Abstract
Objective
Inequities in access to health care contribute to persisting disparities in health care outcomes. We constructed a geographic information systems analysis to test the association between income and access to the existing health care infrastructure in a nationally representative sample of US residents. Using income and household size data, we calculated the odds ratio of having a distance > 10 miles in nonmetropolitan counties or > 1 mile in metropolitan counties to the closest facility for low-income residents (i.e., < 200% Federal Poverty Level), compared to non-low-income residents.
Results
We identified that in 954 counties (207 metropolitan counties and 747 nonmetropolitan counties) representing over 14% of the US population, low-income residents have poorer access to health care facilities. Our analyses demonstrate the high prevalence of structural disparities in health care access across the entire US, which contribute to the perpetuation of disparities in health care outcomes.
Keywords: Health disparities, Low income, Health care access, Health care infrastructure
Introduction
Inequities in access to health care contribute to persisting disparities in health care outcomes. This has been highlighted by the Coronavirus Disease 2019 (COVID-19) pandemic, which has disproportionately affected racial and ethnic minority groups and socially disadvantaged communities. Income disparities in access to health care and health outcomes have been widely documented over the decades [1–3]. Previous studies have also demonstrated that low spatial access to care was associated with poor health care and outcomes [4]. However, there is little evidence to address whether income disparities in spatial access to health exist across the US counties. We therefore constructed a geographic information systems analysis to test the association between income and access to the existing health care infrastructure in a nationally representative sample of US residents.
Main text
Materials and methods
We obtained addresses of rural health centers and hospital outpatient departments from the Centers for Medicare and Medicaid Services, of community pharmacies from the National Council for Prescription Drug Programs, and of federally qualified health centers from the Health Resources and Services Administration. The US population was characterized with the 2010 US Synthetic Population by RTI International.
We used ArcGIS Network Analyst and the US Geological Survey National Transportation Dataset [2] to estimate the driving distance to the closest facility for a 1% sample of the population, as previously described. [3] Using income and household size data, we calculated the odds ratio of having a distance > 10 miles in nonmetropolitan counties or > 1 mile in metropolitan counties to the closest facility for low-income residents, compared to non-low-income residents. Low income was defined as household income < 200% Federal Poverty Level [4]. The 1 mile cutoff in metropolitan counties and 10 miles cutoff in nonmetropolitan counties were selected based on definitions of food deserts by US Department of Agriculture [5]. Metropolitan and nonmetropolitan counties were classified following the National Center for Health Statistics Urban–Rural Classification Scheme for Counties [5].
Results
Among 2,982,544 residents in the national sample, 32.4% were categorized as low-income and 14.8% lived in nonmetropolitan counties. Approximately 75% of the nonmetropolitan county residents lived within 10 miles of a facility, and 53% of the metropolitan county residents lived within 1 mile of a facility.
Among 1166 metropolitan counties, we identified 43 counties where low-income residents had significantly higher odds of having a driving distance > 1 mile to the closest facility. In 164 additional metropolitan counties, low-income residents had a higher likelihood of having a driving distance > 1 mile to the closest facility, though not statistically significant. (Fig. 1A) The forementioned 207 metropolitan counties accounted for almost 27 million Americans. Table 1 lists the most populated metropolitan counties with significant disparities in access to health care facilities, including 6 counties in Texas.
Fig. 1.
