Abstract
Cutaneous fungal infections are common in humans and are associated with significant physical and psychological distress to patients. Although conventional topical and/or oral anti-fungal medications are commonly recommended treatments, drug resistance has emerged as a significant concern in this patient population, and safer, more efficacious, and cost-effective alternatives are warranted. Recent studies have reported effectiveness of photodynamic therapy (PDT) against fungal infections without severe adverse effects. In this review, we briefly discuss the mechanisms underlying PDT, current progress, adverse effects, and limitations of this treatment in the management of superficial and deep fungal infections.
Keywords: photodynamic therapy, fungal infection, review
Introduction
Cutaneous fungal infections are categorized as superficial and deep infections and are associated with significant physical and psychological distress to patients. Conventional therapy may be ineffective, particularly for deep fungal infections. Furthermore, antifungal agents may cause severe adverse effects, such as liver toxicity, drug interactions, and drug resistance.1 Some superficial fungal infections, such as tinea pedis and cruris are recommended treatment continued for two weeks, post clinical cure for topical agents, and recalcitrant cases usually need continued systemic therapy to eliminate pathogens,2 which is known to reduce patient compliance and remains therapeutically challenging in clinical practice.
Reportedly, photodynamic therapy (PDT) is effective against fungal infections and serves as an alternative treatment strategy. PDT was originally discovered in 1900 and was used for its anti-microbial action; however, this treatment is gradually being accepted as an anti-fungal treatment option since the 1980s.3
The rapid onset of action, mild adverse effects, combinations with other therapies, and applicability in patients with contraindications to other drugs or in those with unresponsiveness to oral antifungal agents serve as advantages of PDT. Little to no risk of development of resistance and its repeatability are other advantages of this treatment. Currently, PDT is widely used to treat many cutaneous fungal infections, such as onychomycosis, tinea capitis, pityriasis versicolor (PV), oral candidiasis, vulvovaginal candidiasis (VVC), chromoblastomycosis (CBM) and cutaneous sporotrichosis, among others, of which onychomycosis is the focus of most research. PDT is a potentially promising therapeutic alternative for treatment of cutaneous fungal infections.
In this review, we discuss the published mechanisms underlying PDT, in addition to representative research on PDT in superficial and deep skin mycoses, and summarize the reported efficacy and limitations of this therapy for the management of fungal infections.
Mechanisms Underlying the Effects of Photodynamic Therapy
PDT involves the use of the following three elements: a photosensitizer (PS), a light source, and molecular oxygen.1 The PS frequently used in clinical practice include 5-aminolevulinic acid (5-ALA), methylamino levulinate (MAL), and methylene blue (MB). Light sources include red, green, and blue light, and lasers, among others. The mechanism underlying PDT effects is as follows: the PS absorbs energy under the action of light, changes its energy state, and reacts with oxygen molecules to generate reactive oxygen species (ROS), which selectively injure the infected or proliferative tissue.
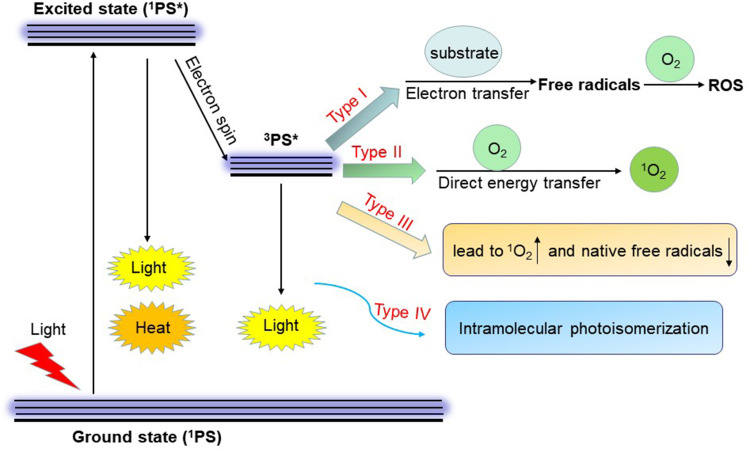
PS produce their effects via the following mechanisms: A Type I reaction involves an interaction between the PS and the substrate, which generates free radicals, including hydroxyl radicals, hydrogen peroxide, and a superoxide anion that reacts with oxygen molecules to generate ROS, which cause fungal apoptosis.4 A Type II reaction involves direct transfer of energy from the PS to oxygen to form singlet oxygen (1O2), a potent ROS,5 which initiates cell injury (Figure 1).6
Figure 1.
Mechanisms of action of photodynamic therapy. Following light absorption, excited state 3PS* reacts with O2 to produce ROS and 1O2 (type I and II reactions). Type III PSs combine properties leading to the generation of 1O2 and reduction of native free radicals in target cells. Type IV mechanism involves a structural change from excited state 1PS* by photoisomerization to enable molecular target binding of the activated PS* to its cellular target site. (* represents the excited state).
Abbreviations: PS, photosensitizer; 1PS, singlet photosensitizer; 3PS, triplet photosensitizer; ROS, reactive oxygen species; 1O2, singlet oxygen; O2, oxygen.
Type III and IV reactions have also been described in the literature.7,8 These reactions are cytotoxic to intracellular structures in the absence of oxygen. Type III PSs are usually classified as antioxidant carrier sensitizers (ACS), which result in the generation of efficient 1O2 and reduce the concentration of native free radicals in target cells. A Type IV reaction involves binding of a PS to its cellular target site after the activation of light excitation. Among the aforementioned mechanisms underlying PDT effects, Type I and II are indirect reactions, whereas Type III and IV reactions lead to direct activation of the PS molecule, which produces secondary reactions independent of interactions with oxygen (Figure 1).
ROS are key participants in phototoxic reactions. Some in vitro experiments have shown the possible mechanisms contributing to the growth-inhibiting effect of PDT, including destruction of biofilm formation and fungal cell wall structure secondary to enhanced ROS production.5,9,10 PDT produces oxidative damage to cellular structures and DNA, causes structural modifications in the plasma membrane, and inhibits enzymatic systems.11 Studies have reported that PDT-mediated therapy directly destroys microorganisms and also promotes neutrophil and lymphocyte infiltration at the affected sites to augment its fungicidal effect.12,13
Role of Photodynamic Therapy in Superficial Fungal Infections
Onychomycosis
Onychomycosis is one of the most common superficial fungal infections encountered in clinical practice, with a relapse rate of 25%–30%.14 It is caused by dermatophytes, yeasts, and non-dermatophyte molds (NDMs).15 The most common etiological pathogen is Trichophyton rubrum, one of the dermatophytes.16 Many topical and oral agents cannot penetrate the nail plate and are not absorbed owing to the insufficient blood supply to the nail plate, which is invariably thickened in a diseased state.14 Currently, PDT is a promising strategy to enhance nail penetration. A systemic review showed that PDT led to negative results on microscopy and/or culture studies in 67% of patients (N = 58) who received this treatment.17 PDT combined with other physical therapies, such as lasers results in good penetration of the nail plate. A clinical trial (n=7) in which PDT with combined with carbon dioxide (CO2) laser to treat recurrent onychomycosis reported a mycological cure rate of 100%.18 Some in vitro experiments and mouse models have shown that PDT could disrupt bacterial and fungal biofilms,19–22 such as Pseudomonas aeruginosa, Staphylococcus aureus, and Candida strains biofilms, which refers to a freely suspended microbial community that provides protection against host defenses.17 Theoretically, the anti-biofilm action of PDT can prevent recurrent onychomycosis.
