Abstract
This study aimed to investigate the association between adult food insecurity (FI) and symptoms of generalized anxiety disorder (GAD) and major depressive disorder (MDD) in two Brazilian cities during the coronavirus disease (COVID-19) pandemic. This study used data derived from a cross-sectional survey of 1693 adults. Interviews were conducted using an electronic questionnaire. The FI was measured using the Brazilian Food Insecurity Scale. The Generalized Anxiety Disorder-7 was used to measure the symptoms of GAD. The Patient Health Questionnaire-9 was used for MDD symptoms. The association between FI, GAD, and MDD symptoms was investigated using a Poisson regression model with robust variance to estimate the prevalence ratio and 95% confidence interval (95% CI). In regression models, a linear association between FI levels and outcomes was observed, with severe food insecurity having a 3.56 higher prevalence of GAD symptoms (95% CI: 2.23, 5.68) and a 3.03 higher prevalence of MDD (95% CI: 1.55, 5.90). In the stratified analyses, worse results were observed for females and males, individuals with non-white race/skin color, those without children, and those with lower monthly family income. In conclusion, the FI was associated with symptoms of GAD and MDD, and the sociodemographic characteristics interfered in this association. Therefore, we recommend the improvement of public health and social protection policies for food-insecure people.
Keywords: Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), Anxiety, Depression, Food Insecurity, COVID-19
Abbreviations: FI, Food Insecurity; GAD, Generalized Anxiety Disorder; MDD, Major Depressive Disorder
Highlights
-
•
FI was consistently associated with symptoms of GAD and MDD during the pandemic.
-
•
FI is linearly associated with anxiety and depression symptoms.
-
•
Participants at any FI level had more negative feelings (e.g., depressed mood).
-
•
The mental health impact of FI is sensitive to sociodemographic characteristics.
-
•
The results obtained may contribute to the cross-cultural consistency of the theme.
1. Introduction
The complex scenario of coping with the coronavirus disease (COVID-19) pandemic poses a huge challenge to epidemiological surveillance and public policy management (Fang et al., 2021). The World Health Organization (WHO) recommended various measures to curb the disease proliferation, including personal protective measures (e.g., hand hygiene) and physical distancing measures (e.g., isolation of cases and quarantine). Furthermore, lockdown or shutdown measures were implemented, resulting in movement restrictions, geographical area quarantines, school closures, and international travel restrictions (WHO - World Health Organization, 2020a). Moreover, the continued COVID-19 pandemic has caused the closure of work-posts, layoffs, and reduced working hours, directly affecting monthly family income (Prochazka et al., 2020) and access to essential supplies (Fang et al., 2021).
In Brazil, omissions and delays in applying specific interventions within the scope of public health policies to contain the disease may have contributed to an increase in infection and death rates (Mundt, 2021). These events had devastating impacts on the economy and exacerbated the extant food and nutrition insecurity in Brazil (Costa et al., 2021). Increased unemployment rates and inflation, which mainly affects food items, have caused many families to experience food insecurity (FI) (Costa et al., 2021). FI is defined as a lack of physical, social, economic, and regular access to food, with insufficient quality and quantity to meet the nutritional needs of individuals and populations (FAO, 2021; HLPE - Panel of Experts on Food Security and nutrition, 2020a; Pourmotabbed et al., 2020).
The Brazilian Food Insecurity Scale (EBIA) is the primary tool used to assess FI in Brazil (Reichenheim et al., 2016; Salles-Costa et al., 2022). This tool measures the experience of food insecurity based on anxiety or doubt about the future availability of food, damage to the quality and quantity of food, and the impossibility of acquiring food due to a lack of money (Salles-Costa et al., 2022). FI is a growing problem in many countries and reflects the deterioration of the improvement the population nutrition achieved over the past few years (FAO et al., 2021). Moreover, the experience of hunger was already increasing globally even before the COVID-19 pandemic impacted the economy, the reduction in family income, and the supply chain (FAO et al., 2021). The same occurs in Brazil, where a recent study on trends and disparities in severe Food Insecurity reported that severe FI increased from 2013 to 2018 and was experienced by over 1 million new households in 2018 (Salles-Costa et al., 2022).
FI can impact nutritional status, and can lead to psychological suffering owing to the inability to feed oneself and one's family (Pourmotabbed et al., 2020). FI adversely impacts mental health and increases the occurrence of symptoms of generalized anxiety disorder (GAD) and symptoms of major depressive disorder (MDD) (Pourmotabbed et al., 2020). Furthermore, deficiency in nutrient intake as a result of FI (Jomaa et al., 2017; Kirkpatrick & Tarasuk, 2008) can negatively impacts brain functionality and compromise cognition and emotions (Lachance & Ramsey, 2015; Ximenes-da-Silva & Guedes, 2020).
Due to COVID-19, MDD cases increased by 27.6%, while GAD cases increased by 25.6% globally, according to a systematic review (Santomauro et al., 2021). GAD and MDD are associated with changes in mood, disposition, emotions, and way of life in the general population, and have multifactorial causality (Pourmotabbed et al., 2020). Both are disabling disorders that often occur simultaneously (Goodwin & Stein, 2021). GAD is characterized by excessive preoccupation with various events, unrest, tension, and irritability. MDD is characterized by loss of interest and pleasure in performing activities, fatigue, difficulty concentrating, insomnia or excessive sleepiness, and suicidal ideation (Goodwin & Stein, 2021).
Considering the influence of mental health on quality of life (Rahman et al., 2021), it is critical to examine the association between FI and symptoms of GAD and MDD during the COVID-19 pandemic period. This is especially true because it is difficult to monitor the number of GAD and MDD diagnoses due to the lower use of health services by the population. Given the above, this study aimed to (1) analyze potential associations between FI and GAD symptoms and MDD, and (2) compare the potential associations of sociodemographic factors such as sex, race/skin color, having children, and the financial impact of COVID-19.
We hypothesized that there would be a positive association between the severity of food insecurity and symptoms of GAD and MDD and that sociodemographic factors could influence this association. Our hypothesis was based on the following findings: first, females have been described as more vulnerable to poor or fair mental health in relation to FI (Pound & Chen, 2021). Second, differences in race/skin color are associated with a lack of access to culturally appropriate food and services; higher rates of precarious employment and unemployment; and other factors that affect events related to health and well-being, such as FI and access to health services (Odoms-Young, 2018, Hernandez, L. O., Ayala-Guzman, 2022). Third, there is a lower prevalence of food security in households with children (IBGE - Instituto Brasileiro de Geografia e Estatística, 2020b, IBGE - Instituto Brasileiro de Geografia e Estatística. Coordenação de Trabalho e Rendimento; Rio de Janeiro, 2020a; Paquin et al., 2021), which can subsequently impact parental mental health due to their inability to provide food for their children (Fang et al., 2021; Pourmotabbed et al., 2020). Finally, low-income households are particularly vulnerable to FI during the COVID-19 pandemic (Leddy et al., 2020). Moreover, financial losses can also contribute to mental disorders (Fang et al., 2021).
Additionally, there is little evidence of an association between FI and mental health in stressful contexts, such as the COVID-19 pandemic (Fang et al., 2021; Polsky & Gilmour, 2020; Sundermeir et al., 2021), especially in Brazil (Santos et al., 2021). Therefore, including these variables in this study's analyses is justified by the intensification of inequalities during the COVID-19 pandemic, and the interdependence between sociodemographic characteristics and FI (Tarasuk, St-Germain, & Mitchell, 2019) and mental disorders (Cheah et al., 2020).
2. Methods
This cross-sectional study was part of a study entitled “Epidemiological surveillance of COVID-19 in the Inconfidentes Region/MG” (COVID-Inconfidentes Project).
