Abstract
Objective:
The second wave of the Covid-19 pandemic in India was widespread and caused psychological distress among the citizens. Hospitals were running at a premium, increasing deaths and trepidation stories were on air by media, this generated sleep disturbances for many. This study aimed to examine the sleep quality of Covid-19 recovered patients in India during the second wave of the pandemic.
Methods:
Patients who had recently recovered from Covid-19 were invited to participate in this cross-sectional study using various social media platforms. An online survey questionnaire, including socio-demographics, health-related information, Covid-19 related information, and the Pittsburgh Sleep Quality Index (PSQI), was administered in June 2021. Descriptive statistics were used to compare the scores among the mild, moderate, and severe groups. ANOVA was used to find the difference between the groups for global PSQI scores.
Results:
A total of 311 participants (261 mild, 45 moderate, and 5 severe) provided usable responses. The Global PSQI score for the overall study sample was 8.22 ± 3.79. In the severe group, scores were higher 16.8 ± 2.59, and statistically significant from mild or moderate groups. Sleep quality of Covid-19 recovered patients was found to be statistically significantly different based on their gender (P < .001), annual income (P < .001), employment status (P < .001), and marital status (P < .001).
Conclusion:
Females, employment in the private sector, annual income below rupees 11 lakh, and unmarried Covid-19 recovered patients reported poor sleep quality. As our findings indicate poor sleep quality among the Covid-19 recovered patients during the second wave in India, designing psychological interventions is recommended to support their wellbeing post-recovery.
Keywords: India, second wave, Covid-19 recovered patients, Pittsburg Sleep Quality Index
Introduction
The first Coronavirus disease (Covid-19) case was reported in Wuhan, China, in December 2019. 1 The novel coronavirus infection has now spread across the world through human-to-human transmission targeting the respiratory system of the patients. 1 To date, about 218 946 836 confirmed cases and more than 4 539 723 deaths are reported due to the Covid-19 (https://covid19.who.int). This ongoing pandemic has generated psychological distress and adversely impacted the mental health of the community. 2 Symptom like poor sleep quality, stress, anxiety, and depression are reported worldwide. 3
A new term coronasomnia is coined by Semyachkina-Glushkovskaya et al 4 for sleep disturbance associated with Covid-19 and the possible reasons include confinements due to quarantine, anxiety, stress, or financial losses. Studies on sleep restriction induced brain functioning are few. Sleep loss can cause neuroinflammation, which induces Blood Brain Barrier (BBB) disruption with involvement of cytokines, chemokines, and acute-phase proteins; promote changes in cellular components of the BBB, particularly on brain endothelial cells. Apnea a common phenomenon in Covid-19 may be responsible for sleep deprivation, high-sensitivity C-reactive protein (hs-CRP) a marker for inflammation tend to rise in Covid-19. This also increases the permeability of Blood Brain Barrier to inflammatory mediator’s tumor necrosis factor-α (TFN- α), interleukin-1. 4
The outbreak of the Covid-19 pandemic in India was even more widespread during the second wave. 5 Hospitals were struggling to function to their full potential due to insufficient resources such as low oxygen supply, non-availability of beds, increasing deaths, also the media was reporting stories of panic everywhere. 6 The patients who tested positive, their family members, the patients who recovered from Covid-19 and citizens experienced psychological distress.7,8 Covid-19 patients complained about sleep disturbances due to a long period of isolation, suffering, illness relapse threat, and being infectious for others. 6
Very few studies have been conducted to examine the sleep quality of Covid-19 recovered patients during or after the first wave of the pandemic. One study conducted by Kaur et al 6 examined the sleep quality of Indian citizens during the second wave of the pandemic. Therefore, this study measures the objective and subjective sleep quality of Covid-19 recovered patients during the second wave in India. The total duration of sleep, sleep design, and the frequency and amount of disturbances experienced during sleep are a few objective measures.9,10 Satisfactions experienced with overall sleep quality, sleep initiation, sleep maintenance, and perceived feeling of refreshment upon awakening are a few subjective measures.9,10 The overall sleep quality of Covid-19 recovered patients was analyzed at different severity levels, that is, mild, moderate, and severe. In this study, the severity of Covid-19 was defined as mild if treatment was done using medicines prescribed by the doctor, moderate if oxygen therapy was used, and severe if admitted to the hospital’s intensive care unit (ICU).
