Abstract
Background
Increasing the price of alcohol reduces alcohol consumption and harm. The role of food complementarity, transaction costs and inflation on alcohol demand are determined and discussed in relation to alcohol price policies.
Methods
UK Biobank (N = 502,628) was linked by region to retail price quotes for the years 2007 to 2010. The log residual food and alcohol prices, and alcohol availability were regressed onto log daily alcohol consumption. Model standard errors were adjusted for clustering by region.
Results
Associations with alcohol consumption were found for alcohol price (β = −0.56, 95% CI, −0.92 to −0.20) and availability (β = 0.06, 95% CI, 0.04 to 0.07). Introducing, food price reduced the alcohol price consumption association (β = −0.26, 95% CI, −0.50 to −0.03). Alcohol (B = 0.001, 95% CI, 0.0004 to 0.001) and food (B = 0.001, 95% CI, 0.0005 to 0.0006) price increased with time and were associated (ρ = 0.57, P < 0.001).
Conclusion
Alcohol and food are complements, and the price elasticity of alcohol reduces when the effect of food price is accounted for. Transaction costs did not affect the alcohol price consumption relationship. Fixed alcohol price policies are susceptible to inflation.
Keywords: alcohol consumption, public health
Introduction
Fluctuations in the price of goods correspond with a change in the demand for those goods, otherwise known as the price elasticity of demand (PED).1 This applies to alcohol.2–4 An increase in alcohol retail price corresponds with a reduction in alcohol consumption and alcohol-related health harms.5–8 The evidence for this relationship between alcohol retail price and the demand for alcohol is mostly derived from studies examining variations in alcohol retail price over time.4,9 There are also several natural experiments in, for example, Finland and Canada3,6 where an abrupt change in alcohol price coincided with a change in alcohol-related health harms. This evidence has been used to motivate the implementation of a minimum unit (8 g ethanol) price (MUP) to challenge alcohol-related harm in Scotland10 and Wales11 in the UK. The estimates used to inform these policies broadly suggest a PED of ~ −0.5 for alcohol,4,12 meaning that for every 1% increase in alcohol price 0.5 fewer units of alcohol are consumed. These PED estimates informed a MUP of £0.50 in Scotland (May 2018) and Wales (March 2020).
While increasing alcohol retail price is regarded as one of the more effective policies available to reduce the harms from alcohol,13 price is only a component of the demand for alcohol. Both monetary and non-monetary factors influence consumer’s perception of retail price,14–16 meaning that it is alcohol affordability, the meaning given to price by consumers, that is the more appropriate operationalization of price. Affordability is typically defined as a function of price and household income, or residual income following the decision to purchase.17–20 This is notable as other costs should be expected to therefore influence residual income and therefore the demand for alcohol. Here we seek to develop the alcohol affordability construct and consider factors that are expected to influence the demand for alcohol and any implications for alcohol price policy.
First, in Canada and Finland the governments hold a monopoly over alcohol retail3,6: alcohol is typically sold in establishments separated from grocery stores. Conversely, alcohol is not subject to a state monopoly in the UK; it is available through various retail outlets, the prominent suppliers of which are local convenience stores and large grocery stores. In these retail outlets consumers can purchase alcohol, and other household goods alongside food.21,22 Consumers typically budget for their consumption23,24 and as food, a necessity, and alcohol, a luxury, are typically sold with a single point of sale in the UK, it is plausible that the price of food might influence the demand for alcohol. There are two ways to define such a relationship. First, that alcohol is a substitute to food, in which case the demand for alcohol would increase as the price of food increases (consumers spend less on food and purchase more alcohol in its place), or second, as a complement, when the price of food increases the demand for alcohol decreases. This relationship is formalized in Equation (1).
 |
(1) |
QA is the quantity of alcohol consumed and PF is the price of food. If Equation 1 is negative alcohol is a complement to food, if it is positive it is a substitute.25 The implication is that a complementary relationship would imply that food price could be a component of the demand for alcohol and this has not been appropriately determined.4,9
Second, both an increase in alcohol retail price and an increase in alcohol availability are associated with alcohol-related harm.13,26–28 In Canada it is observed that retail price and availability are independent, in respect of the demand for alcohol, and it is reasoned that greater availability means longer opening hours, and greater competition between outlets.26 We suggest a more parsimonious account placing availability as a feature of alcohol affordability. Greater availability implies easier access to alcohol and therefore lower transaction costs, the costs involved with transferring goods in store for consumption at home,29 due to, for example, lower travel costs. If alcohol availability and alcohol retail price are associated, as might be expected with greater competition where density is greater, then this may affect estimates of the PED for alcohol.
Finally, household income, a determinant of alcohol affordability, typically increases over time30 and does so variously by geographic region31 and industry sector.32 There is also a corresponding increase in retail price overtime.33 For example, the UK Consumer Price Index increased from 72.7 in 2000 to 108.8 in 2020.34 This is notable as the implementation of MUP10,11 is not index linked. If the price of beverages susceptible to MUP does not increase with inflation, then the affordability of these beverages is expected to increase over time, as a percentage of residual household income. The utility of a fixed MUP, and therefore estimates of the harms saved, should be expected to wane.
We assess the implications of complementarity, transaction costs and inflation on the demand for alcohol using UK Biobank cohort data linked to retail price data. In addition, models control for a range of individual and household characteristics variously associated with preferences for alcohol.
Methods
Between 2006 and 2010, a population sample of 502 649 adults aged 40–73 years participated in the UK Biobank prospective cohort study at 22 research centres (Appendix 1) located across the UK.35 Participants were registered with the UK National Health Service (NHS) and lived within a radius of 40 km from one of the research centres. Self-reported data were collected using touch-screen questionnaires and interviews35 and participant responses were record linked to routine NHS health data. Information on the assessment procedure, protocol and information on data access is available online (www.ukbiobank.ac.uk).
Data
Biobank
Ethical approval was granted to UK Biobank from the NHS Health Research Authority, Research Ethics Committee (reference 11/NW/0382). The current study was conducted using the UK Biobank Resource and pre-registered (approved application number 15008).
