Abstract
Background:
Fuchs heterochromic iridocyclitis is a chronic, unilateral iridocyclitis characterized by iris heterochromia. The gradual progression of the disease leads to the development of cataracts, glaucoma, and, occasionally, vitreous infiltration. The trigger for inflammation of the iris and ciliary body is still unknown. There are several as yet unconfirmed theories about the mechanism of occurrence, including Toxoplasma gondii infection, immune dysfunction, infiltration of sensitized lymphocytes, and chronic herpes virus infection.
Objective:
The aim of this article is to present a case of Fuchs heterochromic iridocyclitis with complications in form of glaucoma and dense cataract in a female patient during a standard ophthalmologic exam in our clinic. The next aim is to show a proper algorithm of treatment in form of carbonic anhydrase inhibitors antiglaucoma medication, cataract surgery with implantation of the intraocular lens, yag laser capsulothomy.
Case report:
A 55-year-old patient reports to our clinic for an examination. She was informed 7 years ago by her ophthalmologist that her lack of vision in the right eye is irreparable. Ophthalmological examination as well as a positive TORCH test (elevation of IgG for toxoplasma gondii) lead to a diagnosis of Fuchs heterochromic iridocyclitis with complications of glaucoma and dense cataract. Antiglaucoma drops are prescribed, PHACO surgery is performed on the right eye with implantation of the intraocular lens, and yag laser capsulotomy in the follow ups. There was a significant improvement of the visual acuity from light sensation with uncertain projection of the same on the right eye, to 0,5-0,6 Snellen scale. We also educated the patient of her disease as well as the importance of her treatment and follow up consultations.
Conclusion:
Due to the insidious nature of this condition, along with a mild chronic course, most patients with FHI are not aware of the subtle changes that occur in their eyes. One of the most serious complications of FHI is secondary glaucoma, which can cause permanent vision loss in patients. The main cause of poor vision in patients with FHI is caused by cataract formation, with a prevalence of 23% to 90.7%. We placed special emphasis on educating the patient about her condition and the long-term and importance of regular check-ups to prevent possible recurrent or new complications.
Keywords: Fuchs heterochromic iridocyclitis, secondary glaucoma, phacoemulsification, yag laser capsulotomy
1. BACKGROUND
Fuchs iridocyclitis is a chronic, unilateral iridocyclitis characterized by iris heterochromia. It was first described in 1906 (1, 2). Fuchs believed that an unknown process leads to the development of abnormal uveal pigment with milder chronic inflammation, and ultimately causes iris atrophy and secondary glaucoma. Irodocyclitis usually occurs in younger adults with light-colored eyes with minimal symptoms and is usually present without pain or redness of the outer parts of the eye or miosis. The distribution of the disease is the same in both sexes (3). The gradual progression of the disease leads to the development of cataracts, glaucoma, and, occasionally, vitreous infiltration. Although it usually occurs as a unilateral disease, 7.8% -10% of patients have a bilateral form of the disease (2). The trigger for inflammation of the iris and ciliary body is still unknown. There are several as yet unconfirmed theories about the mechanism of occurrence, including Toxoplasma gondii infection, immune dysfunction, infiltration of sensitized lymphocytes, and chronic herpes virus infection (5–8).
Figure 1. and Figure 2. Biomicroscopic view of the anterior chamber of the right eye: clearly visible corneal precipitates as well as gradual lens clouding.

Infectious causes leading to FHI have been extensively studied. Both FHI and ocular toxoplasmosis have well-defined clinical features and unambiguous diagnoses can often be made. A strong association between FHI and ocular toxoplasmosis has been documented. T gondii has been suggested as a possible etiological agent. In Brazil and France, 60% of patients with FHI have been reported to have lesions of the chorioretina consistent with toxoplasmosis (5). The rubella virus, which is well known to cause German measles, is thought to be involved in the pathogenesis of FHI. Exact molecular mechanisms remain a research topic, but the clinical spectrum of rubella uveitis resembles Fuchs’ heterochromic uveitis (FHU) in many respects (9).
2. OBJECTIVE
The aim of this article is to present a case of Fuchs heterochromic iridocyclitis with complications in the form of glaucoma and dense cataract in a female patient during a standard ophthalmologic exam in our clinic. The examination included visual acuity exam, tonometry, biomicroscopic exam, fundoscopy, TORCH laboratory findings. The next aim is to show a proper algorithm of treatment in the form of carbonic anhydrase inhibitors, antiglaucoma drops, cataract surgery with implantation of the intraocular lens, yag laser capsulotomy.
3. METHODS
All medical reports are shown in this article. Every diagnostic tool as well as report is a part from our archived history of the patient and has been thoroughly analysed. We also reviewed available literature using the key words fuchs heterochromic iridocyclitis, secondary glaucoma, phacoemulsification, complicated cataract surgery.
