Abstract
Background
This study was performed to develop and validate machine learning models for early detection of ventilator-associated pneumonia (VAP) 24 h before diagnosis, so that VAP patients can receive early intervention and reduce the occurrence of complications.
Patients and methods
This study was based on the MIMIC-III dataset, which was a retrospective cohort. The random forest algorithm was applied to construct a base classifier, and the area under the receiver operating characteristic curve (AUC), sensitivity and specificity of the prediction model were evaluated. Furthermore, We also compare the performance of Clinical Pulmonary Infection Score (CPIS)-based model (threshold value ≥ 3) using the same training and test data sets.
Results
In total, 38,515 ventilation sessions occurred in 61,532 ICU admissions. VAP occurred in 212 of these sessions. We incorporated 42 VAP risk factors at admission and routinely measured the vital characteristics and laboratory results. Five-fold cross-validation was performed to evaluate the model performance, and the model achieved an AUC of 84% in the validation, 74% sensitivity and 71% specificity 24 h after intubation. The AUC of our VAP machine learning model is nearly 25% higher than the CPIS model, and the sensitivity and specificity were also improved by almost 14% and 15%, respectively.
Conclusions
We developed and internally validated an automated model for VAP prediction using the MIMIC-III cohort. The VAP prediction model achieved high performance based on its AUC, sensitivity and specificity, and its performance was superior to that of the CPIS model. External validation and prospective interventional or outcome studies using this prediction model are envisioned as future work.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12890-022-02031-w.
Keywords: Ventilator-associated pneumonia, MIMIC database, Risk factors, Predictive modeling
Background
Ventilator-associated pneumonia (VAP) is the most common nosocomial pneumonia in critically ill patients [1]. The occurrence of VAP prolongs not only ventilator support but also stays in intensive care units (ICUs) and hospitals, thereby increasing healthcare costs and resulting in a poorer prognosis [2–4]. Studies have shown that some risk factors are associated with VAP. Some risk factors are patient-specific factors, such as age, pre-existing disease (chronic obstructive pulmonary disease, COPD) and a Glasgow coma score of 9 or less [5–7]. Other factors are care-related factors, such as head-of-the-bed angle, emergency intubation, aspiration, previous antibiotic treatment, and reintubation [5, 6, 8].
The early recognition of patients at a high risk of developing VAP and subsequent prevention of its progression are highly valuable in critical care units. Intensivists have been working on a VAP risk prediction model for several years. Several available prediction models are used to predict mortality in VAP patients [9–12]. The Clinical Pulmonary infection Score (CPIS, range from 0 to 12) is a score based on general parameters(body temperature, leukocyte count, volume and character of tracheal secretions, arterial oxygenation, chest X-ray, and culture of tracheal aspirate), it has moderate to good accuracy in VAP prediction and is simple and easy to perform and often used in clinical diagnosis of VAP [13, 14]. However, there is no early risk prediction model for VAP.
Machine learning algorithms have become more important tools since they can be more accurate than traditional logistic regression, which has been suggested by previous comparison studies [15, 16]. Of all machine learning algorithms, the random forest for regression and classification has considerably gained popularity. It is an “ensemble learning” technique consisting of the aggregation of a large number of decision trees. For classification tasks, the output of the random forest is the class selected by most trees and for regression tasks, the mean or average prediction of the individual trees is returned, resulting in a better performance and reduction of variance [16]. The study applied the random forest algorithm to construct a base classifier for early prediction of ventilator-associated pneumonia in critical care patients.
The aim of this study was to use the Medical Information Mart for Intensive Care (MIMIC)-III dataset to develop and validate machine learning models for the early discrimination of patients at a high risk of VAP 24 h after intubation and assess its prognostic accuracy. The MIMIC database is an open, large, single-center database that can be used freely by researchers worldwide, and it has been widely used in the development of predictive models, epidemiological studies, and educational courses [17]. Also, We also compare the performance of Clinical Pulmonary Infection Score (CPIS)-based model (threshold value ≥ 3) using the same training and test data sets.
Methods
Datasets
The MIMIC-III database was used to train, validate and test the models and comprises unidentified health-related data associated with 61,532 ICU stays in multiple critical care units in Beth Israel Deaconess Medical Center between 2001 and 2012 [17]. This database is a publicly available database constructed in compliance with the Health Insurance Portability and Accountability Act. The study protocol was approved by the ethics committee of the First Hospital of China Medical University (No. 2019–197-2).
Data annotation and extraction
In total, 38,515 ventilation sessions were identified in the MIMIC-III database and filtered according to the patient inclusion process depicted in Fig. 1. In total, 10,431 patients aged over 18 years who received mechanical ventilation for longer than 24 h were included in this study. Pneumonia occurring > 48 h after endotracheal intubation and mechanical ventilation were annotated as VAP according to the VAP definition [18]. The other sessions were grouped as non-VAP sessions. When VAP was diagnosed, the presence of infection at other sites was recorded.
Fig. 1.
