Abstract
Background:
Observational studies have reported varying results about the association of velamentous cord insertion (VCI) with adverse pregnancy outcomes.
Objectives:
To evaluate the risk of preterm delivery among singleton pregnancies complicated by VCI.
Search strategy:
Various databases were searched for English-language articles published up to February, 28, 2017, using keywords including VCI; abnormal placentation; abnormal cord insertions; adverse perinatal outcomes; and preterm birth. Outcome measures included preterm delivery; pre-eclampsia; cesarean delivery; fetal demise in utero (FDIU); and small for gestational age (SGA).
Selection criteria:
Only studies involving VCI were included in the meta-analysis.
Data collection and analysis:
Analyses were performed using RevMan version 5.3.5 (The Nordic Cochrane Centre, Copenhagen, Denmark).
Main results:
There were six studies included in the analysis. The VCI and control groups comprised 16 295 and 1 366 485 women, respectively. An increased incidence of preterm delivery was found for the VCI group compared with the control group (11.8% vs 7.0%; adjusted odds ratio [aOR] 1.95, 95% confidence interval [CI] 1.85–2.04). A diagnosis of VCI was also associated with cesarean delivery (aOR 1.17, 95% CI 1.12–1.23), SGA (aOR 1.93, 95% CI 1.83–2.04), and FDIU (aOR 3.96, 95% CI 3.21–4.89).
Conclusion:
The presence of VCI was associated with adverse pregnancy outcomes.
Keywords: Adverse pregnancy outcomes, Cesarean delivery, Preterm birth, Velamentous cord insertion
1 ∣. INTRODUCTION
Velamentous cord insertion (VCI) is an abnormal insertion of the umbilical cord that occurs when the umbilical vessels migrate between the placental membranes before reaching the placental mass. The overall incidence of VCI among singleton pregnancies is 0.4%–2.4%.1,2 This complication has been associated with adverse pregnancy outcomes, including preterm delivery, fetal growth restriction, low Apgar scores, and placental abruption. The pathophysiology of such outcomes is likely secondary to a lack of protective Wharton jelly surrounding the fetal vessels, which in turn leads to abnormal compression or shearing of umbilical vessels during contractions, fetal head descent, or fetal movement.3
The association between VCI and preterm delivery is particularly important as preterm delivery is one of the key contributors to fetal and neonatal death.4 An analysis of preterm delivery among singleton pregnancies with isolated VCI is currently lacking. Some small studies have evaluated preterm delivery as an outcome measure; however, these studies either included other abnormal cord insertions and placental anomalies, or else the findings did not reach statistical significance.3,5-11 A meta-analysis has not yet been conducted to assess the relationship between VCI and preterm delivery in the absence of other cord anomalies. Likewise, no data are available from large controlled studies on which to base clinical management recommendations.
The aim of the present meta-analysis was to evaluate the association between VCI and preterm delivery.
2 ∣. MATERIALS AND METHODS
The present study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines.12 Searches were conducted in the Cochrane Central Register of Controlled Trials and other online databases, including the National library of Medicine database (PubMed), excerpta medica database (Embase), Medical Literature Analysis and Retrieval System (MEDLINE), Latin American and Caribbean Health Science (LILACS) database, Cumulative Index of Nursing and Allied Health Literature (CINAHL), ISI Web of Science, and registers of continuing trials, all from inception to February 28, 2017. A composite of keywords associated with velamentous cord insertions, atypical placentation, anomalous cord insertions, deleterious perinatal outcomes, and preterm delivery was used throughout the search process. Supplementary publications were found by scrutinizing proceedings of global society conferences in maternal–fetal medicine, as well as international summits on preterm delivery and anti-contraction medications, and bibliographies of identified papers and review articles. For trials or observational studies with multiple publications, the data from the best and finished report were used.
The present analysis incorporated observational studies—including case–control, retrospective, and prospective cohort studies—if the outcome of VCI during pregnancy was compared with a control group. As shown in Figure 1, exclusions included studies that involved multiple pregnancies; studies that included participants with other types of abnormal cord insertions; case reports or series; and published abstracts lacking the required information on methodology and data.