2.1. COVID-Inconfidentes Project
The COVID-Inconfidentes Project was a household seroepidemiological survey conducted in the cities of Ouro Preto and Mariana in the Quadrilatero Ferrífero region of southeastern Brazil. The study was conducted in three stages between October and December 2020.
This is a population survey with a probabilistic sample. The sample size calculation was based on the 2010 population estimate (IBGE, 2013) for each city, 95% confidence level, design effect equal to 1.5, estimated proportion of infection, and precision. In addition, for each city, a 20% recomposition percentage was added to the sample size, considering the potential losses.
A three-stage conglomerate sampling design was adopted: census sector, household, and resident to be interviewed. These were selected through probability proportional to the number of households, systematic sampling, and by drawing lots, respectively. To ensure the representativeness of the different socioeconomic levels of the sample, strata were defined according to the average monthly income available in the 2010 census for each city (IBGE, 2013).
The inclusion criteria for the study were adults (aged 18 years and older) with permanent residence in the urban areas of Ouro Preto and Mariana, cognitive ability, and venous access for serological testing. The exclusion criteria were individuals under 18 years old, residents of social centers and long-stay institutions, quarantine due to current diagnosis of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection, cognitive impairment, and infeasibility of collecting blood samples due to difficult venous access.
During the collection period, 5252 households were approached. A total of 1789 randomly selected participants agreed to participate in the survey.
2.2. Data collection
Participant data were obtained through interviews conducted by trained interviewers, who administered a questionnaire on an electronic device in the Data Goal® applicative. Questionnaire was constructed based on previously validated tools. Participants completed a Portuguese structured questionnaire with closed and open-ended questions about sociodemographic characteristics, life habits and health behaviors, health conditions and food intake. Furthermore, blood was collected through venipuncture for laboratory tests for SARS CoV-2 infection and other biochemical analyses. Although data were collected face-to-face, all recommendations of the national protocols to curb the spread of coronavirus were adopted, including the use of personal protection equipment.
A previous study by Meireles et al. (2021) provides detailed information about the methodology and questionnaire of the study.
2.3. Analytic sample
Individuals who did not respond to the questionnaire (n = 9), those with incomplete information on the scales evaluating the symptoms of GAD (n = 44) and MDD (n = 25), and those whose responses did not contain information for calculating sample weight (n = 18) were excluded from the study. Therefore, the final sample comprised 1693 participants.
2.4. Measures
2.4.1. Mental health
The symptoms of GAD and MDD were measured using the Generalized Anxiety Disorder 7-item (GAD-7) and Patient Health Questionnaire-9-item (PHQ-9) scales. The GAD-7 was validated in Brazilian adults in community settings by Moreno et al. (2016). It was also recently validated for adults in Brazil through the application of exploratory factor analysis by Monteiro et al. (2020). Moreover, Santos et al. (2013) validated the PHQ-9 in adults from the general population in Brazil. The respective scales estimate the presence of GAD symptoms and MDD through the sum of scores based on self-reports. The Likert scale includes questions regarding the symptoms of anxiety and depression in the last two weeks. Scores range from 0 to 3 points depending on the frequency of symptoms. A cut-off score of ≥10 was used to confirm the presence of symptoms of GAD and MDD (Kroenke et al., 2001; Spitzer et al., 2006).
2.4.2. Food insecurity
Food insecurity was measured using the Brazilian Food Insecurity Scale (EBIA), validated for the Brazilian population (Pérez-Escamilla & Segall-Corrêa, 2008; Salles- Costa et al., 2022). It is a psychometric scale that examines a family's access to food and assesses the perception and experience of hunger in the household during the previous three months. It used 14 closed questions with yes or no answers. Each positive (yes) and negative (no) answer was assigned a value of 1 and 0, respectively.
The EBIA analysis was performed through the sum of affirmative answers, followed by the classification of the FI severity. The categories were as follows: (1) food security: condition of regular and permanent access to food; (2) mild food insecurity: some uncertainty about access to food; (3) moderate food insecurity: quantitative reduction of food for the family; and (4) severe food insecurity: disruption of eating patterns and experience of hunger. This classification was based on the following cut-off points (IBGE - Instituto Brasileiro de Geografia e Estatística, 2020b, IBGE - Instituto Brasileiro de Geografia e Estatística. Coordenação de Trabalho e Rendimento; Rio de Janeiro, 2020a):
-
⁃
Household that scored zero: food security.
-
⁃
Households with residents over 18 years of age: 1 to 3 points for mild food insecurity, 4 to 5 points for moderate food insecurity, and 6 to 8 points for severe food insecurity.
-
⁃
Households with residents under the age of 18 years: 1–5 points for mild food insecurity, 6–9 points for moderate food insecurity, and 10–14 points for severe food insecurity.
2.5. Descriptive variables and covariates
Socioeconomic and demographic data were evaluated as covariates. Specifically, sex (dichotomous nominal variable - female, male); age (ordinal variable −18 to 34 years, 35–59 years, ≥ 60 years); race/skin color (dichotomous nominal variable - white or non-white); and having children under 18 years old (dichotomous nominal variable - yes, no). Education (ordinal variable - no schooling, ≤ 9 years of schooling, > 9 years of schooling); employment (dichotomous nominal variable - yes, no); the impact of the pandemic on family income (dichotomous nominal variable - no impact on income/had little impact/increased, has decreased a lot); the number of residents in the household (ordinal variable - ≤ 4, >4 and ≤10, >10); and marital status (dichotomous nominal variable - married, unmarried). Current family income was an ordinal variable categorized according to the number of minimum wages received (≤2 minimum wages, > 2 and ≤4 minimum wages, > 4 minimum wages). In Brazil, the minimum wage is the lowest salary that employers can legally pay to their employees and is used as a reference nationally.
Life habits, behaviors, and health conditions were also evaluated. Specifically, SARS-CoV-2 infection (dichotomous nominal variable - yes, no). Physical activity (dichotomous nominal variable - inactive, active); those who had at least 150 min per week of moderately intense physical activity or at least 75 min per week of vigorously intense physical activity were classified as active (WHO - World Health Organization, 2010). Smoking (dichotomous nominal variable - yes, no) and consumption of alcoholic beverages (dichotomous nominal variable - yes, no). Sun exposure was an ordinal variable (low, adequate, high), wherein sun exposure of fewer than 3 times a week or less than 20 min a week was considered low, exposure between 20 and 59 min for at least three times a week was classified as adequate, and exposure greater than or equal to 3 times a week with a duration greater than or equal to 60 min was considered high (Lee, Kim, & Lee, 2020; Lee et al., 2020). Finally, sleep quality was an ordinal variable, with scores from 0 to 4 indicating good sleep quality, scores from 5 to 10 indicating poor sleep quality, and scores above 10 indicating a sleep disorder (Bertolazi et al., 2009).
2.6. Statistical analysis
The collected data were subjected to consolidation and subsequent consistency analysis. To adjust the natural weights of the design and/or correction of problems caused by absence or refusal to answer, the sample weight was calculated. In this calculation, the probabilities of inclusion of the elements in the sample were analyzed, considering the probabilities of the census sector, the household, and an individual aged 18 years or older being drawn.
Pearson's chi-squared test was used to test the association between the two categorical variables. In this study, the symptoms of GAD and MDD were the dependent variables, and FI was the independent variable. To verify the association between the dependent and independent variables, Poisson regression with robust variance was used to determine the prevalence ratio (PR) and 95% confidence interval (95% CI). Covariates related to the dependent variables were used for adjustment purposes according to the literature (current family income) or bivariate analysis (sex, age, race/skin color, number of residents, and quality of sleep).
