Abstract
The COVID-19 pandemic has infected tens of millions worldwide. Healthcare systems have been stretched caring for the most seriously ill and healthcare workers have struggled to maintain non-COVID services leading to backlogs.
Strategies proposed to support the recovery of backlogs include additional administration support; waiting list data validation; enhanced patient communication; and use of systematic improvement methods to make rapid incremental improvements.
As part of COVID-19 recovery, a hospital trust in northern England used the Lean systematic improvement approach to recover the waiting list of a paediatric service to pre-COVID levels. The intervention strategy used a massive-open-online-course (Lean Fundamentals) to support the improvement project lead to follow a structured improvement routine to apply Lean improvement techniques.
By acknowledging that staff were overburdened by the requirements of COVID-19 and that patients were stuck in a system of disconnected processes, administrative activities were redesigned around an ethos of compassionate communication that put patients first.
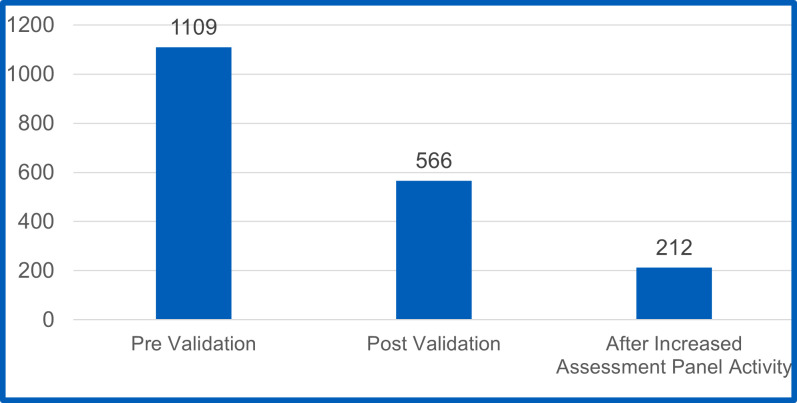
Over a period of 8 weeks, the project reduced the waiting list from 1109 to 212. Waiting times were reduced from a maximum of 36 months to a 70-day average.
Lean is often described in terms of increasing process efficiency and productivity. It is not often associated with staff benefits. However, when seen in the context of unburdening staff to deliver patient care, Lean has potential to support the recovery of both staff and services. Lean Fundamentals, with its accessible massive-online design, may provide a means of supporting such improvement at scale.
Keywords: Quality improvement, Lean management, Paediatrics, COVID-19, Waiting Lists
What is already known on this topic
Systematic quality improvement (S-QI) methods focusing on process improvement, such as Lean, are associated with increasing efficiency and productivity. The impact on healthcare professionals has been reported as mixed.
What this study adds
An empirical case study of S-QI selected for its unique features which include: the combination of compassionate communication with Lean; a focus on staff benefits and process efficiency as a means of unburdening staff as well as improving services; its relevance to current National Health Service context and alignment with operational planning guidance priorities.
How this study might affect research, practice or policy
A concrete example of how the use of compassionate leadership and compassionate communication in practical S-QI work can support the recovery of services and staff.
Problem
The COVID-19 pandemic has infected tens of millions worldwide.1 Internationally, healthcare systems and staff have been stretched, some to breaking point, providing care for the most severe cases.2 3 Governments have imposed major societal constraints and population lockdowns in attempts to limit transmission of the virus. Though effective, such measures have brought with them adverse economic and other social consequences.4 5 Disruption to education, separation of family contact, increased domestic violence and increased loneliness have all been reported.6 7 Recovering from the effects of COVID-19 is a major concern—including for healthcare.6
Recovery has been defined as ‘the process of rebuilding, restoring and rehabilitating society following an emergency’.6 The COVID-19 emergency has significantly impacted healthcare services and staff. Healthcare workers have played a central role in responding to COVID-19 including caring for infected patients and forming strategies to reduce infection and manage the pandemic.8 Many healthcare workers have also experienced major changes to their roles and working patterns as well as exposure to infection and isolation from family and friends.8 9 Stress, anxiety and burnout among healthcare workers have been reported.8 9 Furthermore, under the burden of the pandemic, healthcare workers have struggled to maintain non-COVID services leading to backlogs.10 In the UK’s National Health Service (NHS) waiting lists for routine procedures have risen to over 6 million—almost 10% of the population—with expectations that a significant number of patients are yet to be referred.10–12 Therefore, in healthcare there is a need to recover both services and staff.
