This systematic review and meta-analysis evaluates the prevalence of perinatal depression in both mothers and fathers.
Key Points
Question
How often do both mothers and fathers (parental dyad) experience perinatal mood disorders?
Findings
In this systematic review and meta-analysis of 23 studies with 29 286 couples, up to 3.18% of parental dyads (both mothers and fathers) experienced perinatal depression, and prevalence was higher in the late postnatal period (3-12 months). There were insufficient data on parental perinatal anxiety to draw any conclusions.
Meaning
These findings suggest health care workers caring for new or expectant parents should be aware that both parents can concurrently experience perinatal mood disorders, with consequences for their health and well-being as well as that of their infant.
Abstract
Importance
New and expectant parents experience perinatal mood disorders, with consequences to parenting ability, bonding with the neonate, interpersonal relationships, and health and well-being of parents. Research shows that maternal and paternal perinatal mood disorders are associated, but no recent systematic review has addressed the prevalence of perinatal mood disorders in both mothers and fathers (parental dyad).
Objective
To examine the prevalence of perinatal mood disorders in parental dyads and identify factors associated with perinatal mood disorders in parental dyads.
Data Sources
Ovid (MEDLINE, Embase, and PsycINFO) and Web of Science were searched from January 1, 1990, to June 8, 2021, for observational studies reporting on the prevalence of perinatal depression or anxiety in a parental dyad.
Study Selection
Studies reporting the prevalence of anxiety or depression in both members of a parental dyad were included, with diagnosis according to established criteria (Diagnostic and Statistical Manual of Mental Disorders [Fifth Edition], International Classification of Diseases, 11th Revision) or use of validated screening tools.
Data Extraction and Synthesis
Prevalence data were extracted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Data were analyzed in subgroups: antenatal depression, early postnatal depression (0-12 weeks), late postnatal depression (3-12 months), and perinatal anxiety. Pooled prevalence was calculated using a random-effects meta-analysis model. Quality assessment was performed using Joanna Briggs Institute Appraisal Checklist for Studies Reporting Prevalence Data. Data were analyzed in June 2021.
Main Outcomes and Measures
Prevalence of perinatal anxiety and perinatal depression in parental dyads.
Results
Twenty-three studies were included, with data from 29 286 couples. The pooled prevalence of antenatal depression in both parents was 1.72% (95% CI, 0.96%-2.48%; P < .001). The prevalence of early postnatal depression (up to 12 weeks post partum) was 2.37% (95% CI, 1.66%-3.08%; P < .001) and the prevalence of late postnatal depression (3-12 months post partum) was 3.18% (95% CI, 2.3-4.05; P < .001). Only 3 studies reported on perinatal anxiety in both parents, precluding a quantitative analysis.
Conclusions and Relevance
In up to 3.18% of couples, both parents may concurrently experience perinatal depression. Perinatal health care must consider the mental health needs of parents, both as individuals and as a parental dyad. Further research is needed to examine outcomes in families where both parents experience perinatal mood disorders.
Introduction
Common mental disorders such as anxiety and depression are associated with morbidity for new and expectant parents. Meta-analyses of maternal depression in high-income countries estimate a prevalence of 11% during pregnancy, and 13% in the postnatal period.1 A meta-analysis of paternal depression with data from 21 countries estimated a prevalence of 9.76% during pregnancy and 8.75% during the first postnatal year.2 Prevalence of maternal anxiety varies depending on which disorders are included in the estimate but can be as high as 13%.3 Paternal perinatal anxiety is associated with maternal depression, and the odds of paternal anxiety increase by more than 3-fold when mothers are depressed.4
Psychosocial factors associated with risk for maternal perinatal mood disorders include early life stressors, limited social support, and exposure to intimate partner violence. Pregnancy-related factors, such as unintended pregnancy or somatic symptoms, such as low back pain or nausea and vomiting in pregnancy, also increase the risk of perinatal depression.1,5,6 Factors such as lower levels of education, unemployment, low social support, or marital distress increase the risk of paternal perinatal mood disorders.4,7 A history of mood disorders also increases the risk of perinatal depression or anxiety for both mothers and fathers.1,7 However, it is not currently known whether there are factors that increase the risk of perinatal mood disorders occurring concurrently in both members of the parental dyad (mothers and fathers).
Maternal and paternal mental health are associated,8 and common mental disorders may be experienced concurrently by both members of the parental dyad. Mood disorders in 1 parent may impact the other parent, and there is evidence that paternal depression leads to increased symptoms of depression in mothers during pregnancy and in the first 6 postpartum months.9 Parental perinatal mood disorders are associated with adverse pregnancy outcomes, impaired bonding with the newborn, and behavioral problems in their children.1,10,11 Co-occurrence of mood disorders in both parents may amplify these negative outcomes; however, prevalence data are lacking. This information is necessary to inform health care priority-setting and facilitate a move toward a family-centered model of care that better serves mothers and fathers as they transition to parenthood. The aims of this systematic review were to (1) examine the prevalence of perinatal mood disorders in both parents, and (2) identify factors associated with increased risk of mood disorders for both members of the parental dyad (mother and father).
Methods
The protocol was written according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.12 The study was registered in advance on PROSPERO (CRD42021252140). This systematic review was exempt from institutional review board (IRB) (ethical approval at University College London) as it involves data which are publicly available and the included articles received IRB/ethical approval.
Literature Search
A systematic search was performed on Ovid (MEDLINE, Embase, and PsycINFO) and Web of Science and completed on June 8, 2021. The search strategy combined outcome(s) of interest (depression or anxiety), population of interest (mothers and fathers), and time (perinatal or antenatal or postnatal or postpartum or antepartum or pregnancy).
Study Selection
Observational studies published in English between January 1, 1990, and June 8, 2021, were eligible for inclusion. This date range captures studies published after the Edinburgh Postnatal Depression Scale (EPDS) came into regular use. Intervention studies were not included as the narrower inclusion criteria might limit external validity.
Titles were screened, and irrelevant articles were excluded. A second reviewer screened 50% of the abstracts with 99% consensus. Disagreements were resolved by discussion. Abstracts that met the criteria were selected for full-text review. The screening, full-text review and data extraction were performed using Covidence Web-based software version 2852 (Covidence).
Participants
Studies reporting data for parental dyads (mothers and fathers) were eligible for inclusion. Studies focusing exclusively on special populations (eg, adolescent pregnancy, premature delivery, and parents experiencing a stillbirth) were excluded. These pregnancy complications likely represent differential risk for perinatal mood disorders, and inclusion of these populations would limit generalizability. Case-control studies with a clearly defined low-risk control group were eligible, provided necessary outcome data were available.