The estimates of PR for GAD symptoms and MDD were stratified by sex, race/skin color, having children, current family income, and financial impact of COVID-19. They were also adjusted to remove only stratification variables from each analysis. For this purpose, different FI levels were grouped (mild, moderate, severe), and food security was used as a reference category. Furthermore, an interaction analysis was conducted to investigate the interaction effect of sex and race/skin color with FI. These analyzes were based on data from the literature. FI acts in synergism with sex (Lee, Kim, & Lee, 2020) and race/skin color (Marin-Leon et al., 2011).
Statistical analyses were performed using STATA software (version 13.0; Stata Corporation, College Station, Texas, USA) with a statistical significance of 5%.
2.7. Ethical considerations
This study followed the guidelines and regulatory norms for research involving human subjects and the seroepidemiological investigation protocol for SARS-CoV-2 infection by the WHO (WHO, 2020b). Furthermore, the study was approved by the Research Ethics Committee of the Federal University of Minas Gerais (Protocol No. 4.135.077 and No.4.292.475), and all participants signed a free informed consent form.
3. Results
3.1. Sociodemographic characteristics
Most participants were female (51.1%), 35–59 years old (45.9%), and married (53.4%). Regarding race/skin color, 73.9% identified themselves as non-white. In addition, most participants reported having >9 years of schooling (70.1%), were employed (53.7%), and <4 residents in the household (76.3%).
3.2. Bivariate analysis
Among the 1693 participants who completed the questionnaire, 23.3% identified symptoms of GAD, and 15.6% identified MDD (Table 1).
Table 1.
- Sociodemographic characteristics, life habits, behaviors, and health conditions based on the presence of GAD symptoms and MDD, COVID-Inconfidentes Survey (2020).
| Variables | Total |
Generalized Anxiety disorder symptoms |
p-values* | Major depressive disorder symptoms |
p-values* | |||
|---|---|---|---|---|---|---|---|---|
| % | (95% CI) | Yes |
No |
Yes |
No |
|||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |||||
| Sex | ||||||||
| Female | 51.10 (43.82–58.33) | 64.10 (49.52–76.47) | 47.15 (40.11–54.31) | 0.010 | 74.88 (65.17–82.61) | 46.70 (38.88–54.68) | <0.001 | |
| Male | 48.9 (41.67–56.18) | 35.90 (23.53–50.48) | 52.85 (45.69–59.89) | 25.12 (17.39–34.83) | 53.30 (45.32–61.12) | |||
| Age (years) | ||||||||
| 18 - 34 | 36.52 (31.92–41.38) | 41.25 (28.74–55.01) | 35.09 (28.70–42.05) | 42.12 (29.96–55.31) | 35.49 (29.97–41.42) | |||
| 35 - 59 | 45.87 (41.34–50.47) | 49.76 (38.00–61.55) | 44.69 (38.22–51.34) | 0.126 | 47.15 (36.28–58.29) | 45.63 (40.37–51.00) | 0.219 | |
| ≥60 | 17.61 (14.46–21.28) | 8.98 (5.72–13.83) | 20.23 (16.42–24.65) | 10.74 (6.70–16.77) | 18.88 (15.06–23.40) | |||
| Race/skin color | ||||||||
| White | 26.10 (20.98–31.97) | 26.40 (17.89–37.13) | 26.01 (20.39–32.55) | 0.942 | 37.88 (25.52–52.03) | 23.91 (18.44–30.39) | 0.048 | |
| Non-white | 73.90 (68.03–79.02) | 73.60 (62.87–82.11) | 73.99 (67.45–79.61) | 62.12 (47.97–74.48) | 76.09 (69.61–81.56) | |||
| Education level (years of schooling | ||||||||
| No schooling | 1.53 (0.66–3.51) | 2.40 (0.56–9.79) | 1.27 (0.46–3.46) | 3.95 (1.04–13.85) | 1.09 (00.36–3.22) | |||
| ≤9 | 28.35 (23.82–33.37) | 22.18 (15.41–30.85) | 30.23 (23.84–37.49) | 0.329 | 23.24 (15.58–33.17) | 2.93 (24.08–35.12) | 0.185 | |
| >9 | 70.11 (65.15–74.64) | 75.42 (67.13–82.17) | 68.5 (6.14–74.83) | 72.82 (61.66–81.69) | 69.61 (63.78–74.88) | |||
| Work status | ||||||||
| Not Working/Housework | 46.34 (41.68–51.06) | 46.21 (35.06–57.74) | 46.38 (39.83–53.06) | 0.982 | 55.14 (43.99–65.80) | 44.71 (39.70–49.84) | 0.092 | |
| Currently Employed | 53.66 (48.94–58.32) | 53.79 (42.26–64.94) | 53.62 (46.94–60.17) | 44.86 (34.20–56.01) | 55.29 (50.16–60.30) | |||
| Family income" | ||||||||
| ≤2 minimum wages | 40.59 (35.20–46.21) | 34.26 (24.72–45.26) | 42.56 (35.17–50.29) | 38.42 (27.30–50.90) | 40.98 (35.00–47.24) | |||
| >2 to ≤ 4 minimum wages | 31.99 (26.81–37.64) | 32.78 (23.92–43.06) | 31.74 (26.50–37.49) | 0.420 | 29.6 (20.67–40.43) | 32.41 (26.72–38.68) | 0.665 | |
| >4 minimum wages | 27.42 (22.41–33.08) | 32.96 (19.71–49.60) | 25.70 (19.95–32.45) | 31.98 (21.06–45.30) | 26.61 (21.21–32.8) | |||
| Income during the pandemic | ||||||||
| No impact on income/had little impact/increased | 77.93 (73.17–82.06) | 75.55 (6.59–83.16) | 78.66 (73.55–83.01) | 0.480 | 76.94 (67.11–84.51) | 78.12 (72.82–82.62) | 0.809 | |
| Has decreased a lot | 22.07 (17.94–26.83) | 24.45 (16.84–3.41) | 21.34 (16.99–26.45) | 23.06 (15.49–32.89) | 21.88 (17.38–27.18) | |||
| Number of residents in the household | ||||||||
| ≤4 | 76.32 (71.19–80.78) | 70.21 (57.27–80.56) | 78.17 (73.13–82.49) | 67.98 (54.51–79.00) | 77.86 (72.92–82.12) | |||
| >4 to ≤ 10 | 23.16 (18.85–28.11) | 27.72 (1.81–39.95) | 21.78 (17.46–26.82) | 0.019 | 29.55 (19.35–42.30) | 21.98 (17.74–26.89) | 0.008 | |
| >10 | 0.52 (0.15–1.76) | 2.07 (0.56–7.39) | 0.05 (0.07–0.38) | 2.47 (0.52–10.84) | 0.16 (0.03–0.73) | |||
| Food insecuritya | ||||||||
| Food security | 62.48 (56.14–68.41) | 49.71 (38.05–61.40) | 66.35 (59.93–72.22) | 41.70 (30.22–54.16) | 66.32 (59.35–72.64) | |||
| Mild food insecurity | 34.56 (29.00–40.57) | 42.81 (32.51–53.78) | 32.05 (26.36–38.34) | <0.001 | 50.97 (39.11–62.72) | 31.52 (25.52–38.21) | 0.001 | |