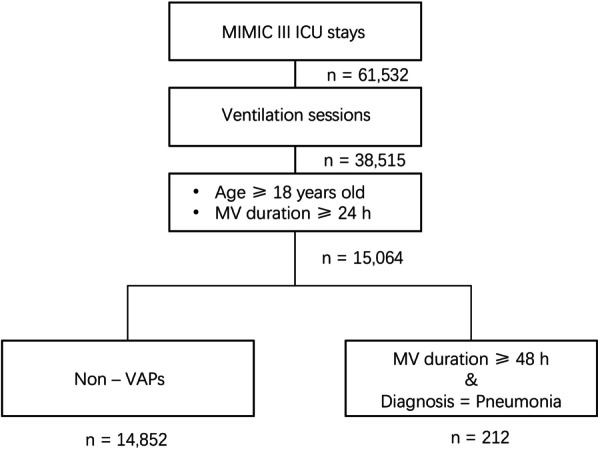
Study profile. MIMIC, Medical Information Mart for Intensive Care; MV Mechanical ventilation; VAP, ventilator-associated pneumonia; ICU, intensive care unit
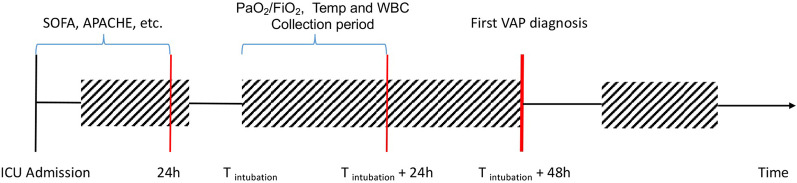
To detect the risk of the first occurrence of VAP early, a set of 42 variables (features) were extracted from the MIMIC-III dataset according to our previous studies and literature [5–8, 19], including age, sex, admission source [medical intensive care unit (MICU), others ( CCU (Coronary Care Unit), SICU(Surgical Intensive Care Unit), CSRU(Cardiac Surgery Recovery Unit) and ISICU(Trauma Surgical Intensive Care Unit))] and type (emergency, elective), reintubation, pre-existing diseases, the worst value of the partial pressure of the arterial oxygen/fraction of inspired oxygen (PaO2/FiO2) ratio, white blood cell count (WBC), body temperature in the first 24 h after ventilation, the worst value of the APACHE III and its subcomponents, the sequential organ failure assessment (SOFA) and its subcomponents in the first 24 h after admission to the ICU, coma, aspiration, sepsis, bacteremia, trauma/polytrauma, fracture and pneumothorax (the detailed information of these 42 variables is provided in Additional file 4: Table S1). Figure 2 shows the timeline for VAP diagnosis and VAP variable extraction.
Fig. 2.
Timeline for the first VAP prediction and VAP variable extraction. ICU, intensive care unit; SOFA, Sequential Organ Failure Assessment; APACHE, Acute Physiology and Chronic Health Evaluation; PaO2/FiO2, the partial pressure of arterial oxygen/ fraction of inspired oxygen; WBC, white blood cell count; VAP, ventilator-associated pneumonia
Data splitting and sampling
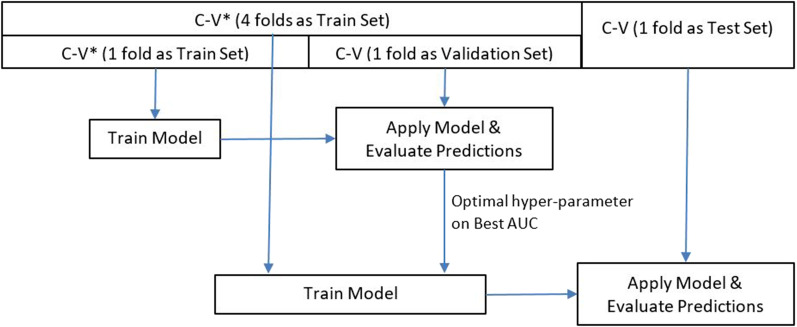
Figure 3 describes the pipeline applied for the model training, validation and testing. The included dataset was divided into a training dataset and test dataset for the five-fold cross-validation in which four folds were used as the training dataset, the remaining fold was used as the test dataset, and the folds were mutually exclusive. To identify the optimal hyperparameter of the model, two-fold cross-validation was performed using the training dataset, and then, the model was retrained using the optimal hyperparameter based on the entire training dataset to learn the model parameters. Due to an extreme imbalance between the number of non-VAP and VAP patients, the negative dataset was divided into 100 subgroups for resampling. Stratified sampling was used to ensure an even class distribution.
Fig. 3.
Model training, validation and testing pipeline. The dataset was divided into four groups as a training dataset and one group as test dataset for five-fold cross-validation. C-V, cross-validation
Data preprocessing
Additional file 1: Fig. S1 shows the data preprocessing steps. For the numeric variables, if a patient did not have a measurement, the missing value was filled by using the median interpolation of the whole cohort (Additional file 4: Table S1 shows the count and percentage of missing data in the VAP group and non-VAP group; Fisher’s exact test was used to test the significance). For the categorical variables with d categories, the raw data were mapped to a d-dimensional vector, where each dimension corresponded to a different category; however, the categorical variables with two categories (e.g., sex = {F, M}) were sufficiently mapped to {0, 1}. Then, both the numeric and categorical data were normalized for the training dataset, which required min–max feature scaling to adjust for variable values measured on different scales.
