Abstract
The use of cross-sectional imaging and ultrasonography has long complemented endoscopic assessment of inflammatory bowel disease (IBD). Clinical symptoms alone are often not enough to assess disease activity, so a reliance on non-invasive techniques is essential. In this paper, we aim to examine the current use of radiological modalities in aiding the management of patients with IBD. We focus on the various sections of the gastrointestinal tract and how different modalities can aid in assessing current disease state and response to treatments. We also have a look at how newer sequences in cross-sectional imaging and ultrasonography can allow for better differentiation of disease activity (ie, fibrotic vs inflammatory) as well improve evaluation of small bowel, colonic and perianal disease. Furthermore, we examine how advanced image processing has the potential to allow radiology to be a surrogate for biomarkers. An example of this is explored when reviewing the ability of MR sequences to quantify visceral fat, which potentially plays a role in determining disease activity in Crohn’s disease. Lastly, we look into the expected role for artificial intelligence to be used as an adjunct to radiology to better improve IBD evaluation.
Keywords: magnetic resonance imaging, ultrasonography, inflammatory bowel disease, computer tomography, imaging
Key points.
Imaging modalities are key in the delivery of a treat-to-target approach especially where the disease location is inaccessible to ileocolonoscopy.
Ultrasonography has shown very good diagnostic accuracy for disease detection in both new-onset and established disease and is inexpensive. Despite this, access within the UK is limited to specialist and enthusiastic centres
Present diagnostic performance of MRI is excellent though reporting is often subjective. ECCO-ESGAR guidance should be followed to better standardise reporting.
Fibrosis is a complication of intestinal inflammation. Present modalities are not direct measures of intestinal fibrosis and may lack accuracy in the presence of intestinal inflammation. Novel sequences like T2 relaxometry and magnetisation transfer offer a promise in the holy grail of non-invasive accurate measures of intestinal fibrosis and inflammation.
Key points.
Other disease biomarkers like intestinal motility and to a lesser extent visceral fat measures offer strong promise.
Colonic imaging is its infancy. More work needs to be undertaken to completely validate this modality and ensure feasibility in an active inflammatory bowel disease population.
Perianal Crohn’s is a huge disease burden. Present objective MR-based scoring systems are cumbersome and not completely validated. More work is needed to accurately and reliably capture disease burden in this disease complication.
Imaging is an expensive modality that may be affected by subjective reporting by expert radiologists working within very high-volume radiology departments. Further work is needed to better absorb artificial intelligence to improve clinical performance.
Introduction
Endoscopic assessment of inflammatory bowel disease (IBD) can often be impractical and burdensome on both patient and clinician. Complementing endoscopy with radiological imaging has long been established practice in IBD care. With advancements in imaging, there have been great strides in the disease monitoring and management of IBD. Different imaging techniques, including MRI, CT and ultrasonography (US), have led to evolving clinical practice and guidelines. Furthermore, there is a growing role for the use of radiological modalities in researching novel IBD therapies. The aim of this review article is to examine the current modalities available to clinicians when treating IBD patients in an era of advancing technologies. Each modality has been shown to assess various anatomical locations of disease activity. We highlight disease in the small and large bowel and perianal area.
Treatment targets in IBD have increasingly revolved around achieving mucosal and histological remission.1 2 With this in mind, it is desirable that clinicians and radiologists have non-invasive techniques to measure disease activity that is comparable to ileocolonoscopy and histology. With the advancement in image processing, radiological modalities are likely to play a bigger role in monitoring therapies and assessment of postoperative outcomes and disease monitoring. This review will aim to focus on imaging modalities that are viable to be used as repeated measures of disease activity. Hence, we will aim to focus on MRI and small bowel US.
Small bowel
MRI
MRI is used as the gold-standard imaging technique for monitoring luminal small bowel Crohn’s disease (CD). Water-based oral contrast agents are used to distend the small bowel lumen and provide a positive contrast on T2-weighted images and negative contrast on T1-weighted images. The amount and type of oral preparation are set by local site preferences, however, generally at least 1 L of a poorly absorbable material (eg, mannitol solution) is needed for good bowel loop distension. The MR exam normally involves both T2-weighted scans (with and without fat saturation) and fat saturated T1-weighted scans pregadolinium and postgadolinium contrast. In addition, an antispasmodic drug is routinely given to reduce the bowel wall motion.
