Abstract
Eosinophilic oesophagitis is now being diagnosed more often, although there continues to be a significant delay in the recognition of the condition in primary care, and among patients presenting with food bolus obstruction to other specialities like Ears, Nose and Throat and Accident & Emergency. The diagnosis requires endoscopy and biopsy, with six biopsies taken from at least two different areas of the oesophagus. The diagnostic threshold is > 15 eosinophils/high power field or 0.3 mm2. Dietary management although effective is often difficult to carry out due to poor adherence by patients and the need for a specialist dietitian and repeated biopsies. Orodispersible budesonide is very effective for inducing remission and maintaining it long term, with fewer biopsies. Newer targeted biological agents are promising in the treatment of patients who have not responded to conventional treatments. Dilatation of strictures in this condition is safe.
Keywords: DYSPHAGIA, ENDOSCOPY
Key messages.
The diagnosis of eosinophilic oesophagitis is based on histology with >15 eosinophilis/high power field or 0.3 mm2.
Dietary restriction treatment is effective but difficult to implement due to poor adherence.
Orodispersible budesonide is effective treatment for induction of remission and maintenance of response.
Delayed diagnosis and treatment is likely to cause fibrostenotic disease.
Dilatation is safe and effective for stricturing disease.
Introduction
Eosinophilic oesophagitis (EoE) continues to be a challenging condition to diagnose in clinical practice and global epidemiological data indicate a significant delay in diagnosis ranging from 1.5 years to 8 years in both adults and children. The clinical presentation in children can be relatively non-specific with a wide range of symptoms while dysphagia and food bolus obstruction continue to be the predominant symptoms in adults. The diagnosis of EoE requires endoscopy and oesophageal biopsies and the diagnostic criteria are changing with the advent of digital pathology and the criteria for response and remission have also been defined in the last few years. This mini review aims to elucidate how to improve the diagnosis and treatment of this condition, and to prevent long-term fibrotic damage to the oesophagus resulting in strictures.
Clinical epidemiology and presentation
EoE was first described in 19891 but has been steadily increasing in incidence over recent decades. This increase in incidence over the last few decades has been irrespective of an increased awareness of the condition and endoscopic biopsy protocols—its prevalence ranges from 30 to 70/100 000.2
EoE is an allergic disease, likely related to allergen exposure both through the air and food. It is at least three times more common in males than females, in younger patients, and in those with a history of atopy.3
In adults and teenagers, the hallmark symptom is that of dysphagia,4 and in the acute situation, of food bolus obstruction, but in those with more chronic symptoms, diet and lifestyle may have been accommodated to tolerate these symptoms. Adult patients with classical gastro-oesophageal reflux disease (GORD) symptoms are unlikely to have a diagnosis of EoE, but the conditions can coexist.5 In children, symptoms are less specific and vary with age, including feeding difficulties even with failure to thrive, vomiting, abdominal pain, gastro-oesophageal reflux, chest pain, dysphagia and food impaction.6
Natural history of disease
Untreated EoE is associated with stricture formation, food bolus obstruction and need for emergency endoscopy.7 Furthermore, there are associated psychological implications to untreated disease and its effects on the ability of patients to eat, socialise and live without fear of food bolus obstruction. At least 25% of adult patients and 40% of children with EoE have symptoms of anxiety or depression.8 9
Diagnosis
Endoscopy
The diagnosis of EoE is made by endoscopy and oesophageal biopsy. Endoscopy should be performed to obtain histology from any patient in whom the clinician is suspicious of a diagnosis of EoE, with appropriate symptoms even in the absence of any endoscopic features of EoE. A normal endoscopy does not preclude the diagnosis of EoE, in the absence of biopsies.