Background
In the UK, alongside vaccinating the population against COVID-19, supporting the recovery of staff and accelerating the recovery of elective services are the top priorities for England’s NHS.13 The pandemic has had a significant impact on NHS activity, and elective care in particular has been disrupted.10 13 As the pandemic struck, a major risk was care capacity being overwhelmed by seriously ill patients. To mitigate this, the NHS in England postponed non-urgent routine treatment to free up hospital capacity for patients who had COVID-19. It has been estimated that during the first 8 months of 2020, referrals for elective hospital care in England reduced by one-third compared with 2019. While significant progress has been made reopening services and increasing activity towards pre-pandemic levels,10 it has been projected that returning to ‘the old normal’ will be insufficient to address both the backlog and new demand.12 Policy think-tanks suggest that radical approaches are required to redesign care pathways.11 12
Health commentators have stated that multiyear investment in the NHS is required to address waiting times and the elective backlog.11 14 For example, the NHS vacancy gap is a recognised problem requiring investment in workforce and a long-term strategy.11 15 Investment in capital infrastructure is also required to expand capacity, particularly in elective diagnostics.11 14 While these policy proposals require significant investment and time to implement, others are more immediately actionable. Other strategies proposed to complement longer-term policies include additional administration support; waiting list data validation; enhanced patient communication; and use of systematic improvement methods to make rapid, incremental improvements—particularly to administrative processes.11 16 17
Administrative processes and staff are essential to deliver quality care.17 18 Administration includes: back-office processes related to general functioning (such as payroll and human resources) and patient administration (such as bed, room and equipment booking); front-office processes involving direct patient contact (such as referrals, appointment booking and discharge); and boundary processes that straddle back and front-office processes (such as updating electronic health records).17 18 Poor administration can adversely impact patient experience and has been associated with poorer health outcomes and service waste.11 17 18 Improving administration has been recommended to the NHS to both support a pressurised and exhausted workforce and help manage the backlog of elective waits.11 17
Poor administration processes can create bureaucratic barriers to access and make appointments difficult for patients to schedule. Service integration can also be compromised where processes fail to keep patient records up to date or share necessary information between clinical teams.17 18 Without accessible administration processes, those who rely most on health and care services can experience low-value care, or find themselves excluded altogether. Therefore, responsive administrative processes and staff skilled in compassionate communication are considered essential enablers of high-quality care.17 19 20
Compassionate communication involves the exchange of ideas and thoughts with people while being empathetic to their situation. Compassionate communication has been described as comprising three components: acknowledging the suffering of another person; expressing caring, kindness and understanding; and withholding judgement.21–23 Compassionate communication also requires action. It is an active process that puts the needs of others first.23–25 Compassionate interactions between staff and patients are necessary to operate responsive, inclusive processes.17 25
Systematic quality improvement (S-QI) methods can play a role in improving processes to address care backlogs.16 S-QI methods with a specific focus on improving processes include Lean.26 Lean is a systematic quality improvement approach originating from Japan’s automotive industry. Lean conceptualises work as processes that can be continuously improved.26 In healthcare, the centrality of patients within care processes is emphasised with the aim of reducing or eliminating processing time that does not add value to them.27
There are other forms of waste that Lean must also consider—such as unevenness in workloads and overburden on people or equipment.28–30 Unevenness can result from irregular scheduling or mismatches in capacity and demand and can lead to overburden. Overburden refers to pushing people or equipment beyond natural limits—which can lead to breakdowns and burnout.28 As an improvement method, Lean must adopt the philosophy of improving all three types of waste: non-value adding process activities; process unevenness and variation; and overburden on staff.29
As part of COVID-19 recovery, a hospital trust in northern England used the Lean systematic improvement approach to address all three types of waste (non-value activities, unevenness and overburden). Aiming to reduce waiting time and improve throughput to pre-COVID levels, the trust improved their administration processes to support the recovery of a paediatric service and the staff that worked within it.
Measurement
The case took place at a hospital trust in northern England providing a paediatric social communication disorder (SCD) service. There was a historical backlog prior to the pandemic and subsequent COVID-19 constraints had limited appointments. Clinical capacity was also further reduced due to COVID-19 illness. Consequently, staff had become overburdened trying to accommodate patient lists of ill colleagues to maintain the service.
An improvement project was established to make rapid improvements to:
Release time to recover the waiting list backlog.
Balance capacity to demand to reduce the wait time for new referrals to the service.
Begin the process of recovering staff from the impact of the COVID-19 pandemic.
The key metrics for improvement were total numbers of patients waiting and waiting time from referral request received date to appointment date with a clinical assessment panel. At the start of the project the waiting list for appointments stood at over 1100 patients with waiting times averaging 421 days with a maximum of over 1200 days.
Design
The improvement project was supported by online knowledge transfer of Lean S-QI techniques and a structured improvement routine through which they could be deployed. Lean Fundamentals is a massive-open-online-course (MOOC) developed by the Improvement Capability Building and Delivery (ICBD) Group within NHS England and Improvement.31 32 Designed to accept unlimited numbers of participants,33 34 MOOCs are efficient, effective alternatives to traditional training formats and can provide health and care staff with free, large-scale access to S-QI knowledge.31 35 36 The Lean Fundamentals MOOC was designed to develop participants’ knowledge and skills through practical application in a tightly scoped improvement project.31 36 An overview of the Lean Fundamentals content and module structure is provided in table 1.
Table 1.