Materials and Methods
This cross-sectional study was conducted in India using an online survey in June 2021. Patients who had recovered from Covid-19 in the last 3 months were contacted through various social media platforms to participate in this survey. Each participant provided electronic informed consent, and his or her participation was kept voluntary. No incentive was given to participate in the study.
Using purposive sampling, patients who recently recovered from Covid-19 across various locations in India were encouraged to participate in the study. An attractive e-poster and a Google Form link were shared over different social media platforms, inviting Covid-19 recovered patients to participate in the study. The Google Form included a brief description of the study, consent of participation, voluntary participation information, and the survey questionnaire. The Google Form was provided in both English and Hindi language. A pilot test was conducted to estimate the time required to complete the questionnaire. It was estimated that each participant would take around 5 to 7 minutes to complete the questionnaire, irrespective of language.
The survey collected data for various socio-demographic variables, including age, gender, education, employment status, annual income, marital status, and area of residence. Health issues like hypertension, diabetes, and asthma were also considered. Data was collected on the level of anxiety patients might be experiencing using GAD-7, the general anxiety disorder scale. 11 One question from PHQ-4, the patients’ health questionnaire 12 to measure the level of depression, was also used. Providing a response was mandatory to all questions, except annual income that was optional.
Covid-19 related information was also collected. Data on the severity of Covid-19 was collected using 3 options, that is, mild if treatment was done using medicines prescribed by the doctor, moderate if oxygen therapy was used, and severe if admitted to the hospital’s intensive care unit (ICU). Data on place of treatment, that is, at home or hospital, was also collected. Information was collected on the type of test administered, that is, RTPCR, Antibody or both. Finally, data was collected on how many days since the patient had recovered from COVID-19, that is, less than 30 days, 30 to 60 days, or more than 60 days.
Pittsburg’s Sleep Quality Index (PSQI) was administered to assess the sleep quality of Covid-19 recovered patients. Seven components of this index, that is (1) subjective sleep quality, (2) sleep latency, (3) sleep duration, (4) habitual sleep efficiency, (5) sleep disturbances, (6) use of sleep medicines, and (7) daytime dysfunction due to sleepiness combine together to generate a global sleep score. 10 Used in several settings, PSQI is a valid and reliable measure. A global PSQI score ⩾5 suggests poor sleep quality of study participants.
The data were analyzed using the SPSS. Descriptive statistics were used to summarize participant’s socio-demographic factors, physical and mental health conditions, and Covid-19 related information. Cross tabulation was used to classify all study participants (N = 311) with respect to patients’ severity of Covid-19, that is, mild (N = 261), moderate (N = 45), and severe (N = 5). Counts and percentages were reported for categorical variables. Chi-square was used to compare the 2 groups for categorical variables. Mean and standard deviation is reported for continuous variables. ANOVA was used to find the difference between the groups for global PSQI scores. In addition to plotting, their distribution connections were made in the diagram to visualize response for Circos plot (http://circos.ca/).
Results
A total of 315 responses were received from the Covid-19 recovered patients. Four responses were excluded due to significant missing data, and 311 responses were included in the analysis (attached as a Supplemental Material). Study participants were further classified based on the Covid-19 severity, that is, 261 as mild, 45 as moderate, and 5 as severe.
More than 70% of the study participants were in the age group of 21 to 40 years, about 60% of them were females, 60% of them had a Master degree, about 70% were employed either in government, private, or self-employed, about 60% of them had annual income more than 5 lakh rupees, about 50% were married. About 90% were residing in urban areas of India. Participants with a history of health conditions included 5% with hypertension, about 30% with diabetes, about 8% with asthma, about 30% with mild anxiety, and 40% with mild depression. For 85% of the participants, the RTPCR test was administered by the authorities, the same percentage of patients were treated at home and about 55% had recovered from Covid-19 in the past 30 to 60 days.
