Abstract
Introduction
Medicinal cannabis is prescribed in Australia for patients with chronic refractory pain conditions. However, measures of safety and effectiveness of different cannabinoids are lacking. We designed an observational study to capture effectiveness, adverse events (AEs), and health-related quality of life (HRQoL) measures in patients prescribed an oral medicinal cannabis formulation at Cannabis Access Clinics through the Cannabis Access Clinics Observational study (CACOS).
Objectives
We aimed to evaluate effectiveness, reported AEs, and change in patient-reported outcomes in individuals prescribed a cannabinoid oil formulation for management of chronic pain.
Methods
A cross-sectional analysis was conducted on patients prescribed an oil formulation of Δ9-tetrahydrocannabinol and cannabidiol for pain symptoms of at least 3-month duration. Clinician-reported AEs were organized by system, organ, class, and frequency. Analysis of patient-reported responses to a questionnaire was conducted using published minimal clinically important differences to determine meaningful change in HRQoL over time.
Results
More than half (n = 91/151, 60.3%) of the participants experienced at least one AE during the observation period (mean 133 ± 116 days). No serious AEs were reported. Patient-reported pain impact scores were significantly reduced across the cohort (p = 0.034), and pain intensity scores verged on significance (p = 0.053). The majority of patients saw meaningful improvements in sleep (49.3%) and fatigue (35.6%).
Conclusion
This analysis presents real-world data collected as part of standard of care. More than one-third of patients benefited from oral medicinal cannabis, which is impactful given the refractory nature of their pain. Amelioration of the impact of pain confirms continued prescribing of this formulation and validates our observational methodology as a tool to determine the therapeutic potency of medicinal cannabinoids.
Keywords: Adverse events, Cannabinoids, Improved pain intensity, Improved pain impact, Medicinal cannabis
Introduction
Chronic pain is defined as pain enduring longer than 3 months involving a spectrum of physical pain, disability, emotional disturbance, and social withdrawal [1]. Chronic pain affects between 15% and 30% of the adult population worldwide [2], including 20% of Australians over the age of 45 [3], and imposes a significant socioeconomic burden on the community [4]. This burden is reflected in a $139.3 billion (2018) cost to the Australian economy, most of which is attributed to reduced quality of life (QoL) [5]. The annual global cost of poorly managed chronic pain has historically exceeded heart disease, cancer, or diabetes by 2-fold [6].
While the mainstay of chronic pain management is pharmacological therapy involving multimodal analgesics (nonsteroidal anti-inflammatory drugs [NSAIDs] and opioids) and adjuvant agents (anxiolytics and muscle relaxants) [7], this approach is rarely sustainable [1]. Opioids are often poorly tolerated, ineffective in the long term [8], and have high potential for abuse [9]. A diverse range of agents are prescribed to address the multidimensional nature of chronic pain and mitigate the known abuse potential. Despite these well-established approaches to treatment, many patients remain dissatisfied and refractory, seeking alternative options to manage their pain and its impact on their day-to-day functioning [10].
The endocannabinoid system is known to control pain at spinal and peripheral levels which has led to the exploration of medicinal cannabis as a treatment option for the management of chronic pain. The cannabis plant contains over 60 cannabinoids with potential to interact with the endocannabinoid system, the two best studied being Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD). These compounds are thought to work in concert to alleviate pain through activation and modulation of cannabinoid, opioid, serotonergic, and transient receptor potential pathways [7]. A cross-sectional survey of Australian medicinal cannabis patients repeatedly cited chronic pain as the most common reason for use [11, 12]. Several long-term prospective open-label studies support the use of medicinal cannabis for this indication [13, 14, 15, 16]. These findings informed the Australian medicines regulator, the Therapeutic Goods Administration (TGA) guidelines, that found “moderate” evidence to support medicinal cannabis as a treatment for chronic non-cancer pain [17]. However, these studies are limited in their translatability to the Australian context. Inhalational (smoked or vaporized) administration of medicinal cannabis has limited applicability when demographic and practical considerations favour oral administration. Furthermore, there is minimal information available to permit product identity, assessment of consistency, and measures of efficacy due to the diverse range of products accessed in these studies.
Since November 2016, Australian clinicians have been permitted to prescribe cannabis-based products to patients under the Special Access and Authorized Prescribed Schemes. Anecdotally, prescribers benefit from disease-specific prescription guidelines, emerging professional development programs, and ongoing feedback from their patients.
As the prescribing of pharmaceutical-grade medicinal cannabis products manufactured under Good Manufacturing Practice (GMP) continues to increase [18], studies assessing the effectiveness of these quality-controlled products in a real-world setting will become increasingly relevant for Australian prescribers and patients. Accordingly, the study presented here investigates the safety and effectiveness of an orally administered oil formulation of medicinal cannabis containing equal parts of THC and CBD (10 mg/mL THC; 10 mg/mL CBD) prescribed for the treatment of symptoms associated with chronic pain as part of the Cannabis Access Clinics Observational Study (CACOS).
The primary aim of this analysis was to evaluate the effectiveness and characterize adverse events (AEs) and serious adverse events (SAEs) experienced by patients prescribed this oral formulation. The secondary aim was to assess the self-reported health-related quality of life (HRQoL) impact of this therapeutic intervention on a subset of participants using a validated quality of life instrument [19]. The cross-sectional analysis format provides an opportunity to reflect on aspects of study design including sample size and clinical data management.
Methods
Setting and Informed Consent
This study was a multi-centre, prospective, open-label, observational study conducted within CA Clinics, a network of general practice clinics throughout Australia that specialize in prescribing cannabinoid formulations. Participants gave informed consent to allow analysis of observational data collected as part of their routine clinical care. This study (CACOS study) was approved by the Bellberry Human Research Ethics Committee (Applied Cannabis Research, ref: 2019-04-338).
Study Population
Patients were prescribed an orally administered oil formulation containing equal parts of THC and CBD (10 mg/mL THC; 10 mg/mL CBD; LGP Classic 10:10; Little Green Pharma, Perth, WA, Australia) for the treatment of pain as a symptom of a chronic pain condition as determined by the treating clinician at CA Clinics (Table 1). This formulation mimics other mixtures of CBD and THC except that it is administered as an oil-based liquid formulation rather than a spray [7]. For the purposes of this study, we used the definition of chronic pain as described by the International Association for the Study of Pain [20]. Candidates for this study were included if they met the following criteria: (1) adult aged 18 years or over, (2) reporting pain symptoms of at least 3-month duration, (3) previously tried and failed other analgesics, (4) sufficient cognitive function and English language skills to complete questionnaires, and (5) seeking medicinal cannabis therapy within the CA Clinics network. Candidates were excluded from the study if they (1) had any severe cognitive, medical, or psychiatric condition that impaired their ability to provide informed consent and complete questionnaires, (2) were women who were pregnant or breastfeeding, or (3) were administering a medicinal cannabis formulation other than the LGP Classic 10:10.
Table 1.
