ABSTRACT
The significance of COVID-19 vaccine has been declared and this study synthesizes the attitudes and determinants in vaccination hesitancy of college students. We searched in PubMed, Web of Science, Cochrane Library and CNKI to enroll the related studies. The modified NOS was used for quality evaluation. Proportion and OR with 95% CI were pooled to estimate the acceptance rates and determinants of COVID-19 vaccination. Data of 34 studies involving 42 countries were pooled. The pooled acceptance rate of COVID-19 vaccination among all the college students was 69% and varies between countries, while medical students have a slightly higher acceptancy rate. Knowledge, trust conception, social behavior, and information sources were important for their decision. Most of the college students intended to COVID-19 vaccination, but the proportion varied among countries. Governments should strengthen credibility, convey trusted information with media influences and improve vaccination services in urging students to be vaccinated.
KEYWORDS: COVID-19, college students, vaccination hesitancy, determinants, meta-analysis
Introduction
All countries were facing an unprecedented public health challenge for the global pandemic of coronavirus disease 2019 (COVID-19).1 Vaccination is the most effective method for the blocking of prevalence of infectious diseases; by vaccine administration, many infectious diseases, such as smallpox measles and poliomyelitis were controlled or even eradicated during the past century.2–4 Researchers have proven the safety and scientific validity of COVID-19 vaccines based on large field trials, presenting a promising effective way to control the transmission of SARS-CoV-2.5 Currently, there are four main types of COVID-19 vaccines available globally, according to the different designing methods: inactivated vaccines, virus vector vaccines, subunit vaccines and nucleic acid vaccines.6–8 As of 9 October 2021, more than six billions vaccine doses against COVID-19 have been administered on a global scale.9 From the view of epidemiologists, gaining “herd immunity” by vaccination more than 67% of citizens in each country, theoretically, will block sustained transmission for COVID-19.10,11 High vaccine coverage is especially critical for growing antimicrobial resistance and booming international travel.12 Additionally, though being considerable debate for preventing transmission, vaccine uptake was proved to reduce more than 50% (from 59% to 100%) risk for severe illness of COVID-19.13–15 However, vaccine hesitancy is a barrier for getting immunity to fight against the COVID-19, which grabbed the attention of scientists and government officers.16 The Strategic Advisory Group of Experts (SAGE) Working Group on Vaccine Hesitancy defined vaccine hesitancy as a delay in acceptance or refusal of vaccination despite availability of vaccination services.17 Vaccine hesitancy has led a surge of outbreaks in vaccine-preventable diseases, for example, measle outbreak in the United States in 2011, because the vaccine coverage in communities was below the levels needed to maintain herd immunity.18
Previous studies have revealed that vaccine hesitancy is a complex phenotype, with different reasons, including different populations, environmental, agent, and host factors, varying across countries.19–22 The proportion intending to vaccinate against COVID-19 reported in the meta-analysis by Robinson et al. was .72921 and another study estimated the global COVID-19 vaccination willingness at 66.01%.23 However, the intention varies substantially between different populations, for example, the prevalence of unwillingness to vaccinate against COVID-19 in older people was 27.03%,24 while the willingness was 51% for healthcare workers.22 Sociodemographic and socioeconomic status, experiences with COVID-19, perceived risk, attitudes, beliefs, and perceptions about COVID-19, and COVID-19 vaccine were frequently studied in vaccine acceptance or refusal. In whole population studies, middle-aged and elderly people, males, higher education level, the white race, higher income was significantly associated with increased likelihood of vaccination.21,23 But in studies of healthcare workers, who was male, aged over 30 years or having a history of influenza vaccination was intending to vaccination.22 Shakeel et al. deduced that low levels of education and awareness, inefficient government efforts, and initiatives, as well as conspiracy theories and misinformation about the COVID-19 vaccine on social media may explain the different vaccine hesitancy across countries and continents.25 These facts highlighted the necessity of a comprehensive review of different populations and effective interventional educational strategy to enhance the vaccination rate, finally putting an end to this pandemic.
Although older people are at greater infection-fatality risks for COVID-19,26,27 young adults are vulnerable to coronavirus infection and more likely to transmit the virus. First, young people often work in areas at high risk for exposure to the coronavirus, such as restaurants, schools, manufactories, and retail shops. Additionally, since young people were less likely to get severe infection of COVID-19, they may have a false sense of confidence regarding their safety, with ignoring community pandemic guidelines and not wearing masks. Consistent with a report from Bruine de Bruin, adults aged under 30 years old have the higher risk than elders in getting COVID-19 infection.28 In addition, college students can be particularly affected by campus outbreaks and spread the coronavirus when they return home or go out for social activities. Therefore, college students could be an ideal population to investigate their view for COVID-19 since they are well-educated and open-minded, and supposed to be the active spreader of the pandemic.29 However, variations in vaccine acceptance in college students in different reports ranged from .64 to .86.30–33 A systematic review analyzing the worldwide COVID-19 vaccine-hesitancy in college students could provide scientific evidence for governments and non-governmental organizations to formulate strategies for the future immunization plan. Hence, the principal objective of this meta-analysis was to comprehensively investigate the intention to vaccine uptake against COVID-19 and its influencing factors among college students to promote vaccination-based interventions. Moreover, college students majoring in the health science (e.g., clinical medicine, dentistry, nursing and preventive medicine) will represent the population of healthcare workers in the future, so they would be analyzed as the subgroups.
Method
Search strategy
Medline/PubMed, the Cochrane Library, Web of Science, and the China National Knowledge Infrastructure (CNKI) were searched for articles that published up to 31 December 2021. The following Medical Subject Heading (MeSH) terms and related derivative were searched according to the corresponding search formula in the above databases: ((“COVID-19”[All Fields] OR “SARS-CoV-2”[All Fields] OR “2019-nCoV”[All Fields]) AND (“vaccination”[All Fields] OR “vaccine”[All Fields] OR “immunization”[All Fields]) AND “college students” [All Fields] OR “university students” [All Fields] OR “undergraduate students” [All Fields])). We also googled the reference lists, minutes of the meeting, and unpublished data for additional reports.
Inclusion criteria
Studies included featured the following: (1) it was a cross-sectional study; (2) it had an effective sample size >30; (3) it investigated full-time undergraduate and postgraduate students aged 18 years and above; (4) it provided odds ratios (ORs) with 95% confidence intervals (95% CIs) or enough information to calculate them. For reports investigated the same population, only the most recent study or the report with the larger number of participants was included. We defined the proportion of vaccination acceptance as the percentage of respondents who were willing to get available COVID-19 vaccines, have vaccinated or were planning to in the future.
Quality assessment
This meta-analysis followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. We reviewed and assessed the validity of included studies according to the modified Newcastle-Ottawa Scale (NOS) for cross-sectional studies.34 The total score of NOS is 10 points. Articles scored ≥6 were classified as high quality, 5 and 4 as moderate quality, ≤ 3 as low quality. Low-quality articles were excluded in further analyses.
Data extraction
The following data were extracted from the original reports: first authors, publication year, studied region, investigation time, sampling method, sample size, response rate, age, sex, vaccination intention, as well as associated adjusted variables and risk estimates (ORs with 95% CIs). When both unadjusted and adjusted estimates were available, adjusted estimates were preferred over the unadjusted ones. We have also collected the 7-day average number of new cases and cumulative confirmed cases of all research works during investigation time, provided by Johns Hopkins CSSE (if the investigation time of included studies was reported with month, we assumed it as the last day of this month).35 All data extraction, integration, and bias assessments were accomplished independently by two reviewers (Geng and Cao). Then, any discrepancies were resolved by consensus with a third reviewer (Liu). Since this meta-analysis was based on previously published studies, ethical approval, or patient consent was not required.
Statistical analysis
Because the included studies differed in sampling method, time and region of survey, and medical services, high potential heterogeneity was assumed. A random-effects model analysis was used to calculate the pooled results. The associated determinants of COVID-19 vaccination were pooled when these were not less than three studies and all studied populations had the same reference groups. The I2 statistic was used to assess heterogeneity (defined as I2 >75% as high heterogeneity). For studies with high heterogeneity, besides random-effects model, heterogeneous analysis was also conducted by hierarchical analysis, the leave-one-out method, and meta regression as well as discussion of the sensitivity. Egger’s test was used to assess publication bias. All the data were analyzed with Stata 16.0 (StataCorp, Texas, US). P < .05 (2-sided) was considered statistically significant in all analyses.
