Abstract
Background
Patellofemoral (PF) instability is a syndrome involving several factors and conditions. Trochlear dysplasia (TD) has been shown to be the feature most frequently diagnosed in patients with OPI (Objective Patellar Instability). Even the patella might have an altered shape. Articulating during growth with an abnormal trochlea might lead the patellar posterior surface to modify accordingly, becoming congruent with the trochlear shape. A mismatch between the two articulating surfaces has a role in patellofemoral dislocations.
Rarely and in case of a highly dysplastic patella, reshaping only the trochlear groove might lead subsequently to an incongruence between the two bones.
When isolated sulcus-deepening trochleoplasty does not restore a congruent patellofemoral tracking tested perioperatively, further surgical procedures might be required.
Methods
A medial closing wedge patellar osteotomy (MCWPO) added to sulcus deepening trochleoplasty should be performed to create a congruent patellofemoral joint.
Indications for this procedure are Wiberg type III or IV patella with an intraoperative abnormal patellar tracking after the sulcus deepening trochleoplasty procedure has been concluded.
Results
From January 2012 to August 2020, 21 (6 right and 15 left knees) sulcus deepening trochleoplasties with a concomitant medial closing wedge patellar osteotomy have been performed. The mean follow up was 35,25 months (ranging from 10 to 60 months). The average Kujala, IKDC and Lysholm score were respectively 70,14 ± 15,51; 55,75 ± 7,12 and 77,12 ± 14,80. No further patellar dislocation has been assessed in those patients during follow up.
Conclusion
This technique has shown good and promising clinical outcomes and should be considered when treating patients with a still unsatistactory patellofemoral tracking after the sulcus deepening trochleoplasty has been performed due to a patella-trochlea shape mismatch.
Keywords: Patellar closing wedge, Patellar osteotomy, Patollofemoral instability, Patella, Trochlea dysplasia
1. Introduction
Patellofemoral (PF) instability is a syndrome involving several factors and conditions.1 Trochlear dysplasia (TD) has been shown to be the feature most frequently diagnosed in patients with OPI (Objective Patellar Instability).2 Different procedures have been described to modify the trochlear shape and deepen the angle within the lateral and medial facet.
Even the patella might have an altered shape. Articulating during growth with an abnormal trochlea might lead the patellar posterior surface to modify accordingly, becoming congruent with the trochlear shape.
The Classification of patellar shape, which is divided in four types, was first proposed by Wiberg3 in 1941 and later modified by Baumgartl4 in 1966 (Fig. 1).
Fig. 1.
The Classification of patellar shape. Type 1: the medial facet is concave and has almost the same area of the lateral facet. Type 2: the medial facet is still concave, but is smaller than the lateral face. Type 3: the medial facet is convex and is almost vertical. Type 4: the medial facet is absent.
The Patella has seven facets, with the two more distal ones articulating with the trochlea in extension. It has been shown that the rate of dysplasia in the patella decreases scrolling proximally. In patients with OPI and trochlear dysplasia, patellar shape modifies, with the medial articulating surface becoming smaller compared to the lateral one (increased facet ratio), along its length from proximal to distal.5,6
Not only the trochlear shape but also a mismatch between the two articulating surfaces has a role in patellofemoral dislocations.
Rarely and in case of a highly dysplastic patella, reshaping only the trochlear groove might lead subsequently to an incongruence between the two bones.
When isolated sulcus-deepening trochleoplasty does not restore a congruent patellofemoral tracking tested perioperatively, further surgical procedures might be required. At our institution a closing wedge osteotomy of the patella performed medially is therefore added in those cases, to recreate a congruent PF joint.
Our aim was to present a surgical technique of patellar osteotomy in cases with incongruence between a newly shaped trochlea and a native dysplastic patella.
2. Osteotomies of the Patella
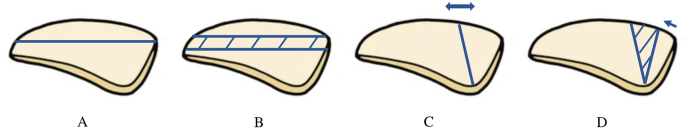
Originally, the osteotomy of the patella has been described mainly to address patellar chondromalacia and patellofemoral pain, not mentioning patellar instability (Fig. 2).