Cohort demographics for AE and PROMIS analyses
| AE analysis (n = 151) | PROMIS analysis (n = 71) | p value# | ||
|---|---|---|---|---|
| Age, mean (SD) | 54.6 (15.9) | 55.3 (15.4) | 0.75 | |
| Sex, n (%) | ||||
| Female | 84 (55.6) | 39 (54.9) | >0.9 | |
| Male | 67 (44.4) | 32 (45.1) | ||
| Pain Indication, n (%) | ||||
| Arthritis | 42 (27.8) | 17 (23.9) | ||
| Chronic pain unspecified | 33 (21.9) | 12 (16.9) | ||
| Neuropathic pain | 34 (22.5) | 19 (26.8) | ||
| Other musculoskeletal pain | 25 (16.6) | 18 (25.4) | ||
| Fibromyalgia | 18 (11.9) | 13 (18.3) | ||
| Cancer pain | 11 (7.3) | 2 (2.8) | 0.65 | |
| Migraine | 7 (4.6) | 5 (7.0) | ||
| Endometriosis | 6 (4.0) | 6 (8.5) | ||
| Trigeminal neuralgia | 3 (2.0) | 2 (2.8) | ||
| CRPS | 2 (1.3) | 1 (1.4) | ||
| Postherpetic neuralgia | 1 (0.7) | 1 (1.4) | ||
| Observation period, mean (SD), days^ | 133.3 (115.6) | 139.2 (116.4) | 0.72 | |
| Average dose, mean (SD), mg/day | ||||
| THC | 22.4 (13.0) | 22.4 (13.0) | >0.9 | |
| CBD | 22.4 (13.0) | 22.4 (13.0) | >0.9 |
Other musculoskeletal pain covered presentations such as neck pain, back pain, and pain following injury.
Period between reporting of AEs by the clinician or period elapsed between first and last PROMIS-29 completion. The period is directly relevant to the period of data collection being analysed for each cohort.
value calculated using unpaired Student's t test or Fisher's exact test for sex and Kruskal-Wallis test for pain indication group comparisons.
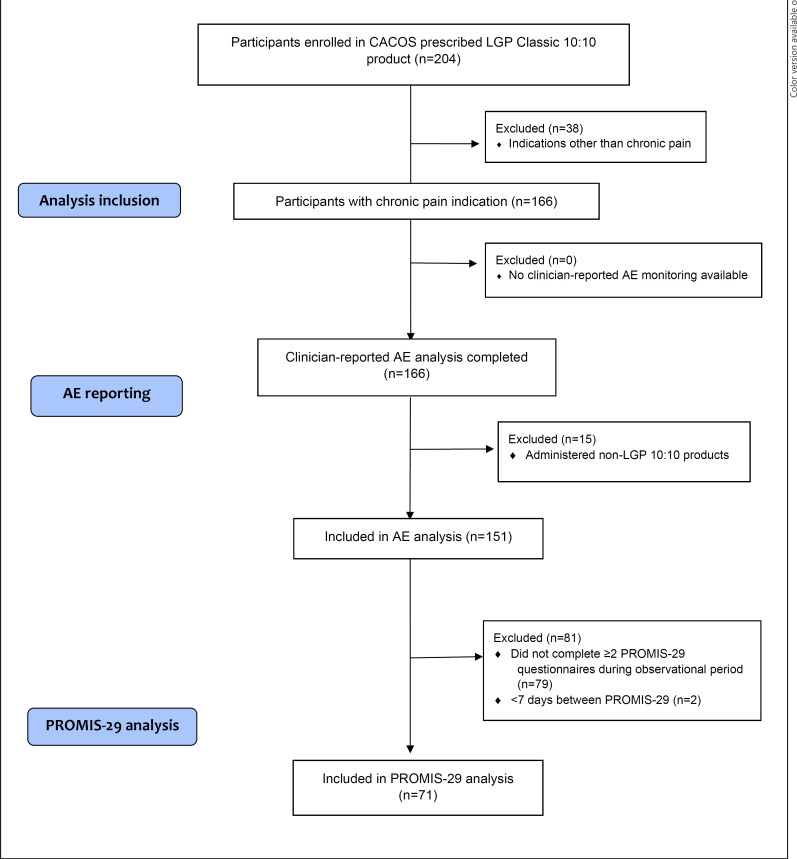
Data were collected between December 2018 and May 2020 from 151 participants. Clinical consult data were extracted from electronic medical records, and patient-reported outcome measures were captured and stored using Research Electronic Data Capture (REDCap). Details of the analysis cohort selection criteria are shown in Figure 1.
Fig. 1.
Cohort inclusion for AE and PROMIS analysis from CACOS participants that were prescribed the LGP Classic 10:10 product. Two analysis cohorts were identified: the AE cohort (n = 166) and the PROMIS subgroup (n = 85).
AE Reporting
Clinician-reported AEs and SAEs were collected at regular patient monitoring visits conducted as part of routine standard of care. The participant information consent form advised patients on the study to visit their clinician once monthly for the first 3 months of treatment and once per 3-month period thereafter. Clinicians reported the severity (mild/moderate/severe) and relatedness (unlikely/possibly/probably) of AEs within the clinical notes. In the event these details were missing in consult notes for some AE cases, a medical doctor and pharmacist were consulted to retrospectively apply these categories to each relevant AE. SAEs and AEs were categorized using the Medical Dictionary for Regulatory Activities (MedDRA, version 2019AB), a dictionary designed for use in the registration, documentation, and safety monitoring of medicinal products using a System Organ Classes (SOC) hierarchy and Common Terminology Criteria for Adverse Event (CTCAE, version 5.0) definitions. CTCAE is a web-based application to assist in locating appropriate AE terms.
In addition to AE monitoring during clinical visits, patients completed an online questionnaire during their treatment that included the question “Have you been experiencing any side effects from your medicinal cannabis prescribed by CA Clinics”? They were then given the option to choose from a list of possible side effects or choose “Other” or “None.” Patients did not report the severity of these side effects. This questionnaire was sent to participants once per week (online suppl. Fig. 1; for all online suppl. material, see www.karger.com/doi/10.1159/000521492).
Patients who self-reported an AE in this questionnaire were contacted by their CA Clinics clinician to assess the type of AE, relatedness to study treatment, and severity. These clinician-verified patient data are reported here, as well as AEs reported during clinical visits.
Patient-Reported Outcomes Measurement Information System Analysis
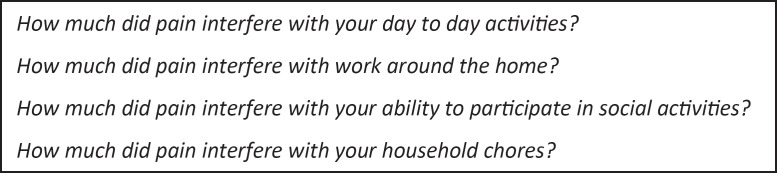
The PROMIS-29 (v2.0) is a validated, generic (disease non-specific) health-related quality of life (HRQoL) tool consisting of patient-reported outcome measures across seven domains used to evaluate physical, mental, and social health and wellbeing in people with chronic illnesses [21]. It has been used as a primary way to measure change in HRQoL [22]. Figure 1 provides an outline of analysis inclusion. Figure 2 shows the survey items..