Biobank participants (mean age 57.03 years, SD = 8.09) were sampled from March 2006 to October 2010; 40,658 were non-drinkers (either former drinker or never drinker) and excluded. Drinkers reported either their average weekly or average monthly glasses of alcoholic beverages consumed (red wine, champagne or white wine, pint of beer or cider, spirits, fortified wine, other). Beverages were converted to grams of ethanol per typical glass (12 g red wine, 11.3 g white wine, 19.9 g beer, 9.2 g spirits, 9.6 g fortified wine). The question relating to ‘other’ alcoholic beverage specified alcopops containing an estimated 12 g alcohol. There were 387 160 available responses with consumption data (mean = 20.07 g/day, min = 0 g/day, max = 904.97 g/day) and following case-wise deletion on other regression variables, the final analytic sample was 226 548 participants (mean = 20.75 g/day, SD = 19.78).
Price data
The use of unweighted Office for National Statistics (ONS) price data follows methods described elsewhere.36 The ONS samples typically consumed services and items to derive the UK Retail Price and Consumer Price indices. The methodology describing the sampling is available elsewhere.37 The prices are collected by region (Appendix 1) each month. They are described by high level Divisions (Appendix 2), and more granular Groups and Classes. Two Divisions are of interest here, ‘Food and Non-Alcoholic Beverages’ and ‘Alcoholic Beverages and Tobacco’, these include the Groups ‘Alcoholic beverages’, ‘Tobacco’ and ‘Non-alcoholic beverages’ allowing prices for alcohol, tobacco and food to be separated. The unweighted average food item price was calculated by month and year and merged into the UK Biobank data by region (Appendix 1), and the month and year when participants completed the survey, as was the average price of alcohol.36 As the primary hypothesis concerns the retail sale of alcohol, alcohol was further described on an item by item basis according to whether the price quote was for on-trade (e.g. bars, nightclubs) or off-trade (e.g. grocery stores) by description (e.g. ‘bottle of lager in nightclub’) and price.36 The on-trade sale of alcohol carries a price premium therefore allowing items such as ‘spirit-based drink 275 ml’ to be identified as an on-trade beverage (Appendix 3). On-trade items were dropped. Finally, price quotes for several items in 2006 were missing descriptions and were apparently unique. Given 0.76% of UK Biobank participants were recruited in 2006, these data were dropped.
Alcohol availability
The UK Biobank Urban Morphometric Platform38 contains data concerning the neighbourhood in which residents live, including details of the density of premises licensed for the sale of alcohol within multiscale catchments of each UK Biobank participants’ residence. The variables describing the density of licensed premises (Public House, Bar or Nightclub; Restaurant or Cafeteria; Other Licensed Premise) within 1000 m were associated (Spearman ρ > 0.42, P < 0.001, for each comparison) and were reduced to a single ‘availability’ index using factor analysis (factor loadings were, respectively, 0.805, 0.821, 0.582).
Covariates
ICD10 diagnostic codes were available for all primary, secondary and external causes across all hospital inpatient records in UK Biobank. These were searched for alcohol-specific codes (Appendix 4)39 across all coding fields.40 Those with one or more alcohol-codes were identified and this binary variable included in analyses. Access to a car was included. Large out of town grocery stores have used alcohol as a loss-leader to attract custom41 and access to a car may therefore effect transaction costs. Additional demographic, and socioeconomic indicators were further included (Table 1). Missing values on household income were imputed using the median category (£31 000 to £51 999).
Table 1.
Descriptive statistics
| Mean | Proportion | 95% CI | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Alcohol consumption (g/day) | 20.751 | 20.669 | 20.832 | |
| Alcohol price (£) | 9.917 | 9.916 | 9.919 | |
| Food price (£) | 2.470 | 2.469 | 2.470 | |
| Alcohol availability | ||||
| Public house/bar/night club | 2.696 | 2.678 | 2.714 | |
| Restaurant/zafeteria | 4.123 | 4.087 | 4.159 | |
| Other licensed premise/vendor | 0.925 | 0.919 | 0.932 | |
| Household income | ||||
| < £18 000 | 0.160 | 0.159 | 0.162 | |
| £18 000 to £30 999 | 0.223 | 0.221 | 0.224 | |
| £31 000 to £51 999 | 0.355 | 0.353 | 0.357 | |
| £52 000 to £100 000 | 0.205 | 0.204 | 0.207 | |
| > £100 000 | 0.056 | 0.056 | 0.057 | |
| Socioeconomic status (Townsend) | −1.490 | −1.502 | −1.479 | |
| General health | ||||
| Excellent | 0.174 | 0.172 | 0.176 | |
| Good | 0.601 | 0.599 | 0.603 | |
| Fair | 0.192 | 0.191 | 0.194 | |
| Poor | 0.032 | 0.032 | 0.033 | |
| Age (years) | 56.848 | 46.815 | 56.880 | |
| Gender (male = 1) | 0.498 | 0.496 | 0.500 | |
| Ethnicity (white = 1) | 0.034 | 0.033 | 0.034 | |
| Qualifications | ||||
| College or university | 0.357 | 0.355 | 0.359 | |
| None | 0.132 | 0.131 | 0.134 | |
| Employment | ||||
| Paid employment | 0.603 | 0.601 | 0.605 | |
| Retired | 0.325 | 0.323 | 0.327 | |
| Sick | 0.021 | 0.021 | 0.022 | |
| Unemployed | 0.015 | 0.014 | 0.015 | |
| Voluntary | 0.032 | 0.032 | 0.033 | |
| Student | 0.002 | 0.002 | 0.002 | |
| Uses tobacco | 0.069 | 0.068 | 0.070 | |
| Access to a car | 0.837 | 0.832 | 0.842 | |
| Activity | ||||
| Moderate (days/week) | 3.622 | 3.612 | 3.632 | |
| Vigorous (days/week) | 1.912 | 1.904 | 1.920 | |
| Walk (days/week) | 5.411 | 5.403 | 5.419 | |
| Reducing alcohol consumption | ||||
| For health reasons | 0.175 | 0.174 | 0.177 | |
| For other reasons | 0.213 | 0.212 | 0.215 | |
| Self-diagnosis | ||||
| Neurological condition | 0.019 | 0.019 | 0.020 | |
| Alcohol problem | 0.001 | 0.000 | 0.001 | |
| Alcohol-specific ICD10 code | 0.004 | 0.003 | 0.004 | |
| Number of household occupants | ||||
| 1 | 0.168 | 0.167 | 0.170 | |
| 2 | 0.473 | 0.471 | 0.476 | |
| 3 | 0.159 | 0.157 | 0.160 | |
| 4 | 0.145 | 0.144 | 0.147 | |
| 5 | 0.040 | 0.039 | 0.041 | |
| 6 | 0.008 | 0.008 | 0.008 | |
| >6 | 0.006 | 0.006 | 0.007 | |
| Home owed outright | 0.528 | 0.526 | 0.530 | |
| Home owned with mortgage | 0.392 | 0.390 | 0.394 | |
| Season | ||||
| Spring | 0.279 | 0.277 | 0.281 | |
| Summer | 0.262 | 0.260 | 0.263 | |
| Autumn | 0.261 | 0.259 | 0.262 | |
| Winter | 0.199 | 0.197 | 0.201 | |
Analysis
Only respondents with non-zero alcohol consumption were included. Data were analysed using Ordinary Least Square regression in Stata MP v16.0,42 with standard errors corrected using ONS region.
