Abstract
Background
While socioeconomic status has been linked to hospital readmissions for several conditions, reliable measures of individual socioeconomic status are often not available. HOUSES, a new measure of individual socioeconomic status based upon objective public data about one's housing unit, is inversely associated with overall hospitalization rate but it has not been studied with respect to readmissions.
Purpose
To determine if patients in the lowest HOUSES quartile are more likely to be readmitted within 30 days (short-term) and 180 days (long-term).
Methods
A retrospective cohort study of 11 993 patients having 21 633 admissions was conducted using generalized linear mixed-effects models.
Results
HOUSES quartile did not show any significant association with early readmission. However, when compared to the lowest HOUSES quartile, the second quartile (OR = 0.90, 95%CI 0.83-0.98) and the third quartile (OR = 0.91, 95%CI 0.83-0.99) were associated with lower odds of late readmission while the highest quartile (OR = 0.91, 95%CI 0.82-1.01) was not statistically different.
Conclusion
HOUSES was associated with late readmission, but not early readmission. This may be because early readmissions are influenced by medical conditions and hospital care while late readmissions are influenced by ambulatory care and home-based factors. Since HOUSES relies on public county assessor data, it is generally available and may be used to focus interventions on those at highest risk for late readmission.
Keywords: managerial epidemiology, medical informatics, health outcomes, social determents of health, hospital readmission
Introduction
Hospital readmission within 30 days of dismissal remains a major issue in the United States healthcare system despite a recent downward trend. 1 Unplanned hospital readmissions have often been considered markers of potentially poor quality healthcare.2–5 Various strategies to reduce readmissions have been evaluated, including financial penalties, transitions of care programs, and prediction algorithms.6–8 However, to continue to reduce readmission rates, interventions targeting specific risk factors for readmission should be addressed. For example, socioeconomic status (SES) has been linked to readmission, especially in elderly patients and those hospitalized for cardiac conditions like heart failure, acute myocardial infarction, and valve surgery.9–12
At its core SES reflects a “differential access to desired resources”. 13 Those resources typically center around three themes: income & material goods, education & skills, or occupation & social relationships.13,14 Throughout history, including in ancient Greece, Egypt, and China, SES has been linked to health outcomes. 13 More recently, groups with lower SES had higher mortality and worse self-assessment of health in a 2008 study of 22 European countries, although the magnitude differed between countries. 15 SES affects one's health by impacting “health care, environmental exposures and health behavior”. 16
Much has been done to evaluate various measures of SES and their effect on readmission rates. A 2014 study evaluating readmission in a single hospital system for Medicare beneficiaries ages 65 years and older found that patients living in high poverty neighborhoods were 24% more likely to be readmitted within 30 days of discharge compared to patients not living in high poverty neighborhoods. 17 Low education and low income have been associated with increased readmission among patients with heart failure and community-acquired pneumonia. 18 In patients with decompensated cirrhosis, those from the three lowest income quartiles had significantly higher 30-day readmission rates compared to those in the highest quintile. 19 Finally, limited education was associated with increased sixty-day readmission rates among community dwelling Medicare beneficiaries. 20
Despite its importance, reliable individual-level SES data rarely exist in retrospective research datasets. 21 Self-reported income or education levels are subject to social desirability bias and reluctance to disclose.22,23 Individual SES within aggregated proxies such as census blocks or zip codes often varies widely, particularly in rural areas, and only results in correct quintile classification 29% of the time (an example of misclassification bias).24–26 Thus, to address readmission risk, better tools to assess SES are needed. To meet this need, an individual-level housing-based SES measure, termed HOUSES, was developed. HOUSES is based on the universal availability of objective and current real property data in nearly all United States counties via the county tax assessor's office and the premise that a person's housing situation is indicative of their family unit's access to resources. 27 The HOUSES index is conceptually associated with a person's wealth and income, control over life circumstances, and access to resources, 27 and logistically does not require contact with patients to measure their SES (eg, income or education). Instead, patients’ addresses which are always available in electronic health records, are linked to real property data from the county assessor's office enabling evaluation of their individual SES.
Patients in the lowest HOUSES quartile are more likely to be hospitalized, yet little is known about how HOUSES correlates with readmissions. 28 The aim of this study was to compare readmission rates between patients in the lowest HOUSES quartile to higher quartiles. We hypothesized that patients in the lowest HOUSES quartile were more likely to be readmitted both in the short-term (30 days) and long-term (180 days) even after controlling for other demographic and disease severity factors known to be associated with readmissions.
