Abstract
Background: The prognosis of cervical cancer (CC) is poor and not accurately reflected by the primary tumor node metastasis staging system. Our study aimed to develop a novel survival-prediction model.
Methods: Hallmarks of CC were quantified using single-sample gene set enrichment analysis and univariate Cox proportional hazards analysis. We linked gene expression, hypoxia, and angiogenesis using weighted gene co-expression network analysis (WGCNA). Univariate and multivariate Cox regression was combined with the random forest algorithm to construct a prognostic model. We further evaluated the survival predictive power of the gene signature using Kaplan-Meier analysis and receiver operating characteristic (ROC) curves.
Results: Hypoxia and angiogenesis were the leading risk factors contributing to poor overall survival (OS) of patients with CC. We identified 109 candidate genes using WGCNA and univariate Cox regression. Our established prognostic model contained six genes (MOCSI, PPP1R14A, ESM1, DES, ITGA5, and SERPINF1). Kaplan-Meier analysis indicated that high-risk patients had worse OS (hazard ratio = 4.63, p < 0.001). Our model had high predictive power according to the ROC curve. The C-index indicated that the risk score was a better predictor of survival than other clinicopathological variables. Additionally, univariate and multivariate Cox regressions indicated that the risk score was the only independent risk factor for poor OS. The risk score was also an independent predictor in the validation set (GSE52903). Bivariate survival prediction suggested that patients exhibited poor prognosis if they had high z-scores for hypoxia or angiogenesis and high risk scores.
Conclusions: We established a six-gene survival prediction model associated with hypoxia and angiogenesis. This novel model accurately predicts survival and also provides potential therapeutic targets.
Keywords: cervical cancer, overall survival, hypoxia, angiogenesis, SsGSEA
Introduction
Cervical cancer (CC) is a malignant tumor that seriously threatens women’s health, ranking fourth in female-specific cancers (Cohen et al., 2019). In 2018, diagnosed cases reached over 560,000, and deaths numbered 300,000 (Bray et al., 2018). Although progress has been made in CC prevention, screening, and treatment (e.g., modern targeted technology and immunotherapy), the therapeutic effect remains insufficient (Li et al., 2016; Vu et al., 2018), even as annual incidence and associated mortality increase. Relapse and metastasis are major factors associated with CC-related deaths. However, the current tumor node metastasis staging system is ineffective in predicting patient prognosis. Therefore, a more efficient prognostic model or new prognostic markers are urgently needed to improve the clinical outcomes of patients with CC.
Recent applications of precision medicine and the advancement of second-generation sequencing have led to a growing number of studies that construct genomic models for cancer prognostic assessment (Cheng et al., 2019; Liu et al., 2021). Although some studies have established a prognostic model for CC, its limitations preclude widespread use in clinical practice (Chen H. et al., 2020; Chen et al., 2020c).
Previous studies have suggested that hypoxia in many cancers, including pancreatic cancer, neuroblastoma, gastric cancer, and bladder cancer, is closely related to poor prognosis (Chen et al., 2020b; Cangelosi et al., 2020; Jiang et al., 2021; Tao et al., 2021). The hypoxia risk model of glioma may reflect the strength of tumor immune response and independently predict prognosis. A hypoxia-related lncRNA signature and nomogram accurately predicted overall survival (OS) and disease-free survival of patients with gastric cancer (Chen et al., 2020b). Additionally, angiogenesis plays a critical role in tumor growth and metastasis, with data indicating a close connection to poor prognosis in lung adenocarcinoma, hepatocellular carcinoma, and breast cancer (Kerbel, 2008; Chen Y. et al., 2019; Teleanu et al., 2019; Korobeinikova et al., 2020; Yang et al., 2021). Angiogenesis-related genetic markers can effectively predict the prognosis of patients with gastric cancer, while angiogenesis-related gene-based nomograms allow for more precise risk stratification (Ren et al., 2020). However, the value of combining hypoxia- and angiogenesis-related gene expression in CC prognosis has rarely been investigated.
Therefore, our study aimed to establish a new prediction model for hypoxia and angiogenesis. First, through statistical analysis of data from The Cancer Genome Atlas (TCGA), we identified hypoxia and angiogenesis as two critical risk factors affecting the OS of patients with CC. We then established a gene signature related to hypoxia and angiogenesis and confirmed its predictive accuracy using a separate validation set from the Gene Expression Omnibus (GEO). Furthermore, we explored correlations between the risk model and immune infiltration.
Materials and Methods
Dataset Preparation and Data Processing
Clinical and transcriptome data from 257 patients with CC were collected from TCGA (http://cancergenome.nih.gov/) for use as training sets. A prognostic model was established from these data. The GSE52903 dataset from GEO (http://www.ncbi.nlm.nih.gov/geo/), containing transcriptome and clinical data of 54 patients with CC, was used as the validation set. As all data were downloaded from public databases, ethical approval was not required for this study.
Candidate Gene Selection and Signature Establishment
Hallmark gene sets were downloaded from the Molecular Signatures Database (MSigDB) v.7.5.1 (https://www.gsea-msigdb.org/gsea/msigdb). Cancer hallmarks were assessed using single-sample gene set enrichment analysis (ssGSEA), implemented with R package “gsva” (Barbie et al., 2009; Liberzon et al., 2011). Hazard ratios (HR) of CC hallmarks were calculated using univariate Cox proportional hazards (Cox-PH) regression, implemented with R package “survival.” Based on ssGSEA scores and transcriptome data, a scale-free co-expression network was established using the weighted gene co-expression network analysis (WGCNA) R package to identify modules most related to hypoxia and angiogenesis (Langfelder and Horvath, 2008). Gene significance (GS) was calculated from correlations between individual genes and ssGSEA scores of hypoxia and angiogenesis. Associations between gene expression and module eigengenes were identified with module membership. Using the selection criteria of p < 0.0001 for GS and p < 0.01 for univariate Cox regression, 109 candidate genes were identified from the module that had the strongest association with hypoxia and angiogenesis. The importance of survival-related genes was ranked using the random forest algorithm. A Monte Carlo simulation with 100 iterations and 5 forward steps was performed (Ishwaran et al., 2008). The risk score model was established according to multivariate Cox regression using the following formula: risk score = β1x1+ β2x2+β3x3 + ⋯βNxN. Next, the best gene combination was selected based on log-rank p values obtained from Kaplan–Meier (KM) analysis.
Survival Analysis Based on the Risk Model
Relationships between the best combination of genes and CC hallmarks were estimated using gene co-expression correlations (based on Pearson’s). Patients were classified into high- and low-risk groups with their median risk scores. Significant between-group differences in prognosis were determined using KM analysis. Prediction accuracy of the risk model was tested with a time-dependent receiver operating characteristic (tROC) curve and the area under the curve of the ROC (AUC) (Heagerty et al., 2000). Univariate and multivariate Cox regression models were used to evaluate the independent predictive values of each prognostic factor. The predictive accuracy of the risk model and individual prognostic factors was calculated using the concordance index (C-index) (Pencina and D'Agostino, 2004). Risk scores and hypoxia/angiogenesis hallmarks were combined for survival analyses and prognosis assessments in the training set.
