Abstract
Introduction
Globally, maternal morbidity and mortality have increased during the COVID-19 pandemic. Given the high burden of maternal and neonatal mortality in Kenya prior to COVID-19, front line health workers, including nurse-midwives, must be competent to ensure continued quality maternal services. Knowledge and awareness of COVID-19 transmission influence nurse-midwives risk perception and ability to implement prevention strategies.
Objective
We examined nurse-midwives’ knowledge, attitudes, and preparedness in managing pregnant and postpartum women with COVID-19 in Kenya.
Methods
A cross-sectional online survey was conducted among 118 nurse-midwives between July 2020 and November 2020. A 31-item survey comprising 15 knowledge, 11 attitude, and five preparedness questions was administered using SurveyMonkey. A link to the survey was distributed among nurse-midwives via email. Multiple logistic regression analysis was used to assess associations between the variables. A p-value <.05 was considered statistically significant.
Results
Eighty-five participants were included in the final analysis (response rate 72%). Most participants were female (n = 69, 81.2%), 52.9% (n = 45) worked in labor wards, and 57.6% (n = 49) worked in rural hospitals. Overall, 71% (n = 57) of participants had sufficient knowledge about managing COVID-19 in pregnant and postpartum women. However, only 63% were willing to receive COVID-19 vaccination. Nurse-midwives working in urban areas were 3.7 times more likely to have positive attitudes than those in rural areas (odds ratio 3.724, 95% confidence interval 1.042–13.31; p = .043).
Conclusion
Nurse-midwives’ responses to the Kenyan government's COVID-19 guidelines for managing and caring for pregnant women were inconsistent. Continued professional development for nurse-midwives is important to ensure they stay abreast of evolving COVID-19 guidelines for maternal health. Our findings also suggest vaccine hesitancy may be a hurdle for ongoing COVID-19 vaccination.
Keywords: COVID-19, midwives, pregnancy and childbirth, maternity care, vaccine hesitancy, midwives’ attitude
Introduction
The COVID-19 pandemic caused widespread disruption of reproductive, maternal, newborn, and child health (RMNCH) services in low- and middle-income countries. Adverse effects of the pandemic included maternal, perinatal, and child morbidity and mortality from infection with SARS-CoV-2 (Lokken et al., 2021; World Health Organization, 2021c; Zambrano et al., 2020). Although many governments prioritized maternal health as an essential core service, measures to reduce infection affected how women and children accessed healthcare (Roberton et al., 2020; Semaan et al., 2020). Given that Kenya had a high burden of maternal and neonatal mortality before the outbreak of COVID-19, front line healthcare workers such as nurse-midwives must be competent to ensure continued quality maternal services (Gitobu et al., 2018).
COVID-19 can be transmitted by respiratory droplets from symptomatic and asymptomatic individuals or through direct contact with infected surfaces or aerosols in poorly ventilated areas (World Health Organization, 2021a). Following the first reported COVID-19 case on March 13, 2020, the Kenyan government imposed countrywide lockdowns with multiple restrictions, including curfews and limitations on congregating and hospitality services. However, as of June 2021, COVID-19 infections and deaths continue to rise in Kenya, and a third wave emerged with new variants of concern (World Health Organization, 2021b).
Review of the Literature
Globally, maternal morbidity and mortality increased during the COVID-19 pandemic (Ashish et al., 2020; Chmielewska et al., 2021; Lokken et al., 2021). The ongoing pandemic means the full scope of the impact of COVID-19 on access to RMNCH has not yet been determined, but there are reports of reduced antenatal attendance and reduced facility births, possibly because of government lockdown curfews and fear of infection (Goyal et al., 2021; Ombere, 2021; Pallangyo et al., 2020; UNFPA, 2020). An analysis of the early impact of COVID-19 on the maternal infrastructure in Kenya showed increasing trends in adolescent pregnancy rates, stillbirths, and maternal mortality (Shikuku et al., 2021; Shumba et al., 2020). Kenya has made substantial progress in reducing the maternal mortality ratio per 100,000 live births (from 708 in 2000 to 342 in 2017), but continued progress is at risk because of COVID-19.
Research suggests that pregnant women may be at increased risk for severe illness associated with SARS-CoV-2 infection. Immunological and physiological adaptive changes during pregnancy mean pregnant women are vulnerable, and therefore more predisposed to COVID-19 infection than the general population (Allotey et al., 2020; Luo & Yin, 2020). Furthermore, emerging evidence shows that pregnant women are also at high risk for hospitalization, mechanical ventilation, intensive care unit admission, and mortality following SARS-CoV-2 infection (Ashish et al., 2020; Delahoy et al., 2020; Lokken et al., 2021; Zambrano et al., 2020). Consequently, pregnant women with suspected or confirmed COVID-19 infection should be carefully monitored (World Health Organization, 2021a). Front line HCWs also need to be aware that pregnant women with moderate to severe COVID-19 require hospitalization and may require assisted ventilation for respiratory failure and additional interventions to improve maternal and fetal survival. This is particularly true for pregnant women with various comorbidities that have COVID-19. Currently, no antiviral agent has been approved for use in Kenya, and vaccination if being implemented among high-risk groups. However, data on the safe use of COVID-19 vaccines in pregnancy are scarce (Rasmussen et al., 2021).
HCWs are in direct contact with patients with COVID-19; therefore, they are at high risk for infection and transmission of the virus to their families and communities. However, front line HCWs continue to provide direct care for patients despite an increased workload, inadequate resources, personal risk for infection, risk for transmission to family members, and loss of colleagues and patients (Mehta et al., 2021). Furthermore, anxiety, depression, personal isolation, and financial stress affected HCWs’ ability to cope during the pandemic (Carmassi et al., 2020; Giusti et al., 2020; Onchonga et al., 2021). Protecting HCWs’ physical and mental health is therefore a priority for health institutions and policymakers. This means infection prevention and control (IPC) training is central in raising awareness and strengthening prevention strategies.
Knowledge and awareness of COVID-19 transmission influence nurse-midwives’ perceptions of risk and their ability to implement prevention strategies (Bhagavathula et al., 2020). Several studies have explored HCWs’ knowledge, attitudes, and practice during the COVID-19 pandemic (Abdel Wahed et al., 2020; Alsoghair et al., 2021; Majid et al., 2020). However, there is a paucity of studies that explicitly examined HCWs’ knowledge and perceptions of managing pregnant women in the context of COVID-19. Therefore, this study aimed to (1) assess the level of knowledge, (2) examine the attitudes, and (3) determine the preparedness of nurses and midwives in managing pregnant and postpartum women with COVID-19. Caring for pregnant women during a pandemic is important as the adaptation changes in pregnancy mean they are immunologically and physiologically vulnerable. They may also experience additional anxiety and fear for themselves and their unborn baby.
Methods
Study Design, Setting, and Participants
This study used a descriptive cross-sectional design. Participants were nurse-midwives working at a private university hospital and those currently working in public and private institutions around the country and enrolled part-time in the Bachelor of Science in Nursing/Midwifery upgrade programs at a university in Nairobi between July 1, 2020, and November 24, 2020. Bachelor's students were practicing nurse-midwives from around Kenya with a diploma in nursing or midwifery who attended university twice a week. The target population was registered nurse-midwives working in Kenyan maternity units; an estimated 118 nurse-midwives work in these units.