Various PSs are used for PDT; however, these may show different levels of antifungal effects. Reportedly, nail penetration of MB is better than that of ALA, and MB is therefore associated with higher complete cure rates.1,23,24 MB usually does not require pre-treatment except in patients with nail hyperkeratosis measuring at least 2 mm, who require nail microabrasion.25 In contrast, ALA requires pre-treatment and prolonged exposure because the ALA molecule is required to undergo enzymatic conversion into a protoporphyrin for pre-use activation.25 Furthermore, high water solubility and absorption bands in the red spectrum are important features that determine selection of PS for the treatment of onychomycosis.26
New-generation PSs wrapped in nanoemulsions are shown to have good effectiveness and a high safety profile.27 A clinical trial using aluminum-phthalocyanine chloride with nanoparticles reported photoactivation for treatment of deeper nail layers.28 Two other studies have shown that light-induced gold nanoparticles could inhibit spore germination and achieve high complete cure rates.29,30 Nanoemulsions may serve as an excellent delivery system for PS and enhance penetration of aqueous tunnels created by pre-treatment using urea solution.28 Newer PS may possess intrinsically good nail penetration capacity, which may reduce incubation time, obviate the need for pre-treatment, and also be effective under low-oxygen conditions.31
Evidence from many in vitro studies supports the role of PDT as a potential therapeutic alternative for Trichophyton rubrum infection. Rose Bengal and Citrus aurantifolia essential oil (Citrus EO) PS activated by light are shown to reduce the growth of T. rubrum.32,33 Citrus EO is activated by sunlight, and no special light source is required. Sylsens B was shown to be an effective PS to prevent T. rubrum microconidia germination.26 Although these in vitro studies have shown promising results, no clinical trials have corroborated these findings. Further in vivo studies are required to verify the fungicidal effects of these agents (Table 1).
Table 1.
Overview of the Treatment Regimen, Outcome, and Side Effects for PDT Treatment of Fungal Infections Articles Cited in This Review
| References | Study Type | Case Number | Fungal Species | PS | Light Source | Light Wavelength (nm) | Light Dose (J/cm2) | Treating Sessions (Interval Time) | Combination Treatment | Outcome | Follow Up | Adverse Effects |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Onychomycosis | ||||||||||||
| de Oliveira GB et al18 | Clinical trial | 7 |
T. rubrum (n=6); Epidermophyton floccosum (n=1) |
16% MAL | LED | NA | NA | 2 sessions (60-day intervals) | Fractional CO2 laser 10.600 nm | 1-year follow-up: MC 100%; ClC 79% (15/19) (nail four quadrants count) 43% (entire nail plate) No relapse. |
30 days; 1 year |
NA |
| Morgado LF et al28 | Clinical trial | 20 included (16 finished) |
NA | AlClPc (entrapped in nanoemulsions) | LED (red light) | 660 | 30.9 | 4.45±1.76 sessions (15-days interval) | No | MC 40% ClC 60% |
1 month | Pain (VAS 2.76±1.87) |
| Tawfik AA et al29 | In vivo experience (rabbit) | 80 | T. mentagrophytes | 3 groups: MB; Gold nanoparticles; MB + gold nanoparticles |
LED (red and green light) | Red (650); Green (530) |
80; 100 |
4 sessions (48-hours intervals) | No | CC: MB 40%; Gold nanoparticles 96%; MB + gold nanoparticles 34% |
48 hours after the 4th session | NA |
| Cronin L et al32 | In vitro study | Spore suspension (A300=0.6) | T. rubrum | Rose Bengal | Laser (green) | 532 | 68; 133; 228 | NA | No | Percentage growth inhibition 15–51% | NA | NA |
| Fekrazad R et al33 | In vitro study | Suspensions (106 cells/ mL) | C.albicans; T.rubrum | Citrus EO; Indocyanine green |
Infrared (IR) laser; Natural and tungsten lights | 810±10 (IR laser) | 55 (IR laser) | NA | No | Cell reduction rates: Citrus EO + natural and tungsten light: 99.99% (C.albicans and T.rubrum); Indocyanine green + IR laser: 91.67% (C.albicans) 74.5% (T.rubrum); Fluconazole + IR laser: 38.5% (T.rubrum) |
NA | NA |
| Smijs TG et al26 | In vitro study | Suspension and spore solution | T. rubrum | Sylsens B; DP mme |
Red light | 600 | 108 | NA | No | Inhibition rates: Suspension cultures: Sylsens B (10μM-50μM): 100% DP mme (30μM): 95%; Microconidia: Sylsens B (1–5μM): 100% DP mme (4–5μM): 80–90% |
2 days; 7 days; 3 months |
NA |
| Tinea pedis (interdigital type) | ||||||||||||
| Sotiriou E et al35 | Clinical trial | 10 |
T. rubrum (n=4); T. mentagrophytes (n=6) |
20% 5-ALA | Red light | 570–670 | 50 | 1 or 3 sessions (2-week intervals) | No | CC after 3 treatments: 60% (6/10) CC at the end of follow-up: 30% (3/10) |
2 months | Burning sensation during irradiation, erythema up to 1 week after therapy. |
| Calzavara-Pinton PG et al36 | Clinical trial | 9 |
T. mentagrophytes (n=4); T. rubrum (n=2); C. albicans (n=3) |
20% 5-ALA | Broadband red light | 575–700 | 75 | 1 or 4 sessions (1-week interval) | No | CC after 1 or 4 treatments: 67% (6/9) CC at the end of follow-up: 22% (2/9) |
4 weeks | Localized erythema and edema during and soon after exposure; pain; desquamation after 3–5 days. |
| Tinea cruris | ||||||||||||
| Sotiriou E et al40 | Clinical trial | 10 | T. rubrum | 20% 5-aminolevulinic acid (ALA) | Red light | 570–670 | 50 | 1–2 sessions (2-week intervals) | No | MC after 1–2 treatments: 80% (8/10) MC at the end of follow-up: 40% (4/10) |
8 weeks | Mild burning and stinging during the exposure; erythema and edema up to 3–4 days after therapy. |
| Tinea Capitis | ||||||||||||
| Lu J et al42 | Case report | 1 | NA | 20% 5- ALA | LED | 630 | 80 | 3 sessions (1-week interval) | Itraconazole 100 mg/day | CC 1/1 No recurrence. |
3 months | Burning sensation during irradiation; temporary edema, erythema, itch, and stinging up to 1 week after therapy. |
| Pityriasis versicolor (PV) | ||||||||||||
| Alberdi E et al43 | Pilot trial | 5 | Malassezia spp. | 2% MB | Red LED lamp | 630±5 | 37 | 6 sessions (2-week intervals) | No | CC: 5/5 No relapse. |
4 weeks; 22 weeks |
Hypopigmentation, no other side effects or pain. |
| Oral candidiasis | ||||||||||||
| Freire F et al47 | In vitro study; in vivo study in a murine model |
107 CFU/mL of suspension (OD570); 15 BALB/c mice |
C. albicans | Methylene blue (MB); new methylene blue (NMB) |
Red diode laser | 660 | 10; 20; 40; 60 J |
5 days of daily treatment | Potassium iodide (KI) | Log reduction of CFU/mL: MB+KI (40 J): 2.31 log NMB (60 J): 1.77 log Reduction of mice bioluminescent photon flux (log10): MB+KI (40J): 2 log NMB (60 J): 1 log |
