Abstract
This perspectives piece focuses on the detrimental cost of ignoring vaccines and refusing vaccination against COVID-19 in the United States. Much of the existing literature regarding the consequences of the unvaccinated emphasizes the impact to population health; however, few academic articles have explored the burden the unvaccinated pose to various sectors of society. This paper analyzes the impact that the unvaccinated have on healthcare systems, the US economy, and global health. Throughout the COVID-19 pandemic, unvaccinated populations were found to have put significant strain on healthcare systems, depleting medical resources and contributing to high rates of healthcare worker shortages. Furthermore, research suggests that between November and December 2021, over 692,000 preventable hospitalizations occurred in unvaccinated individuals, costing the US economy over $13.8 billion. Lastly, it is proposed that the strong international presence of the US, when coupled with high levels of disease transmissibility in the unvaccinated, provides a significant threat to global health. In conclusion, the unvaccinated have caused impacts far beyond that of population health; they have also posed a burden to healthcare systems, the economy, and global public health.
Keywords: public health, COVID-19, vaccination, immunization, COVID-19 vaccine, unvaccinated, cost, burden, economic impact, global public health
Introduction
Roughly 24 months since its initial emergence and numerous variants later, the world is still held captive by the COVID-19 pandemic. COVID-19, having permeated nearly all aspects of society and having ravaged our world for over 2 years, has infected over 455 million people and claimed 6 million lives [1]1. In September 2020, it surpassed the number of fatalities resulting from the 1918 influenza and became the deadliest pandemic in the US [2]. Fortunately, the introduction of the COVID-19 vaccine in late 2020 has led to subsiding infection rates [3]. With the vaccine having been deemed the most effective tool in combatting the spread of COVID-19, there has been a national push for widespread immunization throughout the country [4]. Despite these efforts, however, many individuals have refrained from receiving the COVID-19 vaccine, with the collective refusal to be vaccinated having negative ramifications on society. The vast majority of cases, hospitalizations, and deaths related to COVID-19 are among unvaccinated individuals [5]2. Consequently, the current rhetoric regarding COVID-19 vaccines has largely focused on how unvaccinated populations have directly affected population health. However, there has been less discussion on how the hesitation or refusal to be vaccinated against COVID-19 has broader societal impacts. Therefore, this begs the question: beyond the detrimental effect to population health, what is the cost of ignoring vaccines and remaining unvaccinated?
Resource Impacts
It has been well-established that those unvaccinated against COVID-19 are significantly more likely to risk hospitalization and death compared to those who are vaccinated, with research estimating that unvaccinated individuals are between 10-15 times more likely to be hospitalized compared to those who are vaccinated [6,7]. With significantly higher hospitalization rates among the unvaccinated, research has aimed to measure the impacts that unvaccinated populations have had on health systems. Research published by the Kaiser Family Foundation found that between June and November 2021, there were 692,000 preventable COVID-19 hospitalizations among unvaccinated adults [8]. These hospitalizations all required the expenditure of medical resources and healthcare personnel, taxing a healthcare system that was already over-burdened and impacting resource access.
The COVID-19 pandemic caused an unprecedented strain on our nation’s healthcare system, with the soaring number of COVID-19 hospitalizations causing supply and demand issues in the medical sector. As unvaccinated patients crowded hospitals, health facilities found themselves lacking enough resources to accommodate the number of patients [9]. Countless stories have emerged on how providing treatment to the unvaccinated was often to the detriment of other patients [9,10]. Hospitals have been overburdened to the point where patients arriving for non-COVID related issues are being transferred to hospitals in other states [10]. Patients in need of immediate operations have had to wait days to be seen by a doctor [10,11]. Hospitals have had to turn away cancer patients because there were no more hospital beds available in the facility [12]. One hospital was forced to dismiss a brain cancer patient because the hospital had reached maximum capacity, with 90% of beds having been taken by unvaccinated patients sick with COVID-19 [12]. Another hospital had to turn down a man experiencing a cardiac emergency, with doctors contacting 43 hospitals across three states in search of a facility that had the ability to take an extra patient. Not one of those hospitals had the capacity to treat him. The man died waiting for care [13].
