification of incident hypertension
Following a standard protocol, resting blood pressure was measured in the seated position using auscultatory methods with a mercury sphygmomanometer. Systolic and diastolic pressure was recorded as the first and fifth Korotkoff sounds after at least 5 minutes of rest. Two readings separated by 2 minutes were averaged. If the first 2 readings differed by more than 5 mm Hg, additional readings were obtained and averaged.
Incident hypertension was defined as resting systolic or diastolic blood pressure at least 130/80 mm Hg or self-reported, physician-diagnosed hypertension20. We previously verified the accuracy of self-reported, physician-diagnosed hypertension in this cohort and observed 98% sensitivity and 99% specificity21. This method of case ascertainment is similar to those used in other established epidemiologic studies on hypertension22,23. We used the first examination as the baseline measure and followed up participants for incident hypertension from the second through their final examinations. Follow-up was calculated from baseline examination to the first event of hypertension for those participants who developed hypertension or the last examination through 2005 for those who were hypertension free. This method of case identification has been used and described in our previous papers24.
Potential confounders
Potential confounding variables include age, sex, alcohol consumption, diabetes, hypercholesterolemia, and parental history of hypertension. This information was collected during baseline examinations according to the Cooper Clinic’s standardized manual of operation. After an overnight fast of at least 12 hours, an extensive physical examination and preventive health evaluation were performed. The examination included measures of blood pressure, blood for chemistry analyses, personal health history, and lifestyle habits. Diabetes mellitus was defined as a physician diagnosis, insulin use, or fasting glucose ≥7 mmol/L (126mg/dL). Hypercholesterolemia was defined as a physician diagnosis or total cholesterol ≥6.2 mmol (240 mg/d).
Statistical analysis
Baseline characteristics of the study population were characterized by estimated cardiorespiratory fitness tertiles in men and women. Differences in covariates were tested using F-tests. Sex-specific Cox regression models were used to examine the association between non-exercise estimated cardiorespiratory fitness and risk of developing hypertension. Hazard Ratios (HRs) and 95% confidence intervals (CIs) were reported as an index of the strength of association. Two models were tested: 1) age-adjusted model; 2) multivariable-adjusted model including the following covariates: age (in years), year of baseline examination, heavy alcohol intake (>14 drinks/week in men, or >7 drinks/week in women), presence of diabetes or hypercholesterolemia (yes/no for each), and parental history of hypertension (yes/no). We assessed linear trends in the association of non-exercise estimated cardiorespiratory fitness with the risk of hypertension. We also examined non-exercise estimated cardiorespiratory fitness as a continuous variable so that each HR represents the risk associated with a 1-MET increase in the exposure variable. We then performed stratified analyses across components of non-exercise estimated cardiorespiratory fitness, as follows: age (<median, ≥median), BMI (<median, ≥median), waist circumference (<median, ≥median), resting heart rate (<median, ≥median), physical active (inactive, active), and smoking status (current smoker, nonsmoker). The proportional hazards assumptions were met by comparing the log-log survival plots. Analyses were conducted in 2021 using SAS, version 9.4, with alpha set at P<.05.
RESULTS
At baseline, the mean (SD) age of the study participants was 42.8 (9.0) yr for men and 42.9 (9.0) yr for women. Men in the upper tertile fitness group were more likely to have a lower BMI and waist circumference, to have a more favorable lipid and blood pressure profile, to have a healthier lifestyle (as reflected by smoking and physical activity), and to have a lower rate of chronic conditions (as reflected by hypercholesterolemia and diabetes) as compare with lower tertile cardiorespiratory fitness (Table 2). Women in the upper tertile fitness group were more likely to have a lower BMI, waist circumference and resting heart rate, to have more favorable blood pressure profile, were less likely to be a current smoker, and less likely to have hypercholesterolemia and family history of hypertension as compare with lower tertile cardiorespiratory fitness (Table 3).
TABLE 2.