Ethical Considerations
This study was conducted in accordance with the 1964 Helsinki Declaration. Ethical approval was granted by the AKU Institutional Ethics Review Committee (ref #2020/IERC-70), and a research permit was granted by the National Commission for Science, Technology, and Innovation (ref #NACOSTI/P/20/6778). Participation in this study was voluntary and anonymous and no personal information was obtained. Electronic informed consent was obtained from all participants.
Sampling
This study included registered nurse-midwives that worked with pregnant women and newborns in antenatal, labor and delivery, postnatal, and newborn units. The inclusion criteria included nurse-midwives working at a private university hospital and those currently working in public and private institutions around the country and enrolled part-time in the Bachelor of Science in Nursing/Midwifery upgrade programs at a university in Nairobi. Census sampling was used because the population was deemed to be small. Consistent with previous research, a response rate of 70% is considered appropriate and representative for an online epidemiological survey (Morton et al., 2012).
Study Tool
Data were collected with a self-administered online questionnaire that was administered using SurveyMonkey. A link to the survey was distributed via participants’ email addresses. All questions were in English. The survey covered four areas: (a) demographic and background information, including age, gender, designation, education level, training, employment status, job title and location, working experience, and marital status; (b) training undertaken on the management of pregnant women with COVID-19; (c) knowledge about differences between COVID-19 and other respiratory diseases, transmission routes, recommended personal protective equipment (PPE), and management of pregnant and postpartum women in the context of the COVID-19 pandemic; and (d) nurse-midwives’ attitudes toward care and management of pregnant women and newborns with COVID-19.
At the time of the study, there were no validated survey tools. We developed the questionnaire based on guidelines from the World Health Organization (WHO) and the Kenyan Ministry of Health. The researchers developed two sets of questions that assessed knowledge, attitudes, and practice related to COVID-19 management among pregnant and postpartum women. The first set of questions was presented as factual (true/false) statements on COVID-19 management, and the second set requested that participants indicated their agreement with specific statements on a five-point Likert scale (1 = “strongly disagree,” 2 = “disagree,” 3 = “uncertain,” 4 = “agree,” and 5 = “strongly agree”). The knowledge questions were weighted with scores of 1 for correct answers and 0 for incorrect answers.
Statistical Analyses
Data were extracted from SurveyMonkey into Microsoft Excel, cleaned, and then exported to SPSS version 23.0 for coding and analysis. Descriptive statistics (mean, standard deviation [SD], and range) were used to present numerical data. Categorical data were summarized and presented as frequencies and percentages. To assess participants’ knowledge and attitudes, ratings of agree and strongly agree on the five-point Likert scale were scored as 1 point and ratings of uncertain, disagree, and strongly disagree were scored as 0. There were 11 items covering attitudes and 10 items exploring knowledge; therefore, an attitude score ≥6 was considered the cutoff point to indicate a positive attitude, and a knowledge score ≥5 was considered to indicate sufficient knowledge. A multiple logistic regression model was used to assess the associations between the dependent variables (attitude and knowledge) and independent variables (sociodemographic characteristics: gender, age, years of practice as a nurse-midwife, and place of work). Adjusted odds ratios (OR), 95% confidence intervals (CI), and p-values were used to determine the presence of significant associations between the categorical dependent and independent variables. A p-value <.05 was considered statistically significant.
Results
In total, 85 nurse-midwives participated in this study, giving a response rate of 72%. Most participants were female (n = 69, 81.2%), 52.9% (n = 45) worked in labor wards, and 57.6% (n = 49) worked in rural hospitals. The average age was 36.83 years (SD = 6.38 years; range 22–54 years). Most participants (n = 68, 80.0%) were nurse-midwives registered as a Kenya Registered Community Health Nurse and 76.5% (n = 65) had more than five years of nursing/midwifery practice (Table 1).
Table 1.
Participants’ Demographic Characteristics.
| Variables | n | % | |
|---|---|---|---|
| Gender | Female | 69 | 81.2 |
| Male | 16 | 18.8 | |
| Age, years | ≤30 | 10 | 13.2 |
| 31–40 | 47 | 61.8 | |
| >40 | 19 | 25.0 | |
| Designation | KRCHN | 68 | 80.0 |
| BScN/M | 17 | 20.0 | |
| Department | Antenatal | 15 | 17.6 |
| Labor ward | 45 | 52.9 | |
| Outpatient | 14 | 16.5 | |
| Family planning clinic/Newborn unit/Postnatal ward | 11 | 12.9 | |
| Place of work | Urban | 36 | 42.4 |
| Rural | 49 | 57.6 | |
| Years of practice | ≤5 | 20 | 23.5 |
| 6–10 | 34 | 40.0 | |
| 11–15 | 19 | 22.4 | |
| ≥16 | 12 | 14.1 |
KRCHN = Kenya Registered Community Health Nurse; BScN/M = Bachelor of Science in Nursing/Midwifery.
Nurse-Midwives’ Knowledge About the Management of COVID-19
Table 2 shows participants’ level of knowledge about managing pregnant and postpartum women with COVID-19. Most nurse-midwives (n = 57, 71.25%) were knowledgeable and most (n = 56, 70%) strongly disagreed that mental health and psychological status were not important in emergency preparedness planning for COVID-19. Similarly, most participants (n = 64, 80%) strongly agreed that frequent handwashing with soap and water or using alcohol-based sanitizer was advised. In addition, 55 participants (68.75%) indicated that pregnant women should be encouraged to visit a facility if they were sick with fever, cough, or had difficulty breathing. However, relatively few participants (n = 22, 27.5%) reported that the effects of COVID-19 on pregnancy, birth, and puerperium were fully understood.
Table 2.
Comparison of Knowledge About Managing COVID-19 Among Participants.