Fig. 2.
PROMIS-29 questionnaire items assessing “pain impact.”
Patient data were included in the analysis if they had completed a minimum of two PROMIS-29 questionnaires during the observational period, at the time of cross-sectional sampling. PROMIS-29 data were excluded from participants who failed to complete two or more questionnaires. This questionnaire was sent to participants once per week (online suppl. Fig. 1).
The observational period for each patient was defined as the time between first and last data points collected. The minimum observation period for inclusion in the analysis was defined as ≥7 days given the PROMIS-29 is validated to a 7-day period. Analyses of PROMIS-29 domains were conducted using T-score reference tables from the PROMIS-29 v2.0 conversion tables [21]. Pain impact scores were calculated based on NIH Task Force recommendations [23].
Statistical Analysis
Data were analysed using SPSS Statistics 1.0.0.1327 (IBM, Armonk, NY, USA) and GraphPad Prism v8 (GraphPad, San Diego, CA, USA) for descriptive statistics. Effectiveness of treatment was explored through the PROMIS-29 survey consisting of 8 pain domains, 7 of which use 5-point Likert scales and 1 of which uses a 10-point Likert scale. Raw scores were converted to standardized T scores using the PROMIS-29 scoring manual (v2.1). Means and standard deviations were calculated for continuous variables, and frequency as a proportion of the group was calculated for categorical variables. Paired Student's t test was used for comparison of PROMIS T-score means over the observation period. Unpaired Student's t test was used to compare continuous variable means. The χ2 test (or Fisher's exact test when n < 20) was used to compare categorical variables. A p value below 0.05 was used to indicate statistical significance in all analyses.
Results
Demographics
One hundred and fifty-one participants contributed to the AE analysis, and a subset (71 participants) contributed to the PROMIS-29 analysis. The mean age of the AE analysis cohort was 54.6 (±15.9) years, with a slightly higher proportion of females (55.6%) than males. The most common chronic pain conditions included arthritis (n = 42; 27.8%), neuropathic pain (n = 34; 22.5%), and other musculoskeletal pain (n = 25; 16.6%). The mean observation period was 133.3 (±114.5, range: 9–392) days (Table 1). The mean daily dose of cannabinoids for the AE analysis cohort was 22.4 ± 13.0 mg THC and 22.4 ± 13.0 mg CBD administered as a ∼2.25 mL volume of oral oil.
A majority of subjects in this analysis group presented with a single chronic pain condition (n = 134/151, 88.7%), while the remainder presented with two or more chronic pain conditions. The mean age of the PROMIS-29 analysis cohort was 55.3 (±15.4) years, with a slightly higher proportion of females (54.9%) than males. The most common chronic pain conditions included neuropathic pain (n = 19, 26.8%), other musculoskeletal pain (n = 18, 25.4%), and arthritis (n = 17, 23.9%). The mean observation period was 139.2 (±116.4, range: 9–392) days (Table 1). The mean daily dose of cannabinoids for the PROMIS analysis cohort was 22.4 ± 13.0 mg for THC and 22.4 ± 13.0 mg CBD, administered as a ∼2.25 mL volume of oral oil.
A majority of subjects in this analysis group presented with a single chronic pain condition (n = 45/71, 63.4%), while the remainder presented with two or more chronic pain conditions. The mean cannabinoid dose was significantly lower at the first time point compared with the last time point collected (THC, 25.1 ± 27.5 mg, and CBD, 25.1 ± 27.5 mg, for the first time point compared with THC, 29.4 ± 24.0 mg, and CBD, 29.4 ± 24.0 mg, for the last time point; per day; two-way ANOVA; time point p < 0.0001; cannabinoid p > 0.05). No significant differences between analysis cohort demographics were found (p > 0.05) (Table 1).
Mild Adverse Events Associated with Medicinal Cannabis Were Observed within the Study Cohort
Over half (n = 91/151; 60.3%) of the total AE analysis cohort (n = 151) experienced at least one AE during the observational period, as reported by their clinician, while 39.7% (n = 60/151) of patients had no AEs. A total of 196 AEs were attributed to 91 subjects, highlighting that some patients experienced multiple AEs. The mean AEs reported (by clinicians) per participant were 2.2. Table 2 describes the AEs reported for the analysis cohort within the defined observational period (n = 151).
Table 2.
Clinician-reported adverse events for LGP Classic 10:10 product during the observational period
| MedDRA system organ class | AEs, (n) | Patients reporting AE, (n) |
|---|---|---|
| Psychiatric disorders, n (%) | ||
| Total | 66 (34) | 57 (63) |
| Somnolence | 25 (38) | 23 (40) |
| Anxiety | 9 (14) | 7 (12) |
| Insomnia | 8 (12) | 7 (12) |
| Confusional state | 3 (5) | 2 (4) |
| Disorientation | 4 (6) | 3 (5) |
| Euphoria | 4 (6) | 4 (7) |
| Paranoia | 4 (6) | 3 (5) |
| Dissociation | 3 (5) | 3 (5) |
| Depression | 3 (5) | 3 (5) |
| Hypervigilance | 2 (3) | 1 (2) |
| Tachyphrenia | 1 (2) | 1 (2) |
| Gastrointestinal disorders, n (%) | ||
| Total | 43 (22) | 34 (37) |
| Dry mouth/throat | 18 (42) | 14 (41) |
| Nausea | 13 (30) | 10 (29) |
| Diarrhoea | 6 (14) | 5 (15) |
| Abdominal discomfort | 3 (7) | 3 (9) |
| Nausea and vomiting | 1 (2) | 1 (3) |
| Constipation | 2 (5) | 1 (3) |
| Nervous system disorders, n (%) | ||
| Total | 38 (19) | 31 (34) |
| Dizziness | 10 (26) | 10 (32) |
| Paraesthesia | 5 (13) | 3 (10) |
| Memory impairment | 4 (11 | 3 (10) |
| Vertigo | 4 (11) | 2 (6) |
| Sedation | 3 (8) | 3 (10) |
| Restlessness | 3 (8) | 2 (6) |
| Seizure | 2 (5) | 2 (6) |
| Dysgeusia | 2 (5) | 2 (6) |
| Agitation | 2 (5) | 1 (3) |
| Tremor | 1 (3) | 1 (3) |
| Gait disturbance | 1 (3) | 1 (3) |
| Headache | 1 (3) | 1 (3) |
| General disorders and administration site conditions, n (%) | ||
| Total | 28 (12) | 21 (22) |
| Fatigue | 6 (39) | 6 (48) |
| Lethargy | 11 (39) | 7 (33) |
| Balance problems | 0 (11) | 0 (14) |
| Pain | 2 (7) | 2 (10) |
| Irritability | 1 (4) | 1 (5) |
| Metabolism and nutritional disorders, n (%) | ||
| Total | 7 (4) | 6 (7) |
| Increased appetite | 4 (57) | 3 (50) |
| Decreased appetite | 3 (43) | 3 (50) |
| Eye disorders, n (%) | ||
| Total | 7 (4) | 4 (4) |
| Ocular discomfort | 3 (43) | 1 (25) |
| Dry eyes | 2 (29) | 1 (25) |
| Flushing in eyes | 1 (14) | 1 (25) |
| Eye swelling | 1 (14) | 1 (25) |
| Cardiac disorders, n (%) | ||
| Total | 6 (3) | 5 (5) |
| Increased blood pressure | 5 (83) | 4 (75) |
| Palpitations | 1 (17) | 1 (25) |
| Skin and subcutaneous tissue disorders, n (%) | ||
| Total | 2 (1) | 2 (2) |
| Skin irritation | 1 (50) | 1 (50) |
| Skin burning sensation | 1 (50) | 1 (50) |
| Musculoskeletal and connective tissue disorders, n (%) | ||
| Total | 2 (1) | 2 (2) |
| Muscle tightness | 1 (50) | 1 (50) |
| Muscle twitching | 1 (50) | 1 (50) |
| Social circumstances, n (%) | ||
| Total | 2 (1) | 1 (1) |
| Rumination | 1 (50) | 1 (100) |
| Social withdrawal | 1 (50) | 1 (100) |
| Vascular disorders, n (%) | ||
| Total | 1 (0.5) | 1 (1) |
| Orthostatic hypotension | 1 (100) | 1 (100) |
| Blood and lymphatic system disorders, n (%) | ||
| Total | 1 (0.5) | 1 (1) |
| Anaemia | 1 (100) | 1 (100) |
| Ear and labyrinth disorders, n (%) | ||
| Total | 1 (0.5) | 1 (1) |
| Tinnitus | 1 (100) | 1 (100) |
| Total# | 196 | 91 |
Patients could experience a single AE on multiple occasions, and hence the number of patients often exceeding the total number of AEs.