| Moderate food insecurity | 2.22 (1.35–3.63) | 5.01 (2.61–9.41) | 1.37 (0.71–2.61) | 5.25 (2.67–10.07) | 1.66 (0.87–3.13) | |||
| Severe food insecurity | 0.75 (0.42–1.33) | 2.47 (1.22–4.95) | 0.23 (0.10–0.49) | 2.07 (0.88–4.78) | 0.5 (0.22–1.13) | |||
| Marital status | ||||||||
| Married | 53.41 (47.38–59.34) | 49.77 (37.92–61.64) | 54.51 (48.59–60.32) | 0.412 | 41.57 (30.71–53.31) | 55.60 (49.04–61.97) | 0.036 | |
| Unmarried | 46.59 (40.66–52.62) | 50.23 (38.36–62.08) | 45.49 (39.68–51.41) | 58.43 (46.69–69.29) | 44.40 (38.03–50.96) | |||
| SARS-CoV-2 infection | ||||||||
| No | 95.19 (93.57–96.42) | 95.02 (91.14–97.25) | 95.25 (93.53–96.53) | 96.42 (92.93–98.22) | 94.97 (93.06–96.37) | |||
| Yes | 4.81 (3.58–6.43) | 4.98 (2.75–8.86) | 4.75 (3.47–6.47) | 0.881 | 3.58 (1.78–7.07) | 5.03 (6.63–6.94) | 0.382 | |
| Physical activity levelb | ||||||||
| Active | 34.66 (27.42–42.69) | 35.01 (22.73–49.65) | 34.55 (27.92–45.85) | 0.936 | 29.53 (20.20–40.97) | 35.60 (27.39–44.76) | 0.386 | |
| Inactive | 65.34 (57.31–72.58) | 64.99 (50.35–77.27) | 65.45 (58.15–72.08) | 70.47 (59.03–79.80) | 64.40 (55.24–72.61) | |||
| Smoking | ||||||||
| No | 84.10 (79.54–87.70) | 86.42 (81.03–90.45) | 83.40 (78.04–87.65) | 0.315 | 82.22 (72.79–88.88) | 84.45 (79.32–88.49) | 0.614 | |
| Yes | 15.9 (12.20–20.46) | 13.58 (9.55–18.97) | 16.60 (12.35–21.96) | 17.78 (11.12–27.21) | 15.55 (11.51–20.68) | |||
| Physical activity levelb | ||||||||
| Active | 34.66 (27.42–42.69) | 35.01 (22.73–49.65) | 34.55 (27.92–45.85) | 0.936 | 29.53 (20.20–40.97) | 35.60 (27.39–44.76) | 0.386 | |
| Inactive | 65.34 (57.31–72.58) | 64.99 (50.35–77.27) | 65.45 (58.15–72.08) | 70.47 (59.03–79.80) | 64.40 (55.24–72.61) | |||
| Alcohol intake | ||||||||
| No | 40.77 (35.10–46,70) | 39.50 (29.76–50.14) | 41.16 (35.31–47.27) | 0.749 | 52.19 (39.47–64.64) | 38.66 (32.65–45.03) | 0.602 | |
| Yes | 59.23 (53.30–64.90) | 60.50 (49.86–70.24) | 58.84 (52.73–64.69) | 47.81 (35.36–60.53) | 61.34 (54.97–67.35) | |||
| Sun exposurec | ||||||||
| Low | 8.28 (6.38–10.69) | 4.02 (2.28–0.07) | 9.58 (7.19–56.47) | 0.064 | 4.58 (2.56–8.07) | 8.97 (6.78–11.77) | 0.166 | |
| Adequate | 52.55 (45.88–59.12) | 59.99 (46.37–72.22) | 50.29 (44.09–56.47) | 62.49 (49.14–74.17) | 50.71 (43.08–58.30) | |||
| High | 39.17 (32.43–46.35) | 35.99 (23.56–50.62) | 40.14 (34.30–46.26) | 32.93 (21,46–46.88) | 40.33 (32.67–48.49) | |||
| Sleep quality° | ||||||||
| Good | 47.03 (43.14–50.96) | 28.21 (15.90–44.96) | 52.75 (46.69–58.72) | 7.85 (4.68–12.89) | 54.28 (50.01–58.49) | |||
| Bad | 34.27 (30.01–38.79) | 41.60 (30.85–53.21) | 32.04 (25.77–39.04) | 0.014 | 46.57 (35.81–57.65) | 31.99 (27.24–37.15) | <0.001 | |
| Sleep disorder | 18.70 (14.95–23.13) | 30.19 (22.52–39.16) | 15.21 (11.33–20.12) | 45.58 (34.25–57.9) | 13.72 (10.32–18.02) | |||
Notes: * p-value from Pearson's chi-squared test. "Family income: minimum wage value (2020): BRL 1045.00 ≈ USD 194.25 (1 USD = 5.3797 BRL). a Food insecurity: scores = 0 food security (to all households), scores 1 to 3 = mild food insecurity, scores 4 to 5 = moderate food insecurity, scores 6 to 8 = severe food insecurity (to households with residents over 18 years); and scores 1 to 5 = mild food insecurity, scores 6 to 9 = moderate food insecurity, scores 10 to 14 = severe food insecurity (to households with residents under the age of 18 years); b Physical activity level - active: ≥150 min of moderate physical activity or≥75 min of vigorous physical activity (WHO - World Health Organization, 2010). c Sun exposure: low sun exposure = duration <20 min or frequency <3 times a week, adequate sun exposure = duration of 20–59 min and frequency≥3 times a week and high sun exposure = duration≥60 min or frequency ≥ 3 times a week. ° Sleep quality: scores of 0–4 = good sleep quality, scores of 5–10 = bad sleep quality and scores >10 = sleep disorder.
The prevalence of GAD symptoms was associated with the female sex (χ2 = 34.737, p = 0.010) and a greater number of residents in the household (χ2 = 30.723, p = 0.019). The prevalence of MDD was associated with female sex (χ2 = 70.916, p < 0.001), white race/skin color (χ2 = 22.204, p = 0.048), a greater number of residents in the household (χ2 = 31.086, p = 0.008), and the absence of a partner (χ2 = 17.639, p = 0.036). In addition, the presence of GAD symptoms and MDD was more frequent among participants who experienced some level of food insecurity in the household, and those with poor sleep quality or sleep disorders (Table 1).
Regarding FI, 37.5% of participants experienced some level of food insecurity (mild, moderate, or severe). Table 1 shows that 62.5%, 34.6%, 2.22%, and 0.8% of participants lived in a household that was food secure, mildly food insecure, moderately food insecure, and severely food insecure, respectively.
3.3. Multivariable models
In the multivariable model, FI levels were linearly associated with the dependent variables. Regarding the prevalence of GAD symptoms and MDD based on levels of food insecurity (Table 2), those who reported mild food insecurity (PR: 1.40, 95% CI: 1.05, 1.87), moderate food insecurity (PR: 2.61, 95% CI: 1.71, 4.00) and severe food insecurity (PR: 3.56, 95% CI: 2.23, 5.68) had a higher prevalence of GAD symptoms than those with food security.
Table 2.
– Estimate of the prevalence ratio of food insecurity according to the presence of symptoms of GAD and MDD, COVID-Inconfidentes Survey (2020).