| Knowledge about management of COVID-19 | Strongly disagree n (%) | Disagree n (%) | Uncertain n (%) | Agree n (%) | Strongly agree n (%) |
|---|---|---|---|---|---|
| Mental health and psychological status are not an important part of emergency preparedness planning for COVID-19. | 57 (71.25) | 13 (16.25) | 1 (1.25) | 4 (5.00) | 5 (6.25) |
| Effects of COVID-19 on pregnancy, birth, and puerperium are fully understood. | 12 (15.00) | 27 (33.75) | 28 (35.00) | 10 (12.50) | 3 (3.75) |
| Frequent handwashing with soap and water or sanitization is advised. | 8 (10.00) | 2 (2.50) | 1 (1.25) | 5 (6.25) | 64 (80.00) |
| Surgical face masks should only be used when handling a client with confirmed COVID-19. | 56 (70.00) | 15 (18.75) | 1 (1.25) | 2 (2.50) | 6 (7.50) |
| Pregnant women should be encouraged to visit any facility if sick with fever, cough, or difficulty breathing. | 5 (6.25) | 2 (2.50) | 5 (6.25) | 13 (16.25) | 55 (68.75) |
| Women are discouraged from having accompanied hospital visits. | 14 (17.50) | 26 (32.50) | 4 (5.00) | 23 (28.75) | 13 (16.25) |
| Pregnant women may be more susceptible to COVID-19 than the general population. | 6 (7.50) | 2 (2.50) | 9 (11.25) | 32 (40.00) | 31 (38.75) |
| Consultation via telephone and video is encouraged during pregnancy. | 4 (5.00) | 12 (15.00) | 10 (12.50) | 32 (40.00) | 22 (27.5) |
Table 3 shows the results of the bivariate analysis of knowledge about COVID-19 management and participants’ sociodemographic characteristics. Males were 28.2% less likely to have sufficient knowledge about the management of COVID-19 than females (OR 0.718, 95% CI: 0.138–3.741), although the difference was not statistically significant (p = .694). Participants working in urban hospital settings (n = 28) had higher knowledge about managing COVID-19 than those working in rural areas (n = 35), with a 22.2% likelihood of having greater knowledge (OR 0.718, 95% CI: 0.138–3.741). However, the difference in the knowledge gap between those working in rural and urban areas was not statistically significant (p = .784). Moreover, nurse-midwives with 6–10 years of practice reported the highest knowledge (n = 26), whereas individuals with more than 21 years of practice recorded the lowest knowledge (n = 3) despite their long duration of practice. Participants with more than 20 years of practice were 7.2% less likely to have sufficient knowledge about managing COVID-19 than those with ≤5 years of practice (OR 0.928, 95% CI: 0.037–23.544; p = .964). In addition, more nurse-midwives aged 31–40 years (n = 40) reported sufficient knowledge about managing COVID-19 among pregnant and postpartum women than in other age groups.
Table 3.
Sociodemographic Factors Associated with Knowledge About Managing COVID-19.
| Knowledge | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Insufficient | Sufficient | ||||
| n (%) | n (%) | Adjusted OR | 95% CI | p value | ||
| Gender | Female | 11 (16.9) | 54 (83.1) | Ref | ||
| Male | 3 (20.0) | 12 (80.0) | 0.718 | 0.138–3.741 | .694 | |
| Place of work | Rural | 8 (18.6) | 35 (81.4) | Ref | ||
| Urban | 5 (15.2) | 28 (84.8) | 1.224 | 0.0289–5.186 | .784 | |
| Years of practice as a nurse/midwife | ≤5 | 3 (16.7) | 15 (83.3) | Ref | ||
| 6–10 | 5 (16.1) | 26 (83.9) | 1.164 | 0.187–7.245 | .871 | |
| 11–15 | 3 (15.8) | 16 (84.2) | 2.021 | 0.236–17.290 | .520 | |
| 16–20 | 1 (14.3) | 6 (85.7) | 1.700 | 0.091–31.638 | .722 | |
| ≥21 | 2 (40.0) | 3 (60.0) | 0.928 | 0.037–23.544 | .964 | |
| Age group (years) | ≤30 | 1 (11.1) | 8 (88.9) | Ref | ||
| 31–40 | 6 (13.0) | 40 (87.0) | 0.7 | 0.055–8.869 | .783 | |
| >40 | 5 (26.3) | 14 (73.7) | 0.36 | 0.020–6.340 | .485 | |
OR = odds ratio; CI = confidence interval.
The average score for knowledge about managing COVID-19 among pregnant and postpartum women was 74.2% (SD = 14.8). Specifically, for precautions during triage of antenatal clients, most participants reported the need to wear a medical face mask (n = 72, 84.7%) and sanitize frequently after each client (n = 74, 87.1%). Moreover, most participants indicated that pregnancy danger signs should be included as part of antenatal education (n = 71, 83.5%), and that triage criteria should include assessment for conditions that may exacerbate COVID-19 (n = 75, 88.2%). However, only 17 (20%) participants reported that surgical contraceptives should be delayed until COVID-19 was resolved, and 46 (54.1%) believed all pregnant women should continue with monthly antenatal clinic visits.
Knowledge of PPE required during labor for women with suspected COVID-19 was evident in nurse-midwives in both rural and urban hospital settings. For example, most participants reported gloves (n = 77, 90.6%), medical masks (n = 71, 83.5%), gowns (n = 78, 91.8%), and face shields (n = 74, 87.1%) should be worn. For postnatal care during the COVID-19 pandemic, including for new mothers with COVID-19, 20% (n = 17) of participants in both rural and urban hospital settings reported that surgical contraceptives should be delayed until COVID-19 was resolved, and 41 (48.2%) thought breastfeeding initiation should be delayed until the mother had washed her hands and breasts with soap and water (Table 4).
Table 4.
Knowledge About COVID-19 Management Practices.
| Knowledge assessment (N = 85) | Correct answer | Correct score n (%) |
|---|---|---|
| Mother to child transmission of COVID-19 can occur through: | ||
| Blood transfusion | No | 66 (77.6) |
| Amniotic fluid | No | 68 (80.0) |
| Breastmilk | No | 58 (68.2) |
| Saliva | Yes | 65 (76.5) |
| Urine | No | 79 (92.9) |
| When conducting triage of an antenatal client, the nurse/midwife should: | ||
| Maintain at least a 1-meter distance from the client | Yes | 64 (75.3) |
| Wear a medical face mask | Yes | 72 (84.7) |
| Sanitize frequently and after contact with each client | Yes | 74 (87.1) |
| Wear full PPE | No | 63 (74.1) |
| Wear gloves | Yes | 51 (60) |
| The following statements are true about the management of a pregnant woman with suspected COVID-19: | ||
| Antenatal screening should be suspended to allow treatment of COVID-19 | False | 68 (80) |
| Pregnancy danger signs should be included as part of antenatal education | True | 71 (83.5) |
| All pregnant women should continue with monthly antenatal clinic visits | True | 46 (54.1) |
| The following is true when caring for a woman in labor: | ||
| Triage criteria should include assessment for conditions that may exacerbate COVID-19 | True | 75 (88.2) |
| Birth partners should be encouraged to accompany the woman into the delivery room | False | 61 (71.8) |
| A COVID-19 suspected/positive mother should wear a medical mask during the entire labor process | True | 72 (84.7) |
| General anesthesia is recommended for a COVID-19 suspected or positive mother | False | 77 (90.6) |
| When conducting delivery for a woman with suspected COVID-19, the midwife should don the following PPE: | ||
| Gloves | Yes | 77 (90.6) |
| Medical mask | Yes | 71 (83.5) |
| Gown | Yes | 78 (91.8) |
| Goggles | Yes | 73 (85.9) |
| Face shield | Yes | 74 (88.1) |
| Coverall | Yes | 53 (62.4) |
| Head cover | Yes | 68 (80) |
| Rubber boots | Yes | 75 (88.2) |
| Heavy-duty gloves | No | 67 (78.8) |
| The following is correct about postnatal care for women during the COVID-19 pandemic: | ||
| COVID-19-negative women who deliver through SVD should be kept for no more than 24 h for observation before discharge | True | 62 (72.9) |
| Postpartum family planning should be encouraged before a woman leaves the hospital | True | 50 (58.8) |
| Surgical contraceptives should be delayed until COVID-19 is resolved | True | 17 (20) |
| Low-risk postpartum women should be reviewed at 6 weeks (SVD) and 2 weeks (CS) | True | 67 (78.8) |
| The following statements are true regarding the care of a COVID-19-positive mother: | ||
| COVID-19-positive mothers should be separated from their infants after birth | False | 64 (75.3) |
| Breastfeeding initiation should be delayed until the mother has washed her hands and breasts with soap and water | True | 41 (48.2) |
| A COVID-19-positive mother can breastfeed her newborn if she is wearing an N95 mask | True | 61 (71.8) |
| A COVID-19 positive mother can express breast milk | True | 60 (70.6) |
| Women with comorbidities should be accorded individualized care | True | 65 (76.5) |
| Average score | 74.2% (SD = 14.8) | |
PPE = personal protective equipment; SVD = spontaneous vaginal delivery; SD = standard deviation.
