Abstract
Although isolated central nervous system (CNS) relapses are rare, they may become a serious clinical problem in intensively treated patients with high-risk neuroblastoma (NBL). The aim of this study is the presentation and assessment of the incidence and clinical course of isolated CNS relapses. Retrospective analysis involved 848 NBL patients treated from 2001 to 2019 at 8 centres of the Polish Paediatric Solid Tumours Study Group (PPSTSG). Group characteristics at diagnosis, treatment and patterns of relapse were analysed. Observation was completed in December 2020. We analysed 286 high risk patients, including 16 infants. Isolated CNS relapse, defined as the presence of a tumour in brain parenchyma or leptomeningeal involvement, was found in 13 patients (4.5%; 8.4% of all relapses), all of whom were stage 4 at diagnosis. Isolated CNS relapses seem to be more common in young patients with stage 4 MYCN amplified NBL, and in this group they may occur early during first line therapy. The only or the first symptom may be bleeding into the CNS, especially in younger children, even without a clear relapse picture on imaging, or the relapse may be clinically asymptomatic and found during routine screening. Although the incidence of isolated CNS relapses is not statistically significantly higher in patients after immunotherapy, their occurrence should be carefully monitored, especially in intensively treated infants, with potential disruption of the brain-blood barrier.
Keywords: Central nervous system, Clinical course, Isolated relapse, Metastases, Neuroblastoma
Background
Neuroblastoma (NBL) is the most common extracranial solid tumour in children and one of the most common causes of death in paediatric oncology [1, 2]. The treatment results improved after implementation of new treatment modalities such as high-dose chemotherapy (HDC) followed by autologous stem cell rescue (ASCR), retinoid therapy and immunotherapy, including patients in the high-risk group [3–6]. However, concerns have been raised that intensive treatment may modify the pattern of relapses.
Central nervous system (CNS) involvement at diagnosis and isolated CNS relapses are rare in children with primary extracranial tumours, including NBL. There are limited data presenting brain metastases in children, but clinical reports on different extracranial tumours suggest a frequency of 1.5–4.9% [7–9], with frequency which is even higher in autopsy studies (6–13%) [10, 11]. The estimated 3-year risk of CNS relapses in NBL reaches 8% [12], with CNS being either isolated or one of the sites involved in multiorgan relapse.
The CNS can act as a “sanctuary site” for cancer cells because the blood-brain barrier may impede the penetration of most chemotherapeutic agents [13]. Additionally, antibodies used in immunotherapy do not penetrate into the brain [14], which may influence the frequency of isolated CNS relapses in children undergoing immunotherapy.
The aim of the study is the presentation, assessment of incidence, and assessment of the clinical course of isolated CNS relapses in NBL patients treated at 8 centres of the Polish Paediatric Solid Tumours Study Group (PPSTSG).
Patients and methods
From 1st January, 2001 to 31st December, 2017, 848 patients with NBL were diagnosed at 8 centres of the PPSTSG, including 286 patients with high risk disease. The data were collected till December 2019 and the follow-up was completed in December 2020. The high-risk group included 260 stage 4 patients (including 9 infants with MYCN amplification and 251 patients over 1 year of age, irrespective of MYCN status), 23 patients with stage 2 or 3 with MYCN amplification (including 4 infants), and 3 infants with 4 s MYCN amplified tumours. The mean age at diagnosis was 43.4 months (range 0.2 – 186.3). The characteristics of the group are presented in Table 1.
Table 1.
Characteristics of high-risk neuroblastoma patients
| Number of patients | 848 |
| Number of high-risk patients | 286 |
| Stage 4 patients > 1 year of age | 251 |
| Stage 4 infants with MYCN amplification | 9 |
| Patients with localised disease with MYCN amplification > 1 year of age | 19 |
| Infants with localised MYCN amplified tumours | 4 |
| Stage 4 s with MYCN amplification | 3 |
| MYCN status (n) | |
| Amplification present | 116 |
| No amplification | 119 |
| Unknown | 51 |
| Age (months) | |
| range | 0.8 – 186.3 |
| mean | 43.3 |
| median | 32.4 |
For the high-risk group, children were treated according to HR-NBL-1/SIOPEN (High Risk Neuroblastoma Study 1.0 of SIOP-Europe) protocols [15, 16], including intensive chemotherapy induction (Rapid COJEC – alternating cycles of vincristine, carboplatin and etoposide; vincristine and cisplatin; and vincristine, etoposide and cyclophosphamide; in a case of poor response, 2 cycles of topotecan, vincristine and doxorubicin could have been added) and HDC (busulfan, melphalan or carboplatin, etoposide and melphalan) with ASCR. The details of treatment are reported elsewhere [15, 16]. Surgery, radiotherapy of the primary tumour site (21 Gy) and 13-cis retinoic acid (160 mg/m2/day for 14 days, 6 cycles every 4 weeks) were used as a standard in all patients. From 2012, children also received immunotherapy (ch14.18cho, 100 mg/m2/cycle, 5 cycles). The other protocols used included prolonged chemotherapy mostly according to the Japanese protocol [17] (vincristine, cisplatin, doxorubicin, cyclophosphamide, no HDC) or other individually established chemotherapy protocols, surgery and radiotherapy of the primary tumour site in most cases (dose 21–36.5 Gy). Therapy with 13-cis retinoic acid was introduced depending on clinicians’ decisions.
Altogether, 205 children received therapy according to the HR-NBL-1/SIOPEN protocol (the first group), and 81 patients had different chemotherapy protocols, without HDC (the second group). In 91 children out of 205 (44.4%) treated according to HR-NBL-1/SIOPEN, immunotherapy with ch14.18cho was given in the first line treatment.