Baseline characteristics by fitness categories in men.
| Non-exercise estimated cardiorespiratory fitness tertiles |
|||||
|---|---|---|---|---|---|
| All | T1 (lower) | T2 (middle) | T3 (upper) | Plinear Trend | |
| Characteristic | (N=4403) | (N=1466) | (N=1469) | (N=1468) | |
|
| |||||
| Age (yr) | 42.8 (9.0) | 43.1 (9.2) | 42.7 (9.1) | 42.4 (8.7) | 0.11 |
| Body mass index | 25.1 (2.7) | 27.7 (2.5) | 24.9 (1.5) | 22.9 (1.4) | <0.0001 |
| Waist circumference (cm) | 89.9 (8.5) | 97.4 (7.4) | 89.5 (5.1) | 82.9 (5.7) | <0.0001 |
| Resting heart rate | 56 (9) | 62 (9) | 56 (8) | 51 (7) | <0.0001 |
| Total cholesterol (mmol/L) | 5.3 (1.2) | 5.5 (1.0) | 5.3 (1.4) | 5.0 (0.9) | <0.0001 |
| Triglycerides (mmol/L) | 1.3 (0.9) | 1.6 (1.2) | 1.2 (0.7) | 1.0 (0.5) | <0.0001 |
| Systolic blood pressure (mmHg) | 112 (8) | 113 (8) | 111 (8) | 111 (8) | <0.0001 |
| Diastolic blood pressure (mmHg) | 72 (5) | 73 (4) | 72 (5) | 71 (5) | <0.0001 |
| Fasting blood glucose (mmol/L) | 5.4 (0.7) | 5.5 (0.7) | 5.4 (0.7) | 5.3 (0.5) | <0.0001 |
| Estimated cardiorespiratory fitness (METs) | 13.4 (1.2) | 12.2 (0.9) | 13.5 (0.5) | 14.5 (0.6) | <0.0001 |
| Current smoker (%) | 14.7 | 23.9 | 13.8 | 6.4 | <0.0001 |
| Heavy alcohol drinker* (%) | 5.8 | 6.5 | 5.9 | 5.0 | 0.25 |
| Physically active† (%) | 84.0 | 66.4 | 88.6 | 97.1 | <0.0001 |
| Hypercholesterolemia‡ (%) | 14.7 | 20.4 | 15.0 | 8.7 | <0.0001 |
| Diabetes mellitus§ (%) | 1.6 | 2.5 | 1.9 | 0.5 | 0.0001 |
| Parental history of hypertension (%) | 10.9 | 12.4 | 9.9 | 10.4 | 0.06 |
Data are presented as % or mean (SD).
Heavy alcohol drinker was defined as drinks per week >14 in male or >7 in female. One drink of alcohol is defined as 12 oz (3.41 dL) of beer, 5 oz (1.421 dL) of wine, or 1.5 oz (0.4262 dL) of hard liquor.
Physically active was defined as have leisure-time physical activity during the past three months.
Hypercholesterolemia was defined as a physician diagnosis or total cholesterol ≥6.2 mmol/L.
Diabetes mellitus was defined as a physician diagnosis, insulin use, or fasting glucose ≥7 mmol/L.
TABLE 3.
Baseline characteristics by fitness categories in women.
| Non-exercise estimated cardiorespiratory fitness tertiles |
|||||
|---|---|---|---|---|---|
| All | T1 (lower) | T2 (middle) | T3 (upper) | Plinear Trend | |
| Characteristic | (N=1110) | (N=368) | (N=3739) | (N=369) | |
|
| |||||
| Age (yr) | 42.9 (9.0) | 42.9 (9.7) | 43.2 (9.0) | 42.5 (8.4) | 0.53 |
| Body mass index | 22.2 (2.8) | 24.4 (3.3) | 21.7 (1.7) | 20.4 (1.2) | <0.0001 |
| Waist circumference (cm) | 70.4 (7.5) | 75.4 (8.7) | 69.4 (5.7) | 66.4 (4.4) | <0.0001 |
| Resting heart rate | 62 (9) | 68 (9) | 62 (7) | 55 (6) | <0.0001 |
| Total cholesterol (mmol/L) | 5.0 (1.4) | 5.1 (1.0) | 5.1 (2.1) | 4.9 (0.8) | 0.23 |
| Triglycerides (mmol/L) | 1.0 (1.6) | 1.1 (0.7) | 1.0 (2.6) | 0.8 (0.3) | 0.06 |
| Systolic blood pressure (mmHg) | 105 (9) | 106 (9) | 106 (9) | 104 (9) | <0.0001 |
| Diastolic blood pressure (mmHg) | 70 (6) | 71 (6) | 70 (6) | 69 (6) | 0.001 |
| Fasting blood glucose (mmol/L) | 5.6 (1.5) | 5.2 (0.5) | 6.5 (2.6) | 5.1 (0.8) | 0.38 |
| Estimated cardiorespiratory fitness (METs) | 10.7 (0.8) | 9.9 (0.7) | 10.8 (0.4) | 11.4 (0.4) | <0.0001 |
| Current smoker (%) | 7.6 | 13.3 | 6.2 | 3.3 | <0.0001 |
| Heavy alcohol drinker* (%) | 9.5 | 10.1 | 9.7 | 8.7 | 0.80 |
| Physically active† (%) | 84.5 | 63.0 | 91.2 | 99.2 | <0.0001 |
| Hypercholesterolemia‡ (%) | 8.7 | 12.2 | 7.8 | 6.2 | 0.01 |
| Diabetes mellitus§ (%) | 2.2 | 1.6 | 3.2 | 1.6 | 0.23 |
| Parental history of hypertension (%) | 21.9 | 24.5 | 23.9 | 17.3 | 0.03 |
Data are presented as % or mean (SD).