Attitudes Toward Management of COVID-19 in Pregnant and Postpartum Women
Attitude is an essential component in nursing that enhances the assessment and understanding of individuals’ perceptions of issues and the process of care. Table 5 presents the analysis of nurse-midwives’ attitudes toward the management of COVID-19 during pregnancy and puerperium. Most nurse-midwives indicated a high degree of agreement with various attitude constructs regarding the management of COVID-19 during pregnancy and the postpartum period. For example, 46 (60.5%) participants thought COVID-19 could be reduced by HCWs’ active participation in hospital infection control, and 42 (55.3%) believed COVID-19-positive pregnant and postnatal women should be isolated from other patients with COVID-19. Nevertheless, most participants feared getting COVID-19 from exposure at work (n = 62, 81.6%), and 66 (86.9%) were worried about transmitting the virus to family members from their exposure at work. In addition, only 34.2% of the participants reported that they were not afraid to be the first HCW to come into contact with a pregnant patient with COVID-19.
Table 5.
Nurse-Midwives’ Attitudes Toward Managing COVID-19.
| Attitude toward managing COVID-19 during pregnancy and puerperium | Strongly disagree n (%) | Disagree n (%) | Uncertain n (%) | Agree n (%) | Strongly agree n (%) |
|---|---|---|---|---|---|
| I fear that I will get COVID-19 from exposure at work. | 5 (5.6) | 3 (3.9) | 6 (7.9) | 29 (38.2) | 33 (43.4) |
| I am worried one of my family members may get COVID-19 from my exposure at work. | 4 (5.3) | 3 (3.9) | 3 (3.9) | 30 (39.5) | 36 (47.4) |
| I am not afraid to be the first healthcare worker to come into contact with a pregnant patient with COVID-19. | 23 (30.3) | 14 (18.4) | 13 (17.1) | 22 (28.9) | 4 (5.3) |
| I am confident in my ability to don PPE. | 9 (11.8) | 8 (10.5) | 15 (19.7) | 29 (38.2) | 15 (19.7) |
| I am confident in my ability to doff PPE. | 10 (13.2) | 8 (10.5) | 16 (21.1) | 29 (38.2) | 13 (17.1) |
| I am confident in my ability to care for a woman with COVID-19 during pregnancy and childbirth. | 8 (10.5) | 12 (15.8) | 27 (35.5) | 25 (32.9) | 4 (5.3) |
| COVID-19-positive pregnant and postnatal women should be kept in isolation from the other COVID-19 patients. | 3 (3.9) | 1 (1.3) | 2 (2.6) | 28 (36.8) | 42 (55.3) |
| I would voluntarily disclose my status if I come into contact with a COVID-19 patient. | 4 (5.3) | 4 (5.3) | 8 (10.5) | 27 (35.5) | 33 (43.4) |
| I must frequently update myself on COVID-19. | 1 (1.3) | 2 (2.6) | 0 (0.0) | 20 (26.3) | 53 (69.7) |
| Prevalence of COVID-19 can be reduced by the active participation of healthcare workers in hospital infection control programs. | 2 (2.6) | 1 (1.3) | 2 (2.6) | 25 (32.9) | 46 (60.5) |
| If a COVID-19 vaccine was available, I would have it. | 7 (9.2) | 2 (2.6) | 19 (25.0) | 18 (23.8) | 30 (39.5) |
PPE = personal protective equipment.
Although female participants (n = 39) reported more positive attitudes than males (n = 10), further analysis showed that the odds of having a positive attitude toward managing COVID-19 among male nurse-midwives were 30% higher than that among female nurse-midwives (OR 1.295, 95% CI: 0.317–5.282) (Table 6). However, the difference was not statistically significant (p = .719). Moreover, significantly more participants working in urban areas had positive attitudes toward managing COVID-19 than those working in rural areas. The odds of having a positive attitude among participants working in urban areas were 3.7 times higher than individuals working in rural areas (OR 3.724, 95% CI: 1.042–13.31; p = .043). Similarly, participants with 11–15 years of practice were nine times more likely to have a positive attitude toward managing COVID-19 among pregnant and postpartum women than individuals with ≤5 years of practice (OR 9.049, 95% CI: 1.342–61.01; p = .024). Overall, only years of practice and place of work were significantly associated with nurse-midwives’ positive attitudes toward managing COVID-19 among pregnant and postpartum women.
Table 6.
Sociodemographic Factors Associated with Nurse-Midwives’ Attitudes Toward Managing COVID-19 in Pregnant and Postpartum Women.
| Attitude | ||||||
|---|---|---|---|---|---|---|
| Characteristics | Negative | Positive | Adjusted OR | 95% CI | p value | |
| n (%) | n (%) | |||||
| Gender | Female | 22 (36.1) | 39 (63.9) | Ref | ||
| Male | 5 (33.3) | 10 (66.7) | 1.295 | 0.317–5.282 | .719 | |
| Place of work | Rural | 17 (40.5) | 25 (59.55) | Ref | ||
| Urban | 8 (25.8) | 23 (74.2) | 3.724 | 1.042–13.31 | .043* | |
| Years of practice as a nurse/midwife | ≤5 | 8 (47.1) | 9 (52.9) | Ref | ||
| 6–10 | 12 (40.0) | 18 (60.0) | 2.62 | 0.528–12.996 | .238 | |
| 11–15 | 4 (22.2) | 14 (77.8) | 9.049 | 1.342–61.01 | .024* | |
| 16–20 | 1 (16.7) | 5 (83.3) | 8.842 | 0.500–156.47 | .137 | |
| ≥21 | 2 (40) | 3 (60) | 2.711 | 0.114–64.612 | .538 | |
| Age group, years | ≤30 | 3 (37.5) | 5 (62.5) | Ref | ||
| 31–40 | 15 (34.1) | 29 (65.9) | 0.197 | 0.022–1.794 | .149 | |
| >40 | 6 (31.6) | 13 (68.4) | 0.245 | 0.019–3.135 | .28 | |
OR = odds ratio; CI = confidence interval.