There has been significant research interest recently in capturing and quantifying the motility of the bowel with several groups producing various measures of the wall motion.3 The method used in MRI is called cine-MRI and involves capturing multiple images at the same location in the body (either in two dimensions or three dimensions (3D)) allowing the local displacement of the bowel walls to be visualised. In CD, there have been several papers which provide evidence that motility of the bowel is reduced in inflammatory disease and reduction in the terminal ileum motility has been linked to histology and endoscopy.4
Newer MR sequences such as diffusion-weighted imaging (DWI), magnetisation transfer (MT) imaging and dynamic contrast enhancement (DCE) imaging along with MR relaxometry (quantitative T1 and T2 imaging) have been investigated in the small bowel in the research domain. The principle aims of these newer sequences are to provide separate information on the inflammatory and fibrotic tissues in CD, which can be difficult to differentiate with conventional imaging, hence allowing for better-targeted treatments. The MT ratio (MTR) measured prospectively in vivo has been correlated with histopathological surgical samples and the degree of fibrosis was significantly positively correlated with MTR.5 For DWI, there have been several prospective and retrospective studies showing restricted diffusion in inflamed CD bowel loops. Many of these studies are single centre and small sample sizes and the lack of a standardised protocol for measuring the apparent diffusion coefficient makes interpretation more complex.6 DCE imaging, which looks to quantify the uptake of the gadolinium contrast in the tissue of interest, has also been applied retrospectively and prospectively in luminal CD and has been shown to be sensitive to inflammatory disease.7 All these newer sequences which provide potential biomarkers of CD need further prospective investigations and validation in large scale multicentre clinical trials to fully understand their potential in monitoring luminal CD. Table 1 selects some recent studies illustrating the diagnostic accuracy of MRI and US (which will be discussed later) in identifying fibrosis and inflammation compared with histopathological reference standards.
Table 1.
Studies measuring diagnostic accuracy of different MRI and US modalities in detecting fibrosis and inflammation in Crohn’s disease against histopathological/surgical specimens
| Author (n=number of study participants) |
Modality | Anatomical location | Fibrosis | Inflammation/Ulceration | ||
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |||
| Rimola et al n=4143 | MRI T2 | Small bowel, colonic | 94 | 89 | 85 | 100 |
| Huang et al n=2744 | MRI T2 | Small bowel | 92 | 90 | n/a | n/a |
| Zhang et al n=2645 | MRI-IVIM-DWI | Small bowel, colonic | 93 | 82 | n/a | n/a |
| Li et al n=315 | MT-MRI | Small bowel | 96 | 92 | n/a | n/a |
| Chen et al n=3546 | US+SWE | Small bowel, colonic | 70 | 92 | 88 | 58 |
| Ding et al n=2547 | US+pSWE | Small bowel, colonic | 75 | 100 | n/a | n/a |
IVIM-DWI, intravoxel incoherent motion-diffusion weighted imaging; MT, magnetisation transfer; n/a, not available; pSWE, point shear wave elastography; SWE, shear wave elastography; US, ultrasonography.
Visceral fat
Historically, energy storage has been considered the primary function of adipose tissue. However, it is now known that adipose tissue responds to and influences many physiological processes.8 Crohn et al had established the association between IBD and changes to mesenteric fat as increased visceral adipose tissue (VAT) volume in his original work.9 Since then, extensive work has been dedicated to understanding the role of mesenteric fat in IBD. Visceral fat hypertrophy, or fat wrapping, refers to the extension and thickening of mesenteric fat to cover the small or large intestine. Visceral fat hypertrophy has been found to correlate well with fibrosis, muscular hypertrophy, transmural inflammation and stricture formation.10
In the case of obesity, adipocytes enlarge, expanding VAT in the abdomen. However, histological evidence shows that in the case of visceral fat hypertrophy due to intestinal inflammation, the number of adipose cells increases around inflamed areas, and the cells become smaller in size and higher in density.11
The exact cause of fat wrapping in CD has been widely debated. Recent studies suggest that fat wrapping is triggered by the translocation of viable gut microbiota to mesenteric adipose tissue. While clinicians used to consider it an outcome of the disease pathology changes, relatively recent work indicates that it may be a contributing factor of inflammation as adipocytes in patients ith CD were found to be a source of cellular proinflammatory cytokines (tumour necrosis factor alpha and C reactive protein (CRP).12 Studies showed that the inclusion of the mesentery in ileocolic resection for CD is associated with a reduction in disease recurrence.13
In cross-sectional imaging, fat wrapping appears as an increased VAT volume. Figure 1 demonstrates this on MRI in a patient with CD compared with a healthy volunteer with similar body mass index. While CT has been extensively used to study VAT growth due to its sensitivity to tissue density, fat and water separation techniques in MRI have a vital role in evaluating fat tissue.14 Studies have attempted to assess the extent of fat wrapping in CD by segmenting the VAT and subcutaneous fat (SAT) and calculating the abdominal fat ratios (VAT:SAT), which were reported to be higher in patients with CD due to fat wrapping. Results show that abdominal fat ratios correlated well with disease activity measures like CRP, erythrocyte sedimentation rate and clinical disease activity scores.15 While most studies evaluating the extent of visceral fat hypertrophy in cross-sectional imaging use a single slice around the third lumbar spine (L3), volumetric measurements of abdominal fat could reveal more about visceral fat hypertrophy. Advancements in image processing and machine learning algorithms aid in characterising VAT and SAT tissues leading to easier adaptation of abdominal fat ratios as a biomarker for CD activity and progression.