The severity analysis revealed the majority of AEs reported (n = 168/196; 85.7%) were mild (grade 1), as opposed to moderate (n = 54/196; 27.6%; grade 2) or severe (n = 10/196; 5.1%; grade 3) in intensity, per the grading defined by the TGA and CTCAE reporting requirements. No grade 4 or 5 events were reported.
The relatedness of the AEs to medicinal cannabis treatment was reported. Most AEs were probably related (n = 150/196, 76.5%) or possibly related (n = 76/196, 38.8%) as opposed to unlikely related (n = 6/196, 3.1%) to treatment with LGP Classic 10:10 oil. No SAEs were reported within the observational period for this cohort of patients.
Psychiatric and Gastrointestinal-Related AEs Accounted for the Majority Reported
The majority of the cohort experienced at least one AE (n = 91/151; 60.3%). AEs were classified by the MedDRA SOC and reported based on frequency and the number of patients experiencing each AE (Table 2). The majority of AEs experienced fell under psychiatric disorders (n = 66/196; 33.7%), followed by gastrointestinal disorders (n = 43/196; 21.9%) and nervous system disorders (n = 38/196; 19.4%). The two former categories accounted for ∼55% of all reported AEs. Somnolence (n = 23/196; 11.7%) and dry mouth/throat (n = 14/196, 7.1%) were the most common AEs experienced.
Improvements in Pain Intensity and Pain Impact Scores Were Observed
Within the PROMIS-29 analysis subset (n = 71), we found a significant improvement in the impact of pain and an improvement verging on significance for pain intensity when comparing first and last completed questionnaires within the observational period for each subject (Table 3). Analysis showed a reduction in overall pain intensity scores (−0.6 ± 2.5-point reduction; ∼9% decrease; p = 0.053) approaching significance. When pain intensity changes were assessed using the published minimal clinically important differences (MCID) value [23] (2.0 change), 32.9% of the cohort was improved compared with 45.2% unchanged and 21.9% worsened. The average intensity change in those that improved (n = 24) was a 3.2 ± 1.9-point reduction (p < 0.0001) compared to a 2.6 ± 0.6-point increase in those that had worsened pain intensity (n = 16; p < 0.0001).
Table 3.
Change to PROMIS domains over the observational period with medicinal cannabis treatment [23, 24, 25, 26]
| Measure (range) | First (n = 71) mean (SD) | Last (n = 71) mean (SD) | p value | Improved n (%) | Not changed n (%) | Worsened n (%) | MCID |
|---|---|---|---|---|---|---|---|
| PROMIS-29 domains | |||||||
| Pain intensity (0–10) | 6.3 (2.1) | 5.7 (2.3) | 0.053 | 24 (32.9) | 33 (45.2) | 16 (21.9) | 2.0 [23] |
| Domains as T-scores (population mean | 50, SD 10) | ||||||
| Pain interference | 64.7 (7.9) | 63.5 (8.4) | 0.16 | 27 (37) (34.1) | 26 (35.6) | 20 (27.4) | 2.0 [23] |
| Fatigue | 54.9 (10.6) | 55.5 (10.3) | 0.62 | 26 (35.6) | 25 (34.2) | 22 (30.1) | 2.5 [24] |
| Sleep disturbance | 53.6 (10.0) | 51.4 (9.5) | 0.13 | 36 (49.3) | 11 (15.1) 13 | 26 (35.6) | 2.0^ |
| Anxiety | 52.7 (8.6) | 53.2 (10.2) | 0.61 | 17 (23.3) | 37 (50.7) | 19 (26.0) | 2.3 [25] |
| Depression | 53.2 (8.8) | 52.8 (9.1) | 0.67 | 17 (23.3) | 37 (50.7) | 19 (26.0) | 3.0 [25] |
| Satisfaction with social role | 40.5 (9.5) | 40.4 (8.3) | 0.93 | 23 (31.5) | 34 (46.6) | 16 (21.9) | 2.0^ |
| Physical function | 35.8 (8.3) | 36.2 (7.7) | 0.58 | 26 (35.6) | 30 (41.1) | 17 (23.3) | 1.9 [23, 26] |
| Impact score (raw score, 8–50) | 33.5 (10.2) | 31.1 (10.0) | 0.034* | 35 (47.9) | 21 (28.8) | 17 (23.3) | 3.0 [23] |
| Impact shift | − | − | − | 17 (23.6) | 43 (58.3) | 13 (18.1) | − |
Bold values indicate the placement of the cohort majority. Impact shift is defined as change from mild impact (8–27) to moderate impact (28–34) to severe impact (>35) based on impact score cutoffs. A positive impact shift shows patients changed in a positive direction from a detrimental impact level to a lesser one (i.e., severe → moderate/moderate → mild). MCID, minimal clinically important difference.
MCID = 2.0 as default given there is no published MCID value in the literature to reference.
p < 0.05 compared to first (paired Student's t test).
Impact score was also calculated based on responses to targeted pain impact items (Fig. 2). A significant decrease in pain impact score was found overall, with the mean impact score reduced by 2.3 ± 9.4 points (p = 0.034). Of those with a meaningful improvement (based on minimal clinically important difference [MCID] = 3.0; n = 35), a mean 9.6 ± 7.9-point decrease was observed (p < 0.0001). Most subjects experienced an improvement in pain impact (47.9%) suggesting that the reduction in pain intensity was having an effect on patients' quality of life that was not reflected in the pain intensity measurements. Conversely, a mean 8.7 ± 4.5-point increase was seen in those with worsened pain impact outcomes (p < 0.0001, n = 17).