Table 1 provides the socio-demographic characteristics, health conditions, and Covid-19 related information of the study participants. Also, a comparison between mild, moderate, and severe is presented.
Table 1.
Socio-demographic characteristics of the study participants.
| Variable | N = 311 (%) | Mild (N = 261) (%) | Moderate (N = 45) (%) | Severe (N = 5) (%) | P Value |
|---|---|---|---|---|---|
| Age | |||||
| <20 y | 10 (3.2) | 10 (3.8) | 0 (0) | 0 (0) | .002 |
| 21-40 y | 229 (73.6) | 179 (68.6) | 45 (100) | 5 (100) | |
| 41-60 y | 69 (22.2) | 69 (26.4) | 0 (0.0) | 0 (0) | |
| >61 y | 3 (1.0) | 3 (1.1) | 0 (0) | 0 (0) | |
| Gender | |||||
| Male | 123 (39.5) | 111 (42.5) | 12 (26.7) | 0 (0) | .025 |
| Female | 188 (60.5) | 150 (57.5) | 33 (73.3) | 5 (100.0) | |
| Education | |||||
| <High school | 5 (1.6) | 5(1.9) | 0 (0) | 0 (0) | <.001 |
| High school | 21 (6.8) | 16 (6.1) | 0 (0) | 5 (100) | |
| Under graduate | 95 (30.5) | 83 (31.8) | 12 (26.7) | 0 (0) | |
| Masters | 190 (61.1) | 157 (60.2) | 33 (73.3) | 0 (0) | |
| Employment status | |||||
| Employed (Government) | 18 (5.8) | 18 (6.9) | 0 (0.0) | 0 (0.0) | <.001 |
| Employed (Private) | 101 (32.5) | 72 (27.6) | 29 (64.4) | 0 (0) | |
| Self-employed | 107 (34.4) | 91 (34.9) | 16 (35.6) | 0 (0) | |
| Unemployed | 85 (27.3) | 80 (30.7) | 0 (0) | 5 (100) | |
| Annual income (INR) | |||||
| <5 Lakh | 111 (35.7) | 101 (39.3) | 6 (13.3) | 4 (100.0) | <.001 |
| 5-10 Lakh | 109 (35.0) | 75 (29.2) | 34 (75.6) | 0 (0) | |
| 11-15 Lakh | 70 (22.5) | 65 (25.3) | 5 (11.1) | 0 (0) | |
| >15 Lakh | 16 (5.1) | 16 (6.2) | 0 (0) | 0 (0) | |
| Marital status | |||||
| Married | 155 (49.8) | 132 (50.6) | 23 (51.1) | 0 (0) | .163 |
| Unmarried | 150 (48.2) | 123 (47.1) | 22 (48.9) | 5 (100) | |
| Divorced | 6 (1.9) | 6 (2.3) | 0 (0) | 0 (0) | |
| Area | |||||
| Rural | 22 (7.1) | 22 (8.4) | 0 (0) | 0 (0) | .104 |
| Urban | 289 (92.9) | 239 (91.6) | 45 (100.0) | 5 (100.0) | |
| Hypertension | |||||
| No | 295 (94.9) | 245 (93.9) | 45 (100) | 5 (100) | .199 |
| Yes | 16 (5.1) | 16 (6.1) | 0 (0) | 0 (0) | |
| Diabetes | |||||
| No | 278 (89.4) | 233 (89.3) | 40 (88.9) | 5 (100.0) | .737 |
| Yes | 33 (10.6) | 28 (10.7) | 5 (11.1) | 0 (0) | |