Heavy alcohol drinker was defined as drinks per week >14 in male or >7 in female. One drink of alcohol is defined as 12 oz (3.41 dL) of beer, 5 oz (1.421 dL) of wine, or 1.5 oz (0.4262 dL) of hard liquor.
Physically active was defined as have leisure-time physical activity during the past three months.
Hypercholesterolemia was defined as a physician diagnosis or total cholesterol ≥6.2 mmol/L.
Diabetes mellitus was defined as a physician diagnosis, insulin use, or fasting glucose ≥7 mmol/L.
During a mean 5 years of follow-up, 61.7% men and 39.5% women developed hypertension. In the fully adjusted model, there was an inverse association between incremental tertiles of cardiorespiratory fitness and incident hypertension in the entire cohort and when men and women were considered separately (Table 4). In the overall sample, upper and middle cardiorespiratory fitness had 23% (95% CI 0.70–0.84) and 9% (95% CI 0.83–0.99) lower risk of developing hypertension compared to those in the lower tertiles, respectively. The risk of hypertension was 10% lower for each 1-MET increase in cardiorespiratory fitness. The pattern of the association between cardiorespiratory fitnessand incident hypertension in men was similar as the overall sample. However, only the upper fitness tertile was statistically different from the referent in women.
TABLE 4.
Association of estimated cardiorespiratory fitness and development of hypertension in men and women.
| N/cases | Model 1* | Model 2† | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | ||
|
| |||
| Men | |||
| T1 (Lower) | 1466/939 | 1.00 | 1.00 |
| T2 (Middle) | 1469/893 | 0.87 (0.80–0.96) | 0.90 (0.82–0.99) |
| T3 (Upper) | 1468/885 | 0.74 (0.68–0.81) | 0.78 (0.71–0.86) |
| P for linear trend | <0.0001 | <0.0001 | |
| Per 1- MET increase | 0.89 (0.86–0.92) | 0.91 (0.88–0.94) | |
| Women | |||
| T1 (Lower) | 368/149 | 1.00 | 1.00 |
| T2 (Middle) | 373/142 | 0.91 (0.72–1.14) | 0.94 (0.74–1.18) |
| T3 (Upper) | 369/147 | 0.64 (0.51–0.81) | 0.70 (0.55–0.88) |
| P for linear trend | 0.0001 | 0.002 | |
| Per 1- MET increase | 0.75 (0.66–0.85) | 0.79 (0.69–0.89) | |
| All | |||
| T1 (Lower) | 1834/1088 | 1.00 | 1.00 |
| T2 (Middle) | 1842/1053 | 0.88 (0.80–0.95) | 0.91 (0.83–0.99) |
| T3 (Upper) | 1837/1032 | 0.73 (0.67–0.79) | 0.77 (0.70–0.84) |
| P for linear trend | <0.0001 | <0.0001 | |
| Per 1- MET increase | 0.88 (0.85–0.91) | 0.90 (0.87–0.93) | |
Model 1 adjusted for age; additional adjusted for gender for all.
Model 2 adjusted all variables in model 1 plus year of baseline examination, heavy alcohol intake, presence of diabetes and hypercholesterolemia, and parental history of hypertension.
Across strata of the variables in the non-exercise equation in the overall sample (Figure 2), an inverse association between higher cardiorespiratory fitness and incident hypertension was observed across age, BMI, waist circumference, and resting heart rate groups (All P for linear trend < 0.05). In addition, higher level of cardiorespiratory fitness was associated with lower risk of hypertension among those who were active and those who were not current smoker.