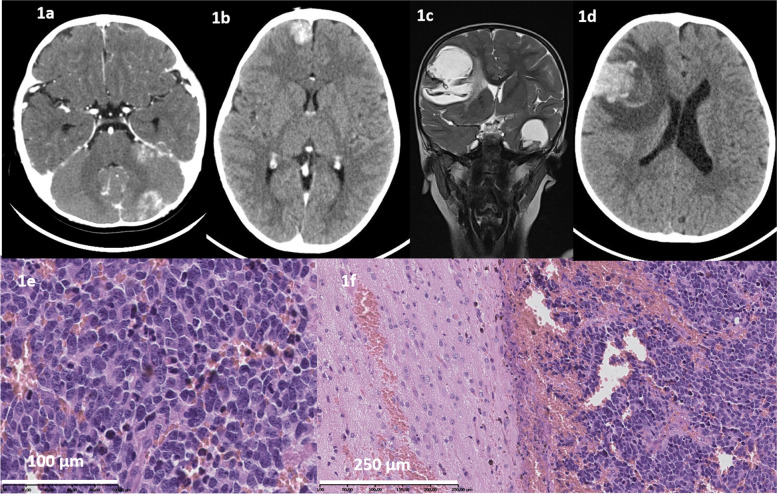
Isolated CNS relapse was defined as parenchymal (Fig. 1a-d) or leptomeningeal involvement, with or without the presence of NBL cells in the cerebrospinal fluid, and/or NBL cells found on histopathological examination of brain tumour or haematoma (Fig. 1e-f). Patients with CNS metastases originating in the skull bones were excluded from the analysis. The relapse was defined as isolated if the CNS was the only site of relapse in patients in complete remission or the relapse was the only new lesion in patients with stable disease at any other sites. All patients had either full evaluation of disease status (imaging, bone marrow examination and I123- or I131- metaiodobenzylguanidine (MIBG) scintigraphy) or post mortem examination to exclude other potential metastatic lesions. Only the first relapses were analysed.
Fig. 1.
a. Computed tomography (CT) of the head, routine examination after induction. Tumour at area of tent of cerebellum, 24 × 14 mm, with possible bleeding to tumour, irregular masses on both sides of tent of cerebellum and in interpedicular cistern. b. In the right frontal lobe, the focal lesion 19 × 19 mm with small calcifications. c. Magnetic resonance (MRI), metastases in both hemispheres, left frontal lobe 46 × 61 mm, left temporal lobe 36 × 27 mm, bleeding to tumour. d. At the right frontal lobe the focal lesion 38 × 35x36mm, with oedema; mass effect – shift of the middle line structures to the left e.) NBL undifferentiated subtype, removed CNS tumor. Hematoxylin–eosin staining, 45 × f. NBL undifferentiated subtype, in removed CNS tumor – on the right site.. Hematoxylin–eosin staining, 20x
The study was carried out in accordance with the Declaration of Helsinki and the recommendations of the Ethics Committee of Jagiellonian University Medical College, Kraków, Poland. All treatment protocols were approved by the Ethics Committee of the Jagiellonian University Medical College and legal representatives signed the informed consent for treatment and data analysis. No additional consent is required for retrospective analysis. Statistical analysis was performed with Statistica Software; the chi-square test and t-test were used, with a significance level 0.05.
Results
Among 286 children with diagnosed HR-NBL, relapse was diagnosed in 161 (56.3%), including 103 (50.2%) relapses in 205 children treated with the SIOPEN protocol and 59 (72.8%) relapses in 81 children treated with conventional chemotherapy. The difference between these 2 groups was statistically significant (p = 0.0001). From 2001 to 2019, isolated CNS relapses were confirmed in 13 patients (8.4% of all relapses). Incidence of isolated CNS relapses was 10.7% in the first group (11 out of 103 relapses) and 3.4% in the second group (2 out of 59 relapses). The difference between groups was not statistically significant (p = 0.1).
Taking into consideration the employment of immunotherapy, 28 (30.8%) relapses occurred in 91 patients treated with immunotherapy and in 118 (63.1%) of 195 patients treated without immunotherapy in the first line treatment. The difference between groups was statistically significant (p < 0.0001). Six (6.6%) cases of isolated CNS relapse were diagnosed among 91 patients in whom immunotherapy was employed in the first line therapy and 7 cases (3.6%) among 195 patients without immunotherapy in the first line treatment. The difference between the groups was not statistically significant (p = 0.26). In the group treated with SIOPEN protocols, the CNS relapse occurred before the time of scheduled immunotherapy in five patients, during immunotherapy in three patients, and after immunotherapy (3–6 months) in three patients.
Clinical data on patients with isolated CNS relapse are presented in Tables 2 and 3.
Table 2.