Figure 1.
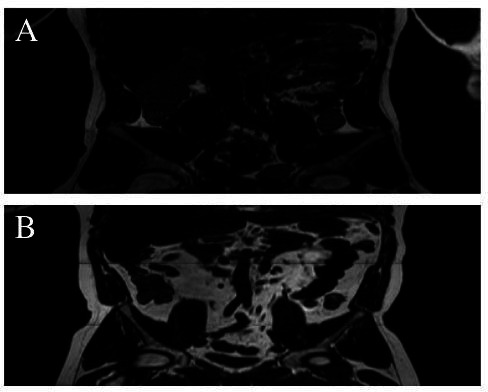
MR images of visceral adipose tissue as seen in Crohn’s disease (B) compared with healthy volunteer of same body mass index (A).
Ultrasonography
Small bowel (enteric) US is an alternative to MRE for assessment of small bowel CD, and has the potential to significantly reduce waiting times, speed up clinical decision making and improve patient experience and outcomes.16 17 US is well tolerated by patients with IBD.18 19 Besides being quick, well tolerated, relatively inexpensive and readily available, US is reported and interpreted at the time of scanning and allows for early clinical decision making in routine IBD care.16 20 21
US is widely used for assessing and monitoring IBD internationally.20 22 The National Insitute for Health and Care Research (NIHR)-funded METRIC (MR enterography or ultrasound in Crohn's disease) trial is the largest comparative diagnostic accuracy trial of MRE and US in CD. The study reported that sensitivity for detecting small bowel disease was 97% and 92% for MRE and US, respectively. Specificity was 96% for MRE and 84% for US.17 These findings were concordant in both new diagnosis and suspected relapse.17 23 Recent studies have also illustrated the use of US elastographyin detecting fibrosis in bowel segments, potentially adding a new dimension to US in IBD management.
There is an appetite for the uptake of US in the UK for assessment of CD, however, there remains a significant number of UK centres with little or no access to an US service.24 There is a reported difference in the levels of confidence that clinicians in the UK have in using US as a diagnostic tool, with clinicians reporting they are less confident using US than MRE to make clinical treatment decisions.24 The reason for this is likely multifactorial and will require a future programme of work to understand why this is the case.
Multiple sources refer to US being inexpensive, however, there is little empirical evidence within the included sources to support this claim, therefore future work related to assessing the cost-effectiveness of the use of US in IBD services is required.17 21 25
Recent unpublished work involving stakeholder (patients with IBD, gastroenterologists, radiologists, IBD nurse specialists and National Health Service (NHS) service managers) interaction has shown these end-users to be enthusiastic about the potential use of US in IBD services. Perceived barriers to US adoption in the UK may be related to willingness to change current working practices, access to training, financial outlay and service sustainability. An implementation framework or package of evidence is needed to better inform practice and allow a seamless expansion of this imaging platform.
Large bowel
MRI, CT and US have been used to assess colonic inflammation in IBD. With the comparison to the ileo-colonoscopy, these non-invasive tools are considered better tolerated and generally less costly. These non-invasive tools may possibly enhance the colonic disease outcomes by accelerating the decision making.
