Abstract
Background and Objectives
Nursing staff turnover is a substantial concern for nursing homes that care for millions of older individuals, especially during the coronavirus disease 2019 pandemic. Low pay is considered as one of the key reasons for high turnover. However, we do not know whether increasing wages can lead to lower turnover. In this study, we fill this gap in our understanding by analyzing the relationship between wages and nursing staff turnover.
Research Design and Methods
We obtained data on hourly wages (Medicare Cost Reports), turnover (Iowa Department of Human Services), and nursing home and resident characteristics (Nursing Home Compare and LTCFocus) from 2013 to 2017. We summarized the characteristics of nursing homes as well as turnover trends over time. Next, we used pooled ordinary least squares (OLS) and facility fixed effects regressions to examine the relationship between wages and turnover adjusting for nursing home and resident characteristics.
Results
Among the 396 nursing homes in Iowa, average hourly wage was $27.0 for registered nurses (RNs), $21.6 for licensed practical nurses (LPNs), and $14.1 for certified nurse aides (CNAs) during 2013–2017. Average turnover rates were increasing over time for all staff types and in 2017, turnover rates were 46.0% for RNs, 44.4% for LPNs, and 64.7% for CNAs. In both pooled OLS and facility fixed effects regressions, higher wages were associated with lower turnover of CNAs but not LPNs or RNs. The magnitude of the effect of wages on turnover for CNAs was lower in facility fixed effects regressions.
Discussion and Implications
We found a significant relationship between hourly wages and turnover for CNAs but not for LPNs or RNs. Focusing on higher wages alone may not lead to lower turnover of all types of nursing staff in nursing homes. We should also focus on nonwage factors related to turnover.
Keywords: Aging, Long-term care, Postacute care
Translational Significance: High turnover of RNs, LPNs, and CNAs in nursing homes has been an ongoing concern to policymakers and nursing homes and this problem has been amplified during the coronavirus disease 2019 pandemic. One of the approaches recommended to reduce turnover is to increase wages. However, our findings suggest that increasing wages reduce turnover for CNAs but not for LPNs or RNs. Facilities should also focus on nonwage factors such as fringe benefits, staff empowerment, and organizational culture to reduce turnover.
Background and Objectives
High rates of nursing staff turnover are a substantial concern for nursing homes that care for millions of older individuals whose physical and cognitive impairments make them vulnerable, especially in the middle of a pandemic like coronavirus disease 2019 (COVID-19). There is considerable variation in turnover rates across different states. In Florida, licensed nurse turnover rate was 34.7% during the 2002–2009 period (Thomas et al., 2013), whereas in California, licensed nurse turnover rate was 52% during the 2005–2011 period (Antwi & Bowblis, 2018). Similarly, a national survey of nursing homes in 2004, the latest available national survey, suggests that registered nurse (RN) turnover was 56.1% with the turnover of nurse assistants as high as 74.5% (Donoghue, 2010). A more recent study used Payroll-Based Journal data and found much higher median turnover rates for RNs (102.9%), licensed practical nurses (LPNs; 79.8%), and certified nursing aides (CNAs; 98.8%) between 2017 and 2018 (Gandhi et al., 2021). Several studies have examined the role of job design, organizational, and local economic factors on nursing staff turnover in nursing homes (Banaszak-Holl & Hines, 1996; Castle & Engberg, 2006; Donoghue, 2010) as well as the adverse impact of turnover on quality (Antwi & Bowblis, 2018; Lerner et al., 2014). Low wages are often considered one of the reasons for high turnover in nursing homes, but the empirical evidence is unclear.
High nursing staff turnover in nursing homes is associated with higher mortality (Antwi & Bowblis, 2018) and an increased number of deficiency citations (Antwi & Bowblis, 2018; Lerner et al., 2014). A recent study found that nursing staff turnover was associated with an increased likelihood of infection control citation, which is particularly concerning in the midst of the COVID-19 pandemic (Loomer et al., 2021). There is also some evidence to suggest that CNA turnover is associated with higher odds of pressure ulcers, pain, and urinary tract infections in nursing homes (Trinkoff et al., 2013). With every staff member who leaves, the nursing homes need to hire new staff who, even with training, might need more time understanding the regulatory standards as well as needs and preferences of residents. A low turnover of staff may also suggest that employees are happy at their workplace and in turn may provide quality care. When turnover rates are low, each staff working in the facility has more experience dealing with the needs of the residents and can meet the regulatory standards (Antwi & Bowblis, 2018). Despite several studies highlighting the importance of lower staff turnover in improving nursing home quality, very few studies have examined potential ways to lower staff turnover including the role played by wages.
From the employer’s perspective, high nursing staff turnover can be financially costly because employers need to replace departing staff with new ones and hiring/training new staff requires resources. In addition, spending money on advertising and/or training new hires also takes away resources that could potentially be spent on quality improvement efforts. There may be a business case for nursing staff retention (Jones & Gates, 2007) with one study estimating the cost per RN turnover exceeding $80,000 (Jones, 2008). However, not all studies agree on the business case for reducing turnover with one cross-sectional study suggesting that higher turnover is associated with lower costs; it may be that economizing on staff training and wages while accepting higher turnover is cost-saving for nursing homes (Mukamel et al., 2009). Economic theory suggests that increasing wages relative to wages paid in the local market should lead to decreases in voluntary turnover of staff (Kim, 1999). Thus, nursing homes may be able to reduce turnover by increasing wages. However, the findings from the few studies that have examined the effect of wages on nursing staff turnover are mixed. In a study of Texas nursing homes, higher wages were associated with lower turnover for CNAs but not for RNs or LPNs (Kash et al., 2006). Similarly, another study using national survey data from 2004 found that higher wages are associated with lower odds of nursing assistant turnover (Temple et al., 2009). However, some studies have found no relationship between wages and turnover for CNAs (Donoghue, 2010; Kennedy et al., 2020), and one study found that higher LPN wages are associated with higher LPN turnover (Donoghue, 2010).