Figure 2.
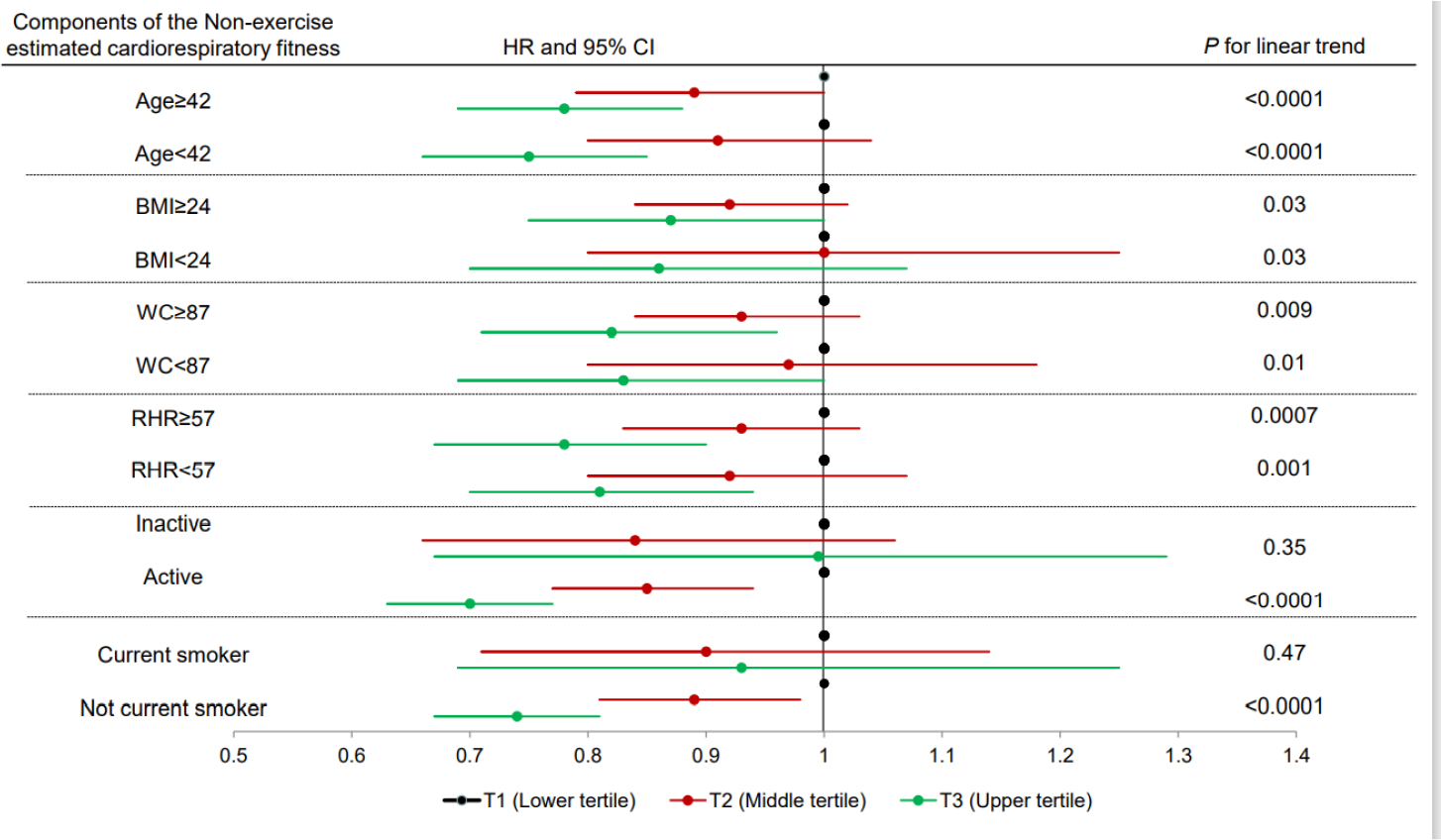
Multivariable*-adjusted hazard ratios (HRs) and 95% confidence intervals (CIs) of incident hypertension by tertiles of estimated cardiorespiratory fitness across strata of the variables in the non-exercise equation in the overall sample. *Adjusted by age, sex, year of baseline examination, heavy alcohol intake, presence of diabetes and hypercholesterolemia, and parental history of hypertension. T1 (lower tertile) is the referent. BMI, body mass index; WC, waist circumference; RHR, resting heart rate.