Patients with isolated relapse in CNS group characteristics at the time of the first diagnosis
| Pts | Age at Dx (y, m) | Gender | Stage at Dx | Primary site Metastases at diagnosis |
MYCN amplification/ Type of pathology |
Skull bones involvement at Dx | First line therapy |
|---|---|---|---|---|---|---|---|
| 1 | 2y 2 m | F | 4 |
Adrenal gland Bones, BM, LN |
Yes UH |
Yes |
HR-NBL SIOPEN No anti-GD2 |
| 2 | 2y 2 m | M | 4 |
Retroperitoneal space Bones, BM, LN |
Yes UH |
Yes – intracranial penetration |
HR-NBL SIOPEN No anti-GD2 |
| 3 | 5 m | F | 4 |
Adrenal gland, Bones, BM, liver, kidneys, lungs, chest wall |
Yes UH |
No |
HR-NBL SIOPEN No anti-GD2 |
| 4 | 3 m | F | 4 |
Adrenal gland Bones, BM, LN, lungs, liver, kidneys |
Yes UH |
No |
HR-NBL SIOPEN With anti-GD2 |
| 5 | 2y 6 m | F | 4 |
Adrenal gland Bones, BM |
Not evaluated UH |
Yes | Conventional chemotherapy |
| 6 | 3y 7 m | F | 4 |
Mediastinum Bones, BM, LN, CSN, pleura |
No UH |
Yes – CNS infiltration | HR-NBL SIOPEN with anti-GD2 |
| 7 | 2y 7 m | M | 4 |
Adrenal gland Bones, BM, LN |
No UH |
Yes | Conventional chemotherapy |
| 8 | 10 m | M | 4 |
Retroperitoneal space BM |
Yes UH |
No |
HR-NBL SIOPEN No anti-GD2 |
| 9 | 11 m | M | 4 |
Adrenal gland Bones, BM, LN |
Yes UH |
Yes – infiltration of skull base |
HR-NBL SIOPEN With anti-GD2 |
| 10 | 2y 4 m | F | 4 |
Retroperitoneal space Bones, BM |
No FH |
Yes |
HR-NBL SIOPEN No anti-GD2 |
| 11 | 1y 8 m | M | 4 |
Adrenal gland LN, mediastinum, bones, BM |
Yes UH |
Yes |
HR-NBL SIOPEN With anti-GD2 |
| 12 | 1y 11 m | M | 4 |
Adrenal gland LN, bones, BM |
Yes UH |
Yes – penetrating to CNS |
HR-NBL SIOPEN With anti-GD2 |
| 13 | 6y 1m2 | M | 4 |
Retroperitoneal space Bones, BM |
No UH |
No |
HR-NBL SIOPEN With anti-GD2 |
Dx diagnosis, y year, m month, M male, F female, UH unfavourable histopathology, FH favourable histopathology, BM bone marrow, LN lymph nodes
Table 3.
CNS relapse presentation, treatment, and course of disease
| Pt | Time from diagnosis to CNS relapse (months) | Relapse presentation | Relapse therapy | Disease status and time to relapse | Disease course after relapse |
|---|---|---|---|---|---|
| 1 | 5 |
Facial nerve palsy, strabismus Tumour in CT NBL cells in CSF and in removed tumour |
Surgery, RTX, chemotherapy, intrathecal chemotherapy | CR; on treatment after induction and surgery | Local progression 6 months from relapse, death 7 months from relapse |
| 2 | 6 |
Intracranial bleeding No tumour in CT NBL cells in removed tumour |
Surgery | CR; on treatment – before HDC | Died 2 weeks after event |
| 3 | 5 |
Accidental diagnosis CT: infiltration of meninges, bleeding into the tumour |
Chemotherapy, intrathecal chemotherapy |
PR; on treatment - after induction |
Died 3 weeks after event bleeding into tumour |
| 4 | 12 |
Intracranial bleeding No radiological symptoms NBL in postmortem examination |
No therapy |
CR; on treatment - therapy of MRD |
Died 5 days after event |
| 5 | 8 |
Headache, nausea, vomiting Tumour in CT NBL cells in removed tumour |
Surgery, radiotherapy, chemotherapy, 13 cis RA | CR; after end of treatment | CR in CNS; disseminated bone relapse 39 months after relapse; no 3rd line treatment. Died of disease |
| 6 | 15 | Facial nerve palsy | Chemotherapy | PR; on treatment – therapy of MRD | Local progression and death 3 months after relapse |
| 7 | 26 |
Headache, nausea, vomiting Tumour in CT |
Chemotherapy, radiotherapy, no surgery (tumour regression on chemotherapy) | CR; after end of treatment | Alive in CR > 9 years after relapse |
| 8 | 8 |
Intracranial bleeding No radiological symptoms NBL in postmortem examination |
No therapy | CR; on treatment – after radiotherapy | Died 2 days after event |
| 9 | 20 |
Headache, nausea, vomiting 2 tumours in CT NBL cells in removed tumour |
Surgery, chemotherapy, radiotherapy, ibritumomab | CR; 3 months after end of treatment | Alive in CR, 2,5 years after relapse |
| 10 | 8 |
Intracranial bleeding No radiological symptoms NBL in postmortem examination |
No therapy | PR; on treatment – after HDC, before ASCR | Died 7 days after event |
| 11 | 16 |
Headache 3 metastases in CT |
No therapy | CR, during immunotherapy | Died of disease 3 months after event |
| 12 | 14 |
No symptoms; mild headache on a day of planned CT Tumour on CT – routine screening |
Surgery, chemotherapy, radiotherapy | CR: during immunotherapy | Alive, 2nd CNS relapse after 9 months |
| 13 | 20 |
Headache, vomiting Infiltration of meninges in MRI, NBL cells in cerebrospinal fluid |
Chemotherapy, radiotherapy | CR; 6 months after end of immunotherapy | Died of disease progression |
Dx diagnosis, NBL neuroblastoma, CNS central nervous system, CT computed tomography, RTX radiotherapy, CR complete remission, PR partial remission, MRD minimal residual disease, MRI magnetic resonance imaging
Clinical and biological data on children with isolated CNS relapse
In 12 out of 13 patients, MYCN status is known. Eight (66.7%) out of twelve patients had MYCN amplification. All patients had unfavourable histopathology at diagnosis. Although all patients were stage 4 at the time of diagnosis, the metastatic pattern was not constant. Nine (69.2%) out of 13 patients had skull bone involvement and in 3 patients (23.1%), the CNS was primarily involved by continuity with skull bone infiltration.
Pathologic verification of CNS lesions at relapse was obtained in 11 patients, including four with NBL cells found in haematomas, three with NBL cells presented in cerebrospinal fluid and five with histopathological evaluation of tissue received after tumour removal (one of them had also previous positive CSF evaluation).