Staff retention has also been widely used in the literature to evaluate worker stability. While turnover rate is often measured by the number of terminations as a proportion of total number of staff over a given period, retention accounts for employment duration (Donoghue, 2010). A study using 2004 data from the National Nursing Home Survey found that a $1 increase in wages is associated with 2.1 additional months of tenure among CNAs (Wiener et al., 2009). In addition to wages, characteristics such as age and education were significant predictors of job tenure (Wiener et al., 2009). In contrast, owner-managed nursing homes had higher worker retention rates in Ohio, but higher wages were not associated with better retention, suggesting that organization structure associated with managerial ownership may be a significant factor in retention (Huang & Bowblis, 2020). In yet another study using data of Ohio nursing homes, neither higher wages nor empowerment were associated with high CNA retention on their own but the interaction between higher wages and higher empowerment was significantly associated with retention (Kennedy et al., 2021). While we only have access to turnover data in our study, the literature on staff retention provides additional insights into staff stability in nursing homes.
Most of the existing research on the role of wages on nursing home staff turnover or retention relies on a cross-sectional analysis of nursing home data from 1 year (Donoghue, 2010; Kennedy et al., 2020, 2021; Temple et al., 2009) or pooled cross-sectional analysis (Huang & Bowblis, 2020). Researchers have attempted to measure staff empowerment or managerial styles in some of these studies, but there is still potential for other unobserved, unmeasured confounding factors (e.g., organizational culture and the physical work environment) that are correlated with both wages and turnover. Cross-sectional data analyses are vulnerable to such omitted variable bias. In this study, we attempt to address the limitations of previous studies by using longitudinal data from Iowa to examine the variation in wages within facilities over time and its effect on nursing staff turnover. Facility fixed effects (FE) models allow us to control for time-invariant facility-level unobservable factors. In addition to wages, many other factors may be associated with nursing home staff turnover. Several studies have examined the role of job design, organizational, and local economic factors on nursing staff turnover in nursing homes (Banaszak-Holl & Hines, 1996; Castle & Engberg, 2006; Donoghue, 2010). In this study, we examine the role of wages on staff turnover using longitudinal data while adjusting for different organizational and local economic factors. Findings from facility FE analyses are more reliable compared to pooled or cross-sectional analyses. Our results from facility FE regressions will use within-facility variation to assess the effect of changes in wages on turnover.
Research Design and Methods
Data
We obtain information on wages and other characteristics from 2013 to 2017 using several different data sources. We use Medicare Cost Reports to obtain information on nursing staff wages, staffing level, and occupancy. We obtain nursing staff turnover information directly from the Iowa Department of Human Services (DHS). Both wages and turnover are measured during the same year. We use Long-Term Care Facts on care in the United States (LTCFocus) and Nursing Home Compare to obtain nursing home and resident characteristics. We link these data sets using federal provider ID.
All freestanding Medicare-certified nursing homes are required to file cost reports with the Centers of Medicare and Medicaid Services (CMS) on an annual basis. Providers report data including bed days available and inpatient days, based on which we can derive occupancy levels. Since 2011, CMS requires Medicare-certified nursing homes to provide expenditure data for full-time and part-time direct care employees who are directly hired and under contract, including RNs, LPNs, CNAs, and other medical and therapy staff (Wells & Harrington, 2013). Using these cost report data filed by nursing homes, we calculate hourly wage and staffing hours per resident day (HPRD) of RNs, LPNs, and CNAs from 2013 to 2017.
A small fraction of facilities submit multiple cost reports in a year. We follow strategies used in existing studies to clean up cost report data before extracting any measures and merging with other data sets (Bowblis & Brunt, 2014; Sharma et al., 2019, 2021). We first combine multiple reports of the same provider based on the fiscal year begin date and fiscal year end date. For each year, we only include cost reports with a full year data (365 ± 5 days) and those whose fiscal year ended in the same calendar year.
Iowa DHS collects employee turnover data for all nursing homes operating in Iowa on an annual basis, including nursing, medical, administrative, and other staff. We directly obtained data on nursing staff turnover from the Iowa DHS.
We obtain nursing home and resident-level information from two sources: Long-Term Care Facts on care in the United States (LTCFocus, n.d.) and Nursing Home Compare. LTCFocus aggregates individual resident-level data to the facility level. Using the LTCFocus data, we obtained resident- and facility-level characteristics including resident demographic characteristics such as age, gender, and race, activities of daily living (ADL) index, number of beds, occupancy levels, payer mix (percent of Medicaid residents and percent of Medicare residents), and chain membership. We also derive the Herfindahl–Hirschman Index (HHI), a measure of market competitiveness, based on the number of beds and using the county as the geographic market boundary. We obtain profit status and Social Security Administration (SSA) code for county from Nursing Home Compare.