Outcome Measures
Studies reporting the incidence or prevalence of perinatal mood disorders, or providing sufficient data to permit calculation, were included. Diagnoses had to be based on clinical criteria (Diagnostic and Statistical Manual of Mental Disorders [Fifth Edition] or International Classification of Diseases, 11th Revision) or use of a validated screening questionnaire to identify those at risk (eg, EPDS). Diagnoses must have been rendered during pregnancy or in the first 12 months after childbirth, and mothers and fathers had to be assessed as a parental unit. Review articles or studies performed solely for validation of a screening tool were not included. Full inclusion and exclusion criteria can be found in eAppendix 1 in the Supplement.
Quality Assessment
Study quality was assessed using Joanna Briggs Institute Critical Appraisal for Studies Reporting Prevalence Data.13,14 This tool covers essential domains of population, measurement, and statistical approach.15 If sample size calculations were not reported, then the sample size was assessed according to whether the study was powered to detect a 15% prevalence of maternal depression within a 5% margin of error and 95% confidence. This value was chosen as it is the upper limit of prevalence reported in the literature.1 Thus, a minimum sample size of 196 couples met this criterion.
Statistical Analysis
Prevalence values of depression or anxiety in mothers, fathers, and couples were extracted. The 95% CIs were calculated for all prevalence values and these data were imported into StataMP statistical software version 16 for Mac (StataCorp) for meta-analysis. Data were analyzed in June 2021.
Outcome data were arranged in 4 subgroups: antenatal depression, early postnatal depression (up to 12 weeks [3 months] after delivery), late postnatal depression (>3-12 months after delivery), and anxiety. Postnatal depression in the year following childbirth was subdivided to reflect what is commonly considered the fourth trimester (up to 12 weeks after delivery).16 The pooled prevalence of antenatal, early postnatal, and late postnatal parental depression was calculated within a 95% CI, and a threshold of 2-sided P ≤ .05 was established as statistical significance using the metaprop test in Stata. The metaprop command incorporates a Freeman-Tukey double arsine transformation of the prevalence data. A random-effects meta-analysis model was chosen to account for diverse study designs, as it assumes that the prevalence estimate will vary across these studies. Statistical heterogeneity was estimated using the I2 statistic, which determines how much variation is because of true study differences and not because of chance. We performed a sensitivity analysis to assess whether the meta-analysis results were influenced by the exclusion of 2 outlying studies.
Results
Search Results
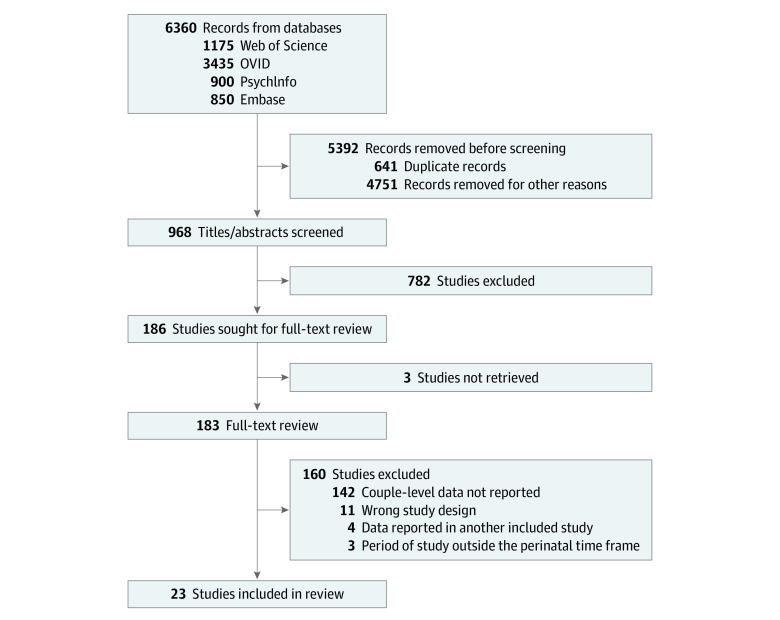
The systematic search yielded 6360 references of which 23 studies (29 286 couples) met criteria for inclusion in the review. Figure 1 displays the study flowchart of the search results. The primary reviewer (K.L.S.) screened all studies and a second reviewer screened 50% with 99% consensus between reviewers. Full-text review was performed for 183 studies (Figure 1).
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-anlyses Flow Diagram of Search Results and Review of Studies for Inclusion.
Description of Studies
Most studies were either cross-sectional or cohort studies. Six studies used data from larger cohorts at 1 or more points in time, providing cross-sectional analyses.17,18,19,20,21,22 Sample size varied from 51 couples to more than 12 000 couples.16,17,18,19,20,21,22,23,24,25
Most studies assessed postnatal depression. In 6 studies (26%), data were presented for the antenatal period.23,24,25,26,27,28 Two studies reported couple-level data for both antenatal and postnatal time points.25,27 All studies were performed in high-income countries (according to World Bank gross national income per capita criteria),29 apart from 1 that was performed in Brazil.30
All studies used validated screening tools to assess risk of mood disorders. The most common tool was the EPDS, used for both mothers and fathers in 23 studies17,18,19,20,21,22,23,24,25,26,27,28,30,31,32,33,35,36,37,38,39,40,41 (74%). Although the EPDS has been validated in many different settings, the cutoff varies, and this is reflected in the range of cutoffs used (8-13). The Center for Epidemiologic Studies Depression Scale was used in 5 studies,22,27,28,31,32 while the Beck Depression Inventory, Second Edition and General Health Questionnaire were used by 1 study.33 One study used the Kessler-6 scale, which measures nonspecific distress or mental illness.34 Studies17,18,19,20,21,22,23,24,25,26,27,28,30,31,32,33,35,36,37,38,39,40,41 were grouped according to the outcome studied and key details are listed in the Table.