Preparedness for Managing Pregnant and Postpartum Women with COVID-19 Among Nurse-Midwives
Most participants (78.8%) reported having undertaken IPC training and 69.4% had received an overview of COVID-19 (Table 7). However, the findings indicated low preparedness for the management of COVID-19 during pregnancy (23.5%), labor and delivery (27.0%), and puerperium (20.0%).
Table 7.
Training About COVID-19.
| Training on COVID-19 received | n (%) | Place of work | |
|---|---|---|---|
| Rural n (%) | Urban n (%) | ||
| Overview of COVID-19 | 59 (69.4) | 31 (52.5) | 28 (47.5) |
| Management of COVID-19 patients | 35 (43.5) | 15 (42.9) | 20 (57.1) |
| Management of COVID-19 during pregnancy | 20 (23.5) | 7 (35.0) | 13 (65.0) |
| Management of COVID-19 during labor and delivery | 23 (27.0) | 9 (39.1) | 14 (60.9) |
| Management of COVID-19 during puerperium | 17 (20.0) | 6 (35.3) | 11 (64.7) |
| Infection prevention and control | 67 (78.8) | 37 (55.2) | 30 (44.8) |
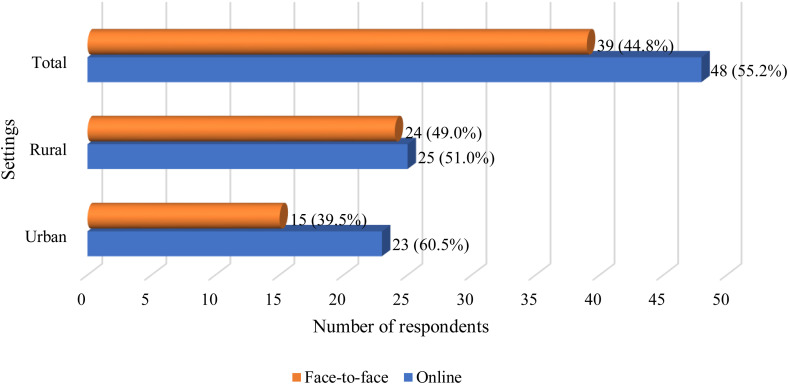
As shown in Figure 1, most participants had received online training on the management of COVID-19 (55.2%), and 44.8% received face-to-face training. Further analysis revealed that a larger proportion of nurse-midwives working in urban hospital settings had received online training compared to those in rural hospitals (60.5% vs. 51%).
Figure 1.
Mode of training on COVID-19 management.
Table 8 summarizes participants’ training on the use of PPE. Although most participants had received training on donning gloves (81.1%), medical masks (82.3%), gowns (69.4%), and goggles (67.0%), only 20.0% had received training on donning heavy-duty gloves and 45.9% had received training on coveralls. Similarly, most had received training on doffing gloves (81.1%), medical masks (80.0%), face shields (63.5%), and rubber boots (58.8%), but fewer participants had received training on doffing coveralls (47.0%) and heavy-duty gloves (20.0%).
Table 8.
Participants’ Training on Donning and Doffing Personal Protective Equipment.
| Type of PPE | Donning PPE | Doffing PPE | ||||
|---|---|---|---|---|---|---|
| Place of work | n (%) | Place of work | n (%) | |||
| Rural n (%) | Urban n (%) | Rural n (%) | Urban n (%) | |||
| Gloves | 38 (55.1) | 31 (44.9) | 69 (81.1) | 37 (53.6) | 32 (46.4) | 69 (81.1) |
| Medical mask | 40 (57.1) | 30 (42.9) | 70 (82.3) | 39 (57.4) | 29 (42.6) | 68 (80.0) |
| Gown | 29 (49.2) | 30 (50.8) | 59 (69.4) | 31 (50.0) | 31 (50.0) | 62 (72.9) |
| Goggles | 28 (49.1) | 29 (50.9) | 57 (67.0) | 28 (50.0) | 28 (50.0) | 56 (65.9) |
| Face shield | 24 (46.2) | 28 (53.8) | 52 (61.1) | 26 (48.1) | 28 (51.9) | 54 (63.5) |
| Coverall | 16 (41.0) | 23 (59.0) | 39 (45.9) | 18 (45.0) | 22 (55.0) | 40 (47.0) |
| Head cover | 24 (47.1) | 27 (52.9) | 51 (60.0) | 26 (49.1) | 27 (50.9) | 53 (62.3) |
| Rubber boots | 23 (46.0) | 27 (54.0) | 50 (58.8) | 24 (48.0) | 26 (52.0) | 50 (58.8) |
| Heavy-duty gloves | 10 (58.8) | 7 (41.2) | 17 (20.0) | 10 (58.8) | 7 (41.2) | 17 (20.0) |
PPE = personal protective equipment.
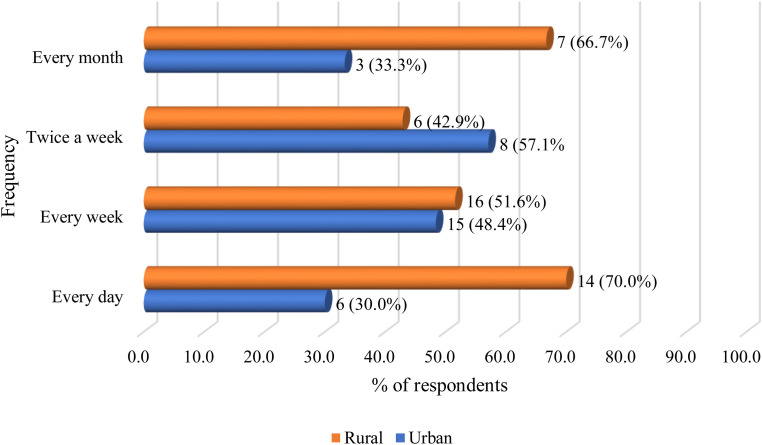
As shown in Figure 2, most participants working in rural and urban hospital settings reported that they would benefit from weekly updates on the management of COVID-19. Of those who thought they would benefit from daily updates 70%, were from rural areas compared to 30% urban.
Figure 2.
Frequency of COVID-19 management updates.
Discussion
This study was conducted to assess knowledge about, attitudes toward, and preparedness for managing pregnant and postpartum women with COVID-19 among nurse-midwives in Kenya. To our knowledge, this is the first study conducted in Kenya or the wider African region that assessed these factors among nurse-midwives. Globally, few studies have examined nurse-midwives knowledge about the management of pregnant and postpartum women during infectious disease pandemics. Data in this study were collected six months after the outbreak of the COVID-19 pandemic in Kenya. Therefore, IPC measures for COVID-19 and HCW training were operational throughout Kenya. Our participants worked across a large coverage area, and the majority of participants (57.6%) were from rural areas. In Kenya, rural counties reported fewer cases of COVID-19 compared with urban counties and had limited access to information, COVID-19 diagnosis, and support services. Our findings highlighted that a number of factors affected nurse-midwives’ knowledge, attitudes, and preparedness, which could be useful to inform future infectious disease training and disaster preparedness.