Fig. 2.
A. Osteotomy in the coronal plane. B. The patella thinning osteotomy. C. Opening wedge sagittal osteotomy. D. Closing sagittal wedge osteotomy.
Dellis was the first one, in 1977, suggesting to perform a simple osteotomy in the coronal plane to decrease its intraosseous pressure in patients with chondromalacia patellae.7 (Fig. 2A).
Vaquero and Arriaza proposed to perform “the patella thinning osteotomy” in the coronal plane for severe anterior knee pain, as an alternative to tibial tuberosity advancement, to reduce the PF joint reaction force and therefore the subchondral bone pressure8 (Fig. 2B).
Morscher was the first author describing an opening wedge sagittal osteotomy, with the aim of treating patellofemoral pain, by correcting the PF joint incongruity and increasing the area of cartilage contact during ROM (range of motion) between the medial patellar facet and the femoral condyle. The aim of this technique was to improve cartilage nutrition and reducing the pressure within the patellar bone9 (Fig. 2C).
Hejgaard and Arnoldi showed a 92% rate of patellofemoral pain relief after this procedure.10,11
Griss modified the Morscher's procedure from an opening to a closing sagittal wedge osteotomy. The author proposed it as a treatment for chondropatia and/or an early stage osteoarthritis, showing good clinical results at one year of follow-up. The technique's aim was to improve the PF joint congruity by removing an anteriorly based bone wedge and lifting one of the patella facets.12 (Fig. 2D).
Papers describing a patellar osteotomy for treating OPI patients are uncommon, and only few of them considered it associated with trochleoplasty.
Albee proposed an opening-wedge lateral femoral distal osteotomy associated with a dorsal closing-wedge patellar osteotomy.13
Badhe and Forster evaluated four OPI patients treated with the Albee's procedure. An increased PF stability with residual pain was reported, which might be due to lateral condyle elevation, leading to higher PF pressure.14
Paar evaluated on sheeps the sagittal opening wedge patellar osteotomy, as described by Morscher,9 associated with a deepening trochleoplasty, showing good results.15
Koch assessed the results of 2 patients undergoing a Bereiter's trochleoplasty associated to a sagittal closing wedge patellar osteotomy.16 The PF joint congruence was satisfactory without any cases of necrosis and nonunion.
Saragaglia et al. suggested to perform a patelloplasty, rather than an osteotomy, to treat OPI patients. The technique included the removal of the bulge frequently present distally at the medial facet in case of patellar dysplasia.17
Choufani et al. described in their case report the outcomes of an OPI patient treated with lateral closing wedge patellar osteotomy, fixed with non-absorbable transosseous sutures. After 12 months, no pain or instability recurrence was reported.18
3. Indications
Patellar osteotomy is a rare and effective option to be considered in carefully selected patients with objective patellar instability treated with sulcus deepening trochleoplasty.
Our institution preferred technique is the medial closing-wedge patellar osteotomy (MCWPO). Indications for this procedure are a patellar shape classified as Wiberg type III or IV associated to maltracking checked during surgery once the trochlear reshaping has been concluded.
Highly dysplastic patellae might not fit properly in the newly shaped trochlear groove, causing persistence of PF maltracking. Patellar osteotomy, modifying the shape of the patella might increase the PF joint congruence.
The goal of this procedure is to create a medial and lateral patellar facets, forming an angle congruent to the reshaped trochlear groove.
4. MCWPO: advantages
The patellar osteotomy is a technically demanding procedure with a not insignificant risk of abnormal or pathologic bone healing.19 This little flat bone articulating with the trochlea, has a poor vascularization.
The patella is supplied entirely by an arterial anastomotic ring which is made up by six different arteries. This network involves the anterior recurrent tibial artery and the inferior medial, inferior lateral, superior medial, superior lateral and supreme genicular arteries.
Two vessel pathways originating from this anastomotic ring vascularize the patella bone. The first pathway branches lying anteriorly, penetrate the cortex through the vascular foramina. The second pathway enters the borders directly through the peripatellar arteries.
