Abstract
Background
Multiple options are available for the tibial insert in total knee arthroplasty (TKA). A systematic review (SR) and network meta-analysis (NMA) to compare available randomized controlled trials (RCTs) could assist with decision making. We aim to show that designs with increased conformity may improve function and satisfaction without an increase in complications though posterior stabilized (PS) inserts will likely have more flexion.
Methods
A search of MEDLINE, EMBASE, and the Cochrane Library was performed. Studies were limited to RCTs evaluating cruciate retaining (CR), PS, anterior stabilized (AS), medial pivot (MP), bicruciate retaining (BR), and bicruciate stabilizing (BCS) inserts. Mean differences (MD) were used for patient reported outcome measures (PROMs) and odds ratios (OR) for reoperation rates and MUA. A systematic review was performed for satisfaction.
Results
27 trials were identified. The NMA showed no difference from a statistical or clinical standpoint for PROMs evaluated. There was a statistical difference for increased flexion for PS knees (3 degrees p 0.04). There were no differences in the MUA or reoperation rates. There was insufficient information to determine if a specific insert improved satisfaction.
Discussion
The results of this NMA show no statistical or clinical difference in PROMs. There was higher flexion for PS knees though the amount was not clinically significant. There was insufficient data for conclusions on patient satisfaction. Therefore, the surgeon should evaluate the clinical situation to determine the best insert rather than choose and insert based on functional scores, patient satisfaction, or complication rates.
Keywords: Polyethylene Inserts, Insert design, polyethylene design, network meta-analysis, systematic review, knee kinematics
Background
Despite recent improvements in peri-operative pain control and rapid recovery, up to 20% of TKA patients are not satisfied, mainly due to persistent pain.1,2 While gross instability manifesting as pain is the second most common reason for revision,3 subtle instability and altered knee kinematics manifesting as pain in daily activities are likely causes of inadequate patient satisfaction. Various tibial insert designs have been created attempting to mimic native knee kinematics to attempt to improve function and satisfaction while avoiding complications.
Traditional cruciate-retaining (CR; Figure 1) and posterior stabilized (PS; Figure 1) designs have demonstrated excellent survivorship4,5 including data from multiple registries.6–8 However, CR knees have been reported to have abnormal knee kinematics secondary to paradoxical motion (lack of rollback, paradoxical forward femoral motion, and rotational pivot mechanics with the pivot potentially in the lateral compartment)9 due to non-anatomic surfaces.10 Drawbacks to PS knees include additional bone resection for the cam and post mechanism, which increases the risk of condylar fracture.11 In addition, post failure and patellar clunk syndrome12 are also potential drawbacks.
Figure 1. Various Polyethylene Design Types.
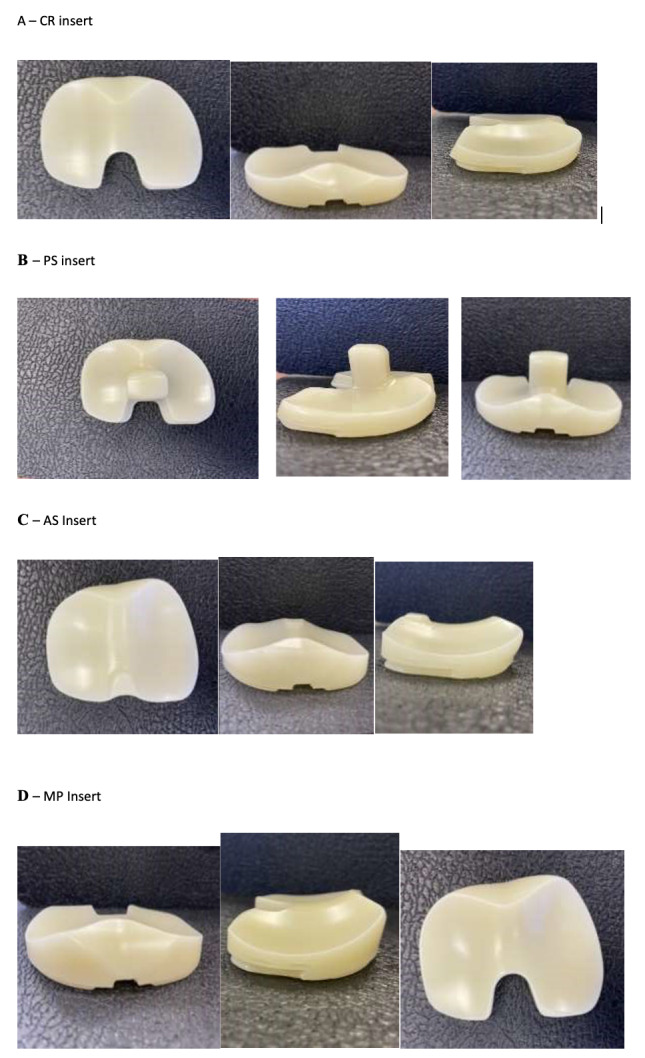
A – Cruciate Retaining (CR), B – Posterior Stabilized (PS), C – Anterior Stabilized (AS), D – Medial Pivot (MP)
Anterior stabilized (AS), bicruciate retaining (BR), bicruciate stabilized (BCS), and medial pivot (MP) inserts have been developed to improve stability, with the intent of improving patient satisfaction. AS (Figure 1) inserts intended to be utilized with a CR femur with or without a competent posterior cruciate ligament (PCL) have a deeper, more conforming geometry that is aimed to improve kinematics. However, the increased conformity can result in higher medial and patellofemoral contact pressure and wear.13,14 Despite these concerns, no significant differences have been noted between AS and traditional CR or PS outcomes in most clinical studies.15
MP (Figure 1) inserts incorporate a medial deep-dish portion and a relatively flat lateral side in an attempt to recreate the native tibial plateau geometry and medial pivot knee kinematics.15 Improved patient satisfaction has been reported with MP design, but there have been concerns reported regarding the potential for stiffness and increased wear due to the increased medial conformity.15 However, some studies have also shown no difference in need for MUA.16
BR designs require preservation of an island of bone for retention both the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL), in order to theoretically retain near-normal knee kinematics.17,18 However, there have been notable complications associated with the BR design including early failure, lateral pain, stiffness, and tibial island fracture.17,18
BCS inserts use an asymmetric cam-post mechanism in an attempt to restore more normal knee kinematics.19,20 This device also utilizes a more congruent medial compartment and a more concave lateral compartment, like the MP design. These features allow more external rotation and accommodate high flexion, which help approximate normal kinematics; however, there have been concerns about lateral knee pain and posterior positioning of the femur leading to quadriceps inefficiency.21,22
The six different fixed bearing polyethylene insert designs discussed above have significant differences in design and kinematics. Multiple RCTs have compared two polyethylene insert designs8,13,14,17–37 but a trial comparing all six designs has not been conducted to date, partly due to a lack of feasibility. So, there is a paucity of level I evidence on comparative safety and efficacy of various tibial insert designs.