DISCUSSION
Non-exercise estimated cardiorespiratory fitness demonstrated a graded inverse association with incident hypertension during follow-up in both men and women in a large cohort with a wide age range. Various studies have shown that, higher level of cardiorespiratory fitness is associated with lower risk of hypertension. A recent meta-analysis25 summarized 9 original studies4,17,26–32 from 8 different cohorts and identified a 37% (95% CI: 30–44%) reduction in hypertension risk among individuals with high versus low cardiorespiratory fitness and 15% (95% CI: 9–20%) risk reduction with moderated versus low cardiorespiratory fitness and each 1-MET increment of cardiorespiratory fitness was associated with an 8% risk reduction of hypertension. Our results are comparable to the Veterans Affairs Medical Centers Study30 where the authors also reported a 42% lower risk of progression to hypertension in the High-Fit category (>10 METs) compared to the Least-Fit category (≤6.5 METs) among 2303 male veterans with prehypertension. The 10% risk reduction per 1-MET increment of non-exercise estimated cardiorespiratory fitness was consistent with the recent meta-analysis where cardiorespiratory fitness was objectively measured via maximal or submaximal exercise test25. To the best of our knowledge there is no study demonstrating an inverse association between cardiorespiratory fitness estimated from a non-exercise equation and incident hypertension.
The inverse association between non-exercise estimated cardiorespiratory fitness and incident hypertension generally was consistent in strata of men and women as well as across the four components of non-exercise equation (age, BMI, waist circumference, and resting heart rate). There were no significant gender differences in the hypertension risk by estimated cardiorespiratory fitness. For both men and women, an inverse association was observed between higher levels of cardiorespiratory fitness and risk of developing hypertension and remained significant for model 2. The inverse association between estimated cardiorespiratory fitness and hypertension was consistent regardless of BMI, but this is not consistent with the meta-analysis from Cheng et al25 which showed that the protective effect of cardiorespiratory fitness in lean subjects (BMI < 25 kg/m2) was probably stronger than in overweight/obese participants (BMI ≥ 25 kg/m2). The consistency of our findings with others reinforces the hypothesis that higher fitness, whether it is indicated by physical activity level17,33,34, exercise test determined cardiorespiratory fitness17 or algorithm estimated cardiorespiratory fitness is associated with lower blood pressures.
Physical activity is the main determinant of cardiorespiratory fitness35 and although genetics are a significant contributor, most individuals can raise their fitness through participation in moderate and vigorous physical activities, such as brisk walking, bicycling, and jogging, for 30 minutes or more on most days of the week36. Several mechanisms may explain the beneficial impact of physical activity on hypertension. Firstly, some evidence from randomized control trial and observational studies show that exercise has favorable effects on SBP/DBP, glucose homeostasis, blood, lipids, body fatness, and endothelial function, which are affecting factors for hypertension in the body34. Second, high physical activity is associated to the decreased secretion of pro-inflammatory cytokines, improved insulin sensitivity, and reduced oxidative stress which can modify the risk of developing hypertension34–36. Furthermore, low physical activity is associated with increased sympathetic nervous system activity and high levels of cardiometabolic risk factors including body fat, insulin resistance, inflammation, oxidative stress, and poor lipid profile37.
The present study has several limitations. Firstly, we used the 2017 guideline to define hypertension which significantly limited our sample size since many individuals were classified with baseline hypertension therefore were removed from the analysis. Secondly, the number of women in the study were relatively low which limited further subgroup analyses across sex and the six components of non-exercise estimated cardiorespiratory fitness. Thirdly, the study was conducted among a group of highly educated non-Hispanic white participants with middle-to-upper social economic status and limited number of women which limits the external validity. However, the homogeneity of our sample strengthens the internal validity of our findings by reducing potential confounding by unmeasured factors related to socioeconomic status, such as income, education, or prestige. Medication data were not available in our records. However, we used both measured blood pressure and physician-diagnosed hypertension based on patients’ report to identify hypertension events during follow-up examinations, and hopefully some medication information such as beta blocker, a commonly used blood pressure lowering drug, might be incorporated into physician’s diagnosis. We did not have sufficient information on dietary habits to include in our analysis and we did not assess familial fitness or hypertension. It is possible that residual confounding by these factors may exist, although it seems unlikely that it would account for all the observed association between estimated cardiorespiratory fitnessand hypertension. Lastly, the non-exercise equation was chosen based on our previous work, therefore, we do not know if the key findings might be influenced by cardiorespiratory fitness estimated from other non-exercise equations. Future studies with larger samples of women, more diverse population, and estimated cardiorespiratory fitness produced from other non-exercise equations are warranted to provide a better picture of the relationship between estimated cardiorespiratory fitness and hypertension.