Table. Studies Included in the Systematic Review.
| Variable and source (country) | Study aim(s) | Study design | Time of assessment | Couples, No. | Screening tool | Cutoff | Prevalence of depression in both parents, % |
|---|---|---|---|---|---|---|---|
| Antenatal depression | |||||||
| Raskin et al,27 1990 (US) | Describe the pattern of antenatal and postnatal depression in participants from childbirth classes | Cohort | Third trimester | 86 | CES-D | ≥16 | 4.7 |
| Escriba-Agueiret al,26 2008 (Spain) | Determine whether there are gender differences in effect of psychosocial and personal factors on depression; recruited women attending clinic during their third trimester | Cross-sectional | Third trimester | 664 | EPDS-Spanish | ≥13 (women); ≥11 (men) | 1.5 |
| Conde et al,25 2011 (Portugal) | Examine the interaction between attachment style and partner support with perinatal mood disorders among parents recruited from antenatal clinic | Cohort | Second trimester | 63 | EPDS-Portuguese | ≥10 | 3.2 |
| Della Vedova et al,24 2019 (Italy) | Examine the relationship between prenatal attachment and mood disorders among couples recruited from childbirth classes | Cross-sectional | Third trimester | 93 | EPDS-Italian | ≥10 | 0 |
| Kiepura et al,23 2020 (Poland) | Estimate the prevalence of antenatal depression and anxiety among first-time parents recruited from antenatal classes | Cross-sectional | Third trimester | 169 | EPDS | ≥12 | 1.2 |
| Mangialavori et al,28 2021 (Italy) | Examine the association between perceived stress, dyadic satisfaction, and antenatal depression among a community sample of first-time parents | Cross-sectional | Third trimester | 138 | CES-D | ≥16 | 4.37 |
| Early postnatal depression | |||||||
| Raskin et al,27 1990 (US) | Describe the pattern of antenatal and postnatal depression in participants from childbirth classes | Cohort | 8 wk post partum | 86 | CES-D | ≥16 | 4.7 |
| Ballard et al,37 1994 (UK) | Examine whether postnatal depression in couples recruited from maternity ward is higher than expected by chance | Cohort | 6 wk post partum | 178 | EPDS | ≥13 | 4.49 |
| Lane et al,36 1997 (Ireland) | Determine the correlates and variables associated with postnatal depression among a sample of women recruited in postpartum ward | Cross-sectional | 6 wk post partum | 173 | EPDS | ≥13 | 0.58 |
| Soliday et al,31 1999 (US) | Examine postnatal functioning in both parents and the outcomes associated with children’s development. Recruited from childbirth class, 10 secondary recruits | Cross-sectional | 4-6 wk post partum | 51 | CES-D | ≥17 | 19.6 |
| Pinheiro et al,30 2006 (Brazil) | Estimate the prevalence of paternal postnatal depression, and the association with maternal depression in a random sample of new parents | Cross-sectional | 6-12 wk post partum | 386 | BDI-Portuguese | ≥19 | 3.37 |
| Matthey et al,33 2000 (Australia) | Estimate the prevalence of postnatal depression in first-time parents recruited from clinic in second trimester | Cohort | 6 wk post partum | 157 | EPDS, BDI, GHQ | EPDS ≥13; BDI ≥10 (women) and ≥7 (men); GHQ ≥8 | 2.77 |
| Currò et al,39 2009 (Italy) | Determine the role of the pediatrician in detecting postnatal depression. Participants recruited by pediatricians at first well-baby visit | Cross-sectional | 2-8 wk post partum | 497 | EPDS | ≥10 (women); ≥8 (men) | 6.2 |
| Nishimura et al,32 2010 (Japan) | Determine risk factors for depression and EPDS cutoff score among fathers; mothers recruited at the postnatal check | Cross-sectional | 4-6 wk post partum | 129 | CES-D, EPDS | CES-D ≥16; EPDS ≥9 (women); ≥8 (men) |
6.2 |
| Conde et al,25 2011 (Portugal) | Examine the interaction between attachment style and partner support with perinatal mood disorders among parents recruited from antenatal clinic | Cohort | 12 wk post partum | 63 | EPDS-Portuguese | ≥10 | 1.6 |
| Kerstis et al,21 2012 (Sweden) | To determine whether parental relationship discord is associated with postpartum depression among a cohort of new parents attending child health centers | Cross-sectional analysis of cohort study | 12 wk post partum | 249 | EPDS-Swedish | ≥10 | 2.4 |
| Anding et al,35 2015 (Germany) | Determine prevalence of depressive symptoms in both parents using data from the German Midwife Prevention Study | Cross-sectional | 2 wk post partum | 276 | EPDS-German | ≥13 (women); ≥11 (men) | 2.9 |
| Kerstis et al,20 2016 (Sweden) | Describe the association between parental depressive symptoms and bonding with infant among a population-based cohort recruited from hospital | Cross-sectional analysis of cohort study | 6 wk post partum | 727 | EPDS-Swedish | ≥10 | 1.38 |
| Massoudi et al,40 2016 (Sweden) | Estimate the prevalence and correlation of maternal and paternal postnatal depression among a population-based sample of parents | Cross-sectional | 12 wk post partum | 858 | EPDS-Swedish | ≥12 | 1.5 |
| Leung et al,19 2017 (Canada) | Determine the variables associated with postnatal depression among couples using data from the APrON study | Cross-sectional analysis of cohort study | 12 wk post partum | 846 | EPDS | ≥10 (women); ≥9 (men) | 2.3 |
| Clavenna et al,41 2017 (Italy) | Determine the prevalence of parental depression among parents attending pediatric visits | Cross-sectional | 8-12 wk post partum | 1410 | EPDS-Italian | ≥13 | 0.6 |
| Nishigori et al,17 2019 (Japan) | Determine the prevalence of parental depression using data from the Japan Environment and Children’s Study | Cross-sectional | 4 wk post partum | 1023 | EPDS-Japanese | ≥9 (women), ≥8 (men) | 2.24 |
| Nakamura et al,18 2020 (France) | Examine the association between support during pregnancy and parental postnatal depression using data from the ELFE study | Cross-sectional analysis of cohort study | 8 wk post partum | 12 386 | EPDS | ≥12 (women), ≥10 (men) | 1.35 |
| Takehara et al,38 2020 (Japan) | Examine the prevalence of psychological distress in the first postnatal year using data from Comprehensive Survey of Living Conditions | Cross-sectional | 0-12 wk post partum | 734 | Kessler-6 | ≥9 | 3.4 |
| Late postnatal depression | |||||||
| Ballard et al,37 1994 (UK) | Examine whether postnatal depression in couples recruited from maternity ward is higher than expected by chance | Cohort | 6 mo post partum | 148 | CES-D | ≥16 | 4.7 |
| Paulson et al,22 2006 (US) | Determine whether postnatal depression is associated with parenting behaviors using data from early childhood longitudinal study | Cross-sectional analysis of cohort study | 9 mo post partum | 5089 | CES-D | ≥10 | 2.9 |
| Matthey et al,33 2000 (Australia) | Estimate the prevalence of postnatal depression in first-time parents recruited from clinic in second trimester | Cohort | 12 mo post partum | 146 | EPDS, BDI, GHQ | EPDS ≥13; BDI ≥10 (women) and ≥8 (men); GHQ ≥8 | 6.57 |
| Nishigori et al,17 2019 (Japan) | Determine the prevalence of parental depression using data from the Japan Environment and Children’s Study | Cross-sectional analysis of cohort study | 6 mo post partum | 1330 | EPDS-Japanese | ≥9 (women); ≥8 (men) | 2.33 |
| Takehara et al,38 2020 (Japan) | Examine the prevalence of psychological distress in the first postnatal year using data from Comprehensive Survey of Living Conditions | Cross-sectional | >3-6 mo | 872 | Kessler-6 | ≥9 | 1.8 |
| >6-9 mo | 937 | 4.5 | |||||
| >9-12 mo post partum | 971 | 3.6 | |||||
| Perinatal anxiety | |||||||
| Kiepura et al,23 2000 (Poland) | Estimate the prevalence of antenatal depression and anxiety among first-time parents recruited from antenatal classes | Cross-sectional | Third trimester | 169 | STAI | Trait ≥8; state ≥7 (STEN) | NR |
| Conde et al,25 2011 (Portugal) | Examine the interaction between attachment style and partner support with perinatal mood disorders among parents recruited from antenatal clinic | Cohort | Second trimester | 63 | STAI | ≥45 | 4.8 |
| 3 mo post partum | 3.2 | ||||||
| Della Vedova et al,24 2019 (Spain) | Examine the relationship between prenatal attachment and mood disorders among couples recruited from childbirth classes | Cross-sectional | Third trimester | 93 | EPDS-3A | ≥6 | 0 |
Abbreviations: APrON, Alberta Pregnancy Outcomes and Nutrition; BDI, Beck Depression Inventory; CES-D, Center for Epidemiologic Studies Depression Scale; ELFE, Etude Longitudinale Française depuis l'Enfance (French longitudinal study of children); EPDS, Edinburgh Postnatal Depression Scale; GHQ, General Health Questionnaire; NR, not reported; STAI, State-Trait Anxiety Inventory; STEN, standard tens score.
