Abstract
Despite our understanding of pancreatic cancer (PC), the majority of patients with this disease are incurable. Both the incidence and mortality rates for PC have increased over the last decade. At diagnosis, the majority of patients have locally advanced PC, less than 20% of patients are eligible for potentially curative resection and approximately one-third have metastatic disease. The combination of frequent advanced presentation, low resection rates and poor responses to chemotherapy make PC one of the most lethal tumours. The treatment goals are to maintain local control, manage tumour-related morbidities and improve quality of life. Patients with inoperable PC are likely to experience significant symptoms associated with their tumour, including pancreatic insufficiency, nutritional deficiencies, pain, biliary obstruction, gastric outlet obstruction and diabetes. As a result, guidance on the management of patients with inoperable PC is critical. PC is commonly referred centrally to specialist centres particularly for surgery; however, the majority do not undergo surgical intervention and thus the importance of pancreaticobiliary physicians and endoscopists. This review will focus on the non-operative management of patients with unresectable pancreatic adenocarcinoma and review some of the issues that centralisation has contributed to.
Keywords: PANCREATIC CANCER, EXOCRINE PANCREATIC FUNCTION, DIABETES MELLITUS
Key messages.
Pancreatic cancer (PC) is one of the most important causes of cancer-related mortality among all solid organ malignancies, with less than 20% of patients eligible for potentially curative resection.
Cross-sectional imaging with contrast pancreas triple phase is the standard for diagnosis and staging of PC. Endoscopy ultrasound scan serves an important role when the diagnosis is uncertain, a biopsy is needed or therapeutic intervention.
The foundations of treatment for incurable PC are palliation and improving quality of life. Referral to palliative care specialists to help patients and their families to access and use palliative care services at the very beginning of treatment is beneficial.
Key messages.
Managing pain according to the ‘analgesic ladder’ is the standard approach. Neurolytic celiaccoeliac plexus block has been used to combat severe pain, at times, resulting in a decreased requirement for drugs and their unwanted side effects.
Symptoms of biliary and gastric outlet obstruction (GOO) can be treated with palliative interventions in a number of different ways, depending on patient choice and local expertise. Palliative endoscopic interventions have a very good success rate and should be the first choice in the majority of situations for biliary obstruction. GOO is more complicated and the therapeutic intervention depends uponon patient factors and local experience/availability.
Pancreatic exocrine replacement therapy is recommended in the majority of patients with PC in the head of the gland. However, the evidence for treatment is not associated with significant improvements in survival, weight change or quality of life in patients with advanced PC.
Introduction
Pancreatic cancer (PC) rarely has no symptoms in its early stages, posing a unique challenge for early detection, frequently referred to as a silent illness. By the time symptoms manifest, the majority of patients have either locally advanced or metastatic disease rendering them unsuitable for curative surgery.1 The signs and symptoms vary according to the stage of the disease and the location of the primary tumour: 70% of cases involve the pancreatic head, neck or uncinated process; 20% involve the body or tail; or 10% involve multifocal disease.2 The majority of pancreatic head tumours cause right-upper quadrant or epigastric pain (79%), jaundice (56%), nausea or vomiting due to gastric outlet obstruction (GOO) (51%), diarrhoea (43%) and steatorrhea due to pancreatic insufficiency (25%). Weight loss is common to all forms of PC and is often multifactorial.3 The vast majority are adenocarcinomas but other histological types can occur including adenosquamous and neuroendocrine tumours. This review will only cover adenocarcinomas. Table 1 shows the key areas of management for the PB physician.
Table 1.