FIGURE 1.
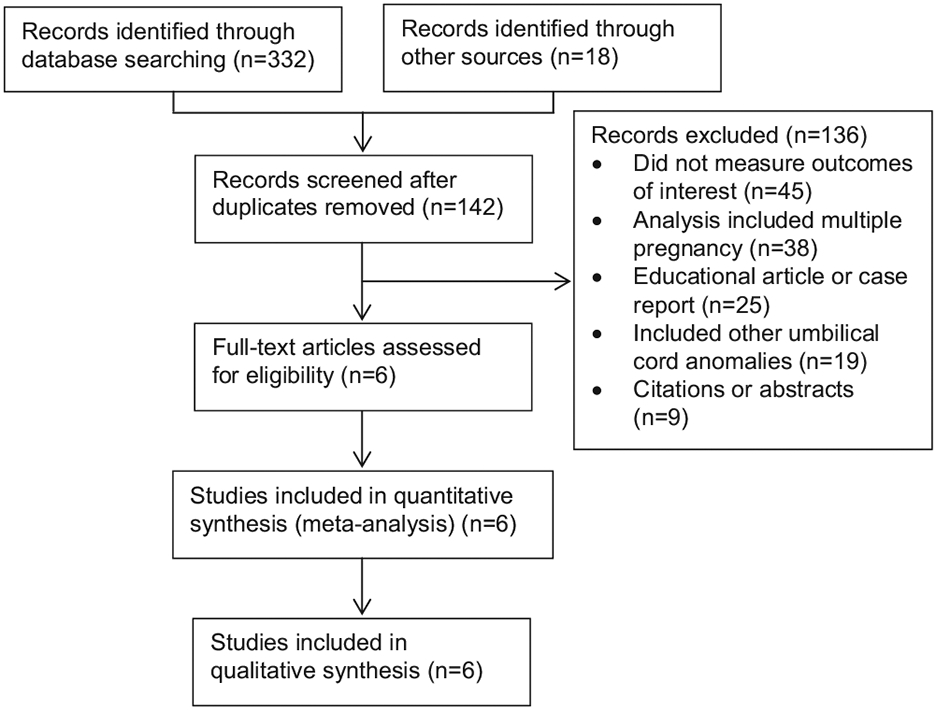
Flow diagram of study selection.
All suitable published studies were retrieved and independently reviewed by two investigators (SdlR and ACE) to determine their eligibility for inclusion in the present analysis; any disagreements were resolved through joint discussion. Authors of selected studies were contacted by email to provide further information regarding the methods and/or outcome measures.
Two investigators (SdlR and ACE) independently abstracted the data from each eligible study, without modification of the original findings, using customized forms. Any differences were resolved through joint discussion to reach a consensus. Crude and adjusted estimates evaluating for confounding variables were extracted from individual studies when available. Risk of bias was assessed using the Methodological Index for Non-Randomized Studies.12 Seven domains related to risk of bias were evaluated for each study included in the present analysis: aim (i.e. provision of an unambiguous objective); rate (i.e. response rate of patients following inclusion into studies); data (i.e. prospective collection of information); bias (i.e. unbiased evaluation of the stated outcome measures); time (i.e. an appropriate duration of follow-up); loss (i.e. the number of participants lost to follow-up); and size (i.e. a clear statement of the minimum number of participants required for statistical power). Judgments were categorized (by SdlR and ACE) as low, high, or unclear risk of bias, with any discrepancies resolved through joint discussion.
The primary outcome measure was preterm delivery (<37 weeks). Secondary outcome measures included pre-eclampsia, fetal demise in utero (FDIU), small for gestational age (SGA) neonates, and the need for cesarean delivery.