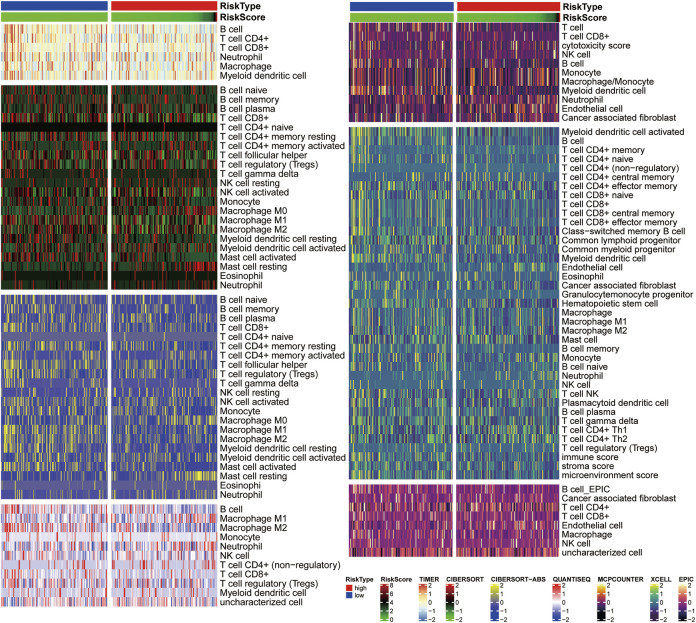
Correlation Analysis Between Risk Scores and Tumor Immune Microenvironment
Correlations between immune cell infiltration and risk scores were analyzed using the following analysis tools: TIMER, CIBERSORT, CIBERSORT-ABS, quanTIseq, MCPCOUNTER, EPIC, and xCELL. A heatmap was constructed to assess immune infiltration levels in high- and low-risk groups.
Bioinformatics and Statistical Analysis
To identify CC-related genes, ssGSEA was performed using hypoxia and angiogenesis genomes from MSigDB (Subramanian et al., 2005). Data analysis and figure generation were conducted using R (version 4.1.1; https://www.r-project.org/). Both ssGSEA and risk scores were normalized using z-scores. Survival probability was assessed using KM analyses, and between-group differences in survival were determined using log-rank tests. Univariate and multivariate Cox regressions were performed to determine the effect of each factor on progression-free survival (PFS) and OS. The predictive capacity of risk models and cancer hallmarks were measured using tROC and AUC analyses (Heagerty et al., 2000), while risk-model prognostic accuracy was reflected in the C-index.
Results
Research Design
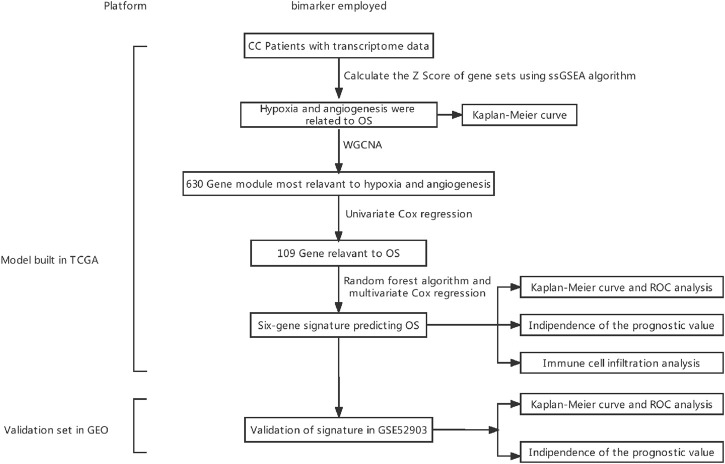
Figure 1 depicts the research protocol to generate a survival prediction model for patients with CC. We identified hypoxia and angiogenesis as the two cancer hallmarks most associated with OS. Next, we identified core hypoxia- and angiogenesis-related genes for survival prediction using a combination of WCGNA, univariate/multivariate Cox regression, and the random forest algorithm. We then used these core genes to build risk models for OS prediction. Finally, we assessed and validated the prognostic predictive power of the risk model in training and validation cohorts. Table 1 summarizes patient-related data.
FIGURE 1.
Experimental flowchart. CC, cervical cancer; WGCNA, weighted gene co-expression network analysis; ssGSEA, single-sample gene set enrichment analysis; OS, overall survival; ROC, receiver operating characteristic.
TABLE 1.
Clinical data from The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO).
| Characteristic | TCGA | GEO | p |
|---|---|---|---|
| n | 257 | 54 | |
| Status, n (%) | 0.074 | ||
| Alive | 195 (62.7%) | 34 (10.9%) | |
| Dead | 62 (19.9%) | 20 (6.4%) | |
| Stage, n (%) | 0.141 | ||
| Stage I | 146 (46.9%) | 27 (8.7%) | |
| Stage II | 56 (18%) | 8 (2.6%) | |
| Stage III | 39 (12.5%) | 15 (4.8%) | |
| Stage IV | 16 (5.1%) | 4 (1.3%) | |
| grade, n (%) | |||
| G1 | 18 (7%) | ||
| G2 | 127 (49.4%) | ||
| G3 | 112 (43.6%) | ||
| age, median (IQR) | 46 (38, 56) | 49 (41, 65.5) | 0.220 |
Hypoxia and Angiogenesis Were Key Hallmarks Affecting OS
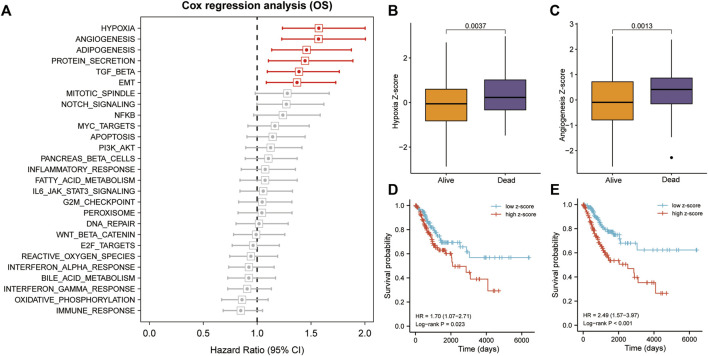
We calculated and ranked Cox coefficients in terms of cancer-hallmark ssGSEA scores and the corresponding survival data of the training cohort. Univariate Cox-PH regression revealed that hypoxia and angiogenesis had a stronger influence on survival than adipogenesis, protein secretion, TGF-beta signaling, epithelial-mesenchymal transition, mitotic spindle, NOTCH signaling, NFKB, MYC-targets, apoptosis, PI3K/AKT signaling, pancreas-beta cells, or inflammatory response (Figure 2A). Hypoxia and angiogenesis z-scores were significantly higher in patients who died than in those who lived during the follow-up period (p < 0.05; Figures 2B,C). Using median risk scores, we assigned 257 patients with CC in the training cohort to high- and low-risk groups. Survival analysis indicated that patients with high hypoxia z-scores had poor OS (HR = 1.70, p = 0.023; Figure 2D), as did patients with high angiogenesis z-scores (HR = 2.49, p < 0.001; Figure 2E).
FIGURE 2.
Hypoxia and angiogenesis were the key cancer hallmarks affecting OS in patients with CC. (A) Hypoxia and angiogenesis had a strong influence on OS, according to the univariate Cox-PH regression. (B,C) Patients with CC who died during follow-up had significantly higher z-scores for hypoxia and angiogenesis. (D,E) Patients with high hypoxia and angiogenesis z-scores had poorer OS, according to KM analysis. TGF, transforming growth factor; NFKB, nuclear factor kappa B; PI3k/Akt, phosphatidylinositol-3- kinase/serine-threonine kinase; EMT, epithelial-mesenchymal transition; KM, Kaplan–Meier.