Scarce healthcare resources are being utilized by a population that made the conscious decision to refuse the COVID-19 vaccine, yet seeks treatment when they fall victim to this same disease. Despite the morbid irony, however, the issue doesn’t lie in the fact that the unvaccinated were provided treatment; it lies in the fact that their treatment was often at the expense of those around them.
Economic Impacts
In addition to resource depletion, the unvaccinated have caused significant economic damage. Various studies indicate that the average COVID-19 hospitalization costs over $20,000 per patient [8]. Evidence suggests that average costs are much higher in patients that require prolonged hospitalization and extensive medical support, the majority of which are unvaccinated [14,15]. These costs are primarily supported by insurance companies and taxpayer dollars; the out-of-pocket costs for a COVID-19 hospitalization averages $3,800 for those with private insurance and $1,500 for those with Medicare [16]. Therefore, the burden of the unvaccinated is placed on the economy as a whole, including taxpayers, rather than the individuals incurring those costs. In the first comprehensive report estimating the financial burden of the unvaccinated, the Kaiser Family Foundation published research concluding that preventable hospitalizations among the unvaccinated had cost over $13.8 billion between June and November 2021 [8].
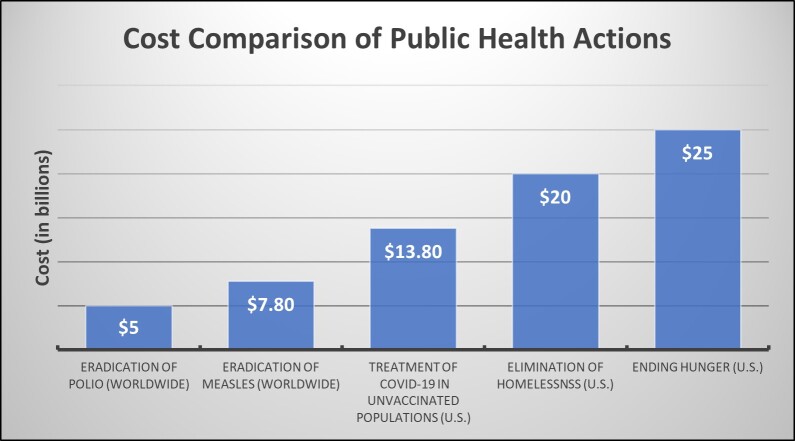
In an attempt to grasp the enormity of this economic impact, I compared the cost of treating preventable COVID-19 hospitalizations in unvaccinated patients to the estimated costs of addressing various public health issues. As Figure 1 demonstrates, preventable COVID-19 hospitalizations among the unvaccinated were more costly than the estimated cost of eradicating polio and measles worldwide, and is comparable to the estimated cost of eliminating homelessness and hunger, respectively, in the US [17-20]. Furthermore, in highlighting the relative comparability of these costs, it is crucial to acknowledge that the multi-billion dollar cost of treating the unvaccinated for a 6-month period rivals the costs of eliminating and eradicating public health issues that have existed for decades.
Figure 1.
The estimated costs of addressing various public health issues and how they compare to the costs of treating COVID-19 hospitalizations among unvaccinated populations between June and November 2021.
Global Health Impacts
The United States has accounted for a significant portion of COVID-19 cases worldwide, with over 79 million COVID-19 cases deriving from the US [1]. Despite constituting approximately 4% of the world’s population, the US accounts for over 17% of COVID-19 cases globally [1]. Table 1 depicts the ten countries with the highest number of COVID-19 infections to date. Table 1 also explores each country’s total number of COVID-19 cases as a percent representative of COVID-19 cases worldwide, calculated by dividing each’s country’s total number of COVID-19 cases by the total number of COVID-19 cases globally [1]. Additionally, the table includes the percent of fully vaccinated citizens in each country, defined as having received one dose of the Johnson & Johnson vaccine or two doses of the Pfizer or Moderna vaccine, respectively. Among the countries with the highest number of COVID-19 cases, the US has one of the lowest vaccination rates and is one of only two high-income countries with national vaccination rates below 70% [1].