| Asthma | |||||
| No | 303 (97.4) | 253 (96.9) | 45 (100.0) | 5 (100.0) | .455 |
| Yes | 8 (2.6) | 8 (3.1) | 0 (0.0) | 0 (0) | |
| Hypertension and diabetes | |||||
| No | 306 (98.4) | 256 (98.1) | 45 (100.0) | 5 (100.0) | .615 |
| Yes | 5 (1.6) | 5 (1.9) | 0 (0) | 0 (0) | |
| Anxiety | |||||
| Minimal (0-4) | 112 (36.0) | 96 (36.8) | 16 (35.6) | 0 (0.0) | .313 |
| Mild (5-9) | 95 (30.5) | 79 (30.3) | 14 (31.1) | 2 (40.0) | |
| Moderate (10-14) | 70 (22.5) | 59 (22.6) | 8 (17.8) | 3 (60.0) | |
| Severe (15-21) | 34 (10.9) | 27 (10.3) | 7 (15.6) | 0 (0) | |
| Depression | |||||
| Minimal | 117 (37.6) | 98 (37.5) | 19 (14.2) | 0 (0) | .074 |
| Mild | 127 (40.8) | 109 (41.8) | 15 (33.3) | 3 (60.0) | |
| Moderate | 44 (14.1) | 38 (14.6) | 4 (8.9) | 2 (40.0) | |
| Severe | 23 (7.4) | 16 (6.1) | 7 (15.6) | 0 (0) | |
| Type of test | |||||
| RTPC | 267 (85.9) | 224 (85.8) | 38 (84.4) | 5 (100.0) | .470 |
| SERO (Antibody) | 10 (3.2) | 10 (3.8) | 0 (0) | 0 (0) | |
| Both | 34 (10.9) | 27 (10.3) | 7 (15.6) | 0 (0) | |
| Place of treatment | |||||
| Hospital | 43 (13.8) | 24 (9.2) | 14 (31.1) | 5 (100.0) | <.001 |
| Home | 268 (86.2) | 237 (90.8) | 31 (68.9) | 0 (0) | |
| Recovered from Covid-19 | |||||
| <30 d | 66 (21.2) | 57 (21.8) | 5 (11.1) | 4 (80.0) | .003 |
| 30-60 d | 176 (56.6) | 142 (54.4) | 33 (73.3) | 1 (20.0) | |
| >60 d | 69 (22.2) | 62 (23.8) | 7 (15.6) | 0 (0) | |
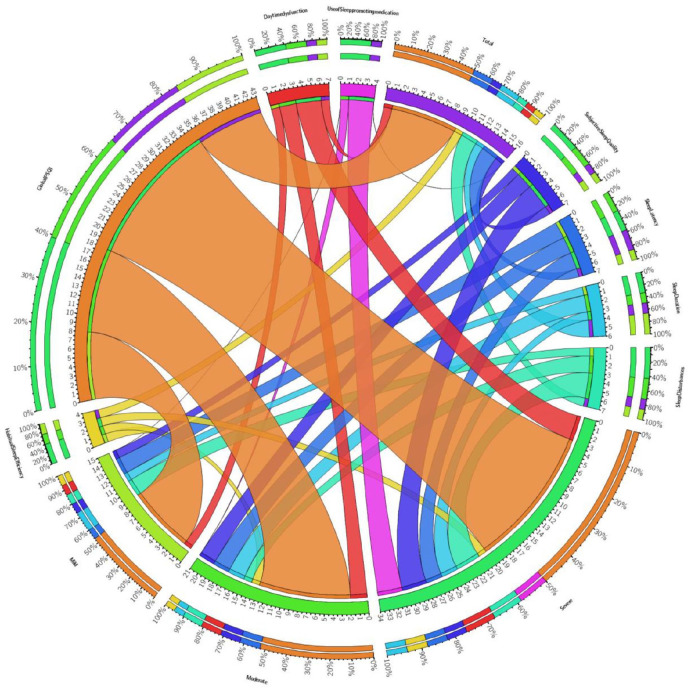
Participant’s sleep quality was measured using PSQI, and data on the PSQI scores are presented in Table 2 and visually presented in Figure 1. The Global PSQI score for the overall study sample was 8.22 ± 3.79. Scores were higher for severe (16.8 ± 2.59) and moderate (10.73 ± 3.83) when compared with mild (7.62 ± 3.42) and were also statistically significant. About 78% of the sample was above the cutoff point of PSQI score ⩾5, indicating poor sleep quality, but no statistically significant difference was found among the groups. Covid-19 recovered patients with mild severity level had better subjective sleep quality, longer sleep latency, fewer sleep disturbances, less use of sleep medicines, lower daytime dysfunction due to sleepiness when compared with moderate and severe groups.