Results
The ONS average price of alcohol was £9.83 (SD = 0.52, min = £8.69, max = £11.47) and the average price of food was £2.44 (SD = 0.18, min = £2.06, max = £2.77; Appendix 5). Both alcohol (B = 0.001, 95% CI 0.0004 to 0.001) and food (B = 0.001, 95% CI = 0.0005 to 0.0006) price increased linearly with time (Fig. 1), and an ordered logit also yielded a positive relationship between year of survey and household income (B = 0.088, 95% CI, 0.080 to 0.097).
Fig. 1 .
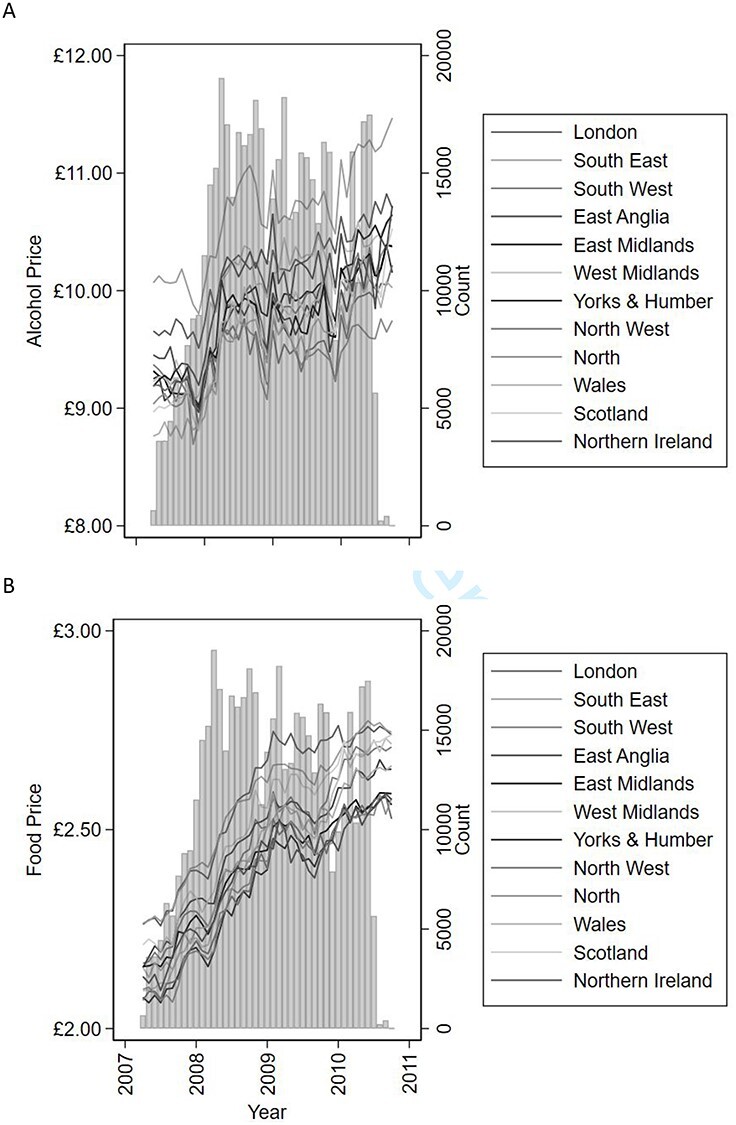
Number of UK Biobank participants recruited by month (panel A and panel B, vertical columns), overlaid with the average monthly price of alcohol across the 12 regions (panel A) and the average monthly price of food across the 12 regions (panel B).
While the planned analyses treated the available data as cross-sectional, the temporal aspect of the price data both had the advantage of variation across time and region, but required the data were detrended before inclusion in models. The predicted residuals had the minimum price added, plus one, so that the range did not cross zero, and the log was taken. Unadjusted regression (n = 226,608 for all analyses) of standardized log alcohol price on log alcohol consumption yielded a significant relationship (b = −0.64, 95% CI –0.66 to −0.61) and between the log price of food and log alcohol consumption (b = −1.48, 95% CI = −1.52 to −1.44). Table 1 presents descriptive statistics and Table 2 the full regression results. Log residual alcohol price and log residual food price were correlated (ρ = 0.57, P < 0.001), however the variance inflation factors (VIFs) suggest this association was not of concern (alcohol VIF = 1.60, food VIF = 1.63).
Table 2.