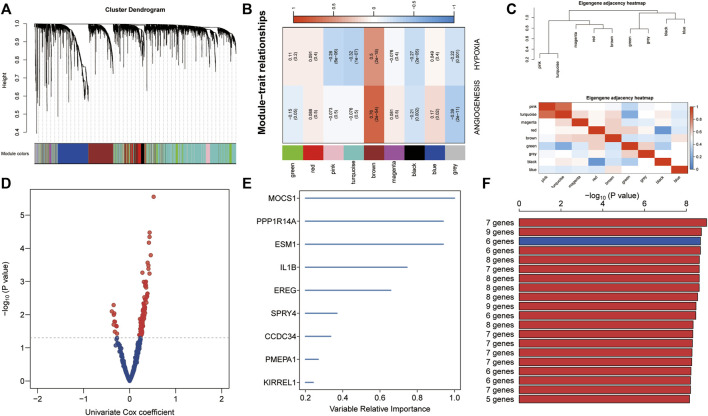
Establishment of Prognostic Gene Signature Related to Hypoxia and Angiogenesis
To identify highly connected modules of co-expressed transcripts, we performed WGCNA using ssGSEA z-scores of hypoxia and angiogenesis from the training set and genome-wide microarray data (Figure 3A). Of the eight non-gray modules, the brown one was the most significantly related to hypoxia and angiogenesis (r > 0.5, p < 0.0001; Figure 3B). We displayed the correlation of co-expressed modules as a module eigengene adjacency heatmap (Figure 3C). We then used GS < 0.001 as the criterion for selecting key genes from the brown module. Univariate Cox regressions on these genes yielded 109 candidates with prognostic potential ( p < 0.05; Figure 3D). From these candidate genes, the random forest supervised classification algorithm then extracted the top 10 (EREG, ESM1, NAMPT, SERPINF1, PPP1R14A, MOCS1, ITGA5, NRP1, SPRY4, and DES) (Figure 3E), forming 1024 risk model combinations. Using KM analysis and comparing -log10 Plog-rank values, we determined that the optimal risk model was the one with six genes (MOCSI, PPP1R14A, ESM1, DES, ITGA5, and SERPINF1). We considered that a good model should contain as few genes as possible (Figure 3F). The formula for establishing our model was as follows: risk score = 0.160 × MOCSI + 0.370 × PPP1R14A + 0.223 × ESM1 + (-0.246) × DES + 0.323 × ITGA5 + (-0.248) × SERPINF1.
FIGURE 3.
Establishment of hypoxia- and angiogenesis-related gene signatures. (A) Eight non-gray modules were confirmed using WGCNA. (B) The brown module was most significantly related to hypoxia and angiogenesis (r > 0.5, p < 0.0001). (C) Module eigengene adjacency heatmap displaying correlations of co-expressed modules. (D) Key genes from the brown module were screened. Univariate Cox regression was used to identify 109 candidate genes with prognostic potential. (E) The random forest supervised classification algorithm selected 10 genes from the 109 candidate genes. (F) The six-gene risk model was ranked first in KM analysis to identify optimal risk models.
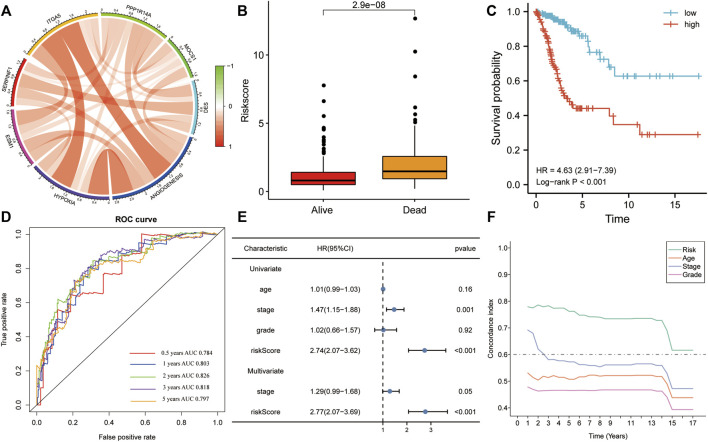
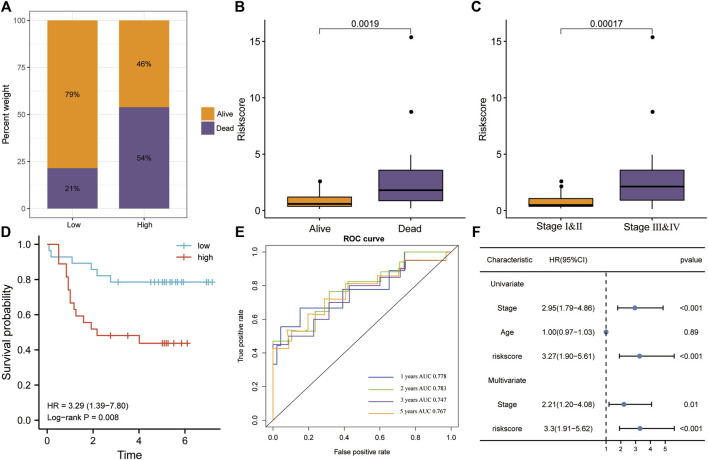
The Risk Score Is an Independent OS Predictor in the Training Set
In the training set, all six genes were positively associated with hypoxia and angiogenesis (Figure 4A). Risk scores were significantly higher in the mortality group during follow-up (Figure 4B). The results of KM analysis for OS revealed that patients with high-risk scores had a poorer prognosis than those with low-risk scores (HR = 4.63, p < 0.001; Figure 4C). Additionally, the AUC-ROC analysis indicated that risk scores successfully predicted the 0.5-, 1-, 2-, 3-, and 5-year OS (AUC > 0.7; Figure 4D). Univariate and multivariate Cox regression for OS in the training set revealed that the risk score was the only significant independent risk factor among all tested clinicopathological variables (p < 0.001; Figure 4E). Moreover, the C-index indicated that the risk score had the best OS predictive ability (Figure 4F).
FIGURE 4.
The risk score was the only significant independent risk factor affecting OS in the training set. (A) Correlation of the gene signature with hypoxia and angiogenesis. (B) The risk score was significantly higher in the mortality group during follow-up. (C) Patients with a high risk score had a poorer OS, according to KM analysis. (D) The risk score was a good predictor of OS (AUC > 0.7). (E) Univariate and multivariate Cox regression for OS revealed that risk score was the only significant independent risk factor among multiple clinicopathological variables. (F) The C-index indicated that the risk score had the best OS predictive ability among the clinicopathological variables. AUC, area under the ROC curve; HR, hazard ratio.
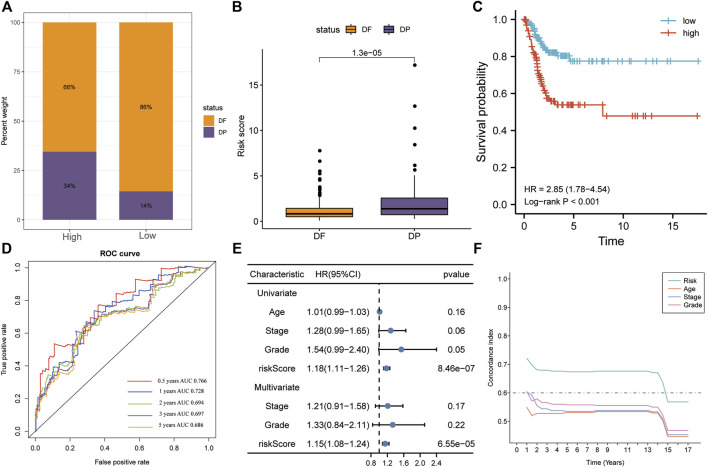
The Risk Score Is an Independent PFS Predictor in the Training Set
The high-risk group had a greater proportion of patients with disease progression, whereas the low-risk group had a greater proportion of patients without progression (Figure 5A). During follow-up, risk scores were significantly higher in the disease-progression group than in the no-progression group (p < 0.01; Figure 5B). Patients with high risk scores had a poorer prognosis than those with low risk scores (KM analysis, HR = 2.85, p < 0.001; Figure 5C). The AUC-ROC analysis indicated that risk scores predicted 0.5-, 1-, 2-, 3-, and 5-year PFS (AUC > 0.68; Figure 5D). Like in OS, the risk score was the only significant independent risk factor for PFS (univariate/multivariate Cox regressions, p < 0.001; Figure 5E) and had the best predictive ability (Figure 5F).