Table 2.
Findings of the PSQI scores of Covid-19 recovered patients.
| Variable | N = 311 | Mild (N = 261) | Moderate (N = 45) | Severe (N = 5) | P Value |
|---|---|---|---|---|---|
| PSQI | |||||
| PSQI (C1) Subjective Sleep Quality | 1.50 ± 0.9 | 1.35 ± 0.83 | 2.02 ± 0.81 | 2.60 ± 0.55 | <.001 |
| PSQI (C2) Sleep Latency | 1.60 ± 0.8 | 1.50 ± 0.82 | 2.24 ± 0.80 | 2.00 ± 0.0 | <.001 |
| PSQI (C3) Sleep Duration | 1.40 ± 0.8 | 1.39 ± 0.77 | 1.49 ± 1.14 | 1.60 ± 0.55 | .669 |
| PSQI (C4) Habitual Sleep Efficiency | 0.87 ± 1.04 | 0.84 ± 0.99 | 0.98 ± 1.25 | 1.60 ± 1.52 | .212 |
| PSQI (C5) Sleep Disturbances | 1.3 ± 0.6 | 1.25 ± 0.52 | 1.56 ± 0.50 | 3.00 ± 0.00 | <.001 |
| PSQI (C6) Use of Sleep promoting medication | 0.31 ± 0.8 | 0.23 ± 0.72 | 0.44 ± 0.84 | 3.0 ± 0.0 | <.001 |
| PSQI (C7) Daytime dysfunction | 1.2 ± 0.96 | 1.02 ± 0.91 | 2.00 ± 0.67 | 3.00 ± 0.00 | <.001 |
| Global PSQI | 8.22 ± 3.79 | 7.62 ± 3.42 | 10.73 ± 3.83 | 16.8 ± 2.59 | <.001 |
| Prevalence of poor sleep quality (⩾ 5 points) | 245 (78.8%) | 204 (78.2%) | 37 (82.2%) | 4 (80.0%) | .826 |
Figure 1.
Evaluation of people’s sleep quality after Covid-19 contraction.
Table 3 and Figure 1 presents the comparison between various independent variables and global PSQI scores using ANOVA. A significant difference between male and female participants was observed on PSQI score (P < .001), with females showing lower sleep quality. The participants’ employment status had a statistically significant difference on PSQI score (P < .001) with employment in the private sector was found to be associated with lower sleep quality. A statistically significant difference between the annual income of study participants was observed for PSQI score (P < .001), with an income group of 5 to 10 lakh (below average) showing lower sleep quality. A significant difference was observed between study participants’ marital status on PSQI score (P < .001), with unmarried and divorced showing lower sleep quality. A significant difference between the severity of Covid-19 among study participants was observed on PSQI score (P < .001) with severe and moderate showing lower sleep quality compared with mild. A significant difference between the place of treatment of study participants was observed on PSQI score (P < .001), with patients treated at the hospital showing lower sleep quality.
Table 3.
Association of independent variables and Global PSQI score using ANOVA.