Quality Assessment
Most studies were judged to be of moderate quality. Participants were commonly recruited from antenatal or postnatal clinics or childbirth classes, which is appropriate as expectant or new parents are the population of interest. Most studies provided detailed inclusion and exclusion criteria, limiting participants to low-risk parents. Sample sizes were fairly small (<196 couples) in 10 studies (43%), and 1 study used secondary recruitment to increase the number of participants, potentially leading to selection bias.31 Response rates were greater than 60% in 19 of the 23 studies. Two studies had suboptimal response rates, and this was addressed in their discussion as a source of nonresponse bias.32,33 Two studies did not provide adequate information to determine response rates.17,35 See eAppendix 2 in the Supplement for full quality assessment.
Outcome Measures
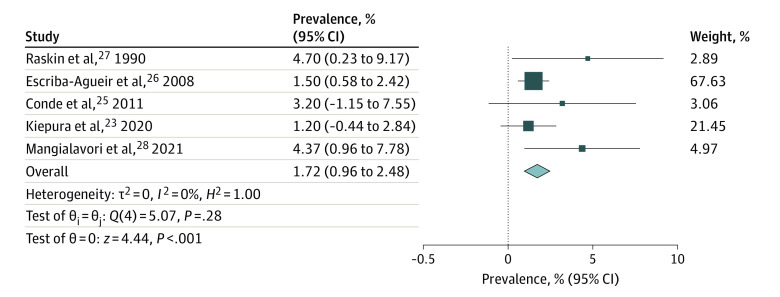
Antenatal Depression
Prevalence of antenatal depression in both members of a parental dyad ranged from 0% to 4.7%, with study sample sizes between 63 and 664 couples (Table). The study by Della Vedova et al24 was an outlier, as no men had antenatal depression according to screening with the abbreviated EPDS 3-A. Therefore, data from the 5 remaining studies (1120 couples) assessing antenatal parental depression were meta-analyzed, yielding a pooled prevalence of 1.72% (95% CI, 0.96%-2.48%; P < .001; I2 = 0%) (Figure 2).
Figure 2. Prevalence of Antenatal Depression in Parental Dyads.
Forest plot shows the pooled prevalence of antenatal depression in parental dyads according to random-effects meta-analysis. Size of boxes is a visual representation for the weight of that study in the meta-analysis. Whiskers indicate the 95% confidence interval for the prevalence in each study. The diamond indicates the pooled prevalence (%) according to the random-effects meta-analysis estimate of effect size. Diameter of the diamond reflects the 95% CI for the estimate.
Postnatal Depression
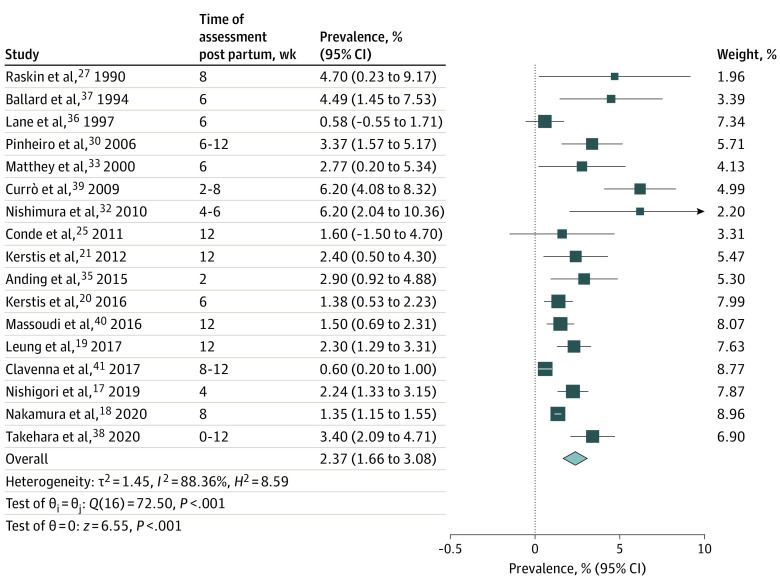
Eighteen studies examined depression in the early postnatal period (≤12 weeks after delivery). Five studies assessed parental depression in the later postnatal period (>3-12 months).
Early Postnatal Depression
Studies assessing depression up to 12 weeks post partum provided data from 20 229 couples. Point prevalence for early postnatal depression in both parents varied from 0.58% to 19.6%. Lane et al36 assessed postnatal depression both at 3 days and 6 weeks post partum. Mild mood changes in the first 2 weeks post partum can be common in women and are usually due to hormonal changes; therefore, measurements at 6 weeks post partum were used for the analysis. Soliday et al31 used the CES-D to assess depression in 51 couples 4 to 6 weeks after childbirth. Almost 20% of couples met criteria for postnatal depression. This prevalence was far higher than values reported by other studies and was subject to selection bias as the authors used secondary recruitment for 10 couples. This study was, therefore, excluded from the meta-analysis. Random-effects meta-analysis of the remaining 17 studies (20 178 couples) yielded a pooled prevalence of 2.37% (95% CI, 1.66%-3.08%; P < .001; I2 = 88.36%) for early postnatal depression in parental dyads (Figure 3).