Finally, we merge the data with Rural–Urban Commuting Area Codes using ZIP code to identify nursing homes operating in urban and rural areas. We also use three county-level variables relevant to wages and staff turnover in nursing homes. We obtain the population of individuals aged 65 years and older from the U.S. Census Bureau and use it to calculate the number of nursing home beds per 1,000 individuals aged 65 and older. We obtain annual unemployment rates from the Bureau of Labor Statistics and per capita income from the Bureau of Economic Analysis. We link the county-level data with provider-level data using county SSA code.
Study Sample
Of the 2,092 observations on 439 unique nursing homes with turnover data from 2013 to 2017, we were able to merge 1,925 observations with Medicare Cost Report, LTCFocus, Nursing Home Compare, and county-level contextual measures. We excluded 71 observations without key variables, with occupancy greater than 100%, with unreasonable staffing levels (i.e., have zero RN hours but have 60 or more beds, have total staffing HPRD that are less than 0.5 or more than 12), or with unreasonable hourly wages that are below $7.25 (the minimum wage in Iowa in our study period). In addition, we excluded 138 observations for outlier data: wages in the top or bottom one percentile, or turnover in the top one percentile. Our final sample includes 1,716 observations on 396 unique nursing homes from 2013 to 2017.
Measurements
Outcomes
Our outcome variables include the annual turnover rates of RNs (including Director of Nursing [DON]), LPNs, and CNAs in Iowa nursing homes. Turnover rates are collected by the Iowa DHS and are defined as the total number of terminations for the given staff type divided by the average number of employees for that staff type during the given year. This definition of turnover is consistent with previous studies (Donoghue, 2010; Kennedy et al., 2020).
Key independent variables
Our key independent variables are the average hourly wages (in U.S. $) of directly employed RNs, LPNs, and CNAs (excluding contracted staff). We calculate hourly wage for each staff type by dividing the total wages and salaries (excluding fringe benefits; Worksheet S-3, Part-V, Column 1, Lines 1–3) by the number of paid hours (Worksheet S-3, Part-V, Column 4, Lines 1–3). When calculating RN hourly wage, we also incorporate the salary and paid hours associated with Nursing Administration (Worksheet S-3, Part-III, Line 7). We adjust all wages to 2017 dollars.
Covariates
In empirical models, we control for a set of resident- and facility-level characteristics that may affect the relationship between nursing staff hourly wage and turnover, including ADL index, age, percent of female, percent of White, number of beds, occupancy rate, payer mix (percent of Medicare-pay residents and percent of Medicaid-pay residents), staffing levels (defined as the number of staffing HPRD), for-profit status, multifacility organization, urban, and whether located in a competitive market (Banaszak-Holl & Hines, 1996; Castle & Engberg, 2006; Donoghue, 2010; Kennedy et al., 2020). Occupancy rate is derived from the number of total inpatient days (Worksheet S-3, Part I, Column 7, sum of Lines 1 and 2) divided by a number of bed days available (Worksheet S-3, Part I, Column 2, sum of Lines 1 and 2). RN HPRD is calculated by dividing the sum of paid hours of directly employed RN, contracted RN (Worksheet S-3, Part-V, Line 14), and Nursing Administration by total inpatient days. LPN and CNA HPRD are calculated by dividing the summed paid hours of directly employed staff and contracted labor for each type of staff by total inpatient days. We created a binary measure of market competitiveness based on HHI. Using the number of beds, we define an unconcentrated market as one that has HHI <0.15 (U.S. Department of Justice & Federal Trade Commission, 2010). All the regressions also control for three county-level contextual measures: number of nursing home beds per 1,000 older adults as a measure of supply, per capita income (adjusted to 2017 dollars) as a measure of economic health, and the unemployment rate as a measure of local labor market characteristics (Banaszak-Holl & Hines, 1996).
Statistical Analyses
We summarize the characteristics of the pooled sample of nursing homes in Iowa using means and standard deviations for continuous variables and counts and proportions for categorical variables. We assess the trends in turnover and hourly wages of RNs, LPNs, and CNAs from 2013 to 2017 using bar charts and trended lines. To compare our findings to existing studies of turnover that are cross-sectional in nature, we initially examine the relationship between nursing staff hourly wage and turnover using linear pooled regression models. However, time-invariant factors at the facility level could bias our relationship between wages and turnover in pooled regressions. In pooled regressions, the relationship observed between wages and turnover could occur due to the correlation of wages with other unobserved factors. While we can attempt to control for unobserved factors such as manager’s quality, we are still unsure about whether we have captured all such factors. Thus, we examine the relationship between wages and turnover using linear facility FE regression models that control for facility-level time-invariant factors. This approach supports estimation of the impact of a facility’s changes in wages on changes in turnover. We conducted subgroup analyses by profit status, urban/rural location, and market concentration. Finally, we checked the robustness of our findings by restricting our sample of nursing homes to only those that have complete data in all years. In all regressions, we control for secular trends in wages and turnover by including dummy variables for the years. We cluster standard errors at the facility level to account for the correlations among error terms over time for a given facility.