Endoscopic features suggestive of disease include the presence of oedema (loss of vascular markings), rings (trachealisation), exudates (white plaques), furrows (vertical lines) and stricture (narrow calibre oesophagus).10 This is called the EREFS Score (Edema, Rings, Exudates, Furrows and Stricture, with each category having a score of 0, 1 or 2). Adults and children with clinical symptoms consistent with EoE such as dysphagia or food bolus obstruction should prompt endoscopists to take several biopsies from the oesophagus, even if it looks macroscopically normal; in one study, up to 8% of children with EoE had a normal appearing oesophageal mucosa.6
A Schatzki ring is also associated with EoE in almost 20% of cases, even in the absence of endoscopic signs of EoE.11
Biopsies should be obtained from any patient with dysphagia in whom no other explanation for their symptoms is found at endoscopy. In adults with reflux symptoms refractory to proton pump inhibitor (PPI) therapy, the yield of a positive diagnosis of EoE through routine biopsy is much lower and hence not indicated.5 In children, any child with chronic reflux symptoms not resolving on PPI should undergo endoscopy with multiple biopsies, especially if comorbidities may disguise clinical symptoms, for example, developmental or communication problems.
PPIs can inhibit eosinophil migration and reduce eosinophil counts, thus masking the diagnosis, and as such, it is usually recommended to withdraw PPI therapy for 3 weeks prior to endoscopy.12
Given the patchy nature of the disease,13 biopsy protocols have been proposed to increase the chance of histological confirmation. Eosinophil counts are typically higher in the stomach than the tubular oesophagus, and as such biopsies should be obtained from squamous mucosa within the tubular oesophagus away from the gastro-oesophageal junction. Thus, multiple biopsies from different sites in the oesophagus are considered optimal, with at least 6 biopsies offering a >97% chance of making a positive diagnosis.14
Histology
The definitive diagnosis of EoE is made by an elevated eosinophil count on oesophageal biopsy. This has typically been proposed as >15 eosinophils per high-power field.4 However, this threshold was based on conventional optical microscopy, and has not accounted for differences between conventional optical microscopes, with a potential for variation between institutions.13 An improvement to this threshold based on digital microscopy, with a eosinophil count of >60 eosinophils/mm2 was recently suggested as part of an International consensus statement.15 However, given the patchy nature of the disease, it has been proposed that counting eosinophil rich areas within a smaller field (0.3 mm2, which equates to a conventional optical high power field) may be more optimal. Therefore, a count of 15 eosinophils/0.3 mm2 (equivalent to 50 eosinophils/mm2) would provide a greater chance of a positive diagnosis.13
Management
Diet
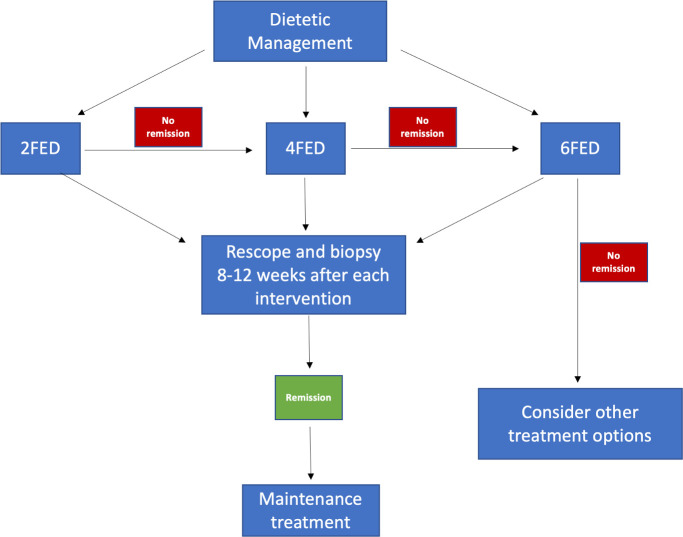
Dietary management of EoE involves the restriction of several foods that have been shown to be associated with oesophageal inflammation—these include gluten, milk, nuts, soya, fish and eggs. A desirable advantage of dietary therapy is that it has the potential to avoid drug use. However, there are considerable disadvantages and includes the fact that most patients with EoE have multiple food triggers and attempting to find which these are involves multiple endoscopies (average of seven endoscopies before a stable diet is established). The traditional approach to diet has been to eliminate many foods (six typically and these include wheat, milk, rice, legumes, eggs and seafood) but even this list is not comprehensive and only 70% of patients have successful induction of remission on these.16 Dietary restriction also involves reintroduction of foods, and obtaining oesophageal biopsies, which can be difficult both for the clinician and the patient, and very expensive. A further difficulty is that if more than two foods have to be excluded the compliance to such a diet is very poor in clinical practice. Even in clinical trials with enthusiastic specialist dietetic support, most patients (>60%) were unable to sustain their exclusion diet for more than a year (only 24/67 in one long-term elimination diet study in adults),17 and the psychological impact of such diets can be worse than the symptoms of the disease.18 Currently most centres supporting dietary therapy advocate a step up dietary exclusion starting with two foods, viz. milk and wheat and escalating to four and six-food elimination if no response is achieved with each step. These are the most common triggers of eosinophilic inflammation and up to 40% of patients may respond with clearance of inflammation and symptom improvement on dietary restriction. However, not all patients are compliant with a dietary approach and specialist dietitian involvement is usually required to avoid nutritional deficiencies (especially calcium and magnesium). Similar to drug therapies, the cessation of a successful diet is followed within a few months by return of symptomatic disease (figure 1).