Full regression models for the price of alcohol, the price of food and alcohol availability on alcohol consumption
| Alcohol consumption (log g/day) | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | P | β | 95% CI | P | β | 95% CI | P | β | 95% CI | P | |||||
| Lower | Upper | Lower | Upper | Lower | Upper | Lower | Upper | |||||||||
| Log alcohol price | −0.559 | −0.924 | −0.195 | 0.013 | −0.264 | −0.500 | −0.028 | 0.036 | −0.569 | −0.944 | −0.194 | 0.014 | −0.261 | −0.498 | −0.025 | 0.037 |
| Log food price | −1.020 | −1.399 | −0.641 | 0.002 | −1.066 | −1.446 | −0.686 | 0.001 | ||||||||
| Alcohol availability | 0.049 | 0.028 | 0.071 | 0.003 | 0.056 | 0.038 | 0.074 | 0.001 | ||||||||
| Household income (reference: <£18 000) | ||||||||||||||||
| £18 000 to £30 999 | 0.073 | 0.057 | 0.089 | <0.001 | 0.082 | 0.059 | 0.105 | 0.001 | 0.071 | 0.056 | 0.085 | <0.001 | 0.080 | 0.059 | 0.101 | <0.001 |
| £31 000 to £51 999 | 0.108 | 0.061 | 0.156 | 0.003 | 0.125 | 0.065 | 0.184 | 0.004 | 0.105 | 0.062 | 0.147 | 0.002 | 0.121 | 0.066 | 0.176 | 0.004 |
| £52 000 to £100 000 | 0.220 | 0.128 | 0.312 | 0.003 | 0.247 | 0.141 | 0.354 | 0.003 | 0.213 | 0.129 | 0.298 | 0.002 | 0.241 | 0.141 | 0.340 | 0.003 |
| > £100 000 | 0.348 | 0.141 | 0.554 | 0.009 | 0.391 | 0.172 | 0.610 | 0.008 | 0.333 | 0.142 | 0.525 | 0.008 | 0.376 | 0.173 | 0.579 | 0.007 |
| Socioeconomic status (Townsend) | 0.020 | 0.007 | 0.033 | 0.013 | 0.024 | 0.006 | 0.042 | 0.020 | 0.015 | 0.002 | 0.028 | 0.034 | 0.018 | 0.001 | 0.036 | 0.045 |
| General health (reference: excellent) | ||||||||||||||||
| Good | −0.004 | −0.021 | 0.013 | 0.540 | −0.006 | −0.022 | 0.011 | 0.390 | −0.003 | −0.020 | 0.014 | 0.638 | −0.005 | −0.021 | 0.012 | 0.477 |
| Fair | −0.029 | −0.075 | 0.017 | 0.151 | −0.031 | −0.079 | 0.016 | 0.137 | −0.027 | −0.072 | 0.018 | 0.167 | −0.029 | −0.075 | 0.017 | 0.152 |
| Poor | −0.131 | −0.187 | −0.075 | 0.003 | −0.132 | −0.187 | −0.078 | 0.003 | −0.128 | −0.182 | −0.075 | 0.003 | −0.129 | −0.181 | −0.078 | 0.002 |
| Age (months/100) | −0.062 | −0.103 | −0.021 | 0.014 | −0.054 | −0.094 | −0.014 | 0.020 | −0.062 | −0.102 | −0.022 | 0.013 | −0.054 | −0.093 | −0.014 | 0.019 |
| Gender (male = 1) | 0.758 | 0.679 | 0.837 | <0.001 | 0.754 | 0.678 | 0.830 | <0.001 | 0.757 | 0.678 | 0.835 | <0.001 | 0.753 | 0.677 | 0.829 | <0.001 |
| Ethnicity (white = 1) | −0.685 | −0.978 | −0.392 | 0.003 | −0.642 | −0.956 | −0.327 | 0.005 | −0.682 | −0.965 | −0.400 | 0.003 | −0.637 | −0.937 | −0.336 | 0.004 |
| Qualifications | ||||||||||||||||
| College or university | −0.053 | −0.111 | 0.005 | 0.066 | −0.046 | −0.107 | 0.015 | 0.106 | −0.058 | −0.117 | 0.001 | 0.052 | −0.052 | −0.114 | 0.011 | 0.084 |
| None | 0.036 | −0.021 | 0.094 | 0.154 | 0.023 | −0.035 | 0.080 | 0.334 | 0.039 | −0.016 | 0.094 | 0.122 | 0.025 | −0.030 | 0.081 | 0.278 |
| Employment (reference: paid employment) | ||||||||||||||||
| Retired | 0.034 | 0.020 | 0.049 | 0.003 | 0.031 | 0.018 | 0.043 | 0.003 | 0.036 | 0.021 | 0.050 | 0.003 | 0.032 | 0.019 | 0.044 | 0.002 |
| Sick | 0.070 | 0.010 | 0.130 | 0.031 | 0.064 | −0.003 | 0.131 | 0.058 | 0.073 | 0.015 | 0.131 | 0.025 | 0.066 | 0.001 | 0.132 | 0.049 |
| Unemployed | 0.078 | 0.027 | 0.130 | 0.014 | 0.094 | 0.033 | 0.155 | 0.013 | 0.079 | 0.027 | 0.131 | 0.014 | 0.095 | 0.034 | 0.156 | 0.012 |
| Voluntary | −0.015 | −0.053 | 0.023 | 0.340 | −0.007 | −0.041 | 0.027 | 0.577 | −0.016 | −0.053 | 0.020 | 0.286 | −0.009 | −0.040 | 0.023 | 0.494 |
| Student | −0.065 | −0.123 | −0.007 | 0.036 | −0.059 | −0.103 | −0.015 | 0.021 | −0.066 | −0.125 | −0.008 | 0.035 | −0.060 | −0.104 | −0.016 | 0.019 |
| Uses tobacco | 0.370 | 0.294 | 0.446 | <0.001 | 0.371 | 0.291 | 0.450 | <0.001 | 0.370 | 0.291 | 0.448 | <0.001 | 0.370 | 0.288 | 0.452 | <0.001 |
| Access to a car | 0.009 | 0.005 | 0.013 | 0.003 | 0.006 | 0.001 | 0.011 | 0.025 | 0.011 | 0.007 | 0.015 | 0.001 | 0.008 | 0.004 | 0.012 | 0.007 |
| Activity | ||||||||||||||||
| Moderate (days/week) | <0.001 | −0.003 | 0.003 | 0.873 | 0.001 | −0.002 | 0.003 | 0.389 | <0.001 | −0.002 | 0.003 | 0.759 | 0.001 | −0.001 | 0.003 | 0.273 |
| Vigorous (days/week) | 0.007 | 0.001 | 0.013 | 0.033 | 0.007 | 0.001 | 0.013 | 0.035 | 0.007 | 0.001 | 0.013 | 0.029 | 0.007 | 0.001 | 0.013 | 0.029 |