The aims of this study are to evaluate the comparative efficacy (patient reported outcome scores, range of motion, and patient satisfaction) and safety (reoperation and MUA) of six different fixed bearing polyethylene insert designs, using network meta-analysis (NMA) of randomized controlled trials (RCTs).
Methods
Literature Search
We searched for relevant studies in the Medline, EMBASE, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Controlled Register of Trials (CENTRAL), and Institute of scientific information (ISI) Web of Knowledge, from inception to February 2021. All searches were limited to randomized controlled trials in humans published in English language. The following search terms were applied for systematic searching: “total knee arthroplasty” OR “knee replacement” AND “ultra-congruent” OR “deep dish” OR “anterior stabilized” OR “medial pivot” OR “medial stabilized” OR “ball and socket” OR “posterior stabilized” OR “cruciate retaining” OR “posterior stabilized plus” AND “randomized controlled trial”.
Study selection
Inclusion criteria were RCTs comparing two or more fixed bearing polyethylene inserts used for patients with primary knee osteoarthritis and reporting patient reported outcomes at minimum 6-month follow-up. Exclusion criteria were study design other than RCT, studies with inflammatory or posttraumatic osteoarthritis. Title and abstract screening were performed by two authors and full texts of all selected studies were then reviewed for selection confirmation. Any disagreements were resolved by discussion.
Included studies
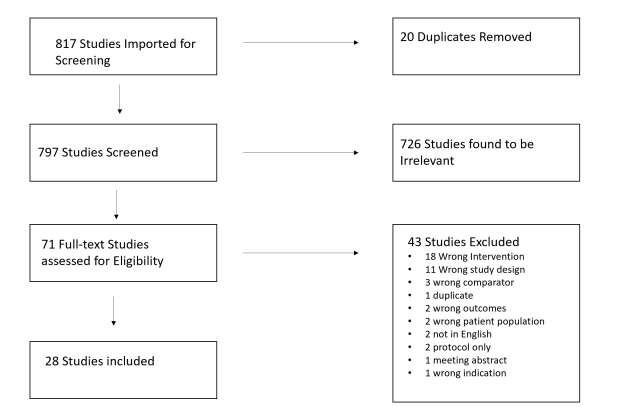
As shown in the PRISMA flow diagram (Figure 2) 817 studies were identified from database searches, and after removing duplicates, 797 were screened for inclusion. The abstract and title review yielded 71 articles that required full-text review. Of these, 28 met inclusion criteria for the systematic review and meta-analysis. One of these 28 studies excluded as it was a further follow-up of a previous trial leaving 27 trials in total.32
Figure 2. PRISMA Diagram.
Data Extraction
The data was independently extracted by two reviewers using web-based systematic review program, Covidence (www.covidence.org, Melbourne, Australia). The following information was extracted from the included articles: first author, year of publication, patient demographics, insert designs, patient reported outcome scores, range of motion, satisfaction and adverse events including manipulations and reoperations. Any disagreement concerning the data extraction was resolved by discussion.
Assessment of Study Quality
Two authors assessed the risk of bias of all included studies using the Cochrane Collaboration Tool Risk of Bias Assessment Tool (Robvis).38,39 The tool assesses the risk of: selection bias (“sequence generation” and “allocation sequence concealment”), performance bias (“blinding of participants and personnel”), detection bias (“blinding of outcome assessment”), attrition bias (“incomplete outcome data”), and reporter bias (“selective outcome reporting”).40,41 The risk of each individual bias was assessed as high risk, low risk, or uncertain risk.