| Generalized anxiety disorder |
p- values* | Major depressive disorder |
p- values* | |||
|---|---|---|---|---|---|---|
| PR | (95% CI) | PR | (95% CI) | |||
| Food security | 1 (Ref) | 1 (Ref) | ||||
| Mild food insecurity | 1.56 | (1.11–2.19) | 0.012 | 2.21 | (1.36–3.59) | 0.002 |
| Moderate food insecurity | 2.84 | (1.77–4.56) | <0.001 | 3.55 | (1.86–6.76) | <0.001 |
| Severe food insecurity | 4.14 | (2.93–5.87) | <0.001 | 4.15 | (1.91–9.01) | <0.001 |
| Adjustment 1 | ||||||
| Food security | 1 (Ref) | 1 (Ref) | ||||
| Mild food insecurity | 1.49 | (1.07–2.08) | 0.019 | 2.03 | (1.34–3.07) | 0.001 |
| Moderate food insecurity | 2.70 | (1.78–4.12) | <0.001 | 3.23 | (1.89–5.52) | <0.001 |
| Severe food insecurity | 3.56 | (2.64–4.79) | <0.001 | 3.14 | (1.42–6.94) | 0.005 |
| Adjustment 2 | ||||||
| Food security | 1 (Ref) | 1 (Ref) | ||||
| Mild food insecurity | 1.48 | (1.02–2.14) | 0.041 | 2.14 | (1.28–3.55) | 0.004 |
| Moderate food insecurity | 2.77 | (1.70–4.50) | <0.001 | 3.49 | (1.83–6.66) | <0.001 |
| Severe food insecurity | 3.99 | (2.75–5.78) | <0.001 | 4.05 | (1.92–8.56) | <0.001 |
| Adjustment 3 | ||||||
| Food security | 1 (Ref) | 1 (Ref) | ||||
| Mild food insecurity | 1.40 | (1.05–1.87) | 0.021 | 2.13 | (1.51–3.00) | <0.001 |
| Moderate food insecurity | 2.61 | (1.71–4.00) | <0.001 | 2.80 | (1.72–4.55) | <0.001 |
| Severe food insecurity | 3.56 | (2.23–5.68) | <0.001 | 3.03 | (1.55–5.90) | 0.001 |
Notes: *p-value from Poisson Regression with robust variance. Adjustment 1: sex; Adjustment 2: age (years); Adjustment 3: sex, age, race/skin color, number of residents in the household, sleep quality and family income. Food insecurity: scores = 0 food security (to all households), scores 1 to 3 = mild food insecurity, scores 4 to 5 = moderate food insecurity, scores 6 to 8 = severe food insecurity (to households with residents over 18 years); and scores 1 to 5 = mild food insecurity, scores 6 to 9 = moderate food insecurity, scores 10 to 14 = severe food insecurity (to households with residents under the age of 18 years).
Regarding MDD, those who reported mild food insecurity (PR: 2.13, 95% CI: 1.51, 3.00), moderate food insecurity (PR: 2.80, 95% CI: 1.72, 4.55), and severe food insecurity (PR: 3.03, 95% CI: 1.55, 5.90) had a higher prevalence of MDD than those with food security (Table 2). Additionally, there was an association between FI with emotions and self-perceived mental health conditions, as presented in Supplementary Material.
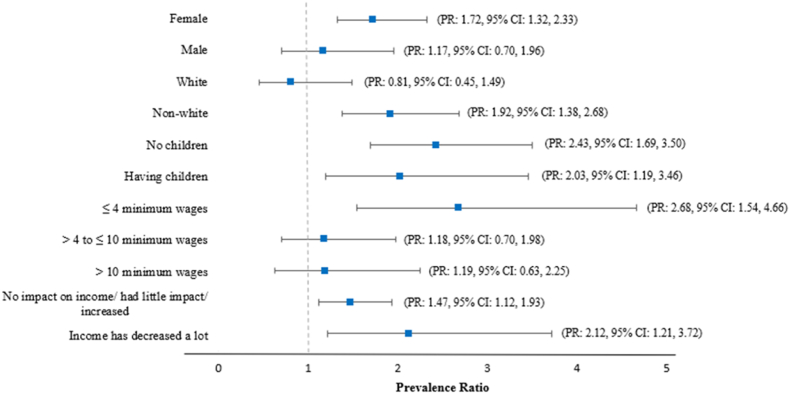
FI was associated with GAD symptoms among female participants, participants with non-white race/skin color, and those with a family income of ≤4 minimum wages. Moreover, the association between FI and GAD symptoms was not restricted to participants who had children or reduced family income during the pandemic (Fig. 1). When testing the interaction between FI and sex (PR: 0.66, 95% CI: 0.30, 1.44) and FI and race/skin color (PR: 1.97, 95% CI: 0.85, 4.55) with GAD symptoms, we did not observe any interaction between them.
Fig. 1.
Association of food insecurity with generalized anxiety disorder symptoms stratified by sex, race/skin color, having children or no children, current family income, and financial impact of COVID-19. COVID-Inconfidentes Survey (2020). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Note: Models adjusted for sex, age, race/skin color, number of residents in the household, sleep quality and family income. The stratification variable was removed from each analysis. Different FI levels were grouped (mild, moderate, severe), and food security was used as a reference category.
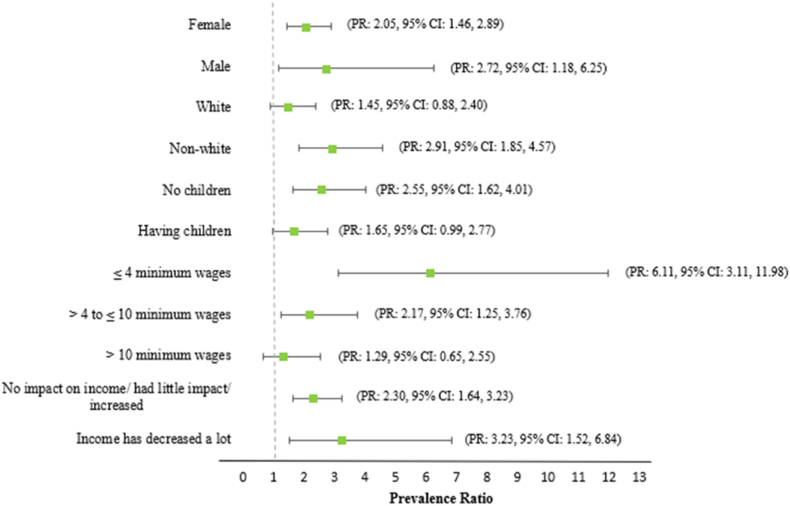
Concerning MDD, FI was associated with the prevalence among participants with non-white race/skin color, those who did not have children under the age of 18 years, and those with a family income of ≤10 minimum wages. The association between FI and MDD was not exclusive to those who had reduced family income during the pandemic, or to female participants. In our study, the strength of the association between FI and MDD was greater among males (PR: 2.72, 95% CI: 1.18, 6.25 vs PR: 2.05, 95% CI: 1.46, 2.89). Additionally, the strength of the association was greater among participants with a family income of ≤4 minimum wages (PR: 6.11, 95% CI: 3.11, 11.98) and among those whose family income was greatly reduced due to the pandemic (PR: 3.23, 95% CI: 1.52, 6.84) (Fig. 2). Similar to GAD, we did not observe the interaction between FI and sex (PR: 1.22, 95% CI: 0.37, 3.90) and between FI and race/skin color (PR: 2.34, 95% CI: 0.79, 6.89) with MDD.
Fig. 2.
Association of food insecurity with major depressive disorder symptoms stratified by sex, race/skin color, having children or no children, current family income, and financial impact of COVID-19. COVID-Inconfidentes Survey (2020). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Note: Models adjusted for sex, age, race/skin color, number of residents in the household, sleep quality and family income. The stratification variable was removed from each analysis. Different FI levels were grouped (mild, moderate, severe), and food security was used as a reference category.
4. Discussion
This study investigated the association between FI and symptoms of GAD and MDD in two Brazilian cities during the coronavirus disease (COVID-19) pandemic. The results suggest that FI during the pandemic was associated with symptoms of GAD and MDD. Regarding the study hypothesis, a positive association proportional to severity was observed between FI and GAD and MDD symptoms, which confirms previous findings that addressed the association between lack of food access and mental health deterioration (Fang et al., 2021; Polsky & Gilmour, 2020; Sundermeir et al., 2021). However, this study explored how the social and economic factors affect the association between FI and mental health. Given the above, specific results were observed for both sexes, individuals with non-white race/skin color, without children, and with lower monthly family income. Therefore, the findings from this study are consistent with prior research, and these results are important because they provide necessary information for the expansion and improvement of public health and social protection policies that promoting food security.