| Walk (days/week) | 0.015 | 0.008 | 0.023 | 0.005 | 0.015 | 0.008 | 0.023 | 0.005 | 0.014 | 0.007 | 0.021 | 0.005 | 0.014 | 0.007 | 0.022 | 0.006 |
| Reducing alcohol consumption | ||||||||||||||||
| For health reasons | −0.193 | −0.212 | −0.174 | <0.001 | −0.193 | −0.209 | −0.177 | <0.001 | −0.194 | −0.213 | −0.175 | <0.001 | −0.193 | −0.209 | −0.178 | <0.001 |
| For other reasons | −0.489 | −0.542 | −0.436 | <0.001 | −0.488 | −0.543 | −0.433 | <0.001 | −0.488 | −0.540 | −0.436 | <0.001 | −0.487 | −0.542 | −0.432 | <0.001 |
| Self-diagnosis | ||||||||||||||||
| Neurological condition | −0.040 | −0.078 | −0.003 | 0.041 | −0.043 | −0.084 | −0.002 | 0.043 | −0.040 | −0.077 | −0.003 | 0.041 | −0.043 | −0.084 | −0.002 | 0.043 |
| Alcohol problem | 0.652 | 0.501 | 0.804 | <0.001 | 0.650 | 0.474 | 0.827 | 0.001 | 0.651 | 0.499 | 0.804 | <0.001 | 0.649 | 0.471 | 0.827 | 0.001 |
| Alcohol-specific ICD10 code | 0.580 | 0.388 | 0.773 | 0.001 | 0.582 | 0.398 | 0.766 | 0.001 | 0.579 | 0.384 | 0.775 | 0.001 | 0.581 | 0.393 | 0.769 | 0.001 |
| Number of household occupants (reference = 1) | ||||||||||||||||
| 2 | −0.009 | −0.035 | 0.018 | 0.414 | −0.018 | −0.036 | <0.001 | 0.048 | −0.004 | −0.032 | 0.024 | 0.725 | −0.013 | −0.032 | 0.006 | 0.127 |
| 3 | −0.087 | −0.099 | −0.075 | <0.001 | −0.093 | −0.109 | −0.076 | <0.001 | −0.080 | −0.095 | −0.065 | <0.001 | −0.085 | −0.103 | −0.067 | <0.001 |
| 4 | −0.136 | −0.153 | −0.118 | <0.001 | −0.138 | −0.157 | −0.119 | <0.001 | −0.128 | −0.149 | −0.107 | <0.001 | −0.130 | −0.150 | −0.109 | <0.001 |
| 5 | −0.183 | −0.227 | −0.138 | <0.001 | −0.180 | −0.217 | −0.144 | <0.001 | −0.175 | −0.226 | −0.124 | 0.001 | −0.172 | −0.215 | −0.128 | <0.001 |
| 6 | −0.194 | −0.292 | −0.095 | 0.005 | −0.189 | −0.293 | −0.086 | 0.007 | −0.185 | −0.278 | −0.093 | 0.005 | −0.180 | −0.275 | −0.084 | 0.006 |
| >6 | −0.179 | −0.306 | −0.052 | 0.017 | −0.175 | −0.307 | −0.044 | 0.021 | −0.175 | −0.297 | −0.053 | 0.017 | −0.171 | −0.297 | −0.044 | 0.020 |
| Home owed outright | 0.069 | 0.033 | 0.105 | 0.006 | 0.065 | 0.029 | 0.102 | 0.008 | 0.069 | 0.026 | 0.111 | 0.011 | 0.065 | 0.021 | 0.109 | 0.015 |
| Home owned with mortgage | 0.096 | 0.059 | 0.134 | 0.002 | 0.090 | 0.054 | 0.127 | 0.002 | 0.097 | 0.052 | 0.141 | 0.004 | 0.091 | 0.046 | 0.135 | 0.005 |
| Season (reference: spring) | ||||||||||||||||
| Summer | −0.043 | −0.088 | 0.002 | 0.057 | −0.044 | −0.096 | 0.008 | 0.079 | −0.045 | −0.086 | −0.005 | 0.036 | −0.047 | −0.093 | −0.001 | 0.047 |
| Autumn | −0.098 | −0.166 | −0.030 | 0.016 | −0.087 | −0.166 | −0.007 | 0.039 | −0.099 | −0.165 | −0.033 | 0.014 | −0.088 | −0.166 | −0.009 | 0.036 |
| Winter | −0.066 | −0.125 | −0.007 | 0.035 | −0.024 | −0.077 | 0.029 | 0.281 | −0.067 | −0.125 | −0.010 | 0.031 | −0.023 | −0.075 | 0.029 | 0.279 |
| Constant | 2.977 | 2.678 | 3.277 | <0.001 | 2.938 | 2.592 | 3.284 | <0.001 | 2.980 | 2.680 | 3.280 | <0.001 | 2.939 | 2.591 | 3.287 | <0.001 |
As food price and alcohol availability were added (Table 2) the coefficient on alcohol price reduced from −0.56 to −0.26 (Chow test χ2 = 13.76, P < 0.001). The coefficient on food price was negative (Model 4, Table 2), implying that the quantity of alcohol consumed decreases as the price of food increases.
The fully adjusted model (Model 4, Table 2) was repeated, stratifying by level of alcohol consumption. The current UK guidelines are that individuals should not consume more than 14 units (where 1 unit is 8 g ethanol) each week, equivalent to 16 g ethanol/day. Coefficients were compared for low consumption (<= 16 g/day, n = 119,461) to coefficients for those drinking over 16 g/day (n = 101 960). For each of alcohol price (low consumption β = −0.35, 95% CI, −0.38 to −0.32; high consumption β = 0.005, 95% CI, −0.01 to 0.02; χ2 = 5.31, P = 0.02), food price (low consumption β = −1.00, 95% CI = −1.06 to −0.94; high consumption β = −0.13, 95% CI, −0.16 to −0.09; χ2 = 8.26, P < 0.01) and availability (low consumption β = 0.05, 95% CI, 0.05 to 0.06; high consumption β = 0.01, 95% CI, 0.003 to 0.01; χ2 = 79.23, P < 0.001) coefficients significantly fell moving from low to high alcohol consumers, although there is no significant effect of alcohol price on alcohol consumption for high consumption individuals. Thus alcohol demand is more inelastic to changes in price for high alcohol consumers.