Knowledge
Our findings indicated that 77% of participants had sufficient knowledge about COVID-19, which was lower than findings reported from Vietnam (88.4%) (Huynh et al., 2020) and Nigeria (78.6%) (Ayinde et al., 2020). However, knowledge in our study was higher than that in studies from Ethiopia (Asemahagn, 2020) (70%), Uganda (Olum et al., 2020) 69%, Bangladesh (Ferdous et al., 2020) (48.3%), and other low- and middle-income countries (53%) (Semaan et al., 2020). Interestingly, the level of knowledge among our participants was similar irrespective of gender, age, place of work, and years of practice. Although studies show a difference in expertise between diploma and bachelor level nurses, most nurses in Kenya are community health registered nurses. We did not have a sufficient sample to make this assessment (Aiken et al., 2011); however, we cannot rule out the possibility that education level may be associated with the level of knowledge.
Rural and remote areas in Kenya are understaffed, and there are challenges to recruitment and retention because of poor infrastructure, limited training opportunities, high workloads, and inadequate supplies. In contrast to other studies where HCWs from urban areas had more knowledge than those from rural areas (Ayinde et al., 2020; Zenbaba et al., 2020), we found no significant difference in knowledge between nurse-midwives working in urban and rural settings. This may be related to variations in study topics, study periods, and IPC training among nurse-midwives working in maternal and child health. Furthermore, restricted movement because of COVID-19 mitigation measures led to innovative online training strategies to reach nurse-midwives in rural areas in Kenya.
In this study, the mean knowledge score was 74%, which indicated good knowledge among participating nurse-midwives. However, knowledge about managing COVID-19 during the antenatal (72%), labor/delivery (83.3%), and postnatal (63%) periods varied. In addition, nurse-midwives’ responses regarding knowledge of guidelines were inconsistent, including continuing antenatal visits, surgical contraceptives, separation of infants from COVID-positive mothers after birth, and the presence of birth partners during delivery. This highlighted a critical issue that needs special attention from policymakers and hospital administrators because the lack of a clear understanding of guidelines may contribute to the low uptake of maternal and reproductive services (Kimani et al., 2020).
Attitudes
Generally, most participants (64%) had positive attitudes toward the prevention and control of COVID-19, which was similar to findings from Nigeria (Ayinde et al., 2020). However, we found that nurse-midwives working in urban areas were 3.7 times more likely to have positive attitudes than those in rural areas. This may be attributed to training, access to PPE, diagnostics, and resources to manage advanced COVID-19 cases (Shaibu et al., 2021). Kenya also had more COVID-19 cases in urban areas, which may have led to better awareness and confidence in caring for pregnant women with COVID-19.
Most nurse-midwives were afraid of exposure to COVID-19 at work and transmitting the virus to family members. These findings support those from previous studies in Vietnam (Huynh et al., 2020), Italy (Ramaci et al., 2020), and China (Zhang et al., 2020) that reported similar attitudes. However, only 63% of participants were willing to receive a COVID-19 vaccine in this study. This finding indicated vaccine hesitancy was likely to be a hurdle for the ongoing COVID-19 vaccination process. This finding was similar to a recent study conducted in Hong Kong that explored the potential uptake of the COVID-19 vaccine among nurses (Kwok et al., 2021). As of May 2021, only 136,000 front line HCWs (out of 1.2 million targeted) had been vaccinated in Kenya. Vaccine hesitancy threatens infection control in African countries (Afolabi & Ilesanmi, 2021), and HCWs’ vaccine hesitancy can also weaken trust and negatively influence vaccine uptake by the general population (Karafillakis et al., 2016).
We identified discrepancies in participants’ confidence in doffing and donning PPE. For example, nurse-midwives in rural settings were 72% less likely to agree that they were confident in their ability to doff PPE compared with participants from urban hospital settings (OR 0.280, 95% CI: 0.078–1.000; p = .050); this difference was statistically significant. It was also concerning that many participants were not confident in caring for pregnant women with COVID-19 during pregnancy and childbirth. This finding may reflect a lack of specific training on the management of pregnant women with COVID-19 during pregnancy and childbirth.
Preparedness
Previous studies showed that IPC training and having clear guidelines predicted improved knowledge and practice (Asemahagn, 2020; Olum et al., 2020; Zenbaba et al., 2020). The primary aim of IPC training is to enhance knowledge about the disease and prevention measures, including accessing required PPE and guidelines. In this study, a majority of participants (56.5%) had received online training and 45.9% had received face-to-face training. Most nurse-midwives had been trained to don and doff gloves, masks, gowns, goggles, face shields, and head covers. However, many had not received training on using coveralls, rubber boots, and heavy-duty gloves. Furthermore, most nurse-midwives received training on IPC and an overview of COVID-19, but only 20%–27% had received training on the management of care of women during pregnancy, labor, and the postnatal period. This indicated a critical gap in training that may negatively impact the care of pregnant women. Given the high maternal mortality and morbidity in the region, stakeholders need to address this critical area of concern. Educational interventions should prioritize nurse-midwives’ ability to manage women during the childbirth continuum.
Strengths and Limitations
Although this study included nurse-midwives working in a range of areas, there were some limitations that affected the generalizability of the findings. Our findings were based on data collected using an online survey platform; therefore, nurse-midwives without internet access and technology were excluded. This study only included nurse-midwives enrolled in a private university nursing program and working in a private hospital; therefore, the results may not reflect all nurse-midwives in Kenya. In addition, the sample size was small and may not be adequate to measure all significant differences between the groups. As this study was conducted at the beginning of the COVID-19 pandemic, there were no available validated tools to examine this phenomenon. The questionnaire used was not piloted, limiting the findings’ reliability and sensitivity. However, this study indicated that management of vulnerable populations such as pregnant women during the COVID-19 pandemic warrants special consideration to address the identified issues.
Implications for Practice
Our findings have implications for continued nursing education and practice. The knowledge and awareness of COVID-19 transmission influence nurse-midwives’ risk perception and ability to implement prevention strategies (Bhagavathula et al., 2020). Insufficient knowledge on managing pregnant and postpartum women could directly affect practice and lead to poor infection control techniques, further increasing adverse outcomes. Our findings highlight the need for tailored training on COVID-19 management for women during pregnancy, childbirth, and the postnatal period, focusing on gaps identified in different regions, particularly on the care of women during pregnancy, labor, and the postnatal period. Additional education should emphasize that pregnant women are at high risk for developing severe diseases and requiring hospitalization, mechanical ventilation, and critical care support. The COVID-19 pandemic is a rapidly evolving crisis with a miscellany of information; therefore, it may be useful for the policymakers or nursing organizations such as NCK to collate, summarize, and disseminate current evidence through easily accessible and credible platforms. Beyond more training, further research is needed to explore how nurse-midwives’ knowledge of COVID-19 affects their clinical practice. There is also the need for psychological and emotional support for nurse-midwives caring for patients on the front line. Without the strategic implementation of specific knowledge on the care of pregnant women during this ongoing pandemic, maternal and child morbidity and mortality outcomes may exacerbate.