This osteotomy technique proposed offers different advantages. The approach is the same used for the sulcus deepening trochleoplasty, as the patellar border exposed is the medial one. It preserves the anterior nutrient foramina, without compromising the principal blood supply to this sesamoid bone. The patellar eversion enable to manage the osteotomy without violating the articular cartilage. It leads to a wider contact which prevents from abnormal bone healing. It enables to reach a solid fixation using transosseous absorbable sutures. It allows more accurately to reshape a patellar articular surface with symmetric facets, placing the ridge laterally.
5. Preoperative planning
For MCWPO the preoperative planning is the same used in a standard way for OPI patients. PF pain and feeling of instability are frequent experiences described those patients.
Subjective findings include the presence of patellofemoral pain and/or feeling of instability.
During the preoperative physical examination the apprehension and medial tilt tests are carried out and the PF tracking is evaluated.
Radiological assessment consists in: weightbearing coronal and true sagittal radiographs, a 30° axial radiograph and MRI (Magnetic Resonance Imaging) slice imaging. The trochlear and patellar shape are classified according respectively the Dejour20 and Wiberg3 and Baumgartl4 classifications. The distance between the anterior tibial tubercle and the deepest point of the groove (TT-TG) is assessed. Finally the patellar height is evaluated through the Caton- Deschamps index.21
Sulcus deepening trochleoplasty is indicated at our institution in patients with OPI and a Dejour TD type B or D.
6. Surgical technique
The patient, in the supine position receives sedation and regional anesthesia. After placing a thigh tourniquet, the affected knee is positioned at 90° of flexion. The lower extremity is prepped and draped in the usual sterile manner.
A 10 cm straight incision is made beginning 5 cm proximal to the upper patellar pole. The medial parapatellar approach is performed to expose the trochlear groove. The reshaping procedure of the trochlea is performed as described previously.22
After the trochlear groove has been restored, the patellofemoral tracking and therefore the congruence between the two articulating surfaces is assessed. When the PF tracking is still abnormal, which occurs frequently with Wiberg type 3 or 4, a MCWPO is performed.
After exposing the medial patellar edge, an oscillating blade is used to remove a whole-lenght wedge of bone. The osteotomy cuts should be performed up to the patellar midline, at the same level of the planned ridge (Fig. 3A).
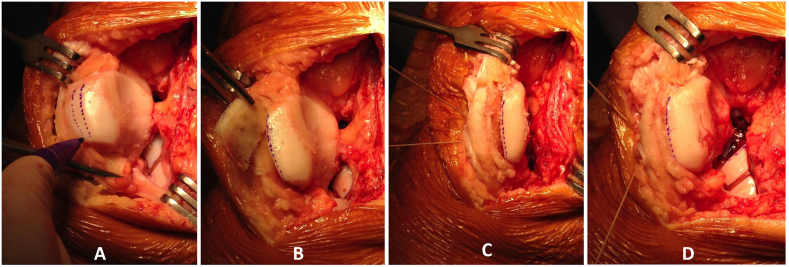
Fig. 3.
(A–D). Intraoperative images showing the patellar osteotomy technique in a right knee (Patient n°4). The knee is view from the front, with its proximal part at the top of the pictures. The patella is everted and its medial side exposed. A. The thickness of the wedge is drawn with a pencil. B. The bone wedge is cut with an oscillating saw; the tip of the wedge should end at the midline of the patella. C. Two transfixiant holes are drilled in the medial facet of the patella, passing both sides of the osteotomy. D. The osteotomy is closed and fixed with absorbable sutures.
The osteotomy should be performed at least 5 mm below the subchondral bone to avoid any damage to the cartilage surface. The wedge is then removed and the osteotomy is closed and fixed with two transosseous suture (Fig. 3B).
A 1.7 mm drill is used to perform two sagittal full-thickness holes, slightly lateral from the patellar medial edge.
A Vicryl suture 2 (Ethicon, Somerville, NJ) is driven through each hole. The osteotomy is then closed by tying both sutures (Fig. 3. C- D) (Fig. 4).