Model development and performance measurement
Since there were many more non-VAP instances than VAP instances, we divided the non-VAP instances into 100 subgroups with mutual exclusivity. One subgroup of non-VAP instances was combined with the VAP dataset to train one model; then, 100 models were combined based on the performance average or major voting as the final model. The ensemble method was applied to 100 subgroups of non-VAP instances in combination with VAP instances as shown in Additional file 2: Fig. S2.
The random forest algorithm was applied to construct the classifier. The area under the receiver operating characteristic (ROC) curve (AUC), accuracy, sensitivity and specificity of the prediction model were evaluated. Furthermore, we used an original CPIS-based model for the early detection of VAP as a benchmark model to compare with our machine learning model, and the performance of the classification model was evaluated using the same training and test datasets. The performance is described as the mean ± SD to indicate the performance distribution of the subgroups, and the SD was used to determine whether any overfitting of the model occurred in certain datasets.
The Bayes search method was applied to fine-tune the hyperparameters of the base classifier using the validation set. In the random forest classifier, the optimal number of estimators of the hyperparameter was adjusted to 104, which was randomly obtained via Bayes search in the range from 1 to 300.
Statistical analysis
In the analysis of the clinical characteristics of both the VAP and non-VAP groups, the numeric variables are described as medians and interquartile ranges (IQRs; represented by the 25th and 75th percentile values), and the categorical variables are described as counts and percentages. To compare the two groups, we used Fisher’s exact test for the categorical variables and the Mann–Whitney U-test for the numeric variables. A p-value less than 0.05 was considered statistically significant. Python3.0 was used to perform the statistical, sklearn.model was used to perform model building.
Results
According to the screening criteria shown in Fig. 1, 38,515 ventilation sessions were included with 212 VAP sessions between 2001 and 2012 in the MIMIC-III cohort, and the incidence density was 2 per 1,000 ventilator-days. The median time on mechanical ventilation from endotracheal intubation to the first VAP episode was 5.4 days (IQR, 3.2 days to 8.5 days). None of these VAP patients had infections in other sites. The missing counts and percentages of the 42 variables in the overall, VAP, and non-VAP groups are shown in Additional file 4: Table S1. Compared with the overall study cohort, the non-VAP group had significantly higher missing albumin and acid–base scores in the APACHE III and respiration scores in SOFA. However, the VAP group had a higher missing percentage of pulmonary alveolus-arterial difference of oxygen pressure/partial pressure of oxygen (A-aDO2/PaO2) and urine output.
The univariate analysis indicated that compared to the control group, the VAP group in the study cohort had a significantly different admission source and type (p < 0.001); specifically, the VAP group had a significantly higher ratio of patients from the MICU, and only one VAP patient was not transferred from the emergency department (see details in Table 1). The worst value of the PaO2/FiO2 ratio in the first 24 h after ventilation was significantly deteriorated (p < 0.001) in the VAP group compared with that in the control group. The reintubation ratio did not significantly differ (p = 0.823) between the VAP group and non-VAP group, whereas the VAP group demonstrated a significantly higher ratio in aspiration (p = 0.004). Regarding pre-existing diseases, there was no difference between the VAP group and non-VAP group, except for hypertension.