Figure 1.
Dietary management algorithm. FED, food elimination diet.
In children, the decision for an elimination diet involves parental choices and concerns, and is more likely to be selected for younger children, with the parental wish to treat an underlying cause and to avoid potentially longer-term medication and fear of potential side effects. Moreover, about 50% of children have additional atopies, and a significant proportion are already on an elimination diet for IgE-mediated food allergies which however are considered to be unrelated to the development of EoE.6 While historically the concept had been to start with a six food elimination diet for faster symptom control which yielded remission rates of in 67%–70%, it is increasingly recognised that a step up approach with two food elimination diet (milk plus wheat or milk plus egg) accomplished also good remission rates of about 45%, is better tolerated, and can either be followed up by a step up approach (adding to the elimination either wheat or egg plus soya) or used as an acceptable maintenance therapy.6 16 19 However the review, advice and regular assessment of a paediatric dietitian is essential to prevent nutritional deficiencies.
Follow-up after therapy might in the future be more economical and more patient friendly if it could be done by a minimally invasive technique, such as the Cytosponge (Medtronic, USA). This device has been tested in screening dysphagia patients for EoE and has shown a 85% sensitivity and 75% specificity when compared with the gold standard of endoscopy and biopsy.20 However, more work needs to be done on this, so that the potential advantages of this non-invasive approach can be realised in routine practice.
Drugs
Proton pump inhibitors
The history of drug therapy for EoE had been fraught with unsuccessful outcomes where a range of 20%–60% of patients had therapeutic responses. Until recently no therapy was able to maintain successful therapy over a year in >50%.21 PPIs were found, rather by accident than design, to have a partial response in 70% but only a complete symptom response and histological response in 25%–40% and maintaining this for >1 year22 was only possible in 50% of those who initially responded, that is, 12%–20% of all patients. The mechanism of action of PPI response in EoE is a partial inhibition of the cytokine Eotaxin-3 which attracts eosinophils to the oesophagus, but they have no direct action on mast cells, fibroblasts or other cytokine mediators of the chronic inflammatory response in EoE. They may also improve epithelial barrier function through desmoglein. The effect of PPI in a European cohort of children was less convincing, reaching remission rates of only 25% as primary treatment.6
The role of steroids
For the past 10–15 years treatment of EoE has relied on the use of adapted products of topical steroid therapy for bronchial asthma. Swallowed sprays from inhalers, and the use of home-made mixtures of budesonide in syrups have had some degree of efficacy but complicated by misunderstanding among patients and care providers about their use, resulting in no standardisation of dose or delivery, as well as the majority of the drug not staying in the oesophagus with variable results. Systemic steroids are not indicated in EoE which is a chronic organ specific disease and the systemic use of steroids is complicated by potential serious systemic side effects, and by a lack of delivery of a high dose concentration to the oesophageal mucosa.