| Variable | Mean (St. dev.) | F | P-value |
|---|---|---|---|
| Age | |||
| <20 y | 8.50 (2.46) | 2.25 | .082 |
| 21-40 y | 8.49 (4.03) | ||
| 41-60 y | 7.45 (3.00) | ||
| >61 y | 4.66 (1.53) | ||
| Gender | |||
| Male | 7.09 (2.85) | 19.17 | <.001* |
| Female | 8.96 (4.15) | ||
| Education | |||
| <High school | 12.80 (0.83) | 5.07 | .002 |
| High school | 10.29 (4.33) | ||
| Under graduate | 7.89 (2.71) | ||
| Masters | 8.04 (3.79) | ||
| Employment status | |||
| Employed (Government) | 3.22 (1.59) | 12.86 | <.001* |
| Employed (Private) | 8.90 (4.15) | ||
| Self-employed | 8.34 (3.09) | ||
| Unemployed | 8.33 (3.76) | ||
| Annual income (INR) | |||
| <5 Lakh | 8.07 (3.58) | 10.03 | <.001* |
| 5-10 Lakh | 9.45 (7.18) | ||
| 11-15 Lakh | 7.18 (4.26) | ||
| >15 Lakh | 5.06 (1.12) | ||
| Marital status | |||
| Married | 7.37 (3.25) | 8.93 | <.001* |
| Unmarried | 9.0 (4.15) | ||
| Divorced | 10.83 (2.1) | ||
| Area | |||
| Rural | 8.36 (3.60) | 0.03 | .856 |
| Urban | 8.21 (3.18) | ||
| Health history | |||
| Not present | 8.12 (4.05) | 0.76 | .382 |
| Present | 8.22 (3.79) | ||
| Anxiety | |||
| Minimal (0-4) | 8.04 (3.67) | 0.28 | .840 |
| Mild (5-9) | 8.29 (3.69) | ||
| Moderate (10-14) | 8.17 (3.73) | ||
| Severe (15-21) | 8.70 (4.67) | ||
| Depression | |||
| Minimal | 8.25 (3.53) | 1.37 | .252 |
| Mild | 8.09 (4.00) | ||
| Moderate | 7.75 (3.09) | ||
| Severe | 9.65 (4.90) | ||
| Severity of Covid-19 | |||
| Mild (Treatment with only medicine) | 7.62 (3.42) | 30.81 | <.001* |
| Moderate (Oxygen therapy required) | 10.73 (3.83) | ||
| Severe (ICU) | 16.8 (2.59) | ||
| Place of treatment | |||
| Hospital | 10.25 (4.93) | 14.97 | <.001* |
| Home | 7.89 (3.48) | ||
| Recovered from Covid-19 | |||
| <30 d | 8.04 (3.84) | 4.39 | .013 |
| 30-60 d | 8.71 (3.81) | ||
| >60 d | |||
P < .001.
Discussion
This study examines the sleep quality of Covid-19 recovered patients in India. To the best of our knowledge, this is the first study that examines the sleep quality of Covid-19 recovered patients after the critical second wave experienced by the Indian citizens. A significant finding of this study is that the sleep quality of Covid-19 depends on the severity. Participants who received treatment at home using only medicines prescribed by the doctor, that is, in the mild group, were found to have better sleep quality than participants in the moderate group who received oxygen therapy or in the severe group who were admitted to the hospital’s intensive care unit (ICU).
Cytokines may play a key role in modulating the BBB function during sleep restriction via the overexpression of the tumor necrosis factor α, interleukin-1 beta, interleukin-6, interleukin-17, C reactive protein, allograft inflammatory factor 1 (Iba-1), matrix metalloproteinase 9 (MMP-9) and A2A adenosine receptors.13-17 Sleep deprivation induces a low-grade systemic inflammation characterized by the release of inflammatory molecules such cytokines, chemokine and acute phase proteins promoting cellular changes in BBB.18,19 These parameters could be measured and their relationship with the sleep quality may be determined in the future studies.
The quality of sleep of patients after Covid-19 was found to be better in men than in women. Sleep quality, perhaps due to concerns about the future, was not good for individuals employed or self-employed in the private sector, while those employed in the public sector were found to have better sleep quality. Annual income had a significant difference in the sleep quality of Covid-19 recovered patients, where the income group of rupees 11 lakh per annum and above were found to have better sleep quality in comparison with the income group of less than rupees 11 lakh per annum. Finally, there was a statistically significant difference in sleep quality of COVID-19 recovered patients in marital status, married patients were found to have better sleep quality than single or divorced patients due to better emotional and social support.