Table 1. COVID-19 Case Totals Among Ten Countries, Along with a Calculated Percent Estimate Representative of Each Country’s Total Number of Infections Relative to the Total Number of Global COVID-19 Infections.
| Countries with the Highest Number of COVID-19 Infections | ||||
| Country | Fully vaccinated | Total COVID-19 Cases | Percent of World’s COVID Cases | |
| 1 | United States | 66.0% | 79,517,492 | 17.40% |
| 2 | India | 59.3% | 42,990,991 | 9.41% |
| 3 | Brazil | 74.7% | 29,361,024 | 6.43% |
| 4 | France | 78.1% | 23,565,274 | 5.16% |
| 5 | United Kingdom | 73.6% | 19,673,347 | 4.31% |
| 6 | Germany | 75.7% | 17,202,756 | 3.77% |
| 7 | Russia | 50.0% | 17,040,721 | 3.73% |
| 8 | Turkey | 63.4% | 14,534,239 | 3.18% |
| 9 | Italy | 79.1% | 13,323,179 | 2.92% |
| 10 | Spain | 84.6% | 11,223,974 | 2.46% |
With comparatively low vaccination rates, the US poses a serious threat to global health. COVID-19’s infectious nature is exacerbated by the unvaccinated, who have higher levels of disease transmissability compared to vaccinated populations [21]. COVID-19 transmissibility in the US is especially problematic given the country’s robust international presence. The US has the second highest amount of international tourism, with over 166 million people having visited in 2019 [22]. The US is also the largest trading nation in the world, with trade agreements in over 200 regions and countries [23]. Consequently, the US’ identity as an integral player in the global community plays a large role in global health, with the likelihood that if an infectious disease is pervasive throughout the US, the disease is also rampant in other parts of the world given the US’ strong involvement in international affairs. This relationship magnifies the far-reaching impacts of the unvaccinated, whose comparatively higher rates of disease transmissability contribute to the rapid spread of disease on both a domestic and global scale [22].
Additional Healthcare Impacts
As someone with experience in immunization research and epidemiology vis-à-vis one of California’s COVID-19 Response Teams, I have seen both the benefit of immunizations and the detriment of remaining unvaccinated. Moreover, I understand that there are immeasurable costs resulting from communicable disease outbreaks. Unlike the hospitalization costs of the unvaccinated, certain consequences cannot be adequately quantified, including the widespread impact on healthcare workers.
In an effort to combat COVID-19, millions of healthcare workers across the country mobilized to provide care for their communities, working back-to-back shifts, tending to a number of patients that far exceeded hospital capacity, and risking exposure to a deadly disease every time they went to work. Under these unfathomable expectations, the healthcare sector saw skyrocketing burnout rates among employees, with 20% of healthcare workers having resigned within the first year after COVID-19 emerged [24]. Among the healthcare workers who remained in their jobs, roughly 80% noted that staffing shortages affected their ability to provide safe and adequate patient care [24]. Additionally, healthcare workers faced the threat of disease exposure, risking their lives to provide care for those unprotected against COVID-19. To date, more than 3,600 healthcare workers have died since treating COVID-positive patients [25]. Both the burnout rates and death rates compounded the shortage of healthcare workers in the country. These losses have forced health facilities to have to hire and train thousands of individuals to compensate for those impacted by COVID-19. Currently, there are no analyses that measure how burnout and staff shortages have affected healthcare workers and the patients to whom they provided care, or the costs associated with replacing healthcare workers.
Conclusion and Future Recommendations
I frequently ask myself, “at what cost?.” People are refusing to be vaccinated against COVID-19…and at what cost?
Unvaccinated individuals have caused an extensive burden on our healthcare system, cost the economy billions of dollars, and pose a significant risk to global health.