NA | NA |
| Campos L et al48 | Case report | 1 | Candida spp. | 0.01% MB | Laser | 660 | 178 | 1 session | No | ClC: 1/1 | 72 hours | NA |
| Chibebe JJ et al49 | In vivo experiment in Galleria mellonella model | 16/group |
C. albicans Can14 (wild-type); Can37 (fluconazole-resistant) |
MB (1 mM) | Red light | 660±15 | 0.9 | 1 time | Fluconazole (14 mg/kg) | Can14: MB-PDT prolonged suivival. Can37: MB-PDT reduced fungal burden by 0.2 log; MB-PDT+fluconazole prolonged suivival. |
100 hours - 150 hours | NA |
| Esophageal candidiasis (EC) | ||||||||||||
| Qiu H et al51 | Clinical study | 2 | Candida spp. | Photocarcinorin (PSD-007) | Semiconductor laser | 630 | 135; 270 | 1–3 sessions (1-month and 6-month intervals) | No | Case 1: CC 2/2 EC lesions Case 2: CC 1/1 EC lesions No recurrence in two cases. |
14 months; 24 months |
Substernal pain within 5–7 days after PDT. (both cases) A low-grade fever lasted for 5 days post PDT. (case 1) |
| Vulvovaginal candidiasis (VVC) | ||||||||||||
| de Santi M et al55 | In vivo study in a murine model | 37 | C. albicans | MB (100 μM); PpNetNI (10 μM) |
Laser (MB); LED (PpNetNI) |
660 nm (laser); 630 nm (LED) |
6048 (laser); 85 (LED) |
1 time | No | Reduction of fungal CFUs: 1 order of magnitude (both PSs) |
7 days | No |
| Machado-de-Sena RM et al56 | In vivo study in a murine model | 77 | C. albicans | MB (1 mM) | Red laser | 660 | 18 J; 36 J | 1 or 2 sessions (24-hour intervals) | No | Reduction of fungal CFUs: 1session: 1.62 log (after 24 h) 1.16 log (after 96 h); 2 sessions: 1.66 log (after 24 h) |
24 hours; 96 hours |
NA |
| Chromoblastomycosis (CBM) | ||||||||||||
| Hu Y et al58 | Case report; in vitro study |
1 case; 0.5–2.5×103 conidia/mL (in vitro) |
F. monophora | 20% 5-ALA | LED | 635 | 10 J | Case: 2 sessions (each including 9 times, 1-week interval) |
Case: Terbinafine (250 mg/day) In vitro study: No combination. |
Case: Mycological cure and clinical greatly improvement. In vitro study: Reduce fungal CFUs by 2–4 log. |
Case: 1 year; In vitro study: 7 days |
Hypopigmentation |
| Lyon JP et al59 | In vitro study | Suspension of 1–5×106 CFU/mL | F. pedrosoi; Cladophialophora carrionii | MB (16 μg/mL; 32 μg/mL; 64 μg/mL) | LED | NA | 200 mW/cm2 | 1 time | No | Reduction of fungal CFUs: 4 log approximately (32 μg/mL achieved better result) | 7–10 days | NA |
| Huang X et al60 | In vivo study in Galleria mellonella model | No specific description | F. monophora | 5- ALA | Laser (red light) | NA | NA | 1 session | No | Extend median survival by 2.5 days. Increase hemocyte density by 1.34×103 cells/μL 4h after PDT. |
10 days | No |
| Hu Y et al9 | Case series; in vitro study |
5 cases; Suspension: 0.5–2.5×103 conidia/mL |
F. nubica (n=1); F. pedrosoi (n=2); F. monophora (n=2) |
20% 5- ALA | LED (white light) | 635 | 36.8 mW/cm2 (10 J) | Cases: 4–9 sessions (1- or 2-week intervals) |
Cases: Oral itraconazole 400 mg/day; oral terbinafine 250 mg/day In vitro study: Itraconazole 1μg/mL |
Cases: MC: 3/5 CC: 2/5 Clinical improvement: 3/5 No new lesions. In vitro study: Reduced approximately 2×103 CFUs of F. monophora. |
Cases:6 months - 2 years | Hypopigmentation (n=2) |
| Yang W et al61 | Case report | 1 | F. monophora | 20% 5-ALA | LED (red light) | 630 | 90 | 3 sessions (10-day intervals) | Itraconazole 400 mg/day | CC: 1/1 No relapse. |
3 months | Pain and burning sensation during irradiation; Mild pain, swelling, and exudation whining 3–5 days after PDT. |
| Huang X et al62 | Case report | 1 | F. pedrosoi | 10% ALA | Red light | 633±10 | 80–100 mW/cm2 | 6 sessions (1-week interval) | No | CC: 1/1 No recurrence. |
6 months | NA |
| Lan Y et al63 | Case report | 1 | F. monophora | 20% ALA | Red light | 633±10 | 96 | 4 sessions (1-week interval) | Isotretinoin 20 mg/day; Oral terbinafine 250 mg/day, itraconazole 400 mg/day; CO2 laser. |
MC: 1/1 Clinical improvement. |
4 months | No |
| Sporotrichosis | ||||||||||||
| Gilaberte Y et al66 | Case report and in vitro study | 1 case; Suspension optical density McFarland values 0.5. |
Sporothrix schenkii | Case:1% MB; In vitro study: MAL (0–6 M); MB (1 μM); NMB (1.25 μM); DMMB (1.5 μM) |
LED | 635 nm (case); 639.8±10 nm (in vitro study) |
37 | Case: 3 and 5 sessions (2-week intervals) |
No | Case: Clinical improvement; In vitro study: Reduce fungal cells by 6 log10 CFUs (MB, NMB, DMMB), No change of CFU (MAL). |
NA | Pain during irradiation (score 4 on a VAS) |
| Phaeohyphomycosis | ||||||||||||
| Liu H et al68 | Case report | 1 | Exophiala spinifera | 20% ALA | Red light | 633 | 120 mW/cm2 | 3 sessions (1-week interval) | Oral terbinafine 250 mg/day, itraconazole 200 mg/day | MC: 1/1 Clinical improved greatly. |
3 months | Mild burning and temporary pain during irradiation; hyperpigmentation. |
| Majocchi’s granuloma (MG) | ||||||||||||
| Shi L et al12 | Case report; in vitro study; in vivo study in guinea pig model |
1 case; In vitro study: suspension 1–5×105 CFU/mL |
T. tonsurans | Case: 10% ALA; In vitro study: 5 mM ALA; In vivo study: 10% ALA |
LED | Case: 635 In vitro and in vivo study: 633 |
Case:120; In vitro study: 50, 100, 150, 175, 200; In vivo study: 90. |
Case: 3 sessions (3- or 4-week intervals) | No | Case: CC 1/1; no recurrence. In vitro study: Reduced approximately 4×105 CFU/mL of fungal concentrations. (175 and 200 J/cm2) In vivo study: Reduced the clinical lesions scoring by 6. |
Case: 3 months; In vitro study: 7 days; In vivo study: 14 days |
Case: Inflammatory exudation after 1st PDT. In vivo study: Erythema and exudation 24–48 hours after PDT. Scabs formed on the 8th day. |
| Mucormycosis | ||||||||||||
| Liu Z et al11 | In vitro study | 6 strains; Conidia concentra- tion of 1–3×106 CFU/mL |
R. oryzae | MB (8, 16, and 32 μg/mL) | LED | 635±10 | 12 | 1 time | No | CFU reductions: 1.1 log10 (8 μg/mL MB); 2.2 log10 (16 μg/mL MB); 4.3 log10 (32 μg/mL MB). |
24 hours | NA |
Abbreviations: PS, photosensitizer; PDT, photodynamic therapy; ALA, aminolevulinic acid; MAL, methyl aminolevulinate; MB, methylene blue; NMB, new methylene blue; DMMB, 1.9-dimethylmethylene blue; DP mme, deuteroporphyrin monomethylester; Citrus EO, citrus aurantifolia essential oil; AlClPc, aluminium-phthalocyanine chloride; PpNetNI, Protoporphyrin IX; LED, Light-Emitting Diode; CO2, carbon dioxide; MC, mycological cure; ClC, clinical cure; CC, complete cure; CFU, colony forming unit; VAS, visual analogue scale; NA, not available; T., Trichophyton; C., Candida; F., Foncecaea; R., Rhizopus.