Sleep Disturbance and Fatigue Significantly Improved in the Majority of Patients
There were no statistically significant improvements across the other PROMIS-29 domains when comparing mean T-scores across the observation period (Table 3). However, the majority of subjects who reported changes to fatigue and sleep disturbance domains noted improvements (sleep disturbance 49.3% improved; fatigue 35.6% improved) (Table 3). Evaluation of only those that were improved (based on MCID cutoffs) showed a significant improvement in sleep disturbance T-scores (−12.5 ± 6.5 points; p < 0.0001; n = 36) and fatigue T-scores (−8.6 ± 4.5 points; p < 0.0001, n = 26). These subjects received an average daily dose of 21.0 ± 10.1 mg THC + 21.0 ± 10.1 mg CBD.
Similarly, evaluation of only those that reported worsening fatigue showed significantly increased T-scores (+11.85 ± 8.7 points; p < 0.0001, n = 22). The same was seen in subjects reporting increased sleep disturbance (+11.2 ± 7.2 points; p < 0.0001, n = 26). It is noted that within the sleep domain, participants appeared either to have improved or to have worsened sleep, unlike other domains where the majority were categorized as “not changed.”
A dose analysis was completed for the sleep disturbance domain with subjects stratified based on improvement, no change, or worsening of sleep disturbance. The average daily dose in subjects who improved was lower (21.0 ± 10.1 mg THC + 21.0 ± 10.1 mg CBD) relative to the daily dose in subjects who reported no change (21.1 ± 13.3 mg THC plus 31.1 ± 13.3 mg CBD) or worsening (25.1 ± 16.1 mg THC plus 25.1 ± 16.1 mg CBD) in sleep disturbance.
Anxiety and Depression Score Changes Were in Line with Other Domains
The majority of the cohort reported no change in anxiety (50.7%) and depression (50.7%) domains based on MCID cutoff analysis (MCIDs 2.3 and 3.0, respectively) (Table 3). The relative division between improvement, no change, and worsening in these two mental health domains was consistent with other domains including physical functioning, pain interference, and social satisfaction.
Discussion
The present study analyses real-world evidence (RWE) collected as part of the standard of care to explore safety, tolerability, and self-reported effectiveness of a medically prescribed pharmaceutical-grade medicinal cannabis product (LGP Classic 10:10). Within the cohort, the majority of subjects experienced at least one AE during the observation period, with no SAEs reported. Encouragingly, pain impact scores were significantly reduced across the cohort (Table 3). Additionally, most subjects reported improvements in sleep disturbance and fatigue, both known to be highly related to one's ability to manage and cope with pain [27].
The use of a standardized pharmaceutical-grade GMP-manufactured product within the cohort ensures quality and consistency allowing direct dose comparability across patients. Coupled with clinician oversight and monitoring, the findings presented here allow for clinically relevant insights to be gained that are lacking from anecdotal reports of poorly defined cannabis use.
We have focused our comparisons of the current analysis with those of existing published studies of nabiximols (Sativex®; GW Pharma Ltd., Salisbury, UK), as both products are administered orally and contain an equivalent ratio of THC to CBD (1:1 THC:CBD). There are comparative differences worth noting in that nabiximols is an oromucosal spray, whereas LGP Classic 10:10 is an oil formulation. Despite this difference, nabiximols provides a useful comparator as a GMP-manufactured pharmaceutical-grade product that has been evaluated extensively in regulator-approved trials and clinical studies for pain indications [28, 29, 30, 31, 32, 33] in contrast to recent large cohort studies examining inhaled formulations alone or in combination with oral formulations [2, 13, 14, 15, 34].
Analgesic Effects Are Consistent with Existing Clinical Trials of Nabiximols
Pain impact scores were significantly reduced across the study population. The average daily dose reported in this study (22.4 mg THC and 22.4 mg CBD) closely resembled that of previously published clinical studies of nabiximols that reported consistent improvements in pain-related outcome measures [29, 30, 31, 32, 33, 35].
Johnson et al. [31] reported nabiximols (23 mg THC and 22 mg CBD per day) was effective in management of intractable cancer-related pain, with 43% of patients achieving ≥30% improvement in mean pain score, an effect not seen with THC alone and consistent with long-term follow-up [32]. Furthermore, Ueberall et al. [33] showed a lower nabiximols dose (19.2 mg THC and 17.8 mg CBD per day) leads to reductions in pain and improvement in the subjective experience of pain in a mixed chronic pain condition cohort (n = 800), which is consistent with the amelioration of pain intensity we found in the current study.
Tolerance was not directly assessed in this study cohort; however, due to the up-titrating nature of medicinal cannabis prescribing, an average higher cannabinoid dose was associated with the final time point compared to the first. The up-titrating nature of medicinal cannabis prescribing may fully explain this phenomenon, or there may be some level of tolerance developed. Additional analyses exploring tolerance are needed in observational cohorts to address this question. Analyses of this kind may be possible in a complete analysis of the CACOS data at the study close, as opposed to within a cross-sectional analysis such as is presented here. Two published long-term follow-up studies [30, 32] showed no evidence of tolerance to a 1:1 THC:CBD oral formulation being developed.
Changes to Sleep Disturbance Are Consistent with Existing Clinical Trials of Nabiximols
Sleep disturbance decreased in the current study cohort (49.3% reporting meaningful improvements based on MCID) which is consistent with the outcomes of several trials of nabiximols. Specifically, two studies [29, 30] showed sleep disturbance was improved with nabiximols over a 4-week period with a similar dosing schedule (26 mg THC and 24 mg CBD per day), while a study in multiple sclerosis patients (mean dose 19.7 mg THC and 18.3 mg CBD) showed significantly less sleep disruption after 12 weeks of treatment compared to baseline [35]. Additionally, Ueberall et al. [33] reported approximately half of the cohort had improvements in sleep quality with nabiximols (at equivalent doses), which is consistent with the proportion improved in the current analysis.
Interestingly, while Johnson et al. [31] found no effect of nabiximols on sleep quality after 2 weeks, the follow-up study of mean length 25 days (range: 2–579) saw reduced sleep disruption, potentially suggesting a longer time period is required for sleep effects to be observed. Portenoy et al. [28] also reported improved sleep and pain over a 5-week period with low (2.7–10.8 mg THC and 2.5–10 mg CBD daily) and moderate nabiximols doses (16.2–27 mg THC and 15–25 mg CBD daily). However, a higher-dose group (29.7–43.2 mg THC and 27.5–40 mg CBD daily) did not show such an effect. This potentially suggests sleep improvements are somewhat dose dependent, with higher doses impeding sleep benefit, possibly due to increased AEs (such as anxiety, nausea, or insomnia). This observation is in line with what we have observed in this analysis, with the lowest average cannabinoid dose associated with sleep improvements compared to those reporting unchanged or worsened sleep (with higher average cannabinoid doses). Finally, the average cohort observational period was 133.4 days (Table 1). The subset of patients reporting improved sleep had a mean observational period of 147.2 days (minimum 22.3 days), supporting this longer (>2-week) time period hypothesis in relation to self-reported sleep outcomes. Due to the cross-sectional study design, it is unclear whether the medicinal cannabis lowered pain levels leading to better sleep, or if improvements in sleep disturbance and fatigue were directly due to the benefits of treatment.