A recent meta-analysis reported that the specificity of US and MRI diagnostic modalities to predict active disease in patients with established or suspected IBD was excellent (91%) when using colonoscopy as the gold standard.26 This indicates there is great ability for these non-invasive tools to distinguish disease-active from disease-free patients. While for CD recurrence, accuracy and sensitivity of US for detecting CD were 91% and 94%, respectively, which indicates that US could provide high accurate assessment of the colonic disease activity.27 US was able to identify abnormal small and large bowel segments that were not detected on ileocolonoscopy, in 41 patients out of 115 in which CD was established or suspected.28
Recent work supports the possibility of using contrast-free MRI to evaluate the colonic inflammation accurately. To evaluate colonic CD lesions, T2-weighted (T2W) imaging had the same high accuracy of T1-weighted postcontrast sequences which could help to reduce the risks of having the gadolinium-based contrast, for instance, in patients with renal dysfunction.29
While the current clinical assessment of the T2W to measure the colonic inflammation is a qualitative based, recent studies have used the quantitative T2W which showed more objective disease assessments that could enhance the evaluation of the colonic inflammation in IBD.30 31
Perianal CD
MRI, endoanal ultrasound and perineal US are all modalities used in imaging perianal CD (pCD), dependent on local expertise, although MRI is currently the gold-standard modality for assessing perianal fistula. The European Crohn's and Colitis Organisation (ECCO) and European Society of Gastroenterology and Abdominal Surgery (ESGAR) (ECCO-ESGAR) produced joint guidance in 2021 on optimising radiologist reporting for cross-sectional imaging in IBD, including pCD. A list of key findings is described, which should be included in all reports, including number of fistulae/sinuses/abscesses, Park’s classification for each fistula, description of complex fistula features, and assessment of sphincter integrity.32 It is advocated to use a structured report and consistent terminology to more clearly convey findings and increase the reporting of relevant positive and negative findings to guide management.
Standard perianal MRI protocols include T2, fat-suppressed T2, and T1 preintravenous and postintravenous gadolinium contrast images in at least two planes. Active fistula tracts have high T2 signal (±T2 hypointensity of the fistula wall) and often surrounding oedema (hyperintense on T2). T1 enhancement is used to differentiate fluid or pus in the fistula from fibrosis or granulation tissue. Fistula activity can be assessed subjectively as predominantly fluid/pus filled (hyperintense T2 and rim enhancement on post-contrast T1), predominantly granulation tissue (hyperintense T2 and diffuse enhancement) or predominantly fibrosis (absent or mild intensity T2 and postcontrast T1).
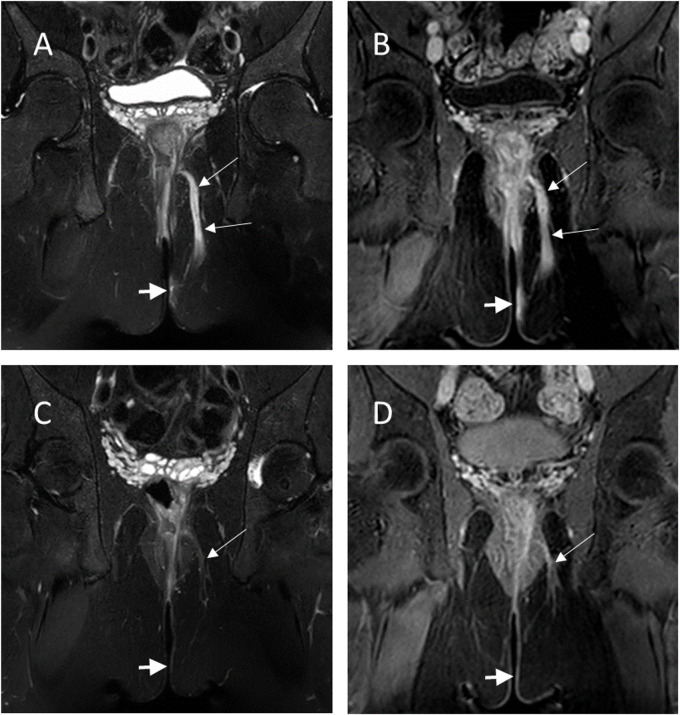
Assessing treatment response for perianal fistulae in CD using MRI may have great clinical significance, both for giving prognostic information as well as assessing long-term response to therapy (figure 2). This is challenging, however, as there is no clear definition of radiological healing. Features suggesting healing include reduction in number of tracts, tract length, extensions and collections, and specifically on MRI include reduction in T2 signal intensity, enhancing granulation tissue or progressively enhancing fibrosis within the tract on T1(37). The subjective nature of these appearances is a recognised limitation.
Figure 2.
MR images showing a perianal fistula (long white arrows), before (A, B) and after 3 months of biological therapy (C, D). A and C are T2-weighted fat saturated images, B and D are T1-weighted postcontrast images. Arrow heads show tissue inflammation as well as fistula tract have substantially reduced following treatment.