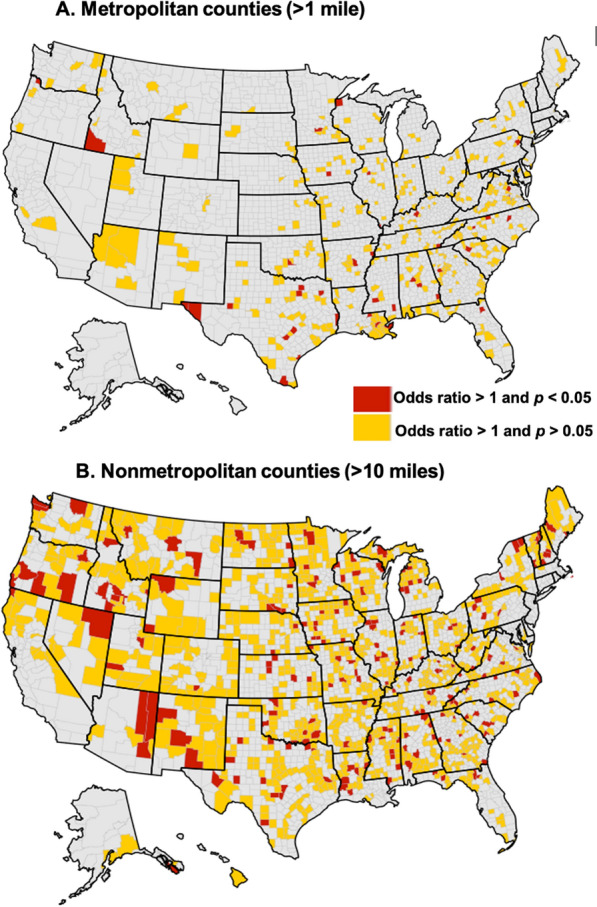
Metropolitan and nonmetropolitan Counties with Disparities in Access to Health Care Facilities. We calculated the odds of having a distance > 1 mile in metropolitan counties (A) or > 10 miles in nonmetropolitan counties (B) to the closest facility for low-income residents, compared to non-low-income residents. Low income was defined as household income < 200% Federal Poverty Level. Red indicates counties where disparities were significant at the p < 0.05 level and yellow indicate counties where disparities were non-significant at the p > 0.05 level. Grey indicates no disparity identified [7–11]
Table 1.
Metropolitan Counties with Significant Disparities in Access to Health Care Facilities at the 1 Mile Threshold
| County Name | State | Population | Proportion of non-low-income population with distance > 1 mi (%) | Proportion of low-income population with distance > 1 mi (%) | Odds ratio of distance > 1 mi for low-income vs. non-low-income |
|---|---|---|---|---|---|
| Dallas | Texas | 2,635,516 | 39 | 44 | 1.18 (1.12, 1.14) |
| Collin | Texas | 1,034,730 | 37 | 42 | 1.21 (1.07, 1.24) |
| San Francisco | California | 881,549 | 2 | 4 | 1.93 (1.43, 1.94) |
| Hidalgo | Texas | 868,707 | 60 | 67 | 1.35 (1.22, 1.34) |
| El Paso | Texas | 839,238 | 42 | 45 | 1.11 (1.02, 1.14) |
| Richmond | Virginia | 230,436 | 26 | 31 | 1.32 (1.08, 1.34) |
| Clay | Florida | 219,252 | 73 | 80 | 1.48 (1.14, 1.44) |
| Monroe | Pennsylvania | 170,271 | 81 | 86 | 1.41 (1.05, 1.44) |
| Guadalupe | Texas | 166,847 | 68 | 76 | 1.50 (1.12, 1.54) |
| Ector | Texas | 166,223 | 51 | 57 | 1.27 (1.02, 1.24) |
| Coweta | Gorgia | 148,509 | 76 | 83 | 1.49 (1.08, 1.44) |
| Hardin | Kentucky | 110,958 | 60 | 67 | 1.39 (1.05, 1.34) |
The table lists counties categorized as metropolitan by the National Center for Health Statistics Urban–Rural Classification Scheme for Counties, with a population of at least 10,000 people, and where low-income residents had a significantly higher risk of having a driving distance > 1 mile to the nearest health care facility, compared to non-low-income residents. Low income was defined as household income < 200% Federal Poverty Level. Counties were ranked by decreasing population
Among 1967 nonmetropolitan counties, we identified 205 counties where low-income residents had significantly higher odds of having a driving distance > 10 miles to the closest facility. In 542 additional nonmetropolitan counties, low-income residents had a higher likelihood of having a driving distance > 10 miles to the closest facility, though not statistically significant. (Fig. 1B) These forementioned 747 nonmetropolitan counties accounted for almost 20 million Americans.
Discussion
Our study has characterized income disparities in driving distance to health care facilities across the entire US. Our analyses demonstrate that in 954 counties (207 metropolitan counties and 747 nonmetropolitan counties) representing over 14% of the US population, low-income residents have poorer access to health care facilities. Our analyses demonstrate the high prevalence of structural disparities in health care access across the entire US, which contribute to the perpetuation of disparities in health care outcomes [1]. Although not the only type of obstacles to health care access, geographic barriers are particularly relevant for low-income populations because they are less likely to own a car and more likely to reside in areas with lower access to public transportation [6]. Investing in equitable health care access in the US should be a leading priority, particularly in the COVID-19 era.