Statistical Analysis
Continuous variables were expressed as mean and standard deviation. Dichotomous variables were reported as odds ratios. When standard errors of the mean or median and range were provided, we calculated the standard deviation by the method described by Hozo et al.42
When trials reported comparable data from multiple pair-wise comparisons, we examined the data using MetaInsight43 network meta-analysis software. Network plots were created and when there was a connected network of evidence, further network analysis was performed using the random effects model. Cruciate retaining inserts were used as the reference treatment for network comparisons. Frequentist meta-analysis was performed and forest plots of the pooled effect estimates (mean difference), and their associated uncertainty (95% confidence intervals) were generated, for all interventions compared to the reference treatment. To adjust for multiple comparisons in the NMA, we utilized the Holm’s Sequential Bonferroni Procedure to adjust the p values.44 Differences were considered clinically significant if they exceeded Minimal Clinically Important Difference (MCID) values. MCID values used for KS clinical, KS functional and OKS were 9, 1045 and 546 respectively. Treatment rankings were plotted in a matrix displaying relative treatment effects with treatments ranked from best to worst along the leading diagonal. Agreement between treatment effect estimates obtained from direct (head-to-head) and indirect (indirect comparisons in network) evidence was examined in consistency tables using 95% confidence intervals and p values with p < 0.05 considered inconsistent.43 Funnel plots were created for each continuous variable using Meta-Essentials47 to assess publication bias utilizing the study standard error compared with the effect size using Cohen’s method.48
Results
Characteristics of included studies
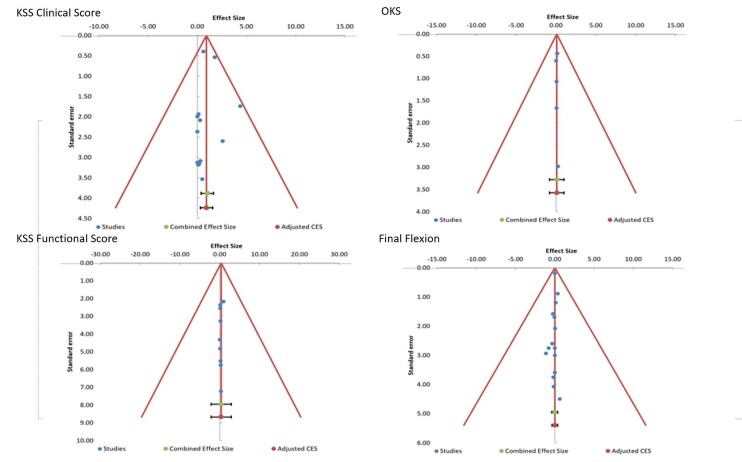
27 RCTs published between 2002 and 2021 with total of 2984 patients were included. 9 trials compared CR and PS,24,27,28,34–36,49–51 5 compared AS and PS,12,23,25,32,33 2 compared CR and AS,31,52 2 compared BCS and PS,21,22,31 1 compared AS and MP,29 4 compared PS and MP,26,37,53,54 1 compared CR and BR,18 3 compared multiple groups (CR, PS, MP,)55 (CR, PS, MP, BR),17 and (CR, PS, RP).56 All studies reported patient outcomes of greater than one year with the exception of the study by Batra et al37 which was 6 months and 21 out of 27 studies had a follow up of 2 years or more. Overall, the risk of bias was considered low. Four of the studies21,32,55,56 were funded by implant manufacturers and were therefore considered at high risk of “other” bias (Figure 3). There was enough data to perform NMA for Knee society clinical and function score (1989 version)57 Oxford knee score,58 maximum flexion > 1 year, MUA and reoperation rates (Figures 5 and 6). Inconsistency (Appendix 1) was low with p-values <0.05. Publication bias was noted to be low based on funnel plots (Figure 4). There was not enough uniform data to perform a NMA for Knee society score (2011 version), KOOS, WOMAC, Forgotten Joint Scores, and patient satisfaction.
Figure 3. Risk of Bias.
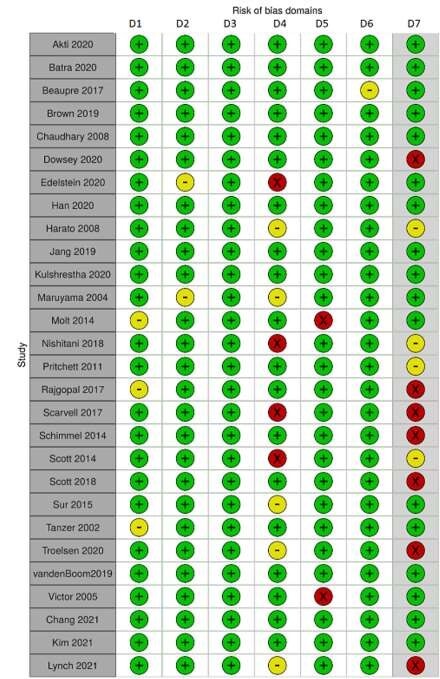
D1: Bias due to Sequence Generation, D2: Bias due to allocation sequence concealment, D3: Bias due to blinding of participants and personnel, D4: Bias due to incomplete outcome data, D5: Bias due to selective reporting, D7: Bias due to other sources.
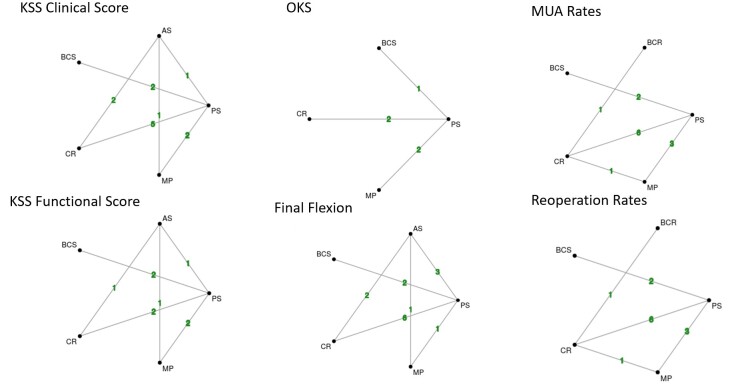
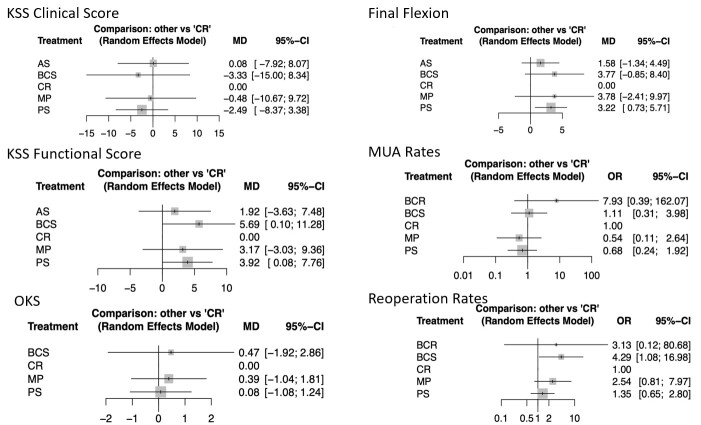
Figure 5. Network Plots.
Figure 6. Forest Plots for the Network Meta-analysis.
Figure 4. Funnel Plots of Continuous Data.
Patient Reported Outcomes
14 studies reported KS clinical scores, 10 reported KS function scores and 7 reported OKS. There were no clinically or statistically significant differences in KS clinical, KS function scores and OKS for the six different inserts in the NMA (Figure 6).