Results
Included studies and general information
A total of 34 studies were found in four databases and other sources. These articles were screened as the process presented in Figure 1, and finally 34 studies were included in the Meta-analysis. Among these studies, nine were performed in the United States,33,36–43 five in China44–48 and three in Italy,30,49,50 respectively, while three were carried out in multiple countries.31,51,52 And 15 of the studies recruited students majored in medical science (included clinical medicine, dental and nursing, etc.)31–33,37,42,47,48,51–58 and 18 studies recruited the non-medical students;30,36,38–41,43–46,49, 50,59–62 one study included the both63(Table 1). Quality scores of these studies ranged from 4 to 8 (mean ± SD: 6.1 ± 1.21), indicating generally good quality (Table 1, Table S1).
Figure 1.
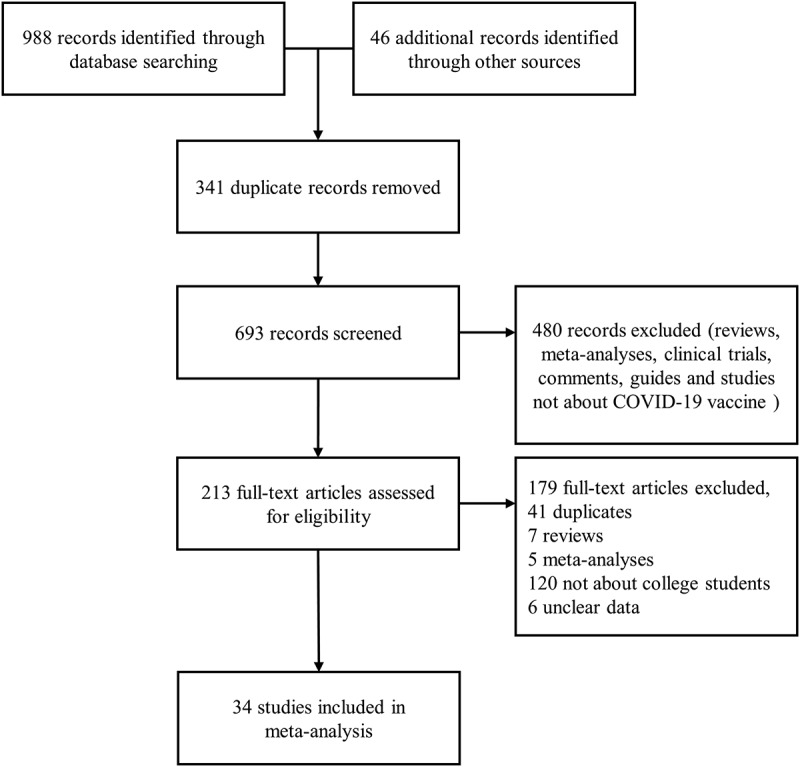
Selection flow chart of reports for inclusion in the meta-analysis.
Table 1.
Characteristics of studies on willingness to COVID-19 vaccination among college students.
| Author | Published year | Country | Survey time | Sampling method | Sample size, n | Effective response rate, % | Age, mean±SD, range or percentage | Sex, male/female |
Vaccination acceptance rate, % | Type | Quality scores |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Harapan | 2020 | Indonesia | March 2020 to April 2020 | Simplified-snowball sampling | 511 | 96.93 | NR | NR | 94.9 | Non-medical students | 7 |
| Wong | 2020 | Malaysia | April 2020 | NR | 99 | NR | NR | NR | 95.0 | Non-medical students | 7 |
| Sun | 2020 | China | March 2020 to April 2020 | NR | 1912 | NR | 20.38 ± 2.10 | 602/1390 | 64.0 | Non-medical students | 7 |
| Qiao | 2020 | US | September 2020 to October 2020 | Convenience sampling | 1062 | NR | 23.83 ± 6.66 | 211/848 | 60.6 | Non-medical students | 6 |
| Barello | 2020 | Italy | NR | NR | 735 | 81.00 | 23.60 ± 4.90 | 602/1390 | 86.1 | Non-medical students | 5 |
| Lucia | 2020 | US | NR | NR | 168 | 34 | NR | 72/96 | 53.0 | Medical students | 4 |
| Sallam | 2021 | Jordan | January 2020 | Chain-referral sampling | 1106 | NR | ≤21 years,63.8%; >21 years, 36.2% | 304/802 | 34.9 | Non-medical students | 8 |
| Pastorino | 2021 | Italy | June 2020 to July 2020 | NR | 436 | 78 | 23.09 (range: 21.32–24.74) | 129/307 | 88.5 | Non-medical students | 7 |
| Alali | 2021 | Kuwait | June 2020 to July 2020 |
NR | 592 | 25.06 | Range: 19-45 | 47/545 | 75.8 | Medical students | 4 |
| Rosental | 2021 | Israel | August 2020 to September 2020 | Opportunity sampling | 628 | NR | 28.06 ± 3.33 (MS); 26.04 ± 3.74 (NS) | 210/418 | 88.1 | Medical and nursing students | 7 |
| Cuschieri | 2021 | Malta | September 2020 to October 2020 | NR | 679 | 32.63 | 18–24 (78.50%) | 219/460 | 56.4 | Medical students | 4 |
| Kelekar | 2021 | US | September 2020, November 2020 to December 2020 | NR | 415 | 34 (Medical),18 (Dental) | NR | NR | 77.3 | Medical students | 4 |
| Silva | 2021 | US | November 2020 | NR | 237 | 44.38 | 18–29 (97%) | 82/155 | 92.0 | Non-medical students | 4 |
| Graupensperger | 2021 | US | November 2020 | NR | 647 | 46.21 | 19.77 ± 1.35 | 228/419 | 91.6 | Non-medical students | 6 |
| Yu | 2021 | China | January 2021 | Random sampling and snowball sampling | 2608 | NR | NR | 1509/1099 | 81.4 | Non-medical students | 7 |
| Szmyd | 2021 | Poland | December 2020 | NR | 1971 | NR | Medical: 20 (range: 20–24); Non-medical: 20 (range: 19–22) |
970/1001 | 92.0 | Medical students and Non-medical students | 7 |
| Bai | 2021 | China | December 2020 to January 2021 | Snowball sampling | 2881 | 99.60 | 19.83 ± 2.02 | 961/1920 | 76.3 | Non-medical students | 7 |
| Patelarou | 2021 | Greece, Albania, Cyprus, Spain, Italy, Czech Republic and Kosovo | December 2020 to January 2021 | NR | 2249 | NR | 21.60 ± 5.60 | 344/1902 | 43.8 | Nursing students | 6 |
| Tavolacci | 2021 | France | January 2021 | Convenience sampling | 3089 | 10.00 | 20.30 ± 1.90 | 883/2206 | 58.0 | Non-medical students | 5 |
| Saied | 2021 | Egypt | January 2021 | Convenience sampling | 2133 | NR | 20.24 ± 1.78 | 742/1391 | 84.1 | Medical students | 6 |
| Wu | 2021 | China | January 2021 | Snowball sampling | 116 | 99.46 | NR | NR | 81.9 | Medical students | 7 |
| Riad | 2021 | Albania, Canada, Croatia, Ecuador, Estonia, Indonesia, Iran, Iraq, Italy, Latvia, Lebanon, Lithuania, Malaysia, Nepal, Pakistan, Palestine, Portugal, Russia, Sudan, Tunisia, Turkey and US | February 2021 | NR | 6639 | NR | 22.06 ± 2.79 | 1836/4682 | 63.6 | Dental students | 5 |
| Sharma | 2021 | US | February 2021 to March 2021 | Quantitative cross-sectional and survey-based research methodology | 282 | 67.79 | 25.00 ± 7.90 | 95/177 | 47.5 | Non-medical students | 8 |
| Jain | 2021 | India | February 2021 to March 2021 | NR | 1068 | NR | NR | 549/519 | 89.4 | Medical students | 6 |
| Kecojevic | 2021 | US | February 2021 to March 2021 | Simple random sampling | 457 | 19.5 | 24.70 ± 6.38 | 109/342 | 63.7 | Non-medical students | 7 |
| Velikonja | 2021 | Slovenia, Poland and Serbia | February 2021 to March 2021 | Snow-ball sampling | 872 | 45.04 | 23.50 ± 6.50 | 97/775 | 35.0 | Nursing students | 6 |
| Gallè | 2021 | Italy | February 2021 to April 2021 | NR | 3226 | NR | 23.30 ± 3.90 | 1421/1805 | 81.3 | Non-medical students | 6 |
| Jiang | 2021 | China | March 2021 | NR | 1488 | 98.41 | <18, .34%; 18-, 10.95%; 19-, 21.91%; 20-, 19.69%; 21-, 23.99%; 22-, 16.20%; 23-, 6.96% | 234/1254 | 84.4 | Nursing students | 5 |
| Kanyike | 2021 | Uganda | March 2021 | NR | 600 | NR | 0–24, 61.2%; ≥24, 38.8% | 377/223 | 37.3 | Medical students | 7 |
| Sovicova | 2021 | Slovakia | March 2021 | NR | 1228 | 22.85 | 22 (range: 18–33) | 361/867 | 71.7 | Medical students | 6 |
| Mascarenhas | 2021 | US | 2020 | NR | 248 | NR | 26.30 ± 3.80 | 104/144 | 56.0 | Dental students | 6 |
| Synnott | 2021 | US | NR | Systematic sampling | 592 | 36.2 | NR | 206/378 | 50.5 | Non-medical students | 5 |
| Alzubaidi | 2021 | UAE | March 2021 | Heterogeneous sampling | 669 | 76.6 | 20.98 ± 3.87 | 126/543 | 68.2 | Non-medical students | 8 |
| Hossain | 2021 | Bangladesh | March 2021 to April 2021 | Convenient sampling | 900 | NR | 23.95 ± 3.38 | 502/398 | 72.7 | Non-medical students | 7 |
NR, not reported.