FIGURE 5.
The risk score was the only significant independent risk factor predicting PFS in the training set. (A) The high-risk group contained a greater proportion of patients with disease progression. (B) Patients with disease progression had significantly higher risk scores. (C) Patients with high risk scores had a poorer prognosis, according to KM analysis. (D) The risk score was a good predictor of PFS (AUC > 0.68). (E) Univariate and multivariate Cox regression for PFS revealed that risk score was the only significant independent risk factor among included clinicopathological variables. (F) The C-index indicated that the risk score had the best PFS predictive ability. PFS, progression-free survival; AUC, area under the ROC curve.
In the training set, KM analysis of OS was conducted on patients after they had been divided into clinicopathological subgroups according to age, stage, and grade. Patients with high risk scores had a worse prognosis than those with low risk scores in all subgroups (Figures 6A–F).
FIGURE 6.
The risk score was a better predictor of OS across multiple subgroups of the training set. (A–F) KM analysis of OS was conducted for various clinicopathological subgroups, including age, stage, and grade. Patients with high risk scores had a worse prognosis.
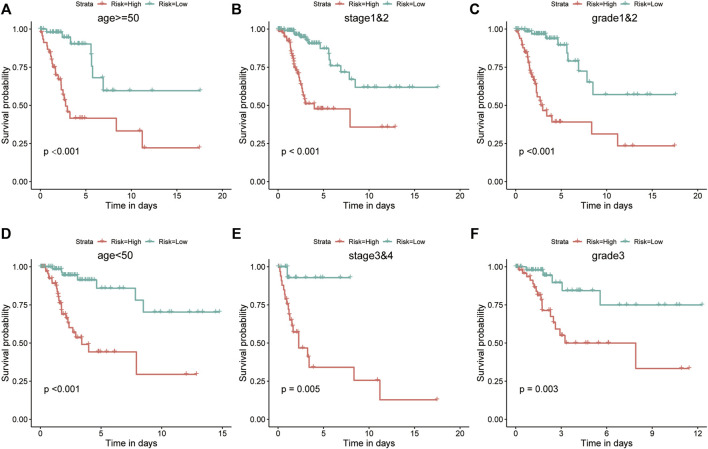
Risk Model Verification in the Validation Set
We validated risk model performance using an independent CC validation set. The high-risk group had a greater proportion of patients who died, whereas the low-risk group had a greater proportion of surviving patients (Figure 7A). Risk scores were significantly higher in the mortality group during follow-up (p < 0.01; Figure 7B). Patients in stages III–IV had significantly higher risk scores than those in stages I–II (p < 0.001; Figure 7C). Patients with high-risk scores had a poorer prognosis in terms of OS than those with low-risk scores (KM analysis, HR = 3.29, p = 0.008; Figure 7D). Risk scores predicted the 1-, 2-, 3-, and 5-year OS in the validation set (AUC > 0.7; Figure 7E), while also being the only significant independent risk factor (univariate/multivariate Cox regressions, p < 0.001; Figure 7F).
FIGURE 7.
Verification of the risk model in the GSE52903 dataset. (A) The high-risk group had higher mortality rates. (B) The risk score was significantly higher in the mortality group during follow-up. (C) Patients in stages III–IV had significantly higher risk scores. (D) Patients with high risk scores had a poorer prognosis, according to KM analysis for OS. (E) The ROC analysis revealed that risk scores accurately predicted OS. (F) Univariate and multivariate Cox regression for OS revealed that risk score was the only significant independent risk factor among included clinicopathological variables.
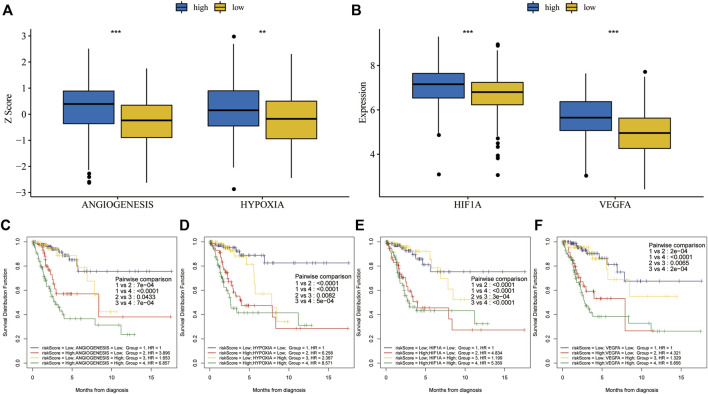
Association and combined survival analysis of risk scores and key cancer hallmarks in the training set.
Hypoxia and angiogenesis z-scores were significantly higher in the high-risk group than in the low-risk group (Figure 8A). Vascular endothelial growth factor A (VEGFA) is a major driver of angiogenesis during tumor progression in various cancers (Krock et al., 2011). Hypoxia-induced factor 1 alpha (HIF1A) is a crucial protein in controlling hypoxia response (Li et al., 2020). HIF1A and VEGFA levels were significantly higher in the high-risk group than in the low-risk group (Figure 8B). When we ran KM analysis on combined risk scores and cancer hallmarks or hallmark-related genes, we found that OS prognosis was best with low risk scores and low hypoxia or angiogenesis z-scores (Figures 8C,D). Similarly, the prognosis was best with low risk scores and low HIF1A or VEGFA expression (Figures 8E,F).
FIGURE 8.
Combined survival analysis of risk scores and key cancer hallmarks in the training set. (A) Hypoxia and angiogenesis z-scores were significantly higher in the high-risk group. (B) HIF1A and VEGFA expression levels were significantly higher in the high-risk group. (C,D) The prognosis was worse in patients with high risk scores and high hypoxia or angiogenesis z-scores, according to KM analysis for OS after combining risk scores and key cancer hallmarks. (E,F) The prognosis was worse in patients with high risk scores and high HIF1A or VEGFA expression, based on KM analysis for OS after combining risk scores and genes related to key cancer hallmarks.
Relative Immune Infiltration Levels in High- and Low-Risk Groups
The heat map illustrates correlations between immune cell infiltration and risk scores (Figure 9). The TIMER analysis demonstrated that B cells and CD4+T cells were more abundant in the low-risk group. Additionally, CIBERSORT analysis showed that the low-risk group had more CD8+T cells, activating NK cells, M1 macrophages, M2 macrophages, and myeloid dendritic cells. The CIBERSORT-ABS analysis also found higher levels of CD8+T cells, CD4+T cells, follicular helper T cells, regulatory T cells, M1 macrophages, M2 macrophages, myeloid dendritic cells, and activated mast cells in the low-risk group. Both analyses revealed that resting mast cell and M0 macrophage levels were higher in the high-risk group. Furthermore, QuanTIseq analyses indicated that the low-risk group had more B cells, M2 macrophages, and CD8+T cells, whereas the high-risk group had more M1 macrophages and neutrophils. The low-risk group had more T cells, B cells, and myeloid dendritic cells, according to MCPCOUNTER analyses, whereas the high-risk group had more monocytes, macrophages, and endothelial cells. Along the same lines, EPIC analyses revealed that the numbers of CD8+T cells, CD4+T cells, B cells, myeloid dendritic cells, cancer-associated fibroblasts, and hematopoietic stem cells, and immune, stromal, and microenvironment scores were higher in the low-risk group. Finally, XCELL analyses suggested that B cell levels were higher in the low-risk group, while EPIC and XCELL analyses both found that endothelial cell levels were higher in the high-risk group.