The statistical analyses were performed according to the Cochrane Collaboration guidelines.13 The data were analyzed using RevMan version 5.3.5 (The Nordic Cochrane Centre, Copenhagen, Denmark). Meta-analysis was performed if no evidence of marked differences in study populations, interventions, or outcome measures were found. For studies that reported statistically proven unadjusted and adjusted risk for confounders, the meta-analysis was performed using a generic inverse variance method to obtain the adjusted risk estimate of the primary outcome measure.14
The summary adjusted odds ratio (aOR) and 95% confidence interval (CI) were calculated for all dichotomous data. Heterogeneity of the data was assessed using I2, defined as the total variation due to between-study differences rather than chance; I2 values range from 0% (no heterogeneity) to 50% or higher (substantial heterogeneity).14 A fixed-effects model was used to pool data where substantial heterogeneity between studies was not detected. By contrast, a random-effects model was used when the causes of substantial heterogeneity could not be determined or if the mean treatment effect was considered to be clinically meaningful. Publication and related biases were assessed visually by examining the symmetry of funnel plots and statistically with the Egger test (data not shown).14 A P value of less than 0.1 indicated statistically significant asymmetry.
3 ∣. RESULTS
The six studies included in the present meta-analysis6-11 are summarized in Table 1. The studies were conducted in Austria9; Finland6,11; Norway8,10; and the USA.7 All six studies included placentas with normal umbilical cord insertions as a control group. The study designs were prospective cohort8,10; retrospective cohort7,11; retrospective hospital-based registry6; and retrospective case–control.9
TABLE 1.
Studies included in the meta-analysis and systematic review.
| Study | Country | Duration | Design | Total no. of participants |
No. of cases of VCI |
Outcome measures | Diagnosis of VCI |
|---|---|---|---|---|---|---|---|
| Ebbing et al.10 | Norway | 1999–2009 | Population-based registry | 623 478 | 9500 | Placental abruption; placenta previa; pre-eclampsia; preterm delivery; operative delivery; low Apgar score; transfer to NICU; malformations; delivery weight; perinatal death; placental weight; and the ratio of delivery weight to placental weight | Postnatal examination |
| Ebbing et al.8 | Norway | 1999–2013 | Population-based registry | 860 465 | 13 011 | PROM; preterm PROM; spontaneous preterm delivery; and spontaneous preterm delivery without preterm PROM | Postnatal examination |
| Esakoff et al.7 | USA | 2006 | Retrospective cohort study | 482 812 | 2327 | FDIU; SGA; preterm delivery; manual removal of the placenta; cesarean delivery; pre-eclampsia; neonatal seizures; postpartum hemorrhage; and endometritis | Prepartum and postpartum examination, with VCI coded in the medical records |
| Heinonen et al.11 | Finland | 1989–1993 | Retrospective cohort study | 12 750 | 216 | Admission to NICU; FDIU; preterm delivery; low delivery weight; SGA; low Apgar score; fetal pH; and abnormal intrapartum fetal heart rate | Postnatal examination |
| Räisänen et al.6 | Finland | 2000–2011 | Retrospective hospital-based registry | 26 849 | 633 | Gestational age at delivery; cesarean delivery; vacuum delivery; ratio of placenta to fetal mass; umbilical cord length; fetal sex; delivery weight; and malformation | Postnatal examination |
| Yerlikaya et al.9 | Austria | 2003–2013 | Retrospective case–control study | 216 | 108 | Umbilical artery Doppler imaging, pre-eclampsia; pregnancy induced hypertension; growth retardation; FDIU; malformations; gestational age at delivery; cesarean delivery; delivery weight; fetal pH; and low Apgar score | Postnatal examination and prenatal diagnosis |
Abbreviations: FDIU, fetal demise in utero; NICU, neonatal intensive care unit; PROM, premature rupture of membranes; SGA, small for gestational age; VCI, velamentous cord insertion.
Four studies determined the diagnosis of VCI during postnatal examination,6,8,10,11 whereas another study7 reviewed medical records coded for VCI in the prenatal and postnatal periods. Yerlikaya et al.9 conducted both prenatal diagnosis and postnatal examination; however, of the 15 cases diagnosed during the prenatal period, 12 had occurred in the setting of other placental anomalies and so were excluded from the present analysis.