The current study is the first to examine the association between estimated cardiorespiratory fitness and incident hypertension. Our result supports the existing literatures in concluding that fitness determined by a variety of methods is inversely associated with the risk of developing hypertension. Knowing a patient’s cardiorespiratory fitness level might help health care providers identify those high-risk patients with low fitness levels for primary prevention of hypertension such as physical activity counseling. Though we note some limitations of the study, it has laid a comparative groundwork for future non-exercise estimated fitness equations to predict incident hypertension in other cohorts which should include larger numbers of women and more diverse populations.
Clinical Significance.
Access to cardiorespiratory fitness is limited due to the cost and burden of exercise testing.
Non-exercise algorithms utilizing patients’ health records data can be used to estimate cardiorespiratory fitness.
This study linked non-exercise estimated cardiorespiratory fitness to incident hypertension.
Knowing a patient’s fitness level might help health care providers identify those high-risk patients with low fitness levels for primary prevention of hypertension.
ACKNOWLEDGMENT
We thank the Cooper Clinic physicians and technicians for collecting the baseline data, and staff at the Cooper Institute for data entry and data management.
DISCLOSURE
This work was supported by National Institutes of Health grants AG06945, HL62508, and DK088195. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declarations of Competing Interest
None. The authors declared no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DATA AVAILABILITY
The data underlying this article cannot be shared publicly due to an agreement with the Cooper Institute. However, a limited working dataset might be shared on reasonable request to the corresponding author.
REFERENCES
- 1.Centers for Disease Control and Prevention. Hypertension cascade: hypertension prevalence, treatment and control estimates among U.S. adults aged 18 years and older apply the criteria from the American College of Cardiology and American Heart Association’s 2017 hypertension guideline – NAHENS 2015–2018. Atlanta, GA: U.S. Department of Health and Human Services; 2021. Accessed January 23, 2022. [Google Scholar]
- 2.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. The Lancet. 2005;365(9455):217–223. doi: 10.1016/s0140-6736(05)17741-1 [DOI] [PubMed] [Google Scholar]
- 3.Carnethon MR, Evans NS, Church TS, et al. Joint associations of physical activity and aerobic fitness on the development of incident hypertension: Coronary artery risk development in young adults. Hypertension. 2010;56(1):49–55. doi: 10.1161/HYPERTENSIONAHA.109.147603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chase NL, Sui X, Lee DC, Blair SN. The association of cardiorespiratory fitness and physical activity with incidence of hypertension in men. American Journal of Hypertension. 2009;22(4):417–424. doi: 10.1038/ajh.2009.6 [DOI] [PubMed] [Google Scholar]
- 5.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA - Journal of the American Medical Association. 2009;302(4):401–411. doi: 10.1001/jama.2009.1060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity and the risk of death in women: The St. James Women Take Heart Project. Circulation. 2003;108(13):1554–1559. doi: 10.1161/01.CIR.0000091080.57509.E9 [DOI] [PubMed] [Google Scholar]
- 7.Kodama S CLINICIAN ‘ S CORNER Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortalit1. Kodama S. CLINICIAN ‘ S CORNER Cardiorespiratory Fitness as a Quantitative Predictor of All-Cause Mortality and Cardiovascular Events. J Am Med Assoc. 2009; Journal of American Medical Association. 2009;301(19):2024–2035. [DOI] [PubMed] [Google Scholar]
- 8.Kokkinos P, Myers Jonathan, Kokkinos John Peter, et al. Exercise capacity and mortality in black and white men. Circulation. 2008;117(5):614–622. doi: 10.1161/CIRCULATIONAHA.107.734764 [DOI] [PubMed] [Google Scholar]