Acceptance of vaccination
For vaccination uptake, the result suggested that the pooled acceptance proportion of all college students (4,2543 subjects) was .69 (95% Cl: .64–.75, heterogeneity I2 = 99.5%, P < .001) (Figure 2). In subgroup analysis of regions, the pooled proportion of studies in the US was .66 (95% CI: .54–.77; heterogeneity I2 = 96.3%, P < .001), which was lower than that of China (.77, 95% CI .72–.82; heterogeneity I2 = 96.9%, P < .001). And the acceptance proportion in Italy was .85 (95% CI: .80–.90; heterogeneity I2 = 87.7%, P < .001) (Table 2, Figure S1). Since the willingness may change with pandemic of COVID-19, time of survey was also analyzed: 15 studies conducted in 2020 with a pooled willingness proportion of .72 (95% CI: .64–.80; heterogeneity I2 = 98.2%, P < .001); and 16 studies in 2021 that the pooled proportion was .70 (95% CI: .66–.74; heterogeneity I2 = 97.7%, P < .001) (Table 2, Figure S2). The pooled acceptance proportion of non-medical students was similar to medical students (.72, 95% CI: .66–.78 vs .66, 95%CI: .57–.75, P > .05) (Table 2, Figure S3). In medical students, the pooled willingness of nursing students and dental students were .60 (95% CI: .35–.85, heterogeneity I2 = 99.0%, P < .001) and .60 (95% CI: .54–.67, heterogeneity I2 = 45.7%, P = .159), respectively, which was lower than that of entire medical students with a proportion of .74 (95% CI: .67–.81, heterogeneity I2 = 97.1%, P < .001) (Table 2). In general, the acceptance rate of COVID-19 vaccination differed among countries, but neither pandemical year nor major of college students showed difference in vaccination wiliness.
Figure 2.
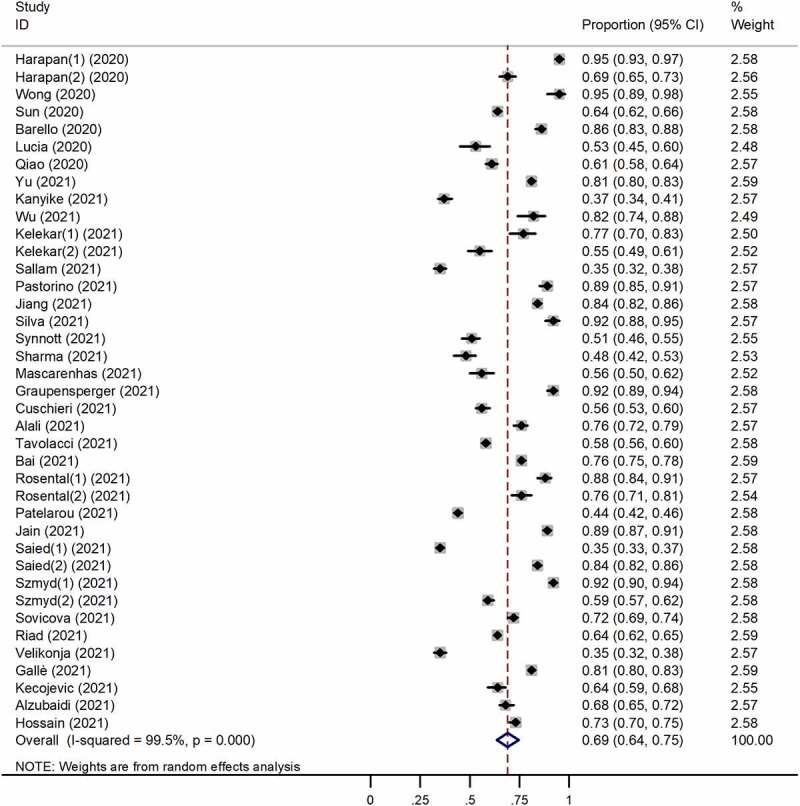
Forest plots of COVID-19 vaccine acceptance among college students.
Table 2.
COVID-19 vaccine acceptance rate among college student after subgroup analysis.
| |
|
|
Heterogeneity |
|
|---|---|---|---|---|
| Subgroup | No. of studies | Pooled rate (95% CI) | I2 (%) | P value |
| Region | ||||
| United States | 9 | 0.66 (.54–.77) | 96.3 | <.001 |
| China | 5 | 0.77 (.72–.82) | 96.9 | <.001 |
| Italy | 3 | 0.85 (.80–.90) | 87.7 | <.001 |
| Time of survey | ||||
| 2020 | 15 | 0.72 (.64–.80) | 98.2 | <.001 |
| 2021 | 16 | 0.70 (.66–.74) | 97.7 | <.001 |
| Population | ||||
| Non-medical student | 19 | 0.72 (.66–.78) | 99.3 | <.001 |
| Medical student | 16 | 0.66 (.57–.75) | 99.6 | <.001 |
| Medical student | ||||
| Medical student | 11 | 0.74 (.67–.81) | 97.1 | <.001 |
| Nursing student | 4 | 0.60 (.35–.85) | 99.0 | <.001 |
| Dental student | 3 | 0.60 (.54–.67) | 45.7 | 0.159 |
Determinants of COVID-19 vaccination acceptance in college students
After reviewing the associated determinants of COVID-19 vaccination, four types of factors were frequently analyzed: demographic characteristics (age, gender, grade, and major), experience for COVID-19 (personal or others of infection), personal views (e.g., support or concerns about COVID-19 and vaccination) and vaccination behavior (vaccination in the past 5 years) (Table 3). As shown in Table 3, age, gender, and grade presented no influence on vaccination wiliness, while medical students were associated with higher odds of intending to vaccinate than non-medical students (OR = 2.75, 95% CI: 2.00–3.50). For experience with the disease, students who had been infected with COVID-19 did not intend to vaccinate (OR = .49, 95% CI: .19–.78) but the experience of relatives or friends’ infection did not impact the intend for vaccination (OR = 1.06, 95% CI: .65–1.46). In personal view, students who were concerning about infection with COVID-19 (OR = 1.41, 95% CI: 1.05–1.78), perceived sufficient knowledge about COVID-19 (OR = 1.22, 95% CI: 1.02–1.42), the students who realized the importance of COVID-19 (OR = 1.24, 95% CI: 1.14–1.33) or supported the compulsory vaccination for public (OR = 2.33, 95% CI: 1.13–3.53) were more likely to get vaccinated. While the participants who were worries about the adverse effect (OR = .57, 95% CI: .40–.73), getting a compulsory vaccination of COVID-19 (OR = .32, 95% CI: .06–.69) made them refuse COVID-19 vaccine. Interestingly, infection risk and previous vaccine behavior showed no association with acceptance for COVID-19 vaccination.
Table 3.