Tinea Pedis
Tinea pedis is a common fungal skin infection; topical antifungal medications remain the mainstay of treatment, and oral antifungal drugs are considered in cases of infection that remain refractory to local therapy.34 Tinea pedis is a chronic and contagious condition with reservoir effect; therefore, long-term treatment (over >4 weeks) is recommended in recalcitrant cases.2 PDT was attempted for the management of tinea pedis to overcome the limitations of long-term drug therapy. However, this approach was not more effective than conventional therapies. Two clinical studies investigated ALA-PDT for the treatment of interdigital tinea pedis, the most common type of mycotic infection of the feet.35,36 In the two studies, complete cure rates were obtained at 30% and 22% at follow-up. ALA-PDT treatment of interdigital tinea pedis showed lower response rates than conventional topical allylamines (naftifine and terbinafine) therapy with mycological cure rates of 62%–100% and clinical cure rates of 66%–86%.37 It may be attributable to the fact that PDT treatment administered to irregular surfaces may result in light-blind areas, which may serve as a source of re-infection (Table 1).
Tinea Cruris
Tinea cruris is a fungal infection of the groin, buttocks, and perineal and perianal skin. Reportedly, cure rates range from 80% to 90% following accurate diagnosis and optimal therapy.38 However, an alarming trend of recalcitrant tinea cruris is being observed, with reduced treatment compliance in patients.39 PDT has been attempted to overcome this concern; however, long-term outcomes were not favorable.
In a clinical trial that included 10 patients with tinea cruris caused by Trichophyton, the author administered 20% 5-ALA-PDT (570–670 nm wavelengths) at a light dose of 50 J/cm2 for 4 hours/ session. Direct microscopy performed after 1–2 sessions showed negative results in 8 patients (80%). However, only 4 patients (40%) showed sustained healing at 8-week follow-up.40 Recurrence rates were as high as 50% in this study, which suggests that PDT may not be adequately effective for the eradication of fungi. The unsatisfactory therapeutic response to PDT may be attributed to high humidity and temperature in the groin, which affect the cellular uptake of ALA (Table 1).
Tinea Capitis
Tinea capitis is one of the most common fungal infections observed in pre-pubertal children.41 Oral antifungal medications are considered standard therapy for tinea capitis; however, the increasing prevalence of resistant strains and adverse events limit the use of conventional antifungal treatment. Lu et al42 reported a case of relapsed suppurative tinea capitis in a child who showed mycological and clinical cure after ALA-PDT plus itraconazole treatment administered over three sessions. Treatment included topical application of 20% 5-ALA and an occlusive dressing for 3 hours, followed by irradiation using a light-emitting diode (LED) light (630 nm, 80 J/cm2) for 20 min/session. The authors observed that PDT destroyed metabolically active cells in addition to resistant forms such as conidia. PDT may serve as a useful adjunct for the treatment of refractory tinea capitis (Table 1).
Pityriasis Versicolor
Pityriasis versicolor (PV) is a chronic recurrent fungal infection of the stratum corneum. Although guidelines recommend systemic therapy for PV, this chronic condition is characterized by refractoriness to treatment. MB and MAL are common PSs used for the treatment of PV because the hydrophilicity of MB limits it to the stratum corneum, and the lipophilicity of MAL, restrains lipophilic Malassezia.1,43 Alberdi et al43 used MB-PDT (2% MB and a red LED lamp [λ= 630±5 nm, 37 J/cm2]) to treat 5 women with disseminated PV on the back. MB-PDT administered over six sessions with a 2-week interval between sessions led to complete cure and good cosmetic outcomes without recurrence at the 6-month follow-up. The authors also recommended MB-PDT as a potential prophylactic treatment owing to its cost-effective and highly selective features (Table 1).
Oral Candidiasis
Oral candidiasis is a common opportunistic fungal infection typically observed in immunocompromised patients. Infection control is extremely important in these patients to avoid serious and often fatal outcomes. Candida albicans is the most common pathogen that causes oral candidiasis. Compared with its planktonic form, the biofilm-forming species is more pathogenic and necessitates a higher concentration of PS and a longer incubation period.44–46 A study performed by Freire et al, which included biofilm growth in vitro and in a mouse model showed the efficacy of new methylene blue (NMB)-mediated PDT against C. albicans.47 Both the survival fraction analysis (log reduction of colony forming units (CFU/mL)) of C. albicans and histopathological examination showed eradication of fungi. The authors also observed that potassium iodide (KI) potentiated MB-PDT, which may be secondary to the fact that KI provides a greater number of electrons to MB to initiate a Type I photochemical reaction.
A case report and an in vivo experiment in the Galleria mellonella model have described that MB-PDT could rapidly heal oral lesions caused by drug-resistant C. albicans strains and reduce the fungal burden by 0.2 log in the animal model.48,49 However, the role of PDT in the prevention of drug resistance remains unclear.
In addition to oral lesions, C. albicans causes esophageal candidiasis (EC), particularly in immunocompromised hosts such as in patients with cancer, AIDS, diabetes, or a glucocorticoid-dependent state.50 Qiu et al51 successfully treated EC and controlled the progression of esophageal cancer using photocarcinorin-mediated PDT. Photocarcinorin (PSD-007), a mixed porphyrin preparation, is used as a PS; however, the mechanism of photo-oxidative injury remains unknown (Table 1).
Vulvovaginal Candidiasis
Vulvovaginal candidiasis (VVC) affects approximately 75% of women of child-bearing age; C. albicans is the main pathogen associated with this infection.52 The azole family of drugs is widely used against Candida infection; however, these drugs block the activity of some essential enzymes and lead to adverse effects.53 The etiological agents implicated in VVC, including C. albicans and C. glabrata may be resistant to antifungal agents, including fluconazole.54 PDT represents a novel therapeutic adjuvant without deleterious effects.