Results
We summarized the characteristics of the pooled sample in Table 1. On average, Iowa nursing homes had 71.7 beds. About 57.5% of nursing homes were for-profit and a similar percentage (57.8%) were owned by multifacility organizations. As expected, a small fraction of the nursing homes were in urban areas (30.2%) and only 20.3% were in the unconcentrated market. Total occupancy level in Iowa nursing homes was low at 79.1% compared to national average of 85% in 2017 (Medicare Payment Advisory Commission, 2019). Percent of residents on Medicaid pay was 47.7% and percent of residents on Medicare pay was 7.9%. Average age of the nursing home residents was 83.3 years and average ADL index was 14.3. A large majority of the nursing home population in Iowa nursing homes was White (96.9%). Hourly wages for RNs, LPNs, and CNAs were $27.0, $21.6, and $14.1, respectively, during our study period. To put the wage rates in context, the 2017 national mean hourly wages for RNs, LPNs, and CNAs employed in nursing facilities were $31.6, $22.6, and $13.2 according to the U.S. Bureau of Labor Statistics.
Table 1.
Descriptive Statistics of All Nursing Homes in Iowa From 2013 to 2017
| Variables | Mean (SD) | N | % |
|---|---|---|---|
| ADL index | 14.27 (2.08) | ||
| Number of beds | 71.70 (30.15) | ||
| Occupancy % | 79.09 (12.55) | ||
| Resident payer mix % | |||
| Medicare pay | 7.86 (7.13) | ||
| Medicaid pay | 47.65 (16.99) | ||
| Age | 83.35 (4.97) | ||
| Female % | 69.67 (9.24) | ||
| White % | 96.95 (6.20) | ||
| Staffing hours per resident day | |||
| RN | 0.76 (0.26) | ||
| LPN | 0.63 (0.22) | ||
| CNA | 2.47 (0.62) | ||
| For-profit | 987 | 57.5% | |
| Multifacility organization | 992 | 57.8% | |
| Urban | 518 | 30.2% | |
| Unconcentrated market | 348 | 20.3% | |
| County-level characteristics | |||
| Per capita income (in $1,000) | 47.03 (5.89) | ||
| Number of nursing home beds per 1,000 individuals aged 65 and older | 67.67 (23.35) | ||
| Unemployment rate % | 3.90 (0.89) | ||
| Staffing hourly wage $ | |||
| RN hourly wage | 26.97 (3.52) | ||
| LPN hourly wage | 21.59 (2.27) | ||
| CNA hourly wage | 14.09 (1.45) | ||
| Number of observations | 1,716 | ||
| Number of unique providers | 396 |
Note: ADL = activities of daily living; RN = registered nurse; LPN = licensed practical nurse; CNA = certified nurse aide; HPRD = hours per resident day.
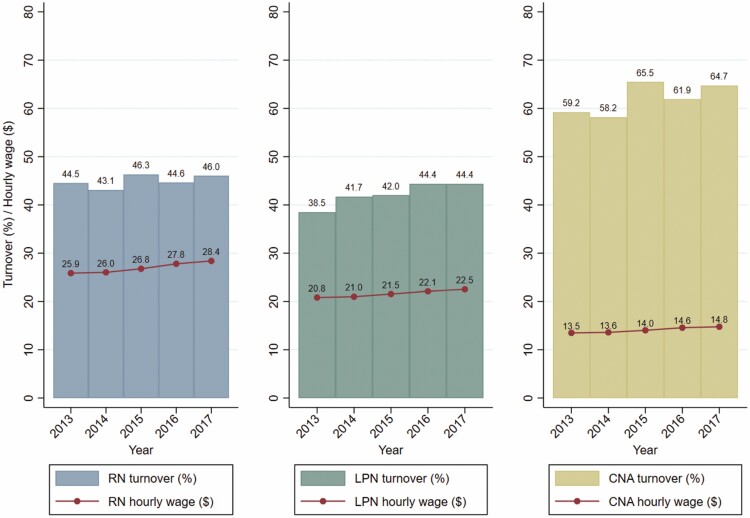
Figure 1 shows the trends in the annual turnover rates and hourly wages of each type of nursing staff from 2013 to 2017. All staff types saw increased rates of turnover over time. RN and LPN turnover rates were high at 46.0%, and 44.4%, respectively, in 2017. However, CNA turnover rate was the highest among the three staff types at 64.7% in 2017. From 2013 to 2017, RN wages increased by $2.5 per hour, LPN wages increased by $1.7 per hour, and CNA wages increased by $1.3 per hour.
Figure 1.
Trends of turnover and hourly wages of RNs, LPNs, and CNAs in Iowa nursing homes from 2013 to 2017. Note: RN = registered nurse; LPN = licensed practical nurse; CNA = certified nurse aide.
Table 2 presents the results from pooled ordinary least squares (OLS) and facility FE regressions. Controlling for other factors, higher wages were significantly associated with lower turnover of CNAs in both pooled regressions and FE regressions, but the findings were not significant for RNs or LPNs at 5% level. In both pooled and facility FE regressions, higher staffing levels were associated with lower turnover for the corresponding staff types. None of the county-level characteristics were associated with turnover in the facility FE regressions.
Table 2.