Finally, the fully adjusted model (Model 4, Table 2) was repeated stratifying by SES quintile to explore the policy relevance of the results by deprivation (Table 3).
Table 3.
Fully adjusted coefficients for alcohol price and log food price on log alcohol consumption (g/day) by socioeconomic quintile (a greater value represents greater deprivation)
| Alcohol (g/day) | Log alcohol price | Log food price | ||
|---|---|---|---|---|
| SES Townsend | n | Mean (95% CI) | β (95% CI) | β (95% CI) |
| −6.26 to −3.95 | 45 328 | 19.753 (19.589 to 19.917) | −0.159 (−0.350 to 0.031) | −1.187*** (−1.624 to −0.751) |
| −3.96 to −2.83 | 45 343 | 19.898 (19.728 to 20.068) | −0.217** (−0.377 to −0.057) | −1.101*** (−1.513 to −0.689) |
| −2.84 to −1.48 | 45 294 | 20.196 (20.020 to 20.373) | −0.217** (−0.361 to −0.072) | −1.238*** (−1.568 to −0.908) |
| −1.49 to 0.93 | 45 322 | 21.114 (20.923 to 21.305) | −0.270** (−0.435 to −0.105) | −1.100*** (−1.386 to −0.815) |
| 0.94 to 10.16 | 45 321 | 23.118 (22.894 to 23.343) | −0.486* (−0.859 to −0.112) | −0.747* (−1.334 to −0.161) |
*** P < 0.001,
** P < 0.01,
* P < 0.05.
Consistent with expectations, as the availability of alcohol increased, so did consumption. Household income and number of occupants, both likely to influence household finances, were associated with alcohol consumption. Those who had contacted healthcare services for alcohol-related reasons and those who self-diagnosed as having a ‘problem’ with alcohol consumed more alcohol, whereas those in general poor health consumed less alcohol. Students consumed less alcohol than their non-student peers, although given the age (mean age = 48.33 years, SD = 6.37) of the cohort UK Biobank students might be more mature than typically aged UK students.
Discussion
Main finding of this study
The initial relationship between price and alcohol consumption suggested a price elasticity of −0.56, within the margin of error of previous estimates.4,12 However, including the price of food, which is associated with the price of alcohol over time, reduced this estimate to −0.26, half previous estimates. This complementary relationship deserves further attention. In particular whether this is unique to countries where alcohol is sold alongside food21,22 and whether it generalizes to jurisdictions where alcohol is retailed separately from usual groceries. If the way alcohol is retailed influences consumption then consideration should be given to how alcohol is retailed in the UK and whether separate stores for alcohol and food, as is found in Canada and Finland for example, provide greater opportunity to challenge the harms associated with alcohol consumption. Furthermore, if the complementary relationship between alcohol and food described here is a consequence of how alcohol is retailed then pricing policies might be undermined if retailers offset an increase in alcohol price by reducing the price of food or increase the availability of alcohol.
Consistent with similar work, there was a robust dose–response relationship between income and alcohol consumption,19,43 confirming the role of affordability, which we broadened to include alcohol availability. Greater availability reduces transaction costs, a construct that may explain the relationship between access to a car and alcohol consumption as a car provides easier access to less expensive out-of-town grocery stores.41,44 We suggest that consumers are versatile, willing to alter how they acquire alcohol to maximize affordability, and may make greater use of local convenience stores as alcohol price increases as MUP is introduced44 as doing so reduces transaction costs. However, how different consumer groups might budget for alcohol alongside necessities such as food, and whether food is a necessity for those who are alcohol dependant deserves attention. Health, diet and alcohol are related,45,46 notably for dependant drinkers where a thiamine hydrochloride nutritional deficiency can contribute to brain injury.47,48 The effect of alcohol availability on consumption, however, did not influence the relationship between price and consumption, consistent with previous findings.26
In the UK, MUP has been set at £0.50 in Scotland10 and Wales11 but has not been index linked, meaning that the £0.50 MUP remains constant over time. Price inflation and an increase in household income was notable, stable characteristics of the UK economy. MUP imposes greater profit margins on low-cost alcohol and it is feasible that the retail price of these items will not increase inline with inflation. Residual household income for items susceptible to MUP may decline and the affordability of these items will increase. It would be perspicacious to adjust MUP according to the retail price and income indices. Without doing so the anticipated effectiveness of MUP should be expected to wane following implementation.
While the emphasis here is on financial disincentives to consume alcohol, it is notable that SES was associated with consumption. It is established that alcohol-related harm is greater in more deprived communities, despite the belief that there are comparable or lower levels of reported alcohol consumption compared to less deprived groups.49–51 The current analyses challenge this latter assumption, finding that alcohol consumption increases as deprivation increases. Moreover, the PED for alcohol increases as deprivation increases, suggesting that price policies maybe more effective in more deprived communities where both consumption and harm is greatest.
Limitations
The results presented here must be interpreted according to the limitations involved with cross-sectional research. Causation cannot be inferred, and it is feasible that those who choose to drink more alcohol are drawn to areas where alcohol and food are cheaper. This is partially offset by arguments that the demand for alcohol is causally associated with alcohol retail price.52 Further, UK Biobank is specific to those in middle and later life. However, in the UK, the age group most likely to experience alcohol-related hospital admission are between 45 and 64 years of age and 57% of all alcohol-specific deaths occur in the 50- to 69-year age group,53 suggesting the cohort considered here is relevant. Finally, there may be fixed regional differences in alcohol consumption that may confound estimates and that cannot be accounted for in the cross-sectional nature of the data analysed here.
In sum, alcohol is a complement to food, a relationship that has not been acknowledged in estimates of the PED for alcohol. If the results generalize outside of the cohort considered here, then the PEDs used in modelling policy effectiveness are likely overstated. But it is also feasible that the way alcohol is retailed may influence this relationship and that therefore separating alcohol and grocery sales, as is typical in many jurisdictions, should be considered. Alcohol price policy should also recognize heterogenous alcohol consumers and that high and low consumers may be impacted by price changes in food and alcohol to different extents. Further, any alcohol price policy should be index linked to account for variations in alcohol affordability over time.
What is already known on this subject?