Reported Adverse Events Are Consistent with Existing Published Studies
More than half of the participants (60.3%) experienced at least one AE during the observation period with no SAEs experienced, as reported by their treating clinicians. This proportion of AEs is consistent with existing studies of medicinal cannabis products [36, 37] and analgesics including opioids [38].
The most common AEs reported in the literature for nabiximols are consistent with those in the present study. These included psychiatric (somnolence), gastrointestinal (dry mouth and nausea), and nervous system-related (dizziness), all of which presented with mild to moderate severity in chronic pain trials of nabiximols within a dose range similar to the present study [29, 30, 31, 32, 35]. At the time of reporting, the World Health Organization adverse drug reaction database (VigiAccessTM) also aligns with our findings, with nervous system disorders (39%), gastrointestinal disorders (33%), and psychiatric disorders (23%) being the most commonly reported SOC classes for nabiximols adverse drug reactions [39].
While fewer well-controlled studies of medicinal cannabis in chronic pain exist outside those involving nabiximols, the findings of the present study reinforce the observation that THC at an intermediate-dose/or mixture is effective in alleviating chronic pain and improving HRQoL, while unbridled THC exposure can cause undesirable side effects [13, 14, 15, 16]. One such side effect is anxiety. Interestingly, we did not observe any significant changes to anxiety or depression scores in the study cohort despite some patients taking meaningful doses of THC. This is an important finding given that THC has been shown to have dose-dependent effects on anxiety responses [40].
The majority of AEs reported in the literature are typically associated with THC-containing medications as opposed to CBD-only medications and may also be linked to the excipients (i.e., oral oil). The AEs most commonly reported in medications where the predominant active pharmaceutical ingredient is CBD (notably studies using EpidiolexTM, which lacks THC [41, 42, 43]) are mild to moderate pyrexia, upper respiratory tract infection, and somnolence, as well as gastrointestinal upset [41, 42, 43]. However, these studies involved an epilepsy cohort with fever disorders. Furthermore, high doses of anticonvulsants were administered concomitantly with a relatively high CBD dosing regimen (i.e., 10–20 mg/kg/day), a combination known to elevate the risk of AEs [44]. These clinically significant differences in the study population make comparisons with the findings of the current study challenging.
Psychosis-related AEs typically ascribed to chronic use of THC [40, 45], including psychosis, euphoria, hallucinations, and paranoia, were reported at low frequency within the current study (Table 2). One potential explanation for this may be related to the drug formulation (i.e., oral oil). Oral administration prevents rapid-onset high THC concentrations that are typical of inhaled products [46, 47, 48], potentially reducing the incidence of THC-related side effects. In comparison, pharmacokinetic studies of oral THC-containing products have shown a delay in reaching peak plasma concentration (>2 h) compared with inhaled administration [47, 48].
The Relevance of RWE in the Context of Medicinal Cannabis
In the absence of randomized controlled trials (RCTs), our data show that analysis of RWE collected as part of patients' routine care can yield useful information. RCTs are the gold standard required to determine drug efficacy; however, there is a scarcity of this level of research activity among the medicinal cannabis sector.
The research scarcity may in part be explained by the inability to create and protect intellectual property because cannabinoids are naturally occurring compounds that have been used medicinally, but without evidence for millennia. This experience precludes many traditional drivers of commercial drug development because of likely failure to recoup R&D costs through market exclusivity of the end-registered product. Our observational approach and retrospective analyses of data collected as part of standard care must be prioritized to ensure prescribing of medicinal cannabis is evidence based.
Limitations
There are some limitations to the interpretation of our data. Notably, the study was not controlled. It was observational in nature and relied upon the accuracy of patient-reported information. Patient observations were not validated independently. The observation period varied broadly across the study population given the cross-sectional nature of the analysis; some patients were recently enrolled while others were 12 months into their course of treatment. There has been no attempt to correct for observation period length for each individual participant and relate this to their patient-reported outcomes, beyond ensuring a minimum of 7 days between survey completion. The irregularity of patient reporting intervals has also not been accounted for in the PROMIS-29 analysis. Furthermore, we did not sub-classify our patients or make other attempts to control for selection bias for things such as pain syndromes or response rate. Participants taking more than one medicinal cannabis product concurrently during the observation period (including the test product) were excluded from analysis.
While data on AEs related to drug-drug interactions were not explicitly collected as part of our study, it is a notable area to be explored in future studies given the known interactions between cannabinoids and metabolism of other prescribed drugs [49, 50]. It should be noted that all participants within the analysed cohort had previously tried and failed other analgesics prior to being prescribed medicinal cannabis. A proportion of participants were still taking concomitant medications for their pain or other conditions including opioids and/or NSAIDs. While we are able to identify those participants that were taking additional medications, an analysis of the influence of these substances is beyond the scope of this study. The monitoring of expectancy effects associated with perceived effectiveness of the study intervention is also beyond the scope of this study.
Future studies need to include formal monitoring of any changes to the administration of opioids or analgesic medications for patients being prescribed medicinal cannabis products. This was absent from the current analysis, and therefore we cannot comment on how changes to other medications may have affected the patient-reported outcomes presented here. Polypharmacy for chronic pain patients is an important consideration. As such, amendments to our protocol need to be made to capture data on changes to other concomitant medications, especially opioids in the future.
Tolerability would best be assessed through establishing rates of AEs among study dropouts. This information is gathered in clinical notes to be included in subsequent CACOS study analyses. Subsequent analyses will also benefit from inclusion of severity and relatedness information by AE type.
Finally, we recognize that the experience of pain is complex − a merging of sensory and affective processes. The affective component of pain is thought to be modulated by opioid and endocannabinoid neurotransmitter systems [51]. Despite administering a cannabinoid receptor modulator and recognizing that participants were administering additional pain medications, this study does not explore an important affective feature of pain treatment: the expectation surrounding effectiveness of treatment also known as a placebo effect. This is an emergent theme in cannabinoid research, and future work should interrogate participants' expectations as part of routine questionnaires.
Conclusions
The results of this study demonstrated a significantly positive effect of LGP Classic 10:10 oral medicinal cannabis oil on the impact of pain (as measured by using the PROMIS-29 HRQoL tool). A reduction in pain intensity scores verged on significance (p = 0.053). This is a clinically relevant finding considering that this patient cohort comprises refractory cases where relief has not been obtained with existing medications, including opioids, NSAIDs, and steroids.
This analysis also highlights that medicinal cannabis is not efficacious for all, a finding that is consistent with most other drug classes. Successful treatment of one-third of refractory patients has significant impacts on the total refractory population size and greatly affects the HRQoL of those who have found relief with medicinal cannabis. This study further highlights the need for continued research in this field, ideally comprising follow-on RCTs that can more adequately address dose, responder characteristics, and potential effect size.