The discussion on how unvaccinated populations affected society primarily revolves around population health. Moving forward, however, it is essential to shift the narrative to include how resource access, the economy, and global health are impacted by unvaccinated populations as well. This shift in perspective is crucial, as many arguments in opposition to the COVID-19 vaccine claim that vaccination measures hinder the economy [26]. As discussed, research supports the opposite sentiment: unvaccinated populations have been directly correlated to–and responsible for–catastrophic blows to the US economy. Furthermore, politicians have claimed that getting vaccinated against COVID-19 has no far-reaching impacts beyond the vaccine recipient, despite the overwhelming evidence discrediting these statements [27]. Therefore, in discussing the widespread impacts of the unvaccinated, broadening the conversation to include topics beyond population health can help dispel the rampant amounts of misinformation and fraud arguments opposing the COVID-19 vaccine. It is not enough to look at how the unvaccinated have affected population health; in order to comprehend the extensive societal burden of the unvaccinated, we need to discuss the impacts to the healthcare system, the US economy, and global public health.
Glossary
- COVID-19
Coronavirus disease 2019
Footnotes
1All data collected referred to in the paper were up-to-date as of March 2022.
2Throughout this article, unvaccinated individuals refers to those who are 18 years of age or older and are eligible to receive the COVID-19 vaccine, but refrain from doing so based on non-medical reasons.
References
- COVID-19 Dashboard [Internet]. Johns Hopkins Coronavirus Resource Center. 2020. January–. Available from: https://coronavirus.jhu.edu/map.html
- McKeever A. COVID-19 surpasses 1918 flu as deadliest pandemic in U.S. history [Internet]. 2021. September. Available from: https://www.nationalgeographic.com/history/article/covid-19-is-now-the-deadliest-pandemic-in-us-history
- Approves First FD. COVID-19 Vaccine [Internet]. U.S. Food and Drug Administration. 2021. August. Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-covid-19-vaccine
- President Biden Announces New Actions to Protect Americans Against the Delta and Omicron Variants as We Battle COVID-19 this Winter [Internet]. 2021. December 2. Available from: https://www.whitehouse.gov/briefing-room/statements-releases/2021/12/02/fact-sheet-president-biden-announces-new-actions-to-protect-americans-against-the-delta-and-omicron-variants-as-we-battle-covid-19-this-winter/
- Scobie HM, Johnson AG, Suthar AB, Severson R, Alden NB, Balter S, et al. Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status - 13 U.S. Jurisdictions, April 4-July 17, 2021. MMWR Morb Mortal Wkly Rep. 2021. Sep;70(37):1284–90. 10.15585/mmwr.mm7037e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Cases, Hospitalizations, and Deaths by Vaccination Status [Internet]. Washington State Department of Health. 2022. March 2. Available from: https://doh.wa.gov/sites/default/files/2022-02/421-010-CasesInNotFullyVaccinated.pdf
- Millman J. Omicron Breakthrough Infections Soar, But Unvaccinated Far More Likely to Be Hospitalized – NBC New York [Internet]. NBC4. 2022. January 3. Available from: https://www.nbcnewyork.com/news/coronavirus/ny-covid-hospitalizations-top-2021-surge-levels-as-omicron-drives-95-of-cases/3476250/
- Amin K, Cox C. Unvaccinated COVID-19 hospitalizations cost billions of dollars - Peterson-KFF Health System Tracker [Internet]. Peterson-KFF Health System Tracker. 2021. December 22. Available from: https://www.healthsystemtracker.org/brief/unvaccinated-covid-patients-cost-the-u-s-health-system-billions-of-dollars/
- Boone R. COVID-19 surge forces health care rationing in parts of West [Internet]. AP News. 2021. September 16. Available from: https://apnews.com/article/health-public-health-coronavirus-pandemic-idaho-a0729894b42af1c3dadeccaffeabea0c