The Relationship Between Hourly Wages and Turnover—Pooled OLS and Facility Fixed Effects Regressions
| Variables | Pooled OLS | Facility fixed effects | ||||
|---|---|---|---|---|---|---|
| RN turnover | LPN turnover | CNA turnover | RN turnover | LPN turnover | CNA turnover | |
| RN hourly wage $ | −0.55 (0.30) | −0.48 (0.47) | ||||
| LPN hourly wage $ | −0.95 (0.49) | −1.10 (0.69) | ||||
| CNA hourly wage $ | −3.51*** (0.82) | −1.80* (0.81) | ||||
| ADL index | 0.36 (0.59) | 1.12 (0.60) | 1.99*** (0.52) | 0.47 (0.77) | −0.24 (0.86) | 1.34* (0.57) |
| Number of beds | −0.02 (0.04) | −0.00 (0.04) | −0.01 (0.04) | −0.38 (0.40) | −0.06 (0.44) | −0.20 (0.22) |
| Occupancy % | −0.37*** (0.10) | −0.31*** (0.09) | −0.18* (0.09) | −0.21 (0.19) | −0.38 (0.20) | 0.03 (0.13) |
| Resident payer mix % | ||||||
| Medicare pay | 0.31 (0.17) | 0.01 (0.17) | −0.00 (0.15) | 0.11 (0.19) | −0.08 (0.21) | −0.21 (0.12) |
| Medicaid pay | 0.12 (0.09) | 0.13 (0.08) | 0.11 (0.08) | −0.06 (0.10) | 0.03 (0.10) | −0.14 (0.08) |
| Age | −0.33 (0.41) | −0.62 (0.32) | −0.45 (0.33) | −0.73 (0.75) | 0.23 (0.85) | −0.05 (0.57) |
| Female % | 0.21 (0.14) | 0.31* (0.13) | 0.17 (0.12) | −0.05 (0.18) | −0.09 (0.20) | −0.10 (0.14) |
| White % | −0.26 (0.18) | −0.39* (0.19) | −0.32 (0.19) | −0.21 (0.32) | 0.11 (0.37) | −0.30 (0.19) |
| Staffing hours per resident day | ||||||
| RN | −10.45* (4.32) | 5.51 (4.04) | 4.35 (4.26) | −14.02 (7.88) | 2.37 (7.10) | 1.72 (5.99) |
| LPN | 9.76 (4.99) | −14.89** (5.59) | 10.46* (4.80) | 0.31 (8.03) | −43.05*** (9.89) | 15.00* (7.33) |
| CNA | −4.95** (1.75) | −4.65** (1.66) | −12.86*** (1.91) | 0.99 (3.28) | −2.77 (3.71) | −14.67*** (2.96) |
| For-profit | 2.16 (2.44) | 4.70* (2.20) | 3.02 (2.29) | 1.58 (5.64) | −9.18 (7.44) | −6.46 (4.68) |
| Multifacility organization | 2.01 (2.44) | 0.17 (2.27) | −2.78 (2.33) | 1.32 (5.57) | 5.52 (5.96) | 1.91 (5.39) |
| Urban | 9.56* (4.31) | 10.36* (4.14) | 9.44* (3.79) | |||
| Unconcentrated market | −2.47 (4.78) | −1.09 (4.62) | −1.46 (4.15) | |||
| County-level characteristics | ||||||
| Number of nursing home beds per 1,000 individuals aged 65 and older | −0.15** (0.06) | −0.08 (0.06) | −0.17** (0.05) | −0.07 (0.23) | 0.28 (0.24) | −0.10 (0.16) |
| Per capita income (in $1,000) | 0.23 (0.23) | 0.17 (0.20) | −0.17 (0.21) | −0.55 (0.54) | 0.62 (0.57) | 0.45 (0.38) |
| Unemployment rate % | 0.45 (1.76) | −1.14 (1.64) | 0.83 (1.78) | 3.39 (3.13) | −3.44 (3.72) | 4.38 (2.49) |
Notes: N = 1,716. OLS = ordinary least square; RN = registered nurse; LPN = licensed practical nurse; CNA = certified nurse aide; ADL = activities of daily living. In both pooled OLS and facility fixed effects models, we control for year dummies. Robust standard errors clustered at the facility level are reported in parentheses.
*p < .05, **p < .01, ***p < .001.
Table 3 presents the results from pooled and facility FE regressions for the subgroups by profit status (Panel A), rurality (Panel B), and market concentration (Panel C). CNA hourly wages are associated with lower CNA turnover in facility FE regressions among for-profit facilities. Although the directions are as expected, we do not find significant associations between wages and turnover for CNAs in other subgroups in facility FE regressions. We also see evidence suggesting that LPN hourly wages are associated with lower LPN turnover in rural and concentrated markets. Hourly wages have no significant relationship with turnover for RNs in any of the subgroups in facility FE regressions.
Table 3.