FIGURE 9.
Correlation analysis of immune cell infiltration and risk scores. A Heatmap of seven different methods shows relative infiltration levels in high- and low-risk groups.
Discussion
The poor prognosis of CC remains a serious threat to women’s health, although human papillomavirus vaccination and screening have significantly reduced incidence and mortality. Early diagnosis and treatment are essential for improving CC prognosis, but reliable diagnostic and prognostic biomarkers are currently lacking.
Hypoxia and angiogenesis both predict poor prognosis in patients with CC (Vaupel and Mayer, 2007; Ding et al., 2019). Hypoxia involves insufficient oxygen supply to cells, tissues, or organs. Multiple studies have established its role in cancer tumorigenesis, development, invasion, metastasis, recurrence, and drug resistance (Rezaeian et al., 2017; Jing et al., 2019; Fico and Santamaria-Martinez, 2020). By promoting tumor angiogenesis, hypoxia facilitates rapid tumor growth, metastasis, and immune escape (Zhang, 2012; Dai et al., 2017). Unsurprisingly, a hypoxic microenvironment is closely associated with CC occurrence and development (Hockel et al., 1996). HIF-1α is activated in the hypoxic tumor microenvironment and modulates many transcription factors that allow cells to survive in unfavorable conditions (Semenza, 2012). Additionally, paclitaxel-resistant CC cells (HeLa-R cells) exhibit upregulated HIF1-α expression, and downregulation of HIF1-α re-sensitized HeLa-R cells to paclitaxel (Peng et al., 2014). Hypoxia-related genes appear to have latent prognostic value. For example, hCINAP (required for hypoxia-induced EMT and apoptosis) may play a role in CC metastasis and is a potential therapeutic target for CC (Zhang et al., 2021). Likewise, hypoxia-induced ZEB1 promotes CC progression via CCL8-dependent tumor-associated macrophage recruitment (Chen X.-J. et al., 2019).
Angiogenesis is the process of new vessel formation and a hallmark of solid tumors, including CC (Folkman, 1990). Substantial evidence has shown that angiogenesis contributes to CC development, progression, and metastasis (Kodama et al., 1999). Angiogenesis is important not only in tumor growth but also in hematogenous metastasis, as tumor blood vessels can provide nutrients and oxygen, while disposing metabolic waste. Angiogenesis is activated when the balance between stimulatory and inhibitory elements shifts towards pro-angiogenic factors (Hanahan and Folkman, 1996; Payen et al., 2015). One of the most important angiogenesis regulators is VEGF-A, a major proangiogenic cytokine in tumor growth and progression (Kerbel, 2008). VEGF-A also acts in CC (Cheng et al., 2000) and is associated with poor prognosis (Jin et al., 2017; Kaddu-Mulindwa et al., 2021).
Accumulating evidence suggests that hypoxia is closely associated with angiogenesis (Sui et al., 2017; Wen et al., 2019). Previous studies have revealed that HIF-1α regulates VEGFA expression via HIFα-dependent transcriptional activity (Manalo et al., 2005). Furthermore, antiangiogenic drugs help inhibit tumor growth and metastasis via the HIF-1α signaling pathway (Rey et al., 2017). To date, hypoxia-related prognostic gene signatures have been studied in prostate cancer (Yang et al., 2018), lung adenocarcinoma (Mo et al., 2020), and hepatocellular carcinoma (Zhang et al., 2020), whereas angiogenesis-related prognostic gene signatures have been studied in gastric cancer (Ren et al., 2020), renal clear cell carcinoma (Zheng et al., 2021), and breast cancer (Bender and Mac Gabhann, 2013). These findings revealed the prognostic value of hypoxia- and angiogenesis-related genes, along with their potential as therapeutic targets in CC.
However, these studies had certain flaws. First, hypoxia- or angiogenesis-related gene signatures were constructed based on considering individual genes reported in the literature, without considering that both processes likely involve entire gene networks. Second, such studies rarely investigated the prognosis predictive capacity of combining hypoxia-related gene signatures and angiogenesis-related gene signatures.
Therefore, our study established a new prognostic model based on gene signatures that correlate with hypoxia and angiogenesis. First, we applied ssGSEA and Cox-PH regressions to identify hypoxia and angiogenesis as cancer hallmarks most significantly associated with OS in patients with CC. Because hypoxia can promote angiogenesis, the two phenotypes are strongly correlated. Subsequently, we used WGCNA to identify the gene module most strongly associated with both processes. We then obtained prognostic hub genes (including MOCS1, PPP1R14A, ESM1, DES, ITGA5, and SERPINF1) after univariate Cox regression, random forest algorithm, and KM analysis. This method allowed us to comprehensively identify genes associated with both phenotypes, given that the regulation of hypoxia and angiogenesis occurs in a network. These analyses will enhance our understanding of hypoxia and angiogenesis regulatory mechanisms. Next, survival analysis of training and validation sets demonstrated that our six-gene prognostic model independently predicted OS in patients with CC. Finally, immune cell infiltration analysis suggested that high-risk patients had significantly lower infiltration levels.
Each of the six genes have been implicated in cancer. PPP1R14A is involved in the pathogenesis of human melanoma. It drives Ras activity and tumorigenesis by activating the growth-promoting ERM family and inhibiting the tumor suppressor merlin (Riecken et al., 2016). ESM1 has been widely explored in various cancers, including prostate cancer, hepatocellular carcinoma, and head and neck squamous cell carcinoma; it also has prognostic value in esophageal cancer (Calderaro et al., 2019; Xu et al., 2019; Cui et al., 2021; Pan et al., 2021). ITGA6 is an oncogene in various cancers (Raab-Westphal et al., 2017), including CC, where it is overexpressed and associated with proliferation and invasion (Yang J. et al., 2019). In contrast to these genes, MOCS1, DES, and SERPINF1 are poorly understood. Thus, their potential biological functions require further research.
Dysfunction of the antitumor immune system is closely related to CC development and progression (Chen Z. et al., 2019; Liu J. J. et al., 2020; Liu X. et al., 2020). High levels of activated memory CD4+T cells predict a better prognosis in patients with CC (Wang et al., 2019). The correlation between risk stratification and immune cell infiltration further demonstrates the predictive power of our six-gene prognostic model.
Previously, a nine-lncRNA signature was established to predict the 1 year PFS in patients with CC; this model had an AUC of 0.793, 0.780, and 0.742 in two GEO test sets and one TCGA test set, respectively (Mao et al., 2019). A seven-gene prognostic signature for CC had also been developed using GEO data, predicting 1-, 3-, and 5-year OS with AUC of 0.74, 0.76, and 0.81, respectively (An et al., 2022). Another study established 11 immune-related gene signatures to assess OS in patients with CC, yielding 3- and 5-year AUC of 0.733 and 0.747 (Yang S. et al., 2019). For our six-gene prognostic risk model, the AUC at 1, 2, 3, and 5 years is 0.784, 0.803, 0.826, 0.818, and 0.797 in the training set, and 0.778, 0.783, 0.747, and 0.767 in the validation set. Compared to the previous models, ours showed better predictive power.