However, in the last few years, a specific formulation of topical steroid for oesophageal coating with budesonide has been available (Budesonide orodispersible tablets, Jorveza) and approved by Medicines and Healthcare products Regulatory Agency (MHRA) and National Institute for Health and Care Excellence in the UK; it has become the recommended therapy for induction of remission and maintenance of response in EoE.23 Topical budesonide is also safe and free of systemic steroid side effects because it is almost 90% metabolised in the liver during first pass after absorption from the gastrointestinal (GI) tract.
Budesonide orodispersible treatment (BOT) has been shown to be effective at 12 weeks during an induction of remission trial involving a course of 1 mg two times per day, with complete resolution of eosinophils in >90% of patients and in all parts of the oesophagus, and complete symptom remission in 85%.23 In the placebo-controlled trials, complete remission was seen in 84%, and a placebo symptom response seen in 12.5%.22 The quality of swallow improvement is dramatic for patients who are able to re-socialise and eat free of restrictions both in the type of food they eat and the company they can keep while eating, as reflected in the quality of life assessment in this study.
The side effects of orodispersible budesonide treatment are minimal, with oral thrush (candidiasis) being a symptomatic problem in 5% but easily treated with nystatin suspension for 10 days, without stopping the budesonide therapy.23 The medication is an effervescent tablet held on the tongue for up to 2 min while it dissolves in saliva, without taking any fluids. It is really important that the treatment is taken without washing it off the wall of the oesophagus where it will have its action. In contrast to taking asthma therapies, it is essential not to wash out the mouth after taking it, as even if the wash is spat out it will still remove much of the dissolved therapy from the saliva. We advise not eating or drinking for as long as possible in order to maximise therapeutic effect. The information for patients states that eating can occur after 30 min, but for optimal effect taking it last thing at night before going to bed, and after teeth brushing allows uninterrupted therapeutic application to the oesophagus for up to 8 hours. The second dose can be taken after meal such as the midday lunch, in a similar fashion.
For children, the preferred topical steroid is budesonide because the application of inhaled swallowed fluticasone is considered more difficult to implement practically and efficiently.6 While a licensed form of topical budesonide has been successfully introduced for induction and maintenance in Italy,24 another preparation is currently been evaluated in a placebo-controlled, randomised double blinded trial in several European countries including the UK.25 The effect of oral viscous budesonide formulations has been shown to accomplish remission rates of more than 70% in different carrier substances (in the UK comprising Splenda, Linctus, Ora-Blend, Honey and others according to local protocols).19 The dosage of 1 mg is used for children less than 150 cm or up to 11 years, or 2 mg for children from 12 years or greater 150 cm.26
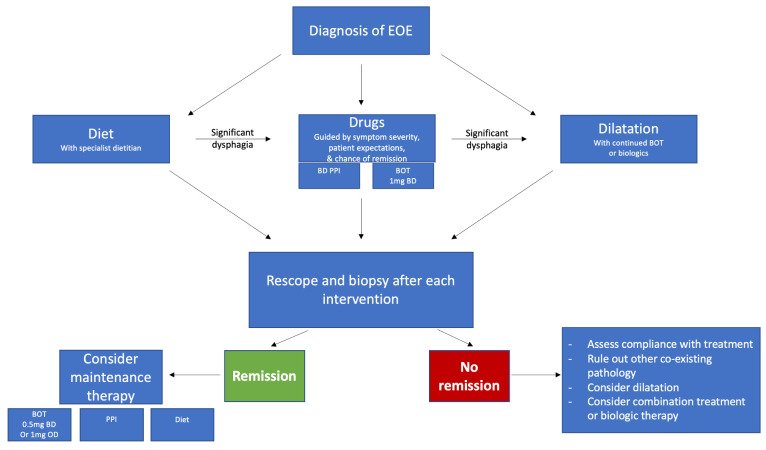
Studies subsequent to the pivotal trial on this therapy have all replicated the outcomes,27 showing that the therapy is equally effective in clinical practice and not just in a carefully controlled randomised clinical trial. EoE patients seen in routine practice are a mixture of those with daily severe symptoms and those who have intermittent and mild symptoms. The randomised clinical trial of BOT was performed in patients who had severe symptoms and who had already failed a trial of PPI therapy. It is likely that the rate of success would be higher in a trial of all comers rather than those who fail a PPI trial. Given the fact that the long-term remission on maintenance with PPI is only 12%–20% of the total patients with EoE, there is every expectation that the wider use of BOT will show a >65% efficacy of maintenance (histological and symptom normalisation) for all patients with EoE. This would dramatically improve the quality of life for all patients with EOE who have more than mild or occasional symptoms28 (figure 2).