- 9.Artero EG, Jackson AS, Sui X, et al. Longitudinal algorithms to estimate cardiorespiratory fitness: Associations with nonfatal cardiovascular disease and disease-specific mortality. Journal of the American College of Cardiology. 2014;63(21):2289–2296. doi: 10.1016/j.jacc.2014.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta S, Rohatgi A, Ayers CR, et al. Cardiorespiratory fitness and classification of risk of cardiovascular disease mortality. Circulation. 2011;123(13):1377–1383. doi: 10.1161/CIRCULATIONAHA.110.003236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross R, Blair SN, Arena R, et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Vol 134.; 2016. doi: 10.1161/CIR.0000000000000461 [DOI] [PubMed] [Google Scholar]
- 12.Kaminsky LA, Arena R, Beckie TM, et al. The importance of cardiorespiratory fitness in the United States: The need for a national registry: A policy statement from the american heart association. Circulation. 2013;127(5):652–662. doi: 10.1161/CIR.0b013e31827ee100 [DOI] [PubMed] [Google Scholar]
- 13.Nes BM, Janszky I, Vatten LJ, Nilsen TIL, Aspenes ST, WislØff U. Estimating V̇O2peak from a nonexercise prediction model: The HUNT study, Norway. Medicine and Science in Sports and Exercise. 2011;43(11):2024–2030. doi: 10.1249/MSS.0b013e31821d3f6f [DOI] [PubMed] [Google Scholar]
- 14.Jackson AS, Sui X, O’Connor DP, et al. Longitudinal cardiorespiratory fitness algorithms for clinical settings. American Journal of Preventive Medicine. 2012;43(5):512–519. doi: 10.1016/j.amepre.2012.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. American Journal of Preventive Medicine. 2005;29(3):185–193. doi: 10.1016/j.amepre.2005.06.004 [DOI] [PubMed] [Google Scholar]
- 16.Stamatakis E, Hamer M, O’Donovan G, Batty GD, Kivimaki M. A non-exercise testing method for estimating cardiorespiratory fitness: associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts. European heart journal. 2013;34(10):750–758. doi: 10.1093/eurheartj/ehs097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow CE, LaMonte MJ, FitzGerald SJ, Kampert JB, Perrin JL, Blair SN. Cardiorespiratory fitness is an independent predictor of hypertension incidence among initially normotensive healthy women. American Journal of Epidemiology. 2006;163(2):142–150. doi: 10.1093/aje/kwj019 [DOI] [PubMed] [Google Scholar]
- 18.Kampert JB, Blair SN, Barlow CE, Kohl HW. Physical activity, physical fitness, and all-cause and cancer mortality: A prospective study of men and women. Annals of Epidemiology. 1996;6(5):452–457. doi: 10.1016/S1047-2797(96)00059-2 [DOI] [PubMed] [Google Scholar]
- 19.BLAIR SN, KANNEL WB, KOHL HW, GOODYEAR N, WILSON PWF. SURROGATE MEASURES OF PHYSICAL ACTIVITY AND PHYSICAL FITNESS: EVIDENCE FOR SEDENTARY TRAITS OF RESTING TACHYCARDIA, OBESITY, AND LOW VITAL CAPACITY. American Journal of Epidemiology. 1989;129(6):1145–1156. doi: 10.1093/oxfordjournals.aje.a115236 [DOI] [PubMed] [Google Scholar]
- 20.Levine GN, Al-Khatib SM, Beckman JA, et al. Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–1324. doi: 10.1161/HYP.0000000000000066/-/DC129133354 [DOI] [Google Scholar]
- 21.Blair SN, Goodyear NN, Gibbons LW, Cooper KH, Cooper Clinic Gibbons the. Physical Fitness and Incidence of Hypertension in Healthy Normotensive Men and Women. http://jama.jamanetwork.com/ [PubMed] [Google Scholar]
- 22.PAFFENBARGER RS Jr., WING AL, HYDE RT, JUNG DL. PHYSICAL ACTIVITY AND INCIDENCE OF HYPERTENSION IN COLLEGE ALUMNI. American Journal of Epidemiology. 1983;117(3):245–257. doi: 10.1093/oxfordjournals.aje.a113537 [DOI] [PubMed] [Google Scholar]
- 23.Huang Z, Willett WC, Manson JE, et al. Annals of Internal Medicine Body Weight, Weight Change, and Risk for Hypertension in Women. Vol 128.; 1998. http://annals.org/pdfaccess.ashx?url=/data/journals/aim/19899/ [DOI] [PubMed] [Google Scholar]