Conclusion
Our analyses demonstrate the high prevalence of structural disparities in health care access across the entire US, which contribute to the perpetuation of disparities in health care outcomes.
Limitation
Non-significant disparities are presented because our 1% sampling of the US population may have resulted in under-power to detect disparities among nonmetropolitan counties at the statistical significance level.
Acknowledgements
None.
Abbreviation
- COVID-19
Coronavirus disease 2019
Author contributions
JG designed the study, executed the disparities analyses, and drafted the first draft of the manuscript. SD contributed to study design, obtaining funding, identification of facilities for inclusion in the study, and supervision of disparities analysis. LAB conceptualized of the study and was responsible for the acquisition of data and supervision of geographic information system analysis. ST contributed to the study design and executed the geographic information system analyses. URE contributed to the generation of the study question, study design, and drafting of the manuscript. CM contributed to study design and drafting of the manuscript. IH supervised the project and was responsible for obtaining funding, coordinating research efforts, and supervising analyses and manuscript writing. All authors read and approved the final manuscript.
Funding
This work was funded by the West Health Policy Center. Hernandez is funded by the National Heart, Lung and Blood Institute (grant number K01HL142847). The funder was involved in the design and conduct of the study, in the interpretation of results, and in the preparation and review of the manuscript. The funder was not involved in collection, management, or analysis of the data. The study was not submitted to the funder for approval, and the funder had no role in the decision to submit the manuscript for publication.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
Not applicable (no human subject or animal involved).
Consent for publication
Not applicable (Our analysis has not used an individual person’s data).
Competing interests
Hernandez has received consulting fees from Pfizer, outside of the submitted work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jingchuan Guo, Email: guoj1@ufl.edu.
Inmaculada Hernandez, Email: inhernandez@health.ucsd.edu.
Sean Dickson, Email: sdickson@westhealth.org.
Shangbin Tang, Email: shangbin.tang@pitt.edu.
Utibe R. Essien, Email: uessien@pitt.edu
Christina Mair, Email: cmair@pitt.edu.
Lucas A. Berenbrok, Email: berenbro@pitt.edu
References
- 1.Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Geological Survey. National Transportation Dataset (NTD)-ScienceBase-Catalog. https://www.sciencebase.gov/catalog/item/4f70b1f4e4b058caae3f8e16. Accessed March 31, 2021.
- 3.Berenbrok LA, Shangbin T, Kim CC, et al. Access to potential COVID-19 vaccine administration facilities: a geographic information systems analysis. West Health Institute. https://s8637.pcdn.co/wp-content/uploads/2021/02/Access-to-Potential-COVID-19-Vaccine-Administration-Facilities-2-2-2021.pdf. Published 2021.
- 4.US Department of Health and Human Services. Office of the Assistant Secretary for Planning and Evaluation. 2010 HHS Poverty Guidelines. https://aspe.hhs.gov/2010-hhs-poverty-guidelines. Accessed 31 Mar 2021.
- 5.National Center for Health Statistics. Urban Rural Classification Scheme for Counties. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Accessed 7 Jan 2021.
- 6.2009 National Household Travel Survey. Mobility Challenges for Households in Poverty. https://nhts.ornl.gov/briefs/PovertyBrief.pdf. Accessed 31 Mar 2021.
- 7.Chokshi DA. Income, poverty, and health inequality. JAMA. 2018;319(13):1312. doi: 10.1001/jama.2018.2521. [DOI] [PubMed] [Google Scholar]
- 8.Kanter GP, Segal AG, Groeneveld PW. Income disparities in access to critical care services. Health Aff (Millwood) 2020;39(8):1362–1367. doi: 10.1377/hlthaff.2020.00581. [DOI] [PubMed] [Google Scholar]
- 9.McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. 2020;8:231. doi: 10.3389/fpubh.2020.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016;6(11):e013059. doi: 10.1136/bmjopen-2016-013059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Characteristics and Influential Factors of Food Deserts [Internet]. https://www.ers.usda.gov/publications/pub-details/?pubid=45017. Accessed 15 Apr 2022
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