Figure 3. Prevalence of Early Postnatal Depression in Parental Dyads.
Forest plot shows the pooled prevalence of early postnatal depression (0-12 weeks after childbirth) in parental dyads according to random-effects meta-analysis. Size of boxes is a visual representation for the weight of that study in the meta-analysis. Whiskers indicate the 95% confidence interval for the prevalence in each study. The diamond indicates the pooled prevalence (%) according to the random-effects meta-analysis estimate of effect size. Diameter of the diamond reflects the 95% CI for the estimate.
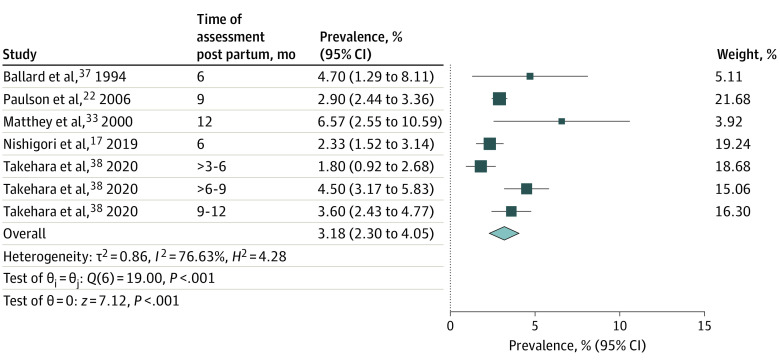
Late Postnatal Depression
Five studies assessed parental depression in the late postnatal period (>3-12 months). This represents data from 9493 couples, and point prevalence values ranged from 1.8% to 4.7%.17,22,33,37,38 Random-effects meta-analysis yielded a pooled prevalence of 3.18% (95% CI, 2.3-4.05; P < .001; I2 = 76.63) for late postnatal depression in parental dyads (Figure 4).
Figure 4. Prevalence of Late Postnatal Depression in Parental Dyads.
Forest plot shows the pooled prevalence of late postnatal depression (3-12 months after childbirth) in parental dyads according to random-effects meta-analysis. Size of boxes is a visual representation for the weight of that study in the meta-analysis. Whiskers indicate the 95% confidence interval for the prevalence in each study. The diamond indicates the pooled prevalence (%) according to the random-effects meta-analysis estimate of effect size. Diameter of the diamond reflects the 95% CI for the estimate.
Anxiety
Three studies addressed parental perinatal anxiety, recruiting a low-risk group of mostly first-time parents from antenatal clinics or childbirth classes. Conde et al25 evaluated anxiety among Portuguese parents using the State-Trait Anxiety Inventory self-report scale, and rates of perinatal anxiety were high for both mothers (19%) and fathers (7.9%-11%). Kiepura et al23 also used the State-Trait Anxiety Inventory, and almost 10% of men and 7.7% of women met criteria for elevated state anxiety. However, in the study by Della Vedova et al,24 no men met criteria for perinatal anxiety. In contrast, a recent meta-analysis estimated the prevalence of perinatal paternal anxiety to be 10.69% (95% CI, 8.14%-13.91%).42 Further research is needed to determine the prevalence of parental perinatal anxiety, and to identify the ideal screening tool for use in this population.
Related Factors
The association between mood disorders in both parents and other covariates was not uniformly assessed in included studies, precluding statistical analysis. A narrative summary is presented here. In 3 studies,17,19,30 maternal antenatal depression was associated with increased risk of postnatal depression in both members of the parental dyad. Socioeconomic factors, such as unemployment, longer paternal working hours, and low income, were also associated with depression in couples.35,37,38 Relationship issues, such as low marital satisfaction, frequent quarrels, or perceived low support, were associated with mood symptoms in both parents.21,26
Sensitivity Analyses
Two studies were excluded from the primary analysis as they were significant outliers (Della Vedova et al24 and Soliday et al31). A sensitivity analysis including these 2 studies did not significantly change the results of the primary meta-analysis (see eFigure 1 and eFigure 2 in the Supplement for primary and secondary analyses for antenatal depression, respectively; see eFigure 3 and eFigure 4 in the Supplement for primary and secondary analyses for early postnatal depression, respectively ). Subgroup analyses were performed to determine potential contributors to heterogeneity. The depression screening tool varied among studies, with a majority using the EPDS. Subgroup analysis demonstrated a difference in the prevalence of postnatal depression between studies that used the EPDS and those that did not (2.22% [95% CI, 1.5-2.95] vs 3.26% [95% CI, 2.56-3.96]; P = .04) (eFigure 5 in the Supplement).
Discussion
The pooled prevalence of antenatal depression in parental dyads (mothers and fathers) was 1.72%. This estimate is limited by the small number of studies. Previous studies demonstrate that parents experiencing depression during pregnancy are more likely to experience postnatal depression. According to longitudinal cohort data, the odds of postnatal depression (measured by EPDS score) have been shown to increase by more than 3-fold for women with antenatal depression.19 This association was even more striking among men, with an odds ratio of 9.11 (95% CI, 5.40-15.4; P < .001).19 These findings underscore the need to address antenatal depression in new and expectant parents. However, the limited data on antenatal mood disorders within the parental dyad suggests that future research in this area is needed.
The prevalence of early postnatal depression (0-12 weeks after delivery) in both parents was estimated to be 2.37%. In high-income countries such as the US and the UK, more than 80% of women and more than 70% of men become parents.43,44,45,46 Therefore, with prevalence rates of 2% to 3% for depression in both members of the parental dyad, the potential burden of disease is considerable.
Perinatal depression can follow a protracted course; most men and women who have depressive symptoms at 4 and 8 weeks post partum continue to have symptoms at 6 months post partum, and some develop symptoms in the later postnatal period.9 In this review, the pooled prevalence of parental depression was higher in the later postnatal period (>3-12 months) (3.18% vs 2.37%), although the 95% CIs overlapped. Future research should determine the longitudinal course of perinatal mood disorders coexisting in both parents, which may change clinical practice. The clinical focus on postnatal depression usually centers on the first 12 weeks post partum, reflected in practice guidelines.47 However, our findings suggest that clinical attention to perinatal mood disorders may need to extend beyond the early postnatal period.