As alcohol becomes more affordable alcohol consumption increases and this relationship has informed price polices, introduced to challenge alcohol-related harm.
What this study adds?
Alcohol consumption increases as food price decreases suggesting the price of food may also influence alcohol purchase decisions. This relationship has not been accounted for in estimates of reduced alcohol-related harm due to alcohol MUP policies in the UK and it is feasible such policies are less effective than currently assumed. Alcohol transactions costs, the costs of transferring alcohol in store for consumption at home, are independent in respective of alcohol demand and have no bearing on price policy. Both food and alcohol prices are susceptible to inflation, a feature not accounted for in fixed alcohol price policies.
Supplementary Material
Acknowledgements
This work was supported by funds from the Economic and Social Research Council, the Medical Research Council and Alcohol Research UK to the ELAStiC Project (ES/L015471/1). This work was conducted using the MRC Dementias Platform UK (DPUK; www.biorxiv.org/content/10.1101/582155v2). DPUK is a Public Private Partnership funded by the Medical Research Council (MR/L023784/1 and MR/009076/1). For further information on this resource visit www.dementiasplatform.uk. Jesse Smith acknowledges support from the Fulbright Commission and Cardiff University. We thank Allyson Smith for assistance with the ONS data. The funders had no role in the development of this manuscript or interpretation of data. We thank Yvette Amos for comments on an earlier version of this manuscript.
Simon C. Moore, Professor of Public Health Research
Orpen Bella, Research Assistant
Smith Jesse, Fulbright Scholar
Sarkar Chinmoy, Associate Professor of GIS, Urban Health and Environment
Chenlu Li, Risk Advisory Manager
Jonathan Shepherd, Emeritus Professor in Oral & Maxillofacial Surgery
Sarah Bauermeister, Senior Data & Science Manager
Contributor Information
Simon C Moore, Violence Research Group, School of Dentistry, Cardiff CF14 4XY, UK; Crime and Security Research Institute, Cardiff University, Cardiff CF10 3AE, UK.
Bella Orpen, Crime and Security Research Institute, Cardiff University, Cardiff CF10 3AE, UK.
Jesse Smith, Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement, School of Social Sciences, Cardiff University, Cardiff CF10 3BD, UK.
Chinmoy Sarkar, Healthy High Density Cities Lab, HKUrbanLab, The University of Hong Kong, Hong Kong.
Chenlu Li, Deloitte LLP, London EC4A 3HQ, UK.
Jonathan Shepherd, Violence Research Group, School of Dentistry, Cardiff CF14 4XY, UK; Crime and Security Research Institute, Cardiff University, Cardiff CF10 3AE, UK.
Sarah Bauermeister, Department of Psychiatry, University of Oxford, Warneford Hospital, Oxford OX3 7JX, UK.
Conflict of interest
None.
References
- 1. Bordley RF. Relating elasticities to changes in demand. J Bus Economic Stat 1985;3(2):156–8. [Google Scholar]
- 2. Hobday M, Gordon E, Lensvelt Eet al. The effect of price increases on predicted alcohol purchasing decisions and choice to substitute. Addict Res Theory 2016;24(6):441–9. [Google Scholar]
- 3. Stockwell T, Auld MC, Zhao Jet al. Does minimum pricing reduce alcohol consumption? The experience of a Canadian province. Addiction 2012;107(5):912–20. [DOI] [PubMed] [Google Scholar]
- 4. Wagenaar AC, Salois MJ, Komro KA. Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction 2009;104(2):179–90. [DOI] [PubMed] [Google Scholar]
- 5. Heeb JL, Gmel G, Zurbrugg Cet al. Changes in alcohol consumption following a reduction in the price of spirits: a natural experiment in Switzerland. Addiction 2003;98(10):1433–46. [DOI] [PubMed] [Google Scholar]
- 6. Herttua K, Makela P, Martikainen P. An evaluation of the impact of a large reduction in alcohol prices on alcohol-related and all-cause mortality: time series analysis of a population-based natural experiment. Int J Epidemiol 2011;40(2):441–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vaaramo K, Puljula J, Tetri Set al. Mortality of harmful drinkers increased after reduction of alcohol prices in northern Finland. Neuroepidemiology 2012;39(3–4):156–62. [DOI] [PubMed] [Google Scholar]
- 8. Wagenaar AC, Tobler AL, Komro KA. Effects of alcohol tax and price policies on morbidity and mortality: a systematic review. Am J Public Health 2010;100(11):2270–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Holmes J, Meng Y, Meier PSet al. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: a modelling study. Lancet 2014;383(9929):1655–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alcohol and drugs: minimum unit pricing: Scottish Government. Accessed October 2020. https://www.gov.scot/policies/alcohol-and-drugs/minimum-unit-pricing/.
- 11. Minimum unit pricing of alcohol: Welsh Government. Accessed October 2020. https://gov.wales/minimum-unit-pricing-alcohol.
- 12. Gallet CA. The demand for alcohol: a meta-analysis of elasticities. Aus J Agric Resource Economics 2007;51(2):121–35. [Google Scholar]
- 13. Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet 2009;373(9682):2234–46. [DOI] [PubMed] [Google Scholar]
- 14. Zeithaml VA. Consumer perceptions of price, quality, and value: a means-end model and synthesis of evidence. J Marketing 1988;52(3):2–22. [Google Scholar]
- 15. Samuelson PA. Consumption theory in terms of revealed preference. Dent Econ 1948;15(60):243–53. [Google Scholar]
- 16. Monroe KB. Buyers’ subjective perceptions of price. J Market Res 1973;10(1):70–80. [Google Scholar]
- 17. Niëns L, Van de Poel E, Cameron Aet al. Practical measurement of affordability: an application to medicines. Bull World Health Organ 2012;90:219–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brown A, Deaton A. Surveys in applied economics: models of consumer behaviour. Economic J 1972;82(328):1145–236. [Google Scholar]
- 19. Jiang H, Livingston M. The dynamic effects of changes in prices and affordability on alcohol consumption: an impulse response analysis. Alcohol Alcohol 2015;50(6):631–8. [DOI] [PubMed] [Google Scholar]
- 20. Nelson JP. Alcohol affordability and alcohol demand: cross-country trends and panel data estimates, 1975 to 2008. Alcohol Clin Exp Res 2014;38(4):1167–75. [DOI] [PubMed] [Google Scholar]
- 21. Nakamura R, Pechey R, Suhrcke Met al. Sales impact of displaying alcoholic and non-alcoholic beverages in end-of-aisle locations: an observational study. Soc Sci Med 2014;108:68–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Out of the Way? Alochol Displays in Supermarkets Cardiff: Alcohol Concern Cymru; 2011. Accessed October 2020. https://s3.eu-west-2.amazonaws.com/files.alcoholchange.org.uk/documents/Out_of_the_way_Final.pdf.