Statement of Ethics
This study (CACOS study) was reviewed and approved by the Bellberry Human Research Ethics Committee (Applied Cannabis Research, Approval No. 2019-04-338). Written informed consent was obtained from participants to participate in the study.
Conflict of Interest Statement
L.N.W. reports personal fees from Little Green Pharma, outside the submitted work. All other authors have no conflicts of interest to declare.
Funding Sources
This project was jointly funded by Little Green Pharma (LGP) and Applied Cannabis Research (ACR). Participants were prescribed an LGP cannabinoid medication by clinicians from Cannabis Access Clinics (CAC). ACR analysed observational data from consenting CAC patients.
Author Contributions
S.A. and M.B. ran data analysis. S.A., M.B., L.N.W., and J.B. wrote the body of the manuscript. S.A., L.N.W., and J.B. prepared the manuscript for submission to the journal. M.H. advised on patient records. M.H. and S.N. provided specialist medical and technical advice.
Data Availability Statement
The data that support the findings of this study are not publicly available. The data are contained within patient records that are securely stored for access by CAC staff and researchers only. Further enquiries can be directed to the corresponding author.
Supplementary Material
Supplementary data
Acknowledgments
The authors wish to thank Ms. Belen Gomez and Dr. Natalie Beveridge for their assistance in establishing the data collection facilities for this project.
References
- 1.Hylands-White N, Duarte RV, Raphael JH. An overview of treatment approaches for chronic pain management. Rheumatol Int. 2017;37((1)):29–42. doi: 10.1007/s00296-016-3481-8. [DOI] [PubMed] [Google Scholar]
- 2.Campbell G, Hall WD, Peacock A, Lintzeris N, Bruno R, Larance B, et al. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: findings from a 4-year prospective cohort study. Lancet Public Health. 2018;3((7)):e341–50. doi: 10.1016/S2468-2667(18)30110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Institute of Health and Welfare . Chronic pain in Australia. Canberra, Australia: AIHW; 2020. [Google Scholar]
- 4.Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and profile of high-impact chronic pain in the United States. J Pain. 2019;20((2)):146–60. doi: 10.1016/j.jpain.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Economics DA. The cost of pain in Australia: painaustralia. Canberra, Australia: ACT; 2019. p. p. 117. [Google Scholar]
- 6.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13((8)):715–24. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Überall MA. A review of scientific evidence for THC:CBD oromucosal spray (Nabiximols) in the management of chronic pain. J Pain Res. 2020;13:399–410. doi: 10.2147/JPR.S240011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the space randomized clinical trial. JAMA. 2018;319((9)):872–82. doi: 10.1001/jama.2018.0899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Penington Institute . Australia's annual overdose report. Victoria, Australia: Penington Institute; 2019. [Google Scholar]
- 10.O'Brien T, Breivik H. The impact of chronic pain-European patients' perspective over 12 months. Scand J Pain. 2012;3((1)):23–9. doi: 10.1016/j.sjpain.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Lintzeris N, Mills L, Suraev A, Bravo M, Arkell T, Arnold JC, et al. Medical cannabis use in the Australian community following introduction of legal access: the 2018–2019 online cross-sectional cannabis as medicine survey (CAMS-18) Harm Reduct J. 2020;17((1)):37. doi: 10.1186/s12954-020-00377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lintzeris N, Driels J, Elias N, Arnold JC, McGregor IS, Allsop DJ. Medicinal cannabis in Australia, 2016: the cannabis as medicine survey (CAMS‐16) Med J Aust. 2018;209((5)):211–6. doi: 10.5694/mja17.01247. [DOI] [PubMed] [Google Scholar]
- 13.Ware MA, Wang T, Shapiro S, Collet JP, COMPASS study team Cannabis for the management of pain: assessment of safety study (COMPASS) J Pain. 2015;16((12)):1233–42. doi: 10.1016/j.jpain.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Bellnier T, Brown GW, Ortega TR. Preliminary evaluation of the efficacy, safety, and costs associated with the treatment of chronic pain with medical cannabis. Ment Health Clin. 2018;8((3)):110–5. doi: 10.9740/mhc.2018.05.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Safakish R, Ko G, Salimpour V, Hendin B, Sohanpal I, Loheswaran G, et al. Medical cannabis for the management of pain and quality of life in chronic pain patients: a prospective observational study. Pain Med. 2020;21((11)):3073–86. doi: 10.1093/pm/pnaa163. [DOI] [PubMed] [Google Scholar]
- 16.Haroutounian S, Ratz Y, Ginosar Y, Furmanov K. Saifi F. Meidan R, et al. The effect of medicinal cannabis on pain and quality-of-life outcomes in chronic pain. Clin J Pain. 2016;32((12)):1036–43. doi: 10.1097/AJP.0000000000000364. [DOI] [PubMed] [Google Scholar]
- 17.TGA (Therapeutic Goods Administration) Therapeutic goods administration. Canberra, Australia: 2017. Guidance for the use of medicinal cannabis in the treatment of chronic non-cancer pain in Australia; p. p. 36. [Google Scholar]
- 18.Therapeutic Goods Administration . Access to medicinal cannabis products: SAS Category B approval statistics. Canberra, Australia: 2020. Available from: https://www.tga.gov.au/access-medicinal-cannabis-products-1. [Google Scholar]
- 19.Hays RD, Spritzer KL, Schalet BD, Cella D. PROMIS®-29 v2. 0 profile physical and mental health summary scores. Qual Life Res. 2018;27((7)):1885–91. doi: 10.1007/s11136-018-1842-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merskey H. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. Pain J. 1986;3:226. [PubMed] [Google Scholar]
- 21. HealthMeasures: PROMIS: National Institutes of Health.