Determinants of COVID-19 vaccination willingness among college students.
| Survey item | No. of studies | Pooled OR (95%CI) | Heterogeneity |
|
|---|---|---|---|---|
| I2 (%) | P value | |||
| Demographic characteristics | ||||
| Age | 12 | 1.10 (0.97-1.22) | 89.9 | <0.001 |
| Female | 12 | 0.85 (0.69-1.02) | 78.6 | <0.001 |
| Grade (senior vs junior) | 5 | 1.41 (0.95-1.87) | 82.0 | <0.001 |
| Major (medical vs non-medical) | 5 | 2.75 (2.00-3.50) | 87.9 | <0.001 |
| Experience with COVID-19 | ||||
| Self-experience of COVID-19 infection themselves | 6 | 0.49 (0.19-0.78) | 38.2 | 0.167 |
| People on whose social network getting COVID-19 infection | 6 | 1.06 (0.65-1.46) | 90.3 | <0.001 |
| People on whose social network died of COVID-19 infection | 3 | 0.89 (0.55-1.23) | 0.0 | 0.604 |
| Personal views about COVID-19 and vaccination | ||||
| Knowledge about COVID-19 vaccines | 3 | 1.22 (1.02-1.42) | 71.7 | 0.007 |
| With higher exposure risk of COVID-19 | 7 | 1.16 (0.99-1.33) | 97.8 | <0.001 |
| Concerns about getting infection with COVID-19 | 4 | 1.41 (1.05-1.78) | 90.1 | <0.001 |
| Importance of COVID-19 vaccination for individuals | 4 | 1.24 (1.14-1.33) | 0.0 | 0.870 |
| Vaccination is better than none | 3 | 0.88 (0.07-1.68) | 95.8 | <0.001 |
| Trust in vaccine information from medical experts | 4 | 2.29 (0.75-3.83) | 35.9 | 0.197 |
| Concerns about the adverse effects of COVID-19 vaccines | 6 | 0.57 (0.40-0.73) | 90.7 | <0.001 |
| Support the compulsory COVID-19 vaccination of public | 3 | 2.33 (1.13-3.53) | 42.2 | 0.177 |
| Getting vaccinated if it is compulsory | 3 | 0.32 (-0.06-0.69) | 88.8 | <0.001 |
| Vaccination Behavior | ||||
| Have other vaccination in the past five years | 9 | 1.08 (0.82-1.34) | 46.7 | 0.037 |
Other related factors excluded in meta-analysis
Since some studies have investigated some factors associated with COVID-19 vaccination but these data were insufficient for pooling, we sorted out the positive results presented in Table 4 for further discussion.
Table 4.
Determinants not included in the meta-analysis.
| Authors (year) | Item |
|---|---|
| Sun et al. (2020) |
a Lower socioeconomic status (OR=1.49, 95%CI: 1.21-1.83); a COVID-19 prosocial behaviors (OR=1.19, 95%CI: 1.07-1.33); a Perceived COVID-19 societal stigma (OR=0.86, 95%CI: 0.78-0.95); a Concerns over time necessary for participating in a medical study (OR=0.60, 95%CI: 0.43-0.83); c Informed consent signature (OR=0.55, 95%CI: 0.40-0.75). |
| Qiao et al. (2020) |
b Getting information from: scientists (OR=1.23, P=0. 240), pharmaceutical companies (OR=0.79, P=0.042). b Trusted information sources: social media (OR=0.86, P=0.037), mass media (OR=1.28, P<0.001), health agencies (OR=1.22, P=0.004), scientists (OR=1.19, P=0.033), pharmaceutical companies (OR=1.16, P=0.002). |
| Sallam et al. (2021) | a Public university (OR=2.10, 95%CI: 1.40-3.30); |
| Pastorino et al. (2021) |
b Fear about the increase in deaths (OR=1.58, 95%CI: 1.18-2.10); b Suffering from distance to friends during pandemic containment (OR=1.30, 95%CI: 1.10-1.67). |
| Kelekar et al. (2021) |
a I would like to be involved in a COVID-19 vaccine trial (OR=2.30, 95%CI: 1.53-3.47); a I am concerned that a COVID-19 vaccine may not be effective (OR=2.78, 95%CI: 1.80-4.36); a As an adult, I have ever decided not to get a vaccine for reasons other than illness or allergy (OR=0.41, 95%CI: 0.23-0.73); b The COVID-19 vaccination should be mandatory for all health care providers (OR=5.18, 95%CI: 3.15-8.76). |
| Szmyd et al. (2021) |
a Depression (OR=0.930, 95%CI: 0.867-0.997); b The fear of passing on the disease to relatives (OR=1.255, 95%CI: 1.113-1.413). |
| Bai et al. (2021) |
a Urban residents (OR=1.409, 95%CI: 1.152-1.724); a Heard about COVID-19 vaccine previously (OR=1.659, 95%CI: 1.268-2.710); a Feel vaccine could keep you free of COVID-19: yes VS no (OR=1.957, 95%CI: 1.286-2.979), not sure VS no (OR=2.009, 95%CI: 1.331-3.034); a Suggest your family to inject vaccine: yes VS no (OR=17.745, 95%CI: 12.271-25.660), not sure VS no (OR=2.580, 95%CI: 1.760-3.782). |
| Patelarou et al. (2021) |
a Working in healthcare facilities during the COVID-19 pandemic (OR=0.63, 95%CI: 0.48-0.82); a Trust in government (OR=1.85, 95%CI: 1.49-2.29); |
| Saied et al. (2021) | a Self‐perception of own health status: bad VS very bad (OR=1.196, 95%CI: 0.436-3.279), average VS very bad (OR=0.506, 95%CI: 0.282-0.909), good VS very bad (OR=0.675, 95%CI: 0.499-0.913), very good VS very bad (OR=0.733, 95%CI: 0.566-0.950). |
| Kecojevic et al. (2021) |
a Positive Attitude regarding COVID-19 vaccine (OR=1.16, 95%CI: 1.04-1.29); b Family member or friend received COVID-19 vaccine (OR=5.03, 95%CI: 2.00-2.60). |
| Kanyike et al. (2021) |
a Marital status: single VS married (OR=2.1, 95%CI: 1.1-3.9). a I have ever been reluctant or hesitate to get a vaccination before (OR=0.60, 95%CI: 0.40-0.90). |
| Alzubaidi et al. (2021) |
a Positive beliefs and attitudes toward the COVID19 vaccination (OR=1.336, 95%CI: 1.122-1.590); a Believing that social distancing would not need to be followed if vaccinated (OR=0.890, 95%CI: 0.812-0.976); c Perceiving easy access to a vaccination center (OR=1.220, 95%CI: 1.100-1.353). |
aIndividual factors, bSocial environmental factors, cVaccine or vaccination service factors.
Social environmental factors were important for vaccination wiliness. Fear of the increasing deaths, suffering from distance to friends during pandemic containment or concerns for passing the virus to relatives made them more likely to accept COVID-19 vaccine.49,63 And COVID-19 vaccine uptake of respondents’ relatives or friends also have a beneficial impact on their attitudes and behaviors (e.g., advising relatives and friends to vaccinate).41,46 Surprisingly, the information sources of the COVID-19 affected the respondents’ attitude toward vaccination. If scientists disseminated vaccine knowledge, it would be conducive to the students’ vaccination. The information from mass media, health agencies, and pharmaceutical companies was trusted by college students and improved their willingness to vaccination, implying the importance of media in information transmission for college students.36 Pharmaceutical companies’ information as sources of COVID-19 vaccine did not promote vaccine reception. Information of COVID-19 vaccine from social media and students who had hesitancy of other vaccines were more reluctant to accept COVID-19 vaccine as well36,57 (Table 4). And suffering high levels of stigmatization hindered the COVID-19 vaccination.44 Vaccine or vaccination service factors also influence the vaccination acceptance rate for COVID-19. Signing informed consent documents before vaccination could reduce the wiliness for vaccination but perceiving easy access to a vaccination center increase the acceptance rate.44
Sensitivity analysis and publication bias
Because of heterogeneity of the pooled results, we conducted a sensitivity analysis of all the studies (Figure 3). We found slightly significant publication bias in 34 studies (P = .041). Four studies (Sallam et al., Patelarou et al., Velikonja et al. and Kanyike et al.) significantly affected the heterogeneity of merged results.51,52,57,61 Among them, two (Patelarou et al. and Velikonja et al.) were joint surveys of multiple countries51, 52and the other two performed in Jordan and Uganda where had no new case reported during the surveys.57, 64 Though the investigating time, regions, new cases, and cumulative cases were included for meta-regression analysis, no significant factors were observed (Table S2). After excluding four studies above, no significant graphic or statistical bias was identified by linear regression analysis (Egger’s test) (P = .188) (Figure 4).
Figure 3.