Table 1.
Demographic and clinical characteristics of study cohort in MIMIC III
| Overall (n = 10,431) |
VAP group (n = 212) |
Non-VAP group (n = 10,219) |
p value | |
|---|---|---|---|---|
| Age(years), median(IQR) | 66.3 (53.1–76.0) | 66.3 (52.1–77.8) | 66.3 (53.1–76.0) | 0.387 |
| Gender, n(%) | 0.107 | |||
| Male | 5937 (56.9) | 109 (51.4) | 5828 (57.0) | |
| Female | 4494 (43.1) | 103 (48.6) | 4391 (43.0) | |
| Admission source, n(%) | < 0.001 | |||
| MICU | 4089 (39.2) | 154 (72.6) | 3935 (38.5) | |
| Other ICU | 6342 (60.8) | 58 (27.4) | 6284 (61.5) | |
| Admission type, n(%) | < 0.001 | |||
| Emergency | 9504 (91.1) | 211 (99.5) | 9293 (90.9) | |
| Elective | 927 (8.9) | 1 (0.5) | 926 (9.1) | |
| Reintubation, n(%) | 3294 (31.6%) | 65 (30.7%) | 3229 (30.6%) | 0.823 |
| Pre-existing Diseases, n(%) | ||||
| COPD | 101 (1.0%) | 2 (0.9%) | 99 (1.0) | 1.0 |
| Diabetes | 2698 (25.9) | 60 (28.3) | 2638 (25.8) | 0.428 |
| Hypertension | 4943 (47.4) | 80 (37.7) | 4863 (47.6) | 0.004 |
| Solid tumor | 313 (3.0) | 8 (3.8) | 305 (3.0) | 0.537 |
| Metastatic tumor | 418 (4.0) | 5 (2.4) | 413 (4.0) | 0.286 |
| Renal failure | 1721 (16.5) | 26 (12.3) | 1695 (16.6) | 0.111 |
| Liver failure | 1653 (15.9) | 22 (10.4) | 1631 (16.0) | 0.028 |
| PaO2/FiO2, median(IQR) | 240.0 (178.5–315.4) | 194.17 (150.0–256.5) | 241.0 (179.4–316.7) | < 0.001 |
| WBC(K/uL), median(IQR) | 12.8 (9.2–17.7) | 13.2 (9.8–18.0) | 12.8 (9.2–17.7) | 0.121 |
| Body temperature(℃), median(IQR) | 37.8 (37.3–38.4) | 37.9 (37.3–38.6) | 37.8 (37.3–38.4) | 0.255 |
| APACHE III score, median(IQR) | 50.0 (37.0–66.0) | 53.0 (40.75–64.0) | 50.0 (37.0–66.0) | 0.031 |
| HR | 5.0 (0.0–7.0) | 5.0 (0.0–7.0) | 5.0 (0.0–7.0) | 0.028 |
| MAP | 15.0 (7.0–15.0) | 15.0 (7.0–15.0) | 15.0 (7.0–15.0) | 0.197 |
| Temperature | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | < 0.001 |
| RR | 6.0 (0.0–6.0) | 6.0 (0.0–9.0) | 6.0 (0.0–6.0) | 0.001 |
| A-aDO2/PaO2 | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | < 0.001 |
| Hematocrit | 3.0 (3.0–3.0) | 3.0 (3.0–3.0) | 3.0 (3.0–3.0) | 0.269 |
| WBC | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.083 |
| Creatinine | 0.0 (0.0–7.0) | 0.0 (0.0–7.0) | 0.0 (0.0–7.0) | 0.484 |
| UO | 5.0 (0.0–7.0) | 5.0 (0.0–7.0) | 5.0 (0.0–7.0) | 0.013 |
| BUN | 7.0 (2.0–11.0) | 7.0 (2.0–11.0) | 7.0 (2.0–11.0) | 0.094 |
| Sodium | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | 0.016 |
| ALB | 0.0 (0.0–6.0) | 0.0 (0.0–6.0) | 0.0 (0.0–6.0) | 0.087 |
| Bilirubin | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.008 |
| Glucose | 0.0 (0.0–3.0) | 3.0 (0.0–3.0) | 0.0 (0.0–3.0) | 0.017 |
| Acid–base | 3.0 (1.0–6.0) | 3.0 (1.0–5.0) | 3.0 (1.0–6.0) | 0.077 |
| GCS | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.017 |
| SOFA score, median(IQR) | 6.0 (4.0–9.0) | 6.0 (4.0–8.0) | 6.0 (4.0–9.0) | 0.034 |
| Respiration | 3.0 (0.0–3.0) | 3.0 (2.0–3.0) | 3.0 (0.0–3.0) | 0.014 |
| Coagulation | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | < 0.001 |
| Liver | 0.0 (0.0–1.0) | 0.0 (0.0–0.0) | 0.0 (0.0–1.0) | 0.004 |
| Cardiovascular | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 1.0 (1.0–3.0) | 0.022 |
| CNS | 0.0 (0.0–1.0) | 0.0 (0.0–0.0) | 0.0 (0.0–1.0) | 0.008 |
| Renal | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 1.0 (0.0–2.0) | 0.471 |