Methods
Study Setting and Population
A preexisting retrospective dataset consisting of all adult primary care hospitalizations at our institution from January 1, 2011 thru December 31, 2013 was available for use in this study. As described previously by Garrison et.al., all patients were local community members who had given consent for retrospective chart review research and had an identified primary care physician at one of five primary care clinical sites near Rochester, Minnesota. 29 Patients discharged from a psychiatric unit or labor and delivery were excluded. In addition, a small number of patients (441) enrolled in an intensive care transitions management program for frail high-risk seniors were excluded. The dataset contained 26 278 admissions to general medical, surgical, and intensive care services from 14 663 unique patients. Data regarding age, sex, race, marital status, address, prior hospitalizations and emergency department (ED) visits, length of stay, and the Charlson comorbidity index 30 were available.
HOUSES Score
Following Mayo Clinic Institutional Review Board approval, the above dataset was combined with an individual measure of SES termed HOUSES. Briefly, using principal component analysis, four attributes of real property data available at the county assessor's office (number of bedrooms, number of bathrooms, square footage of the unit, & estimated building value of the unit) were used to construct the HOUSES score. 27 The HOUSES score demonstrates criterion validity with education, income, Hollingshead Index (HS), and Nakao-Treas Index (NT) in Olmsted County, MN (R = 0.29-0.54, P < .001) and Jackson County, MO (R = 0.39-0.59, P < .001), respectively. 27 The HOUSES score also demonstrates construct validity by predicting (often better than other SES measures) a broad range of health outcomes which are known to be inversely associated with SES such as acute myocardial infarction, coronary artery disease, diabetes, rheumatoid arthritis, asthma, pneumococcal pneumonia, mood disorders, hypertension, transplantation failure, and overall mortality.28,31–37
The patient's current address at initial admission was used to formulate their HOUSES score. HOUSES scores are available for owner occupied properties as well as rental properties, including multi-unit dwellings which take into account each individual unit's characteristics and proportional valuation. The composite score is standardized by converting each attribute of a person's domicile to a z-score based upon all property data within the county for a given year and summing the four attributes. A higher HOUSES score indicates higher SES. Based upon prior experience with HOUSES data, the first quartile often has substantially different disease outcomes, thus we converted the HOUSES score to a quartile rank for analysis.28,37
Cohort
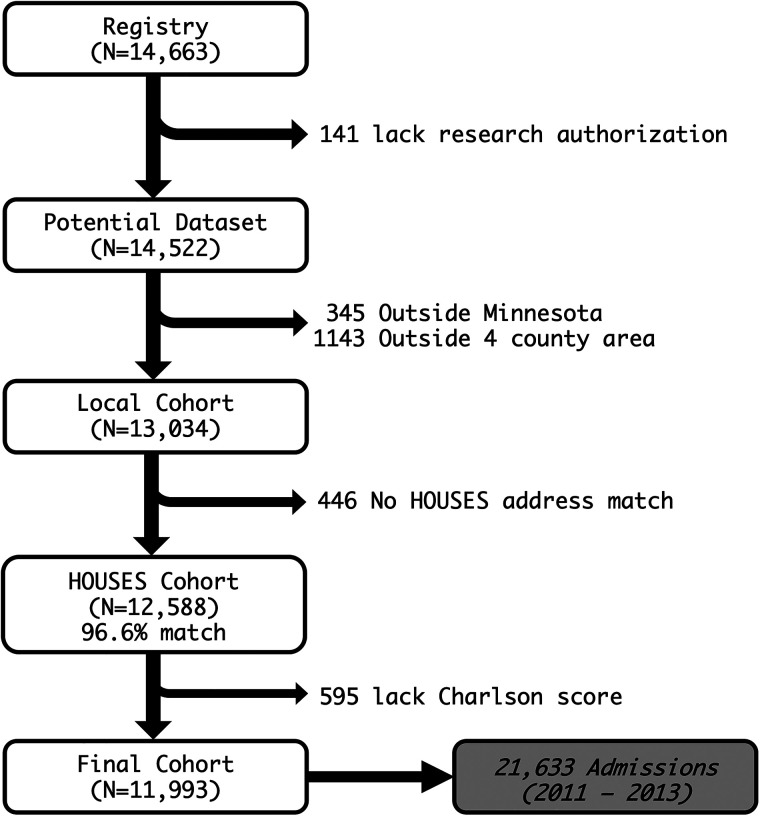
Starting with the 14 663 patients in the preexisting dataset, 141 patients who subsequently rescinded their research authorization were excluded. HOUSES data was only available in 2013 for four counties in southeast MN (Olmsted, Dodge, Goodhue, Wabasha), thus 1488 patients residing outside this four-county area were excluded. 96.6% (12 588) of the remaining patients were able to be matched with corresponding HOUSES data based upon their address at the time of admission. Finally, 595 patients who lacked sufficient recent ICD9/10 codes to calculate the Charlson Comorbidity data were excluded, leaving a final cohort of 11 993 patients having 21 633 admissions (Figure 1).