4. CASE REPORT
A 55-year-old patient reports to our clinic for an optical correction. She explained that her ophthalmologist informed her 7 years ago that “she will never see with her right eye” and that the condition is irreparable. Visual acuity at first examination in the right eye was light sensation with uncertain projection of the same, on the left 0.8-0.9 sc. Further examination of the anterior segment of the right eye reveals diffuse precipitates on the cornea, especially noticeable in the Artls triangle, blue iris, slightly shallow anterior chamber without pathological content and gradual clouding of the lens, synechiae are not observed; left eye with brown iris and initial sclerosis of the lens. By applanation tonometry, values of 23 mmHg / 20 mmHg are obtained with a pachymetry correction factor of 2.4 on both eyes. Gonioscopic examination: angle open, medium width, neat pigmentation on both sides, Schaffer IV; Schei I.
Due to the degree of clouding of the lens, it is not possible to perform an adequate examination of the fundus of the right eye, examination of the fundus of the left eye: PNO clearly limited, retinal level, C / D 0.6, macular area with insufficient foveal reflex, blood vessels discreetly narrowed. An ultrasound examination of the right eye is performed where opacities of the corpus vitreum are found.
We diagnosed the patient with Fuchs’ heterochromic iridocyclitis, and explained that the lack of vision in the right eye was not irreparable. Additional diagnostics are proposed in the form of TORCH laboratory findings, with results of extremely elevated IgG antibodies to Toxoplasma, which correlates with anamnestic data that the patient lived in a house with three cats as a teenager, one of whom always slept with her in bed. On the day of the examination, a carbonic anhydrase inhibitor is prescribed as antiglaucoma therapy, and the patient is explained that this is a long-term and chronic therapy, and educated of the importance of regular and constant use of the same.
Figure 3. Operational course of phacoemulsification with the installation of an intraocular lens:a–paracentesis to allow adequate access to the natural lens, b–methylene blue staining to better visualization of the anterior capsule, c – capsulorhexis, d + e–process of phacoemulsification of natural lenses, f–condition after phacoemulsification and remnant removal of the epicortex, g–installation of intraocular lens with positioning of the same, h + i application of antibiotics and air bubble in the anterior chamber.
Figure 4. Biomicroscopic view of the anterior chamber of the right eye on the first day after surgical cataract treatment: discrete centropupillary keratitis, air bubble present, medium wide pupil, PCIOL neatly positioned.
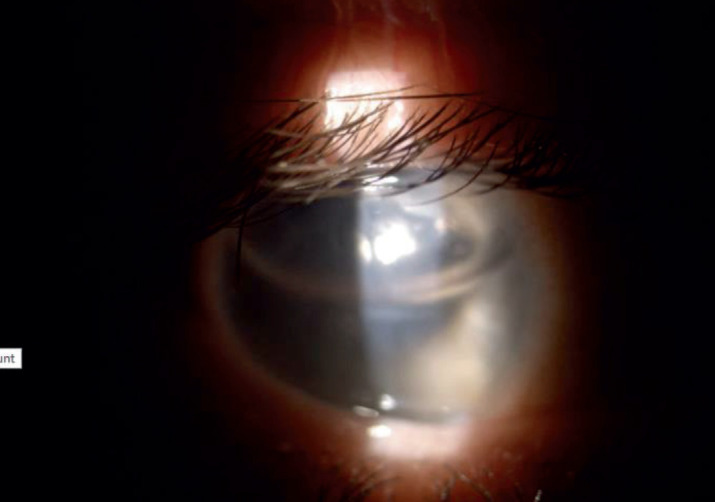
Figure 5. Biomicroscopic view of the anterior chamber after yag laser capsulotomy of the right eye.

Laser trabeculoplasty is not indicated due to a possible additional inflammatory response. For the next step in the treatment algorithm, the decision was made to operate on the cataract of the right eye with the implantation of an intraocular lens.
The operative course is going smoothly, the patient is discharged home the same day. On the first follow up on the day after the cataract operation discrete keratitis is observed centropupillary, which responds positively to the corticosteroid subconjunctival treatment, the patient’s visual acuity from previous VOD: L + P +/- increases to VOD: 0.7 without correction 20 days after cataract surgery.
The patient comes for regular check-ups, primarily to monitor the diagnosed glaucoma caused by FHI – we perform OCTs of the optic disk, macula, and visual field testing. 14 months after the operation, the patient underwent a yag laser capsulotomy of the right eye due to the present opacification of the posterior capsule.
The patient is scheduled for a follow-up examination after yag laser capsulotomy where VOD: 0.5-0.6 sc, VOS: 0.9 TOD: 15 mmmHg TOS: 17 mmHg with antiglaucoma therapy in the form of carbonic anhydrase inhibitors.
5. DISCUSSION
Fuchs’ heterochromic iridocyclitis is a chronic, typically unilateral anterior uveitis. The exact etiology of the occurrence is unknown. When first described, Fuchs had many theories about what caused this unique pathology; however, over the years, many of them have been largely refuted, and contagious theory remains one of the more likely causes. The demographics of the patient population vary according to incidence, age of onset of symptoms, and complication rates depending on the subpopulation being studied. Most patients experience vision changes mainly due to secondary complications, such as cataracts and glaucoma. Treatment of these complications leads to a good prognosis (10).