Areas that require assessment and management in patients with unresectable pancreatic cancer: a toolbox
| Key area | Assessment | Management |
| Diagnosis | Adequate imaging (triple-phase pancreatic CT) and review in MDT. Tissue sampling usually by EUS |
Firm histological diagnosis made sufficient to allow systemic chemotherapy |
| Pain | Pain scores Pain ladder |
Optimisation of analgesia Use of adjuncts Coeliac plexus neurolysis |
| Biliary obstruction | Liver function tests and imaging showing dilated bile ducts | Predominantly ERCP and stent insertion PTC and stent insertion EUS-guided biliary drainage |
| GOO | GOO symptoms score Imaging showing dilated stomach |
Surgical gastrojejunostomy in patients with good prognosis Duodenal stent insertion Evolving role of EUS-guided gastrojejunostomy |
| Pancreatic exocrine insufficiency | Location of tumour increases risk (Head>body> tail) Faecal elastase level in selected cases |
Treatment with pancreatic enzyme replacement therapy in the high risk Dietitian assessment |
| Diabetes/glycaemic control | Capillary glucose HbA1c |
Dietitian assessment Early involvement of the diabetes team |
| Venous thromboembolic events | High index of suspicion Low threshold for treatment |
Use of low molecular weight heparin when thromboembolism detected |
| Mental health | Open discussion Specialist nurse assessment |
Review by cancer nurse specialist Early involvement of community palliative care team Consider treatment of depression/anxiety when detected |
ERCP, endoscopic retrograde cholangiopancreatography; EUS, endoscopic ultrasound; GOO, gastric outlet obstruction; HbA1a, Haemoglobin A1c; MDT, Multidisciplinary team meeting; PTC, Percutaneous Transhepatic cholangiography.
Diagnosis and treatment
There is no current screening programme for PC in the UK outside of clinical trials. Tumour markers such as carbohydrate antigen 19.9 (Ca 19.9) have low diagnostic value with a sensitivity of 70%–90% and of specificity 68%–91%. False positive Ca 19.9 has been seen in several areas particularly interstitial lung disorders and so is not useful as a diagnostic test even in jaundiced patients.4
The mainstay of diagnosis uses a combination of imaging and histology. Abdominal ultrasound is a reasonable first imaging test particularly in patients with jaundice but the pancreas is often not well visualised due to overlying bowel gas and does not give enough information about potential distant metastatic sites. Transabdominal ultrasound does not have sufficient sensitivity and specificity to exclude a diagnosis of PC. The current gold standard is triple-phase pancreatic CT scanning, which allows for full staging with a sensitivity of 89%–97% and specificity of 95%.5 As CT reporting is not ‘real time’ like ultrasound, images can be reviewed locally and at regional centres. MRI has similar sensitivity (81%–99%) and specificity (70%–93%) but is often not used first line in the UK due to better accuracy and staging of distant lesions with CT.6 All patients should be presented and discussed at a multidisciplinary team meeting dedicated to care of patients with PC. If deemed operable, then biopsy may or not be requested dependent on surgical preference. In cases where the diagnosis is uncertain or the tumour appears to be inoperable (either due to local or distant disease or patient factors) tissue sampling is needed to make the diagnosis and guide further treatments.6
Endoscopic ultrasound (EUS) is the modality of choice for sampling lesions in the pancreas. Historically, systematic reviews and meta-analyses of EUS with fine needle aspiration has reported a sensitivity and specificity of around 85% with various adjunctive techniques used to enhance yield. More recently, fine needle biopsy using novel needle designs has radically improved the yield of EUS-guided sampling such that sensitivity and accuracy are now >90% and inadequate sample rates are very low.7 This is clearly a role for the pancreaticobiliary (PB) physician as in the UK the majority of endoscopists performing EUS are gastroenterologists. It is important to decide which patients should go forward for EUS and biopsy. In patients with a clearly diagnostic CT scan and would not be considered fit for chemotherapy based on performance status do not require a biopsy. Obtaining a biopsy (which has a defined morbidity rate) should be offered to those patients in whom it will lead to meaningful change in their management and therapy.
Following biopsy, patients are usually referred to oncology for treatment and are usually discharged from gastrointestinal services. Whether this is best for patient outcomes is uncertain as ongoing gastrointestinal issues may be best dealt with by a gastroenterologist.
In the UK, the most common treatment is chemotherapy using regimens such as folfirinox or gemcitabine.8 Prognosis is still poor with overall survival currently being 6% at 5 years but there has been improvement in 1–2 year survival for those patients who are fit enough to endure regimens such as folfirinox. Despite there being clear benefits of receiving chemotherapy, one study showed that up to 50% of patients with advanced PC did not receive any chemotherapy.9 Therefore, it is important to establish the goals of treatment for patients with inoperable PC including symptom management, controlling disease progression, managing nutrition and maintaining quality of life.