Previous studies conducted to examine the sleep quality of Covid-19 recovered patients suggest similar results. Reports from China and Pakistan also report poor sleep quality or insomnia among the Covid-19 recovered patients.20,21 Mazza et al 22 reported that female patients have poor sleep quality than men. Females are more likely to express their sleep problems and psychological distress.23,24 Results of this study are not in agreement with the study of Kaur et al 6 where poor sleep quality was reported in higher socioeconomic status, results in this study depict poor sleep quality among the lower and middle-income groups. This was probably due to worries for future financial security and the impact of lockdown on the employment sources as experienced during the first wave of the pandemic. A study conducted in Indonesia shows that married participants had lower anxiety levels than unmarried participants. 25
Sleep problems among the Covid-19 patients could be due to many reasons including quarantine, social isolation, uncertainty, financial stress, and health status.26,27 Due to long-term home quarantine or hospitalization, Covid-19 patients experience subjective loneliness that might lead to poor sleep quality even upon recovery. 28 Information regarding a surge in the number of cases of Covid-19 patients and expected waves of the pandemic is speculated in media, creating a sense of uncertainty. This might also lead to poor sleep quality among the recovered patients. 29 Quite a few individuals even lost their job during the pandemic. The potential financial stress among the high-income group participants might also lead to poor sleep quality. 26 A perceived fear of transmitting the virus to others, significantly their family members might also contribute to the poor sleep quality among Covid-19 recovered patients. Therefore, designing and implementing psychological interventions to assist Covid-19 recovered patients are essential to managing their poor sleep quality and other mental health issues. 30
Conclusion
Sleep quality of the Covid-19 recovered patients is adversely impacted during the second wave in India. In the ongoing pandemic, managing the sleep quality of Covid-19 recovered patients is an essential aspect of their overall wellbeing post-recovery. In future studies, psychological interventions could be designed, and experiments could be conducted to enhance the sleep quality of Covid-19 recovered patients. Also, a longitudinal study could be conducted to study the ongoing changes in the sleep quality of Covid-19 recovered patients.
Supplemental Material
Supplemental material, sj-xlsx-1-exn-10.1177_26331055221109174 for Sleep Quality of Covid-19 Recovered Patients in India by Raina Chhajer and Sunil Dutt Shukla in Neuroscience Insights
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: RC: conception of the study, variables, literature review, data collection, and interpretation. SS: research design, analysis, interpretation, and discussion. Both authors contributed to the article and approved the submitted version.
ORCID iD: Sunil Dutt Shukla  https://orcid.org/0000-0002-4467-3106
https://orcid.org/0000-0002-4467-3106
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Shereen MA, Khan S, Kazmi A, Bashir N, Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Xiang Y-T, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Salehinejad MA, Azarkolah A, Ghanavati E, Nitsche MA. Circadian disturbances, sleep difficulties and the COVID-19 pandemic. Sleep Med. 2022;91:246-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Semyachkina-Glushkovskaya O, Mamedova A, Vinnik V, et al. Brain mechanisms of COVID-19-sleep disorders. Int J Mol Sci. 2021;22:6917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Faruqui N, Raman VR, Shiv J, Chaturvedi S, Muzumdar M, Prasad V. Informal collectives and access to healthcare during India’s COVID-19 second wave crisis. BMJ Glob Health. 2021;6:e006731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaur T, Ranjan P, Chakrawarty A, et al. Association of sociodemographic parameters with depression, anxiety, stress, sleep quality, psychological trauma, mental well-being, and resilience during the second wave of COVID-19 pandemic: a cross-sectional survey from India. Cureus. 2021;13:e16420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Menon V, Kar SK, Ransing R, Arafat SMY. Impending second wave of COVID-19 infections: what India needs to do? Asia Pac J Public Health. 2021;33:456-457. [DOI] [PubMed] [Google Scholar]