Figure 2.
Management algorithm for eosinophilic oesophagitis (EOE). BOT, budesonide orodispersible treatment.
Current research on monoclonal antibodies using targeted anti-interleukin 4 receptor inhibitor (dupilumab) and anti-interleukin 5 receptor inhibitor (benralizumab) may introduce specific drugs targeted at cytokine blockade and other aspects of the Th2 inflammatory pathways in EoE. Dupilumab has recently received Food and Drug Administration (FDA) approval in the USA for use in EoE.
Dilatation
The indication for dilatation is stricture or for failure of symptoms to respond following BOT in a non-compliant oesophagus.29 It is important to understand that severe dysphagia can persist even when a stricture is not visible, because the lack of distensibility of the oesophageal wall can cause complete bolus obstruction even if the lumen looks open at endoscopy. A 12 mm bolus will get completely stuck in an oesophagus that is 11 mm diameter on endoscopy.
The frequency of a patient needing a dilatation therapy has greatly reduced since the introduction of effective topical steroid therapy. But if a patient has had chronic or severe symptoms it is important that they are offered a dilatation before deciding a therapy is unsuccessful. The fibrosis seen in chronic disease may take a lot longer than 3 months to resolve, and offering a dilatation but continuing the budesonide orodispersible tablets to maintain control of the inflammation will reduce recurrence of fibrosis. The whole oesophagus should be stretched not just a perceived narrowing and the lumen should optimally be brought to a size that is consistent with the patients size and behaviour—up to 18 mm diameter for younger patients who are likely to eat a steak, or perhaps 15 mm or less for an elderly patient who may be of slight build and likley to eat softer foods.29
Follow-up
It is well recognised that there is poor correlation between symptoms in patients with EoE and histological status.30 As such, it is generally considered best to treat to a histological remission (<15 eosinophils/high power field or 0.3 mm2) rather than symptom improvement alone, as patients with partial improvement in eosinophil count may report a higher response rate than their histology would suggest, and hence may lead to under treatment with the potential risk of subsequent stricture formation.
Data from dietary,31 PPI21 and orodispersible steroid treatments23 would suggest the optimal time for endoscopic re-assessment and biopsy would be within the 8–12 weeks range. In those in a histological remission, lower-dose maintenance therapy can be considered, and in those who have not achieved sufficient suppression of their eosinophil count to <15 eosinophils/0.3 mm2, alternative treatment options can be reviewed.
By using a therapy such as budesonide orodisperible tablets, that is effective in the majority (85%) of patients, the number of repeat endoscopies needed to find an effective therapy will be greatly reduced. In the current climate of difficult access to endoscopy a strategy that limits follow endoscopy to just one occasion is preferable to one that takes up to seven scopes (as with the six food elimination diet) depending on the type of elimination diet used and if a step up or top down approach has been chosen and implemented.
Summary and key points
The diagnostic criteria for EoE is a peak eosinophil count of >15 eosinophils/high power field or 0.3 mm2 in multiple oesophageal biopsies taken from different areas of the oesophagus.
Oesophageal biopsies must be taken even if the endoscopic appearance of the oesophagus is normal in a patient with a history of dysphagia or food bolus obstruction.
PPIs should be withdrawn for at least 3 weeks prior to endoscopy in any patient suspected to have this condition.
Dietary restriction with 2, 4 or 6-foods is effective in treatment but with low adherence rates and the need for a specialist dietitian overview and repeated biopsies.
Orodispersible treatment with budesonide is very effective in induction of remission and maintenance of remission over a 12-month period.
Confirmation of histological remission after treatment, with eosinophil count of <15/hpf is associated with better long term outcomes and lower fibrostenotic complications in EoE.