Overview of the Lean Fundamentals massive-open-online-course modules
| Module | Description |
| 0. Course induction | Orients participants to the learning platform functionality, course objectives and learning compact. Helps participants consider their improvement project scope. |
| 1. Improvement Kata introduction | Provides a structured, four-step routine for learning and applying improvement science and helps participants establish and communicate their project. |
| 2. Introduction to Lean | Introduces the principles of Lean and helps participants to consider how value is defined and how waste manifests within processes. |
| 3. The building blocks of processes | Demonstrates the effect of process variation and helps participants to design it out and document processes through observation and waste elimination. |
| 4. The flows of healthcare | Introduces participants to seven flows that comprise healthcare processes and how to observe, document and process map them. |
| 5. Workplace organisation | Helps participants apply a five-step process to organise workplaces and use visual methods to design more effective, efficient and reliable processes. |
| 6. Pursuing perfection | Introduces a structured approach to continuous improvement through iterative experimentation using the model-for-improvement and plan-do-study-act cycles. |
Following beta-test completion in January 2021, Lean Fundamentals supported COVID-19 vaccination centres to improve throughput and flow.31 36 Though aimed at improving vaccination processes, some participants undertook other projects—including the one reported here. The project lead was a MOOC participant that followed the course modules, activities and structured improvement approach, applying them to the paediatric SCD service. The case was selected for further study for its unique features which included: a focus on all three types of waste defined by Lean (non-value activities, overburden and unevenness); the combination of compassionate communication with Lean; and its relevance to current NHS context and alignment with operational planning guidance priorities.
To develop the case study, data were collected while delivering the Lean Fundamentals MOOC. Case studies are empirical inquiries investigating contemporary phenomena within their real-world context. They are suitable when the contextual conditions in which the phenomenon being studied are pertinent.37 Case study methods have also been identified as useful for understanding improvement interventions to guide future improvement strategies.38 Data collection comprised:
Artefacts submitted to the Lean Fundamentals MOOC by the improvement project lead (such as aim statements, process analysis templates and waste observations).
Participant feedback from the MOOC—typically in the form of comments made against the MOOC’s modules and content illustrating what was being learnt and how this was being applied.
MOOC project improvement report—a concise report submitted by the improvement project lead describing the initial impact of their improvement project.
Following completion of the MOOC by the improvement project lead, the authors contacted them as a key informant to explore their project in detail. An in-depth interview was conducted online via video conference, recorded and later transcribed.
Working to the Standards for Quality Improvement Reporting Excellence reporting guidelines,39 40 the data were used to prepare the case and present it in a standard quality improvement report format using a heading structure first proposed by Moss and Thompson and refined by BMJ Publishing Group.41 42
Strategy
The project was led by an administration manager working on a bank basis to cover the vacant SCD coordinator role. Relatively new to the NHS, the improvement project lead had first joined the NHS as a vaccinator. Prior to that, they had worked in various management and administrative roles, predominantly in the retail sector, but had no previous experience with Lean.
The intervention strategy followed the Lean Fundamentals MOOC which supported the improvement project lead to implement the structured improvement routine and apply the Lean S-QI techniques. The structured improvement routine used ‘improvement Kata’.36 43 44 Drawn from the Lean improvement practices of Toyota, the improvement Kata routine comprises four steps: understand the direction and challenge; grasp the current situation; establish the next target condition; and experiment towards the target condition.36 43 44 An overview of the improvement Kata steps are described in table 2.
Table 2.
Improvement Kata steps
| Step | Description |
| 1. Understand the direction and challenge | Establish a clear improvement aim linked to an organisational priority. |
| 2. Grasp the current situation | Use various process analysis techniques to study the current state in detail. |
| 3. Establish the next target condition | Articulate a series of target conditions for how processes should operate to achieve the overall aim. |
| 4. Experiment towards the target condition | Apply successive iterations of plan-do-study-act experiments to achieve each target condition and the overall aim. |
In this case, the organisational priority was to recover both the backlog and staff (the specific aims are set out in section 3, above). To understand the current state, an observational study, or waste-walk, was used by the improvement project lead to identify bottlenecks, delays and process wastes (relating to time, motion, information flow defects and rework). Following this, a series of target conditions were articulated for how processes should operate. Successive iterations of plan-do-study-act (PDSA) experiments were then conducted to achieve each target condition and the overall improvement aims. Target conditions and PDSA experiments are summarised in online supplemental data and described in full below.
bmjoq-2022-001914supp001.pdf (61.5KB, pdf)
Lean process analysis of the current condition was undertaken via observation in the work place. The project lead identified delays and disruptions in information flow due to lack of job role clarity and mismatched skill/task alignment. Issues observed included significant clinical time used on administrative processes and administrative processes that were largely manual and time consuming to carry out. Furthermore, clinicians and medical secretaries had no time to verify and cleanse patient and waiting list data. Therefore, the primary target list (PTL) of patients that needed to be seen was not up to date. This meant it was difficult to know the status of patients and whether they were actively waiting for an appointment or had already been discharged—either by choice or because they had been seen.