Conclusion
Although most participants had undertaken IPC training and received an overview of COVID-19, they had low preparedness to manage COVID-19 during pregnancy, labor, and puerperium. Most participants had positive attitudes toward the prevention and control of COVID-19; however, they were afraid of contracting COVID-19 and transmitting the virus to their families. Nurse-midwives’ responses were inconsistent regarding the Kenyan government's COVID-19 guidelines for managing and caring for pregnant women. It is recommended that continued professional development be offered to nurse-midwives so that they can stay abreast of evolving COVID-19 guidelines for maternal health. It is also recommended that addressing vaccine hesitancy among nurses and midwives be prioritized, as this has implications for their advocacy for the public to be vaccinated. Moreover, insufficient uptake of vaccinations by nurses and midwives increases the risk of COVID-19 infections by new variants, which could lead to more hospitalizations, inadequate staffing, increased workloads, lack of trust in COVID-19 vaccines among the public, and further straining a fragile health system. Building trust in COVID-19 vaccination efforts among the general population should start with increasing nurses’ uptake of the COVID-19 vaccines. This will require evidence-based interventions that are informed by large-scale mixed methods studies designed to explore push-pull factors in vaccine hesitancy among HCW and harness local expertise to implement contextual interventions to increase uptake. In addition, a collaborative effort involving a communication strategy that includes social media, the government health care workers, and other relevant stakeholders like the Nursing Council of Kenya, and Nurses’ Associations, among others, will be required to facilitate vaccine uptake.
Footnotes
Authors’ Note: Ethical approval was granted by the Aga Khan University Institutional Ethics Review Committee (ref #2020/IERC-70), and a research permit was granted by the National Commission for Science, Technology, and Innovation (ref #NACOSTI/P/20/6778).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: Aga Khan University Kenya, School of Nursing and Midwifery Dean’s Fund (ref #June 2020).
ORCID iDs: Rose Maina https://orcid.org/0000-0002-4548-8252
Rachel Wangari Kimani https://orcid.org/0000-0002-7735-7302
Carolyne K. Nyariki https://orcid.org/0000-0001-8756-7752
References
- Abdel Wahed W. Y., Hefzy E. M., Ahmed M. I., Hamed N. S. (2020). Assessment of knowledge, attitudes, and perception of health care workers regarding COVID-19: A cross-sectional study from Egypt. Journal of Community Health, 45(6), 1242–1251. 10.1007/s10900-020-00882-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afolabi A. A., Ilesanmi O. S. (2021). Dealing with vaccine hesitancy in Africa: The prospective COVID-19 vaccine context. The Pan African Medical Journal, 38(3). 10.11604/pamj.2021.38.3.27401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L. H., Cimiotti J. P., Sloane D. M., Smith H. L., Flynn L., Neff D. F. (2011). Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care, 49(12), 1047–1053. 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, Debenham L, Llavall AC, Dixit A, Zhou D, Balaji R, Lee SI, Qiu X, Yuan M, Coomar D, Sheikh J, Lawson H, Ansari K, van Wely M, … for PregCOV-19 Living Systematic Review Consortium. (2020). Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ, 370, m3320. 10.1136/bmj.m3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsoghair M., Almazyad M., Alburaykan T., Alsultan A., Alnughaymishi A., Almazyad S., Alharbi M., Alkassas W., Almadud A., Alsuhaibani M. (2021). Medical students and COVID-19: Knowledge, preventive behaviors, and risk perception. International Journal of Environmental Research and Public Health, 18(2), 842. https://www.mdpi.com/1660-4601/18/2/842. 10.3390/ijerph18020842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asemahagn M. A. (2020). Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: A cross-sectional survey. Tropical Medicine and Health, 48(1), 1–11. 10.1186/s41182-020-00254-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashish K., Gurung R., Kinney M. V., Sunny A. K., Moinuddin M., Basnet O., Paudel P., Bhattarai P., Subedi K., Shrestha M. P. (2020). Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: A prospective observational study. The Lancet Global Health, 8(10), e1273–e1281. 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayinde O., Usman A. B., Aduroja P., Gbolahan A. (2020). A cross-sectional study on Oyo state health care workers knowledge, attitude and practice regarding corona virus disease 2019 (COVID-19).
- Bhagavathula A. S., Aldhaleei W. A., Rahmani J., Mahabadi M. A., Bandari D. K. (2020). Knowledge and perceptions of COVID-19 among health care workers: Cross-sectional study. JMIR Public Health and Surveillance, 6(2), e19160–e19160. 10.2196/19160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Foghi C., Dell'Oste V., Cordone A., Bertelloni C. A., Bui E., Dell'Osso L. (2020). PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: What can we expect after the COVID-19 pandemic. Psychiatry Research, 292, 113312. 10.1016/j.psychres.2020.113312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewska B., Barratt I., Townsend R., Kalafat E., van der Meulen J., Gurol-Urganci I., O'Brien P., Morris E., Draycott T., Thangaratinam S., Le Doare K., Ladhani S., von Dadelszen P., Magee L., Khalil A. (2021). Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. The Lancet Global Health, 9(6), e759–e772. 10.1016/S2214-109X(21)00079-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delahoy M. J., Whitaker M., O’Halloran A., Chai S. J., Kirley P. D., Alden N., Kawasaki B., Meek J., Yousey-Hindes K., Anderson E. J. (2020). Characteristics and maternal and birth outcomes of hospitalized pregnant women with laboratory-confirmed COVID-19—COVID-NET, 13 states, March 1–August 22, 2020. Morbidity and Mortality Weekly Report, 69(38), 1347–1354. 10.15585/mmwr.mm6938e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdous M. Z., Islam M. S., Sikder M. T., Mosaddek A. S. M., Zegarra-Valdivia J., Gozal D. (2020). Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: An online-based cross-sectional study. PLoS One, 15(10), e0239254. 10.1371/journal.pone.0239254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitobu C. M., Gichangi P. B., Mwanda W. O. (2018). The effect of Kenya’s free maternal health care policy on the utilization of health facility delivery services and maternal and neonatal mortality in public health facilities. BMC Pregnancy and Childbirth, 18(1), 77. 10.1186/s12884-018-1708-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giusti E. M., Pedroli E., D'Aniello G. E., Badiale C. S., Pietrabissa G., Manna C., Badiale M. S., Riva G., Castelnuovo G., Molinari E. (2020). The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Frontiers in Psychology, 11, 1684. 10.3389/fpsyg.2020.01684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M., Singh P., Singh K., Shekhar S., Agrawal N., Misra S. (2021). The effect of the COVID–19 pandemic on maternal health due to delay in seeking health care: Experience from a tertiary center. International Journal of Gynecology & Obstetrics, 152(2), 231–235. 10.1002/ijgo.13457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huynh G., Nguyen T. N. H., Vo K. N., Pham L. A. (2020). Knowledge and attitude toward COVID-19 among healthcare workers at district 2 hospital, Ho Chi Minh city. Asian Pacific Journal of Tropical Medicine, 13(6), 260. 10.4103/1995-7645.280396 [DOI] [Google Scholar]