A study performed by de Santi et al reported the use of MB- and protoporphyrin IX (PpNetNI)-mediated PDT to treat VVC in a mouse model.55 The authors observed reductions of one order of magnitude in the CFUs of C. albicans after 7-day treatment without any adverse effects on the vaginal mucosa at the ultrastructural level. In addition to its fungicidal effect, PDT reduced edema and abscess formation, which provided adequate time for the host immune system to eradicate the fungi.55
Machado-de-Sena et al observed reduction in the fungal burden and inflammation in a murine model of VVC within 24 hours of completion of MB-PDT (Table 1).56 However, fungal recolonization occurred 96 hours after PDT because this organism is a commensal that colonizes the healthy human mucosa. The authors speculated that MB-PDT may inhibit the formation of germ tubes, which contribute significantly the virulence of C. albicans. Additionally, PDT minimizes the harmful effects of toxins on the vaginal mucosa and is therefore a safe therapeutic choice.56
Photodynamic Therapy for Subcutaneous or Deep Fungal Infections
Chromoblastomycosis
Chromoblastomycosis (CBM), a chronic granulomatous subcutaneous fungal infection caused by dematiaceous fungi is associated with low cure and high relapse rates.9 Fonsecaea monophora, Fonsecaea pedrosoi, and Cladophialophora carrionii are the most common fungal species associated with CBM. Notably, fibrosis is a major obstacle to successful oral antifungal management. Owing to diverse clinical manifestations and etiological agents, the optimal therapy for CBM remains uncertain. PDT has emerged as a promising physical approach to treating CBM, particularly in the early stages of the disease.57
Two in vitro experiments have shown that ALA-PDT and MB-PDT significantly decreased fungal CFUs in CBM by 2–4 and 4 orders of magnitude, respectively.58,59 Clinical trials have reported that muriform cells pose a therapeutic challenge; following tissue invasion, fungi are transformed into muriform cells, which aid with immune system evasion and antifungal drug resistance. PDT may directly destroy muriform cells or stimulate the host immune response. An in vivo experiment in the Galleria mellonella model confirmed the antimicrobial effect of ALA-PDT via immunomodulation of innate immunity secondary to increased hemocyte density, cell morphological transformation, and pathogen sensitivity.60
Combination therapy including PDT and systemic antifungal drugs is preferred in clinical practice, because most patients present for evaluation with moderate or severe disease. There are some successful clinical practices for PDT in patients with complex CBM using ALA-PDT associated with itraconazole or terbinafine.9,58,61 A sequential PDT protocol after failed drug therapy showed fungicidal effects similar to those observed with combination therapy.62 In patients with CBM post PDT treatments, most lesions showed clear improvement, and mycological examination results were negative after the last therapy session, with a few pigmentary changes but no new lesions on long-term follow-up.9
In addition to the combination of two methods, comprehensive treatment using several methods may be beneficial. Lan et al63 reported that PDT combined with oral antifungal agents, isotretinoin, and CO2 laser showed antifungal activity against clinical CBM (Table 1). The CO2 laser slightly injures the skin surface and thereby promotes penetration of the PS; such comprehensive management produces synergistic inhibitory effects.
Moreover, in vitro susceptibility tests may not accurately predict clinical response. A study has reported that several isolates of pathogenic strains from patients were sensitive to oral antifungal drugs but showed resistance in vivo.9 The overall patient status, phenotypic changes, differential gene regulation, and biofilm formation by dermatophytes may affect treatment efficacy.64 Therefore, clinical trials that determine the response rate of specific fungi to PDT are urgently needed.
Sporotrichosis
Sporotrichosis, a fungal infection caused by the Sporothrix schenckii complex, a thermally dimorphic species, is often restricted to cutaneous, subcutaneous tissue, and lymphatic vessels.65 Oral itraconazole is commonly used for treatment of sporotrichosis; however, drug-induced hepatotoxicity remains a serious concern. PDT is an effective alternative for localized fungal infections without severe adverse effects.
Gilaberte et al66 reported complete microbiological and clinical cures in a patient with recalcitrant cutaneous sporotrichosis, who received intralesional 1% MB-PDT combined with intermittent low-dose itraconazole. The authors also performed an in vitro photoinactivation test on the fungus isolated from the patient and observed that three phenothiazinium PSs (MB, NMB, and 1.9-dimethyl methylene blue) produced a 6 log10 fungicidal effect, whereas MAL did not inhibit fungal growth, even at high concentrations (6 M). This result was consistent with the clinical outcomes observed in the patient (Table 1). Reportedly, the S. schenckii complex produces melanoid pigments that absorb light and scavenge ROS to limit the efficacy of PDT.67 The fungicidal efficacy of MB-PDT specifically against S. schenckii complex may be attributed to the method of administration, low optical interference, and high ROS production.66
Phaeohyphomycosis
Phaeohyphomycosis is a fungal infection that includes a wide spectrum of infections of the epidermis and subcutaneous tissues in addition to systemic involvement. It is caused by melanized fungi, and no standard antifungal therapy is currently available for this infection. Liu et al68 reported the use of ALA-PDT as adjuvant therapy combined with oral itraconazole and terbinafine to treat an elderly immunocompromised woman with phaeohyphomycosis caused by Exophiala spinifera. The authors used 20% 5-ALA red light (633 nm) at an intensity of 120 mW/cm2 administered over three sessions. Mycological evaluation showed negative results with significantly improved lesions and no notable adverse effects (Table 1).
Majocchi’s Granuloma
Majocchi’s granuloma (MG) is a deep suppurative granulomatous perifolliculitis primarily caused by T. rubrum. Shi et al12 reported a case of refractory MG that was successfully treated after three-cycles of ALA-PDT. The lesions were treated using a plum-blossom needle before incubation with 10% ALA, followed by irradiation using red LED light (635 nm) at a power density of 100 mW/cm2 for 120 J/cm2. The authors simultaneously used the clinical strain isolated of the patient for in vitro and in vivo experiments in a guinea pig model. Both in vitro and in vivo experiments demonstrated that ALA-PDT directly destroys the structural framework of the fungal cells and thereby inhibits T. tonsurans and also recruits CD4+ T lymphocytes (Table 1).
Mucormycosis
Mucormycosis, most commonly caused by Rhizopus oryzae is an aggressive and invariably fatal opportunistic fungal infection that originates in the nasal tissues and spreads into the paranasal sinuses and deep organs with a rapid angioinvasive course. Mucorales are resistant to most triazoles, and surgical debridement is associated with specific limitations.11 Liu et al11 observed that MB-PDT inhibited the growth of R. oryzae and enhanced its susceptibility to azoles and amphotericin B in vitro, which explains the synergistic effects of antifungal agents combined with PDT, which was observed in the clinic to some extent (Table 1).
Adverse Effects Associated with Photodynamic Therapy for the Management of Fungal Infections
Usually, most adverse effects of PDT, including local erythema, edema, pain, burning and stinging sensations, and itching, which occur within the first PDT session are mild and tolerable.69,70 Slight blistering and minimal exudation may occur in a few patients. Hyper- or hypopigmentation or scars may persist over a long period of time, particularly in patients with deep fungal infections using ALA-PDT.71 However, most adverse effects are temporary and usually disappear within 2 weeks after PDT.72
Current Limitations of Photodynamic Therapy Used Against Fungal Infections
Although significant research has focused on the role of PDT against fungal infections in recent years, most studies have provided proof-of-concept evidence in case reports in contrast to clinical data obtained through large-scale randomized controlled trials to confirm the long-term efficacy and safety of PDT, to optimize PDT protocols, and definitively establish PS for optimal benefit in specific fungal infections.
Comparison between articles is difficult owing to heterogeneity across studies, which results in a lack of high-quality meta-analyses. Notably, with regard to PDT, the type and concentration of PS, incubation time, light source, wavelengths used, energy, density, duration of exposure to irradiation, frequency of treatment, and growth of microorganisms, among such variables differed across studies, and in view of the diverse treatment settings, results too tend to vary widely, which may interfere with the accuracy of results, with regard to the efficacy of PDT.