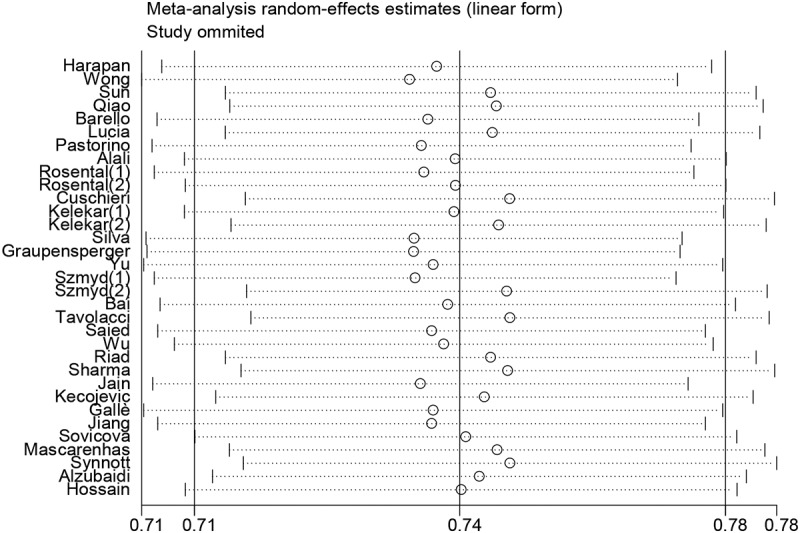
Sensitivity analyses for difference.
Figure 4.
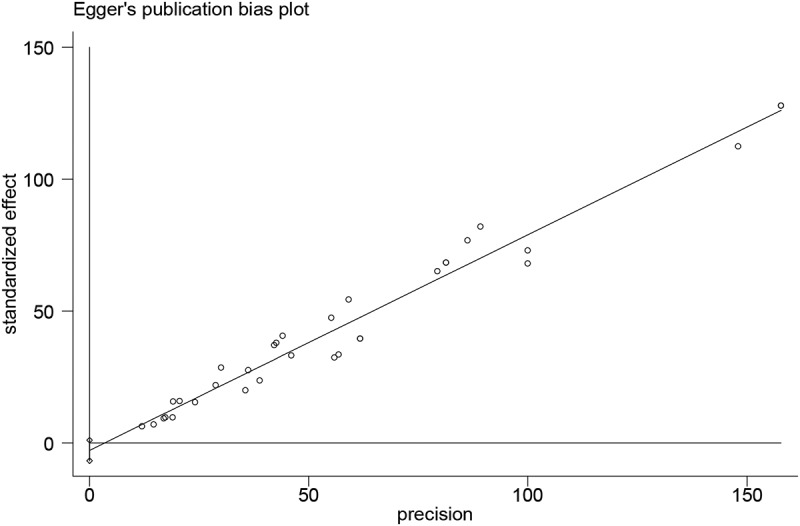
Egger’s plots of publication bias for the studies in this meta-analysis.
Discussion
Global public health system is facing unprecedented challenges because of the pandemic of COVID-19. High vaccination coverage for “herd immunity” globally was critical to end the pandemic,65, 66 and commercialized vaccines demonstrating high protection rate were authorized to prevent the infection. However, young people, though at greater risk for exposure and virus transmission, was less likely to uptake COVID-19 vaccine.67 As the most active youth group,college students were prone to suffering from outbreaks of COVID-19. Investigation on the willingness and associated factors of college students’ vaccination hesitancy would be favorable evidence for the government to formulation policies to promote vaccination. In our study, we systematic reviewed the acceptance proportion of COVID-19 among college students and determinants of willingness for vaccine uptake based on existing studies, suggesting the necessity of knowledge education and belief promotion for young adults, as well as the importance of credibility of government.
Overall, the acceptance proportion of COVID-19 vaccine in college students was about .70 on a global scale. There were great differences in college students’ attitudes toward COVID-19 vaccines in different countries.68 In Europe, the lowest vaccination intention was 13% (also the lowest in all studied countries), revealed by an investigation in Slovenia, Poland, and Serbia by Velikonja et al.52 And the study by Patelarou et al. including seven European countries reported a second lowest vaccination intention (44%),51 among which Kosovo (38.5%), Albania (32.6%) and Czech Republic (21.4%) presented the low acceptance proportions. Surprisingly, Italian college students’ willingness to vaccinate were comparatively high (.85, 95% CI: .80, .90). This could be explained by the impact of the rapidly increased cases in campus, leading to social isolation, concern for personal health and psychological distress.69,70 The rates in some other countries were also significantly lower, such as Jordan (35%), Uganda (37%), and some investigations of multination.51,52,57,61 This may be due to that no new cases were reported in Jordan and Uganda during the time of the surveys.57,61 Additionally, major knowledge gaps and inequities in vaccine distribution could also be the reasons for low intentions in Uganda.71,72 An effective international mutual aid system named COVAX, has been set up to help African countries achieve equal distribution of vaccine, effective preservation, and vaccination due to their difficulties in vaccine access.71 Comparatively, college students from Asian countries had relatively higher acceptance (Indonesia: 94.9%, Malaysia: 95.0%, Israel: 88.1%, India: 89.4%, the pooled proportion of China: 77.0%). The phenomenon was not limited to college student groups; a meta-analysis of the public by Sallam et al. showed that the entire population acceptance of COVID-19 vaccine were comparatively high in East and Southeast Asia.64 College students in the US, Europe and Africa were relatively less willing to receive the COVID-19 vaccine. The results were almost consistent with previous studies of the public,64 which may be the results of the public’s concerns about the effectiveness and safety of vaccines in different regions, from a study which reported an emerging inverse relationship between vaccine sentiments and socio-economic status.73 Correspondingly, the acceptance proportion of college student in the U.S. were lower. The conspiracy theories, “Gates had himself created the virus” for example, were proved to be barriers to controlling the spread of COVID-19 in the U.S., by a resistance to both preventive behaviors and future vaccination for the virus.74 Psychologists believed that belief in conspiracy theories was driven by motives for understanding one’s environment, being safe and in control of one’s environment, and maintaining a positive image of the self and the social group, of which the first two were what people needed during the pandemic of COVID-19.75 It is not possible to stop people from spreading ill-founded rumors but effective strategies would slowdown the spread of rumors.76 To improve the vaccine acceptance rate, government institutions should first and foremost implement strategies to eliminate the concerns about COVID-19 vaccines.
Our finding also indicated the importance of the trust in government is, as well as trustworthy sources of information and reliable guidance, especially in an uncertain and rapidly changing situation like COVID-19 pandemic, in that personal views about COVID-19 and vaccine were substantial determinants on college students’ vaccine hesitation; studies have suggested that vaccination trust was not only dependent on vaccine knowledge but also comes from trust in authorities, health professionals, government, or public health institutions.36,77 A global survey of the potential acceptance of a COVID-19 vaccine revealed that participants reporting higher levels of trust in information from government were more likely to be vaccinated, with the fact that acceptance in countries with strong trust in central governments (China, South Korea and Singapore) tend to exceed 80%.20 An example of how government ruined the government credibility is Philippines, whose Food and Drug Authority (FDA) overturned the stipulations that the emergency use of authorization of China vaccine Sinovac was not granted for health frontliners and the elderly and those with comorbidities in February 2021, inducing distrust in governments and experts, as well as misinformation or rumors, widespread.78 Additionally, response to vaccination in media of public figures, like football players, actors, and leaders, may urge students to get vaccinated. According to the results of Qiao et al., students obtained information on the COVID-19 vaccine from mass media, health agencies, and scientists would increase the likelihood of vaccination.36 Dissemination of scientific information by mainstream media or influencer would be beneficial for increase in the public (college students included) vaccination acceptance rate for COVID-19; since the willingness of college students was consistently associated with that of entire population in different countries, indicating the influence of overall social circumstances and policies of the country.21 However, any negative news or attitude related to COVID-19 vaccine may weaken public confidence in vaccination, with the fact that 22% of Brazilians, raising for 9% in 4 months, refuse to be vaccinated since their president expressed his refusal for vaccines against COVID-19 in local media.79 Therefore, more efforts are needed to strengthen the credibility of government and the utility of media influences, providing honest information about the benefits and risks of immunization, which would also mitigate their negative impact of rumors.