Related Factors
This review assessed parental perinatal mood disorders in low-risk pregnancies. Complications in pregnancy such as stillbirth, preterm labor, or HIV are likely factors associated with risk for perinatal mood disorders. However, the impact of pregnancy complications on the prevalence of mood disorders in both parents was beyond the scope of this review.
Factors such as low relationship satisfaction and socioeconomic hardship were associated with higher prevalence of mood disorders in parental dyads.21,26,35,37,38 This highlights the need to consider health and well-being in a wider context. Focusing on the social determinants of health as well as the relationship between expectant parents may identify couples at risk for perinatal mood disorders. Future research should examine factors associated with increased risk for mood disorders in a parental dyad, and whether they differ from factors associated with risk for isolated maternal or paternal mood disorders.
Potential Impacts
According to the results of this review, both members of the parental dyad experience perinatal mood disorders in up to 3 out of 100 couples. This has consequences for the individual’s health and well-being, their ability to parent their child, as well as the mental and physical health of their children.1,10 Parental perinatal mood disorders also increase relationship discord and risk of separation.48
There is evidence that a healthy father-child relationship can mitigate against poorer child outcomes in cases of maternal depression.49,50 In cases of paternal depression, a healthy mother-child relationship will likely offer similar protection.51 However, when both parents are depressed, this buffering effect is lost, further increasing the risk for poor mental and physical health outcomes for their child. Awareness of the coexistence of common mental health disorders in both members of a parental dyad allows for a paradigm shift in the provision of perinatal care. In the UK, there is usually a single postnatal visit for mothers during the first 6 to 8 weeks after childbirth.47 However, review of electronic health records suggests that up to 40% of new mothers may not have this consultation,52 and fathers are seldom included. Perhaps it is time to rethink the current model of postnatal care and move toward a holistic model of care that better supports both parents during the antenatal period and extends beyond the early perinatal period.
Limitations
This study had limitations. Although we sought to investigate both anxiety and depression, there were limited data available on perinatal anxiety in both mothers and fathers. Anxiety and depression often coexist in the general population, with up to 67% of patients with major depression meeting criteria for an anxiety disorder.53 A recent meta-analysis reported the prevalence of maternal comorbid anxiety and depression to be 9.5% during pregnancy and 8.2% in the first 6 months post partum.54 Paternal perinatal anxiety rates are higher than in the general population (10.69% vs 3.8%).42 This illustrates the need for future research on anxiety in parental dyads during the transition to parenthood.
There were data from 15 different countries, improving the generalizability, particularly to other high-income countries. However, the inclusion of studies from several different countries using a range of screening tools contributes to the observed heterogeneity. A random-effects meta-analysis was adopted to account for the between-study heterogeneity55; however, this model gives a higher weight to smaller studies, possibly limiting the validity of the results obtained. Smaller sample size also means that those study estimates are less precise.
Most of the studies used cross-sectional data, limiting the analysis of covariates that may be associated with the prevalence of perinatal parental mood disorders. Although several studies excluded patients with a history of mental health problems, this was not done uniformly. Thus, it is impossible to identify true incident cases. Although some studies followed a cohort of patients, there were insufficient data to comment on the course of perinatal mood disorders for the parental dyad. To understand the trajectory of perinatal depression in the parental dyad, longitudinal data following large cohorts will be required.
Most studies were conducted in high-income countries; therefore, the findings may not apply to low- or middle-income countries. Given that rates of maternal depression and anxiety are higher in low- or middle-income countries than high-income countries,1,56 further research should address the prevalence of mood disorders in parental dyads in this context. Additionally, the systematic search did not yield any studies that examined perinatal mood disorders in both parents outside of a heteronormative context. Future research should consider the full spectrum of family-building.
Conclusions
This review found that both mothers and fathers experienced depression in up to 3% of couples. Given the presence of substantial heterogeneity, conclusions are tentative. Further research should examine the coexistence of mood disorders in new or expectant parents, and the ideal screening tool, particularly for new or expectant fathers.
eAppendix 1. Inclusion and Exclusion Criteria
eAppendix 2. Quality Assessment Using Joanna Briggs Institute Criteria for Prevalence Studies
eFigure 1. Forest Plot of Prevalence of Parental Antenatal Depression (Primary Analysis)
eFigure 2. Forest Plot of Prevalence of Parental Antenatal Depression (Secondary Analysis)
eFigure 3. Forest Plot of Prevalence of Early Postnatal Depression (Primary Analysis)
eFigure 4. Forest Plot of Prevalence of Early Parental Postnatal Depression (Secondary Analysis)
eFigure 5. Subgroup Analyses Based on Time of Postpartum Assessment and Depression Screening Tool Used
References
- 1.Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384:1775-1788. doi: 10.1016/S0140-6736(14)61276-9 [DOI] [PubMed] [Google Scholar]
- 2.Rao WW, Zhu XM, Zong QQ, et al. Prevalence of prenatal and postpartum depression in fathers: a comprehensive meta-analysis of observational surveys. J Affect Disord. 2020;263:491-499. doi: 10.1016/j.jad.2019.10.030 [DOI] [PubMed] [Google Scholar]
- 3.Viswasam K, Eslick GD, Starcevic V. Prevalence, onset and course of anxiety disorders during pregnancy: a systematic review and meta analysis. J Affect Disord. 2019;255:27-40. doi: 10.1016/j.jad.2019.05.016 [DOI] [PubMed] [Google Scholar]