Two studies evaluated emergent or elective cesarean delivery.6,10 Given the clinical implication of VCI, if there was a stratification between emergent and scheduled cesarean deliveries, only emergent procedures were included in the present analysis as, in theory, VCI would not affect the number of scheduled cesarean deliveries. If there was no stratification, all cesarean deliveries were included so as to include procedures performed for urgent or emergent reasons.8,11 Esakoff et al.7 reported only primary cesarean deliveries; their data were included as this approach excluded repeat cesarean delivery as an indication.
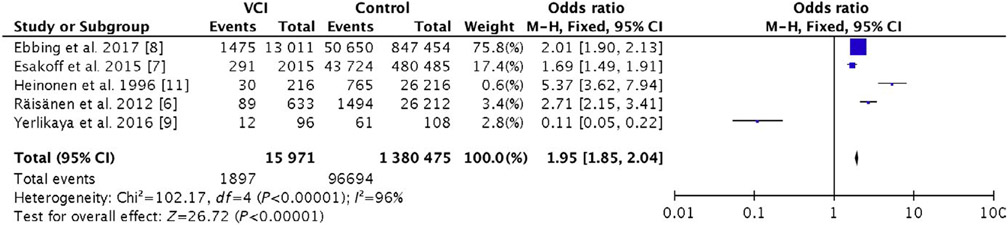
The incidence of preterm delivery was 11.8% in the VCI group versus 7.0% in the control group (aOR 1.95, 95% CI 1.85–2.04) (Fig. 2). The 2017 study by Ebbing et al.8 was used to analyze the primary outcome measure (preterm delivery) as it had been evaluated in both of the studies conducted by these investigators. Accounting for the overlapping data, a total of 1 383 092 cases were included in the present meta-analysis. In all, 16 295 patients were diagnosed with VCI and 1 366 485 comprised the non-VCI control group. The incidence of VCI was 1.1%.
FIGURE 2.
Forest plot for the risk of preterm delivery among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
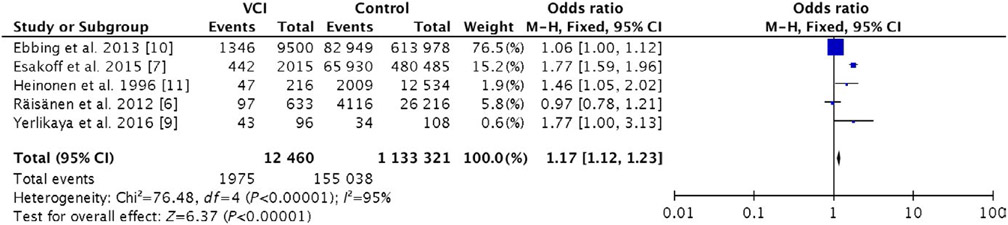
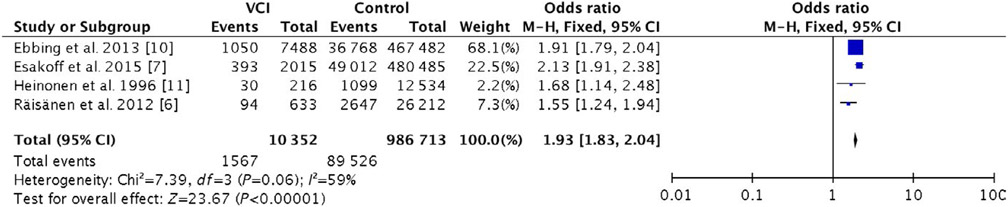
The risk of cesarean delivery was higher in the VCI group than in the control group (15.8% vs 13.6%; aOR 1.17, 95% CI 1.12–1.23). Furthermore, there was an increased risk of SGA neonates in the VCI group when compared to the control group (15.4% vs 9.1%; aOR 1.93, 95% CI 1.83–2.04). Figures 3 and 4 outline the risks of cesarean delivery and SGA, respectively. The incidence of FDIU was 3.4% in the VCI group and 0.4% in the control group (aOR 3.96, 95% CI 3.21–4.89) (Fig. S1). By contrast, a diagnosis of VCI was not associated with an increased risk of pre-eclampsia (Fig. S2); the incidence was 5.3% in the VCI group and 6.0% in the control group (aOR 0.94, 95% CI 0.37–2.40).