Intriguingly, vaccine hesitation is not directly related to vaccination behavior, in the fact that people still felt hesitant even after get vaccinated.18 The reasons are complex.80 A review suggested that vaccination hesitancy involved emotional, cultural, social, spiritual, and political factors, as well as cognitive factor.80 And most of factors were separately or simultaneously investigated in the studies included in our meta-analysis. Among them, experience with COVID-19, personal views about COVID-19 and vaccination, and vaccination behavior were the most frequently asked questions, and some of them were significantly correlated with vaccination hesitancy of college students. Notably, researchers explored some social, political, and cultural elements that may promote the acceptance by college students (Tables 3 and 4). College students are knowledgeable, full of energy and creativity, fast accessing for information and in the stage of concepts and values formation, but emotional and fear of restraint. So, if they knew the outcomes of infection and perceived the importance of vaccine uptake, they would weight and take actions (Table 3).33,42,44,58,63,81–83 However, mandatory vaccination and consent signature (though have to) would reduce the wiliness for vaccination in college students. Also, they were easily affected by conspiracy ideation (discussed above), religiosity and political position, as well as distance requirement and quarantine rules in pandemic.71,84 Even though, they have a sense of responsibility toward society, e.g., the fear of passing virus to relatives make them acceptable for vaccination,63 while they also concern about the increasing deaths due to COVID-19 infection.49 And they were also encouraged and affected by friends or relatives, because they enjoyed sharing their life (e.g., vaccination experiences) or information of COVID-19 (e.g., vaccination information).85 Utilizing the media resources mentioned above would greatly promote the vaccination wiliness of college students. In addition, it was interesting that students who had self-experience of COVID-19 infection were not willing to get vaccination. The result could be explained by the misconception of passive immunity86 and implied that the COVID pandemic should be controlled by active prevention, because the herd immunity from natural infection of most population may suffer from stronger hesitancy or even vaccination resistance if another virus attacks. Last but not the least, available and convenient vaccine or vaccination service were important drivers for college students to get vaccinated,33,41,42,58 and it was also the main reason for vaccine hesitation in economically backward areas.87 For Africa and other areas, the supply of the vaccine should be the priority.
The acceptance of COVID-19 vaccine between non-medical students and medical students were similar. After adjusting for other factors, medical students appeared to have a substantially higher rate of willingness. Among medical students, the willingness of nursing and dental students was significantly lower than that of other medical students. It is noteworthy that dentists and nurses might undergo the higher risk for the SARS-CoV-2 virus exposure due to the intimate contact with patients and the aerosols and droplets containing viruses.5,88 Mandated vaccination could not maximize the social responsibility of healthcare workers but medical health personnel should be the advocates and educators in against COVID-19.89 Since recommended by healthcare workers, vaccine confidence and self-efficacy would increase intention for vaccination in public health, education in medical students were significantly meaningful for improving the perceptions against the pandemic in entire population. On the other hand, the influencing factors of vaccine hesitation can be divided into three categories: individual factors, social environmental factors, vaccine or vaccination service factors.17 For individual factors, gender, age, and grades did not affect intention of COVID-19 vaccination of college students in our study while previous studies found that gender and age influenced vaccination acceptance in the public and healthcare workers.21,22 It might be explained by the diversity of values and knowledge in all population with wider age ranges, another possible reason was that college students’ active social behavior, and the age and gender difference would be covered.
This systematic review has the limitations. First, considering the inevitable heterogeneity of the pooled results, in addition to the random effect model and hierarchical analysis, we also performed sensitivity analysis and meta regression to identify the source of heterogeneity. In the sensitivity analysis, we found that four studies had a great impact on the pooled results.51,52,57,64 Based on these results, we considered that the investigation time, region, new cases and cumulative cases might affect the pooled results. However, meta regression showed no significant results. Moreover, more determined factors and reasonable indicators should be considered in the future research. In addition,due to the process of review and publication, this study cannot provide the latest meta results. And small sample sizes and sources of different countries which might inevitably cause some bias. Thus, more research on vaccination wiliness in college students is still needed in the future. Finally, the included studies only considered college students rather than the entire population, which might make our study within limits.
Conclusion
In conclusion, most of the college students intend to accept vaccination of COVID-19 and the proportion varied among countries. The lower acceptance proportion in some countries needs more attention. Medical students were more likely to accept the COVID-19 vaccine. Knowledge of COVID-19, trust conception and social behavior were important determinants in students’ vaccination wiliness. Vaccine information on social media significantly impacts the vaccine acceptance among college students. For governments, strengthening credibility and conveying trusted information with media influences, as well as improving vaccination services, are critical in urging college students to be vaccinated.
Supplementary Material
Acknowledgments
Thanks to all the authors of the studies on vaccination hesitancy.
Funding Statement
The Science and Technology Planning Project of Shantou (180712174010611); Special Fund for Science and Technology of Guangdong Province (no.: SFK2020-53-42); Special Grant for Key Area Programs of Guangdong Department of Education (no.: 2021ZDZX2023).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Author contributions
Conceptualization, C.L. and H.G.; data extraction and analysis, H.G., K.C. and J.Z.; draft writing, H.G.; manuscript reviewing, C.L., G.W. and K.W.; project administration, G.W. and K.W. All authors have read and agreed to the published version of the manuscript.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2054260.
References
- 1.Sohrabi C, Alsafi Z, O’-Neill N, Khan M, Kerwan A, Al-Jabir A, Iosifidis C, Agha R.. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–13. PMID: 32112977. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Initiative, G.P.E. Global eradication of wild poliovirus type 2 declared. Geneva: World Health Organization; 2015. Sep 20 [accessed 2022 Jan 29]. https://polioeradication.org/news-post/global-eradication-of-wild-poliovirus-type-2-declared/. [Google Scholar]
- 3.Measles . Progress towards global control and regional elimination, 1998-1999. Wkly Epidemiol Rec. 1999;74(50):429–34. PMID: 10647325. [PubMed] [Google Scholar]
- 4.Strassburg MA. The global eradication of smallpox. Am J Infect Control. 1982;10(2):53–59. PMID: 7044193. doi: 10.1016/0196-6553(82)90003-7. [DOI] [PubMed] [Google Scholar]
- 5.Meethil AP, Saraswat S, Chaudhary PP, Dabdoub SM, Kumar PS. Sources of SARS-CoV-2 and other microorganisms in dental aerosols. J Dent Res. 2021;100(8):817–23. PMID: 33977764. doi: 10.1177/00220345211015948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadoff J, Gray G, Vandebosch A, Cardenas V, Shukarev G, Grinsztejn B, Goepfert PA, Truyers C, Fennema H, Spiessens B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201. PMID: 33882225. doi: 10.1056/NEJMoa2101544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richmond P, Hatchuel L, Dong M, Ma B, Hu B, Smolenov I, Li P, Liang P, Han HH, Liang J, et al. Safety and immunogenicity of S-Trimer (SCB-2019), a protein subunit vaccine candidate for COVID-19 in healthy adults: a phase 1, randomised, double-blind, placebo-controlled trial. Lancet. 2021;397(10275):682–94. PMID: 33524311. doi: 10.1016/S0140-6736(21)00241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh EE, Frenck RW Jr., Falsey AR, Kitchin N, Absalon J, Gurtman A, Lockhart S, Neuzil K, Mulligan MJ, Bailey R, et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N Engl J Med. 2020;383(25):2439–50. PMID: 33053279. doi: 10.1056/NEJMoa2027906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.W.H.O . WHO Coronavirus (COVID-19) dashboard; [accessed 2022. Jan 29]. https://covid19.who.int/.