Most studies have focused on only a few fungal diseases such as onychomycosis, oral candidiasis, and CBM that are commonly observed in clinical practice or are refractory to standard therapy.15,31,48,57,63 Further studies are needed to gain deeper insight into the exact mechanisms underlying cell death and enhanced susceptibility of fungi to antifungal medications.9,11,60
Few clinical studies in the literature have investigated the specific fungal response to PDT. Some studies have reported inconsistent and even contradictory results between in vitro and in vivo experiments.9 Therefore, in vitro experiments may not accurately predict the clinical response to PDT, and systematic clinical evaluation of specific fungal susceptibility to PDT is essential.
Conclusion
PDT may serve as a potential therapeutic alternative to address increasing drug-resistance encountered in patients with cutaneous fungal infections. PDT is effective against onychomycosis, tinea capitis, PV, oral candidiasis, and VVC in patients with superficial fungal infections. However, PDT did not offer any advantages over conazoles for the treatment of tinea pedis and tinea cruris.73 With regard to deep fungal infections, PDT combined with antifungal drugs was shown to improve treatment efficacy in patients with CBM, sporotrichosis, phaeohyphomycosis, MG, and mucormycosis.
To summarize, PDT is safe and effective and is occasionally useful as a prophylactic and cosmetic tool. Most adverse effects of PDT are limited, temporary, and tolerable. PDT monotherapy or PDT combined with oral antifungal medications may be a promising therapeutic strategy for the management of recurrent or severe cutaneous fungal infections.
Acknowledgments
This work was supported by grants from the Scientific Research Project of the Traditional Chinese Medicine Bureau of Guangdong Province (Grant no-20212147).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Shen JJ, Jemec G, Arendrup MC, et al. Photodynamic therapy treatment of superficial fungal infections: a systematic review. Photodiagnosis Photodyn Ther. 2020;31:101774. doi: 10.1016/j.pdpdt.2020.101774 [DOI] [PubMed] [Google Scholar]
- 2.Rajagopalan M, Inamadar A, Mittal A, et al. Expert Consensus On The Management Of Dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18(1):6. doi: 10.1186/s12895-018-0073-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamblin MR. Antimicrobial photodynamic inactivation: a bright new technique to kill resistant microbes. Curr Opin Microbiol. 2016;33:67–73. doi: 10.1016/j.mib.2016.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta AK, Simpson FC. New pharmacotherapy for the treatment of onychomycosis: an update. Expert Opin Pharmacother. 2015;16(2):227–236. doi: 10.1517/14656566.2015.993380 [DOI] [PubMed] [Google Scholar]
- 5.Bhatta AK, Keyal U, Wang X, et al. A review of the mechanism of action of lasers and photodynamic therapy for onychomycosis. Lasers Med Sci. 2017;32(2):469–474. doi: 10.1007/s10103-016-2110-9 [DOI] [PubMed] [Google Scholar]
- 6.Houang J, Perrone G, Mawad D, et al. Light treatments of nail fungal infections. J Biophotonics. 2018;11(3):e201700350. doi: 10.1002/jbio.201700350 [DOI] [PubMed] [Google Scholar]
- 7.Calixto G, de Annunzio SR, Victorelli FD, et al. Chitosan-based drug delivery systems for optimization of photodynamic therapy: a review. Aaps Pharmscitech. 2019;20(7):253. doi: 10.1208/s12249-019-1407-y [DOI] [PubMed] [Google Scholar]
- 8.Scherer KM, Bisby RH, Botchway SW, et al. New approaches to photodynamic therapy from types I, II and III to type IV using one or more photons. Anticancer Agents Med Chem. 2017;17(2):171–189. doi: 10.2174/1871520616666160513131723 [DOI] [PubMed] [Google Scholar]
- 9.Hu Y, Qi X, Sun H, et al. Photodynamic therapy combined with antifungal drugs against chromoblastomycosis and the effect of ALA-PDT on Fonsecaea in vitro. PLoS Negl Trop Dis. 2019;13(10):e7849. doi: 10.1371/journal.pntd.0007849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Martino A, Pavelkova A, Postnikov PS, et al. Enhancement of 5-aminolevulinic acid phototoxicity by encapsulation in polysaccharides based nanocomplexes for photodynamic therapy application. J Photochem Photobiol B. 2017;175:226–234. doi: 10.1016/j.jphotobiol.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 11.Liu Z, Tang J, Sun Y, et al. Effects of photodynamic inactivation on the growth and antifungal susceptibility of rhizopus oryzae. Mycopathologia. 2019;184(2):315–319. doi: 10.1007/s11046-019-00321-2 [DOI] [PubMed] [Google Scholar]
- 12.Shi L, Wu Q, Yang J, et al. ALA-PDT successfully treated Majocchi’s granuloma by directly killing Trichophyton tonsurans and recruiting T lymphocytes. Photodiagnosis Photodyn Ther. 2021;35:102328. doi: 10.1016/j.pdpdt.2021.102328 [DOI] [PubMed] [Google Scholar]
- 13.Kharkwal GB, Sharma SK, Huang YY, et al. Photodynamic therapy for infections: clinical applications. Lasers Surg Med. 2011;43(7):755–767. doi: 10.1002/lsm.21080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aggarwal R, Targhotra M, Kumar B, et al. Treatment and management strategies of onychomycosis. J Mycol Med. 2020;30(2):100949. doi: 10.1016/j.mycmed.2020.100949 [DOI] [PubMed] [Google Scholar]
- 15.Gupta AK, Simpson FC. New therapeutic options for onychomycosis. Expert Opin Pharmacother. 2012;13(8):1131–1142. doi: 10.1517/14656566.2012.681779 [DOI] [PubMed] [Google Scholar]
- 16.Bodman MA, Krishnamurthy K. Onychomycosis; 2022. [PubMed]
- 17.Gupta AK, Versteeg SG, Shear NH. Onychomycosis in the 21st century: an update on diagnosis, epidemiology, and treatment. J Cutan Med Surg. 2017;21(6):525–539. doi: 10.1177/1203475417716362 [DOI] [PubMed] [Google Scholar]
- 18.de Oliveira GB, Antonio JR, Antonio CR, et al. The association of fractional CO2 laser 10.600nm and photodynamic therapy in the treatment of onychomycosis. An Bras Dermatol. 2015;90(4):468–471. doi: 10.1590/abd1806-4841.20153588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collins TL, Markus EA, Hassett DJ, et al. The effect of a cationic porphyrin on Pseudomonas aeruginosa biofilms. Curr Microbiol. 2010;61(5):411–416. doi: 10.1007/s00284-010-9629-y [DOI] [PubMed] [Google Scholar]
- 20.Park JH, Moon YH, Bang IS, et al. Antimicrobial effect of photodynamic therapy using a highly pure chlorin e6. Lasers Med Sci. 2010;25(5):705–710. doi: 10.1007/s10103-010-0781-1 [DOI] [PubMed] [Google Scholar]