Characteristics of CNS relapse
The time from the diagnosis to relapse was 5–26 months (mean 12.5 months, median 12.0 months).
The time to relapse was much shorter in young children with intracranial bleeding being the first presentation of relapse or accidental relapse diagnosis (5–12 months, mean 7.2) than in children with symptomatic relapse (8–26 months, mean 17.4). The difference is statistically significant (p = 0.0002).
Eight relapses were diagnosed in 16 infants with MYCN amplification, seven in stage 4 and one in stage 3 patients. Four of them (50%), all in stage 4 infants, were isolated CNS relapses. In three infants with isolated CNS relapse, ASCR was not carried out because of disease progression that occurred during intensive induction chemotherapy or just before planned HDC.
Clinical manifestation of isolated central nervous system relapse
In intensively treated patients, especially the youngest ones, isolated CNS involvement may be asymptomatic or rapid symptoms of intracranial bleeding may occur, without previous symptoms of CNS involvement.
Intracranial bleeding was the first clinical symptom in 4 (30.2%) out of 13 patients, including three infants, all with MYCN amplification, with acute symptoms of increased intracranial pressure and early invagination. Two of them were diagnosed before planned ASCT and 2 either just before or during immunotherapy. Imaging (computed tomography (CT) and/or magnetic resonance imaging (MRI)) done in three children revealed no evident tumour mass, only intracranial bleeding, and in 1 patient there was a suspicion of bleeding into the tumour. Assessment of meninges on imaging was difficult as no contrast was given. The presence of disseminated neuroblastoma cells in haematoma together with infiltration of meninges with NBL cells was revealed during histopathological examinations in all patients. One patient had a surgery at the time of symptom occurrence, and NBL infiltration was found during post mortem examination in three patients, as rapid progression of invagination and brain death occurred. In all these patients, the symptoms progressed very rapidly. Two of them were hospitalised at the time of episode, the other one, with no symptoms, was seen in an outpatient clinic on the day of the episode. Only one out of four had a mild headache a few days before the episode which was interpreted to be caused by teething. All but one patient was younger than 18 months at the time of relapse, so the potential symptoms were difficult to assess. No CNS lesions were visible in MIBG imaging or/and in CT/MRI done at any time before the relapse.
In two out of four patients, there was an episode of mild head trauma on the day of bleeding, such as falling down while walking (13 and 15 months old at the time of relapse). In both cases, the accident happened in the presence of parents with no loss of consciousness or any other symptoms directly after the accident.
In 2 out of 13 patients (15.4%), there were no clinical symptoms of CNS involvement and the relapse was diagnosed during routine examinations after induction chemotherapy (stage 4 infant with MYCN amplification, leptomeningeal involvement (Fig. 1a) and after 2 cycles of anti-GD2 (stage 4 infant with MYCN amplification at diagnosis, only mild headache on the day of planned CT). The first patient, in spite of the chemotherapy provided, had bleeding to the tumour and died in the course of this episode three weeks after CNS relapse. In the second one, a complete remission was obtained after surgery and chemotherapy, but the second isolated CNS relapse occurred during treatment at the time of the last evaluation.
The other 7 (53.8%) children presented with neurological symptoms of increased intracranial pressure (nausea, vomiting, headache) or focal symptoms, mainly disturbances of cranial nerves (strabismus, paresis of the facial nerve). Symptoms lasted for a few days before the diagnosis and were the reason for performing CNS imaging. All of them were over 18 months old at the time of diagnosis and the time to progression was longer (8–26 months, mean 17.4 months from the first diagnosis).
Only in 3 out of 13 patients the time to relapse was 20 months or longer. including both patients who survived and who are disease free. One of them is alive without the disease > 5 years from the relapse diagnosis and the second one 2.5 years from the relapse diagnosis. The first patient received prolonged chemotherapy as the first line treatment, without HDC, and CNS relapse was treated with chemotherapy according to a brain tumour protocol and radiotherapy without surgery as the tumour regressed after treatment. The second one received the HR-NBL-1/SIOPEN protocol with immunotherapy as the first line treatment, and CNS relapse was treated with surgery, chemotherapy, RTX, and intraventricular compartmental radioimmunotherapy.
Discussion
There are few data reported in the literature on the incidence of isolated CNS relapses in patients with high-risk NBL. The previously reported rate of incidence of CNS relapses was from 2.3% [18] to 16% [19] and up to 25% in small institution studies [20], with a mean of 3.8% [12]. However, most studies did not report only isolated CNS relapses. It is estimated that these account for about 50% of all CNS relapses [12, 18]. In the German Childhood Cancer Registry, 85 patients with CNS involvement were identified, including 57 with isolated CNS relapse [21].
Among 127 patients with stage 4 NBL over one year of age diagnosed at Memorial-Sloan-Kettering, eight patients (6%) developed CNS relapses. In this cohort, there was a tendency towards a higher number of CNS relapses among patients treated with immunotherapy without HDC than in patients that received HDC without immunotherapy (7 out of 67 vs 1 out of 60, respectively) [22]. The retrospective analysis performed by the Children’s Oncology Group showed CNS relapses at first recurrence in 8 out of 434 patients (2%) [18], and in the French cohort, CNS relapses were diagnosed in 8 out of 127 patients (6%) [12]. In the German study, the incidence of CNS relapses was reported in 49 out of 451 patients (11%) treated with HDC [23]. In the Chinese series, brain metastases occurred in 11 out of 106 patients (10.4%), accounting for 20% of all relapses [24]. The frequency of CNS relapses seems not to change over time (1985–2000 [12], 1990–2010 [21]). However, the influence of immunotherapy is still unclear. There are data supporting the thesis that by reducing the incidence of systemic relapses, the number of isolated CNS relapses increases [25], but in the SIOPEN analysis the increased risk of CNS relapse after immunotherapy was not confirmed [26]. In our study, although the incidence of isolated CNS relapses was higher in intensively treated patients and after immunotherapy, the difference was not statistically significant.