Fuchs’ heterochromic iridocyclitis usually occurs in the third to fourth decades of life. Due to the insidious nature of this condition, along with a mild chronic course, most patients will not be aware of the subtle changes that occur in their eyes. Patients are usually asymptomatic, and most diagnoses of FUS are detected during routine eye examinations. Discoloration of the iris of the affected eye is the most common complaint of patients. Another relevant finding in the patient’s medical history will consist of a decrease in visual acuity primarily caused by cataract formation. Some patients may also experience symptoms of elevated intraocular pressure (IOP) such as blurred vision, mild pain, and the appearance of an areola in front of the eye (5).
One of the most serious complications of FHI is secondary glaucoma, which can cause permanent vision loss in patients. Secondary glaucoma has a prevalence of 15-59%. When topical therapy is not sufficient, surgery is required, primarily trabeculectomy surgery.
The main cause of poor vision in patients with Fuchs heterochromic iridocyclitis is caused by cataract formation, with a prevalence of 23% to 90.7% (11). Both clinical and visual patient outcomes are good with different types of cataract extraction strategies consisting of phacoemulsification presented in this paper and small incision cataract surgery. Both surgical techniques provide lower rates of postoperative and intraoperative complications compared to extracapsular cataract extraction (12).
6. CONCLUSION
We presented the case of a 55-year-old patient with Fuchs heterochromic iridocyclitis with pre-existing complications of the disease in the form of secondary glaucoma and dense cataract, as well as the treatment of the complications–adequate antiglaucoma therapy and phacoemulsification with intraocular lens implantation. We placed special emphasis on educating the patient about her condition and the long-term and importance of regular check-ups to prevent possible recurrent or new complications.
Author’s contribution:
All authors were involved in all steps of preparationthis article. Final proofreading was made by the first author.
Conflict of Interest:
There are no conflicts of interest.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Mohamed Q, Zamir E. Update on Fuchs’ uveitis syndrome. Curr Opin Ophthalmol. 2005 Dec;16(6):356–363. doi: 10.1097/01.icu.0000187056.29563.8d. [DOI] [PubMed] [Google Scholar]
- 2.Moshirfar M, Villarreal A, Ronquillo Y. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Jul 25, Fuchs Uveitis Syndrome. 2022 Jan. [PubMed] [Google Scholar]
- 3.Whitcup MS. 5th. Elsevier; 2021. Uveitis – fundamentals and clinical practice. [DOI] [Google Scholar]
- 4.Becker-Shaffer’s Diagnosis and Therapy of the Glaucomas. 8th 2009.
- 5. [March 10th, 2022]. Available at: [DOI]
- 6.Jad A, Céline T, Bahram B, Phuc L, Nathalie C. Fuchs’ heterochromic cyclitis: a post-infectious manifestation of ocular toxoplasmosis? Int Ophthalmol. 2013 Apr;33(2):189–94. doi: 10.1007/s10792-012-9649-7. [DOI] [PubMed] [Google Scholar]
- 7.Chee SP, Jap A. Presumed fuchs heterochromic iridocyclitis and Posner-Schlossman syndrome: comparison of cytomegalovirus-positive and negative eyes. Am J Ophthalmol. 2008 Dec;146(6):883–889.e1. doi: 10.1016/j.ajo.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 8.Jurkunas UV, Bitar M, Rawe I. Colocalization of increased transforming growth factor-beta-induced protein (TGFBIp) and Clusterin in Fuchs endothelial corneal dystrophy. Invest Ophthalmol Vis Sci. 2009 Mar;50(3):1129–1136. doi: 10.1167/iovs.08-2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Gelder RN. Idiopathic no more: clues to the pathogenesis of Fuchs heterochromic iridocyclitis and glaucomatocyclitic crisis. Am J Ophthalmol. 2008 May;145(5):769–771. doi: 10.1016/j.ajo.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 10.de Visser L, Braakenburg A, Rothova A, de Boer JH. Rubella virus-associated uveitis: clinical manifestations and visual prognosis. Am J Ophthalmol. 2008 Aug;146(2):292–297. doi: 10.1016/j.ajo.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 11.Roque Manolette R. Fuchs Heterochromic Iridocyclitis (Fuchs Heterochromic Uveitis) 2020. Mar 03, https://emedicine.medscape.com/article/1208706-overview#a2 .
- 12.Al-Mansour YS, Al-Rajhi AA, Al-Dhibi H, Abu El-Asrar AM. Clinical features and prognostic factors in Fuchs’ uveitis. Int Ophthalmol. 2010 Oct;30(5):501–509. doi: 10.1007/s10792-010-9379-7. [DOI] [PubMed] [Google Scholar]
- 13.Sun YJiY. A literature review on Fuchs uveitis syndrome: An update. Surv Ophthalmol. 2020 Mar-Apr;65(2):133–143. doi: 10.1016/j.survophthal.2019.10.003. [DOI] [PubMed] [Google Scholar]