Flexion
19 studies reported maximum flexion at >1 year follow-up. Mean differences in final flexion for different inserts compared to CR inserts were less than 4 degrees. Flexion was statistically more for PS inserts compared to CR inserts in the NMA (MD 3.2 degrees; CI 0.7 - 5.7) (Figure 6). These differences do not appear clinically significant. Flexion needed for walking, rising from a chair and descending stairs is 65, 70 and 100 respectively (reference). All of the inserts achieved more than 100-degree flexion and so were adequate for all these activities of daily living.
Manipulation Under Anesthesia and Reoperations
MUA rates were reported in 11 studies and reoperation rates in 19 studies. Our analysis found that odds of MUA compared to CR inserts were: BCR 7.93, BCS 1.11, PS 0.68 and MP 0.54. The odds of reoperation compared to CR inserts were: BCS 4.29, BCR 3.13, MP 2.54 and PS 1.35. Many of these differences appear clinically significant, however, they did not meet statistical significance after the Holm’s Sequential Bonferroni Procedure was applied to p-values to account for multiple comparisons. (Figure 6).
Patient Satisfaction
Given the heterogeneity of reported outcomes, we were not able to perform an NMA to evaluate patient satisfaction. Instead, we performed a systematic review of the available 27 studies. 4 studies evaluated KS satisfaction score. 3 showed no difference26,29,55 with one study showing improvement in satisfaction with MP vs PS inserts (32.6 vs 29.5 p 0.0).37 One study evaluated a functional satisfaction question through a survey where they reported 72% of PS inserts were satisfied versus 81% of MP inserts.53 Two studies evaluated VAS satisfaction scores with neither showing significance comparing BCS and PS (88 and 94 p 0.45)22 and CR and PS (19 vs 11 p > 0.05).56 Pritchett et al17 compared multiple inserts and found that patients preferred BR to CR (73.6% vs 18.7% p <0.001) and BR to PS (89.1% vs 4.3% p < 0.001). It showed no difference between BR and MP (48.4% vs. 48.4% p 1.0). It also showed MP inserts had higher satisfaction with MP vs PS (76.2% vs 9.5% p <0.001) and MP vs CR (76% vs 12% p < 0.001). Finally, there was no difference between CR and PS (43.8% vs 42.2% p 0.893). Overall, there is inadequate data to suggest superiority of one insert over the others.
Discussion
Different tibial inserts have been designed to encourage native knee kinematics, provide intrinsic knee stability and adequate satisfaction to all patients. Our analysis of 2984 patients with primary knee osteoarthritis addresses the knowledge gap in comparative efficacy and safety of different fixed bearing tibial inserts.
For patient reported outcomes, we did not find significant differences in 6 different fixed bearing tibial insert designs for KSS clinical score and Oxford knee score. Previous systematic reviews and meta-analysis of CR and PS designs59,60 have shown what?
For final knee ROM, we found that PS inserts studies had 3.2 degree higher final flexion compared to CR inserts. However, it is unlikely that this increase in flexion improves clinical outcomes. Our finding of higher flexion with PS compared to CR inserts is in agreement with multiple other studies.23,24,26,27 A meta-analysis of level IV studies has also shown deeper flexion with PS or BCS designs as compared to CR designs.61 Another meta-analysis and systematic review60 and a systematic review59 of RCTs comparing only PS and CR designs has also demonstrated improved flexion with PS inserts.
For MUA, our analysis showed high rates of MUA with BCR design and low rates of MUA with PS and MP designs compared to CR design. However, these clinically important differences did not meet statistical significance.
Odds of reoperation compared were lowest for CR inserts and highest for BCS (4.29) followed by BCR inserts (3.13), though these clinically important differences did not meet statistical significance. However, study follow up was at most 5 years for the RCTs evaluated. Registry data is available for multiple designs in our study. The MP design has an acceptable 7.4% revision rate at 10 years in the Australian registry and 9.8% at 10 years in the Dutch registry.62 BR knees have reported >90% survivorship free of revision at 10 years for first generation designs,63 whereas one AS design has reported >95% revision-free survivorship at 7 years in a large series.64 Finally, the BCS implant shows comparable revision rates as compared to PS knees at 5 years in single RCTs.65
Recent literature has been heterogeneous in terms of showing whether particular implants improve satisfaction.64,66,67 Though satisfaction is important for patient outcomes following total knee arthroplasty, most of the studies reviewed were powered and designed to evaluate patient reported outcome scores rather than satisfaction. Two studies did show that MP inserts may have improved satisfaction17,37 and one showed that BR inserts may have improved satisfaction.17 However, given the heterogeneity of the data available and the study designs evaluated, we cannot make new meaningful conclusions based on any improvement in patient satisfaction when comparing all six inserts.
Our study has several limitations. First, our results apply only to TKA for primary osteoarthritis and not for other TKA indications such as inflammatory or traumatic arthropathy. Inserts of same type from different manufacturers have subtle design differences which may affect outcomes. This heterogeneity combined with differences in surgical technique may have affected comparisons reported in this analysis. The BR and BCS inserts had fewer studies than the PS or CR inserts which may have introduced type II error. We were also unable to report a meta-analysis regarding satisfaction as the scoring outcomes were too heterogenous. Most trials included had two-year follow-up, which would be considered short-term for TKA. Despite these limitations, this is the first study to date which reports comparisons among six separate TKA polyethylene designs that are designed to produce differing kinematics.
In conclusion, our network metanalysis shows no clinically significant differences in patient reported outcomes in fixed bearing inserts. PS inserts had more knee flexion at >1 year follow-up compared to CR inserts, but the 3-degree difference in flexion does not appear clinically significant. There were clinically important differences in manipulation and reoperation rates of different inserts with high rates of manipulation and reoperations with bi-cruciate retaining and bi-cruciate substituting designs, but these did not meet statistical significance. We advise caution with BCR and BCS designs and feel that inserts should be chosen based upon clinical situation rather than improvements in PROMs, satisfaction, or avoiding complications.