Scoring systems have been developed to allow more objective endpoints from the MR imaging data to aid in monitoring of the disease both in terms of disease progression and response to treatment. The first proposed score—the Van Assche Index utilised only the T2W images to describe six key features; including the anatomical location, extent of the fistulas and any collections of fluid along with the hyper-intensity signal from the T2W images indicating inflammatory response.33 This index was then modified to improve inter-rater reliability by removing features that produced poor agreement.34 However, a more recently published score from the same expert group also incorporated information from the T1-weighted postcontrast scans (MAGNIFI-CD) and out-performed the modified Van Assche in a retrospective study.35 These scoring systems are yet to be fully validated prospectively and time consuming for the expert radiologist to perform and would not be considered for routine clinical care—however, are important for driving forward research and treatment options by proving objective endpoints in clinical trials.
Newer MR sequences that allow more quantification from the images have also been applied to perianal fistulas. These include the use of MT imaging which shows promise at differentiating active from inactive fistulas by observing differences in fibrosis36 and DCE imaging which looks to model the uptake of the gadolinium contrast in the fistula tissue to assess the degree of inflammation.37 More recently quantitative T2 imaging has been applied to pCD with this parameter showing promise of predicting response to treatment when combined with other known influencing factors such as surgery, fistula complexity and baseline CRP levels.38 Although these newer sequences are not currently used clinically and take more time to setup and postprocess, their objective outcomes could allow for a more thorough investigation of the fistulas and better comparison when monitoring over longer time periods.
An area where more research and development is necessary is the visualisation and tracking of the fistulas in 3D. Simple volume measurements have been carried out showing changes with treatment,38 but there is currently no software available to assist the radiologist in defining and viewing the fistula in 3D. This has implications for quantitative imaging as well; with the ability to define the whole fistula tract from a previous scan allowing better comparison of quantitative parameters over the same region and not limiting to what was visible at the time of the current scan only. Artificial intelligence (AI) and improved image processing algorithms may be able to help drive this area forwards.
Automation and AI
Radiomics, computer vision, deep learning and AI promise a revolution in almost every field using cross-sectional medical imaging for diagnosis and follow-up, and this includes of course the IBD field. Automation could help the radiologists reduce interobserver variability, quantify bowel features and score staging more objectively.
Recent examples include semiautomated quantitative measurements (morphomics) of bowel features such as bowel wall thickness and dilation diameter of the lumen from CT enterography.39 This retrospective analysis of 138 exams showed very good maximum bowel wall thickness correlation between the semi-automated method and the mean measurement performed by two radiologists (r=0.702). Another retrospective, multicentre, CT enterography study on 167 patients aimed to classify bowel fibrosis by developing a radiomics model based on machine learning.40 In the test cohort, the radiomics model had good performance across the three centres, with area under the curve (AUC) between 0.724 and 0.816. A machine learning approach was proposed to segment MRI images of the bowel in CD.41 Data from 45 patients yielded a good level of accuracy in the segmentation with Dice values of 0.90±0.04. Another study reported successful segmentation of MRI images the bowel lumen and wall in 23 paediatric Crohn’s patients using curved planar reformatting and a convolutional neural network approach.42
The initial demonstrations show potential for AI applications to IBD cross-sectional imaging. These methods could in future support clinical routine though more studies, refinements and standardisation of approaches are needed.
Conclusion
Imaging has become a core feature of the holistic approach needed in the complex management of IBD. The quality in reporting IBD images is crucial in the management of patients, and the ECCO-ESGAR collaboration has set out to establish a standardised approach when reporting cross-sectional imaging. Hopefully this will allow for a more uniform understanding of disease activity when managing a patient with IBD.
Present non-invasive disease measures still need improving. US could play a more central role in the UK IBD management and possibly move from a radiologist-delivered intervention to a gastroenterologist or IBD nurse specialist delivered service at a UK-wide level. Although MRI is a more accurate test to aid in initial disease mapping, US is patient-friendly and less expensive, potentially allowing for a greater role in disease monitoring.
Fibrosis is an ever-present pathophysiological consequence of chronic inflammation. To this date, direct and reliable non-invasive measures are lacking. Until fibrosis and inflammation can be efficiently comeasured, it will be difficult to accurately measure disease burden, stratify patients appropriately to a surgical or medical-based management and accelerate the pharmacological pipeline of antifibrotic medication.
Finally, all these modalities need to be cost-effective, hence accuracy, speed and repeatability at an affordable price are successful variables to focus on. AI as shown in other clinical modalities has the capability to complement the excellent diagnostic skills of expert radiologists to deliver a better patient care throughout. More research is needed by enthusiastic and skilled IBD groups to deliver this promise.