Referral to palliative care early helps with developing relationships and accessing services pre-emptively. The main issues that a PB physician/endoscopist should get involved with are pain management, nutrition (including endocrine and exocrine insufficiency), biliary obstruction, GOO and thromboembolic risk.
Pain
Nearly 90% of patients suffer from pain in the advanced stages of PC, which can be difficult to manage. A multidisciplinary approach involving pain and palliative medicine specialists would be ideal. The mainstay of initial therapy is to optimise pharmacotherapy options for pain control but also to consider non-pharmaceutical options such as coeliac plexus neurolysis (CPN).10
Pain in PC can be caused by a variety of factors including tissue damage, inflammation, ductal obstruction and infiltration of adjacent structures. In addition, because of the proximity of the tumour to the coeliac axis, the pain often has a neuropathic element.
Managing pain according to the ‘analgesic ladder’ is considered the standard approach for pain control in patients with cancer. Adjunctive use of agents that treat neuropathic pain such as gabapentin or pregabalin may be beneficial.9 Opioid analgesia is often used but this does have other side effects particularly constipation and nausea leading to use of adjunctive medications. In unresectable PC, CPN can be employed to treat pain, which also has the benefit of reducing requirement for other analgesics and their unwanted side effects.
Treatment with CPN has been shown to be beneficial in addition to pharmacotherapy. According to a recent review, EUS-guided CPN is 72.54% effective in patients with PC.11 Furthermore, the morbidity of EUS-guided CPN has been reported to have low complication rates. Analgesic effects have been shown in studies to last one to 2 months, with one review showing up to 92% partial to complete relief after 3 months.12 It should be noted that CPN is not intended to be used in place of pharmacotherapy, but rather as an adjunctive treatment modality in selected patients.
Biliary obstruction
A common complication of PC is biliary tree obstruction resulting in jaundice. An estimated 65%–75% of patients with PC develop biliary obstruction for whom drainage is valuable to alleviate jaundice, pruritus and normalise bilirubin levels to allow palliative chemotherapy. Standard care is placement of a self-expanding metal stent at endoscopic retrograde cholangiopancreatography (ERCP); however, the success rate is less than 100%.13 Conventionally, following failed drainage via ERCP, patients are usually referred for percutaneous stent placement but recent data show this has a high morbidity.14 These data were generated from an assessment of the Hospital Episodes Statistics data which do have some limitations and did not compare both techniques directly. A previous meta-analysis showed that both techniques are largely comparable.15 EUS-guided biliary drainage (EUS-BD) has emerged as an alternative method. Studies comparing both techniques suggest both have similar safety profiles and EUS-BD was not superior to ERCP in terms of relief of malignant biliary obstruction.16 EUS-BD does have some advantages particularly in patients with an inaccessible ampulla either due to tumour invasion or duodenal narrowing.17
Despite this, EUS-BD is relatively new and requires further training in advanced EUS techniques. Additionally, recent UK data have shown that serious adverse events can still occur in up to 20%.17
Gastric outlet obstruction
GOO can occur in up to 25% of patients with unresectable PC and is associated with significant morbidity and decreased quality of life.18 Persistent nausea or vomiting, abdominal discomfort, fullness, early satiety or dehydration may all indicate GOO. Effective palliative treatments are critical in light of these associated symptoms and a significant decline in quality of life.