- 10.Iboi EA, Ngonghala CN, Gumel AB. Will an imperfect vaccine curtail the COVID-19 pandemic in the U.S? Infect Dis Model. 2020;5:510–24. PMID: 32835142. doi: 10.1016/j.idm.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Randolph HE, Barreiro LB. Herd immunity: understanding COVID-19. Immunity. 2020;52(5):737–41. PMID: 32433946. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff TA, et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–46. PMID: 18297169. doi: 10.2471/blt.07.040089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature. 2021;591(7851):520–22. PMID: 33737753. doi: 10.1038/d41586-021-00728-2. [DOI] [PubMed] [Google Scholar]
- 14.Thompson MG, Pierse N, Sue Huang Q, Prasad N, Duque J, Claire Newbern E, Baker MG, Turner N, McArthur C, Team SI. Influenza vaccine effectiveness in preventing influenza-associated intensive care admissions and attenuating severe disease among adults in New Zealand 2012-2015. Vaccine. 2018;36(39):5916–25. PMID: 30077480. doi: 10.1016/j.vaccine.2018.07.028. [DOI] [PubMed] [Google Scholar]
- 15.Murillo-Zamora E, Trujillo X, Huerta M, Rios-Silva M, Mendoza-Cano O. Effectiveness of BNT162b2 COVID-19 vaccine in preventing severe symptomatic infection among healthcare workers. Medicina (Kaunas). 2021;57(8). PMID: 34440952. doi: 10.3390/medicina57080746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–79. PMID: 32785815. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDonald NE, Hesitancy SWGOV. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–64. PMID: 25896383. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 18.Bloom BR, Marcuse E, Mnookin S. Addressing vaccine hesitancy. Science. 2014;344(6182):339. PMID: 24763557. doi: 10.1126/science.1254834. [DOI] [PubMed] [Google Scholar]
- 19.Latkin CA, Dayton L, Yi G, Konstantopoulos A, Boodram B. Trust in a COVID-19 vaccine in the U.S.: a social-ecological perspective. Soc Sci Med. 2021;270:113684. PMID: 33485008. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27(2):225–28. PMID: 33082575. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39(15):2024–34. PMID: 33722411. doi: 10.1016/j.vaccine.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luo C, Yang Y, Liu Y, Zheng D, Shao L, Jin J, He Q. Intention to COVID-19 vaccination and associated factors among health care workers: a systematic review and meta-analysis of cross-sectional studies. Am J Infect Control. 2021;49(10):1295–304. PMID: 34273461. doi: 10.1016/j.ajic.2021.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines (Basel). 2021;9(10). PMID: 34696179. doi: 10.3390/vaccines9101071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Veronese N, Saccaro C, Demurtas J, Smith L, Dominguez LJ, Maggi S, Barbagallo M. Prevalence of unwillingness and uncertainty to vaccinate against COVID-19 in older people: a systematic review and meta-analysis. Ageing Res Rev. 2021;72:101489. PMID: 34662744. doi: 10.1016/j.arr.2021.101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: asSystematic review of associated social and behavioral factors. Vaccines (Basel). 2022;10(1). PMID: 35062771. doi: 10.3390/vaccines10010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bonanad C, Garcia-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-Gonzalez V, Facila L, Ariza A, Nunez J, Cordero A. The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020;21(7):915–18. PMID: 32674819. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020;35(12):1123–38. PMID: 33289900. doi: 10.1007/s10654-020-00698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruine de Bruin W, Isaacowitz D. Age differences in COVID-19 risk perceptions and mental health: evidence from a national U.S. survey conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e24–e29. PMID: 32470120. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monod M, Blenkinsop A, Xi X, Hebert D, Bershan S, Tietze S, Baguelin M, Bradley VC, Chen Y, Coupland H, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021;371(6536). PMID: 33531384. doi: 10.1126/science.abe8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barello S, Nania T, Dellafiore F, Graffigna G, Caruso R. ‘Vaccine hesitancy’ among university students in Italy during the COVID-19 pandemic. Eur J Epidemiol. 2020;35(8):781–83. PMID: 32761440. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riad A, Abdulqader H, Morgado M, Domnori S, Koscik M, Mendes JJ, Klugar M, Kateeb E, Iads-Score OBO. Global prevalence and drivers of dental students’ COVID-19 vaccine hesitancy. Vaccines (Basel). 2021;9(6). PMID: 34072500. doi: 10.3390/vaccines9060566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alali WQ, AlFouzan W, Aljimi D, Al-Tawalah H, Kheirallah KA, Yimer G. Perception and awareness of COVID-19 among health science students and staff of Kuwait University: an online cross-sectional study [Preprint]. J medRxiv. 2021. PMID. 10.1101/2020.12.26.20248891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kelekar AK, Lucia VC, Afonso NM, Mascarenhas AK. COVID-19 vaccine acceptance and hesitancy among dental and medical students. J Am Dent Assoc. 2021;152(8):596–603. PMID: 34030867. doi: 10.1016/j.adaj.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, Perruolo E, Parati G, Fuchs FD, E.S.H.W.G.o.C.R.i.L.R.Settings . Panethnic Differences in Blood Pressure in Europe: a Systematic Review and Meta-Analysis. PLoS One. 2016;11(1):e0147601. PMID: 26808317. doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Csse JH . Coronavirus COVID-19 (2019-nCoV). Baltimore: Johns Hopkins; 2020. Jan 29 [accessed 2022 Jan 29]. https://gisanddata.maps.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6. [Google Scholar]
- 36.Qiao S, Friedman DB, Tam CC, Zeng C, Li X. Vaccine acceptance among college students in South Carolina: do information sources and trust in information make a difference? medRxiv. 2020. PMID: 33300004. 10.1101/2020.12.02.20242982. [DOI] [PubMed] [Google Scholar]
- 37.Lucia VC, Kelekar A, Afonso NM. COVID-19 vaccine hesitancy among medical students. J Public Health (Oxf). 2020. PMID: 33367857. 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Silva J, Bratberg J, Lemay V. COVID-19 and influenza vaccine hesitancy among college students. J Am Pharm Assoc (2003). 2021;61(6):709–14.e1. PMID: 34092517. doi: 10.1016/j.japh.2021.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Graupensperger S, Abdallah DA, Lee CM. Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine. 2021;39(15):2060–67. PMID: 33741191. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharma M, Davis RE, Wilkerson AH. COVID-19 vaccine acceptance among college students: a theory-based analysis. Int J Environ Res Public Health. 2021;18(9):4617. PMID: 33925327. doi: 10.3390/ijerph18094617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kecojevic A, Basch CH, Sullivan M, Chen YT, Davi NK. COVID-19 vaccination and intention to vaccinate among a sample of college students in New Jersey. J Community Health. 2021;46(6):1059–68. PMID: 33905034. doi: 10.1007/s10900-021-00992-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mascarenhas AK, Lucia VC, Kelekar A, Afonso NM. Dental students’ attitudes and hesitancy toward COVID-19 vaccine. J Dent Educ. 2021;85(9):1504–10. PMID: 33913152. doi: 10.1002/jdd.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Synnott CK. College students’ COVID-19 vaccine hesitancy. The Journal of Higher Education Management. 2021;36(2):152–59. PMID. doi: 10.2139/ssrn.3770915. [DOI] [Google Scholar]
- 44.Sun S, Lin D, Operario D. Interest in COVID-19 vaccine trials participation among young adults in China: willingness, reasons for hesitancy, and demographic and psychosocial determinants. medRxiv. 2020. PMID: 32699860. doi: 10.1101/2020.07.13.20152678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu TS, Yang CQ. Analysis on the willingness and influencing factors of COVID-19 vaccination among college students: an empirical study based on 2608 questionnaires (in Chinese). Teacher Education Forum. 2021;34(5):50-61. PMID. [Google Scholar]
- 46.Bai W, Cai H, Liu S, Liu H, Qi H, Chen X, Liu R, Cheung T, Su Z, Ng CH, et al. Attitudes toward COVID-19 vaccines in Chinese college students. Int J Biol Sci. 2021;17(6):1469–75. PMID: 33907510. doi: 10.7150/ijbs.58835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu WG, Deng T, Zhang MQ, Liu ZY, Pu WD, Wang JX. A survey on the attitudes towards COVID-19 vaccination and its’ sociological and psychological influencing factors (in Chinese). Chinese Journal of Clinical Psychology. 2021;29(3):622–25. PMID. doi: 10.16128/j.cnki.1005-3611.2021.03.036. [DOI] [Google Scholar]