So a lot of this was inaccurate record keeping … and the workload was then getting very confused and very difficult to actually manage.
Empathising with the pressures faced by staff, the project lead adopted a compassionate approach to improvement.19 24 45 Therefore, the first target condition aimed to unburden clinical staff and release time for care. PDSA1 removed admin tasks from clinicians with the improvement project lead taking responsibility on a temporary basis to redesign admin processes to support the pathway.
Too many people were involved in chasing too many reports and too much valuable clinician time was being used on clerical tasks—such as chasing school reports, speech and language therapy (SaLT) reports and opt-in/consent forms (also chased by medical secretaries).
If we’re paying a consultant to do a job and they’re having to run around chasing paperwork, that time could actually be used for a patient.
Therefore, the improvement project lead took on the role of SCD coordinator and managed the required reports and paperwork creating a process to ensure that:
All reports received were correctly filed.
The waiting list management spreadsheet was updated with the latest position.
The second target condition aimed to reduce administrative processing time. PDSA2 released admin time by using laptops to access patient records, waiting list data and activity data which were previously accessed manually.
Administrative processes in the SCD service had largely relied on paper records which were accessed and updated manually. Records were stored in a file room adjacent to the clinical reception area leading to much staff movement, back and forward, to access information. Looking at the physical process, the improvement project lead noted that motion waste associated with pulling files manually could be avoided if laptop computers were used to access patient records, waiting list information and the hospital’s patient administration system (PAS). Having access to a corporate laptop, authorisation was requested from the service’s matron for the required access.
So, there was one day where, literally,… I got one consultant done because I was going back and forward with community files to the desk… The next day I was able to go in and spend a full day with the laptop and get everything done [for the remaining consultants].
Furthermore, as the medical secretaries also had access to laptops, the same approach was used to remove motion waste from their processes—freeing up additional administrative time.
The third target condition established a cleansed, validated PTL—which was achieved using released admin time.
The PTL spreadsheet was not up to date. Therefore, it was difficult to know the status of patients and if all relevant paperwork had been received or not. Using time released by adopting laptops, the improvement project lead spent time in the filing room checking and updating records, discharging patients that could be verified as seen and verifying paperwork such as school reports, SaLT reports and consent forms. Patient records were then matched with those on PAS and the PTL updated. This cleansing process reduced the PTL from 1109 to 566 children by identifying the discharge status in paper records.
While such data cleansing may be seen as an arduous task, the project lead viewed it from a compassionate perspective. They empathised with patients and were intrinsically motivated to act.
If it’s a blank on my spreadsheet, I either want to complete or deal with it. A lot of people just don’t want to do the data cleansing—a lot of these children then don’t get diagnosed and they get forgotten about in the system … What if that was my child?
The fourth target condition was to recover the backlog of waits. PDSA3 used released clinical time to prioritise patients and run additional clinical assessment panels.
If you think of the rate of referrals, versus the rate of discharges, we were getting more referrals than were discharges. … Initially we were doing six children per consultant … [now] one of the consultants who actually has the largest [backlog] is trialling doing 12 children per panel.
Removing [the admin] process from [the clinicians] is allowing them to then clinically assess other patients and do different clinics.
The fifth target condition was to ensure future referrals could be seen quickly. PDSA4 used a generic email inbox as a single point of contact and developed new administrative standard work processes to follow-up referrals and schedule appointments as soon as all required information was received (such as speech and language therapy assessments).
So we literally streamlined it all down to one person collating the information and chasing it.
Verifying patients on the PTL with all necessary paperwork (school report, SaLT report and consent form) identified them as ready to go forward for SCD panel appointment with the clinical team. As SaLT reports were required prior to SCD panel appointment, the improvement project lead made process changes to ensure the status of these reports was followed-up. SaLT reports were provided by another organisation and required an explicit opt-in by patients/carers following appointment invitation letters being sent. Many patients/carers were unaware of this and assumed delays were due to COVID-19.
The parents have a lot to be doing, or they may just not get round to making the phone call or answering the letter. So now, the customer journey is feeling [empathy] for that child [and following up].
The project lead withheld judgement and, empathising with service users, introduced compassionate communication into the SCD follow-up process. In the new process designed and trialled by the improvement project lead, the SCD coordinator follows-up all patient referrals to establish if SaLT invitation letters have been sent. When confirmed, they then ring the patient/carer to check if the letter has been received and acted on and whether they wish to opt-in or opt-out of the SaLT assessment and proceed to SCD panel appointment for diagnosis.
There’s not actually one of these where we’ve rang and said ‘do you want to opt out’ and the response has [been ‘yes’] …we then check with the SaLT administrator and they come back and say ‘yes their … [appointment] will be said date’, we then record it, [SaLT report] comes back … [and] it goes straight to panel within what is now 2 months.
Making these process changes has ensured that:
All legacy entries on the spreadsheet were followed-up to verify their status.