Historically, surgical gastrojejunostomy (SGJ) has been considered the gold standard palliative treatment for malignant GOO and has the best results for long-term palliation. However, some patients are not suitable for surgical intervention and therefore endoscopic stent insertion is an option. The main alternatives are duodenal stent (DS) insertion and EUS-guided gastroenterostomy (EUS-GE). The technical success rate of SGJ is high (>98%) and similar to DS insertion (>95%); however, time to resumption of oral intake is faster with DS (average 2–3 days) compared with SGJ (average 5–7 days) and can be performed under conscious sedation. Reintervention rates and stent dysfunction are more common with DS compared with SGJ (18% vs 1%).19 By combining the concepts of an endoscopically delivered stent and positioning away from the tumour, EUS-GE should be superior to either DS or SGJ. The early data show that EUS-GE has a lower success rate (88%) compared with SGJ but similar outcomes regarding adverse events, time to resumption of oral intake and length of stay.20 When compared with DS, the technical and clinical success rates are not statistically significantly different but EUS-GE has a lower reintervention rate (4% vs 20%).
Currently, patients with a short life expectancy should be considered for DS and fitter patients with longer life expectancy should be considered for SGJ or EUS-GE dependent on local expertise and availability.21
Pancreatic exocrine insufficiency
Pancreatic exocrine insufficiency (PEI) is a frequent finding in PC and is frequently caused by the tumour’s obstruction of the main pancreatic duct. PEI is more prevalent in tumours closer to the head of the pancreas and less so in those in the tail. Patients with PC often present with overlapping symptoms such as unintentional weight loss (80%), malnutrition (30%), chronic diarrhoea and steatorrhea all of which have a significant impact on quality of life. The use of pancreatic enzyme replacement therapy (PERT) in patients with PC who have undergone surgical resection is well shown to be beneficial but the evidence is less conclusive in patients with inoperable PC. The data on the role of PERT are conflicting mainly due to issues around study design, PERT dosage, measures of nutritional status and patient inclusion criteria.22 Some studies suggest improvement in survival for those taking PERT but meta-analysis of the four randomised trials showed no changes in weight loss or survival and there were no data on quality of life. There were no significant adverse events, but patients frequently discontinued treatment as their illness entered the terminal phase, with some citing pill burden as a factor. Also, for PERT to be useful, it must be used correctly, with a lot of emphasis on both the prescriber and the patient’s education. For lesions in the head of pancreas, the risk of PEI is very high and should be treated but when the tumour is located further along the pancreas, the risk is lower. The other consideration is the pill burden especially in those with advanced PC as adding a minimum of 16 additional capsules to their routine per day may not be beneficial. Nutritional assessment by a dietitian is also recommended to help with taking PERT but also to assess adequate calorie intake and help maintain weight. This would be especially important in those patients that receive chemotherapy. National Institute for Health and Care Excellence (NICE) guidelines recommend PERT for all; however, there is a paucity of data in patients with unresectable PC and therefore more data are needed to determine which patients are likely to benefit.22
Diabetes
Many cohort and case–control studies indicate that 25%–50% of patients with a diagnosis of PC will have developed diabetes mellitus (DM) within 1–3 years before their diagnosis of malignancy. This new-onset DM is therefore thought to be type 3c diabetes mellitus (T3cDM). Due to a lack of knowledge distinguishing between the two, T3cDM is frequently misdiagnosed as T2DM. T3cDM is the form of diabetes that occurs when the pancreas is damaged, leading to both exocrine and endocrine dysfunction. T3cDM, which is often linked to a history of chronic pancreatitis, PC, pancreatic resection, inflammation and fibrosis in pancreatic tissue. It is estimated that 9% of T3cDM is secondary to PC.23
There are no universally accepted diagnostic criteria for T3cDM. Conceptually, the diagnosis can be made in patients who meet the following three criteria: presence of PEI, pathological pancreatic imaging and absence of T1DM-associated autoimmune markers. Recognition of T3cDM is important as management is challenging due to erratic swings from hypoglycaemia to hyperglycaemic.23 Early referral to a dietitian and the diabetes healthcare team plays an important role in managing and preventing complications by tailoring the goals according to the need and life expectancy.
There were no distinct guidelines for the management of T3cDM in PC. In patients with mild hyperglycaemia, metformin can be used. However, in more severe cases, insulin is the treatment of choice. The nutritional management of T3cDM should include regular dietary assessment and treatment with PERT. Patients must be taking appropriate and adequate amounts of PERT to ensure optimal nutrient absorption and emphasise the importance of maintaining a regular eating pattern. The complications of T3cDM are associated with poorer survival at all stages of PC.24 Patients are more prone to severe episodes of hypoglycaemia due to the absence of other pancreatic hormones particularly glucagon. Patients should be educated on the symptoms and treatment of hypoglycaemia as for T1DM and blood glucose levels should be monitored regularly.