Figure 1.
Cohort development.
Analysis
Dichotomous dependent variables representing readmission or death within 30 (early) or 180 (late) days of hospital discharge were created. The 30-day period was chosen based on the Centers for Medicare and Medicaid Services (CMS) definition of hospital readmission and includes all-cause readmission to any facility within 30 days of initial dismissal. We used the same definition for late (180 day) readmissions by changing the timeframe. Deaths within the specified timeframes were included based upon common convention and the fact someone who dies cannot be readmitted, but may represent a similar failure mode to a readmission. 8 Despite methods to adjust for potentially avoidable readmissions, 38 we considered all readmissions whether planned or not to eliminate subjectivity, decrease complexity, and form an upper bound. Independent confounding variables previously associated with hospital readmission were selected including age, gender, marital status, Charlson Comorbidity score, prior hospitalizations and ED visits, and length of stay.8,20,29,39–48
The unit of analysis was hospital admission during the study period from 1/1/2011 to 12/31/2013. The analysis was not limited only to the initial hospitalization for each patient because readmission risk factors including age, marital status, SES, comorbidities and recent ED or prior hospitalizations often vary over time. Multiple admissions for a single patient were accounted for in the multivariate analysis.
Unadjusted bivariate statistics between the various independent variables including HOUSES and the dependent variable of readmission or death were computed. Wilcoxon rank sum or t-tests were used for continuous numeric data depending on normality. Chi-square or Fisher exact test (for 2 × 2 tables) were used for categorical data. P-values < .05 were considered significant.
A generalized linear mixed-effects model using a random effect intercept to control for repeated admissions on the same patient was used to determine the adjusted odds of early (30 day) and late (180 day) readmission or death versus HOUSES quartile. HOUSES Q1, the poorest quartile, was used as the reference category because it tends to be distinct from Q2, Q3, and Q4 in terms of outcomes.49,50 Because the number of previous hospitalizations in 12 months and the number of previous ED visits over 6 months are highly correlated in our data (Pearson Correlation Coefficient = 0.66), we chose to include only previous hospitalizations in our multivariate analysis to eliminate issues with multicollinearity. 51 95% Confidence Intervals which did not cross unity were considered significant (Pr(>|z|) < 0.05). R version 3.6.1 (http://www.r-project.org/) was used for the analysis.
Results
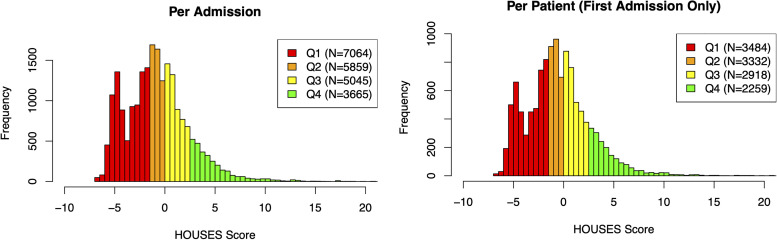
In the dataset of 11 993 patients with 21 633 hospital admissions, there were 3923 (18.1%) readmissions or deaths within 30 days of hospital dismissal. The top 5 dismissing services were General Medicine (5697), followed by Cardiology (2724), Family Medicine (2214), Orthopedic Surgery (2207), and Trauma/Surgery (1407). The overall mean HOUSES score for the dataset was −0.74 (median = −0.98), with the observed HOUSES quartile counts for all admissions being skewed lower as well (see Figure 2).
Figure 2.
Histogram of HOUSES scores.
Table 1 shows the unadjusted bivariate comparison of various factors versus the dependent variable of early hospital readmission or death. Because factors known to be associated with hospital readmission were chosen, all were significant. Patients who were readmitted or died within 30 days of hospital dismissal were older (62.5 vs 63.6 yrs), more likely to be male (46.3% vs 49.6%), more likely to be unmarried (41.4% vs 46.0%), had a higher Charlson comorbidity score (3.0 vs 6.0), had longer hospital stays (2.5 vs 3.3 days), had more ED visits within the previous 6 months (1.0 vs 2.0), and had more hospitalizations within the previous 12 months (0 vs 1.0). Their HOUSES score was lower (−0.94 vs. −0.70, P < .001) and those in the lowest HOUSES quartile had more early readmissions or death than those in the other quartiles (20.0% vs 17.3%, P < .001).
Table 1.