All future SaLT reports received were filed.
The PTL was updated with the latest position.
SaLT reports were followed-up proactively to ensure a fully cleansed position going forward.
Results
In this case, the application of Lean and the improvement project success depended on compassion and compassionate communication with stakeholders (staff and patients). Compassionate communication requires interactions with people that: acknowledge their situation; express caring, kindness and understanding; and withhold judgement.21–23
Impact on the service
The improvement project lead acknowledged the situation of patients and their carers (children and their parents stuck in a system of disconnected processes). Compassionate communication with patients/carers revolved around opting-in to services. Interactions took the form of contacting them, without judgement, regarding their current status and sharing information, sensitively, to guide them on the options available and how to proceed depending on their decision.
I think I take it personally because I look at it like if that was my [child], if that was me.
Over a period of 8 weeks, the project reduced the waiting list from 1109 children at the start of the project to 566 following validation and cleansing and then to 212 after increasing the number of clinical assessment panels. Of the remaining list, many were awaiting SaLT assessment outside of the SCD service’s control—although these were now routinely followed-up for progress updates under the new standard work. The backlog was recovered within 2 months following which capacity was back in line with demand for new referrals. Figure 1 shows the total number waiting for appointment with a clinical assessment panel for the SCD service.
Figure 1.
Total waiting list for clinical assessment panel.
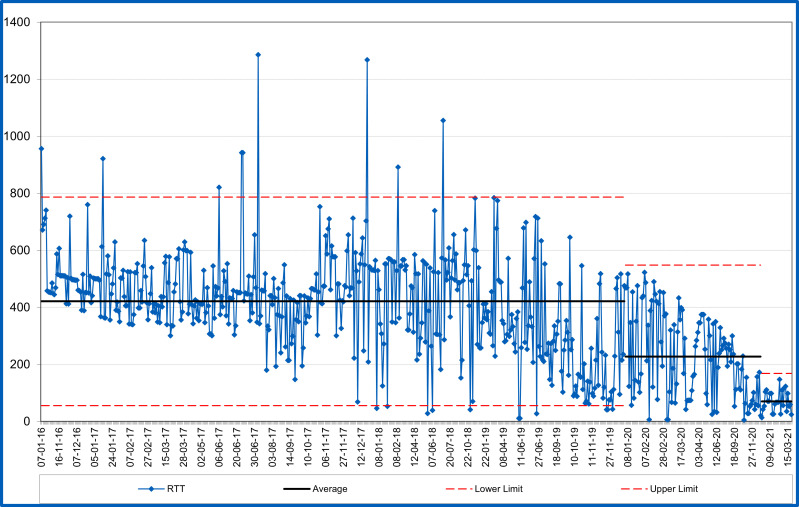
Figure 2 shows the referral to treatment wait time for individual patients, in order of referral received date. Waiting times have reduced from an average of 421 days to an average of 70 days and it is expected this will be sustainable going forward.
Figure 2.
Referral to treatment (RTT) waiting time (in days).
Impact on staff
As well as improving patient waiting times, the changes have also relieved burden and stress on both administrative and clinical staff. The improvement project lead acknowledged the situation of staff (who were overburdened by the requirements of COVID-19). Interactions with staff included both administrative and clinical staff. Administrative staff did not feel in control of their workload and clinical staff had become overburdened and struggled to see how service demands could be met. Compassionate communication involved empathising with their individual situations, both professional and personal, and acting to relieve burden and redesign processes.
The medical secretaries have actually seen a massive difference in their workload, simply because they’re not chasing schools. They’re not then having to relay back and forward from the consultant … Everything’s in a specific spreadsheet. It’s all in one location. It’s one person dealing with it.
I have valued this both professionally [and] personally because I’ve seen the personal impact this has on … our consultants, to streamlining the process, removing the waste, having people focused specifically on their job role, and how much that has actually benefited and added value to [them] emotionally.
Throughout these interactions, no judgement was made. The goal re staff was to improve their situation so that they could focus on providing care in a more sustainable way. Most importantly, the improvement project lead was prepared to act to help improve the situation of all stakeholders by applying Lean S-QI techniques.
Initially my biggest focus [was the] patient but actually, seeing the relief more on our teams and our staff probably means a bit more to me … because I know that the patient process is now streamlined, that patient is going to get good service is going to have good care, but actually now we need to look at how our staff are going to be post-Covid, because that’s going to have a big impact.
Impact on the project lead
The project lead’s willingness to learn and apply new skills and to act to help others by improving services has brought personal and professional benefits. Due to their improvement work, the project lead has secured a promotion and hopes to secure a permanent role in the NHS. They attribute these opportunities, at least in part, to the skills acquired through participating in the Lean Fundamentals MOOC.
I initially joined the programme while on furlough from retail … as a vaccinator [and was] put onto the massive-online course … and with the work that I had done [on vaccinations], I was actually taken on board at [the Trust] as the Improvement Project Manager. Through that track record, and actually what I have done within paediatrics, using the Lean modules, I’ve got a meeting [about] coming across to the NHS full-time. All through Lean Fundamentals.