Footnotes
Twitter: @Shellie_Jean
Contributors: GM is acting as the submission’s guarantor. NS, CLH, IN, MA, SJR, CC and LM have all contributed to the writing of this manuscript. GM is senior and corresponding author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: GM receives funding from AztraZenca and Jansen and is a consultant for Alimentiv.
Provenance and peer review: Commissioned; internally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an update on the selecting therapeutic targets in inflammatory bowel disease (STRIDE) initiative of the International organization for the study of IBD (IOIBD): determining therapeutic goals for Treat-to-Target strategies in IBD. Gastroenterology 2021;160:1570–83. 10.1053/j.gastro.2020.12.031 [DOI] [PubMed] [Google Scholar]
- 2. Bryant RV, Burger DC, Delo J, et al. Beyond endoscopic mucosal healing in UC: histological remission better predicts corticosteroid use and hospitalisation over 6 years of follow-up. Gut 2016;65:408–14. 10.1136/gutjnl-2015-309598 [DOI] [PubMed] [Google Scholar]
- 3. de Jonge CS, Smout AJPM, Nederveen AJ, et al. Evaluation of gastrointestinal motility with MRI: advances, challenges and opportunities. Neurogastroenterol Motil 2018;30:e13257. 10.1111/nmo.13257 [DOI] [PubMed] [Google Scholar]
- 4. Menys A, Puylaert C, Tutein Nolthenius CE, et al. Quantified terminal ileal motility during MR Enterography as a biomarker of Crohn disease activity: prospective Multi-Institution study. Radiology 2018;289:428–35. 10.1148/radiol.2018180100 [DOI] [PubMed] [Google Scholar]
- 5. Li X-H, Mao R, Huang S-Y, et al. Characterization of degree of intestinal fibrosis in patients with Crohn disease by using magnetization transfer MR imaging. Radiology 2018;287:494–503. 10.1148/radiol.2017171221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dohan A, Taylor S, Hoeffel C, et al. Diffusion-Weighted MRI in Crohn's disease: current status and recommendations. J Magn Reson Imaging 2016;44:1381–96. 10.1002/jmri.25325 [DOI] [PubMed] [Google Scholar]
- 7. Zhu J, Zhang F, Luan Y, et al. Can dynamic contrast-enhanced MRI (DCE-MRI) and diffusion-weighted MRI (DW-MRI) evaluate inflammation disease: a preliminary study of Crohn's disease. Medicine 2016;95:e3239. 10.1097/MD.0000000000003239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huh JY, Park YJ, Ham M, et al. Crosstalk between adipocytes and immune cells in adipose tissue inflammation and metabolic dysregulation in obesity. Mol Cells 2014;37:365–71. 10.14348/molcells.2014.0074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Crohn BB, Ginzburg L, Oppenheimer GD. Regional ileitis: a pathologic and clinical entity. 1932. Mt Sinai J Med 2000;67:1323–9. [PubMed] [Google Scholar]
- 10. Peyrin-Biroulet L, Chamaillard M, Gonzalez F, et al. Mesenteric fat in Crohn's disease: a pathogenetic hallmark or an innocent bystander? Gut 2007;56:577–83. 10.1136/gut.2005.082925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shen W, Li Y, Zou Y, et al. Mesenteric adipose tissue alterations in Crohn's disease are associated with the lymphatic system. Inflamm Bowel Dis 2019;25:283–93. 10.1093/ibd/izy306 [DOI] [PubMed] [Google Scholar]
- 12. Kredel LI, Siegmund B. Adipose-tissue and intestinal inflammation - visceral obesity and creeping fat. Front Immunol 2014;5:462. 10.3389/fimmu.2014.00462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Coffey CJ, Kiernan MG, Sahebally SM, et al. Inclusion of the mesentery in ileocolic resection for Crohn's disease is associated with reduced surgical recurrence. J Crohns Colitis 2018;12:1139–50. 10.1093/ecco-jcc/jjx187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Del Grande F, Santini F, Herzka DA, et al. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics 2014;34:217–33. 10.1148/rg.341135130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhou Z, Xiong Z, Shen Y, et al. Magnetic resonance imaging-based body composition is associated with nutritional and inflammatory status: a longitudinal study in patients with Crohn's disease. Insights Imaging 2021;12:178. 10.1186/s13244-021-01121-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Allocca M, Furfaro F, Fiorino G, et al. Point-Of-Care ultrasound in inflammatory bowel disease. J Crohns Colitis 2021;15:143–51. 10.1093/ecco-jcc/jjaa151 [DOI] [PubMed] [Google Scholar]