FIGURE 3.
Forest plot for the risk of cesarean delivery among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
FIGURE 4.
Forest plot for the risk of small for gestational age neonates among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
The secondary outcomes were assessed using the 2013 study by Ebbing et al.10 because the 2017 study by the same investigators8 did not examine pre-eclampsia, SGA or cesarean delivery. A total of 2 006 270 cases were analyzed across all six studies. The studies by Ebbing et el.8,10 included overlapping datasets; however, the analysis of independent outcomes in the 2013 study10 did not overlap with that of the 2017 study.8
4 ∣. DISCUSSION
The present study found that VCI was associated with an increased risk of preterm delivery, SGA neonates, cesarean delivery, and FDIU.
A key strength of the current meta-analysis was the large number of patients included from the most up-to-date published literature in the field. Indeed, to the best of our knowledge, the present study represents the largest analysis of VCI conducted thus far. Consequently, statistically significant relationships (rather than trends) could be identified between VCI and the various outcome measures. By excluding confounding placental and cord diagnoses, an isolated analysis of preterm delivery and VCI was also possible. A further strength of the present study was stratification of the data for clinical implications. The exclusion of elective cesarean deliveries and neonates with intrauterine growth restriction (IUGR) provided an accurate picture of the in utero environment among women diagnosed with VCI. Five of the six studies included in the present meta-analysis determined VCI by postnatal evaluation6-8,10,11; therefore, the apparent flaw noted above also represented a potential strength of the present study. Diagnosis after delivery protected against observer bias as the management of labor management could not be altered on the basis of prior knowledge of VCI.
Limitations reflected the individual studies included in the present meta-analysis. Sample sizes varied from 2049 to 860 465.8 In addition, the diagnosis of VCI required the relevant healthcare personnel to correctly identify VCI and include the diagnosis in the patient’s delivery record. Consequently, VCI might not have been identified if the cord avulsed, the placenta required manual extraction, or the delivery personnel did not attempt to identify the nature of the cord insertion. These data points might not have been represented in the original studies. None of the six studies stratified preterm delivery by etiology; thus, the data included both spontaneous and iatrogenic deliveries before term. The present meta-analysis was therefore unable to delineate the association of VCI with spontaneous preterm delivery. Potential confounding factors influencing the indication and rate of preterm delivery could not be controlled for in the current study.
The published literature suggested an increased risk of cesarean delivery among women with VCI; however, this association did not reach statistical significance within the respective studies.7,9 Performing a comprehensive review of the literature, with a large sample size, allowed the present study to provide a global view of the relationship between these two variables.
The present finding of an increased risk of SGA was supported by the literature6,7; however, the meta-analysis specifically examined SGA neonates and excluded those with IUGR. The literature is inconsistent regarding the measurement of growth restriction with respect to VCI, with some studies using SGA7,9,10 as a parameter and others using IUGR.6,11 The present meta-analysis specifically examined SGA rather than including IUGR as the weight at time of delivery is more accurate and more reflective of the true in utero environment than a sonographic estimation.
An increased risk of FDIU has been associated with VCI.6,7,9,11 The present findings supported that conclusion. Studies in the literature are mixed with regard to the relationship between pre-eclampsia and VCI. Negative associations have been reported but the data did not reach statistical significance owing to small sample sizes.9,11 Esakoff et al.7 noted an increased risk but this finding was also not statistically significant. By contrast, the present meta-analysis found a non-significant deceased risk of pre-eclampsia in the VCI group versus the control group.
