In 1959, an article entitled “An Anaphylactoid Reaction to Vancomycin” hypothesized that vancomycin-induced histamine release from mast cells had clinical manifestations similar to those of anaphylaxis but less severe. The author named this reaction “Red Man Syndrome,” reflecting the diffuse erythema in affected patients, and the term caught on in 1985, when the Journal published a letter entitled “Vancomycin and the Red Man’s Syndrome.”1 Although “red man” might, at first glance, be taken as a straightforward description of a white male patient with an erythematous skin reaction, the term “Red Man” had a ready referent outside medicine, where it had long carried racist connotations.
Like “redskin,” “Red Man” calls up historical narratives that endorse and reinforce discrimination against Native American and Indigenous peoples. Such narratives were deeply embedded in popular culture: L. Frank Baum, the author of the Wizard of Oz, for example, wrote after the massacre at Wounded Knee, “With his fall the nobility of the Redskin is extinguished, and what few are left are a pack of whining curs who lick the hand that smites them.” The song “What Makes the Red Man Red” in the Walt Disney movie of Peter Pan depicts Native Americans as animals.2 Citing this history, some observers have called for replacing the trauma-invoking term,1 yet “Red Man Syndrome” continues to be used by clinicians worldwide.
Current use of this term causes inequities beyond its original racist implications: by implying a white male reference, it perpetuates biases and racial norms that may undermine prompt and equitable diagnoses and treatment. Furthermore, its use as a clinical descriptor supports race-based medicine, the “system by which research characterizing race as an essential, biological variable, translates into clinical practice, leading to inequitable care.”3 And it perpetuates the underrecognition of skin findings in diverse patient populations. We believe it’s time to rename this reaction and pursue systemwide improvements in drug-allergy recognition and documentation that are responsive to diverse patient populations.
Because of the increased prevalence of methicillin-resistant Staphylococcus aureus, vancomycin is now the most commonly used antibiotic in U.S. hospitals, and without a specific infusion protocol, as many as half of patients who receive it experience symptoms consistent with “Red Man Syndrome.”4 Although it’s a common reaction documented in electronic health records (EHRs), it is not documented uniformly across patients. In a 2012 retrospective study, White patients were deemed more likely to experience “Red Man Syndrome” than non-White patients (odds ratio [OR], 12.5; 95% confidence interval [CI], 1.7 to 90.1).5 The investigators inferred that Black race was protective against this reaction — a race-based conclusion suggesting that Black patients have different biologic mast-cell responses to vancomycin. The authors failed to consider other potential mechanisms of under-documentation of “Red Man Syndrome” in non-White patients.
Recently, we reported findings from a cross-sectional study of patients with a vancomycin allergy documented between 2017 and 2019 in two U.S. health care systems. Because “Red Man Syndrome” is not a coded reaction entry in EHRs, we used natural language processing to identify its documentation in all its varied free-text permutations. We found that the syndrome was one of the most commonly documented reactions to vancomycin, accounting for 16% of reactions with classically “allergic” symptoms. However, among patients with reactions possibly representing the syndrome (some combination of rash, flushing, itching, and hives), “Red Man Syndrome” was more likely to be specified in documentation for male than for female patients (OR, 1.30; 95% CI, 1.17 to 1.44) and less likely for Black than for White patients (OR, 0.59; 95% CI, 0.47 to 0.75).4 This slanted application of the term may be attributable to cognitive or implicit biases.
Gender- and race-related bias is problematic for clinical care. The more detailed the drug-allergy documentation in the EHR, the higher the likelihood that a specific drug will be used — or not used — appropriately in the future.4 Incomplete documentation can lead to avoidance or to use of alternative agents, which may adversely affect the quality and cost of care.4 In this case, documented “Red Man Syndrome” tells future clinicians that vancomycin is reasonably safe for readministration, as long as the infusion rate is reduced or the patient is pretreated with an antihistamine (or both). Therefore, any patient with documented “Red Man Syndrome” would probably be retreated with vancomycin if necessary. But patients with documented vancomycin reactions not specified as “Red Man Syndrome” would probably be perceived as truly allergic, warranting strict avoidance of vancomycin.