| Coma adm, n(%) | 6 (0.1%) | 0 (0.0%) | 6 (0.1%) | 1.0 |
| Aspiration adm, n(%) | 32 (0.3%) | 4 (1.9%) | 28 (0.3%) | 0.004 |
| Sepsis adm, n(%) | 548 (5.3%) | 10 (4.7%) | 538 (5.3%) | 0.876 |
| Bacteremia adm, n(%) | 11 (0.1%) | 0 (0.0%) | 11 (0.1%) | 1.0 |
| Trauma adm, n(%) | 202 (1.9%) | 0 (0.0%) | 202 (2.0%) | 0.037 |
| Polytrauma adm, n(%) | 45 (0.4%) | 0 (0.0%) | 45 (0.4%) | 1.0 |
| Fracture adm, n(%) | 27 (0.3%) | 0 (0.0%) | 27 (0.3%) | 1.0 |
| Pneumothorax adm, n(%) | 19 (0.2%) | 0 (0.0%) | 19 (0.2%) | 1.0 |
MICU medical intensive care unit, APACHE III Acute Physiology and Chronic Health Evaluation III, PaO2/FiO2 the partial pressure of arterial oxygen/ fraction of inspired oxygen, WBC white blood cell count, HR heart rate, MAP mean arterial pressure, RR respiratory rate, A-aDO2/PaO2 pulmonary alveolus-arterial difference of oxygen pressure/ partial pressure of oxygen, UO urine output, BUN blood urea nitrogen, ALB albumin, GCS Glasgow Coma Scale, SOFA sequential organ failure assessment, CNS central nervous system, COPD chronic obstructive pulmonary disease, adm admission
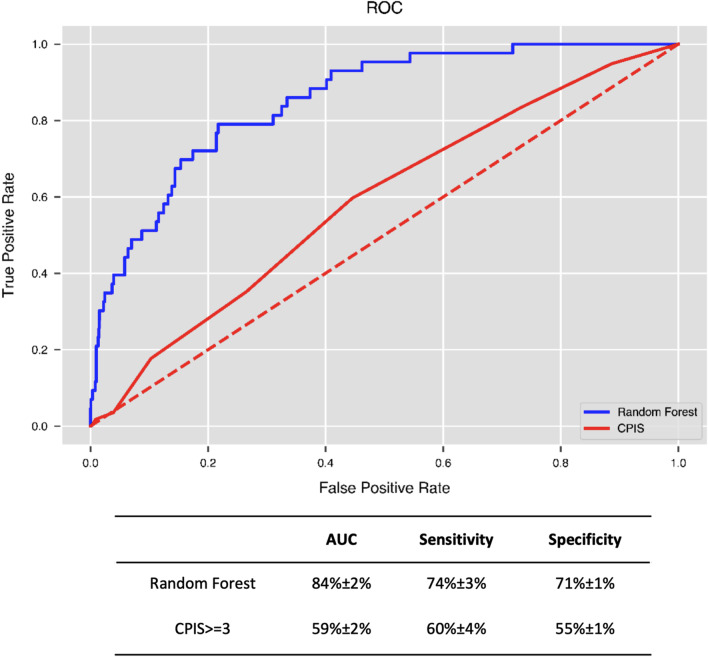
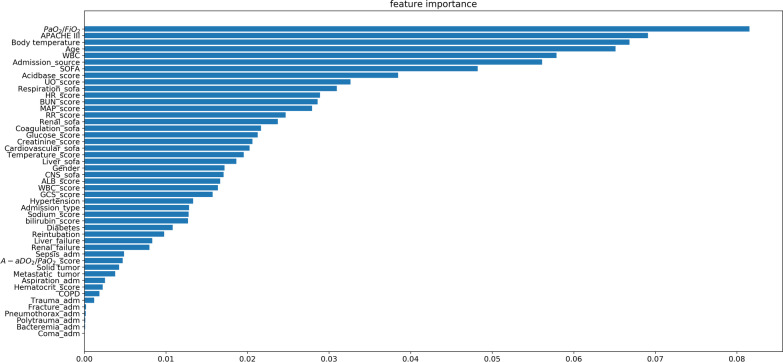
Figure 4 shows that the AUC of the optimal performance corresponding to the random forest model was 84% ± 2% in the validation using the pure testing datasets, and the sensitivity and specificity approached 74 ± 3% and 71 ± 1%, respectively. Using the same test datasets, the best performance of the CPIS-based model was AUC = 59 ± 2%, sensitivity = 60± 4%, and specificity = 55± 1% as CPIS equal to or greater than 3. Figure 5 shows the feature importance of the optimal random forest model, indicating the contribution rankings of the features to the prediction value in the model. The admission source, APACHE III and SOFA scores along with their sub items, age, worst body temperature value, PaO2/FiO2 ratio, and WBC in the initial 24 h after ventilation were the top 10 most important features and contributed over 46% of the total prediction value. The respiration items of the SOFA were the highest contributors to the total SOFA score (4% of the VAP prediction model), indicating the significance of respiration for organ failure.
Fig. 4.
Performances of the VAP predictive model and CPIS model
Fig. 5.
Feature importance in our predictive model of VAP. The feature importance of the optimal random forest model indicates the features’ contribution to the VAP prediction
Discussion
In this retrospective cohort study, we developed and validated a machine learning model for the early detection of VAP patients in the first 24 h after intubation. The final predictive AUC showed a good performance (AUC: 84%, sensitivity: 74%, and specificity: 71%) as an AUC value between 75 and 92% indicates good diagnostic capability [20]. Additionally, our VAP machine learning model achieved better results than the CPIS-based model by almost 25%, and the sensitivity and specificity were improved by almost 14% and 15%, respectively.
A CPIS score threshold of 6 helps to distinguish the presence or absence of pulmonary infection [21]. But in our MIMIC III cohort data, a CPIS score of 6 did not show a good performance. Considering the heterogeneity in the performances of CPIS for the diagnosis of VAP in ventilated patients [13, 14], different score thresholds were tested to determine the best performance. Additional file 3: Fig. S3 shows that when the score was equal to or greater than 3, the CPIS-based model had the best performance. It is for this reason that we have compared our model with a CPIS score ≥ 3 instead of with a CPIS score ≥ 6.