In conclusion, although preterm delivery has numerous etiologies, a relationship was found in the present study between VCI and delivery before 37 weeks. By evaluating VCI in the absence of other placental anomalies, elucidation of the association between VCI and preterm delivery was enhanced. Although a direct causal link cannot yet be established between these two variables, the present study strengthened the evidence supporting such an association.
Supplementary Material
Figure S1. Forest plot for the risk of fetal demise in utero among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
Figure S2. Forest plot for the risk of pre-eclampsia among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
Footnotes
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
SUPPORTING INFORMATION
Additional Supporting Information may be found online in the supporting information tab for this article.
REFERENCES
- 1.Eddleman KA, Lockwood CJ, Berkowitz GS, Lapinski RH, Berkowitz RL. Clinical significance and sonographic diagnosis of velamentous umbilical cord insertion. Am J Perinatol. 1992;9:123–126. [DOI] [PubMed] [Google Scholar]
- 2.Benirschke K, Burton GJ, Baergen RN. Early development of the human placenta. In: Benirschke K, Kaufmann P, eds. Pathology of the Human Placenta. La Jolla: Springer; 2012:41–53. [Google Scholar]
- 3.Hasegawa J, Matsuoka R, Ichizuka K, Sekizawa A, Okai T. Velamentous cord insertion: Significance of prenatal detection to predict perinatal complications. Taiwan J Obstet Gynecol. 2006;45:21–25. [DOI] [PubMed] [Google Scholar]
- 4.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet. 2015;385:430–440. [DOI] [PubMed] [Google Scholar]
- 5.Vahanian SA, Lavery JA, Ananth CV, Vintzileos A. Placental implantation abnormalities and risk of preterm delivery: A systematic review and metaanalysis. Obstet Gynecol. 2015;213:S78–S90. [DOI] [PubMed] [Google Scholar]
- 6.Räisänen S, Georgiadis L, Harju M, Keski-Nisula L, Heinonen S. Risk factors and adverse pregnancy outcomes among births affected by velamentous umbilical cord insertion: A retrospective population-based register study. Eur J Obstet Gynecol Reprod Biol. 2012;165:231–234. [DOI] [PubMed] [Google Scholar]
- 7.Esakoff TF, Cheng YW, Snowden JM, Tran SH, Shaffer BL, Caughey AB. Velamentous cord insertion: Is it associated with adverse perinatal outcomes? J Matern Fetal Neonatal Med. 2015;28:409–412. [DOI] [PubMed] [Google Scholar]
- 8.Ebbing C, Johnsen SL, Albrechtsen S, Sunde ID, Vekseth C, Rasmussen S. Velamentous or marginal cord insertion and the risk of spontaneous preterm birth, prelabor rupture of the membranes, and anomalous cord length, a population-based study. Acta Obstet Gynecol Scand. 2017;96:78–85. [DOI] [PubMed] [Google Scholar]
- 9.Yerlikaya G, Pils S, Springer S, Chalubinski K, Ott J. Velamentous cord insertion as a risk factor for obstetric outcome: A retrospective case–control study. Arch Gynecol Obstet. 2016;293:975–981. [DOI] [PubMed] [Google Scholar]
- 10.Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: A population-based study of 634,741 pregnancies. PLoS ONE. 2013;8:e70380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heinonen S, Ryynänen M, Kirkinen P, Saarikoski S. Perinatal diagnostic evaluation of velamentous umbilical cord insertion: Clinical, doppler, and ultrasonic findings. Obstet Gynecol. 1996;87:112–117. [DOI] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 13.Deeks J, Higgins J, Altman D, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0. The Cochrane Collaboration. 2011. http://handbook-5-1.cochrane.org/. Accessed February 10, 2017. [Google Scholar]
- 14.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Forest plot for the risk of fetal demise in utero among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.
Figure S2. Forest plot for the risk of pre-eclampsia among patients with VCI. Abbreviations: CI, confidence interval; M-H, Mantel-Haenszel test; VCI, velamentous cord insertion.