Newer targeted biological agents are promising to treat patients who lose response or do not respond to orodispersible steroids.
Footnotes
Twitter: @anjan_dhar6
Contributors: All authors contributed equally to the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Attwood SE, Furuta GT. Eosinophilic esophagitis: historical perspective on an evolving disease. Gastroenterol Clin North Am 2014;43:185–99. 10.1016/j.gtc.2014.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arias Á, Pérez-Martínez I, Tenías JM, et al. Systematic review with meta-analysis: the incidence and prevalence of eosinophilic oesophagitis in children and adults in population-based studies. Aliment Pharmacol Ther 2016;43:3–15. 10.1111/apt.13441 [DOI] [PubMed] [Google Scholar]
- 3. Dellon ES. Epidemiology of eosinophilic esophagitis. Gastroenterol Clin North Am 2014;43:201–18. 10.1016/j.gtc.2014.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lucendo AJ, Molina-Infante J, Arias Ángel, et al. Guidelines on eosinophilic esophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J 2017;5:335–58. 10.1177/2050640616689525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. García-Compeán D, González González JA, Marrufo García CA, et al. Prevalence of eosinophilic esophagitis in patients with refractory gastroesophageal reflux disease symptoms: a prospective study. Dig Liver Dis 2011;43:204–8. 10.1016/j.dld.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 6. Hoofien A, Dias JA, Malamisura M, et al. Pediatric eosinophilic esophagitis: results of the European retrospective pediatric eosinophilic esophagitis registry (RetroPEER). J Pediatr Gastroenterol Nutr 2019;68:552–8. 10.1097/MPG.0000000000002215 [DOI] [PubMed] [Google Scholar]
- 7. Schoepfer AM, Safroneeva E, Bussmann C, et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology 2013;145:1230–6. 10.1053/j.gastro.2013.08.015 [DOI] [PubMed] [Google Scholar]
- 8. de Rooij WE, Bennebroek Evertsz' F, Lei A, et al. Mental distress among adult patients with eosinophilic esophagitis. Neurogastroenterol Motil 2021;33:e14069. 10.1111/nmo.14069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris RF, Menard-Katcher C, Atkins D, et al. Psychosocial dysfunction in children and adolescents with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr 2013;57:500–5. 10.1097/MPG.0b013e31829ce5ad [DOI] [PubMed] [Google Scholar]
- 10. van Rhijn BD, Warners MJ, Curvers WL, et al. Evaluating the endoscopic reference score for eosinophilic esophagitis: moderate to substantial intra- and interobserver reliability. Endoscopy 2014;46:1049–55. 10.1055/s-0034-1377781 [DOI] [PubMed] [Google Scholar]
- 11. Müller M, Eckardt AJ, Fisseler-Eckhoff A, et al. Endoscopic findings in patients with Schatzki rings: evidence for an association with eosinophilic esophagitis. World J Gastroenterol 2012;18:6960–6. 10.3748/wjg.v18.i47.6960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Odiase E, Schwartz A, Souza RF, et al. New eosinophilic esophagitis concepts call for change in proton pump inhibitor management before diagnostic endoscopy. Gastroenterology 2018;154:e3:1217–21. 10.1053/j.gastro.2018.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gonsalves N, Policarpio-Nicolas M, Zhang Q, et al. Histopathologic variability and endoscopic correlates in adults with eosinophilic esophagitis. Gastrointest Endosc 2006;64:313–9. 10.1016/j.gie.2006.04.037 [DOI] [PubMed] [Google Scholar]
- 14. Dellon ES, Speck O, Woodward K, et al. Distribution and variability of esophageal eosinophilia in patients undergoing upper endoscopy. Mod Pathol 2015;28:383–90. 10.1038/modpathol.2014.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dellon ES, Liacouras CA, Molina-Infante J, et al. Updated international consensus diagnostic criteria for eosinophilic esophagitis: proceedings of the AGREE conference. Gastroenterology 2018;155:1022–33. 10.1053/j.gastro.2018.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kagalwalla AF, Sentongo TA, Ritz S, et al. Effect of six-food elimination diet on clinical and histologic outcomes in eosinophilic esophagitis. Clin Gastroenterol Hepatol 2006;4:1097–102. 10.1016/j.cgh.2006.05.026 [DOI] [PubMed] [Google Scholar]