Venous thromboembolism
Venous thromboembolism (VTE) is a frequent but still underestimated complication that occurs in patients with PC, resulting in increased morbidity and mortality. Metastatic PC has imposed the most significant risk factor. Recently, in a large prospective multicenter cohort study of patients with PC, 20% of patients developed a VTE event. The cumulative rates of VTE were 13% at 6 months, 20% at 1 year, with a median time from PC diagnosis to VTE of 4 months.25
A systematic review and meta-analysis of patients with PC undergoing chemotherapy concluded that primary thromboprophylaxis was estimated to significantly reduce the risk of symptomatic VTE by approximately 69% with a number needed to treat of 11.9.26 Sensitivity analyses showed that primary prophylaxis with low molecular weight heparin or direct-acting oral anticoagulation, and prophylactic doses or supraprophylactic doses of anticoagulants reduced the risk of VTE by the same magnitude.
Despite multiple study recommendations, primary thromboprophylaxis has not been widely adopted in patients with PC in the community, mainly due to fear of bleeding and additional medication burdens in otherwise frail patients.
Systematic screening of VTE is not recommended in daily clinical practice. However, all patients with PC should receive education on the warning signs and symptoms of VTE to promote self-diagnosis and reporting of VTE symptoms. Decisions to initiate thromboprophylaxis should be made on a case-by-case basis and should be based on a multidisciplinary patient-centred approach after close discussion with the patient.27
Mental health and psychological support
The diagnosis of PC can seem to occur quite rapidly with the patient having to come to terms with having an incurable disease that will shorten their life expectancy quite markedly. One of the roles of the multidisciplinary team is to provide psychological and social support during this time and this is exemplified by cancer nurse specialists and the palliative care team. This area is especially important as a recent study showed a significant increase in psychological symptoms following diagnosis and that pre-existing depression or anxiety were associated with a decreased likelihood of receiving chemotherapy and overall reduced survival.28 Furthermore, it has been shown that carers of patients with PC also suffer from psychological stressors and that the prevalence of carer burden is significant.29 30 Psychological and social support for both the patient and family members is essential and should be addressed directly by all members of the multidisciplinary team.
Conclusions
The majority of patients with unresectable PC have multiple healthcare requirements above the need for tissue sampling including management of biliary and duodenal obstruction, pain, PEI, diabetes and thromboembolic risk (figure 1). The move towards centralisation has taken some of the resources away from non-tertiary centres meaning that those not suitable for resection may be at a disadvantage. The reasons for this are multifactorial but having clinicians with an interest in pancreatic diseases in non-tertiary centres with the knowledge and skills to manage such patients would be advantageous.26 This may improve patient experience and reduce the need for unnecessary travel for diagnostic and/or therapeutic procedures as well as non-procedural interventions when the focus of management is symptom control and quality of life.
Figure 1.
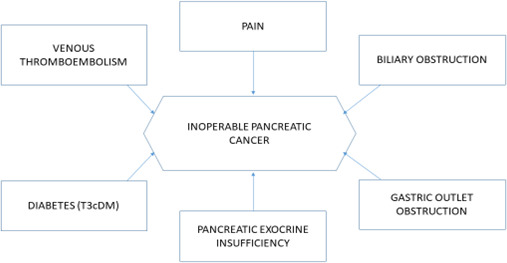
Managing symptoms of inoperable pancreatic cancer. T3cDM, type 3c diabetes mellitus.