According to additional analyses (Supplementary Material), our results indicated that FI participants experienced more negative emotions, such as little interest or pleasure in performing activities, suicidal ideation, depressed mood or lack of perspective, sleep disturbances, trouble relaxing, and excessive worry. This is consistent with other studies (Jones, 2017). According to Jones (2017), FI is associated with higher and lower chances of experiencing negative and positive mental health conditions, respectively. For example, the higher prevalence of negative psychosocial conditions among these individuals may result in guilt, exclusion, difficulty in acquiring food, and feeling powerless regarding the challenging situation that they face (Pourmotabbed et al., 2020). This result supports the notion that FI is associated with mental disorders (Fang et al., 2021; Maynard et al., 2018).
Other aspects that increase the negative impact of FI on mental health are shame, uncertainty about food access; anxiety; and stigma associated with dependence on assistance programs, actions, or donations that condition access to food (Fang et al., 2021; Manfrinato et al., 2021). These are important factors for the occurrence of GAD symptoms and MDD (Fang et al., 2021). Consistent with this point, a cross-sectional study conducted in the United States among 2714 low-income respondents found a positive association between the receipt of charitable food and symptoms of mental disorders. Individuals who received this support were 39% and 37% more likely to have symptoms of anxiety and depression, respectively (Fang et al., 2021).
In addition to socioeconomic and psychosocial issues, FI can interfere with the nutritional status of individuals and with adequate nutrient intake (Jomaa et al., 2017; Kirkpatrick & Tarasuk, 2008). The impairment of adequate food intake can negatively interfere with brain activity because the brain has very high metabolic and nutrient demands to function (Camandola & Mattson, 2017; Lachance & Ramsey, 2015). This perspective enables us to understand the magnitude of the association between FI and GAD and MDD symptoms, which also comprise nutritional and physiological factors. Therefore, insufficient access to adequate quantity and quality of food can affect this association. Thus, public health measures should focus on improving food systems and access to food, especially for families living with low income or experiencing financial difficulties.
In the present study, when we conducted stratified analyses according to sociodemographic characteristics of the participants, we observed that FI had a stronger association with the prevalence of GAD and MDD symptoms. Overall, studies show that females are more likely than males to suffer from common mental disorders, such as anxiety and depression (Filgueiras & Stults-Kolehmainen, 2021; Otten et al., 2021; Schuch et al., 2014; WHO - World Health Organization, 2017). The observed association for females is complex and intertwined with their greater susceptibility to the social and economic consequences that have been exacerbated by the COVID-19 pandemic (Santomauro et al., 2021). Financial disadvantages can be produced by structural inequality between males and females, such as fewer stable jobs and lower wages (Santomauro et al., 2021). Women are thus vulnerable to the acquisition of adequate and healthy food and are more exposed to FI (Visser & Wangu, 2021).
Evidence indicates that the implications of FI on female mental health tend to be also more evident (Pound & Chen, 2021; Visser & Wangu, 2021). Although the reason for this is unclear, several factors may explain this point. First, the negative emotions of FI may be predominantly felt by females (Pound & Chen, 2021), who are commonly the primary caregivers and suppliers of food in their families (Pound & Chen, 2021; Visser & Wangu, 2021). Second, females commonly prioritize the supply of food to the family and consume smaller amounts of food (Visser & Wangu, 2021). This may trigger feelings of deprivation or restricted food choices, and incite psychological distress (Myers, 2020). Moreover, this period impacted the routine of females more, especially regarding the responsibilities of the home, caring for the family, sick relatives, and children – including monitoring school activities (Santomauro et al., 2021). With social restriction measures, there was also a substantial increase in domestic violence cases (Piquero et al., 2021), thus increasing the mental health burden.
Notably, males are more strongly affected by MDD in relation to FI. Although epidemiological studies show a lower prevalence of depression among males, the suicide rate, which is closely related to the severity of depression, is higher among males than females (Ridge et al., 2021). From this perspective, males tend not to report or to underestimate the symptoms of mental disorders and are less likely to access psychological therapies, leading to the underreporting of cases (Affleck et al., 2018). These data show a possible bias in the literature and legitimize the need to focus on prevention and promotion strategies in mental health according to sex. Equally, our results support that public policies aimed to FI should consider data disaggregated by sex (Botreau & Cohen, 2019).
The association observed for non-white race/skin color can be explained by social inequities and unequal access to health services, which is a historical problem (Odoms-Young, 2018). In Brazil, evidence indicates that differences perpetuate and continue to make black and pardo people vulnerable and marginalized regarding access to the labor market, cases of violence, income distribution, educational level, and housing conditions (IBGE, 2019). Additionally, structural racism and discrimination are associated with FI (Odoms-Young, 2018, Hernandez, L. O., Ayala-Guzman, 2022), which can exacerbate the deterioration of mental health. Therefore, the fight against social inequalities in Brazil needs to be studied in the formulation and implementation of public policies aimed at reducing discrepancies.
In the present study, an association between FI and MDD was observed among those who did not have children. According to data from a large national survey, the greatest vulnerability to FI is observed in households with children and/or adolescents (IBGE - Instituto Brasileiro de Geografia e Estatística, 2020b, IBGE - Instituto Brasileiro de Geografia e Estatística. Coordenação de Trabalho e Rendimento; Rio de Janeiro, 2020a). Thus, adults’ concern in providing food for their children can generate a greater psychological overload and favor the occurrence of mental disorders. Regarding our results, it is hypothesized that these childless individuals do not benefit from government programs to socially vulnerable families who have school-age children, such as “Bolsa Família” (Manfrinato et al., 2021) and food kits distributed during the pandemic with resources from the “Programa Nacional de Alimentação Escolar” (MAPA - Ministério da Agricultura Pecuária e Abastecimento; Ministério da Educação, 2020).
Finally, family income is an important predictor of material deprivation and FI, and symptoms of mental disorder are more pronounced in low-income families (Polsky & Gilmour, 2020). In the present study, we observed that there was an association between FI and symptoms of GAD and MDD even among families whose income was not impacted by the pandemic or whose income had increased. Although this result was unexpected, it is not surprising from the perspective of Brazilian economic scenario. Recently, inflation has skyrocketed, causing increases in the prices of fuel, electricity, cooking gas, and food – especially fresh products – the production of which is hampered by seasonal changes (Banco Central do Brasil, 2021). Therefore, although some families have related an increase in their monthly income, this adjustment was not proportional to the increase in inflation, and purchasing power was reduced throughout the Brazilian population (Costa et al., 2021; FAO et al., 2021).
This study had some limitations. First, its cross-sectional design did not allow for assessment of the causality of the observed associations. Residual confounding by unmeasured factors cannot be completely precluded, such as receiving benefits from assistance programs or receiving local government basic food baskets. In addition, health inequities in Brazil due to the social and environmental context and differences in the distribution of health resources among different population groups were not measured. However, several confounding factors associated with dependent variables were adjusted. Additionally, as this was a local study, these results may not represent the Brazilian reality in general, or that of other populations. However, considering that there are specific psychosocial stressors in each region (Jones, 2017), the results obtained in this study may contribute to the cross-cultural consistency of the theme.
We highlight that the data of the present study were derived from a population survey conducted during the pandemic, which is an important source of information on the sanitary situation and health determinants. Additionally, probabilistic sample selection and sample weight provided statistical power to the study, as well as internal and external validity.
5. Conclusion
The results of this study showed a positive association between FI during the pandemic and symptoms of GAD and MDD. Furthermore, individuals with non-white race/skin color, without children, and with a lower monthly family income showed stronger associations. The same was found for women in relation to GAD symptoms and MDD in men.