It seems likely that the documentation differences we observed affect the timing and choice of the antibiotic administered. For example, a White man with documented “Red Man Syndrome” might well receive vancomycin again, whereas a Black or female patient with a similar reaction not labeled “Red Man Syndrome” would probably receive delayed antibiotic treatment with an alternative drug. Since drug allergies are rarely removed from a patient’s EHR,4 a vancomycin allergy is likely to affect a lifetime of clinical decisions.
It is time to rename this reaction using a gender- and race-conscious approach that reinforces, rather than undermines, equitable care delivery. We can move beyond “Red Man Syndrome” just as we have changed problematic eponyms to avoid Nazi associations or confronted race “corrections” in clinical practice.3 This renaming, however, will require substantial work affecting clinical practice, education, and research. We propose the following steps.
First, physicians can stop teaching “Red Man Syndrome” and stop using it in clinical practice. All language used in clinical medicine should be scrutinized for potential harmful effects. The term “Red Man Syndrome” causes harm, which should be enough reason to stop using it. But there is an additional reason: it is not clinically useful because it centers on manifestations in white male patients without considering patients’ diversity. Instead, we recommend using the term “infusion reaction” for all non–immune-mediated drug reactions; these reactions are typically infusion-rate–dependent and can be prevented with rate changes, premedication (e.g., with antihistamines), or both. This change will also facilitate drug-allergy documentation for other drugs that cause infusion reactions.4 “Infusion reaction” should be coded in commercial EHRs to facilitate this change.
Second, we can combat cognitive bias by representing cutaneous findings from drug allergies in diverse patients. Such findings may present differently in patients of different ages, sexes, and races (see images). Clinicians should recognize that vancomycin infusion reaction may present with diffuse erythema, warmth without erythema, isolated palmar erythema, pruritus, urticaria, or in its severe form, symptoms indistinguishable from anaphylaxis. Availability of more diverse images of dermatologic findings can mitigate cognitive biases, such as prototype bias, which leads clinicians to estimate disease probability on the basis of the presentation’s alignment with known prototypes.
Dermatologic Findings in Patients Varying in Age, Sex, and Skin Color.
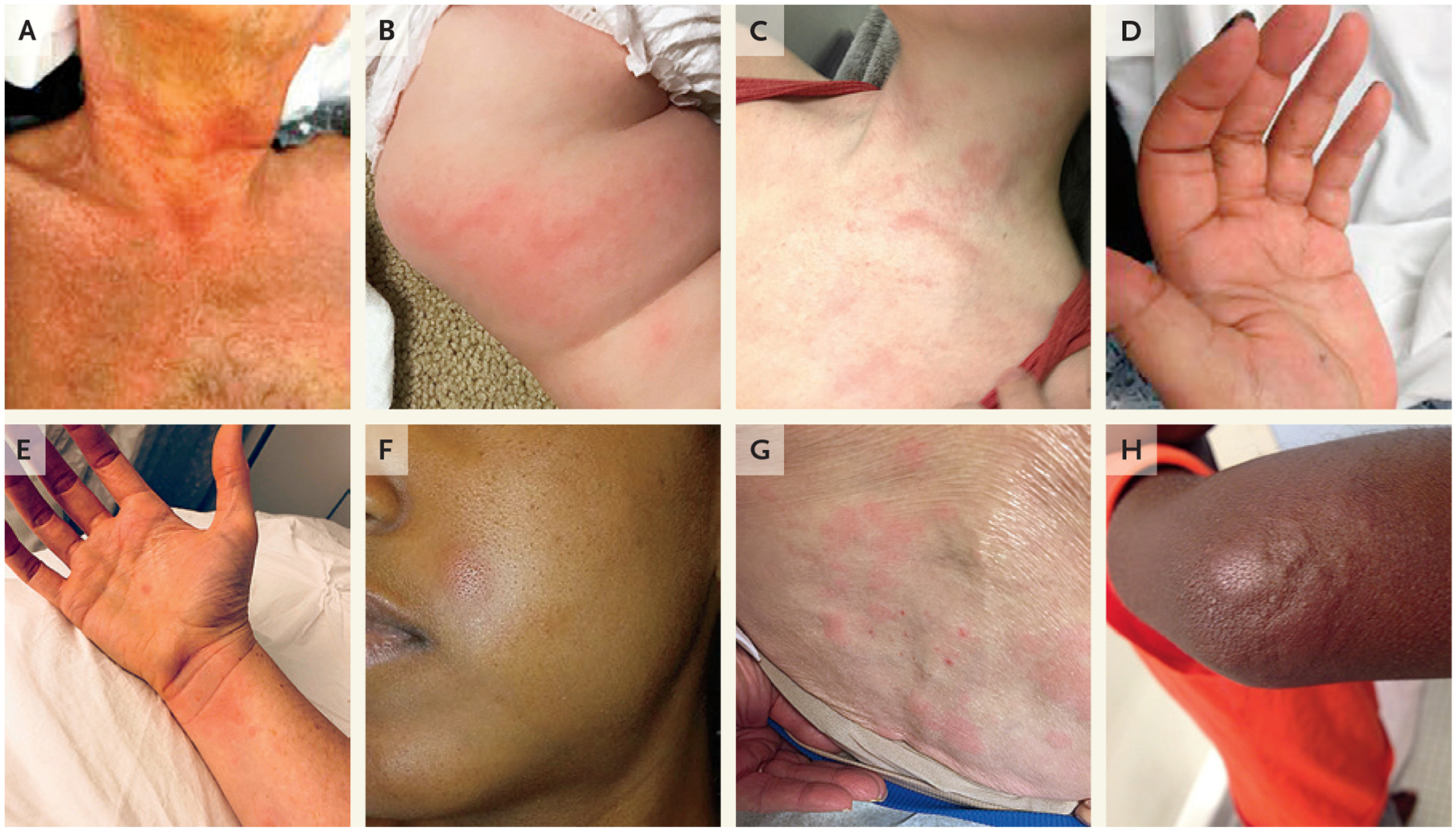
The immediate reaction to drugs, including the vancomycin infusion reaction, can present as erythema that can be confluent or blotchy, typically involving the head and neck but also the trunk, extremities, and palms or soles (Panels A through D) or urticaria that can be localized or diffuse (Panels E through H).