- Heim M, Eilbert N. ‘We’re paralyzed’: Wisconsin hospitals struggle to transfer and place new patients [Internet]. Appleton Post-Crescent. 2021. December 3. Available from: https://www.postcrescent.com/story/news/2021/12/03/covid-wisconsin-hospitals-turning-away-patients-cases-climb-staffs-struggle/8855404002/
- Abelson R. Covid Overload: U.S. Hospitals Are Running Out of Beds for Patients [Internet]. New York Times. 2020. Apr 19. Available from: https://www.nytimes.com/2020/11/27/health/covid-hospitals-overload.html
- Paryani N. Opinion: Unvaccinated covid patients are straining hospitals like mine, where I had to turn a cancer patient away [Internet]. The Washington Post. 2021. August 21. Available from: https://www.washingtonpost.com/opinions/2021/08/21/how-unvaccinated-pandemic-threaten-everyones-health/
- Bella T. Alabama man dies after being turned away from 43 hospitals as covid packs ICUs, family says [Internet]. The Washington Post. 2021. September 12. Available from: https://www.washingtonpost.com/health/2021/09/12/alabama-ray-demonia-hospitals-icu/
- States by the Numbers. COVID-19 Cost Tracker [Internet]. FAIR Health. 2022.Available from: https://www.fairhealth.org/states-by-the-numbers/covid19-heatmap
- Griffin JB, Haddix M, Danza P, Fisher R, Koo TH, Traub E, et al. SARS-CoV-2 Infections and Hospitalizations Among Persons Aged ≥16 Years, by Vaccination Status - Los Angeles County, California, May 1-July 25, 2021 [Internet]. MMWR Morb Mortal Wkly Rep. 2021. Aug;70(34):1170–6. 10.15585/mmwr.mm7034e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Predict R. Out-of-Pocket Medical Bills for COVID-19 May Average $3,800 in 2021: Study [Internet]. U.S. News. 2021 October 18. Available from: https://www.usnews.com/news/health-news/articles/2021-10-18/out-of-pocket-medical-bills-for-covid-19-may-average-3-800-in-2021-study
- Levin A, Burgess C, Garrison LP Jr, Bauch C, Babigumira J, Simons E, et al. Global eradication of measles: an epidemiologic and economic evaluation. J Infect Dis. 2011. Jul;204 Suppl 1:S98–106. 10.1093/infdis/jir096 [DOI] [PubMed] [Google Scholar]
- How Much Would It Cost To End Homelessness In America? [Internet]. Roots Community Health Center. 2021. April 9. Available from: https://rootsclinic.org/how-much-would-it-cost-to-end-homelessness-in-america/
- Team G, Forest N, Team G, Sirafi A. How Much Would It Cost To End World Hunger? [Internet]. GlobalGiving. 2021. March 1. Available from: https://www.globalgiving.org/learn/how-much-would-it-cost-to-end-world-hunger/
- Mandavilli A. A Multibillion-Dollar Plan to End Polio, and Soon [Internet]. New York Times. 2021. June 9. Available from: https://www.nytimes.com/2021/06/09/health/polio-eradication-plan.html
- Science Brief. COVID-19 Vaccines and Vaccination [Internet]. Centers for Disease Control and Prevention. 2021. September 15. Available from: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html [PubMed]
- Roser M. Tourism [Internet]. Our World in Data. n.d. Available from: https://ourworldindata.org/tourism
- Countries & Regions [Internet]. United States Trade Representative. Available from: https://ustr.gov/countries-regions
- Levine DU. Faces Crisis of Burned-Out Health Care Workers [Internet]. U.S. News. 2021. November 15. Available from: https://www.usnews.com/news/health-news/articles/2021-11-15/us-faces-crisis-of-burned-out-health-care-workers
- Spencer J, Jewett C. 12 Months of Trauma: More Than 3,600 US Health Workers Died in Covid’s First Year [Internet]. Kaiser Health News. 2021. April 8. Available from: https://khn.org/news/article/us-health-workers-deaths-covid-lost-on-the-frontline/
- DeSantis R. @GovRonDeSantis [Internet]. Twitter. 2021. October 5. Available from: https://twitter.com/govrondesantis/status/1452626615599517706
- Blake A. Ron DeSantis and the worst fallacy about vaccine skepticism [Internet]. The Washington Post. 2021. [cited 2022 Apr 20]. Available from: https://www.washingtonpost.com/politics/2021/09/07/ron-desantis-worst-fallacy-about-vaccine-skepticism/