Table 1. Characteristics of Studies Included.
| Study | Tibial insert design | Number of Patients | Mean Age in years (yrs) | Minimum Follow-up |
| Tanzer et al34 2002 | CR | 20 | 68 yrs | 24 Months |
| PS | 20 | 67 yrs | ||
| Maruyama et al27 2004 | CR | 20 | 74 yrs | 24 Months |
| PS | 20 | 74 yrs | ||
| Victor et al36 2005 | CR | 22 | 70 yrs | 60 months |
| PS | 22 | 70 yrs | ||
| Harato et al24> 2008 | CR | 99 | 68 yrs | 60 months |
| PS | 93 | 66 yrs | ||
| Chaudhary et al51 2008 | CR | 40 | 69 yrs | 24 months |
| PS | 38 | 70 yrs | ||
| Pritchett68 2011 | CR | 205 | Not reported. Range 45 - 89 yrs | 24 months |
| PS | 152 | |||
| MP | 156 | |||
| BR | 201 | |||
| Scott et al32,69 2014 and 2018 | PS | 56 | 64 yrs | 24 months |
| AS | 55 | 61 yrs | ||
| Schimmel et al22> 2014 | PS | 62 | Not Reported: Range 40 – 70 yrs | 12 months |
| BCS | 62 | |||
| Molt et al28 2014 | CR | 21 | 67 yrs | 24 months |
| PS | 26 | 67 yrs | ||
| Sur et al33 2015 | PS | 22 | 68 yrs | 60 months |
| AS | 22 | 68 yrs | ||
| Scarvell et al21 2017 | PS | 124 | 67 yrs | 24 months |
| BCS | 116 | 67 yrs | ||
| Beaupre et al49 2017 | CR | 51 | 69 yrs | 24 Months |
| PS | 49 | 70 yrs | ||
| Rajgopal et al31 2017 | CR | 105 | Not Reported | 24 Months |
| AS | 105 | |||
| Nishitani et al29 2018 | MP | 33 | 74 yrs | 24 Months |
| AS | 32 | 74 yrs | ||
| Brown et al50 2019 | CR | 15 | 69 yrs | 12 Months |
| PS | 11 | 66 yrs | ||
| VandenBoom et al35 2019 | CR | 59 | 70 yrs | 12 Months |
| PS | 55 | 73 yrs | ||
| Jang et al25 2019 | PS | 45 | 70 yrs | 24 Months |
| AS | 45 | 70 yrs | ||
| Batra et al37 2020 | PS | 53 | 62 yrs | 6 Months |
| MP | 53 | 62 yrs | ||
| Akti et al12 2020 | PS | 33 | 68 yrs | 12 Months |
| AS | 32 | 69 yrs | ||
| Kulshrestha et al26 2020 | PS | 37 | 66 yrs | 24 Months |
| MP | 36 | 64 yrs | ||
| Edelstein et al53 2020 | PS | 25 | 64 yrs | 24 Months |
| MP | 25 | 67 yrs | ||
| Dowsey et al55 2020 | CR | 27 | 70 yrs | 12 Months |
| PS | 26 | 66 yrs | ||
| MP | 29 | 66 yrs | ||
| Troelsen et al18 2020 | CR | 22 | 70 yrs | 24 Months |
| BR | 23 | 68 yrs | ||
| Han et al23 2020 | PS | 34 | 67 yrs | 24 Months |
| AS | 34 | 67 yrs | ||
| Kim et al52 2021 | PS | 50 | 68 yrs | 24 months |
| AS | 50 | 68 yrs | ||
| Chang et al54 2021 | PS | 40 | 69 yrs | 24 months |
| MP | 39 | 68 yrs | ||
| Lynch et al58 2021 | CR | 20 | 70 yrs | 24 Months |
| PS | 17 | 70 yrs |
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57-63. doi:10.1007/s11999-009-1119-9 [DOI] [PMC free article] [PubMed]
- 2. Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of Prospective studies in unselected patients. BMJ Open. 2012;2(1):1-12. doi:10.1136/bmjopen-2011-000435 [DOI] [PMC free article] [PubMed]
- 3. Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today-has anything changed after 10 years? J Arthroplasty. 2013;29(9):1774-1778. doi:10.1016/j.arth.2013.07.024 [DOI] [PubMed]
- 4. Ritter MA, Berend ME, Meding JB, Keating EM, Faris PM, Crites BM. Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop Relat Res. 2001;(388):51-57. doi:10.1097/00003086-200107000-00009 [DOI] [PubMed]
- 5. Whiteside LA. Cementless total knee replacement: Nine- to 11-year results and 10-year survivorship analysis. Clin Orthop Relat Res. 1994;(309):185-192. [PubMed]
- 6. Partridge TCJ, Baker PN, Jameson SS, Mason J, Reed MR, Deehan DJ. Conventional Versus Highly Cross-Linked Polyethylene in Primary Total Knee Replacement. J Bone Jt Surg. 2020;102(2):119-127. doi:10.2106/jbjs.19.00031 [DOI] [PubMed]
- 7. Vertullo CJ, Lewis PL, Lorimer M, Graves SE. The effect on long-term survivorship of surgeon preference for posterior-stabilized or minimally stabilized total knee replacement an analysis of 63,416 prostheses from the Australian Orthopaedic Association national joint replacement registry. J Bone Jt Surg - Am Vol. 2017;99(13):1129-1139. doi:10.2106/JBJS.16.01083 [DOI] [PubMed]
- 8. Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393(10172):655-663. doi:10.1016/s0140-6736(18)32531-5 [DOI] [PMC free article] [PubMed]
- 9. Gray HA, Guan S, Young TJ, Dowsey MM, Choong PF, Pandy MG. Comparison of posterior-stabilized, cruciate-retaining, and medial-stabilized knee implant motion during gait. J Orthop Res. 2020;38(8):1753-1768. doi:10.1002/jor.24613 [DOI] [PubMed]
- 10. Varadarajan K, Zumbrunn T, Rubash HE, Malchau H, Li G, Muratoglu O. Cruciate Retaining Implant With Biomimetic Articular Surface to Reproduce Activity Dependent Kinematics of the Normal Knee. J Arthroplasty. 2015;30(12):2149-2153.e2. doi:10.1016/j.arth.2015.06.018 [DOI] [PubMed]
- 11. Purudappa PP, Ramanan SP, Tripathy SK, Varatharaj S, Mounasamy V, Sambandam SN. Intra-operative fractures in primary total knee arthroplasty - a systematic review. Knee Surg Relat Res. 2020;32(1):1-13. doi:10.1186/s43019-020-00054-3 [DOI] [PMC free article] [PubMed]