- 21.Bapat P, Singh G, Nobile CJ. Visible lights combined with photosensitizing compounds are effective against candida albicans biofilms. Microorganisms. 2021;9(3):500. doi: 10.3390/microorganisms9030500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wiench R, Skaba D, Stefanik N, et al. Assessment of sensitivity of selected Candida strains on antimicrobial photodynamic therapy using diode laser 635 nm and toluidine blue - In vitro research. Photodiagnosis Photodyn Ther. 2019;27:241–247. doi: 10.1016/j.pdpdt.2019.06.007 [DOI] [PubMed] [Google Scholar]
- 23.Harris F, Pierpoint L. Photodynamic therapy based on 5-aminolevulinic acid and its use as an antimicrobial agent. Med Res Rev. 2012;32(6):1292–1327. doi: 10.1002/med.20251 [DOI] [PubMed] [Google Scholar]
- 24.Sotiriou E, Koussidou-Eremonti T, Chaidemenos G, et al. Photodynamic therapy for distal and lateral subungual toenail onychomycosis caused by Trichophyton rubrum: preliminary results of a single-centre open trial. Acta Derm Venereol. 2010;90(2):216–217. doi: 10.2340/00015555-0811 [DOI] [PubMed] [Google Scholar]
- 25.Gilaberte Y, Robres MP, Frías MP, et al. Methyl aminolevulinate photodynamic therapy for onychomycosis: a multicentre, randomized, controlled clinical trial. J Eur Acad Dermatol Venereol. 2017;31(2):347–354. doi: 10.1111/jdv.13842 [DOI] [PubMed] [Google Scholar]
- 26.Smijs TG, van der Haas RN, Lugtenburg J, et al. Photodynamic treatment of the dermatophyte trichophyton rubrum and its microconidia with porphyrin photosensitizers. Photochem Photobiol. 2004;80(2):197–202. doi: 10.1562/2004-04-22-RA-146.1 [DOI] [PubMed] [Google Scholar]
- 27.Senge MO. mTHPC–a drug on its way from second to third generation photosensitizer? Photodiagnosis Photodyn Ther. 2012;9(2):170–179. doi: 10.1016/j.pdpdt.2011.10.001 [DOI] [PubMed] [Google Scholar]
- 28.Morgado LF, Trávolo A, Muehlmann LA, et al. Photodynamic Therapy treatment of onychomycosis with aluminium-phthalocyanine chloride nanoemulsions: a proof of concept clinical trial. J Photochem Photobiol B. 2017;173:266–270. doi: 10.1016/j.jphotobiol.2017.06.010 [DOI] [PubMed] [Google Scholar]
- 29.Tawfik AA, Noaman I, El-Elsayyad H, et al. A study of the treatment of cutaneous fungal infection in animal model using photoactivated composite of methylene blue and gold nanoparticle. Photodiagnosis Photodyn Ther. 2016;15:59–69. doi: 10.1016/j.pdpdt.2016.05.010 [DOI] [PubMed] [Google Scholar]
- 30.Mohsen Hanafy AM. Epidemiology of cutaneous mycosis in the Medina region of Saudi Arabia correlated with studying the effect of light-induced gold nanoparticles on the growth of dermatophytes in vitro. Afr J Microbiol Res. 2012;6(37):37. doi: 10.5897/AJMR12.1101 [DOI] [Google Scholar]
- 31.Simmons BJ, Griffith RD, Falto-Aizpurua LA, et al. An update on photodynamic therapies in the treatment of onychomycosis. J Eur Acad Dermatol Venereol. 2015;29(7):1275–1279. doi: 10.1111/jdv.12950 [DOI] [PubMed] [Google Scholar]
- 32.Cronin L, Moffitt M, Mawad D, et al. An in vitro study of the photodynamic effect of rose bengal on trichophyton rubrum. J Biophotonics. 2014;7(6):410–417. doi: 10.1002/jbio.201200168 [DOI] [PubMed] [Google Scholar]
- 33.Fekrazad R, Poorsattar BMA, Ghasemi BV, et al. Eradication of C. albicans and T. rubrum with photoactivated indocyanine green, Citrus aurantifolia essential oil and fluconazole. Photodiagnosis Photodyn Ther. 2015;12(2):289–297. doi: 10.1016/j.pdpdt.2014.12.009 [DOI] [PubMed] [Google Scholar]
- 34.Nigam PK, Saleh D. Tinea Pedis; 2022. [PubMed]
- 35.Sotiriou E, Koussidou T, Patsatsi A, et al. 5-Aminolevulinic acid-photodynamic treatment for dermatophytic tinea pedis of interdigital type: a small clinical study. J Eur Acad Dermatol Venereol. 2009;23(2):203–204. doi: 10.1111/j.1468-3083.2008.02783.x [DOI] [PubMed] [Google Scholar]
- 36.Calzavara-Pinton PG, Venturini M, Capezzera R, et al. Photodynamic therapy of interdigital mycoses of the feet with topical application of 5-aminolevulinic acid. Photodermatol Photoimmunol Photomed. 2004;20(3):144–147. doi: 10.1111/j.1600-0781.2004.00095.x [DOI] [PubMed] [Google Scholar]
- 37.Korting HC, Rychlik R, Pfeil B. Behandlung der Tinea pedis vom interdigitalen Typ. Systematischer Review [Treatment of interdigital tinea pedis]. Dtsch Med Wochenschr. 2003;128(36):1819–1824. German. doi: 10.1055/s-2003-41969. [DOI] [PubMed] [Google Scholar]
- 38.Hay R. Therapy of skin, hair and nail fungal infections. J Fungi. 2018;4(3):99. doi: 10.3390/jof4030099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhargava P, Nijhawan S, Singdia H, et al. Skin barrier function defect - a marker of recalcitrant tinea infections. Indian Dermatol Online J. 2020;11(4):566–569. doi: 10.4103/idoj.IDOJ_434_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sotiriou E, Panagiotidou D, Ioannides D. 5-Aminolevulininic acid photodynamic therapy treatment for tinea cruris caused by Trichophyton rubrum: report of 10 cases. J Eur Acad Dermatol Venereol. 2009;23(3):341–342. doi: 10.1111/j.1468-3083.2008.02880.x [DOI] [PubMed] [Google Scholar]
- 41.Ely JW, Rosenfeld S, Seabury SM. Diagnosis and management of tinea infections. Am Fam Physician. 2014;90(10):702–710. [PubMed] [Google Scholar]
- 42.Lu J, Li W, Zheng W, et al. Successful treatment of kerion with itraconazole and ALA-PDT: a case report. Photodiagnosis Photodyn Ther. 2019;27:385–387. doi: 10.1016/j.pdpdt.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 43.Alberdi E, Gómez C. Successful treatment of Pityriasis Versicolor by photodynamic therapy mediated by methylene blue. Photodermatol Photoimmunol Photomed. 2020;36(4):308–312. doi: 10.1111/phpp.12555 [DOI] [PubMed] [Google Scholar]
- 44.Seddiki SM, Boucherit-Otmani Z, Boucherit K, et al. Infectivités fongiques des cathéters implantés dues à Candida sp. Formation des biofilms et résistance [Fungal infectivities of implanted catheters due to Candida sp. Biofilms formation and resistance]. J Mycol Med. 2015;25(2):130–135. French. doi: 10.1016/j.mycmed.2015.03.003 [DOI] [PubMed] [Google Scholar]
- 45.Pierce CG, Lopez-Ribot JL. Candidiasis drug discovery and development: new approaches targeting virulence for discovering and identifying new drugs. Expert Opin Drug Discov. 2013;8(9):1117–1126. doi: 10.1517/17460441.2013.807245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gursoy H, Ozcakir-Tomruk C, Tanalp J, et al. Photodynamic therapy in dentistry: a literature review. Clin Oral Investig. 2013;17(4):1113–1125. doi: 10.1007/s00784-012-0845-7 [DOI] [PubMed] [Google Scholar]