- 17. Taylor SA, Mallett S, Bhatnagar G, et al. Diagnostic accuracy of magnetic resonance enterography and small bowel ultrasound for the extent and activity of newly diagnosed and relapsed Crohn's disease (METRIC): a multicentre trial. Lancet Gastroenterol Hepatol 2018;3:548–58. 10.1016/S2468-1253(18)30161-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Grunshaw ND. Initial experience of a rapid-access ultrasound imaging service for inflammatory bowel disease. Gastrointestinal Nursing 2019;17:42–8. 10.12968/gasn.2019.17.2.42 [DOI] [Google Scholar]
- 19. Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 2019;13:144–64. 10.1093/ecco-jcc/jjy113 [DOI] [PubMed] [Google Scholar]
- 20. Bryant RV, Friedman AB, Wright EK, et al. Gastrointestinal ultrasound in inflammatory bowel disease: an underused resource with potential paradigm-changing application. Gut 2018;67:973–85. 10.1136/gutjnl-2017-315655 [DOI] [PubMed] [Google Scholar]
- 21. Radford SJ, Clarke C, Shinkins B, et al. Clinical utility of small bowel ultrasound assessment of Crohn’s disease in adults: a systematic scoping review. Frontline Gastroenterol 2022;13:280–6. 10.1136/flgastro-2021-101897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fraquelli M, Castiglione F, Calabrese E, et al. Impact of intestinal ultrasound on the management of patients with inflammatory bowel disease: how to apply scientific evidence to clinical practice. Dig Liver Dis 2020;52:9–18. 10.1016/j.dld.2019.10.004 [DOI] [PubMed] [Google Scholar]
- 23. Bhatnagar G, Quinn L, Higginson A, et al. Observer agreement for small bowel ultrasound in Crohn's disease: results from the METRIC trial. Abdom Radiol 2020;45:3036–45. 10.1007/s00261-020-02405-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Radford SJ, Taylor S, Moran G. Ultrasound use to assess Crohn’s disease in the UK: a survey of British Society of Gastroenterology Inflammatory Bowel Disease Group members. Frontline Gastroenterol 2022. 10.1136/flgastro-2021-102065. [Epub ahead of print: 18 Jan 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Novak KL, Wilson SR. Sonography for surveillance of patients with Crohn disease. J Ultrasound Med 2012;31:1147–52. 10.7863/jum.2012.31.8.1147 [DOI] [PubMed] [Google Scholar]
- 26. Alshammari MT, Stevenson R, Abdul-Aema B, et al. Diagnostic accuracy of non-invasive imaging for detection of colonic inflammation in patients with inflammatory bowel disease: a systematic review and meta-analysis. Diagnostics 2021;11. 10.3390/diagnostics11101926. [Epub ahead of print: 18 10 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martínez MJ, Ripollés T, Paredes JM, et al. Intravenous contrast-enhanced ultrasound for assessing and grading postoperative recurrence of Crohn's disease. Dig Dis Sci 2019;64:1640–50. 10.1007/s10620-018-5432-6 [DOI] [PubMed] [Google Scholar]
- 28. Wilkens R, Novak KL, Lebeuf-Taylor E, et al. Impact of intestinal ultrasound on classification and management of Crohn's disease patients with inconclusive colonoscopy. Can J Gastroenterol Hepatol 2016;2016:1–9. 10.1155/2016/8745972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Maccioni F, Bruni A, Viscido A, et al. MR imaging in patients with Crohn disease: value of T2- versus T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology 2006;238:517–30. 10.1148/radiol.2381040244 [DOI] [PubMed] [Google Scholar]
- 30. Hoad CL, Marciani L, Foley S, et al. Non-Invasive quantification of small bowel water content by MRI: a validation study. Phys Med Biol 2007;52:6909–22. 10.1088/0031-9155/52/23/009 [DOI] [PubMed] [Google Scholar]
- 31. Scott RA, Williams HG, Hoad CL, et al. MR measures of small bowel wall T2 are associated with increased permeability. J Magn Reson Imaging 2021;53:1422–31. 10.1002/jmri.27463 [DOI] [PubMed] [Google Scholar]