I owe a lot, if not the whole part of my career [in the NHS], to the [ICBD] team and Lean.
Lessons and limitations
There are several lessons that can be drawn from the case study relating to the Lean Fundamentals MOOC, Lean and compassionate communication.
Lean is typically associated with increasing productivity and efficiency by reducing process wastes. However, other wastes to consider are overburden and unevenness.28–30 In this case, Lean was targeted at all three waste types.
First, non-value activities and process wastes were reduced to release administration time to cleanse and manage proactively the PTL. This involved simple tactics such as reducing unnecessary motion and reducing processing time through better use of technology.
Second, overburden on staff was reduced through improved skill/task alignment, clearer job roles and smoother flowing process. This involved removing the burden of administrative coordination from clinicians and focusing their time on patient appointments. The administrative responsibilities of medical secretaries and SCD coordination role were also clarified leading to a smoother flow of information and patient appointments.
Third, unevenness in appointment scheduling was reduced by bringing capacity in line with demand. This involved using freed up administration time to first cleanse the PTL and freed up clinical time to temporarily increase appointments to address the backlog.
In previous studies, the impact of Lean on healthcare professionals has been reported as mixed.30 While positive impacts can include improved teamwork, communication, coordination, motivation and morale, negative impacts include work intensification, job strain, anxiety and stress. Lean implementations resulting in work intensification and stress have been associated with managerial coercion and pressure to execute labour-intensive tasks.30 Such dominant and hierarchical leadership approaches have been reported as ineffective for managing healthcare organisations.25 Conversely, compassionate leadership approaches are considered facilitative of quality improvement and innovation in healthcare.19 25 Therefore, how Lean S-QI methods are used and implemented is a factor.30
The success of Lean S-QI in this case depended on the project lead’s adoption of a compassionate leadership style and compassionate communication with stakeholders (staff and patients). Compassion has been identified as an important component of improvement leadership.19 25 Viewing leadership ‘as a process of influence … [in] interactions between people’, West and Chowla consider compassion ‘a characteristic of interactions rather than necessarily of individuals’.20 Compassionate interactions comprise empathy, withholding judgement and willingness to help.21–23 In this case, the project lead demonstrated such compassionate communication in interactions with patients (helping them to access appointments) and staff (helping them to improve process efficiency and reducing overburden from time pressures).
Compassionate care and S-QI methods have been proposed as essential components of healthcare workers’ roles.45 However, ‘scarce [published] scientific evidence’ has been noted as a limiting factor for implementation.45 Empirical examples illustrating how compassion can contribute to SQ-I projects to improve operational performance are needed. This case study helps address that gap, demonstrating how compassion and compassionate communication contributed practically to implementing Lean SQ-I methods to improve services.
Finally, previous reporting on Lean Fundamentals involved project leads experienced in Lean S-QI techniques, which limited the extent to which their experience was generalisable to the wider NHS.31 In this case, the improvement project lead had no prior experience with Lean but, following the Lean Fundamentals MOOC content and structure, was able to make impactful change. This suggests that prior Lean experience is not a necessary antecedent for successful improvement using Lean Fundamentals. However, it is unclear to what extent the outcome was influenced by other personal attributes of the improvement project lead key informant. Future research might usefully explore this.
Several limitations have been identified.
First, the authors worked on the design and delivery of the Lean Fundamentals online programme. Therefore, there is the potential for positivity bias. To mitigate this, authors have shared drafts of the case with the improvement project lead key informant to verify for accuracy and fairness of the work.
Second, as capacity and demand have been brought into balance, the process changes made should be sustainable. In addition to process changes, though, sustainability has been related to other factors including leadership, culture and organisational infrastructure to support improvement.46 However, a wider assessment of sustainability has not been made and this could be a useful addition to future reports.
Third, it has not been possible to follow-up longitudinally. However, given the urgency and priority currently placed on recovery of services and staff, the project and results to date have been shared as they may be valuable to others working on this challenge. Evaluating the longer-term impact of both Lean’s contribution to the recovery agenda and the Lean Fundamentals MOOC in building Lean improvement capability may be a focus for future studies.
Finally, a single case is presented. Therefore, results may not be generalisable. However, the case does demonstrate the potential contribution of improving administrative processes to manage elective backlogs. Furthermore, the case illustrates the roles that massive-online, Lean S-QI and compassionate communication may play in such improvement.
Conclusion
Policy think-tanks and patient advocacy groups have recommended improvement of administrative processes and management of PTLs to support the recovery of healthcare waiting lists.11 17 This case study suggests the recommendation is actionable and that Lean, combined with compassionate communication, can contribute. While the focus of Lean is often described in terms of increasing process efficiency and productivity, it is not often associated with staff benefits. However, when seen in the context of unburdening staff to deliver patient value, Lean’s potential to help with the required recovery of both staff and services becomes clear. If compassionate leaders can reframe Lean’s focus from ‘eliminating waste’ and ‘increasing productivity’ to ‘unburdening staff to deliver high quality care’, perhaps this potential can be realised more broadly across the NHS. Lean Fundamentals, with its accessible massive-online design, may provide a means of supporting such improvement at scale.