Footnotes
Contributors: This was a commissioned article based upon a planned talk at BSG Live 2022 given by JL. The article was conceived by JL but cowritten with CCY.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. De La Cruz MSD, Young AP, Ruffin MT. Diagnosis and management of pancreatic cancer. Am Fam Physician 2014;89:626–32. [PubMed] [Google Scholar]
- 2. Artinyan A, Soriano PA, Prendergast C, et al. The anatomic location of pancreatic cancer is a prognostic factor for survival. HPB 2008;10:371–6. 10.1080/13651820802291233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Porta M, Fabregat X, Malats N, et al. Exocrine pancreatic cancer: symptoms at presentation and their relation to tumour site and stage. Clin Transl Oncol 2005;7:189–97. 10.1007/BF02712816 [DOI] [PubMed] [Google Scholar]
- 4. Rückert F, Pilarsky C, Grützmann R. Serum tumor markers in pancreatic cancer-recent discoveries. Cancers 2010;2:1107–24. 10.3390/cancers2021107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Valls C, Andía E, Sanchez A, et al. Dual-phase helical CT of pancreatic adenocarcinoma: assessment of resectability before surgery. AJR Am J Roentgenol 2002;178:821–6. 10.2214/ajr.178.4.1780821 [DOI] [PubMed] [Google Scholar]
- 6. Jimenez RE, Fernandez-Del Castillo C. Tumors of the Pancreas.. In: Sleisenger and Fordtran’s gastrointestinal and liver disease. Philadelphia, USA: Elsevier, 2010. [Google Scholar]
- 7. Nayar MK, Paranandi B, Dawwas MF, et al. Comparison of the diagnostic performance of 2 core biopsy needles for EUS-guided tissue acquisition from solid pancreatic lesions. Gastrointest Endosc 2017;85:1017–24. 10.1016/j.gie.2016.08.048 [DOI] [PubMed] [Google Scholar]
- 8. Smyth EN, Bapat B, Ball DE, et al. Metastatic pancreatic adenocarcinoma treatment patterns, health care resource use, and outcomes in France and the United Kingdom between 2009 and 2012: a retrospective study. Clin Ther 2015;37:1301–16. 10.1016/j.clinthera.2015.03.016 [DOI] [PubMed] [Google Scholar]
- 9. Henson KE, Fry A, Lyratzopoulos G, et al. Sociodemographic variation in the use of chemotherapy and radiotherapy in patients with stage IV lung, oesophageal, stomach and pancreatic cancer: evidence from population-based data in England during 2013-2014. Br J Cancer 2018;118:1382–90. 10.1038/s41416-018-0028-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Koulouris AI, Alexandre L, Hart AR, et al. Endoscopic ultrasound-guided celiac plexus neurolysis (EUS-CPN) technique and analgesic efficacy in patients with pancreatic cancer: a systematic review and meta-analysis. Pancreatology 2021;21:434–42. 10.1016/j.pan.2020.12.016 [DOI] [PubMed] [Google Scholar]
- 11. Kaufman M, Singh G, Das S, et al. Efficacy of endoscopic ultrasound-guided celiac plexus block and celiac plexus neurolysis for managing abdominal pain associated with chronic pancreatitis and pancreatic cancer. J Clin Gastroenterol 2010;44:127–34. 10.1097/MCG.0b013e3181bb854d [DOI] [PubMed] [Google Scholar]
- 12. Koulouris AI, Banim P, Hart AR. Pain in patients with pancreatic cancer: prevalence, mechanisms, management and future developments. Dig Dis Sci 2017;62:861–70. 10.1007/s10620-017-4488-z [DOI] [PubMed] [Google Scholar]
- 13. Williams EJ, Taylor S, Fairclough P, et al. Are we meeting the standards set for endoscopy? results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut 2007;56:821–9. 10.1136/gut.2006.097543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rees J, Mytton J, Evison F, et al. The outcomes of biliary drainage by percutaneous transhepatic cholangiography for the palliation of malignant biliary obstruction in England between 2001 and 2014: a retrospective cohort study. BMJ Open 2020;10:e033576. 10.1136/bmjopen-2019-033576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Duan F, Cui L, Bai Y, et al. Comparison of efficacy and complications of endoscopic and percutaneous biliary drainage in malignant obstructive jaundice: a systematic review and meta-analysis. Cancer Imaging 2017;17:27. 10.1186/s40644-017-0129-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park JK, Woo YS, Noh DH, et al. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc 2018;88:277–82. 10.1016/j.gie.2018.03.015 [DOI] [PubMed] [Google Scholar]