Measures aimed at reducing FI in Brazil must involve encouraging family farming, increasing social assistance and public policies for employment and income generation. In addition, the public policies to combat FI must be considered not only in the context of socioeconomic disparities and the human right to adequate food but also regarding the prevention of health problems, such as nutritional deficiencies and, as presented in this study, in relation to mental health. Therefore, we recommend the construction of coping actions for the insufficiency or lack of access to adequate food, the development of new screening methods, and the expansion and improvement of more targeted mental health care policies for food-insecure people. Moreover, longitudinal studies are needed to explore the consequences of FI on the development of GAD and MDD symptoms.
Author's contributions
Thaís S. Sabião - conception and study design; analysis and interpretation of data; writing the manuscript, critical review and final approval.
Raquel D. Mendonça - analysis and interpretation of data, critical review and final approval.
Adriana L. Meireles - conception and coordination of data collection, management of financial resources and final approval.
George L. L. Machado-Coelho - conception and coordination of data collection, critical review, management of financial, supervision and final approval.
Júlia C. C. Carraro - conception and study design, analysis and interpretation of data; critical review, supervision and final approval.
Grants and funding
This study was supported by the "Conselho Nacional de Desenvolvimento Científico e Tecnológico" (CNPq, Distrito Federal, Brazil) and "Coordenação de Aperfeiçoamento de Pessoal de Nível Superior" (CAPES), [Process n° 88887.504994/2020–01] and also included post-graduate scholarships - Funding Code: 001.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank the participants and volunteers of the COVID-Inconfidentes, Ouro Preto and Mariana City Halls, and Municipal Health Offices for the partnership, "Fundaçao de Amparo à Pesquisa do Estado de Minas Gerais" (FAPEMIG), CNPq, CAPES for financial support (Process: 88887.504994/2020–01), the Universidade Federal de Ouro Preto (UFOP) and the Research and Education Group in Nutrition and Collective Health (GPENSC) for their support and incentive. TS Sabião is grateful to the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) - Funding Code:001, for granting a scholarship and to thank Editage (www.editage.com) for English language editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101156.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Affleck W., Carmichael V., Whitley R. Men's mental health: Social determinants and implications for services. Canadian Journal of Psychiatry. 2018;63(9):581–589. doi: 10.1177/0706743718762388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banco Central do Brasil Inflation Report – December 2021. 2021. https://www.bcb.gov.br/en/publications/inflationreport/202112 Disponível em: 23,4.
- Bertolazi A.N., Fagondes S.C., Hoff L.S., Pedro V.D., Menna Barreto S.S., Johns M.W. Validação da escala de sonolência de Epworth em português para uso no Brasil. Jornal Brasileiro de Pneumologia. 2009;35:877–883. doi: 10.1590/s1806-37132009000900009. [DOI] [PubMed] [Google Scholar]
- Botreau h., Cohen m.J. 2019. Gender Inequalities and Food Insecurity: Ten years after the food price crisis, why are women farmers still food-insecure?. Oxfam Briefing Paper. [Google Scholar]
- Camandola S., Mattson M.P. Brain metabolism in health, aging, and neurodegeneration. EMBO Journal. 2017;36(11):1474–1492. doi: 10.15252/embj.201695810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheah Y.K., Azahadi M., Phang S.N., Abd Manaf N.H. Sociodemographic, lifestyle, and health factors associated with depression and generalized anxiety disorder among Malaysian adults. Journal of primary care & community health. 2020;11 doi: 10.1177/2150132720921738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa A.M., Rizzotto M.L.F., Lobato L.V.C. Hunger, unemployment, corruption, and preventable deaths: Faces of necropolitics. Saúde debate. 2021;45(130) [Google Scholar]
- Fang D., Thomsen M.R., Nayga R.M. The association between food insecurity and mental health during the COVID-19 pandemic. BMC Public Health. 2021;21(1):1–8. doi: 10.1186/s12889-021-10631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO - Food and Agriculture Organization of the United Nations, International Fund for Agricultural Development - IFAD, UNICEF, WFP, WHO . FAO; Rome: 2021. The state of food security and nutrition in the world 2021: Transforming food systems for food security, improved nutrition and affordable healthy diets for all.https://www.fao.org/documents/card/en/c/cb4474en/ Disponível em: 2021. [Google Scholar]
- Filgueiras A., Stults-Kolehmainen M. Psychological Reports; 2021. Risk factors for potential mental illness among Brazilians in quarantine due to COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin G.M., Stein D.J. Generalised anxiety disorder and depression: Contemporary treatment approaches. Advances in Therapy. 2021;38(Suppl 2):45–51. doi: 10.1007/s12325-021-01859-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez L.O., Ayala-Guzman C.I. Change and continuity in health inequities related to skin color in Mexico. Social Medicine. 2022;15(1):32–41. [Google Scholar]
- HLPE - Panel of Experts on Food Security and nutrition Food security and nutrition: Building a global narrative towards 2030. Rome. 2020. www.fao.org/cfs/cfs-hlpe Disponível em:
- IBGE - Instituto Brasileiro de Geografia e Estatística . 2013. Atlas do Censo Demografico. [Google Scholar]
- IBGE - Instituto Brasileiro de Geografia e Estatística . IBGE; 2019. Desigualdades sociais por cor ou raça no Brasil.https://biblioteca.ibge.gov.br/visualizacao/livros/liv101681_informativo.pdf Disponível em: [Google Scholar]
- IBGE - Instituto Brasileiro de Geografia e Estatística . IBGE; Rio de Janeiro: 2020. Pesquisa de Orçamentos Familiares 2017-2018: Análise da Segurança Alimentar no Brasil.https://biblioteca.ibge.gov.br/visualizacao/livros/liv101749.pdf Available from: [Google Scholar]
- IBGE - Instituto Brasileiro de Geografia e Estatística. Coordenação de Trabalho e Rendimento; Rio de Janeiro . 2020. Pesquisa de orçamentos familiares 2017-2018: Análise da segurança alimentar no Brasil. [Google Scholar]
- Jomaa L., Naja F., Cheaib R., Hwalla N. Household food insecurity is associated with a higher burden of obesity and risk of dietary inadequacies among mothers in Beirut, Lebanon. BMC Public Health. 2017;17(1):1–14. doi: 10.1186/s12889-017-4317-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A.D. Food insecurity and mental health status: A global analysis of 149 countries. American Journal of Preventive Medicine. 2017;53(2):264–273. doi: 10.1016/j.amepre.2017.04.008. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick S.I., Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. Journal of Nutrition. 2008;138(3):604–612. doi: 10.1093/jn/138.3.604. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachance L., Ramsey D. Food, mood, and brain health: Implications for the modern clinician. Missouri Medicine. 2015;112(2):111. [PMC free article] [PubMed] [Google Scholar]
- Leddy A.M., Weiser S.D., Palar K., Seligman H. A conceptual model for understanding the rapid COVID-19–related increase in food insecurity and its impact on health and healthcare. American Journal of Clinical Nutrition. 2020;112(5):1162–1169. doi: 10.1093/ajcn/nqaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y.M., Kim S.A., Lee D.K. Can current recommendations on sun exposure sufficiently increase serum vitamin D level?: One-month randomized clinical trial. Journal of Korean Medical Science. 2020;35(8) doi: 10.3346/jkms.2020.35.e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.W., shin W.K., Kim Y. Impact of sex and marital status on the prevalence of perceived depression in association with food insecurity. PLoS One. 2020;15(6) doi: 10.1371/journal.pone.0234105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfrinato C.V., Marino A., Condé V.F., Franco M.C.P., Stedefeldt E., Tomita L.Y. High prevalence of food insecurity, the adverse impact of COVID-19 in Brazilian favela. Public Health Nutrition. 2021;24(6):1210–1215. doi: 10.1017/S1368980020005261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAPA - Ministério da Agricultura, Pecuária e Abastecimento; Ministério da Educação . Ministério da Agricultura, Pecuária e Abastecimento/Ministério da Educação; Brasília: 2020. Orientações para a execução do PNAE durante a situação de emergência decorrente da pandemia do Coronavírus (covid-19) [Google Scholar]