- 12. Akti S, Karakus D, Sezgin EA, Cankaya D. No differences in clinical outcomes or isokinetic performance between cruciate-substituting ultra-congruent and posterior stabilized total knee arthroplasties: a randomized controlled trial. Knee Surgery, Sport Traumatol Arthrosc. 2020;(0123456789). doi:10.1007/s00167-020-06275-z [DOI] [PubMed]
- 13. Daniilidis K, Skwara A, Vieth V, et al. Highly conforming polyethylene inlays reduce the in vivo variability of knee joint kinematics after total knee arthroplasty. Knee. 2012;19(4):260-265. doi:10.1016/j.knee.2011.04.001 [DOI] [PubMed]
- 14. Heyse TJ, Becher C, Kron N, et al. Patellofemoral pressure after TKA in vitro: Highly conforming vs. posterior stabilized inlays. Arch Orthop Trauma Surg. 2010;130(2):191-196. doi:10.1007/s00402-009-0920-y [DOI] [PubMed]
- 15. Mazzucchelli L, Deledda D, Rosso F, et al. Cruciate retaining and cruciate substituting ultra-congruent insert. Ann Transl Med. 2016;4(1):1-7. doi:10.3978/j.issn.2305-5839.2015.12.52 [DOI] [PMC free article] [PubMed]
- 16. Barnes CL, Lincoln D, Wilson B, Bushmaier M. Knee manipulation after total knee arthroplasty: comparison of two implant designs. J Surg Orthop Adv. 2013;157(9). [DOI] [PubMed]
- 17. Pritchett JW. Patients Prefer A Bicruciate-Retaining or the Medial Pivot Total Knee Prosthesis. Journal of Arthroplasty. 2011;26(2):224-228. doi:10.1016/j.arth.2010.02.012 [DOI] [PubMed]
- 18. Troelsen A, Ingelsrud LH, Thomsen MG, Muharemovic O, Otte KS, Husted H. Are There Differences in Micromotion on Radiostereometric Analysis Between Bicruciate and Cruciate-retaining Designs in TKA? A Randomized Controlled Trial. Clin Orthop Relat Res. 2020;478(9):2045-2053. doi:10.1097/corr.0000000000001077 [DOI] [PMC free article] [PubMed]
- 19. Ward TR, Burns AW, Gillespie MJ, Scarvell JM, Smith PN. Bicruciate-stabilised total knee replacements produce more normal sagittal plane kinematics than posterior-stabilised designs. J Bone Jt Surg - Ser B. 2011;93 B(7):907-913. doi:10.1302/0301-620X.93B7.26208 [DOI] [PubMed]
- 20. van Duren BH, Pandit H, Price M, et al. Bicruciate substituting total knee replacement: How effective are the added kinematic constraints in vivo? Knee Surgery, Sport Traumatol Arthrosc. 2012;20(10):2002-2010. doi:10.1007/s00167-011-1796-2 [DOI] [PubMed]
- 21. Scarvell JM, Perriman DM, Smith PN, Campbell DG, Bruce WJM, Nivbrant B. Total Knee Arthroplasty Using Bicruciate-Stabilized or Posterior-Stabilized Knee Implants Provided Comparable Outcomes at 2 Years: A Prospective, Multicenter, Randomized, Controlled, Clinical Trial of Patient Outcomes. J Arthroplasty. 2017;32(11):3356-3363.e1. doi:10.1016/j.arth.2017.05.032 [DOI] [PubMed]
- 22. Schimmel JJP, Defoort KC, Heesterbeek PJC, Wymenga AB, Jacobs WCH, Van Hellemondt GG. Bicruciate substituting design does not improve maximal flexion in total knee arthroplasty: A randomized controlled trial. J Bone Jt Surg - Am Vol. 2014;96(10). doi:10.2106/JBJS.M.00277 [DOI] [PubMed]
- 23. Han HS, Kang SB. Anterior-stabilized TKA is inferior to posterior-stabilized TKA in terms of postoperative posterior stability and knee flexion in osteoarthritic knees: a prospective randomized controlled trial with bilateral TKA. Knee Surgery, Sport Traumatol Arthrosc. 2020;28(10):3217-3225. doi:10.1007/s00167-019-05827-2 [DOI] [PubMed]
- 24. Harato K, Bourne RB, Victor J, Snyder M, Hart J, Ries MD. Midterm comparison of posterior cruciate-retaining versus -substituting total knee arthroplasty using the Genesis II prosthesis. A multicenter prospective randomized clinical trial. Knee. 2008;15(3):217-221. doi:10.1016/j.knee.2007.12.007 [DOI] [PubMed]
- 25. Jang SW, Kim MS, Koh IJ, Sohn S, Kim C, In Y. Comparison of Anterior-Stabilized and Posterior-Stabilized Total Knee Arthroplasty in the Same Patients: A Prospective Randomized Study. J Arthroplasty. 2019;34(8):1682-1689. doi:10.1016/j.arth.2019.03.062 [DOI] [PubMed]
- 26. Kulshrestha V, Sood M, Kanade S, Kumar S, Datta B, Mittal G. Early outcomes of medial pivot total knee arthroplasty compared to posterior-stabilized design: A randomized controlled trial. CiOS Clin Orthop Surg. 2020;12(2):178-186. doi:10.4055/cios19141 [DOI] [PMC free article] [PubMed]
- 27. Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19(3):349-353. doi:10.1016/j.arth.2003.09.010 [DOI] [PubMed]
- 28. Molt M, Toksvig-Larsen S. Similar early migration when comparing CR and PS in TriathlonTM TKA: A prospective randomised RSA trial. Knee. 2014;21(5):949-954. doi:10.1016/j.knee.2014.05.012 [DOI] [PubMed]