The Relationship Between Hourly Wages and Turnover—Subgroup Analyses
| Subgroups | Pooled OLS | Facility fixed effects | ||||
|---|---|---|---|---|---|---|
| RN turnover | LPN turnover | CNA turnover | RN turnover | LPN turnover | CNA turnover | |
| Panel A: By for-profit status | ||||||
| For-profit (n = 987) | ||||||
| Hourly wage | −0.06 (0.57) | −0.54 (0.73) | −3.82** (1.20) | −0.74 (0.76) | −0.51 (1.04) | −2.75* (1.24) |
| Nonprofit (n = 729) | ||||||
| Hourly wage | −0.77* (0.35) | −1.39* (0.59) | −2.91** (1.04) | −0.43 (0.55) | −1.75 (0.98) | −0.76 (1.02) |
| Panel B: By urban/rural | ||||||
| Urban (n = 518) | ||||||
| Hourly wage | −0.31 (0.67) | 1.03 (0.96) | −1.08 (1.50) | −0.52 (0.81) | 0.55 (1.38) | −2.82 (1.55) |
| Rural (n = 1,198) | ||||||
| Hourly wage | −0.69* (0.33) | −2.27*** (0.55) | −4.65*** (0.92) | −0.41 (0.53) | −2.03* (0.81) | −1.25 (0.92) |
| Panel C: By market competitiveness | ||||||
| Unconcentrated market (n = 348) | ||||||
| Hourly wage | 0.49 (0.71) | 2.03 (1.21) | 0.83 (1.68) | −0.65 (0.92) | 2.66 (1.67) | −1.81 (2.11) |
| Concentrated market (n = 1,368) | ||||||
| Hourly wage | −0.76* (0.34) | −1.83*** (0.51) | −4.70*** (0.82) | −0.40 (0.53) | −2.07** (0.74) | −1.37 (0.85) |
Notes: RN = registered nurse; LPN = licensed practical nurse; CNA = certified nurse aide. In all regressions, we control for year dummies. Robust standard errors clustered at the facility level are reported in parentheses.
*p < .05, **p < .01, ***p < .001.
The findings from the smaller sample of nursing homes with complete data for all years are largely consistent with our main findings (Supplementary Table A1). Higher wages are associated with lower turnover for CNAs in both pooled and facility FE regressions, but the findings are significant only in the pooled regressions. For RNs and LPNs, the relationship between wages and turnover is not significant at a 5% level in either pooled or facility FE regressions.
Discussion and Implications
In our study, we examined the relationship between hourly wages and turnover for RNs, LPNs, and CNAs using longitudinal data of Iowa nursing homes. In our study, higher hourly wages are associated with lower turnover for CNAs, and the relationship is significant in both pooled OLS and facility FE regressions, although the magnitude of the effect is lower in facility FE regressions. The estimated coefficients for RN and LPN wages did not exhibit a significant relationship to RN and LPN turnover at the 5% level. Subgroup analysis revealed heterogeneous effects of wages on turnover. Higher hourly wages are associated with lower CNA turnover in FE regressions among for-profit facilities but not among nonprofit facilities. Higher LPN hourly wages are associated with lower LPN turnover among rural facilities and among nursing homes in concentrated markets.
Our results on the role of wages on turnover of nursing staff from pooled OLS regressions are generally consistent with the previous literature that has extensively analyzed the relationship between wages and turnover using cross-sectional data. For example, in a study of Texas nursing home facilities, higher wages were associated with lower turnover for CNAs but not RNs or LPNs (Kash et al., 2006). Similarly, a cross-sectional study of a nationally representative nursing home sample found that higher wages were associated with lower turnover of CNAs (Temple et al., 2009). In yet another study, higher starting wages had no significant relationship with RN turnover (Donoghue, 2010). In our study, we exploited the longitudinal data and estimated facility FE regressions to additionally control for unobserved time-invariant facility characteristics. The facility FE regressions from our study also show that higher wages are associated with lower turnover among the CNAs but not for LPNs and RNs. Subgroup analyses from our study suggest that the relationship between wages and turnover for CNAs and LPNs may differ by the type of facilities.
In addition to wages, our findings suggest that nonwage factors may be contributing to the turnover of RNs, LPNs, and CNAs in nursing homes. For example, a dollar increase in CNA wages (a 7% increase from current mean wages of $14.09) is associated with only 1.8 percentage points reduction in CNA turnover in our facility FE regressions suggesting that it is difficult to achieve a substantial reduction in turnover by small increases in wages. Several studies have examined the role of nonwage factors on turnover. For example, health insurance benefits and involvement in care planning may lead to lower turnover (Temple et al., 2009). In a study of hospital nurses, wages were correlated with professional commitment but did not have a significant correlation with intent-to-leave, whereas factors such as marital status, age of the youngest children, and job satisfaction had a significant negative correlation with turnover intention (Lu et al., 2002). In a recent study of Ohio nursing homes, factors such as empowerment and turnover of DON were significant predictors of CNA turnover (Kennedy et al., 2020). Another study found that higher wages coupled with empowerment were associated with higher CNA retention, a measure of staff stability closely related to turnover (Kennedy et al., 2021). In a study of RNs working in intensive care units, researchers found that higher wages were associated with small negative effects on the intent-to-leave, whereas organizational climate was much more important (Stone et al., 2007). Similarly, another study found that factors such as family needs, job satisfaction, and organizational commitment were important predictors of turnover (Brewer et al., 2009).
Our study findings have important implications on the policies designed to address high turnover of RNs, LPNs, and CNAs in nursing homes. Increasing wages paid to nursing staff has been proposed as a strategy to reduce turnover and therefore improve retention, especially among CNAs who provide the majority of the direct care (Denny-Brown et al., 2020; PHI, 2016; Stone et al., 2007; Stone & Wiener, 2001). While offering competitive wages paid to direct care workers is a necessary step to strengthen the workforce in crisis, especially for low-wage earners like CNAs, our results, together with previous literature on the relationship between wages and turnover, suggest that increasing wages alone will not be sufficient to reduce turnover among all types of nursing home staff. Nonwage factors including improving work environment, a culture that empowers staff, as well as fringe benefits such as health insurance should be considered along with higher wages (Brewer et al., 2009; Kennedy et al., 2020; Lu et al., 2002; Stone et al., 2007; Temple et al., 2009).