Low PaO2/FiO2 ratio is one of the main clinical manifestations of ARDS. The typical ARDS manifestations include increased pulmonary vascular permeability, pulmonary edema and alveolar trapping, which lead to refractory hypoxia and decreased pulmonary compliance [22]. The relationship between ARDS and the subsequent development of VAP is complex. In mechanically-ventilated patients, the cyclic stretching of lung cells induces acidification of the milieu, which promotes bacterial growth [23]. Injurious mechanical ventilation may promote the lungs to release cytokines [24, 25]. In addition, alveolar macrophages and neutrophils exhibit reduced bacterial phagocytosis and killing, thereby affecting the lung and systemic antibacterial defenses [24, 26, 27].
We found that the APACHE III and SOFA scores greatly contributed to the final predictive model. The APACHE scoring system is used to describe the severity of illness and predict the outcome of critically ill patients. The APACHE II and III are widely employed in the ICU [28, 29], and the overall goodness-of-fit of the two predictive models was similar. APACHE III expanded the acute physiology score project compared to APACHE II, added the following six parameters: blood urea nitrogen, total bilirubin, blood glucose, albumin, artery CO2 partial pressure (PaCO2) and urine output. These six parameters are more responsive in clinical practice [30, 31]. The APACHE II was better in predicting risk among surgical patients and patients with gastrointestinal disease [30], while the APACHE III score was a good predictor of internal medical conditions and nosocomial pneumonia [31, 32].
Reintubation, aspiration, COPD, trauma, and coma are usually the risk factors of VAP. In our model, only first VAP sessions were accounted for the prediction to avoid intra-correlation between consecutive sessions. That is why reintubation were not in the higher ranking. For aspiration, COPD, trauma and coma, we only included diagnosis in admission as predictor, and then, the ratio in both VAP and non-VAP group is quite low (< 2%, details in Table 1).
A major limitation of this study was that a small number of VAP cases were delayed or missed for various reasons, resulting in a false negative diagnosis of VAP. We acquired the infections sites by using nursing chart. It was possible to be underrecognized or not charted by nurses. Sputum examination is necessary when VAP is suspected. Sputum frequency is reported to be a factor in the VAP prediction model. The definition of VAP has greatly evolved over the last two decades and different definitions are used in clinical practice. Our model is developed based on definitions used between 2001 and 2012. Our solution to circumvent this problem is to take the current definitions of VAP(18) and use a data driven approach to label patients as VAP or non-VAP. This would solve the problem of outdated definitions, time stamping and subjectivity. In our study, the non-VAP group included patients with mechanical ventilation for 24 h rather than patients with 48 h of mechanical ventilation for the following reasons: we selected the worst body temperature values, PaO2/FiO2 ratio, and WBC during the initial 24 h after ventilation and the worst values of the APACHE III and SOFA scores in the first 24 h after admission to the ICU as VAP predictors. If we included patients with 48 h of mechanical ventilation in the control group, some non-VAP patients could be missed. Our predictive model can provide risk stratification for VAP patients within independently-defined patient groups. Prevention guidelines have been developed to allow higher-risk patients to benefit from more aggressive strategies or adjuvant therapy. Additionally, a longer prediction lead time could increase the likelihood that a patient can benefit from early intervention.
Conclusions
We developed and internally validated an automated model for VAP prediction using the MIMIC-III cohort. The VAP prediction model achieved a high performance based on the AUC, sensitivity and specificity, and its performance was superior to that of the CPIS-based model. External validation and prospective interventional or outcome studies using this prediction model are envisioned as future work.
Supplementary Information
Additional file 1: Data pre-processing pipeline.
Additional file 2: Imbalanced dataset model. The non-VAP dataset was divided into 100 subgroups, one of which was combined with the VAP dataset to train the model, and then, 100 models were combined into the final model.
Additional file 3: Performance of CPIS-based model in MIMICIII cohort and selection of optimal threshold selection. From CPIS was a score (t) ranged from 0-12 with 6 subcategories. Performance of CPIS was indicated by using AUROC along with the increase of t. Considering t could only be integer, i.e. t=2,3,4,…, t=3 was selected as cut-off since the drop of sensitivity and increase of specificity could be balanced, i.e. the point with largest Youden index.
Additional file 4: List of 42 variables and missing value in study cohort.
Acknowledgements
Not applicable.
Abbreviations
- VAP
Ventilator-associated pneumonia
- ICU
Intensive care unit
- APACHE III
Acute physiology and chronic health evaluation III
- MIMIC
Medical Information Mart for Intensive Care
- SOFA
Sequential organ failure assessment
- PaO2/FiO2
The partial pressure of arterial oxygen/fraction of inspired oxygen
- WBC
White blood cell count
- COPD
Chronic obstructive pulmonary disease
- ARDS
Acute respiratory distress syndrome
- CPIS
Clinical pulmonary infection score
Author contributions
YL and XM participated in the conception of the idea and conduct of the study, YL and CZ wrote the main manuscript text. CT and QL provided engineering expertise and prepared Figs. 1–5. ZLL, ZFL and DN participated in additional analysis and critical revision. All authors reviewed and approved the submitted form of this manuscript.
Funding
This work was funded by grants from Natural Science Foundation of Liaoning Province (2021-MS-11).