The studies referred to above, except for Matthay et al. [12], reported on data from studies including children over one year of age at the time of diagnosis. As a relatively high number of infants were observed in our cohort, and in this group isolated CNS relapses were 50% of all relapses, the number of CNS relapses may be underestimated in the whole high-risk group, also including patients under one year of age with MYCN amplification. Additionally, in some studies, only patients who received HDC were assessed [23], which excluded early relapses, which seem to be more common in young intensively treated patients.
In the current study, we presented 13 patients with isolated CNS neuroblastoma relapse. The pattern of relapses seems to change with treatment intensification, resulting in early relapses, taking the form of intracranial bleeding, especially in infants.
There are no clear risk factors for isolated CNS relapse. The data in the literature are inconsistent [18, 22]. Identification of statistically significant risk factors for CNS relapse was presented in two previously published studies. The risk factors for CNS recurrence reported by the previous research were lumbar puncture at diagnosis and LDH in one cohort [22] or age, lumbar puncture and MYCN amplification in another cohort [12]. In our group, disseminated disease in infants with MYCN amplification was the risk factor for the early CNS relapse (isolated CNS relapse was found in 25% of all MYCN amplified infants). HDC alone, probably, does not prevent CNS relapse [27]. In the presented data, occurrence of isolated CNS relapses is slightly higher in intensively treated patients with the employment of HDC, but the difference is not statistically significant.
Treatment of this kind of relapse is not established. Chemotherapy has been previously reported to be effective in single cases of patients with CNS NBL relapses, especially when there was the possibility of removing the tumour [24, 28]. With the employment of new treatment modalities, such as a protocol employing intrathecal radiolabelled antibodies [29], this kind of relapse is potentially curable. Moreover, therapy with intrathecal radiolabelled antibodies allows for the reduction of the radiotherapy dosage, which is extremally important in the context of expected toxicities, especially in small children [30].
Results of treatment with chemotherapy and radiotherapy are poor. One of the factors that may influence the prognosis is time to relapse. In our group, only in 3 patients the time to relapse was over 20 months, including 2 patients who survived. In the SIOPEN study, the median time to CNS recurrence from diagnosis was also shorter in comparison to relapses at other sites (p = 0.05) [26]. The longer time to relapse seems to be a better prognostic factor, also for the whole group of NBL patients, independently on the site of relapse [31].
In all reported patients, the parenchymal or leptomeningeal involvement were isolated settings. This supports the theory that CNS metastases are mainly blood-borne [22, 29] and that they may be related to genetic alterations of NBL cells during intensive therapy [12, 32, 33]. Specific genomic lesions, like 18q22.1 gain, may predispose to CNS metastases [34]. These lesions are recurrently acquired during metastatic progression. The TERT gene (5p), associated with telomere maintenance and poor prognosis in NBL [35], is one of the candidate genes associated with CNS involvement [34]. Patients with CNS relapse also have a different specific pattern of microRNA expression, with downregulation of miR-29a as a potential biomarker, potentially playing a role in CNS progression [36]. NBL cells penetrating into the CNS in a haematogenous way may keep their proliferative potential and may be a source of metastases [19, 29, 37]. In some studies, increased incidence of CNS metastases was observed after chemotherapy intensification [22, 28]. Our results also suggest that the natural history of the disease may be changed by intensive treatment. The reason for this may be the disruption of the blood–brain barrier, especially in very young children.
The symptoms of relapse are as described in previous reports. However, it’s important to underline that symptoms are not always present, especially in young children. In our setting, we found patients who either had no clinical symptoms and relapse was found on routine imaging (two patients) or who had severe neurological symptoms of bleeding and invagination was the first clinical presentation (four patients). Intraparenchymal haematoma occurring prior to radiologically detectable CNS metastases are rarely described in the literature [38].
Disease control in other tissues may be improved in the case of carrying out HDC followed by ASCR and immunotherapy [39]. It may decrease the incidence of disseminated relapses and increase the number of isolated relapses, including CNS relapses [25]. The diagnosis of isolated CNS relapse may be a more difficult challenge than disseminated relapses involving the CNS. Routine CNS examination must be taken into consideration at the scheduled time of disease assessment, even without having clear symptoms of CNS involvement reported. Also, whenever neurological symptoms occur during therapy, the relapse should be excluded. MIBG examinations performed at routine time points may not reveal metastases. Evaluation of CNS relapses in MIBG scintigraphy may be difficult; the CNS lesions may be interpreted as skull lesions and leptomeningeal infiltration may be not seen. Moreover, it was described in the literature that MIBG scintigraphy may be negative in confirmed relapses, even in nodular lesions [12]. Although NBL cells are found in histopathology at the time of intracranial bleeding, there may be no radiological symptoms of tumours present during radiological examinations, especially if CT/MRI are carried out without contrast.
This is a retrospective multicentre study, so the authors cannot exclude that some cases of CNS relapses might have been not reported or diagnosed, which is a limitation of the study. However, in all centres the routine imaging of CNS was performed at the most important time points of response evaluation, which let diagnose also asymptomatic relapses.
Conclusions
CNS as a “pharmacological sanctuary” may be a new challenge for relapse diagnosis and treatment, especially with immunotherapy, significantly decreasing the risk of relapses in other organs. Brain evaluation should be recommended for all patients at the time of diagnosis, the time of relapse and at scheduled time points crucial for further therapeutic decisions. This should be also always performed when neurological symptoms occur before they can be interpreted as therapy toxicities, especially during immunotherapy [40]. Stage 4 infants with MYCN amplification must be taken into special consideration, as isolated CNS relapse may occur earlier during the course of therapy in this group of patients and have unspecific clinical presentation.