- 29. Nishitani K, Furu M, Nakamura S, et al. No differences in patient-reported outcomes between medial pivot insert and symmetrical insert in total knee arthroplasty: A randomized analysis. Knee. 2018;25(6):1254-1261. doi:10.1016/j.knee.2018.08.005 [DOI] [PubMed]
- 30. Pritchett JW. Patients Prefer A Bicruciate-Retaining or the Medial Pivot Total Knee Prosthesis. J Arthroplasty. 2011;26(2):224-228. doi:10.1016/j.arth.2010.02.012 [DOI] [PubMed]
- 31. Rajgopal A, Aggarwal K, Khurana A, Rao A, Vasdev A, Pandit H. Gait Parameters and Functional Outcomes After Total Knee Arthroplasty Using Persona Knee System With Cruciate Retaining and Ultracongruent Knee Inserts. J Arthroplasty. 2017;32(1):87-91. doi:10.1016/j.arth.2016.06.012 [DOI] [PubMed]
- 32. Scott DF. Prospective Randomized Comparison of Posterior-Stabilized Versus Condylar-Stabilized Total Knee Arthroplasty: Final Report of a Five-Year Study. J Arthroplasty. 2018;33(5):1384-1388. doi:10.1016/j.arth.2017.11.037 [DOI] [PubMed]
- 33. Sur YJ, Koh IJ, Park SW, Kim HJ, In Y. Condylar-stabilizing tibial inserts do not restore anteroposterior stability after total knee arthroplasty. J Arthroplasty. 2015;30(4):587-591. doi:10.1016/j.arth.2014.11.018 [DOI] [PubMed]
- 34. Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: Balancing the gap. J Arthroplasty. 2002;17(7):813-819. doi:10.1054/arth.2002.34814 [DOI] [PubMed]
- 35. van den Boom LGH, Brouwer RW, van den Akker-Scheek I, et al. No Difference in Recovery of Patient-Reported Outcome and Range of Motion between Cruciate Retaining and Posterior Stabilized Total Knee Arthroplasty: A Double-Blind Randomized Controlled Trial. J Knee Surg. Published online 2019. doi:10.1055/s-0039-1693023 [DOI] [PubMed]
- 36. Victor J, Banks S, Bellemans J, Victor J, Banks S, Bellemans J. Kinematics of posterior cruciate ligament-retaining and-substituting total knee arthroplasty A PROSPECTIVE RANDOMISED OUTCOME STUDY. J BONE Jt Surg. Published online 2005. doi:10.1302/0301-620X.87B5 [DOI] [PubMed]
- 37. Batra S, Malhotra R, Kumar V, Srivastava DN, Backstein D, Pandit H. Superior patient satisfaction in medial pivot as compared to posterior stabilized total knee arthroplasty: a prospective randomized study. Knee Surgery, Sport Traumatol Arthrosc. 2020;(0123456789). doi:10.1007/s00167-020-06343-4 [DOI] [PubMed]
- 38. Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(7829). doi:10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed]
- 39. McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55-61. doi:10.1002/jrsm.1411 [DOI] [PubMed]
- 40. Armijo-Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J Eval Clin Pract. 2012;18(1):12-18. doi:10.1111/j.1365-2753.2010.01516.x [DOI] [PubMed]
- 41. Higgins JP, Altman DG. Assessing Risk of Bias in Included Studies. Wiley Online Library; 2008. doi:10.1002/9780470712184.ch8
- 42. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:1-10. doi:10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed]
- 43. Owen RK, Bradbury N, Xin Y, Cooper N, Sutton A. MetaInsight: An interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res Synth Methods. 2019;10(4):569-581. doi:10.1002/jrsm.1373 [DOI] [PMC free article] [PubMed]
- 44. Gaetano J. Holm-Bonferroni Sequential Correction: An EXCEL Calculator. Published online 2013.
- 45. Lizaur-Utrilla A, Gonzalez-Parreño S, Martinez-Mendez D, Miralles-Muñoz FA, Lopez-Prats FA. Minimal clinically important differences and substantial clinical benefits for Knee Society Scores. Knee Surgery, Sport Traumatol Arthrosc. 2020;28(5):1473-1478. doi:10.1007/s00167-019-05543-x [DOI] [PubMed]
- 46. Clement ND, MacDonald D, Simpson AHRW. The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc. 2014;22(8):1933-1939. doi:10.1007/s00167-013-2776-5 [DOI] [PubMed]
- 47. Suurmond R, van Rhee H, Hak T. Introduction, comparison, and validation of Meta-Essentials: A free and simple tool for meta-analysis. Res Synth Methods. 2017;8(4):537-553. doi:10.1002/jrsm.1260 [DOI] [PMC free article] [PubMed]
- 48. Deeks JJ, Higgins JP. Statistical Algorithms in Review Manager 5. Stat Methods Gr Cochrane Collab. Published online 2010:1-11. doi:10.1016/0022-2836(86)90024-0
- 49. Beaupre LA, Sharifi B, Johnston DWC. A Randomized Clinical Trial Comparing Posterior Cruciate-Stabilizing vs Posterior Cruciate-Retaining Prostheses in Primary Total Knee Arthroplasty: 10-Year Follow-Up. J Arthroplasty. 2017;32(3):818-823. doi:10.1016/j.arth.2016.08.030 [DOI] [PubMed]
- 50. Brown ML, Wendt CS, Seyler TM, Ip EH, Foxworth JL, Lang JE. Gait and Functional Outcomes Between Cruciate Retaining and Cruciate Substituting Implants in Total Knee Arthroplasty: A Prospective, Randomized Study215. J Surg Orthop Adv. 2019;28(03):16-18. doi:10.3113/jsoa.2019.0215 [PubMed]