- 8. Sawant N, Ingawale S, Lokhande U, Patil S, Ayub EFM, Rathi V. Psychiatric sequelae and COVID experiences of post COVID -19 recovered resident doctors and interns of a Tertiary General Hospital in Mumbai. J Assoc Physicians India. 2021;69:22-26. [DOI] [PubMed] [Google Scholar]
- 9. Jahrami H, BaHammam AS, AlGahtani H, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25:503-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buysse DJ, Reynolds Cf, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [DOI] [PubMed] [Google Scholar]
- 11. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [DOI] [PubMed] [Google Scholar]
- 12. Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86-95. [DOI] [PubMed] [Google Scholar]
- 13. Chennaoui M, Sauvet F, Drogou C, et al. Effect of one night of sleep loss on changes in tumor necrosis factor alpha (TNF-α) levels in healthy men. Cytokine. 2011;56:318-324. [DOI] [PubMed] [Google Scholar]
- 14. Zielinski MR, Kim Y, Karpova SA, McCarley RW, Strecker RE, Gerashchenko D. Chronic sleep restriction elevates brain interleukin-1 beta and tumor necrosis factor-alpha and attenuates brain-derived neurotrophic factor expression. Neurosci Lett. 2014;580:27-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vgontzas AN, Zoumakis M, Papanicolaou DA, et al. Chronic insomnia is associated with a shift of interleukin-6 and tumor necrosis factor secretion from nighttime to daytime. Metab Clin Exp. 2002;51:887-892. [DOI] [PubMed] [Google Scholar]
- 16. van Leeuwen WM, Lehto M, Karisola P, et al. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS One. 2009;4:e4589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Okun ML, Coussons-Read M, Hall M. Disturbed sleep is associated with increased C-reactive protein in young women. Brain Behav Immun. 2009;23:351-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pan W, Kastin AJ. The blood-brain barrier: regulatory roles in wakefulness and sleep. Neuroscientist. 2017;23:124-136. [DOI] [PubMed] [Google Scholar]
- 19. Hurtado-Alvarado G, Domínguez-Salazar E, Pavon L, Velázquez-Moctezuma J, Gómez-González B. Blood-brain barrier disruption induced by chronic sleep loss: low-grade inflammation may be the link. J Immunol Res. 2016;2016:4576012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu F, Wang X, Yang Y, et al. Depression and insomnia in COVID-19 survivors: a cross-sectional survey from Chinese rehabilitation centers in Anhui province. Sleep Med. 2022;91:161-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8:416-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health. 2020;17:E3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Barsky AJ, Peekna HM, Borus JF. Somatic symptom reporting in women and men. J Gen Intern Med. 2001;16:266-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khademi M, Vaziri-Harami R, Shams J. Prevalence of mental health problems and its associated factors among recovered COVID-19 patients during the pandemic: a single-center study. Front Psychiatry. 2021;12:602244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harjana NPA, Januraga PP, Indrayathi PA, Gesesew HA, Ward PR. Prevalence of depression, anxiety, and stress among repatriated Indonesian migrant workers during the COVID-19 pandemic. Front Public Health. 2021;9:630295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Becker PM. Overview of sleep management during COVID-19. Sleep Med. 2022;91:211-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van der Velden PG, Hyland P, Contino C, von Gaudecker H-M, Muffels R, Das M. Anxiety and depression symptoms, the recovery from symptoms, and loneliness before and after the COVID-19 outbreak among the general population: findings from a Dutch population-based longitudinal study. PLoS One. 2021;16:e0245057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chatterjee SS, Chakrabarty M, Banerjee D, Grover S, Chatterjee SS, Dan U. Stress, sleep and psychological impact in healthcare workers during the early phase of COVID-19 in India: a factor analysis. Front Psychol. 2021;12:611314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Akıncı T, Melek Başar H. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Med. 2021;80:167-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Álvarez-García HB, Jiménez-Correa U, de Almondes KM. Effectiveness of a brief behavioral intervention for insomnia (BBII) during the COVID-19 pandemic: Mexican case report. Sleep Sci. 2020;13:210-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-exn-10.1177_26331055221109174 for Sleep Quality of Covid-19 Recovered Patients in India by Raina Chhajer and Sunil Dutt Shukla in Neuroscience Insights