Acknowledgements
The authors would like to thank Lukasz Wyrobek, MD, from the Radiology Department of University Children’s Hospital in Krakow and Grazyna Drabik, MD and Damian Mlynarski, MD, from the Pathology Department of University Children’s Hospital in Krakow for a permission to use the pictures, as well as all Paediatric Oncology Departments associated in the Polish Paediatric Solid Tumours Study Group for cooperation and providing patients’ data.
Abbreviations
- CNS
Central nervous system
- NBL
Neuroblastoma
- PPSTSG
Polish Paediatric Solid Tumours Study Group
- HDC
High dose chemotherapy
- ASCR
Autologous stem cell transplantation
- HR-NBL-1/SIOPEN
High Risk Neuroblastoma Study 1.0 of SIOP-Europe
- SIOPEN
International Society of Paediatric Oncology European Neuroblastoma Research Network
- Gy
Grey
- CT
Computed tomography
- MRI
Magnetic resonance
- Dx
Diagnosis
- BM
Bone marrow
- LN
Lymph nodes
- UH
Unfavourable histopathology
- FH
Favourable histopathology
- Y
Years
- m
Months
- M
Male
- F
Female
- RTX
Radiotherapy
- CR
Complete remission
- PR
Partial remission
- MRD
Minimal residual disease
- MIBG
Meta-iodobenzylguanidine
Authors’ contributions
Conception and design of the study: AW, WB. Data collection: AW, JS, MH, MS, ZG, JG, MU, MP, SJ. Data analysis and interpretation, initial manuscript draft: AW. The content was reviewed, edited, and approved by all authors.
Funding
There were no funding sources for this work.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to General Data Protection Regulations but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was carried out in accordance with the Declaration of Helsinki and the recommendations of the Ethics Committee of Jagiellonian University Medical College, Kraków, Poland. All treatment protocols were approved by the Ethics Committee of the Jagiellonian University Medical College and legal representatives signed the informed consent for treatment and data analysis. Patients or guardians of patients provided informed consent for treatment, including data analysis. No additional consent was requested for retrospective analysis.
Consent for publication
Not applicable.
Patients or guardians of patients provided informed consent for treatment, including data analysis. No additional consent was requested for retrospective analysis.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Coughlan D, Gianferante M, Lynch CF, Stevens JL, Harlan LC. Treatment and survival of childhood neuroblastoma: Evidence from a population-based study in the United States. Pediatr Hematol Oncol. 2017;34:320–330. doi: 10.1080/08880018.2017.1373315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balwierz W. Nerwiak zarodkowy współczulny. In: Pietrzyk JJ, Kwinta P, eds. Pediatria. 1st ed.: Wydawnictwo UJ Krakow, 2018: 551–562.
- 3.Matthay KK, Villablanca JG, Seeger RC, Stram DD, Harris RE, Ramsay NK, Swift P, Shimada H, Black T, Brodeur GM, Gerbing RB, Reynolds P. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. N Engl J Med. 1999;341(16):1165–73. doi: 10.1056/NEJM199910143411601. [DOI] [PubMed] [Google Scholar]
- 4.Berthold F, Boos J, Burdach S, Ertmann R, Henze G, Hermann J, Klingebiel T, Kremens B, Schillin FH, Schrappe M, Simon T, Hero B. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomised controlled trial. Lancet Oncol. 2005;6(9):649–658. doi: 10.1016/S1470-2045(05)70291-6. [DOI] [PubMed] [Google Scholar]
- 5.Yu AL, Gilman AL, Ozkaynak MF, London WB, Kreissman SG, Chen HX, Smith M, Anderson B, Villablanca JG, Matthay KK, Shimada H, Grupp SA, Seeger R, Reynold P, Buxton A, Reisfweld RA, Gillies SD, Cohn SL, Marris JM, Sondel PM. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med. 2010;363(14):1324–1334. doi: 10.1056/NEJMoa0911123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ladenstein R, Pötschger U, Valteau-Couanet D, Luksch R, Castel V, Yaniv I, Laureys G, Brock P, Michon JM, Owens G, Trahair T, Chan GCF, Rund E, Schroeder H, Beck-Popovic M, Schreier G, Loibner H, Ambros P, Holmes K, Castellani MR, Gaze MN, Garaventa A, Pearson ADJ, Lode HN. Interleukin 2 with anti-GD2 antibody ch1418/CHO (dinutuximab beta) in patients with high-risk neuroblastoma (HR-NBL1/SIOPEN): a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018;19(12):1617–29. doi: 10.1016/S1470-2045(18)30578-3. [DOI] [PubMed] [Google Scholar]
- 7.Kebudi R, Ayan I, Gorgun O, Agaoglu FY, Vural S, Darendeliler E. Brain metastasis in pediatric extracranial solid tumours: survey and literature review. J Neurooncology. 2005;71:43–48. doi: 10.1007/s11060-004-4840-y. [DOI] [PubMed] [Google Scholar]
- 8.Paulino AC, Nguyen TX, Barker JL. Brain metastasis in children with sarcoma, neuroblastoma and Wilms’ tumour. Int J Radiation Biol Phys. 2003;57:177–183. doi: 10.1016/S0360-3016(03)00502-9. [DOI] [PubMed] [Google Scholar]