Our findings are subject to several limitations. First, our study uses data from Iowa nursing homes and thus, our findings are only generalizable to other states like Iowa. However, Iowa is among the few states that collect nursing staff turnover data on an annual basis and it allowed us to take advantage of longitudinal analysis. Second, facility FE regressions account for unobserved time-invariant facility-level characteristics, and we control for a set of time-varying organizational (e.g., ownership status, payer mix), resident (e.g., acuity), and market-level characteristics (e.g., unemployment), but there may be other time-varying confounders that could bias our results. Even though some of the nonwage factors can be accounted in the facility fixed effects, we did not have data on other time-varying nonwage factors that may contribute to turnover including the tenure of staff types.
We examined the relationship between wages and RN, LPN, and CNA turnover in Iowa nursing homes using robust facility FE regressions and found that higher wages are associated with lower turnover of CNAs but not RNs or LPNs. Our findings suggest that increasing wages may be insufficient to reduce the turnover of all nursing staff. Policymakers and nursing homes should also focus on nonwage factors that may contribute to turnover such as work environment, staff empowerment, as well as fringe benefits such as health insurance.
Supplementary Material
Contributor Information
Hari Sharma, Department of Health Management and Policy, College of Public Health, The University of Iowa, Iowa City, Iowa, USA.
Lili Xu, Department of Health Management and Policy, College of Public Health, The University of Iowa, Iowa City, Iowa, USA.
Funding
This study was partially supported by the New Faculty Research Award, College of Public Health, The University of Iowa.
Conflict of Interest
None declared.
References
- Antwi, Y. A., & Bowblis, J. R. (2018). The impact of nurse turnover on quality of care and mortality in nursing homes: Evidence from the Great Recession. American Journal of Health Economics, 4(2), 131–163. doi: 10.1162/ajhe_a_00096 [DOI] [Google Scholar]
- Banaszak-Holl, J., & Hines, M. A. (1996). Factors associated with nursing home staff turnover. The Gerontologist, 36(4), 512–7. doi: 10.1093/geront/36.4.512 [DOI] [PubMed] [Google Scholar]
- Bowblis, J. R., & Brunt, C. S. (2014). Medicare skilled nursing facility reimbursement and upcoding. Health Economics, 23(7), 821–840. doi: 10.1002/hec.2959 [DOI] [PubMed] [Google Scholar]
- Brewer, C. S., Kovner, C. T., Greene, W., & Cheng, Y. (2009). Predictors of RNs’ intent to work and work decisions 1 year later in a U.S. national sample. International Journal of Nursing Studies, 46(7), 940–956. doi: 10.1016/j.ijnurstu.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Castle, N. G., & Engberg, J. (2006). Organizational characteristics associated with staff turnover in nursing homes. The Gerontologist, 46(1), 62–73. doi: 10.1093/geront/46.1.62 [DOI] [PubMed] [Google Scholar]
- Denny-Brown, N., Stone, D., Hays, B., & Gallagher, D. (2020). COVID-19 intensifies nursing home workforce challenges. US Department of Health and Human Services Assistant Secretary for Planning and Evaluation Behavioral Health, Disability, and Aging Policy. https://aspe.hhs.gov/reports/covid-19-intensifies-nursing-home-workforce-challenges [Google Scholar]
- Donoghue, C. (2010). Nursing home staff turnover and retention: An analysis of national level data. Journal of Applied Gerontology, 29(1), 89–106. doi: 10.1177/0733464809334899 [DOI] [Google Scholar]
- Gandhi, A., Yu, H., & Grabowski, D. C. (2021). High nursing staff turnover in nursing homes offers important quality information. Health Affairs, 40(3), 384–391. doi: 10.1377/hlthaff.2020.00957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, S. S., & Bowblis, J. R. (2020). Workforce retention and wages in nursing homes: An analysis of managerial ownership. Journal of Applied Gerontology, 39(8), 902–907. doi: 10.1177/0733464818795433 [DOI] [PubMed] [Google Scholar]
- Jones, C. B. (2008). Revisiting nurse turnover costs: Adjusting for inflation. The Journal of Nursing Administration, 38(1), 11–18. doi: 10.1097/01.NNA.0000295636.03216.6f [DOI] [PubMed] [Google Scholar]
- Jones, C. B., & Gates, M. (2007). The costs and benefits of nurse turnover: A business case for nurse retention. The Online Journal of Issues in Nursing, 12(3). doi: 10.3912/OJIN.Vol12No03Man04 [DOI] [Google Scholar]
- Kash, B. A., Castle, N. G., Naufal, G. S., & Hawes, C. (2006). Effect of staff turnover on staffing: A closer look at registered nurses, licensed vocational nurses, and certified nursing assistants. The Gerontologist, 46(5), 609–619. doi: 10.1093/geront/46.5.609 [DOI] [PubMed] [Google Scholar]
- Kennedy, K. A., Abbott, K. M., & Bowblis, J. R. (2021). The one-two punch of high wages and empowerment on CNA retention. Journal of Applied Gerontology, 41(2), 312–321. doi: 10.1177/07334648211035659 [DOI] [PubMed] [Google Scholar]