- 4.Chhabra J, McDermott B, Li W. Risk factors for paternal perinatal depression and anxiety: a systematic review and meta-analysis. Psychol Men Masc. 2020;21(4):593.-611. doi: 10.1037/men0000259 [DOI] [Google Scholar]
- 5.Muchanga SMJ, Eitoku M, Mbelambela EP, et al. Association between nausea and vomiting of pregnancy and postpartum depression: the Japan Environment and Children’s Study. J Psychosom Obstet Gyneacol. 2022;43(1):2-10. doi: 10.1080/0167482X.2020.1734792 [DOI] [PubMed] [Google Scholar]
- 6.Long G, Yao ZY, Na Y, Ping Y, Wei S, Mingsheng T. Different types of low back pain in relation to pre- and post-natal maternal depressive symptoms. BMC Pregnancy Childbirth. 2020;20(1):551. doi: 10.1186/s12884-020-03139-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Psouni E, Agebjörn J, Linder H. Symptoms of depression in Swedish fathers in the postnatal period and development of a screening tool. Scand J Psychol. 2017;58(6):485-496. doi: 10.1111/sjop.12396 [DOI] [PubMed] [Google Scholar]
- 8.Thiel F, Pittelkow MM, Wittchen HU, Garthus-Niegel S. The relationship between paternal and maternal depression during the perinatal period: a systematic review and meta-analysis. Front Psychiatry. 2020;11:563287. doi: 10.3389/fpsyt.2020.563287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paulson JF, Bazemore SD, Goodman JH, Leiferman JA. The course and interrelationship of maternal and paternal perinatal depression. Arch Womens Ment Health. 2016;19(4):655-663. doi: 10.1007/s00737-016-0598-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramchandani PG, O’Connor TG, Evans J, Heron J, Murray L, Stein A. The effects of pre- and postnatal depression in fathers: a natural experiment comparing the effects of exposure to depression on offspring. J Child Psychol Psychiatry. 2008;49(10):1069-1078. doi: 10.1111/j.1469-7610.2008.02000.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johannsen BMW, Larsen JT, Laursen TM, Bergink V, Meltzer-Brody S, Munk-Olsen T. All-cause mortality in women with severe postpartum psychiatric disorders. Am J Psychiatry. 2016;173(6):635-642. doi: 10.1176/appi.ajp.2015.14121510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123-128. doi: 10.15171/ijhpm.2014.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C.. Chapter 5: systematic reviews of prevalence and incidence. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis. JBI; 2020. [Google Scholar]
- 15.Migliavaca CB, Stein C, Colpani V, Munn Z, Falavigna M; Prevalence Estimates Reviews–Systematic Review Methodology Group (PERSyst) . Quality assessment of prevalence studies: a systematic review. J Clin Epidemiol. 2020;127:59-68. doi: 10.1016/j.jclinepi.2020.06.039 [DOI] [PubMed] [Google Scholar]
- 16.American College of Obstetricians and Gynecologists . Optimizing postpartum care. May 2018. Accessed April 5, 2022. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/05/optimizing-postpartum-care?utm_source=redirect&utm_medium=web&utm_campaign=otn
- 17.Nishigori H, Obara T, Nishigori T, et al. ; Miyagi Regional Center of Japan Environment & Children’s Study Group . The prevalence and risk factors for postpartum depression symptoms of fathers at one and 6 months postpartum: an adjunct study of the Japan Environment & Children’s Study. J Matern Fetal Neonatal Med. 2020;33(16):2797-2804. doi: 10.1080/14767058.2018.1560415 [DOI] [PubMed] [Google Scholar]
- 18.Nakamura A, Sutter-Dallay AL, El-Khoury Lesueur F, et al. Informal and formal social support during pregnancy and joint maternal and paternal postnatal depression: data from the French representative ELFE cohort study. Int J Soc Psychiatry. 2020;66(5):431-441. doi: 10.1177/0020764020911409 [DOI] [PubMed] [Google Scholar]
- 19.Leung BMY, Letourneau NL, Giesbrecht GF, Ntanda H, Hart M; APrON Team . Predictors of postpartum depression in partnered mothers and fathers from a longitudinal cohort. Community Ment Health J. 2017;53(4):420-431. doi: 10.1007/s10597-016-0060-0 [DOI] [PubMed] [Google Scholar]
- 20.Kerstis B, Aarts C, Tillman C, et al. Association between parental depressive symptoms and impaired bonding with the infant. Arch Womens Ment Health. 2016;19(1):87-94. doi: 10.1007/s00737-015-0522-3 [DOI] [PubMed] [Google Scholar]
- 21.Kerstis B, Engström G, Sundquist K, Widarsson M, Rosenblad A. The association between perceived relationship discord at childbirth and parental postpartum depressive symptoms: a comparison of mothers and fathers in Sweden. Ups J Med Sci. 2012;117(4):430-438. doi: 10.3109/03009734.2012.684805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics. 2006;118(2):659-668. doi: 10.1542/peds.2005-2948 [DOI] [PubMed] [Google Scholar]
- 23.Kiepura E, Kmita G. Antenatal depression and anxiety in primiparous Polish mothers and fathers. Ginekol Pol. 2020;91(1):24-28. doi: 10.5603/GP.2020.0006 [DOI] [PubMed] [Google Scholar]
- 24.della Vedova AM, Cristini C, Bizzi F. Prenatal attachment, distress symptoms and psychosocial variables in a sample of Italian first-time parents. Life Span Disabil. 2019;22(2):255-285. [Google Scholar]
- 25.Conde A, Figueiredo B, Bifulco A. Attachment style and psychological adjustment in couples. Attach Hum Dev. 2011;13(3):271-291. doi: 10.1080/14616734.2011.562417 [DOI] [PubMed] [Google Scholar]
- 26.Escribè-Agüir V, Gonzalez-Galarzo MC, Barona-Vilar C, Artazcoz L. Factors related to depression during pregnancy: are there gender differences? J Epidemiol Community Health. 2008;62(5):410-414. doi: 10.1136/jech.2007.063016 [DOI] [PubMed] [Google Scholar]
- 27.Raskin VD, Richman JA, Gaines C. Patterns of depressive symptoms in expectant and new parents. Am J Psychiatry. 1990;147(5):658-660. doi: 10.1176/ajp.147.5.658 [DOI] [PubMed] [Google Scholar]
- 28.Mangialavori S, Cacioppo M, Terrone G, O’Hara MW. A dyadic approach to stress and prenatal depression in first-time parents: the mediating role of marital satisfaction. Stress Health. 2021;37(4):755-765. doi: 10.1002/smi.3036 [DOI] [PubMed] [Google Scholar]
- 29.The World Bank . GNI per capita, Atlas method (current US$). Accessed August 16, 2021. https://data.worldbank.org/indicator/NY.GNP.PCAP.CD
- 30.Pinheiro RT, Magalhães PVS, Horta BL, Pinheiro KAT, da Silva RA, Pinto RH. Is paternal postpartum depression associated with maternal postpartum depression? population-based study in Brazil. Acta Psychiatr Scand. 2006;113(3):230-232. doi: 10.1111/j.1600-0447.2005.00708.x [DOI] [PubMed] [Google Scholar]
- 31.Soliday E, McCluskey-Fawcett K, O’Brien M. Postpartum affect and depressive symptoms in mothers and fathers. Am J Orthopsychiatry. 1999;69(1):30-38. doi: 10.1037/h0080379 [DOI] [PubMed] [Google Scholar]