- 47.Freire F, Ferraresi C, Jorge AO, et al. Photodynamic therapy of oral Candida infection in a mouse model. J Photochem Photobiol B. 2016;159:161–168. doi: 10.1016/j.jphotobiol.2016.03.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Campos L, Rezende SB, Palma LF, et al. Antimicrobial photodynamic therapy to oral candidiasis not responsive to micafungin in a patient undergoing hematopoietic cell transplantation. Photodiagnosis Photodyn Ther. 2021;34:102296. doi: 10.1016/j.pdpdt.2021.102296 [DOI] [PubMed] [Google Scholar]
- 49.Chibebe JJ, Sabino CP, Tan X, et al. Selective photoinactivation of Candida albicans in the non-vertebrate host infection model Galleria mellonella. BMC Microbiol. 2013;13:217. doi: 10.1186/1471-2180-13-217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weerasuriya N, Snape J. Oesophageal candidiasis in elderly patients: risk factors, prevention and management. Drugs Aging. 2008;25(2):119–130. doi: 10.2165/00002512-200825020-00004 [DOI] [PubMed] [Google Scholar]
- 51.Qiu H, Mao Y, Gu Y, et al. The potential of photodynamic therapy to treat esophageal candidiasis coexisting with esophageal cancer. J Photochem Photobiol B. 2014;130:305–309. doi: 10.1016/j.jphotobiol.2013.11.028 [DOI] [PubMed] [Google Scholar]
- 52.Chew SY, Than LT. Vulvovaginal candidosis: contemporary challenges and the future of prophylactic and therapeutic approaches. Mycoses. 2016;59(5):262–273. doi: 10.1111/myc.12455 [DOI] [PubMed] [Google Scholar]
- 53.Carrillo-Muñoz AJ, Giusiano G, Ezkurra PA, et al. Antifungal agents: mode of action in yeast cells. Rev Esp Quimioter. 2006;19(2):130–139. [PubMed] [Google Scholar]
- 54.Rosa MI, Silva BR, Pires PS, et al. Weekly fluconazole therapy for recurrent vulvovaginal candidiasis: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):132–136. doi: 10.1016/j.ejogrb.2012.12.001 [DOI] [PubMed] [Google Scholar]
- 55.de Santi M, Prates RA, França CM, et al. Antimicrobial photodynamic therapy as a new approach for the treatment of vulvovaginal candidiasis: preliminary results. Lasers Med Sci. 2018;33(9):1925–1931. doi: 10.1007/s10103-018-2557-y [DOI] [PubMed] [Google Scholar]
- 56.Machado-de-Sena RM, Corrêa L, Kato IT, et al. Photodynamic therapy has antifungal effect and reduces inflammatory signals in Candida albicans-induced murine vaginitis. Photodiagnosis Photodyn Ther. 2014;11(3):275–282. doi: 10.1016/j.pdpdt.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 57.Queiroz-Telles F. Chromoblastomycosis: a neglected tropical disease. Rev Inst Med Trop Sao Paulo. 2015;57(Suppl19):46–50. doi: 10.1590/S0036-46652015000700009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hu Y, Huang X, Lu S, et al. Photodynamic therapy combined with terbinafine against chromoblastomycosis and the effect of PDT on Fonsecaea monophora in vitro. Mycopathologia. 2015;179(1–2):103–109. doi: 10.1007/s11046-014-9828-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lyon JP, Moreira LM, de Carvalho VS, et al. In vitro photodynamic therapy against fonsecaea pedrosoi and cladophialophora carrionii. Mycoses. 2013;56(2):157–161. doi: 10.1111/j.1439-0507.2012.02226.x [DOI] [PubMed] [Google Scholar]
- 60.Huang X, Xu M, Pan W, et al. Antimicrobial and immunomodulatory responses of photodynamic therapy in Galleria mellonella model. BMC Microbiol. 2020;20(1):196. doi: 10.1186/s12866-020-01882-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang W, Zhang W, Luo J, et al. 5-aminolevulinic acid-based photodynamic therapy associated with Itraconazole successfully treated a case of chromoblastomycosis. Photodiagnosis Photodyn Ther. 2020;29:101589. doi: 10.1016/j.pdpdt.2019.101589 [DOI] [PubMed] [Google Scholar]
- 62.Huang X, Han K, Wang L, et al. Successful treatment of chromoblastomycosis using ALA-PDT in a patient with leukopenia. Photodiagnosis Photodyn Ther. 2019;26:13–14. doi: 10.1016/j.pdpdt.2019.02.013 [DOI] [PubMed] [Google Scholar]
- 63.Lan Y, Lu S, Zhang J. Retinoid combined with photodynamic therapy against hyperkeratotic chromoblastomycosis: a case report and literature review. Mycoses. 2021;64(1):18–23. doi: 10.1111/myc.13190 [DOI] [PubMed] [Google Scholar]
- 64.Gupta AK, Carviel J, Shear NH. Antibiofilm treatment for onychomycosis and chronic fungal infections. Skin Appendage Disord. 2018;4(3):136–140. doi: 10.1159/000480023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qin J, Zhang J. Sporotrichosis. N Engl J Med. 2019;380(8):771. doi: 10.1056/NEJMicm1809179 [DOI] [PubMed] [Google Scholar]
- 66.Gilaberte Y, Aspiroz C, Alejandre MC, et al. Cutaneous sporotrichosis treated with photodynamic therapy: an in vitro and in vivo study. Photomed Laser Surg. 2014;32(1):54–57. doi: 10.1089/pho.2013.3590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Almeida-Paes R, Frases S, Araújo GS, et al. Biosynthesis and functions of a melanoid pigment produced by species of the sporothrix complex in the presence of L-tyrosine. Appl Environ Microbiol. 2012;78(24):8623–8630. doi: 10.1128/AEM.02414-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu H, Zhang J, Chen Y, et al. Phaeohyphomycosis due to exophiala spinifera greatly improved by ALA-PDT: a case report. Photodiagnosis Photodyn Ther. 2019;28:297–299. doi: 10.1016/j.pdpdt.2019.10.002 [DOI] [PubMed] [Google Scholar]
- 69.Ibbotson SH, Wong TH, Morton CA, et al. Adverse effects of topical photodynamic therapy: a consensus review and approach to management. Br J Dermatol. 2019;180(4):715–729. doi: 10.1111/bjd.17131 [DOI] [PubMed] [Google Scholar]
- 70.Ozog DM, Rkein AM, Fabi SG, et al. Photodynamic therapy: a clinical consensus guide. Dermatol Surg. 2016;42(7):804–827. doi: 10.1097/DSS.0000000000000800 [DOI] [PubMed] [Google Scholar]
- 71.Ibbotson SH. Adverse effects of topical photodynamic therapy. Photodermatol Photoimmunol Photomed. 2011;27(3):116–130. doi: 10.1111/j.1600-0781.2010.00560.x [DOI] [PubMed] [Google Scholar]
- 72.Wollina U, Bitel A, Vojvodic A, et al. Rosacea flare - up after Photodynamic Therapy (PDT) for field cancerization and a review on adverse events with PDT in general. Open Access Maced J Med Sci. 2019;7(18):2998–3001. doi: 10.3889/oamjms.2019.536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Qiao J, Li R, Ding Y, et al. Photodynamic therapy in the treatment of superficial mycoses: an evidence-based evaluation. Mycopathologia. 2010;170(5):339–343. doi: 10.1007/s11046-010-9325-2 [DOI] [PubMed] [Google Scholar]