- 23. Thaler RH. Mental accounting matters. J Behav Decis Mak 1999;12(3):183–206. [Google Scholar]
- 24. Heath C, Soll JB. Mental budgeting and consumer decisions. J Consum Res 1996;23(1):40–52. [Google Scholar]
- 25. Moore SC. Substitution and complementarity in the face of alcohol-specific policy interventions. Alcohol Alcohol 2010;45(5):403–8. [DOI] [PubMed] [Google Scholar]
- 26. Zhao J, Stockwell T, Martin Get al. The relationship between minimum alcohol prices, outlet densities and alcohol-attributable deaths in British Columbia, 2002–09. Addiction 2013;108(6):1059–69. [DOI] [PubMed] [Google Scholar]
- 27. Chaloupka FJ, Wechsler H. Binge drinking in college: the impact of price, availability, and alcohol control policies. Contemp Econ Policy 1996;14(4):112–24. [Google Scholar]
- 28. Gartner A, Farewell DM, Morgan Jet al. Association between alcohol outlet density and alcohol-related mortality in Wales: an e-cohort study. Lancet 2017;390:S14. [Google Scholar]
- 29. Chintagunta PK, Chu J, Cebollada J. Quantifying transaction costs in online/off-line grocery channel choice. Mar Sci 2012;31(1):96–114. [Google Scholar]
- 30. Webber D, O'Neill J. Average Household Income, UK: Financial Year Ending 2019. London: Office for National Statistics, 2020. [Google Scholar]
- 31. Fenton T. Regional Gross Disposable Household Income, UK: 1997 to 2018. London: Office for National Statistics, 2020. [Google Scholar]
- 32. Chiripanhura B. Public and Private Sector Earnings: 2019. London: Office for National Statistics, 2020. [Google Scholar]
- 33. Hendry DF. Modelling UK inflation, 1875–1991. J Appl Economet 2001;16(3):255–75. [Google Scholar]
- 34. United Kingdom Consumer Price Index: 1988 to 2021; Accessed March 2021. Available from:www.rateinflation.com/consumer-price-index/uk-historical-cpi/.
- 35. Sudlow C, Gallacher J, Allen Net al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 2015;12(3):e1001779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Page N, Sivarajasingam V, Matthews Ket al. Preventing violence-related injuries in England and Wales: a panel study examining the impact of on-trade and off-trade alcohol prices. Inj Prev 2017;23(1):33–9. [DOI] [PubMed] [Google Scholar]
- 37. Inflation and price indices Office for National Statistics. Accessed October 2020. https://www.ons.gov.uk/economy/inflationandpriceindices.
- 38. Sarkar C, Webster C, Gallacher J. UK biobank urban morphometric platform (UKBUMP)–a nationwide resource for evidence-based healthy city planning and public health interventions. Ann GIS 2015;21(2):135–48. [Google Scholar]
- 39. Trefan L, Akbari A, Paranjothy Set al. Alcohol misuse: electronic longitudinal alcohol study in communities (ELASTiC) Wales protocol. Int J Population Data Sci 2019;4(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Trefan L, Akbari A, Morgan Det al. Visualisation and optimisation of alcohol-related hospital admissions ICD-10 codes in welsh e-cohort data. Int J Population Data Sci In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bennetts R. IAS briefing paper: Use of alcohol as a loss-leader. Institute of Alcohol Studies: St Ives, 2008. [Google Scholar]
- 42. StataCorp . Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC, 2019. [Google Scholar]
- 43. Jiang H, Livingston M, Room R. How financial difficulties interplay with expenditures on alcohol: Australian experience. J Public Health 2015;23(5):267–76. [Google Scholar]
- 44. Marshall G, Pires T. Measuring the impact of travel costs on grocery shopping. Economic J 2018;128(614):2538–57. [Google Scholar]
- 45. Jones NR, Tong TY, Monsivais P. Meeting UK dietary recommendations is associated with higher estimated consumer food costs: an analysis using the National Diet and nutrition survey and consumer expenditure data, 2008–2012. Public Health Nutr 2018;21(5):948–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Duffey KJ, Gordon-Larsen P, Shikany JMet al. Food price and diet and health outcomes: 20 years of the CARDIA study. Arch Intern Med 2010;170(5):420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Martin PR, Singleton CK, Hiller-Sturmhöfel S. The role of thiamine deficiency in alcoholic brain disease. Alcohol Res Health 2003;27(2):134. [PMC free article] [PubMed] [Google Scholar]
- 48. Sechi G, Serra A. Wernicke's encephalopathy: new clinical settings and recent advances in diagnosis and management. Lancet Neurol 2007;6(5):442–55. [DOI] [PubMed] [Google Scholar]
- 49. Katikireddi SV, Whitley E, Lewsey Jet al. Socioeconomic status as an effect modifier of alcohol consumption and harm: analysis of linked cohort data. Lancet Public Health 2017;2(6):e267–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McDonald SA, Hutchinson SJ, Bird SMet al. Association of self-reported alcohol use and hospitalization for an alcohol-related cause in Scotland: a record-linkage study of 23 183 individuals. Addiction 2009;104(4):593–602. [DOI] [PubMed] [Google Scholar]
- 51. Gartner A, Trefan L, Moore Set al. Drinking beer, wine or spirits–does it matter for inequalities in alcohol-related hospital admission? A record-linked longitudinal study in Wales. BMC Public Health 2019;19(1):1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Boniface S, Scannell JW, Marlow S. Evidence for the effectiveness of minimum pricing of alcohol: a systematic review and assessment using the Bradford Hill criteria for causality. BMJ Open 2017;7(5):e013497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Niblett, P. Statistics on Alcohol: England, 2018. London: NHS Digital, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