Availability of data and materials
The datasets generated and/or analysed during the current study are available in the MIMIC III repository. [https://mimic.mit.edu/].
Declarations
Ethics approval and consent to participate
All methods used in this study were performed in accordance with the Declaration of Helsinki, and the protocol approved by the ethics committee of the First Hospital of China Medical University (No. 2019-197-2)
Consent for publication
Not applicable.
Competing interests
Cong Tian and Qizhong Lin are currently employed by Philips Research China. The remaining authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906. doi: 10.1007/s00134-020-05980-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kollef MH, Hamilton CW, Ernst FR. Economic impact of ventilator-associated pneumonia in a large matched cohort. Infect Control Hosp Epidemiol. 2012;33(3):250–256. doi: 10.1086/664049. [DOI] [PubMed] [Google Scholar]
- 3.Craven DE, Lei Y, Ruthazer R, Sarwar A, Hudcova J. Incidence and outcomes of ventilator-associated tracheobronchitis and pneumonia. Am J Med. 2013;126(6):542–549. doi: 10.1016/j.amjmed.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Mathai AS, Phillips A, Kaur P, Isaac R. Incidence and attributable costs of ventilator-associated pneumonia (VAP) in a tertiary-level intensive care unit (ICU) in northern India. J Infect Public Health. 2015;8(2):127–135. doi: 10.1016/j.jiph.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Akca O, Koltka K, Uzel S, Cakar N, Pembeci K, Sayan MA, Tutuncu AS, Karakas SE, Calangu S, Ozkan T, et al. Risk factors for early-onset, ventilator-associated pneumonia in critical care patients: selected multiresistant versus nonresistant bacteria. Anesthesiology. 2000;93(3):638–645. doi: 10.1097/00000542-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Galal YS, Youssef MR, Ibrahiem SK. Ventilator-associated pneumonia: incidence, risk factors and outcome in paediatric intensive care units at cairo university hospital. J Clin Diagn Res. 2016;10(6):SC06–11.doi:10.7860/JCDR/2016/18570.7920 [DOI] [PMC free article] [PubMed]
- 7.Tejerina E, Frutos-Vivar F, Restrepo MI, Anzueto A, Abroug F, Palizas F, Gonzalez M, D'Empaire G, Apezteguia C, Esteban A, et al. Incidence, risk factors, and outcome of ventilator-associated pneumonia. J Crit Care. 2006;21(1):56–65. doi: 10.1016/j.jcrc.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Rello J, Allegri C, Rodriguez A, Vidaur L, Sirgo G, Gomez F, Agbaht K, Pobo A, Diaz E. Risk factors for ventilator-associated pneumonia by Pseudomonas aeruginosa in presence of recent antibiotic exposure. Anesthesiology. 2006;105(4):709–714. doi: 10.1097/00000542-200610000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Zhou XY, Ben SQ, Chen HL, Ni SS. A comparison of APACHE II and CPIS scores for the prediction of 30-day mortality in patients with ventilator-associated pneumonia. Int J Infect Dis. 2015;30:144–147. doi: 10.1016/j.ijid.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Mirsaeidi M, Peyrani P, Ramirez JA, Improving medicine through pathway assessment of critical therapy of hospital-acquired pneumonia I. Predicting mortality in patients with ventilator-associated pneumonia: The APACHE II score versus the new IBMP-10 score. Clin Infect Dis. 2009;49(1):72–7.doi:10.1086/599349 [DOI] [PubMed]
- 11.Huang KT, Tseng CC, Fang WF, Lin MC. An early predictor of the outcome of patients with ventilator-associated pneumonia. Chang Gung Med J. 2010;33(3):274–282. [PubMed] [Google Scholar]
- 12.Lisboa T, Diaz E, Sa-Borges M, Socias A, Sole-Violan J, Rodriguez A, Rello J. The ventilator-associated pneumonia PIRO score: a tool for predicting ICU mortality and health-care resources use in ventilator-associated pneumonia. Chest. 2008;134(6):1208–1216. doi: 10.1378/chest.08-1106. [DOI] [PubMed] [Google Scholar]
- 13.Gaudet A, Martin-Loeches I, Povoa P, Rodriguez A, Salluh J, Duhamel A, Nseir S, group TAs. Accuracy of the clinical pulmonary infection score to differentiate ventilator-associated tracheobronchitis from ventilator-associated pneumonia. Ann Intensive Care. 2020;10(1):101.doi:10.1186/s13613-020-00721-4 [DOI] [PMC free article] [PubMed]
- 14.Shan J, Chen HL, Zhu JH. Diagnostic accuracy of clinical pulmonary infection score for ventilator-associated pneumonia: a meta-analysis. Respir Care. 2011;56(8):1087–1094. doi: 10.4187/respcare.01097. [DOI] [PubMed] [Google Scholar]