- 51. Chaudhary R, Beaupré LA, Johnston DWC. Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses: A randomized clinical trial. J Bone Jt Surg - Ser A. 2008;90(12):2579-2586. doi:10.2106/JBJS.G.00995 [DOI] [PubMed]
- 52. Kim MS, Koh IJ, Kim CK, Choi KY, Jeon JH. Comparison of Joint Perception Between Posterior-Stabilized and Ultracongruent Total Knee Arthroplasty in the Same Patient. J Bone Jt Surg. 2021;103:44-52. [DOI] [PubMed]
- 53. Edelstein AI, Bhatt S, Wright-Chisem J, Sullivan R, Beal M, Manning DW. The Effect of Implant Design on Sagittal Plane Stability: A Randomized Trial of Medial-versus Posterior-Stabilized Total Knee Arthroplasty. J Knee Surg. 2020;33(5):452-458. doi:10.1055/s-0039-1678524 [DOI] [PubMed]
- 54. Chang JS, Kayani B, Moriarty PD, Tahmassebi JE, Haddad FS. A Prospective Randomized Controlled Trial Comparing Medial-Pivot versus Posterior-Stabilized Total Knee Arthroplasty. J Arthroplasty. Published online 2021. doi:10.1016/j.arth.2021.01.013 [DOI] [PubMed]
- 55. Dowsey MM, Gould DJ, Spelman T, Pandy MG, Choong PF. A Randomized Controlled Trial Comparing a Medial Stabilized Total Knee Prosthesis to a Cruciate Retaining and Posterior Stabilized Design: A Report of the Clinical and Functional Outcomes Following Total Knee Replacement. J Arthroplasty. 2020;35(6):1583-1590.e2. doi:10.1016/j.arth.2020.01.085 [DOI] [PubMed]
- 56. Lynch JT, Perriman DM, Scarvell JM, et al. The influence of total knee arthroplasty design on kneeling kinematics: a prospective randomized clinical trial. Bone Joint J. 2021;103-B(1):105-112. doi:10.1302/0301-620X.103B1.BJJ-2020-0958.R1 [DOI] [PubMed]
- 57. Insall JN, Dorr D, Scott R, Scott W. Knee Society Score Rationale. Clin Orthop Relat Res. 1989;26(4):13-14. [PubMed]
- 58. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80B(1):63-69. doi:10.1302/0301-620x.78b5.0780856 [DOI] [PubMed]
- 59. Longo UG, Ciuffreda M, Mannering N, et al. Outcomes of Posterior-Stabilized Compared with Cruciate-Retaining Total Knee Arthroplasty. J Knee Surg. 2018;31(4):321-340. [DOI] [PubMed]
- 60. Migliorini F, Eschweiler J, Tingart M, Rath B. Posterior-stabilized versus cruciate-retained implants for total knee arthroplasty: a meta-analysis of clinical trials. Eur J Orthop Surg Traumatol. 2019;29(4):937-946. doi:10.1007/s00590-019-02370-1 [DOI] [PubMed]
- 61. Lynch JT, Scarvell JM, Galvin CR, Smith PN, Perriman DM. Influence of component design on in vivo tibiofemoral contact patterns during kneeling after total knee arthroplasty: a systematic review and meta-analysis. Knee Surgery, Sport Traumatol Arthrosc. 2021;29(2):446-466. doi:10.1007/s00167-020-05949-y [DOI] [PubMed]
- 62. Cassar-Gheiti AJ, Jamieson PS, Radi M, Wolfstadt JI, Backstein DJ. Evaluation of the Medial Stabilized Knee Design Using Data From National Joint Registries and Current Literature. J Arthroplasty. 2020;35(7):1950-1955. doi:10.1016/j.arth.2020.02.026 [DOI] [PubMed]
- 63. Boese CK, Ebohon S, Ries C, De Faoite D. Bi-cruciate retaining total knee arthroplasty: a systematic literature review of clinical outcomes. Arch Orthop Trauma Surg. 2020;141(2):293-304. doi:10.1007/s00402-020-03622-0 [DOI] [PubMed]
- 64. Law JI, Hurst JM, Morris MJ, Berend KR, Lombardi VA, Crawford DA. Midterm Outcomes and Survivorship of Anterior Stabilized Versus Cruciate Retaining Bearing in Primary Total Knee Arthroplasty. J Arthroplasty. 2020;36(3):998-1002. doi:10.1016/j.arth.2020.09.053 [DOI] [PubMed]
- 65. Harris AI, Christen B, Malcorps JJ, et al. Midterm Performance of a Guided-Motion Bicruciate-Stabilized Total Knee System: Results From the International Study of Over 2000 Consecutive Primary Total Knee Arthroplasties. J Arthroplasty. 2019;34(7):S201-S208. doi:10.1016/j.arth.2019.02.011 [DOI] [PubMed]
- 66. Samy DA, Wolfstadt JI, Vaidee I, Backstein DJ. A Retrospective Comparison of a Medial Pivot and Posterior-Stabilized Total Knee Arthroplasty With Respect to Patient-Reported and Radiographic Outcomes. J Arthroplasty. 2018;33(5):1379-1383. doi:10.1016/j.arth.2017.11.049 [DOI] [PubMed]
- 67. Warth LC, Ishmael MK, Deckard ER, Ziemba-Davis M, Meneghini RM. Do Medial Pivot Kinematics Correlate With Patient-Reported Outcomes After Total Knee Arthroplasty? J Arthroplasty. 2017;32(8):2411-2416. doi:10.1016/j.arth.2017.03.019 [DOI] [PubMed]
- 68. Pritchett JW. Patients Prefer A Bicruciate-Retaining or the Medial Pivot Total Knee Prosthesis. J Arthroplasty. 2011;26(2):224-228. doi:10.1016/j.arth.2010.02.012 [DOI] [PubMed]
- 69. Scott DF, Smith RR. A prospective, randomized comparison of posterior stabilized versus cruciate-substituting total knee arthroplasty: A preliminary report with minimum 2-year results. J Arthroplasty. 2014;29(9):179-181. doi:10.1016/j.arth.2014.03.050 [DOI] [PubMed]