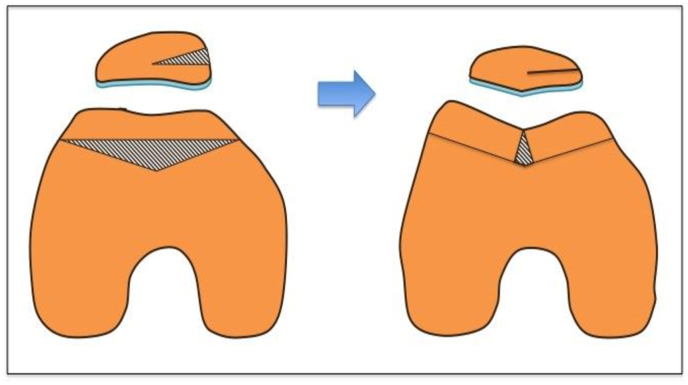
Fig. 4.
The rationale of the technique is to reshape the patella in order to obtain congruence between it and the newly formed trochlea after sulcus deepening trochleoplasty.
The medial patellofemoral ligament (MPFL) reconstruction is always added at the end of each OPI surgery.
The usual post-operative protocol for sulcus deepening trochleoplasty is not modified when a patellar medial closing wedge osteotomy is added.23
The patient is allowed to bear weight as tolerated using crutches. Physical therapy starts the day after surgery. Early muscle activation with isometric strengthening exercises is commenced immediately. Passive 0–90° flexion is allowed to help modelling the shape of both articulating surfaces.
At 45 days the patients are allowed to start closed kinetic chain strengthening exercises (e.g. cycling). At three months, light jogging might be performed. Full activity and return to sport is delayed until at least 6 months after surgery.
7. Results
The hospital database has been analysed retrospectively to quantify the clinical outcomes of this procedure. From January 2012 to august 2020 the senior author has performed 21 (6 right and 15 left knees) sulcus deepening trochleoplasties with a concomitant MCWPO.
The patients (6 males and 15 females) have been evaluated postoperatively with Kujala, IKDC and Lysholm Score at a minimum follow up of 10 months. The mean follow up was 35,25 months (ranging from 10 to 60 months).
The average Kujala, IKDC and Lysholm score were respectively 70,14 ± 15,51; 55,75 ± 7,12 and 77,12 ± 14,80. No further patellar dislocation has been assessed in those patients during follow up.
8. Conclusion
This is the first study showing the preliminary results of medial closing wedge patellar osteotomy associated to sulcus deepening trochleoplasty.
Although the several limitations of this study, this technique has shown good and promising clinical outcomes.
Indications for this technique are very restrictive and it should performed when patellofemoral tracking is still unsatistactory, due to a mismatch between the patellar shape and the newly formed trochlear groove.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Authors contribution
E.G.d.S.: Data curation, writing – review and editing. D.H.D: Methodology, Writing - review and editing.
Declaration of competing interest
Edoardo Giovannetti de Sanctis has no conflict of interest; David H. Dejour receive Royalties from ARTHREX.
Acknowledgements
None.
Contributor Information
Edoardo Giovannetti de Sanctis, Email: edoardo.giovannettids@gmail.com.
David H. Dejour, Email: corolyon@wanadoo.fr.