Bivariate Analysis of Factors Associated with 30d Readmission.
| Variable | Not readmitted (N = 17 710) | Readmitted (N = 3923) | P-Value |
|---|---|---|---|
| Age, mean (SD) | 62.5 (19.3) | 63.6 (19.5) | P = .001 |
| Gender, F (%) | 9518 (53.7%) | 1976 (50.4%) | P < .001 |
| Marital status, not married # (%) | 7338 (41.4%) | 1804 (46.0%) | P < .001 |
| Charlson Comorbidity Score, median (SD) | 3.0 (3.8) | 6.0 (3.9) | P < .001 |
| LOS, median (SD) | 2.5 (4.3) | 3.3 (5.4) | P < .001 |
| ED Visits 6mo, median (SD) | 1.0 (2.9) | 2.0 (5.0) | P < .001 |
| Hospitalizations 12mo, median (SD) | 0.0 (1.6) | 1.0 (3.0) | P < .001 |
| HOUSES score, mean (SD) | −0.70 (3.2) | −0.94 (3.3) | P < .001 |
| HOUSES Quartile | P < .001 | ||
| Q1 # (%) | 5655 (80.05%) | 1409 (19.95%) | |
| Q234 # (%) | 12 055 (82.74%) | 2514 (17.26%) | |
| HOUSES Quartile | P < .001 | ||
| Q1 # (%) | 5655 (80.05%) | 1409 (19.95%) | |
| Q2 # (%) | 4848 (82.74%) | 1011 (17.26%) | |
| Q3 # (%) | 4145 (82.16%) | 900 (17.84%) | |
| Q4 # (%) | 3062 (83.55%) | 603 (16.45%) |
The same held true for late hospital readmission or death within 180 days of hospital dismissal (Table 2). The HOUSES score was lower (−1.21 vs. −0.57, P < .001) and those in the lowest HOUSES quartile had more late readmissions or death than those in other quartiles (43.3% vs 35.8%, P < .001).
Table 2.
Bivariate Analysis of Factors Associated with 180d Readmission.
| Variable | Not readmitted (N = 13 360) | Readmitted (N = 8273) | P-value |
|---|---|---|---|
| Age, mean (SD) | 61.2 (19.2) | 65.1 (19.2) | P < .001 |
| Gender, F #,(%) | 7231 (54.1%) | 4263 (51.5%) | P < .001 |
| Marital Status, Not Married #,(%) | 5290 (39.6%) | 3852 (46.6%) | P < .001 |
| Charlson Comorbidity Score, median (SD) | 3.0 (3.5) | 6.0 (4.0) | P < .001 |
| LOS, median (SD) | 2.3 (3.7) | 3.1 (5.5) | P < .001 |
| ED Visits 6mo, median (SD) | 1.0 (2.2) | 2.0 (4.5) | P < .001 |
| Hospitalizations 12mo, median (SD) | 0.0 (1.1) | 1.0 (2.7) | P < .001 |
| HOUSES Score, mean (SD) | −0.6 (3.2) | −1.0 (3.3) | P < .001 |
| HOUSES Q1 versus Q234, Q1 #,(%) | 4002 (30.0%) | 3062 (37.0%) | P < .001 |
| HOUSES Quartile | P < .001 | ||
| 1 #,(%) | 4002 (56.65%) | 3062 (43.35%) | |
| 2 #,(%) | 3719 (63.47%) | 2140 (36.53%) | |
| 3 #,(%) | 3209 (63.61%) | 1836 (36.39%) | |
| 4 #,(%) | 2430 (66.30%) | 1235 (33.70%) |
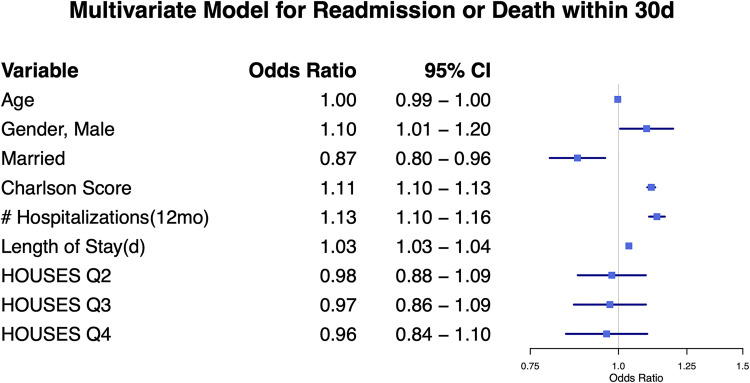
The generalized linear mixed effects model for early readmission or death did not show any significant association with HOUSES quartile (Figure 3). Being married was protective (OR = 0.87, 95%CI 0.80-0.96), while males (OR = 1.10, 95%CI 1.01-1.20) and those with more comorbidities (per Charlson score) (OR = 1.11, 95%CI 1.10-1.13), longer hospital stays (per day) (OR = 1.03, 95%CI 1.03-1.04), and more previous hospitalizations (per number of hospitalizations) (OR = 1.13, 95%CI 1.10-1.16) were more likely to be readmitted or die within 30 days.