Nevertheless, our study had some limitations. First, our findings would be better supported with the inclusion of more machine learning tools. The random forest algorithm is a mature and widely used machine learning method, with relatively stable results. However, new machine learning methods are available that can benefit our investigation, including a novel tool for gene selection and phenotype classification, as well as an efficient algorithm for survival analysis and biomarker selection (Huang et al., 2021; Huang et al., 2022). Using these more advanced techniques should reduce errors from platforms or samples. Another limitation was that we only used one GEO dataset for verification and did not include normal transcript data as a control. Therefore, future studies need to validate the predictive value of our six-gene signature in more CC tissues and adjacent normal tissues. Finally, we still know little about the biological functions of the six hypoxia- and angiogenesis-related genes, necessitating more experiments in the future.
Conclusion
In summary, we established a new six-gene signature for CC and used it to develop a risk model that strengthens prognostic predictions. The six-gene prognostic model should be an effective tool for detecting high-risk patients, enabling early treatment to maximally prevent CC advancement. While possessing high predictive power, this model also has a small number of genes, reducing the economic burden on patients. Thus, it has great potential for clinical application and transformation. The genes chosen for the model play a very important role in tumor development, suggesting that they can be potential therapeutic targets. Our model is not only useful for predicting prognosis, but can also supplement the existing TNM staging method. Once the model is verified in more clinical cases, our data can be generalized to a larger population.
Acknowledgments
The authors would like to thank the staff of the Department of Traditional Chinese Medicine Gynecology, Foshan Fosun Chancheng Hospital, Foshan Clinical Medical College of Guangzhou University of Chinese Medicine, Foshan, Guangdong Province, People’s Republic of China.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: Clinical and transcriptome data were obtained from the TCGA (http://cancergenome.nih.gov/). The GSE52903 dataset was obtained from GEO (http://www.ncbi.nlm.nih.gov/geo/).
Author Contributions
LL and HZ completed data analysis and drafting of the article. PW performed the statistical analysis and charting. SW designed the experiments and revised the manuscript in detail. All the authors have agreed to submit the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflicts of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- An R., Meng S., Qian H. (2022). Identification of Key Pathways and Establishment of a Seven-Gene Prognostic Signature in Cervical Cancer. J. Oncol. 2022, 1–16. 10.1155/2022/4748796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbie D. A., Tamayo P., Boehm J. S., Kim S. Y., Moody S. E., Dunn I. F., et al. (2009). Systematic RNA Interference Reveals that Oncogenic KRAS-Driven Cancers Require TBK1. Nature 462 (7269), 108–112. 10.1038/nature08460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender R. J., Mac Gabhann F. (2013). Expression of VEGF and Semaphorin Genes Define Subgroups of Triple Negative Breast Cancer. PLoS One 8 (5), e61788. 10.1371/journal.pone.0061788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray F., Ferlay J., Soerjomataram I., Siegel R. L., Torre L. A., Jemal A. (2018). Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 68 (6), 394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- Calderaro J., Meunier L., Nguyen C. T., Boubaya M., Caruso S., Luciani A., et al. (2019). ESM1 as a Marker of Macrotrabecular-Massive Hepatocellular Carcinoma. Clin. Cancer Res. 25 (19), 5859–5865. 10.1158/1078-0432.CCR-19-0859 [DOI] [PubMed] [Google Scholar]
- Cangelosi D., Morini M., Zanardi N., Sementa A. R., Muselli M., Conte M., et al. (2020). Hypoxia Predicts Poor Prognosis in Neuroblastoma Patients and Associates with Biological Mechanisms Involved in Telomerase Activation and Tumor Microenvironment Reprogramming. Cancers 12 (9), 2343. 10.3390/cancers12092343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Deng Q., Wang W., Tao H., Gao Y. (2020a). Identification of an Autophagy-Related Gene Signature for Survival Prediction in Patients with Cervical Cancer. J. Ovarian Res. 13 (1), 131. 10.1186/s13048-020-00730-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Hu L., Chen K. (2020b). Construction of a Nomogram Based on a Hypoxia-Related lncRNA Signature to Improve the Prediction of Gastric Cancer Prognosis. Front. Genet. 11, 570325. 10.3389/fgene.2020.570325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Q., Hu L., Huang D., Chen K., Qiu X., Qiu B. (2020c). Six-lncRNA Immune Prognostic Signature for Cervical Cancer. Front. Genet. 11, 533628. 10.3389/fgene.2020.533628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X.-J., Deng Y.-R., Wang Z.-C., Wei W.-F., Zhou C.-F., Zhang Y.-M., et al. (2019a). Hypoxia-induced ZEB1 Promotes Cervical Cancer Progression via CCL8-dependent Tumour-Associated Macrophage Recruitment. Cell Death Dis. 10 (7), 508. 10.1038/s41419-019-1748-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Sun Y., Cui Y., Lei Y., Jiang N., Jiang W., et al. (2019b). High CTHRC1 Expression May Be Closely Associated with Angiogenesis and Indicates Poor Prognosis in Lung Adenocarcinoma Patients. Cancer Cell Int. 19, 318. 10.1186/s12935-019-1041-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Zhu Y., Du R., Pang N., Zhang F., Dong D., et al. (2019c). Role of Regulatory B Cells in the Progression of Cervical Cancer. Mediat. Inflamm. 2019, 1–8. 10.1155/2019/6519427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Q., Huang C., Cao H., Lin J., Gong X., Li J., et al. (2019). A Novel Prognostic Signature of Transcription Factors for the Prediction in Patients with GBM. Front. Genet. 10, 906. 10.3389/fgene.2019.00906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng W. F., Chen C. A., Lee C. N., Wei L. H., Hsieh F. J., Hsieh C. Y. (2000). Vascular Endothelial Growth Factor and Prognosis of Cervical Carcinoma. Obstet. Gynecol. 96 (5 Pt 1), 721–726. 10.1016/s0029-7844(00)01025-5 [DOI] [PubMed] [Google Scholar]
- Cohen P. A., Jhingran A., Oaknin A., Denny L. (2019). Cervical Cancer. Lancet 393 (10167), 169–182. 10.1016/S0140-6736(18)32470-X [DOI] [PubMed] [Google Scholar]
- Cui Y., Guo W., Li Y., Shi J., Ma S., Guan F. (2021). Pan-cancer Analysis Identifies ESM1 as a Novel Oncogene for Esophageal Cancer. Esophagus 18 (2), 326–338. 10.1007/s10388-020-00796-9 [DOI] [PubMed] [Google Scholar]