- 22.Rose AJ, Bayliss E, Huang W, Baseman L, Butcher E, García RE, et al. Evaluating the PROMIS-29 v2.0 for use among older adults with multiple chronic conditions. Qual Life Res. 2018;27((11)):2935–44. doi: 10.1007/s11136-018-1958-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deyo RA, Ramsey K, Buckley DI, Michaels L, Kobus A, Eckstrom E, et al. Performance of a patient reported outcomes measurement information system (PROMIS) short form in older adults with chronic musculoskeletal pain. Pain Med. 2016;17((2)):314–24. doi: 10.1093/pm/pnv046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six patient-reported outcomes measurement information system-cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64((5)):507–16. doi: 10.1016/j.jclinepi.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kroenke K, Yu Z, Wu J, Kean J, Monahan PO. Operating characteristics of PROMIS four-item depression and anxiety scales in primary care patients with chronic pain. Pain Med. 2014;15((11)):1892–901. doi: 10.1111/pme.12537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hays RD, Spritzer KL, Fries JF, Krishnan E. Responsiveness and minimally important difference for the patient-reported outcomes measurement information system (PROMIS) 20-item physical functioning short form in a prospective observational study of rheumatoid arthritis. Ann Rheum Dis. 2015;74((1)):104–7. doi: 10.1136/annrheumdis-2013-204053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013;14((12)):1539–52. doi: 10.1016/j.jpain.2013.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Portenoy RK, Ganae-Motan ED, Allende S, Yanagihara R, Shaiova L, Weinstein S, et al. Nabiximols for opioid-treated cancer patients with poorly-controlled chronic pain: a randomized, placebo-controlled, graded-dose trial. J Pain. 2012;13((5)):438–49. doi: 10.1016/j.jpain.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Rog DJ, Nurmikko TJ, Friede T, Young CA. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology. 2005;65((6)):812–9. doi: 10.1212/01.wnl.0000176753.45410.8b. [DOI] [PubMed] [Google Scholar]
- 30.Rog DJ, Nurmikko TJ, Young CA. Oromucosal Δ9-tetrahydrocannabinol/cannabidiol for neuropathic pain associated with multiple sclerosis: an uncontrolled, open-label, 2-year extension trial. Clin Ther. 2007;29((9)):2068–79. doi: 10.1016/j.clinthera.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 31.Johnson JR, Burnell-Nugent M, Lossignol D, Ganae-Motan ED, Potts R, Fallon MT. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manag. 2010;39((2)):167–79. doi: 10.1016/j.jpainsymman.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Johnson JR, Lossignol D, Burnell-Nugent M, Fallon MT. An open-label extension study to investigate the long-term safety and tolerability of THC/CBD oromucosal spray and oromucosal THC spray in patients with terminal cancer-related pain refractory to strong opioid analgesics. J Pain Symptom Manag. 2013;46((2)):207–18. doi: 10.1016/j.jpainsymman.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 33.Ueberall MA, Essner U, Mueller-Schwefe GH. Effectiveness and tolerability of THC: CBD oromucosal spray as add-on measure in patients with severe chronic pain: analysis of 12-week open-label real-world data provided by the German Pain e-Registry. J Pain Res. 2019;12:1577. doi: 10.2147/JPR.S192174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lucas P, Boyd S, Milloy MJ, Walsh Z. Cannabis significantly reduces the use of prescription opioids and improves quality of life in authorised patients: results of a large prospective study. Pain Med. 2021;22((3)):727–39. doi: 10.1093/pm/pnaa396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Markovà J, Essner U, Akmaz B, Marinelli M, Trompke C, Lentschat A, et al. Sativex® as add-on therapy vs. further optimized first-line ANTispastics (SAVANT) in resistant multiple sclerosis spasticity: a double-blind, placebo-controlled randomised clinical trial. J Neurosci. 2019;129((2)):119–28. doi: 10.1080/00207454.2018.1481066. [DOI] [PubMed] [Google Scholar]
- 36.Vermersch P. Sativex(®) (tetrahydrocannabinol + cannabidiol), an endocannabinoid system modulator: basic features and main clinical data. Expert Rev Neurother. 2011;11((4)):15–9. doi: 10.1586/ern.11.27. [DOI] [PubMed] [Google Scholar]
- 37.Ltd GP . Sativex oromucosal spray: SmPC. Cambridge, UK: EMC; Available from: https://wwwmedicinesorguk/emc/product/602/smpc. [Google Scholar]
- 38.Moore RA, McQuay HJ. Prevalence of opioid adverse events in chronic non-malignant pain: systematic review of randomised trials of oral opioids. Arthritis Res Ther. 2005;7((5)):R1046–51. doi: 10.1186/ar1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.WHO (World Health Organisation) Vigiaccess. Uppsala Monitoring Centre; 2020. [Google Scholar]
- 40.Childs E, Lutz JA, de Wit H. Dose-related effects of delta-9-THC on emotional responses to acute psychosocial stress. Drug Alcohol Depend. 2017;177:136–44. doi: 10.1016/j.drugalcdep.2017.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Devinsky O, Cross JH, Laux L, Marsh E, Miller I, Nabbout R, et al. Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N Engl J Med. 2017;376((21)):2011–20. doi: 10.1056/NEJMoa1611618. [DOI] [PubMed] [Google Scholar]
- 42.Devinsky O, Patel AD, Cross JH, Villanueva V, Wirrell EC, Privitera M, et al. Effect of cannabidiol on drop seizures in the Lennox–Gastaut syndrome. N Engl J Med. 2018;378((20)):1888–97. doi: 10.1056/NEJMoa1714631. [DOI] [PubMed] [Google Scholar]
- 43.Thiele EA, Marsh ED, French JA, Mazurkiewicz-Beldzinska M, Benbadis SR, Joshi C, et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391((10125)):1085–96. doi: 10.1016/S0140-6736(18)30136-3. [DOI] [PubMed] [Google Scholar]
- 44.Gaston TE, Bebin EM, Cutter GR, Liu Y, Szaflarski JP, UAB CBD Program Interactions between cannabidiol and commonly used antiepileptic drugs. Epilepsia. 2017;58((9)):1586–92. doi: 10.1111/epi.13852. [DOI] [PubMed] [Google Scholar]
- 45.Johns A. Psychiatric effects of cannabis. Br J Psychiatry. 2001;178((2)):116–22. doi: 10.1192/bjp.178.2.116. [DOI] [PubMed] [Google Scholar]
- 46.Fabritius M, Chtioui H, Battistella G, Annoni JM, Dao K, Favrat B, et al. Comparison of cannabinoid concentrations in oral fluid and whole blood between occasional and regular cannabis smokers prior to and after smoking a cannabis joint. Anal Bioanal Chem. 2013;405((30)):9791–803. doi: 10.1007/s00216-013-7412-1. [DOI] [PubMed] [Google Scholar]
- 47.Spindle TR, Cone EJ, Schlienz NJ, Mitchell JM, Bigelow GE, Flegel R, et al. Acute effects of smoked and vaporized cannabis in healthy adults who infrequently use cannabis: a crossover trial. JAMA Netw Open. 2018;1((7)):e184841–41. doi: 10.1001/jamanetworkopen.2018.4841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vandrey R, Herrmann ES, Mitchell JM, Bigelow GE, Flegel R, LoDico C, et al. Pharmacokinetic profile of oral cannabis in humans: blood and oral fluid disposition and relation to pharmacodynamic outcomes. J Anal Toxicol. 2017;41((2)):83–99. doi: 10.1093/jat/bkx012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rong C, Carmona NE, Lee YL, Ragguett RM, Pan Z, Rosenblat JD, et al. Drug-drug interactions as a result of co-administering Δ9-THC and CBD with other psychotropic agents. Expert Opin Drug Safety. 2018;17((1)):51–4. doi: 10.1080/14740338.2017.1397128. [DOI] [PubMed] [Google Scholar]
- 50.Morrison G, Crockett J, Blakey G, Sommerville K. A phase 1, open-label, pharmacokinetic trial to investigate possible drug-drug interactions between clobazam, stiripentol, or valproate and cannabidiol in healthy subjects. Clin Pharmacol Drug Dev. 2019;8((8)):1009–31. doi: 10.1002/cpdd.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Broderman M. Pain, pleasure and placebo: the cannabinoids in reward processing and the perception of pain. Ment Health Addict Res. 2016;1((3)):59–63. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Data Availability Statement
The data that support the findings of this study are not publicly available. The data are contained within patient records that are securely stored for access by CAC staff and researchers only. Further enquiries can be directed to the corresponding author.