- 32.Nishimura A, Ohashi K. Risk factors of paternal depression in the early postnatal period in Japan. Nurs Health Sci. 2010;12(2):170-176. doi: 10.1111/j.1442-2018.2010.00513.x [DOI] [PubMed] [Google Scholar]
- 33.Matthey S, Barnett B, Ungerer J, Waters B. Paternal and maternal depressed mood during the transition to parenthood. J Affect Disord. 2000;60(2):75-85. doi: 10.1016/S0165-0327(99)00159-7 [DOI] [PubMed] [Google Scholar]
- 34.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 35.Anding JE, Röhrle B, Grieshop M, Schücking B, Christiansen H. Couple comorbidity and correlates of postnatal depressive symptoms in mothers and fathers in the first two weeks following delivery. J Affect Disord. 2016;190:300-309. doi: 10.1016/j.jad.2015.10.033 [DOI] [PubMed] [Google Scholar]
- 36.Lane A, Keville R, Morris M, Kinsella A, Turner M, Barry S. Postnatal depression and elation among mothers and their partners: prevalence and predictors. Br J Psychiatry. 1997;171:550-555. doi: 10.1192/bjp.171.6.550 [DOI] [PubMed] [Google Scholar]
- 37.Ballard CG, Davis R, Cullen PC, Mohan RN, Dean C. Prevalence of postnatal psychiatric morbidity in mothers and fathers. Br J Psychiatry. 1994;164(6):782-788. doi: 10.1192/bjp.164.6.782 [DOI] [PubMed] [Google Scholar]
- 38.Takehara K, Suto M, Kato T. Parental psychological distress in the postnatal period in Japan: a population-based analysis of a national cross-sectional survey. Sci Rep. 2020;10(1):13700. doi: 10.1038/s41598-020-70727-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Currò V, De Rosa E, Maulucci S, et al. The use of Edinburgh Postnatal Depression Scale to identify postnatal depression symptoms at well child visit. Ital J Pediatr. 2009;35(1):32. doi: 10.1186/1824-7288-35-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Massoudi P, Hwang CP, Wickberg B. Fathers’ depressive symptoms in the postnatal period: prevalence and correlates in a population-based Swedish study. Scand J Public Health. 2016;44(7):688-694. doi: 10.1177/1403494816661652 [DOI] [PubMed] [Google Scholar]
- 41.Clavenna A, Seletti E, Cartabia M, et al. ; Postnatal Depression Study Group . Postnatal depression screening in a paediatric primary care setting in Italy. BMC Psychiatry. 2017;17(1):42. doi: 10.1186/s12888-017-1205-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leiferman JA, Farewell CV, Jewell J, et al. Anxiety among fathers during the prenatal and postpartum period: a meta-analysis. J Psychosom Obstet Gynaecol. 2021;42(2):152-161. doi: 10.1080/0167482X.2021.1885025 [DOI] [PubMed] [Google Scholar]
- 43.Monte LM, Knop B. Men’s fertility and fatherhood: 2014. June 13, 2019. Accessed August 17, 2021. https://www.census.gov/library/publications/2019/demo/p70-162.html
- 44.Livingston G. Childlessness. Pew Research Center . May 7, 2015. Accessed August 16, 2021. https://www.pewresearch.org/social-trends/2015/05/07/childlessness/
- 45.Office for National Statistics . Childbearing for women born in different years, England and Wales: 2019. December 4, 2020. Accessed August 16, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/conceptionandfertilityrates/bulletins/childbearingforwomenbornindifferentyearsenglandandwales/2019
- 46.Office for National Statistics . Births in England and Wales. July 22, 2020. Accessed November 22, 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/livebirths/bulletins/birthsummarytablesenglandandwales/2019
- 47.National Institute for Health and Care Excellence . Postnatal care. April 20, 2021. Accessed September 13, 2021. https://www.nice.org.uk/guidance/ng194/chapter/Recommendations#organisation-and-delivery-of-postnatal-care
- 48.Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. Centre for Mental Health . October, 20 2014. Accessed August 20, 2021. https://www.centreformentalhealth.org.uk/publications/costs-perinatal-mental-health-problems
- 49.Vänskä M, Punamäki RL, Lindblom J, et al. Parental pre-and postpartum mental health predicts child mental health and development. Fam Relat. 2017;66(3):497-511. doi: 10.1111/fare.12260 [DOI] [Google Scholar]
- 50.Brennan PA, Hammen C, Katz AR, Le Brocque RM. Maternal depression, paternal psychopathology, and adolescent diagnostic outcomes. J Consult Clin Psychol. 2002;70(5):1075-1085. doi: 10.1037/0022-006X.70.5.1075 [DOI] [PubMed] [Google Scholar]
- 51.Letourneau N, Leung B, Ntanda H, Dewey D, Deane AJ, Giesbrecht GF; APrON Team . Maternal and paternal perinatal depressive symptoms associate with 2- and 3-year-old children’s behaviour: findings from the APrON longitudinal study. BMC Pediatr. 2019;19(1):435. doi: 10.1186/s12887-019-1775-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smith HC, Saxena S, Petersen I. Postnatal checks and primary care consultations in the year following childbirth: an observational cohort study of 309 573 women in the UK, 2006-2016. BMJ Open. 2020;10(11):e036835. doi: 10.1136/bmjopen-2020-036835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Choi KW, Kim YK, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment. In: Kim YK, ed. Advances in Experimental Medicine and Biology. Vol 1191. Springer; 2020:219-235, doi: 10.1007/978-981-32-9705-0_14 [DOI] [PubMed] [Google Scholar]
- 54.Falah-Hassani K, Shiri R, Dennis CL. The prevalence of antenatal and postnatal co-morbid anxiety and depression: a meta-analysis. Psychol Med. 2017;47(12):2041-2053. doi: 10.1017/S0033291717000617 [DOI] [PubMed] [Google Scholar]
- 55.Schroll JB, Moustgaard R, Gøtzsche PC. Dealing with substantial heterogeneity in Cochrane reviews: cross-sectional study. BMC Med Res Methodol. 2011;11:22. doi: 10.1186/1471-2288-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gelaye B, Rondon MB, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973-982. doi: 10.1016/S2215-0366(16)30284-X [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Inclusion and Exclusion Criteria
eAppendix 2. Quality Assessment Using Joanna Briggs Institute Criteria for Prevalence Studies
eFigure 1. Forest Plot of Prevalence of Parental Antenatal Depression (Primary Analysis)
eFigure 2. Forest Plot of Prevalence of Parental Antenatal Depression (Secondary Analysis)
eFigure 3. Forest Plot of Prevalence of Early Postnatal Depression (Primary Analysis)
eFigure 4. Forest Plot of Prevalence of Early Parental Postnatal Depression (Secondary Analysis)
eFigure 5. Subgroup Analyses Based on Time of Postpartum Assessment and Depression Screening Tool Used