- 32. Kucharzik T, Tielbeek J, Carter D, et al. ECCO-ESGAR topical review on optimizing reporting for cross-sectional imaging in inflammatory bowel disease. J Crohns Colitis 2022;16:523–43. 10.1093/ecco-jcc/jjab180 [DOI] [PubMed] [Google Scholar]
- 33. Van Assche G, Vanbeckevoort D, Bielen D, et al. Magnetic resonance imaging of the effects of infliximab on perianal fistulizing Crohn's disease. Am J Gastroenterol 2003;98:332–9. 10.1016/S0002-9270(02)05909-9 [DOI] [PubMed] [Google Scholar]
- 34. Samaan MA, Puylaert CAJ, Levesque BG, et al. The development of a magnetic resonance imaging index for fistulising Crohn's disease. Aliment Pharmacol Ther 2017;46:516–28. 10.1111/apt.14190 [DOI] [PubMed] [Google Scholar]
- 35. Hindryckx P, Jairath V, Zou G, et al. Development and validation of a magnetic resonance index for assessing fistulas in patients with Crohn's disease. Gastroenterology 2019;157:1233–44. 10.1053/j.gastro.2019.07.027 [DOI] [PubMed] [Google Scholar]
- 36. Pinson C, Dolores M, Cruypeninck Y, et al. Magnetization transfer ratio for the assessment of perianal fistula activity in Crohn's disease. Eur Radiol 2017;27:80–7. 10.1007/s00330-016-4350-2 [DOI] [PubMed] [Google Scholar]
- 37. Horsthuis K, Lavini C, Bipat S, et al. Perianal Crohn disease: evaluation of dynamic contrast-enhanced MR imaging as an indicator of disease activity. Radiology 2009;251:380–7. 10.1148/radiol.2512072128 [DOI] [PubMed] [Google Scholar]
- 38. Alyami A, Hoad CL, Tench C, et al. Quantitative magnetic resonance imaging in perianal Crohn's disease at 1.5 and 3.0 T: a feasibility study. Diagnostics 2021;11. 10.3390/diagnostics11112135. [Epub ahead of print: 17 11 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stidham RW, Enchakalody B, Waljee AK, et al. Assessing small bowel Stricturing and morphology in Crohn's disease using semi-automated image analysis. Inflamm Bowel Dis 2020;26:734–42. 10.1093/ibd/izz196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Li X, Liang D, Meng J, et al. Development and validation of a novel Computed-Tomography Enterography radiomic approach for characterization of intestinal fibrosis in Crohn's disease. Gastroenterology 2021;160:2303–16. 10.1053/j.gastro.2021.02.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mahapatra D, Schuffler PJ, Tielbeek JAW, et al. Automatic detection and segmentation of Crohn's disease tissues from abdominal MRI. IEEE Trans Med Imaging 2013;32:2332–47. 10.1109/TMI.2013.2282124 [DOI] [PubMed] [Google Scholar]
- 42. Lamash Y, Kurugol S, Freiman M, et al. Curved planar reformatting and convolutional neural network-based segmentation of the small bowel for visualization and quantitative assessment of pediatric Crohn's disease from MRI. J Magn Reson Imaging 2019;49:1565–76. 10.1002/jmri.26330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rimola J, Planell N, Rodríguez S, et al. Characterization of inflammation and fibrosis in Crohn's disease lesions by magnetic resonance imaging. Am J Gastroenterol 2015;110:432–40. 10.1038/ajg.2014.424 [DOI] [PubMed] [Google Scholar]
- 44. Huang S-yun, Li X-hua, Huang L. T2* Mapping to characterize intestinal fibrosis in crohn’s disease. J Magn Reson Imaging 2018;48:829–36. 10.1002/jmri.26022 [DOI] [PubMed] [Google Scholar]
- 45. Zhang M-C, Li X-H, Huang S-Y, et al. IVIM with fractional perfusion as a novel biomarker for detecting and grading intestinal fibrosis in Crohn's disease. Eur Radiol 2019;29:3069–78. 10.1007/s00330-018-5848-6 [DOI] [PubMed] [Google Scholar]
- 46. Chen Y-J, Mao R, Li X-H, et al. Real-Time shear wave ultrasound elastography differentiates fibrotic from inflammatory strictures in patients with Crohn's disease. Inflamm Bowel Dis 2018;24:2183–90. 10.1093/ibd/izy115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ding S-S, Fang Y, Wan J, et al. Usefulness of strain elastography, ARFI imaging, and point shear wave elastography for the assessment of Crohn disease strictures. J Ultrasound Med 2019;38:2861–70. 10.1002/jum.14989 [DOI] [PubMed] [Google Scholar]