Third, we can institute multidisciplinary training on best practices for drug-allergy documentation. EHR documentation of drug allergies has deficiencies that extend beyond vancomycin infusion reactions. Despite the importance of such documentation to the quality and safety of care, few clinicians receive training in this area. The minimum useful information in a drug-allergy EHR entry is the drug and the reaction; additional details that could improve subsequent care include date, severity, clinical context, and treatment details. Since myriad health care professionals enter drug allergies in the EHR, training should occur across disciplines.
Fourth, including experts such as allergy specialists in our quality and safety infrastructure and on multidisciplinary antimicrobial stewardship teams can help improve antibiotic-allergy documentation, clarify drug-allergy diagnoses, and optimize antibiotic choices. Pharmacists, particularly those focused on antibiotic stewardship, also represent an invaluable resource for improving antibiotic-allergy documentation.
Finally, race-based reporting of clinical research examining racial differences needs to be challenged. Researchers should acknowledge that race is a social construct and explore how racism, rather than race, contributes to racial inequities.1 It was not that Black patients had different biologic mast-cell responses to vancomycin, but rather that their vancomycin infusion reaction was not identified or not documented.
Implementing these recommendations would mean not only striking racist terminology from our professional vocabulary, but also improving the diagnosis and documentation of all allergic drug reactions for greater clinical precision and patient safety. It would move us one step closer to a safe, just, and equitable health care system.
Footnotes
References
- 1.Austin JP, Foster BA, Empey A. Replace red man syndrome with vancomycin flushing reaction. Hosp Pediatr 2020; 10:623–4. [DOI] [PubMed] [Google Scholar]
- 2.Brave Heart MY, DeBruyn LM. The American Indian Holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res 1998; 8:56–78. [PubMed] [Google Scholar]
- 3.Cerdeña JP, Plaisime MV, Tsai J. From race-based to race-conscious medicine: how anti-racist uprisings call us to act. Lancet 2020; 396:1125–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alvarez-Arango S, Yerneni S, Tang O, et al. Vancomycin hypersensitivity reactions documented in electronic health records. J Allergy Clin Immunol Pract 2020. October 1 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myers AL, Gaedigk A, Dai H, James LP, Jones BL, Neville KA. Defining risk factors for red man syndrome in children and adults. Pediatr Infect Dis J 2012; 31:464–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