- Dai T., Hu Y., Zheng H. (2017). Hypoxia Increases Expression of CXC Chemokine Receptor 4 via Activation of PI3K/Akt Leading to Enhanced Migration of Endothelial Progenitor Cells. Eur. Rev. Med. Pharmacol. Sci. 21 (8), 1820–1827. [PubMed] [Google Scholar]
- Ding X., Jia X., Wang C., Xu J., Gao S.-J., Lu C. (2019). A DHX9-lncRNA-MDM2 Interaction Regulates Cell Invasion and Angiogenesis of Cervical Cancer. Cell Death Differ. 26 (9), 1750–1765. 10.1038/s41418-018-0242-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fico F., Santamaria‐Martínez A. (2020). TGFBI Modulates Tumour Hypoxia and Promotes Breast Cancer Metastasis. Mol. Oncol. 14 (12), 3198–3210. 10.1002/1878-0261.12828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman J. (1990). What Is the Evidence that Tumors Are Angiogenesis Dependent? J. Natl. Cancer Inst. 82 (1), 4–7. 10.1093/jnci/82.1.4 [DOI] [PubMed] [Google Scholar]
- Hanahan D., Folkman J. (1996). Patterns and Emerging Mechanisms of the Angiogenic Switch during Tumorigenesis. Cell 86 (3), 353–364. 10.1016/s0092-8674(00)80108-7 [DOI] [PubMed] [Google Scholar]
- Heagerty P. J., Lumley T., Pepe M. S. (2000). Time-dependent ROC Curves for Censored Survival Data and a Diagnostic Marker. Biometrics 56 (2), 337–344. 10.1111/j.0006-341x.2000.00337.x [DOI] [PubMed] [Google Scholar]
- Hockel M., Schlenger K., Aral B., Mitze M., Schaffer U., Vaupel P. (1996). Association between Tumor Hypoxia and Malignant Progression in Advanced Cancer of the Uterine Cervix. Cancer Res. 56 (19), 4509–4515. [PubMed] [Google Scholar]
- Huang H. H., Peng X. D., Liang Y. (2021). SPLSN: An Efficient Tool for Survival Analysis and Biomarker Selection. Int. J. Intell. Syst. 36 (10), 5845–5865. 10.1002/int.22532 [DOI] [Google Scholar]
- Huang H., Wu N., Liang Y., Peng X., Shu J. (2022). SLNL: A Novel Method for Gene Selection and Phenotype Classification. Int J Intelligent Sys. 10.1002/int.22844 [DOI] [Google Scholar]
- Ishwaran H., Kogalur U. B., Blackstone E. H., Lauer M. S. (2008). Random Survival Forests. Ann. Appl. Stat. 2 (3), 841–860. 10.1214/08-aoas169 [DOI] [Google Scholar]
- Jiang M., Ren L., Chen Y., Wang H., Wu H., Cheng S., et al. (2021). Identification of a Hypoxia-Related Signature for Predicting Prognosis and the Immune Microenvironment in Bladder Cancer. Front. Mol. Biosci. 8, 613359. 10.3389/fmolb.2021.613359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin L., Liu W.-R., Tian M.-X., Jiang X.-F., Wang H., Zhou P.-Y., et al. (2017). CCL24 Contributes to HCC Malignancy via RhoB- VEGFA-VEGFR2 Angiogenesis Pathway and Indicates Poor Prognosis. Oncotarget 8 (3), 5135–5148. 10.18632/oncotarget.14095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing X., Yang F., Shao C., Wei K., Xie M., Shen H., et al. (2019). Role of Hypoxia in Cancer Therapy by Regulating the Tumor Microenvironment. Mol. Cancer 18 (1), 157. 10.1186/s12943-019-1089-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaddu‐Mulindwa D., Rosolowski M., Ziepert M., Regitz E., Assmann G., Bewarder M., et al. (2021). VEGFR2 and VEGFA Polymorphisms Are Not Associated with an Inferior Prognosis in Caucasian Patients with Aggressive B‐cell Lymphoma. Eur. J. Haematol. 106 (1), 100–104. 10.1111/ejh.13526 [DOI] [PubMed] [Google Scholar]
- Kerbel R. S. (2008). Tumor Angiogenesis. N. Engl. J. Med. 358 (19), 2039–2049. 10.1056/NEJMra0706596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodama J., Seki N., Tokumo K., Hongo A., Miyagi Y., Yoshinouchi M., et al. (1999). Vascular Endothelial Growth Factor Is Implicated in Early Invasion in Cervical Cancer. Eur. J. Cancer 35 (3), 485–489. 10.1016/s0959-8049(98)00410-9 [DOI] [PubMed] [Google Scholar]
- Korobeinikova E., Ugenskiene R., Insodaite R., Rudzianskas V., Jaselske E., Poskiene L., et al. (2020). Association of Angiogenesis and Inflammation-related G-ene F-unctional P-olymorphisms with E-arly-stage B-reast C-ancer P-rognosis. Oncol. Lett. 19 (6), 3687–3700. 10.3892/ol.2020.11521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krock B. L., Skuli N., Simon M. C. (2011). Hypoxia-induced Angiogenesis: Good and Evil. Genes & Cancer 2 (12), 1117–1133. 10.1177/1947601911423654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langfelder P., Horvath S. (2008). WGCNA: an R Package for Weighted Correlation Network Analysis. BMC Bioinforma. 9, 559. 10.1186/1471-2105-9-559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H., Wu X., Cheng X. (2016). Advances in Diagnosis and Treatment of Metastatic Cervical Cancer. J. Gynecol. Oncol. 27 (4), e43. 10.3802/jgo.2016.27.e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Zhang Y., Ruan R., He W., Qian Y. (2020). The Novel Interplay between CD44 Standard Isoform and the caspase-1/IL1B Pathway to Induce Hepatocellular Carcinoma Progression. Cell Death Dis. 11 (11), 961. 10.1038/s41419-020-03158-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberzon A., Subramanian A., Pinchback R., Thorvaldsdottir H., Tamayo P., Mesirov J. P. (2011). Molecular Signatures Database (MSigDB) 3.0. Bioinformatics 27 (12), 1739–1740. 10.1093/bioinformatics/btr260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J. J., Ho J. Y., Lee J. E., Hur S. Y., Yoo J., Kim K. R., et al. (2020a). Genomic, Transcriptomic, and Viral Integration Profiles Associated with Recurrent/metastatic Progression in High‐risk Human Papillomavirus Cervical Carcinomas. Cancer Med. 9 (21), 8243–8257. 10.1002/cam4.3426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Lu J., Li W. (2021). A Comprehensive Prognostic and Immunological Analysis of a New Three-Gene Signature in Hepatocellular Carcinoma. Stem cells Int. 2021, 1–25. 10.1155/2021/5546032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Meng L., Chen L., Liang Y., Wang B., Shao Q., et al. (2020b). IL‐6 Expression Promoted by Poly (I:C) in Cervical Cancer Cells Regulates Cytokine Expression and Recruitment of Macrophages. J. Cell Mol. Med. 24 (3), 2284–2293. 10.1111/jcmm.14911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manalo D. J., Rowan A., Lavoie T., Natarajan L., Kelly B. D., Ye S. Q., et al. (2005). Transcriptional Regulation of Vascular Endothelial Cell Responses to Hypoxia by HIF-1. Blood 105 (2), 659–669. 10.1182/blood-2004-07-2958 [DOI] [PubMed] [Google Scholar]
- Mao Y., Dong L., Zheng Y., Dong J., Li X. (2019). Prediction of Recurrence in Cervical Cancer Using a Nine-lncRNA Signature. Front. Genet. 10, 284. 10.3389/fgene.2019.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo Z., Yu L., Cao Z., Hu H., Luo S., Zhang S. (2020). Identification of a Hypoxia-Associated Signature for Lung Adenocarcinoma. Front. Genet. 11, 647. 10.3389/fgene.2020.00647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K. F., Lee W. J., Chou C. C., Yang Y. C., Chang Y. C., Chien M. H., et al. (2021). Direct Interaction of β‐catenin with Nuclear ESM1 Supports Stemness of Metastatic Prostate Cancer. EMBO J. 40 (4), e105450. 10.15252/embj.2020105450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payen V. L., Brisson L., Dewhirst M. W., Sonveaux P. (2015). Common Responses of Tumors and Wounds to Hypoxia. Cancer J. 21 (2), 75–87. 10.1097/PPO.0000000000000098 [DOI] [PubMed] [Google Scholar]