Figure 3.
Multivariate model for readmission or death within 30 days.
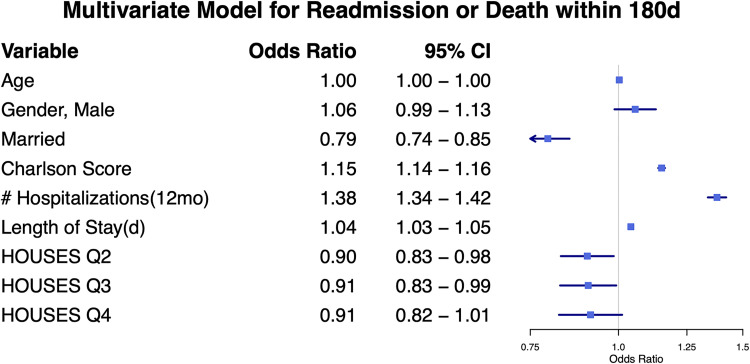
HOUSES quartile was associated with late readmission or death in the generalized linear mixed effects model. When compared to the lowest HOUSES quartile, the second quartile (OR = 0.90, 95%CI 0.83-0.98) and the third quartile (OR = 0.91, 95%CI 0.83-0.99) were associated with significantly lower odds of readmission or death within 180 days of hospital dismissal while the highest quartile (OR = 0.91, 95%CI 0.82-1.01) was not statistically different (see Figure 4). Other factors such as male gender, unmarried status, Charlson comorbidity index, previous hospitalizations, and length of stay were all associated with increased odds of late readmission or death.
Figure 4.
Multivariate model for readmission or death within 180 days.
Discussion
While our hypothesis that HOUSES quartile was associated with early readmission or death following hospital dismissal proved incorrect, HOUSES was associated with late (within 180 days) readmission or death. We believe this difference in association is best explained by the fact that early readmissions are influenced more by medical conditions and hospital care whereas ambulatory care and home-based factors play a larger role in late readmissions.52,53 In the unadjusted analysis of early readmission or death, a lower HOUSES score was associated with readmission or death. However, once demographic (gender, marital status), medical (comorbidities, length of stay), and utilization (number of prior hospitalizations) factors were adjusted for, the socioeconomic (HOUSES) factor was no longer significant. For late readmissions or death, all these factors remained significant.
While late readmissions or death in HOUSES Q2 and Q3 compared to Q1 were significant, HOUSES Q4 was not statistically significant. It had a similar odds ratio (0.9) but a slightly wider 95% confidence interval that barely crossed unity (see Figure 4). This could be a type II statistical error caused by the wider 95% confidence interval resulting from fewer admissions among the highest HOUSES quartile (3665-Q4 vs 5859-Q2 or 5045-Q3, P < .001).
We found our hospitalized patients’ HOUSES scores were skewed lower than the county's general population, consistent with Takahashi, et al's findings that the lowest HOUSES quartile was associated with a higher likelihood of hospitalization. 28 This contributed to the lower proportion and smaller sample size in HOUSES Q4.
The odds of late readmission or death are approximately 10% lower (OR∼0.9) for those with higher SES (Q2, Q3, or Q4 HOUSES) when compared to the lowest quartile SES (Q1 HOUSES) even after adjusting for other demographic, medical, and utilization factors known to affect readmissions. To put this into perspective, having a myocardial infarction, congestive heart failure, stroke, chronic obstructive pulmonary disease, or uncomplicated diabetes mellitus adds a point to the Charlson Comorbidity Index which according to this model and other readmission research, also adds approximately 10-15% (OR∼1.10-1.15/pt) to the odds of readmission. 29 As further evidence of the equivalent risk, a 2017 meta-analysis showed that low SES has a comparable impact on life expectancy as known major health risk factors such as tobacco use, alcohol consumption, insufficient physical activity, raised blood pressure, obesity, and diabetes. 54 The authors called for SES to be considered a modifiable health risk factor so that interventions could be developed to improve health and mortality outcomes. 54
This study used HOUSES, an improved measure of individual SES, to help identify readmission risk. While community level SES indices are widely available from governmental agencies such as the US Census Bureau; they suffer from lack of granularity, wide variations of individual SES within the aggregated data, and poor classification accuracy for individuals.24–26,55 On the other hand, individual SES indices are traditionally more difficult to obtain and potentially biased because they rely on self-report of private data. HOUSES avoids some of these downfalls because it relies on the subject's address and the county assessors public housing data, both of which are generally available.