- Kennedy, K. A., Applebaum, R., & Bowblis, J. R. (2020). Facility-level factors associated with CNA turnover and retention: Lessons for the long-term services industry. The Gerontologist, 60(8), 1436–1444. doi: 10.1093/geront/gnaa098 [DOI] [PubMed] [Google Scholar]
- Kim, M. (1999). Where the grass is greener: Voluntary turnover and wage premiums. Industrial Relations, 38(4), 584–603. doi: 10.1111/0019-8676.00146 [DOI] [Google Scholar]
- Lerner, N. B., Johantgen, M., Trinkoff, A. M., Storr, C. L., & Han, K. (2014). Are nursing home survey deficiencies higher in facilities with greater staff turnover. Journal of the American Medical Directors Association, 15(2), 102–107. doi: 10.1016/j.jamda.2013.09.003 [DOI] [PubMed] [Google Scholar]
- Loomer, L., Grabowski, D. C., Yu, H., & Gandhi, A. (2021). Association between nursing home staff turnover and infection control citations (SSRN Scholarly Paper ID 3766377). Social Science Research Network. https://papers.ssrn.com/abstract=3766377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LTCFocus . (n.d.). LTCFocus Public Use Data sponsored by the National Institute on Aging (P01 AG027296) through a cooperative agreement with the Brown University School of Public Health. doi: 10.26300/h9a2-2c26 [DOI] [Google Scholar]
- Lu, K. -Y., Lin, P. -L., Wu, C. -M., Hsieh, Y. -L., & Chang, Y. -Y. (2002). The relationships among turnover intentions, professional commitment, and job satisfaction of hospital nurses. Journal of Professional Nursing, 18(4), 214–219. doi: 10.1053/jpnu.2002.127573 [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission . (2019). Chapter 8. Skilled nursing facility services (pp. 193–224). MedPAC. https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/mar19_medpac_ch8_sec.pdf [Google Scholar]
- Mukamel, D. B., Spector, W. D., Limcangco, R., Wang, Y., Feng, Z., & Mor, V. (2009). The costs of turnover in nursing homes. Medical Care, 47(10), 1039–1045. doi: 10.1097/MLR.0b013e3181a3cc62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PHI . (2016). Raise the floor: Quality nursing home care depends on quality jobs. PHI. https://phinational.org/resource/raise-the-floor-quality-nursing-home-care-depends-on-quality-jobs/ [Google Scholar]
- Sharma, H., Hefele, J. G., Xu, L., Conkling, B., & Wang, J. W. (2021). First year of skilled nursing facility value-based purchasing program penalizes facilities with poorer financial performance. Medical Care, 59(12), 1099–1106. doi: 10.1097/MLR.0000000000001648 [DOI] [PubMed] [Google Scholar]
- Sharma, H., Konetzka, R. T., & Smieliauskas, F. (2017). The relationship between reported staffing and expenditures in nursing homes. Medical Care Research and Review, 76(6), 758–783. doi: 10.1177/1077558717739214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone, P. W., Mooney-Kane, C., Larson, E. L., Pastor, D. K., Zwanziger, J., & Dick, A. W. (2007). Nurse working conditions, organizational climate, and intent to leave in ICUs: An instrumental variable approach. Health Services Research, 42(3 Pt 1), 1085–1104. doi: 10.1111/j.1475-6773.2006.00651.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone, R., & Wiener, J. M. (2001). Who will care for us? Addressing the long-term care workforce crisis. US Department of Health and Human Services. https://aspe.hhs.gov/reports/who-will-care-us-addressing-long-term-care-workforce-crisis-1 [Google Scholar]
- Temple, A., Dobbs, D., & Andel, R. (2009). Exploring correlates of turnover among nursing assistants in the National Nursing Home Survey. Health Care Management Review, 34(2), 182–90. doi: 10.1097/HMR.0b013e31819c8b11 [DOI] [PubMed] [Google Scholar]
- Thomas, K. S., Mor, V., Tyler, D. A., & Hyer, K. (2013). The relationships among licensed nurse turnover, retention, and rehospitalization of nursing home residents. The Gerontologist, 53(2), 211–221. doi: 10.1093/geront/gns082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinkoff, A. M., Han, K., Storr, C. L., Lerner, N., Johantgen, M., & Gartrell, K. (2013). Turnover, staffing, skill mix, and resident outcomes in a national sample of US nursing homes. The Journal of Nursing Administration, 43(12), 630–636. doi: 10.1097/NNA.0000000000000004 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Justice, & Federal Trade Commission . (2010). Horizontal merger guidelines. US Department of Justice. https://www.justice.gov/atr/horizontal-merger-guidelines-08192010#2d [Google Scholar]
- Wells, J., & Harrington, C. (2013). Implementation of Affordable Care Act provisions to improve nursing home transparency and quality. Kaiser Commission on Medicaid and the Uninsured. https://www.kff.org/medicaid/report/implementation-of-affordable-care-act-provisions-to-improve-nursing-home-transparency-care-quality-and-abuse-prevention/ [Google Scholar]
- Wiener, J. M., Squillace, M. R., Anderson, W. L., & Khatutsky, G. (2009). Why do they stay? Job tenure among certified nursing assistants in nursing homes. The Gerontologist, 49(2), 198–210. doi: 10.1093/geront/gnp027 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.