References
- 1.Dejour D.H., Mesnard G., Giovannetti de Sanctis E. Updated treatment guidelines for patellar instability: "un menu a la carte. J Exp Orthop. 2021;8(1):109. doi: 10.1186/s40634-021-00430-2. Nov 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 3.Roentgenographic G.W. And anatomic studies on the patellofemoral joint with special reference to chondromalacia patellae. Acta Orthop Scand. 1941;12:319–410. [Google Scholar]
- 4.Baumgartl F. Anatomical and clinical importance of the femoropatellar joint. Zentralbl Chir. . 1966;91(14):506–516. [PubMed] [Google Scholar]
- 5.Barnett A.J., Gardner R.O., Lankester B.J., Wakeley C.J., Eldridge J.D. Magnetic resonance imaging of the patella: a comparison of the morphology of the patella in normal and dysplastic knees. J Bone Joint Surg Br. 2007;89(6):761–765. doi: 10.1302/0301-620X.89B6.18995. Jun. [DOI] [PubMed] [Google Scholar]
- 6.Fucentese S.F., von Roll A., Koch P.P., Epari D.R., Fuchs B., Schottle P.B. The patella morphology in trochlear dysplasia--a comparative MRI study. Knee. 2006;13(2):145–150. doi: 10.1016/j.knee.2005.12.005. Mar. [DOI] [PubMed] [Google Scholar]
- 7.Deliss L. Coronal patellar osteotomy: preliminary report of its use in chondromalacia patellae. Proc Roy Soc Med. 1977;70(4):257–259. [PMC free article] [PubMed] [Google Scholar]
- 8.Vaquero J, Arriaza, R. The patella thinning osteotomy. Int Orthop.16:372-376. [DOI] [PubMed]
- 9.Osteotomy E.M. Of the patella in chondromalacia. Preliminary report. Arch Orthop Trauma Surg. 1978;92(2-3):139–147. doi: 10.1007/BF00397950. [DOI] [PubMed] [Google Scholar]
- 10.Hejgaard N.A.C. Osteotomy of the patella in the patellofemoral pain syndrome. The significance of increased intraosseous pressure during sustained knee flexion. Int Orthop. 1984;8(3):189–194. doi: 10.1007/BF00269915. [DOI] [PubMed] [Google Scholar]
- 11.Arnoldi C.C.L.K., Linderholm H. Intraosseous hypertension and pain in the knee. J Bone Joint Surg Br. 1975;57(3):360–363. [PubMed] [Google Scholar]
- 12.P G. Modification of sagittal osteotomy of the patella as treatment of excentric chondromalacia or retropatellar arthrosis. Preliminary communication. Z Orthop Ihre Grenzgeb. 1980;118:822–824. doi: 10.1055/s-2008-1053543. [DOI] [PubMed] [Google Scholar]
- 13.Fh A. The bone graft wedge in the treatment of habitual dislocation of the patellav. Med Recapitulate. 1915;88:257–259. [Google Scholar]
- 14.Badhe N.P., Forster I.W. Patellar osteotomy and Albee's procedure for dysplastic patellar instability. Eur J Orthop Surg Traumatol. 2003;13:43–47. [Google Scholar]
- 15.O P. Deepening of the trochlea femoris and osteotomy of the patella as possible causal therapy of recurrent traumatic patellar dislocations. An experimental study. Unfallchirurg. 1987;90(9):435–440. [PubMed] [Google Scholar]
- 16.Koch P.P., Fuchs B., Meyer D.C., Fucentese S.F. Closing wedge patellar osteotomy in combination with trochleoplasty. Acta Orthop Belg. 2011;77(1):116–121. Feb. [PubMed] [Google Scholar]
- 17.Saragaglia D., Mader R., Blaysat M., Mercier N. Medial facet patelloplasty in patellar instability associated with patellofemoral dysplasia: a report of 26 cases. Orthop Traumatol Surg Res. 2012;98(2):167–172. doi: 10.1016/j.otsr.2011.10.008. Apr. [DOI] [PubMed] [Google Scholar]
- 18.Choufani C., Barbier O., Versier G. Patellar lateral closing-wedge osteotomy in habitual patellar dislocation with severe dysplasia. Orthop Traumatol Surg Res. 2015;101(7):879–882. doi: 10.1016/j.otsr.2015.07.019. Nov. [DOI] [PubMed] [Google Scholar]
- 19.Dejour D., Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc Rev. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. Mar. [DOI] [PubMed] [Google Scholar]
- 20.Dejour D.R.P., Lecoultre B. Douleurs et instabilite rotulienne: essai de classification. Med Hyg. 1998;56:1466–1471. [Google Scholar]
- 21.Caton J. [Method of measuring the height of the patella] Acta Orthop Belg. 1989;55(3):385–386. [PubMed] [Google Scholar]
- 22.Dejour D., Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop. 2010;34(2):311–316. doi: 10.1007/s00264-009-0933-8. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giovannetti de Sanctis E., Mesnard G., Dejour D.H. Trochlear dysplasia: when and how to correct. Clin Sports Med. 2022;41(1):77–88. doi: 10.1016/j.csm.2021.09.001. Jan. [DOI] [PubMed] [Google Scholar]