Although SES has often been thought of as relatively static; targeted interventions to address SES inequities have been found to be beneficial especially when interventions are implemented early in life. 56 More research is needed to determine if health advocacy addressing SES inequities can alter readmission risk in selected populations once they are hospitalized. In any case, our results suggest that hospital and local community health officials could utilize HOUSES data within existing hospital-to-home transition programs to identify patients whose lower SES places them at higher risk of readmission over the following 6 months.
Limitations
Our study was performed at a single institution and within a region that is primarily Caucasian with slightly higher income and education level than the national population. 57 However the HOUSES score has been validated in other populations. 27 Further study in other regions could improve the generalizability of our findings. We were only able to search for hospitalizations within our institution, thus it is possible a small number of readmissions were missed. However, all patients were local and had primary care physicians at our institution. In our experience, these patients rarely seek care outside our institution due to continuity and insurance reasons.8,29,58
Conclusion
Patients with lower SES as indicated by the lowest quartile of HOUSES are more likely to experience late readmission or death following hospitalization than those in higher HOUSES quartiles when other demographic, medical, and utilization factors associated with readmission are considered. However, SES seems to play less of a role in early readmissions where demographic, medical, and utilization factors predominate. This information could be incorporated into existing hospital-to-home transition programs to identify patients whose lower SES places them at greater risk of readmission over the next six months.
Acknowledgments
None.
Author Biographies
Kaitlyn I. Zurek completed her residency in Family Medicine and a Hospital Medicine Fellowship at the Mayo Clinic in Rochester, MN. She is now practicing with Ascension Genesys Hospital in Grand Blanc, MI.
Christopher L. Boswell is a core faculty member of the Mayo Clinic Family Medicine Residency Program – Rochester. He is also the medical director for Family Medicine Inpatient services.
Nathanial E. Miller is a core faculty member of the Mayo Clinic Family Medicine Residency Program – Rochester. He is the medical director for the Kasson-Mayo Family Medicine Clinic.
Jennifer L. Pecina is a practicing family physician in the Department of Family Medicine, Mayo Clinic, Rochester, MN. She is also an accomplished researcher with numerous publications covering various aspects of family medicine.
Matthew D. Decker is a current resident at the Mayo Clinic Family Medicine Residency Program – Rochester. He will attend a Hospital Medicine Fellowship at Mayo Clinic following graduation.
Chung I. Wi is a co-developer of the HOUSES index and currently works for the Department of Pediatric and Adolescent Medicine, Precision Population Science Lab, Mayo Clinic, Rochester, MN.
Gregory M. Garrison is an Associate Professor of Family Medicine at Mayo Clinic. He is Vice Chair of Education for the Mayo Clinic Department of Family Medicine–Midwest. He has practiced family medicine for over 20 years and is currently a core faculty member of the Mayo Clinic Family Medicine Residency in Rochester, MN where he enjoys mentoring the next generation of family physicians. He earned his medical degree at the University of Minnesota and completed a residency in Family Medicine at Mayo Clinic and a fellowship in Medical Informatics at Stanford University. He holds a master’s degree in Medical Informatics and is also board certified in Clinical Informatics. His research interests focus on how organized primary care can improve patient outcomes such as chronic disease management, preventive care, and hospitalizations.
Footnotes
Authors Contributions: KZ: Study design, data analysis, interpretation, manuscript; CLB: Interpretation, manuscript; NM: Interpretation, manuscript; JP: Study design, data collection, manuscript; MD: Interpretation, manuscript; CW: Data collection, manuscript; GMG: Study design, data collection & analysis, interpretation, manuscript. All authors have read and approve of the manuscript.
Ethics Approval: This retrospective study was reviewed and approved by the Mayo Clinic Institutional Review Board (IRB #13-004434). A waiver of informed consent was granted because the work presented minimal risk, involved retrospective review of information already included in the medical record, and all subjects had previously granted permission to use their medical records for research purposes.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Center for Advancing Translational Sciences, (grant number UL1TR002377).