- 9.Stefanowicz J, Izycka-Swieszewska E, Szurowska. Bien E, Szarszewski A, Liberek A, Stempniewicz M, Kloc W, Adamkiewicz-Drozynska E. Brain metastases in paediatric patients: characteristics of a patient series and review of the literature. Folia Neuropahol. 2011;49:271–81. [PubMed] [Google Scholar]
- 10.Graus F, Walker RW, Allen JC. Brain metastases in children. J Pediatr. 1983;103:558–561. doi: 10.1016/S0022-3476(83)80583-6. [DOI] [PubMed] [Google Scholar]
- 11.Vanucci RC, Baten M. Cerebral metastatic disease in childhood. Neurology. 1974;24:981–985. doi: 10.1212/WNL.24.10.981. [DOI] [PubMed] [Google Scholar]
- 12.Matthay KK, Brisse H, Couanet D, Couturier J, Bernard J, Maseri V, Edenne V, Lumbros J, Valtaeau-Couanet D, Michon J. Central nervous system metastases in neuroblastoma. Radiologic, clinical, and biological features in 23 patients. Cancer. 2003;98:155–65. doi: 10.1002/cncr.11448. [DOI] [PubMed] [Google Scholar]
- 13.Deeken JF, Loescher W. The Blood-Brain Barrier and Cancer: Transporters, Treatment, and Trojan Horses. Clin Cancer Res. 2007;13:1663–1674. doi: 10.1158/1078-0432.CCR-06-2854. [DOI] [PubMed] [Google Scholar]
- 14.Razpotnik R, Novak N, Čurin Šerbec V, Raicevic U. Targeting malignant brain tumours with antibodies. Front Immunol. 2017;8:1181. doi: 10.3389/fimmu.2017.01181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.High Risk Neuroblastoma Study of SIOP-Europe (SIOPEN). www.clinicaltrials.gov
- 16.Ladenstein R, Poetschger U, Pearson ADJ, Brock P, Luksch R, Castel V, Yaniv I, Papadakis V, Laureys G, Malis J, Balwierz W, Rund E, Kogner P, Schroeder H, Forjaz de Lacerda A, Beck Popovic M, Bician P, Garami M, Trahair T, Canete A, Ambros PM, Holmes K, Gaze M, Schreier G, Garaventa A, Vassal G, Michon J, ValteauCuouanet D. Busulfan and melphalan versus carboplatine, etoposide and melphalan as high-dose chemotherapy for high-risk neuroblastoma (HR-NBL1/SIOPEN): an international randomized, multi-arm, open-label, phase 3 trial. Lancet Oncol. 2017;18:505–514. doi: 10.1016/S1470-2045(17)30070-0. [DOI] [PubMed] [Google Scholar]
- 17.Iwafuchi M, Utsumi J, Tsuschida Y, Kaneko M, Matsuyana S, Ohmnuma N, Taguchi N, Mugishima H, Yokoyana J, Sasaki S, Yoshida A, Nakagahara N, Fukuzara M, Suita S. Evaluation of patients with advanced neuroblastoma surviving more than 5 years after initiation of an intensive Japanese protocol: A report from the study group of Japan for treatment of advanced neuroblastoma. Med Ped Oncol. 1996;27:515–520. doi: 10.1002/(SICI)1096-911X(199612)27:6<515::AID-MPO2>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 18.DuBois SG, Kalika Y, Lukens JN, Brodeaur GM, Seeger RC, Atkinson JB, Haase GM, Black CT, Perez C, Shimada H, Gebing R, Shram DO, Matthay KK. Metastatic sites in stage IV and IVs neuroblastoma correlate with age, tumour biology, and survival. J Pediatr Hematol Oncol. 1999;21:181–189. doi: 10.1097/00043426-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Blatt J, Fitz C, Mirro J. Recognition of central nervous system metastases in children with metastatic primary extracranial neuroblastoma. Ped Hematol Oncol. 1997;14:233–241. doi: 10.3109/08880019709009493. [DOI] [PubMed] [Google Scholar]
- 20.Astigarraga I, Lejarreta R, Navajs A, Fernandez-Teijero A, Imaz I, Bezanilla JL. Secondary central nervous system metastases in children with neuroblastoma. Med Pediatr Oncol. 1996;27:529–533. doi: 10.1002/(SICI)1096-911X(199612)27:6<529::AID-MPO4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 21.Berthold F, Hoemberg M, Baadsgaard O. Neuroblastoma metastatic to the central nervous system: Survival analyses from the German Childhood Cancer Registry and the literature. J Clin Oncol. 2017;35(15_suppl):105555. doi: 10.1200/JCO.2017.35.15_suppl.10555. [DOI] [Google Scholar]
- 22.Kramer K, Kushner B, Heller G, Cheung NK. Neuroblastoma metastatic to the central nervous system. The memorial sloan-kettering cancer center experience and a literature review. Cancer. 2001;91:1510–9. doi: 10.1002/1097-0142(20010415)91:8<1510::AID-CNCR1159>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 23.Simon T, Berthold F, Borkhardt. Kremens B, De Cordis B, Hero B. Treatment and outcome of patients with relapses, high-risk neuroblastoma: results of German trials. Pediatr Blood Cancer. 2011;56:578–583. doi: 10.1002/pbc.22693. [DOI] [PubMed] [Google Scholar]
- 24.Zhu J, Wang J, Zhen ZJ, Lu SY, Zhang F, Sun FF, Li PF, Huang JT, Cai RQ, Sun XF. Brain metastasis in children with stage 4 neuroblastoma after multidisciplinary treatment. Chin J Cancer. 2015;34:49. doi: 10.1186/s40880-015-0038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheung NK, Cheung IY, Kushner BH, Ostrovnaya I, Chamberlain E, Kramer K, Modak S. Murine anti-GD2 monoclonal antibody 3F8 combined with granulocyte-macrophage colony-stimulating factor and 13-cis retinoic acid in high-risk patients with stage 4 neuroblastoma in first remission. J Clin Oncol. 2012;30:3264–3270. doi: 10.1200/JCO.2011.41.3807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berlanga P, Pasqualini C, Poetschger U, Sanguesa C, Castellani MR, Canete A, Luksch R, Elliot M, Schreier G, Kropf M, Morgenstern D, Papadakis V, Ash S, Ruud E, Brock P, Wieczorek A, Kogner P, Trahair T, Ambros P, Boterberg T, Castel V, Valteau-Couanet D, Ladenstein R. Central nervous system relapse in high-risk stage 4 neuroblastoma: The HR-NBL1/SIOPEN trial experience. Eur J Cancer. 2021;144:1–8. doi: 10.1016/j.ejca.2020.10.020. [DOI] [PubMed] [Google Scholar]