- 17. On W, Paranandi B, Smith AM, et al. EUS-guided choledochoduodenostomy with electrocautery-enhanced lumen-apposing metal stents in patients with malignant distal biliary obstruction: multicenter collaboration from the United Kingdom and ireland. Gastrointest Endosc 2022;95:432–42. 10.1016/j.gie.2021.09.040 [DOI] [PubMed] [Google Scholar]
- 18. Tendler DA. Malignant gastric outlet obstruction: bridging another divide. Am J Gastroenterol 2002;97:4–6. 10.1111/j.1572-0241.2002.05391.x [DOI] [PubMed] [Google Scholar]
- 19. Boghossian MB, Funari MP, De Moura DTH, et al. EUS-guided gastroenterostomy versus duodenal stent placement and surgical gastrojejunostomy for the palliation of malignant gastric outlet obstruction: a systematic review and meta-analysis. Langenbecks Arch Surg 2021;406:1803–17. 10.1007/s00423-021-02215-8 [DOI] [PubMed] [Google Scholar]
- 20. Khashab MA, Bukhari M, Baron TH, et al. International multicenter comparative trial of endoscopic ultrasonography-guided gastroenterostomy versus surgical gastrojejunostomy for the treatment of malignant gastric outlet obstruction. Endosc Int Open 2017;5:E275–81. 10.1055/s-0043-101695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Papanikolaou IS, Siersema PD. Gastric outlet obstruction: current status and future directions. Gut Liver 2022. 10.5009/gnl210327. [Epub ahead of print: 22 Mar 2022]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ammar K, Leeds JS, Ratnayake CB, et al. Impact of pancreatic enzyme replacement therapy on short- and long-term outcomes in advanced pancreatic cancer: meta-analysis of randomized controlled trials. Expert Rev Gastroenterol Hepatol 2021;15:941–8. 10.1080/17474124.2021.1884544 [DOI] [PubMed] [Google Scholar]
- 23. Hart PA, Bellin MD, Andersen DK, et al. Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer(CPDPC). Type 3c (pancreatogenic) diabetes mellitus secondary to chronic pancreatitis and pancreatic cancer. Lancet Gastroenterol Hepatol 2016;1:226–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li D, Yeung S-CJ, Hassan MM, et al. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology 2009;137:482–8. 10.1053/j.gastro.2009.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Frere C, Bournet B, Gourgou S, et al. Incidence of venous thromboembolism in patients with newly diagnosed pancreatic cancer and factors associated with outcomes. Gastroenterology 2020;158:1346–58. 10.1053/j.gastro.2019.12.009 [DOI] [PubMed] [Google Scholar]
- 26. Frere C, Crichi B, Bournet B, et al. Primary thromboprophylaxis in ambulatory pancreatic cancer patients receiving chemotherapy: a systematic review and meta-analysis of randomized controlled trials. Cancers 2020;12:2028. 10.3390/cancers12082028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Frere C. Burden of venous thromboembolism in patients with pancreatic cancer. World J Gastroenterol 2021;27:2325–40. 10.3748/wjg.v27.i19.2325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Davis NE, Hue JJ, Kyasaram RK, et al. Prodromal depression and anxiety are associated with worse treatment compliance and survival among patients with pancreatic cancer. Psychooncology 2022. 10.1002/pon.5945. [Epub ahead of print: 26 Apr 2022]. [DOI] [PubMed] [Google Scholar]
- 29. Dengsø KE, Thomsen T, Andersen EW, et al. The psychological symptom burden in partners of pancreatic cancer patients: a population-based cohort study. Support Care Cancer 2021;29:6689–99. 10.1007/s00520-021-06251-4 [DOI] [PubMed] [Google Scholar]
- 30. Bauer MR, Bright EE, MacDonald JJ, et al. Quality of life in patients with pancreatic cancer and their caregivers: a systematic review. Pancreas 2018;47:368–75. 10.1097/MPA.0000000000001025 [DOI] [PubMed] [Google Scholar]