ORCID iD: Gregory M. Garrison https://orcid.org/0000-0001-6903-4610
References
- 1.Bailey M, Weiss A, Barrett M, Jiang H. Characteristics of 30-Day Readmissions, 2010-2016. Vol HCUP Statistical Brief #248. Rockville, MD: Agency for Healthcare Research and Quality; 2019. [PubMed] [Google Scholar]
- 2.Ashton CM, Kuykendall DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Ann Intern Med. 1995;122(6):415-421. [DOI] [PubMed] [Google Scholar]
- 3.Halfon P, Eggli Y, Pretre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44(11):972-981. [DOI] [PubMed] [Google Scholar]
- 4.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822-1828. [DOI] [PubMed] [Google Scholar]
- 5.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228-1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543-1551. [DOI] [PubMed] [Google Scholar]
- 7.Goncalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst Rev. 2016;2016(1):CD000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garrison GM, Robelia PM, Pecina JL, Dawson NL. Comparing performance of 30-day readmission risk classifiers among hospitalized primary care patients. J Eval Clin Pract. 2017;23(3):524-529. [DOI] [PubMed] [Google Scholar]
- 9.Feng TR, Hoyler MM, Ma X, Rong LQ, White RS. Insurance status and socioeconomic markers affect readmission rates after cardiac valve surgery. J Cardiothorac Vasc Anesth. 2020;34(3):668-678. [DOI] [PubMed] [Google Scholar]
- 10.Shebehe J, Hansson A. High hospital readmission rates for patients aged >/=65 years associated with low socioeconomic status in a Swedish region: a cross-sectional study in primary care. Scand J Prim Health Care. 2018;36(3):300-307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroch E, Duan M, Martin J, Bankowitz RA. Patient factors predictive of hospital readmissions within 30 days. J Healthc Qual. 2016;38(2):106-115. [DOI] [PubMed] [Google Scholar]
- 12.Damiani G, Salvatori E, Silvestrini G, et al. Influence of socioeconomic factors on hospital readmissions for heart failure and acute myocardial infarction in patients 65 years and older: evidence from a systematic review. Clin Interv Aging. 2015;10:237-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56(4):769-784. [DOI] [PubMed] [Google Scholar]
- 14.Baker EH. Socioeconomic status, definition. The Wiley Blackwell Encyclopedia of health, illness, behavior, and society. 2014:2210-2214.
- 15.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468-2481. [DOI] [PubMed] [Google Scholar]
- 16.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood). 2002;21(2):60-76. [DOI] [PubMed] [Google Scholar]
- 17.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence from an urban teaching hospital. Health Aff (Millwood). 2014;33(5):778-785. [DOI] [PubMed] [Google Scholar]
- 18.Calvillo-King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brahmania M, Wiskar K, Walley KR, Celi LA, Rush B. Lower household income is associated with an increased risk of hospital readmission in patients with decompensated cirrhosis. J Gastroenterol Hepatol. 2021;36(4):1088-1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling medicare beneficiaries. Gerontologist. 2008;48(4):495-504. [DOI] [PubMed] [Google Scholar]
- 21.Tourangeau R, Yan T. Sensitive questions in surveys. Psychol Bull. 2007;133(5):859-883. [DOI] [PubMed] [Google Scholar]
- 22.Nederhof AJ. Methods of coping with social desirability bias: a review. Eur J Soc Psychol. 1985;15(3):263-280. [Google Scholar]
- 23.Turrell G. Income non-reporting: implications for health inequalities research. J Epidemiol Community Health. 2000;54(3):207-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xie S, Hubbard RA, Himes BE. Neighborhood-level measures of socioeconomic status are more correlated with individual-level measures in urban areas compared with less urban areas. Ann Epidemiol. 2020;43:37-43.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Demissie K, Hanley JA, Menzies D, Joseph L, Ernst P. Agreement in measuring socio-economic status: area-based versus individual measures. Chronic Dis Can. 2000;21(1):1-7. [PubMed] [Google Scholar]
- 26.Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census-defined geographic areas--the public health disparities geocoding project. Am J Public Health. 2002;92(7):1100-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Juhn YJ, Beebe TJ, Finnie DM, et al. Development and initial testing of a new socioeconomic status measure based on housing data. J Urban Health. 2011;88(5):933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takahashi PY, Ryu E, Hathcock MA, et al. A novel housing-based socioeconomic measure predicts hospitalisation and multiple chronic conditions in a community population. J Epidemiol Community Health. 2016;70(3):286-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garrison GM, Keuseman R, Bania B, Robelia P, Pecina J. Visit entropy associated with hospital readmission rates. J Am Board Fam Med. 2017;30(1):63-70. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. [DOI] [PubMed] [Google Scholar]