- Karafillakis E., Dinca I., Apfel F., Cecconi S., Wűrz A., Takacs J., Suk J., Celentano L. P., Kramarz P., Larson H. J. (2016). Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Vaccine, 34(41), 5013–5020. 10.1016/j.vaccine.2016.08.029 [DOI] [PubMed] [Google Scholar]
- Kimani R. W., Maina R., Shumba C., Shaibu S. (2020). Maternal and newborn care during the COVID-19 pandemic in Kenya: Re-contextualising the community midwifery model. Human Resources for Health, 18(1), 1–5. 10.1186/s12960-020-00518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok K. O., Li K.-K., Wei W. I., Tang A., Wong S. Y. S., Lee S. S. (2021). Editor’s choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. International Journal of Nursing Studies, 114, 103854. 10.1016/j.ijnurstu.2020.103854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lokken, E. M., Huebner, E. M., Taylor, G. G., Hendrickson, S., Vanderhoeven, J., Kachikis, A., Coler, B., Walker, C. L., Sheng, J. S., Al-Haddad, B. J. S., McCartney, S. A., Kretzer, N. M., Resnick, R., Barnhart, N., Schulte, V., Bergam, B., Ma, K. K., Albright, C., Larios, V., … Washington State COVID-19 in Pregnancy Collaborative. (2021). Disease severity, pregnancy outcomes, and maternal deaths among pregnant patients with severe acute respiratory syndrome coronavirus 2 infection in Washington state. American Journal of Obstetrics and Gynecology, 225(1), 77.e1–77.e14. 10.1016/j.ajog.2020.12.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Yin K. (2020). Management of pregnant women infected with COVID-19. The Lancet Infectious Diseases, 20(5), 513–514. 10.1016/S1473-3099(20)30191-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majid U., Wasim A., Bakshi S., Truong J. (2020). Knowledge, (mis-)conceptions, risk perception, and behavior change during pandemics: A scoping review of 149 studies. Public Understanding of Science, 29(8), 777–799. 10.1177/0963662520963365 [DOI] [PubMed] [Google Scholar]
- Mehta S., Machado F., Kwizera A., Papazian L., Moss M., Azoulay É., Herridge M. (2021). COVID-19: A heavy toll on health-care workers. The Lancet Respiratory Medicine, 9(3), 226–228. 10.1016/S2213-2600(21)00068-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton S. M., Bandara D. K., Robinson E. M., Carr P. E. A. (2012). In the 21st century, what is an acceptable response rate? In: Wiley Online Library. [DOI] [PubMed] [Google Scholar]
- Olum R., Chekwech G., Wekha G., Nassozi D. R., Bongomin F. (2020). Coronavirus disease-2019: Knowledge, attitude, and practices of health care workers at Makerere University teaching hospitals, Uganda. Frontiers in Public Health, 8, 181. 10.3389/fpubh.2020.00181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ombere S. O. (2021). Access to maternal health services during the COVID-19 pandemic: Experiences of indigent mothers and health care providers in Kilifi county, Kenya. Frontiers in Sociology, 6, 613042. 10.3389/fsoc.2021.613042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onchonga D., Ngetich E., Makunda W., Wainaina P., Wangeshi D., Viktoria P. (2021). Anxiety and depression due to 2019 SARS-CoV-2 among frontier healthcare workers in Kenya. Heliyon, 7(3), e06351. 10.1016/j.heliyon.2021.e06351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallangyo E., Nakate M. G., Maina R., Fleming V. (2020). The impact of covid-19 on midwives’ practice in Kenya, Uganda and Tanzania: A reflective account. Midwifery, 89, 102775. 10.1016/j.midw.2020.102775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaci T., Barattucci M., Ledda C., Rapisarda V. (2020). Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability, 12(9), 3834. 10.3390/su12093834 [DOI] [Google Scholar]
- Rasmussen S. A., Kelley C. F., Horton J. P., Jamieson D. J. (2021). Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: What obstetricians need to know. Obstetrics and Gynecology, 137(3), 408–414. 10.1097/AOG.0000000000004290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberton T., Carter E. D., Chou V. B., Stegmuller A. R., Jackson B. D., Tam Y., Sawadogo-Lewis T., Walker N. (2020). Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study. The Lancet Global Health, 8(7), e901–e908. 10.1016/S2214-109X(20)30229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semaan, A., Audet, C., Huysmans, E., Afolabi, B., Assarag, B., Banke-Thomas, A., Blencowe, H., Caluwaerts, S., Campbell, O. M. R., Cavallaro, F. L., Chavane, L., Day, L. T., Delamou, A., Delvaux, T., Graham, W. J., Gon, G., Kascak, P., Matsui, M., Moxon, S., … Benova, L. (2020). Voices from the frontline: Findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Global Health, 5(6), e002967. 10.1136/bmjgh-2020-002967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaibu S., Kimani R. W., Shumba C., Maina R., Ndirangu E., Kambo I. (2021). Duty versus distributive justice during the COVID-19 pandemic. Nursing Ethics, 28(6), 1073–1080. 10.1177/0969733021996038. [DOI] [PubMed] [Google Scholar]
- Shikuku D. N., Nyaoke I. K., Nyaga L. N., Ameh C. A. (2021). Early indirect impact of COVID-19 pandemic on utilisation and outcomes of reproductive, maternal, newborn, child and adolescent health services in Kenya: A cross-sectional study. African Journal of Reproductive Health, 25(6), 76–87. 10.29063/ajrh2021/v25i6.9 [DOI] [PubMed] [Google Scholar]
- Shumba C., Maina R., Mbuthia G., Kimani R., Mbugua S., Shah S., Abubakar A., Luchters S., Shaibu S., Ndirangu E. (2020). Reorienting nurturing care for early childhood development during the COVID-19 pandemic in Kenya: A review. International Journal of Environmental Research and Public Health, 17(19), 7028. 10.3390/ijerph17197028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Population Fund. (2020). COVID-19 Technical Brief for Maternity Services. https://www.unfpa.org/sites/default/files/resource-pdf/COVID-19_Maternity_Services_TB_Package_UPDATE_2_14072020_SBZ.pdf
- World Health Organization. (2021a). COVID-19 Clinical management: living guidance, 25 January 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1
- World Health Organization. (2021b). COVID-19 Weekly Epidemiological Update. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---15-june-2021
- World Health Organization. (2021c). Definition and categorization of the timing of mother-to-child transmission of SARS-CoV-2: scientific brief, 8 February 2021 .
- Zambrano L. D., Ellington S., Strid P., Galang R. R., Oduyebo T., Tong V. T., Woodworth K. R., Nahabedian J. F., III, Azziz-Baumgartner E., Gilboa S. M. (2020). Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–October 3, 2020. Morbidity and Mortality Weekly Report, 69(44), 1641. 10.15585/mmwr.mm6944e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zenbaba D., Sahiledengle B., Bogale D. (2020). Practices of healthcare workers regarding infection prevention in bale zone hospitals, Southeast Ethiopia. Advances in Public Health, 2020, Art. no. 4198081, 7. 10.1155/2020/4198081 [DOI] [Google Scholar]
- Zhang M., Zhou M., Tang F., Wang Y., Nie H., Zhang L., You G. (2020). Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. Journal of Hospital Infection, 105(2), 183–187. 10.1016/j.jhin.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]