Footnotes
Contributors: IMS was responsible for reporting on the work, writing and revising the article, and is responsible for the overall content as guarantor. EB contributed to data collection and the writing and revision of the article.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare the following interests: IMS and EB work as improvement and transformation professional in the National Health Service. IMS led the design and delivery of the Lean Fundamentals massive-open-online-course (MOOC). EB managed the project and supported the design and delivery of the Lean Fundamentals MOOC.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The Health Research Authority online decision tool was used to determine that NHS research ethics was not required for the study as it was considered evaluation of service improvement. Participants gave informed consent to participate in the study before taking part.
References
- 1.World Health Organization . WHO coronavirus (COVID-19) Dashboard, 2021. Available: https://covid19.who.int/ [Accessed 28 Mar 2021].
- 2.Greenberg N, Docherty M, Gnanapragasam S, et al. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020;368:m1211. 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- 3.Tanne JH. Covid-19: US hospitals are overwhelmed as cases rise at “alarming rate”. BMJ 2021;374:n2092. 10.1136/bmj.n2092 [DOI] [PubMed] [Google Scholar]
- 4.Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020;584:257–61. 10.1038/s41586-020-2405-7 [DOI] [PubMed] [Google Scholar]
- 5.Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020;584:262–7. 10.1038/s41586-020-2404-8 [DOI] [PubMed] [Google Scholar]
- 6.Boaden R, Powell D, Shaw D, et al. Recovering from COVID-19: the key issues. Journal of Safety Science and Resilience 2020;1:67–9. 10.1016/j.jnlssr.2020.06.002 [DOI] [Google Scholar]
- 7.Sharma A, Borah SB. Covid-19 and domestic violence: an indirect path to social and economic crisis. J Fam Violence 2022;37:1–7. 10.1007/s10896-020-00188-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med 2020;21:1059–66. 10.5811/westjem.2020.7.48684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilson C. Mental health impacts of COVID-19 on NHS healthcare staff, 2020. Available: https://post.parliament.uk/mental-health-impacts-of-covid-19-on-nhs-healthcare-staff/ [Accessed 5 Oct 2020].
- 10.NHS England . Delivery plan for tackling the Covid-19 backlog of elective care, 2022. Available: https://www.england.nhs.uk/coronavirus/publication/delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care/ [Accessed 17 Feb 2022]. [DOI] [PubMed]
- 11.Ede R, Phillips S. A wait on your mind? A realistic proposal for tackling the elective backlog. London: Policy Exchange, 2021. [Google Scholar]
- 12.Gardner T, Fraser C, Peytrignet S. Elective care in England: assessing the impact of COVID-19 in 2020 and where next. London: The Health Foundation, 2020. [Google Scholar]
- 13.NHS England . 2021/22 priorities and operational planning guidance, 2021. Available: https://www.england.nhs.uk/publication/2021-22-priorities-and-operational-planning-guidance/ [Accessed 25 Mar 2021].
- 14.Taylor M. Spending review is an opportunity to invest in the NHS for the future, 2021. Available: https://www.nhsconfed.org/articles/spending-review-opportunity-invest-nhs-future [Accessed 17 Aug 2021].
- 15.Bailey S, Baylis A, Anandaciva S, et al. NHS workforce: our position, 2021. Available: https://www.kingsfund.org.uk/projects/positions/nhs-workforce [Accessed 26 Feb 2021].
- 16.Scott J, Cann H. Moving past Backlogs: how are Q members improving access to services? 2021. Available: https://q.health.org.uk/blog-post/moving-past-backlogs-how-are-q-members-improving-access-to-services/ [Accessed 5 Aug 2021].
- 17.National Voices . Paper works: the critical role of administration in quality care. London: National Voices, 2021. [Google Scholar]
- 18.Ewbank L, Lamming L, Cream J, et al. Admin matters: the impact of NHS administration on patient care, 2021. Available: https://www.kingsfund.org.uk/publications/admin-matters-nhs-patient-care [Accessed 24 Jun 2021].
- 19.Bailey S, West M. What is compassionate leadership? 2022. Available: https://www.kingsfund.org.uk/publications/what-is-compassionate-leadership [Accessed 15 Febr 2022].