- 17. Wang R, Hirano I, Doerfler B, et al. Assessing adherence and barriers to long-term elimination diet therapy in adults with eosinophilic esophagitis. Dig Dis Sci 2018;63:1756–62. 10.1007/s10620-018-5045-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reed CC, Corder SR, Kim E, et al. Psychiatric comorbidities and psychiatric medication use are highly prevalent in patients with eosinophilic esophagitis and associate with clinical presentation. Am J Gastroenterol 2020;115:853–8. 10.14309/ajg.0000000000000597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Algorithm for dietary management of eosinophilic oesophagitis (EoE) in paediatrics*. Available: https://bspghan.org.uk/wp-content/uploads/2021/11/Dietetic-management-of-EoE.pdf
- 20. Katzka DA, Smyrk TC, Alexander JA, et al. Accuracy and safety of the Cytosponge for assessing histologic activity in eosinophilic esophagitis: a two-center study. Am J Gastroenterol 2017;112:1538–44. 10.1038/ajg.2017.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Laserna-Mendieta EJ, Casabona S, Guagnozzi D, et al. Efficacy of proton pump inhibitor therapy for eosinophilic oesophagitis in 630 patients: results from the EoE connect registry. Aliment Pharmacol Ther 2020;52:798–807. 10.1111/apt.15957 [DOI] [PubMed] [Google Scholar]
- 22. Franciosi JP, Mougey EB, Dellon ES, et al. Proton pump inhibitor therapy for eosinophilic esophagitis: history, mechanisms, efficacy, and future directions. J Asthma Allergy 2022;15:281–302. 10.2147/JAA.S274524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lucendo AJ, Miehlke S, Schlag C, et al. Efficacy of budesonide Orodispersible tablets as induction therapy for eosinophilic esophagitis in a randomized placebo-controlled trial. Gastroenterology 2019;157:74–86. e15. 10.1053/j.gastro.2019.03.025 [DOI] [PubMed] [Google Scholar]
- 24. Oliva S, Rossetti D, Papoff P, et al. A 12-week maintenance therapy with a new prepared viscous budesonide in pediatric eosinophilic esophagitis. Dig Dis Sci 2019;64:1571–8. 10.1007/s10620-018-5449-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. EU Clinical Trials Register . Available: Https://www.clinicaltrialsregister.eu/ctr-search/search?query=eosinophilic+esophagitis
- 26. British Society of Paediatric Gastroenterology, Hepatology and Nutrition . Available: Https://bspghan.org.uk/1409-2
- 27. Miehlke S, Hruz P, Vieth M, et al. A randomised, double-blind trial comparing budesonide formulations and dosages for short-term treatment of eosinophilic oesophagitis. Gut 2016;65:390–9. 10.1136/gutjnl-2014-308815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Straumann A, Lucendo AJ, Miehlke S, et al. Budesonide Orodispersible tablets maintain remission in a randomized, placebo-controlled trial of patients with eosinophilic esophagitis. Gastroenterology 2020;159:1672–85. 10.1053/j.gastro.2020.07.039 [DOI] [PubMed] [Google Scholar]
- 29. Sami SS, Haboubi HN, Ang Y, et al. UK guidelines on oesophageal dilatation in clinical practice. Gut 2018;67:1000–23. 10.1136/gutjnl-2017-315414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ravi K, Talley NJ, Smyrk TC, et al. Low grade esophageal eosinophilia in adults: an unrecognized part of the spectrum of eosinophilic esophagitis? Dig Dis Sci 2011;56:1981–6. 10.1007/s10620-011-1594-1 [DOI] [PubMed] [Google Scholar]
- 31. Doerfler B, Bryce P, Hirano I, et al. Practical approach to implementing dietary therapy in adults with eosinophilic esophagitis: the Chicago experience. Dis Esophagus 2015;28:42–58. 10.1111/dote.12175 [DOI] [PubMed] [Google Scholar]