- 15.Deo RC. Machine learning in medicine. Circulation. 2015;132(20):1920–1930. doi: 10.1161/CIRCULATIONAHA.115.001593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Churpek MM, Yuen TC, Winslow C, Meltzer DO, Kattan MW, Edelson DP. Multicenter comparison of machine learning methods and conventional regression for predicting clinical deterioration on the wards. Crit Care Med. 2016;44(2):368–374. doi: 10.1097/CCM.0000000000001571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O'Grady NP, Bartlett JG, Carratala J, et al. Executive summary: management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 Clinical practice guidelines by the infectious diseases society of America and the American thoracic society. Clin Infect Dis. 2016;63(5):575–582. doi: 10.1093/cid/ciw504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang YJ, Li ZL, Wang L, Liu BY, Ding RY, Ma XC. Comparision of risk factors and pathogens in patients with early- and late-onset ventilator-associated pneumonia in intensive care unit. Zhonghua Nei Ke Za Zhi. 2017;56(10):743–746. doi: 10.3760/cma.j.issn.0578-1426.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Jones CM, Athanasiou T. Summary receiver operating characteristic curve analysis techniques in the evaluation of diagnostic tests. Ann Thorac Surg. 2005;79(1):16–20. doi: 10.1016/j.athoracsur.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 21.Bickenbach J, Marx G. Diagnosis of pneumonia in mechanically ventilated patients: what is the meaning of the CPIS? Minerva Anestesiol. 2013;79(12):1406–1414. [PubMed] [Google Scholar]
- 22.Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 23.Pugin J, Dunn-Siegrist I, Dufour J, Tissieres P, Charles PE, Comte R. Cyclic stretch of human lung cells induces an acidification and promotes bacterial growth. Am J Respir Cell Mol Biol. 2008;38(3):362–370. doi: 10.1165/rcmb.2007-0114OC. [DOI] [PubMed] [Google Scholar]
- 24.Chollet-Martin S, Jourdain B, Gibert C, Elbim C, Chastre J, Gougerot-Pocidalo MA. Interactions between neutrophils and cytokines in blood and alveolar spaces during ARDS. Am J Respir Crit Care Med. 1996;154(3 Pt 1):594–601. doi: 10.1164/ajrccm.154.3.8810592. [DOI] [PubMed] [Google Scholar]
- 25.Dreyfuss D, Ricard JD. Acute lung injury and bacterial infection. Clin Chest Med. 2005;26(1):105–112. doi: 10.1016/j.ccm.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 26.Munford RS, Pugin J. Normal responses to injury prevent systemic inflammation and can be immunosuppressive. Am J Respir Crit Care Med. 2001;163(2):316–321. doi: 10.1164/ajrccm.163.2.2007102. [DOI] [PubMed] [Google Scholar]
- 27.Luyt CE, Bouadma L, Morris AC, Dhanani JA, Kollef M, Lipman J, Martin-Loeches I, Nseir S, Ranzani OT, Roquilly A, et al. Pulmonary infections complicating ARDS. Intensive Care Med. 2020;46(12):2168–2183. doi: 10.1007/s00134-020-06292-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36.doi:10.1378/chest.100.6.1619 [DOI] [PubMed]
- 29.Kaya E, Dervisoglu A, Polat C. Evaluation of diagnostic findings and scoring systems in outcome prediction in acute pancreatitis. World J Gastroenterol. 2007;13(22):3090–3094. doi: 10.3748/wjg.v13.i22.3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beck DH, Taylor BL, Millar B, Smith GB. Prediction of outcome from intensive care: a prospective cohort study comparing Acute Physiology and Chronic Health Evaluation II and III prognostic systems in a United Kingdom intensive care unit. Crit Care Med. 1997;25(1):9–15. doi: 10.1097/00003246-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Markgraf R, Deutschinoff G, Pientka L, Scholten T. Comparison of acute physiology and chronic health evaluations II and III and simplified acute physiology score II: a prospective cohort study evaluating these methods to predict outcome in a German interdisciplinary intensive care unit. Crit Care Med. 2000;28(1):26–33. doi: 10.1097/00003246-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Cunnion KM, Weber DJ, Broadhead WE, Hanson LC, Pieper CF, Rutala WA. Risk factors for nosocomial pneumonia: comparing adult critical-care populations. Am J Respir Crit Care Med. 1996;153(1):158–162. doi: 10.1164/ajrccm.153.1.8542110. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Data pre-processing pipeline.
Additional file 2: Imbalanced dataset model. The non-VAP dataset was divided into 100 subgroups, one of which was combined with the VAP dataset to train the model, and then, 100 models were combined into the final model.
Additional file 3: Performance of CPIS-based model in MIMICIII cohort and selection of optimal threshold selection. From CPIS was a score (t) ranged from 0-12 with 6 subcategories. Performance of CPIS was indicated by using AUROC along with the increase of t. Considering t could only be integer, i.e. t=2,3,4,…, t=3 was selected as cut-off since the drop of sensitivity and increase of specificity could be balanced, i.e. the point with largest Youden index.
Additional file 4: List of 42 variables and missing value in study cohort.
Data Availability Statement
The datasets generated and/or analysed during the current study are available in the MIMIC III repository. [https://mimic.mit.edu/].