- 31.Bang DW, Manemann SM, Gerber Y, et al. A novel socioeconomic measure using individual housing data in cardiovascular outcome research. Int J Environ Res Public Health. 2014;11(11):11597-11615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ghawi H, Crowson CS, Rand-Weaver J, Krusemark E, Gabriel SE, Juhn YJ. A novel measure of socioeconomic status using individual housing data to assess the association of SES with rheumatoid arthritis and its mortality: a population-based case-control study. BMJ open. 2015;5(4):e006469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wi CI, St Sauver JL, Jacobson DJ, et al. Ethnicity, socioeconomic status, and health disparities in a mixed rural-urban US community-Olmsted county, Minnesota. Mayo Clin Proc. 2016;91(5):612-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stevens MA, Beebe TJ, Wi CI, Taler SJ, St Sauver JL, Juhn YJ. HOUSES index as an innovative socioeconomic measure predicts graft failure among kidney transplant recipients. Transplantation. 2020;104(11):2383-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harris MN, Lundien MC, Finnie DM, et al. Application of a novel socioeconomic measure using individual housing data in asthma research: an exploratory study. NPJ Prim Care Respir Med. 2014;24(1):14018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Johnson MD, Urm SH, Jung JA, et al. Housing data-based socioeconomic index and risk of invasive pneumococcal disease: an exploratory study. Epidemiol Infect. 2013;141(4):880-887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Greenwood J, Zurek KI, Grimm JM, Wi CI, Vogel JT, Garrison GM. Association of a housing based individual socioeconomic status measure with diabetic control in primary care practices. Prim Care Diabetes. 2022;16(1):78–83. [DOI] [PubMed] [Google Scholar]
- 38.Halfon P, Eggli Y, van Melle G, Chevalier J, Wasserfallen JB, Burnand B. Measuring potentially avoidable hospital readmissions. J Clin Epidemiol. 2002;55(6):573-587. [DOI] [PubMed] [Google Scholar]
- 39.Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. J Am Board Fam Med. 2013;26(1):71-77. [DOI] [PubMed] [Google Scholar]
- 40.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428. [DOI] [PubMed] [Google Scholar]
- 41.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107(1):13-17. [DOI] [PubMed] [Google Scholar]
- 42.Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients >/=65 years of age. Proc (Bayl Univ Med Cent). 2008;21(4):363-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25(3):211-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Billings J, Blunt I, Steventon A, Georghiou T, Lewis G, Bardsley M. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). BMJ open. 2012;2(4):e001667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shulan M, Gao K, Moore CD. Predicting 30-day all-cause hospital readmissions. Health Care Manag Sci. 2013;16(2):167-175. [DOI] [PubMed] [Google Scholar]
- 46.Shadmi E, Flaks-Manov N, Hoshen M, Goldman O, Bitterman H, Balicer RD. Predicting 30-day readmissions with preadmission electronic health record data. Med Care. 2015;53(3):283-289. [DOI] [PubMed] [Google Scholar]
- 47.van Walraven C, Dhalla IA, Bell C, et al. Derivation and validation of an index to predict early death or unplanned readmission after discharge from hospital to the community. Cmaj. 2010;182(6):551-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Walraven C, Wong J, Forster AJ. LACE+ index: extension of a validated index to predict early death or urgent readmission after hospital discharge using administrative data. Open Med. 2012;6(3):e80-e90. [PMC free article] [PubMed] [Google Scholar]
- 49.Greenwood J, Zurek KI, Grimm JM, Wi CI, Vogel JT, Garrison GM. Association of a housing based individual socioeconomic status measure with diabetic control in primary care practices. Prim Care Diabetes. 2022;16(1):78-83. [DOI] [PubMed] [Google Scholar]
- 50.Angstman KB, Wi CI, Williams MD, Bohn BA, Garrison GM. Impact of socioeconomic status on depression clinical outcomes at six months in a Midwestern, United States community. J Affect Disord. 2021;292:751-756. [DOI] [PubMed] [Google Scholar]
- 51.Vatcheva KP, Lee M, McCormick JB, Rahbar MH. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiology (Sunnyvale). 2016;6(2):227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Graham KL, Auerbach AD, Schnipper JL, et al. Preventability of early versus late hospital readmissions in a national cohort of general medicine patients. Ann Intern Med. 2018;168(11):766-774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Herges JR, Borah BJ, Moriarty JP, Garrison GM, Gullerud RE, Angstman KB. Impact of collaborative clinician visits on postdischarge total cost of care in a polypharmacy population. Am J Health Syst Pharm. 2020;77(22):1859-1865. [DOI] [PubMed] [Google Scholar]
- 54.Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status and the 25 x 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet. 2017;389(10075):1229-1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maroko AR, Doan TM, Arno PS, Hubel M, Yi S, Viola D. Integrating social determinants of health with treatment and prevention: a new tool to assess local area deprivation. Prev Chronic Dis. 2016;13:E128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Heckman JJ, Raut LK. Intergenerational long-term effects of preschool - structural estimates from a discrete dynamic programming model. J Econom. 2016;191(1):164-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.QuickFacts. US Census Bureau. 2021. Accessed April 30, 2021. https://www.census.gov/quickfacts/fact/table/MN,dodgecountyminnesota,olmstedcountyminnesota,US/PST045219
- 58.Garrison GM, Keuseman RL, Boswell CL, Horn JL, Nielsen NT, Nielsen ML. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019;10:2150132719840517. [DOI] [PMC free article] [PubMed] [Google Scholar]