- 20.West MA, Chowla R. Compassionate leadership for compassionate health care. In: Gilbert P, ed. Compassion: concepts, research and applications. London: Routledge, 2017: 237–57. [Google Scholar]
- 21.İbrahimoğlu Özlem, Mersin S, Çağlar M. The Turkish adaptation of the compassionate communication scale: a validity and reliability study. Perspect Psychiatr Care 2021;57:43–9. 10.1111/ppc.12522 [DOI] [PubMed] [Google Scholar]
- 22.Neff KD. The development and validation of a scale to measure Self-Compassion. Self and Identity 2003;2:223–50. 10.1080/15298860309027 [DOI] [Google Scholar]
- 23.Ramos Salazar L. Communicating with Compassion: The Exploratory Factor Analysis and Primary Validation Process of the Compassionate Communication Scale [Doctoral Dissertation]. Arizona State University, 2013. [Google Scholar]
- 24.Sinclair S, Norris JM, McConnell SJ, et al. Compassion: a scoping review of the healthcare literature. BMC Palliat Care 2016;15:6. 10.1186/s12904-016-0080-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.West M, Collins B, Eckert R. Caring to change: how compassionate leadership can stimulate innovation in health care. London: The King’s Fund, 2017: 40. [Google Scholar]
- 26.Smith I, Hicks C, McGovern T. Adapting lean methods to facilitate stakeholder engagement and co-design in healthcare. BMJ 2020;368:m35. 10.1136/bmj.m35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burgess N, Currie G, Crump B, et al. Improving together: collaboration needs to start with regulators. BMJ 2019;367:l6392. 10.1136/bmj.l6392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liker JK. The Toyota Way: 14 management principles from the world’s greatest manufacturer. New York, NY: McGraw-Hill, 2004. [Google Scholar]
- 29.Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med 2012;74:364–71. 10.1016/j.socscimed.2011.02.011 [DOI] [PubMed] [Google Scholar]
- 30.Mahmoud Z, Angelé-Halgand N, Churruca K, et al. The impact of lean management on frontline healthcare professionals: a scoping review of the literature. BMC Health Serv Res 2021;21:383. 10.1186/s12913-021-06344-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith IM, Bayliss E, Salisbury H, et al. Operations management on the front line of COVID-19 vaccination: building capability at scale via technology-enhanced learning. BMJ Open Qual 2021;10:e001372. 10.1136/bmjoq-2021-001372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.England NHS, Improvement NHS. Lean online programme, 2021. Available: https://www.england.nhs.uk/sustainableimprovement/lean-online/
- 33.Guerrero M, Heaton S, Urbano D. Building universities’ intrapreneurial capabilities in the digital era: The role and impacts of Massive Open Online Courses (MOOCs). Technovation 2021;99:102139. 10.1016/j.technovation.2020.102139 [DOI] [Google Scholar]
- 34.Mahajan R, Gupta P, Singh T. Massive open online courses: concept and implications. Indian Pediatr 2019;56:489–95. 10.1007/s13312-019-1575-6 [DOI] [PubMed] [Google Scholar]
- 35.Guest C, Wainwright P, Herbert M, et al. Driving quality improvement with a massive open online course (MOOC). BMJ Open Qual 2021;10:e000781. 10.1136/bmjoq-2019-000781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith IM, Smith DTL. Mass production methods for mass vaccination: improving flow and operational performance in a COVID-19 mass vaccination centre using lean. BMJ Open Qual 2021;10:e001525. 10.1136/bmjoq-2021-001525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yin RK. Case study research: design and methods (4th edition. 4th ed. Los Angeles, CA: Sage Publications, 2009. [Google Scholar]
- 38.Baker GR. The contribution of case study research to knowledge of how to improve quality of care. BMJ Qual Saf 2011;20 Suppl 1:i30–5. 10.1136/bmjqs.2010.046490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Davidoff F, Batalden P, Stevens D, et al. Publication guidelines for quality improvement studies in health care: evolution of the Squire project. BMJ 2009;338:a3152. 10.1136/bmj.a3152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogrinc G, Davies L, Goodman D, et al. Squire 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016;25:986–92. 10.1136/bmjqs-2015-004411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moss F, Thompson R. A new structure for quality improvement reports. Qual Health Care 1999;8:76. 10.1136/qshc.8.2.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.BMJ Open Quality . Author guidelines: quality improvement report. Available: https://bmjopenquality.bmj.com/pages/authors/-quality_improvement_programme_report
- 43.Rother M. The Toyota Kata Practice Guide: practicing scientific thinking skills for superior results in 20 minutes a day. USA: McGraw Hill Professional, 2017. [Google Scholar]
- 44.Proudlove N, Furnival J. Toyota kata: a missing link in quality improvement in healthcare? 27th European operations management association conference: EurOMA27. UK: Warwick, 2020: 1818–27. [Google Scholar]
- 45.Lillo-Crespo M, Sierras-Davó MC. Quality Improvement with Compassion: Developing Healthcare Improvement Science in the European Health Professions’ Education. In: Gibbs P, Jameson J, Elwick A, eds. Values of the University in a time of uncertainty. Cham: Springer International Publishing, 2019: 231–40. [Google Scholar]
- 46.Maher L, Gustafson D, Evans A. Sustainability Model & Guide. NHS Institute for Innovation & Improvement: Warwick, 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2022-001914supp001.pdf (61.5KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.