- 24.Lee DC, Sui X, Church TS, Lavie CJ, Jackson AS, Blair SN. Changes in fitness and fatness on the development of cardiovascular disease risk factors: Hypertension, metabolic syndrome, and hypercholesterolemia. Journal of the American College of Cardiology. 2012;59(7):665–672. doi: 10.1016/j.jacc.2011.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng C, Zhang D, Chen S, Duan G. The association of cardiorespiratory fitness and the risk of hypertension: a systematic review and dose–response meta-analysis. Journal of Human Hypertension. 2021;(August 2020):1–9. doi: 10.1038/s41371-021-00567-8 [DOI] [PubMed] [Google Scholar]
- 26.Gando Y, Sawada SS, Kawakami R, et al. Combined association of cardiorespiratory fitness and family history of hypertension on the incidence of hypertension: a long-term cohort study of Japanese males. Hypertension Research. 2018;41(12):1063–1069. doi: 10.1038/s41440-018-0117-2 [DOI] [PubMed] [Google Scholar]
- 27.Kunutsor SK, Kurl S, Laukkanen JA. Association of oxygen uptake at ventilatory threshold with risk of incident hypertension: a long-term prospective cohort study. Journal of Human Hypertension. 2017;31(10):654–656. doi: 10.1038/jhh.2017.39 [DOI] [PubMed] [Google Scholar]
- 28.Crump C, Sundquist J, Winkleby MA, Sundquist K. Interactive effects of physical fitness and body mass index on the risk of hypertension. JAMA Internal Medicine. 2016;176(2):210–216. doi: 10.1001/jamainternmed.2015.7444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Liu K. Cardiorespiratory Fitness in Young Adulthood. Jama. 2003;290(23):3092–3100. http://www.ncbi.nlm.nih.gov/pubmed/14679272 [DOI] [PubMed] [Google Scholar]
- 30.Faselis C, Doumas M, Kokkinos JP, et al. Exercise capacity and progression from prehypertension to hypertension. Hypertension. 2012;60(2):333–338. doi: 10.1161/HYPERTENSIONAHA.112.196493 [DOI] [PubMed] [Google Scholar]
- 31.Juraschek SP, Blaha MJ, Whelton SP, et al. Physical fitness and hypertension in a population at risk for cardiovascular disease: The Henry Ford ExercIse Testing (FIT) Project. Journal of the American Heart Association. 2014;3(6):1–11. doi: 10.1161/JAHA.114.001268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jae SY, Heffernan KS, Yoon ES, et al. Temporal changes in cardiorespiratory fitness and the incidence of hypertension in initially normotensive subjects. American Journal of Human Biology. 2012;24(6):763–767. doi: 10.1002/ajhb.22313 [DOI] [PubMed] [Google Scholar]
- 33.Bakker EA, Sui X, Brellenthin AG, Lee DC. Physical activity and fitness for the prevention of hypertension. Current Opinion in Cardiology. 2018;33(4):394–401. doi: 10.1097/HCO.0000000000000526 [DOI] [PubMed] [Google Scholar]
- 34.Fagard RH. Physical activity, physical fitness and the incidence of hypertension. Journal of Hypertension. 2005;23(2):265–267. doi: 10.1097/00004872-200502000-00005 [DOI] [PubMed] [Google Scholar]
- 35.Bouchard C, An P, Rice T, et al. Familial aggregation of V̇O(2max) response to exercise training: Results from the HERITAGE family study. Journal of Applied Physiology. 1999;87(3):1003–1008. doi: 10.1152/jappl.1999.87.3.1003 [DOI] [PubMed] [Google Scholar]
- 36.Thompson PD, Buchner D, Piña IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A statement from the council on clinical cardiology (subcommittee on exercise, rehabilitation, and prevention) and the council on nutrition, physical. Circulation. 2003;107(24):3109–3116. doi: 10.1161/01.CIR.0000075572.40158.77 [DOI] [PubMed] [Google Scholar]
- 37.Fagard RH. Exercise is good for your blood pressure: Effects of endurance training and resistance training. Clinical and Experimental Pharmacology and Physiology. 2006;33(9):853–856. doi: 10.1111/j.1440-1681.2006.04453.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article cannot be shared publicly due to an agreement with the Cooper Institute. However, a limited working dataset might be shared on reasonable request to the corresponding author.