- Pencina M. J., D'Agostino R. B. (2004). Overall C as a Measure of Discrimination in Survival Analysis: Model Specific Population Value and Confidence Interval Estimation. Stat. Med. 23 (13), 2109–2123. 10.1002/sim.1802 [DOI] [PubMed] [Google Scholar]
- Peng X., Gong F., Chen Y., Jiang Y., Liu J., Yu M., et al. (2014). Autophagy Promotes Paclitaxel Resistance of Cervical Cancer Cells: Involvement of Warburg Effect Activated Hypoxia-Induced Factor 1-α-Mediated Signaling. Cell Death Dis. 5, e1367. 10.1038/cddis.2014.297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raab-Westphal S., Marshall J., Goodman S. (2017). Integrins as Therapeutic Targets: Successes and Cancers. Cancers 9 (9), 110. 10.3390/cancers9090110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren H., Zhu J., Yu H., Bazhin A., Westphalen C., Renz B., et al. (2020). Angiogenesis-Related Gene Expression Signatures Predicting Prognosis in Gastric Cancer Patients. Cancers 12 (12), 3685. 10.3390/cancers12123685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey S., Schito L., Wouters B. G., Eliasof S., Kerbel R. S. (2017). Targeting Hypoxia-Inducible Factors for Antiangiogenic Cancer Therapy. Trends Cancer 3 (7), 529–541. 10.1016/j.trecan.2017.05.002 [DOI] [PubMed] [Google Scholar]
- Rezaeian A.-H., Li C.-F., Wu C.-Y., Zhang X., Delacerda J., You M. J., et al. (2017). A Hypoxia-Responsive TRAF6-ATM-H2ax Signalling axis Promotes HIF1α Activation, Tumorigenesis and Metastasis. Nat. Cell Biol. 19 (1), 38–51. 10.1038/ncb3445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riecken L. B., Zoch A., Wiehl U., Reichert S., Scholl I., Cui Y., et al. (2016). CPI-17 Drives Oncogenic Ras Signaling in Human Melanomas via Ezrin-Radixin-Moesin Family Proteins. Oncotarget 7 (48), 78242–78254. 10.18632/oncotarget.12919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semenza G. L. (2012). Hypoxia-inducible Factors: Mediators of Cancer Progression and Targets for Cancer Therapy. Trends Pharmacol. Sci. 33 (4), 207–214. 10.1016/j.tips.2012.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian A., Tamayo P., Mootha V. K., Mukherjee S., Ebert B. L., Gillette M. A., et al. (2005). Gene Set Enrichment Analysis: a Knowledge-Based Approach for Interpreting Genome-wide Expression Profiles. Proc. Natl. Acad. Sci. U.S.A. 102 (43), 15545–15550. 10.1073/pnas.0506580102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sui H., Zhao J., Zhou L., Wen H., Deng W., Li C., et al. (2017). Tanshinone IIA Inhibits β-catenin/VEGF-mediated Angiogenesis by Targeting TGF-Β1 in Normoxic and HIF-1α in Hypoxic Microenvironments in Human Colorectal Cancer. Cancer Lett. 403, 86–97. 10.1016/j.canlet.2017.05.013 [DOI] [PubMed] [Google Scholar]
- Tao J., Yang G., Zhou W., Qiu J., Chen G., Luo W., et al. (2021). Targeting Hypoxic Tumor Microenvironment in Pancreatic Cancer. J. Hematol. Oncol. 14 (1), 14. 10.1186/s13045-020-01030-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleanu R. I., Chircov C., Grumezescu A. M., Teleanu D. M. (2019). Tumor Angiogenesis and Anti-angiogenic Strategies for Cancer Treatment. Jcm 9 (1), 84. 10.3390/jcm9010084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaupel P., Mayer A. (2007). Hypoxia in Cancer: Significance and Impact on Clinical Outcome. Cancer Metastasis Rev. 26 (2), 225–239. 10.1007/s10555-007-9055-1 [DOI] [PubMed] [Google Scholar]
- Vu M., Yu J., Awolude O. A., Chuang L. (2018). Cervical Cancer Worldwide. Curr. Problems Cancer 42 (5), 457–465. 10.1016/j.currproblcancer.2018.06.003 [DOI] [PubMed] [Google Scholar]
- Wang J., Li Z., Gao A., Wen Q., Sun Y. (2019). The Prognostic Landscape of Tumor-Infiltrating Immune Cells in Cervical Cancer. Biomed. Pharmacother. 120, 109444. 10.1016/j.biopha.2019.109444 [DOI] [PubMed] [Google Scholar]
- Wen Y., Zhou X., Lu M., He M., Tian Y., Liu L., et al. (2019). Bclaf1 Promotes Angiogenesis by Regulating HIF-1α Transcription in Hepatocellular Carcinoma. Oncogene 38 (11), 1845–1859. 10.1038/s41388-018-0552-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Chen X., Huang Z. (2019). Identification of ESM1 Overexpressed in Head and Neck Squamous Cell Carcinoma. Cancer Cell Int. 19, 118. 10.1186/s12935-019-0833-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Jiang B., Hai J., Duan S., Dong X., Chen C. (2019a). Long Noncoding RNA Opa‐interacting Protein 5 Antisense Transcript 1 Promotes Proliferation and Invasion through Elevating Integrin α6 Expression by Sponging miR‐143‐3p in Cervical Cancer. J Cell. Biochem. 120 (1), 907–916. 10.1002/jcb.27454 [DOI] [PubMed] [Google Scholar]
- Yang L., Roberts D., Takhar M., Erho N., Bibby B. A. S., Thiruthaneeswaran N., et al. (2018). Development and Validation of a 28-gene Hypoxia-Related Prognostic Signature for Localized Prostate Cancer. EBioMedicine 31, 182–189. 10.1016/j.ebiom.2018.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S., Wu Y., Deng Y., Zhou L., Yang P., Zheng Y., et al. (2019b). Identification of a Prognostic Immune Signature for Cervical Cancer to Predict Survival and Response to Immune Checkpoint Inhibitors. Oncoimmunology 8 (12), e1659094. 10.1080/2162402X.2019.1659094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Wu G., Li Q., Zheng Y., Liu M., Zhou L., et al. (2021). Angiogenesis-Related Immune Signatures Correlate with Prognosis, Tumor Microenvironment, and Therapeutic Sensitivity in Hepatocellular Carcinoma. Front. Mol. Biosci. 8, 690206. 10.3389/fmolb.2021.690206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B. (2012). CD73 Promotes Tumor Growth and Metastasis. Oncoimmunology 1 (1), 67–70. 10.4161/onci.1.1.18068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang B., Tang B., Gao J., Li J., Kong L., Qin L. (2020). A Hypoxia-Related Signature for Clinically Predicting Diagnosis, Prognosis and Immune Microenvironment of Hepatocellular Carcinoma Patients. J. Transl. Med. 18 (1), 342. 10.1186/s12967-020-02492-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Jiang L., Qin N., Cao M., Liang X., Wang R. (2021). hCINAP Is Potentially a Direct Target Gene of HIF-1 and Is Required for Hypoxia-Induced EMT and Apoptosis in Cervical Cancer Cells. Biochem. Cell Biol. 99 (2), 203–213. 10.1139/bcb-2020-0090 [DOI] [PubMed] [Google Scholar]
- Zheng W., Zhang S., Guo H., Chen X., Huang Z., Jiang S., et al. (2021). Multi-omics Analysis of Tumor Angiogenesis Characteristics and Potential Epigenetic Regulation Mechanisms in Renal Clear Cell Carcinoma. Cell Commun. Signal 19 (1), 39. 10.1186/s12964-021-00728-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: Clinical and transcriptome data were obtained from the TCGA (http://cancergenome.nih.gov/). The GSE52903 dataset was obtained from GEO (http://www.ncbi.nlm.nih.gov/geo/).