- 27.Kushner BH, Kramer K, Modak S, Kernan NA, Reich LM, Paris K, Cheung NKV. Topotecan, thiotepa and carboplatin for neuroblastoma: failure to prevent relapse in the central nervous system. Bone Marrow Transplantaion. 2016;37:271–276. doi: 10.1038/sj.bmt.1705253. [DOI] [PubMed] [Google Scholar]
- 28.De Ioris MA, Crocoli A, Contoli B, et al. Local control in metastatic neuroblastoma in children over 1 year of age. BMC Cancer. 2015;15:79. doi: 10.1186/s12885-015-1082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kramer K, Kushner BH, Modak S, Pandit-Taskar N, Smith-Jones P, Zanzonico P, Humm JL, Xu H, Wolden SL, Souweidare MM< Larson SM, Cheung NKV. Compartmental intrathecal radioimmunotherapy: results for treatment for metastatic CNS neuroblastoma. J Neurooncol. 2010;97(3):409–418. doi: 10.1007/s11060-009-0038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luo LY, Kramer K, Cheung NV, Kushner BH, Modak S, Basu EM, Roberts SS, Wolden SL. Reduced-dose craniospinal irradiation for central nervous system relapsed neuroblastoma. Pediatr Blood Cancer. 2020;67(9):e28364. doi: 10.1002/pbc.28364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.London WB, Castel V, Monclair T, Ambros PF, Pearson AD, Cohn SL, Berthold F, Nakagawara A, Ladenstein RL, Iehara T, Matthay KK. Clinical and biologic features predictive of survival after relapse of neuroblastoma: a report from the International Neuroblastoma Risk Group project. J Clin Oncol. 2011;29(24):3286–92. doi: 10.1200/JCO.2010.34.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palasis S, Morris J, Egelhoff JC. Central nervous system relapse following bone marrow transplantation in stage IV neuroblastoma. Pediatr Hematol Oncol. 1999;16:443–452. doi: 10.1080/088800199277001. [DOI] [PubMed] [Google Scholar]
- 33.Tonini G. Growth, progression and chromosome instability of neuroblastoma: a new scenario of tumorigenesis? BMC Cancer. 2017;17:20–25. doi: 10.1186/s12885-016-2986-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cobrinik D, Ostrovnaya I, Hassimi M, Tickoo SK, Cheung IM, Cheung NKV. Recurrent pre-existing and acquired DNA copy number alterations, including focal TERT gains, in neuroblastoma central nervous system metastases. Genes Chromosom Cancer. 2013;52:1150–1166. doi: 10.1002/gcc.22110. [DOI] [PubMed] [Google Scholar]
- 35.Roderwieser A, Sand F, Walter E, Fisher J, Gecht J, Bartenhagen G, Ackermann S, Otle F, Welte A, Kahlert Y, Lieberz D, Hertwig F, Reinhardt HC, Simon P, Peifer M, Ortmann M, Budner R, Hero B, O’Sullivan RJ, Berthold F, Fischer M. Telomerase is a prognostic marker of poor outcome and a threrapeutic target in neuroblastoma. JCO Precis Oncol. 2019;3:1–20. doi: 10.1200/PO.19.00072. [DOI] [PubMed] [Google Scholar]
- 36.Cheung IY, Farazi TA, Ostrovnaya I, Xu H, Tran H, Mihailovic A, Tuschl T, Cheung NKV. Deep microRNA sequencing reveals downregulation of miR-29a in neuroblastoma central nervous system metastasis. Genes Chromosom Cancer. 2014;53:804–814. doi: 10.1002/gcc.22189. [DOI] [PubMed] [Google Scholar]
- 37.Kellie SJ, Hayes FA, Bowman L, Kovnar EH, Langstan J, Jenkinsc J, 3rd, Pao WJ, Ducos R, Green AA. Primary extracranial neuroblastoma with central nervous system metastases characterization by clinicopathologic findings and neuroimaging. Cancer. 1991;68:1999–2006. doi: 10.1002/1097-0142(19911101)68:9<1999::AID-CNCR2820680926>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 38.Okura H, Yatomi K, Saito Y, Kasuga C, Ishii H, Karagioza K, Miyajima M, Arai H. Unexpected intraparenchymal hematoma caused by brain metastasis in a patient with neuroblastoma: case report. Med Chir (Tokyo) 2011;51(11):784–788. doi: 10.2176/nmc.51.784. [DOI] [PubMed] [Google Scholar]
- 39.Simon T, Hero B, Faldum A, et al. Long term outcome of high-risk neuroblastoma patients after immunotherapy with antibody ch14.18 or oral metronomic chemotherapy. BMC Cancer. 2011;11:21–6. [DOI] [PMC free article] [PubMed]
- 40.Wieczorek A, Manzitti C, Garaventa A, Gray J, Papadakis V, Valteau-Couanet D, Zachwieja K, Poetschger U, Pribill I, Fiedler S, Ladenstein R, Lode HN. Clinical phenotype and management of severe neurotoxicity observed in patients with neuroblastoma treated with dinutuximab beta in clinical trials. Cancers. 1919;2022:14. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due to General Data Protection Regulations but are available from the corresponding author on reasonable request.