- 48.Jiang N, Wei B, Lin H, Wang Y, Chai S, Liu W. Nursing students’ attitudes, knowledge and willingness of to receive the coronavirus disease vaccine: a cross-sectional study. Nurse Educ Pract. 2021;55:103148. PMID: 34311170. doi: 10.1016/j.nepr.2021.103148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pastorino R, Villani L, Mariani M, Ricciardi W, Graffigna G, Boccia S. Impact of COVID-19 pandemic on Flu and COVID-19 vaccination intentions among university students. Vaccines (Basel). 2021;9(2). PMID: 33498282. doi: 10.3390/vaccines9020070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Galle F, Sabella EA, Roma P, De Giglio O, Caggiano G, Tafuri S, Da Molin G, Ferracuti S, Montagna MT, Liguori G, et al. Knowledge and acceptance of COVID-19 vaccination among undergraduate students from central and Southern Italy. Vaccines (Basel). 2021;9(6). PMID: 34200835. doi: 10.3390/vaccines9060638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patelarou E, Galanis P, Mechili EA, Argyriadi A, Argyriadis A, Asimakopoulou E, Brokaj S, Bucaj J, Carmona-Torres JM, Cobo-Cuenca AI, et al. Factors influencing nursing students’ intention to accept COVID-19 vaccination: a pooled analysis of seven European countries. Nurse Educ Today. 2021;104:105010. PMID: 34126322. doi: 10.1016/j.nedt.2021.105010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kregar Velikonja N, Dobrowolska B, Stanisavljevic S, Erjavec K, Globevnik Velikonja V, Verdenik I. Attitudes of nursing students towards vaccination and other preventive measures for limitation of COVID-19 pandemic: cross-sectional study in three European countries. Healthcare (Basel). 2021;9(7). PMID: 34206217. doi: 10.3390/healthcare9070781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rosental H, Shmueli L. Integrating health behavior theories to predict COVID-19 vaccine acceptance: differences between medical students and nursing students. Vaccines (Basel). 2021;9(7). PMID: 34358199. doi: 10.3390/vaccines9070783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cuschieri S, Grech V. A comparative assessment of attitudes and hesitancy for influenza vis-a-vis COVID-19 vaccination among healthcare students and professionals in Malta. Z Gesundh Wiss. 2021:1–8. PMID: 34055572. doi: 10.1007/s10389-021-01585-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saied SM, Saied EM, Kabbash IA, Abdo SAE. Vaccine hesitancy: beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J Med Virol. 2021;93(7):4280–91. PMID: 33644891. doi: 10.1002/jmv.26910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jain J, Saurabh S, Kumar P, Verma MK, Goel AD, Gupta MK, Bhardwaj P, Raghav PR. COVID-19 vaccine hesitancy among medical students in India. Epidemiol Infect. 2021;149:e132. PMID: 34011421. doi: 10.1017/S0950268821001205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, Agira D, Wamala NK, Asiimwe A, Matovu D, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Trop Med Health. 2021;49(1):37. PMID: 33985592. doi: 10.1186/s41182-021-00331-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sovicova M, Zibolenova J, Svihrova V, Hudeckova H. Odds ratio estimation of medical students’ attitudes towards COVID-19 vaccination. Int J Environ Res Public Health. 2021;18(13):6815. PMID: 34201968. doi: 10.3390/ijerph18136815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Setiawan AM, Rajamoorthy Y, Sofyan H, Mudatsir M. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020;8:381. PMID: 32760691. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–14. PMID: 32730103. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sallam M, Dababseh D, Eid H, Hasan H, Taim D, Al-Mahzoum K, Al-Haidar A, Yaseen A, Ababneh NA, Assaf A, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18(5):2407. PMID: 33804558. doi: 10.3390/ijerph18052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tavolacci MP, Dechelotte P, Ladner J. COVID-19 vaccine acceptance, hesitancy, and resistancy among university students in France. Vaccines (Basel). 2021;9(6). PMID: 34203847. doi: 10.3390/vaccines9060654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Szmyd B, Bartoszek A, Karuga FF, Staniecka K, Blaszczyk M, Radek M. Medical students and SARS-CoV-2 vaccination: attitude and behaviors. Vaccines (Basel). 2021;9(2). PMID: 33562872. doi: 10.3390/vaccines9020128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). 2021;9(2). PMID: 33669441. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Anderson RM, Vegvari C, Truscott J, Collyer BS. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020;396(10263):1614–16. PMID: 33159850. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dong M, He F, Deng Y. How to understand herd immunity in the context of COVID-19. Viral Immunol. 2021;34(3):174–81. PMID: 33351708. doi: 10.1089/vim.2020.0195. [DOI] [PubMed] [Google Scholar]
- 67.Benham JL, Atabati O, Oxoby RJ, Mourali M, Shaffer B, Sheikh H, Boucher JC, Constantinescu C, Parsons Leigh J, Ivers NM, et al. COVID-19 vaccine-related attitudes and beliefs in Canada: national cross-sectional survey and cluster analysis. JMIR Public Health Surveill. 2021;7(12):e30424. PMID: 34779784. doi: 10.2196/30424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czajka H, Czajka S, Bilas P, Palka P, Jedrusik S, Czapkiewicz A. Who or what influences the individuals’ decision-making process regarding vaccinations? Int J Environ Res Public Health. 2020;17(12):4461. PMID: 32575879. doi: 10.3390/ijerph17124461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Romeo A, Benfante A, Castelli L, Di Tella M. PsychologicaldDistress among Italian university students compared to general workers during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(5):2503. PMID: 33802514. doi: 10.3390/ijerph18052503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Casacchia M, Cifone MG, Giusti L, Fabiani L, Gatto R, Lancia L, Cinque B, Petrucci C, Giannoni M, Ippoliti R, et al. Distance education during COVID 19: an Italian survey on the university teachers’ perspectives and their emotional conditions. BMC Med Educ. 2021;21(1):335. PMID: 34107926. doi: 10.1186/s12909-021-02780-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Aborode AT, Olofinsao OA, Osmond E, Batubo AP, Fayemiro O, Sherifdeen O, Muraina L, Obadawo BS, Ahmad S, Fajemisin EA. Equal access of COVID-19 vaccine distribution in Africa: challenges and way forward. J Med Virol. 2021;93(9):5212–15. PMID: 34009657. doi: 10.1002/jmv.27095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Petersen E, Ntoumi F, Hui DS, Abubakar A, Kramer LD, Obiero C, Tambyah PA, Blumberg L, Yapi R, Al-Abri S, et al. Emergence of new SARS-CoV-2 variant of concern Omicron (B.1.1.529) - highlights Africa’s research capabilities, but exposes major knowledge gaps, inequities of vaccine distribution, inadequacies in global COVID-19 response and control efforts. Int J Infect Dis. 2022;114:268–72. PMID: 34863925. doi: 10.1016/j.ijid.2021.11.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Larson HJ, de Figueiredo A, Xiahong Z, Schulz WS, Verger P, Johnston IG, Cook AR, Jones NS. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. PMID: 27658738. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Romer D, Jamieson KH. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020;263:113356. PMID: 32967786. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Douglas KM, Sutton RM, Cichocka A. The psychology of conspiracy theories. Curr Dir Psychol Sci. 2017;26(6):538–42. PMID: 29276345. doi: 10.1177/0963721417718261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ball P, Maxmen A. The epic battle against coronavirus misinformation and conspiracy theories. Nature. 2020;581(7809):371–74. PMID: 32461658. doi: 10.1038/d41586-020-01452-z. [DOI] [PubMed] [Google Scholar]
- 77.Wu AC, Wisler-Sher DJ, Griswold K, Colson E, Shapiro ED, Holmboe ES, Benin AL. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern Child Health J. 2008;12(6):766–73. PMID: 17987370. doi: 10.1007/s10995-007-0302-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sabahelzain MM, Hartigan-Go K, Larson HJ. The politics of Covid-19 vaccine confidence. Curr Opin Immunol. 2021;71:92–96. PMID: 34237648. doi: 10.1016/j.coi.2021.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Daniels JP. Health experts slam Bolsonaro’s vaccine comments. Lancet. 2021;397(10272):361. PMID: 33516326. doi: 10.1016/S0140-6736(21)00181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9(8):1763–73. PMID: 23584253. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brewer NT, Chapman GB, Gibbons FX, Gerrard M, McCaul KD, Weinstein ND. Meta-Analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–45. PMID: 17385964. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 82.Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. 2007;26(2):146–51. PMID: 17385965. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- 83.Healy CM, Pickering LK. How to communicate with vaccine-hesitant parents. Pediatrics. 2011;127 Suppl 1:S127–33. PMID: 21502238. doi: 10.1542/peds.2010-1722S. [DOI] [PubMed] [Google Scholar]
- 84.Knobel P, Zhao X, White KM. Do conspiracy theory and mistrust undermine people’s intention to receive the COVID-19 vaccine in Austria? J Community Psychol. 2021;50(3):1269–81. PMID: 34551127. doi: 10.1002/jcop.22714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zimmerman RK, Wolfe RM, Fox DE, Fox JR, Nowalk MP, Troy JA, Sharp LK. Vaccine criticism on the World Wide Web. J Med Internet Res. 2005;7(2):e17. PMID: 15998608. doi: 10.2196/jmir.7.2.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Betton M, Livrozet M, Planas D, Fayol A, Monel B, Vedie B, Bruel T, Tartour E, Robillard N, Manuguerra JC, et al. Sera neutralizing activities against severe acute respiratory syndrome Coronavirus 2 and multiple variants 6 months after hospitalization for Coronavirus disease 2019. Clin Infect Dis. 2021;73(6):e1337–e1344. PMID: 33851216. doi: 10.1093/cid/ciab308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shefer A, Briss P, Rodewald L, Bernier R, Strikas R, Yusuf H, Ndiaye S, Wiliams S, Pappaioanou M, Hinman AR. Improving immunization coverage rates: an evidence-based review of the literature. Epidemiol Rev. 1999;21(1):96–142. PMID: 10520476. doi: 10.1093/oxfordjournals.epirev.a017992. [DOI] [PubMed] [Google Scholar]
- 88.Magnusson K, Nygard K, Methi F, Vold L, Telle K. Occupational risk of COVID-19 in the first versus second epidemic wave in Norway, 2020. Euro Surveill. 2021;26(40). PMID: 34622761. doi: 10.2807/1560-7917.ES.2021.26.40.2001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Oberg EB, Frank E. Physicians’ health practices strongly influence patient health practices. J R Coll Physicians Edinb. 2009;39(4):290–91. PMID: 21152462. doi: 10.4997/JRCPE.2009.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