- Marin-Leon L., Francisco P.M.S.B., Segall-Corrêa A.M., Panigassi G. Household appliances and food insecurity: Gender, referred skin color and socioeconomic differences. Revista Brasileira de Epidemiologia. 2011;14(3):398–410. doi: 10.1590/s1415-790x2011000300005. [DOI] [PubMed] [Google Scholar]
- Maynard M., Andrade L., Packull-McCormick S., Perlman C.M., Leos-toro C., Kirkpatrick S.I. Food insecurity and mental health among females in high-income countries. International Journal of Environmental Research and Public Health. 2018;15(7):1424. doi: 10.3390/ijerph15071424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meireles A.L., et al. COVID-Inconfidentes-SARS-CoV-2 seroprevalence in two Brazilian urban areas during the pandemic first wave: Study protocol and initial results. Scielo preprints. 2021 doi: 10.1590/SciELOPreprints.2720. Submitted for publication. [DOI] [Google Scholar]
- Monteiro R.P., Nascimento B.S., Monteiro T.M.C., da Silva P.D.G., Ferreira A.J.C. Psychometric evidence of the 7-item generalized anxiety disorder questionnaire in Brazil. International Journal of Mental Health and Addiction. 2020:1–12. [Google Scholar]
- Moreno A.L., et al. Factor structure, reliability, and item parameters of the Brazilian- Portuguese version of the GAD-7 questionnaire. Temas em Psicologia. 2016;24(1):367–376. [Google Scholar]
- Mundt A.P. Assessing government responsibility for COVID-19 deaths. The Lancet. 2021;397(10282):1345. doi: 10.1016/S0140-6736(21)00529-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers C.A. Food insecurity and psychological distress: A review of the recent literature. Current nutrition reports. 2020;9(2):107–118. doi: 10.1007/s13668-020-00309-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odoms-Young A.M. Examining the impact of structural racism on food insecurity: Implications for addressing racial/ethnic disparities. Family & Community Health. 2018;41 doi: 10.1097/FCH.0000000000000183. n. Suppl 2 FOOD INSECURITY AND OBESITY, p. S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otten D., et al. Similarities and differences of mental health in women and men: A systematic review of findings in three large German cohorts. Frontiers in Public Health. 2021;9:40. doi: 10.3389/fpubh.2021.553071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquin V., et al. Longitudinal trajectories of food insecurity in childhood and its associations with mental health and functioning in adolescence. JAMA Network Open. 2021;4(12) doi: 10.1001/jamanetworkopen.2021.40085. e2140085-e2140085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Escamilla R., Segall-Corrêa A.M. Indicadores e medidas de insegurança alimentar. Revista de Nutrição. 2008;21(suppl) [Google Scholar]
- Piquero A.R., Jennings W.G., Jemison E., Kaukinen C., Knaul F.M. Domestic violence during the COVID-19 pandemic-Evidence from a systematic review and meta- analysis. Journal of Criminal Justice. 2021;74 doi: 10.1016/j.jcrimjus.2021.101806. n. C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky J.Y., Gilmour H. Food insecurity and mental health during the COVID-19 pandemic. Health Reports. 2020;31(12):3–11. doi: 10.25318/82-003-x202001200001-eng. [DOI] [PubMed] [Google Scholar]
- Pound C.M., Chen Y. Female sex and food insecurity in relation to self-reported poor or fair mental health in Canadian adults: A cross-sectional study using national survey data. Canadian Medical Association Open Access Journal. 2021;9(1):E71–E78. doi: 10.9778/cmajo.20200112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourmotabbed A., et al. Food insecurity and mental health: A systematic review and meta- analysis. Public Health Nutrition. 2020;23(10):1778–1790. doi: 10.1017/S136898001900435X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochazka J., et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data in Brief. 2020;32 doi: 10.1016/j.dib.2020.106174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman T., Hasnain M.D.G., Islam A. Food insecurity and mental health of women during COVID-19: Evidence from a developing country. PLoS One. 2021;16(7) doi: 10.1371/journal.pone.0255392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichenheim M.E., Interlenghi G.S., Moraes C.L., Segall-Corrêa A.M., Pérez-Escamilla R., Salles-Costa R. A model-based approach to identify classes and respective cutoffs of the Brazilian Household Food Insecurity Measurement Scale. Journal of Nutrition. 2016;146(7):1356–1364. doi: 10.3945/jn.116.231845. [DOI] [PubMed] [Google Scholar]
- Ridge D., Smith H., Fixsen A., Broom A., Oliffe J. How men step back–and recover– from suicide attempts: A relational and gendered account. Sociology of Health & Illness. 2021;43(1):238–252. doi: 10.1111/1467-9566.13216. [DOI] [PubMed] [Google Scholar]
- Salles-Costa R., et al. National trends and disparities in severe food insecurity in Brazil between 2004 and 2018. Current Developments in Nutrition. 2022;6(4) doi: 10.1093/cdn/nzac034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro D.F., et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos I.S., et al. Sensibilidade e especificidade do Patient Health Questionnaire-9 (PHQ- 9) entre adultos da população geral. Cadernos de Saúde Pública. 2013;29:1533–1543. doi: 10.1590/0102-311x00144612. [DOI] [PubMed] [Google Scholar]
- Santos L.P., et al. Association between food insecurity and major depressive episodes amid covid-19 pandemic: Results of four consecutive epidemiological surveys from southern Brazil. Public Health Nutrition. 2021:1–25. doi: 10.1017/S1368980021004626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch J.J., Roest A.M., Nolen W.A., Penninx B.W., De Jonge P. Gender differences in major depressive disorder: Results from The Netherlands study of depression and anxiety. Journal of Affective Disorders. 2014;156:156–163. doi: 10.1016/j.jad.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Lowe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sundermeir S.M., Wolfson J.A., Bertoldo J., Gibson D.G., Agarwal S., Labrique A.B. Food insecurity is adversely associated with psychological distress, anxiety and depression during the COVID-19 pandemic. Preventive medicine reports. 2021;24 doi: 10.1016/j.pmedr.2021.101547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarasuk V., St-Germain A.F., Mitchell A. Geographic and socio-demographic predictors of household food insecurity in Canada, 2011–12. BMC Public Health. 2019;19(1):1–12. doi: 10.1186/s12889-018-6344-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser J., Wangu J. Women's dual centrality in food security solutions: The need for a stronger gender lens in food systems' transformation. Current Research in Environmental Sustainability. 2021;3 doi: 10.1016/j.crsust.2021.100094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO - World Health Organization . Vol. 60. World Health Organization; Geneva: 2010. (Global recommendations on physical activity for health). [PubMed] [Google Scholar]
- WHO - World Health Organization . World Health Organization; 2017. Depression and other common mental disorders: Global health estimates.https://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf Disponível em: [Google Scholar]
- WHO - World Health Organization . World Health Organization; 2020. Considerations in adjusting public health and social measures in the context of COVID-19: Interim guidance, 16 April 2020. [Google Scholar]
- WHO - World Health Organization. Population-based age-stratified seroepidemiological investigation protocol for COVID-19 virus infection 2020. https://www.who.int/publications-etail/population-based-age-stratified-seroepidemiological-investigation-protocol-for-covid-19-virus-infection 17 de março de, Disponível em.
- Ximenes-da-Silva A., Guedes R.C.A. Nutrients, neurotransmitters and brain energetics. Frontiers in Neuroscience. 2020;1133 doi: 10.3389/fnins.2020.568937. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.