Abstract
Background.
Alcohol use disorder predicts poor health outcomes among women returning to the community from jail. Twelve-step self-help groups are free and accessible to women leaving jail, but reaching out to strangers can pose a barrier. Pilot work suggested that a volunteer-led “warm handoff” may increase post-release twelve-step self-help group attendance.
Methods.
This randomized trial evaluated the effectiveness of a warm handoff intervention on post-release twelve-step attendance and alcohol use. Participants (189 women with alcohol use disorder) were recruited in jail and followed for 6 months after release. Participants were randomized to: (1) a warm handoff, in which a female twelve-step volunteer met with each woman individually in jail and the same volunteer attended the woman’s first twelve-step meeting with her after release; or (2) enhanced standard care (a list of meetings and community resources). Outcomes included days abstinent from alcohol, drinks per drinking day, alcohol-related problems, twelve-step attendance, twelve-step affiliation, network support for abstinence, number of unprotected sexual occasions, and drug using days.
Results.
Among intervention participants, only 66% were aware that the volunteer tried to contact them after jail, only 38% reported post-jail contact with their volunteers (typically phone), and only four went to meetings with their volunteers post-release. Of 8 post-release outcomes, intervention effects differed on only one (alcohol-related problems).
Conclusion.
Although twelve-step self-help group attendance predicted alcohol abstinence, the volunteer-led warm handoff intervention did not increase twelve-step attendance. The twelve-step tradition of Attraction may inhibit the active outreach required to connect women to services after jail release.
Keywords: Jail, alcohol use disorder, women, 12-step, volunteers, criminal justice, unprotected sex, social support
1. Introduction
Ten million Americans are arrested and held in pretrial jail detention annually (Zeng, 2019). Women who are incarcerated face more severe health, financial, housing, and employment issues (O’Brien, 2001) and have greater severity of alcohol and drug addiction than do men who are incarcerated (Langan and Pelissier, 2001). Nearly 70% of women who are incarcerated have substance use disorders (Lewis, 2006; Teplin et al., 1996). More than one third of women who are incarcerated (39%) meet criteria for alcohol use disorders (AUD); more than 20% were under the influence of alcohol during the offense for which they were arrested (Karberg and James, 2005).
Delivery of alcohol treatment services in jail is challenging. Unlike prison, women in jail are either pretrial (unsentenced) and may be released on bond or are serving very short sentences. The weekly turnover rate in jails is 65% (Minton, 2011). Because women may be in jail only a few days and release times are unpredictable, professional in-jail alcohol treatment and formal post-release alcohol treatment planning are often not feasible (Center for Substance Abuse Treatment, 2005; Solomon et al., 2008). With a few exceptions (Schonbrun et al., 2011; Stein et al., 2010; Strong et al., 2010), most research has focused on prisons, rather than jails.
Discharge from jail represents a high-risk period for the resurgence of substance use and other risky behavior as women re-enter their communities and social networks (Bui and Morash, 2010; Chandler et al., 2009). Post-release alcohol use is associated with poor psychosocial, criminal, and health outcomes such as sexually transmitted infections (STIs), including HIV (Scott and Dennis, 2012; Staton-Tindall et al., 2007). Women who are justice-involved report that addiction/intoxication is the primary reason they engage in unprotected sex (Staton-Tindall et al., 2007). In our previous work with women with hazardous drinking, 42% used alcohol on their first day outside of jail, and 57% drank by the end of the first week (Clarke et al., 2011). Recovery resources that can be easily accessed in the days immediately following jail release (i.e., low-cost, little or no wait) are needed. Alcohol focused twelve-step self-help groups (AFTSSG) are free, volunteer-led, naturally occurring in most communities, and easily accessible.
AFTSSG attendance at least once per week after jail is associated with improvements in drinking and alcohol-related consequences post-incarceration (Schonbrun et al., 2011). Our previous findings indicate that most women with alcohol dependence who leave jail do not attend AFTSSG regularly. Increasing linkage to post-release community AFTSSG meetings may be helpful.
In nearly every U.S. state, there is a subsidiary group (Bridging the Gap; BTG) of AFTSSG members who are willing to serve incarcerated persons re-entering the community by taking them to AFTSSG meetings post-release. However, formerly incarcerated women make limited use of BTG services. Our pilot trials demonstrated that newly released women will reach out to individuals they came to know in jail (Johnson, Schonbrun, and Stein, 2013; Johnson, Williams, et al., 2015). Qualitative pilot work (Johnson et al., 2014; Johnson, Schonbrun, Nargiso, et al., 2013; Johnson, Schonbrun, and Stein, 2013; Johnson, Williams, et al., 2015) identified fear and distrust of strangers as a major barrier to post-release BTG and AFTSSG meeting attendance for women. Many re-entering women preferred not to make the first call post-release (even to someone they knew), and interpreted being called by providers or BTG volunteers as proving they care (Johnson, Schonbrun, and Stein, 2013; Johnson, Williams, et al., 2015). AFTSSG’s current outreach does not link women in jail to AFTSSG outside jail. Instead, it requires them to call a number and leave a message for strangers to connect with BTG services.
We conducted a small (n=14) feasibility trial of an intervention (CLEAR; Community Links to Establish Alcohol Recovery) which facilitated a BTG volunteer coming into the jail to meet the incarcerated woman, develop rapport, discuss AFTSSG meetings and principles, and arrange to contact with the woman after her discharge to attend a twelve-step meeting together (Johnson, Schonbrun, and Stein, 2013). We chose to use BTG volunteers rather than other peer-based approaches (e.g., recovery coaches), because most of the other approaches use paid staff, and jails have minimal resources for professional substance use interventions. BTG is widely available and free. Most (73%) of the women in our pilot study who saw volunteers in jail and completed the 1-month study follow-up met with their volunteers after release from jail, compared to essentially zero who initiated a call to BTG on their own in our previous work (Johnson, Williams, et al., 2015). Participants met with volunteers an average of 4 times. They reported being satisfied with CLEAR and reported pre-post improvements in drinking and drug using days.
This article reports results of a randomized controlled trial evaluating the effectiveness of the CLEAR intervention to enhance the linkage between women with AUD leaving jail and volunteer-led AFTSSG groups occurring in their communities. The standard care control condition consisted of providing women with schedules for local AFTSSG meetings and a handout of reasons to attend a meeting. This is an enhancement to standard care, which consists of no post-discharge alcohol treatment planning. Primary hypotheses were:
-
1
Among incarcerated women with AUD returning to the community from jail, adding an AFTSSG linkage intervention (CLEAR) will result in less alcohol use at follow-up relative to enhanced standard care (ESC), as indexed by more days abstinent from alcohol (primary outcome).
-
2
CLEAR will increase AFTSSG attendance/involvement and network support for abstinence relative to ESC.
Secondary hypotheses were that:
-
3
CLEAR, relative to ESC, will result in fewer unprotected sexual occasions.
-
4
AFTSSG attendance/involvement will mediate the effect of CLEAR on alcohol use
-
5
Days abstinent will mediate the effect of CLEAR on unprotected sexual occasions.
2. Method
The trial was approved by Butler Hospital’s Institutional Review Board (FWA 00000963) and by the regulatory body overseeing research at the participating jail. A three-member external Data Safety and Monitoring Board oversaw data and safety of study participants. The study had a Certificate of Confidentiality. The trial was registered at clinicaltrials.gov (NCT01970293). Study procedures are detailed in Johnson et al (2017).
2.1. Participants and recruitment
Women were recruited from a midsize Northeastern jail. Women were eligible for the study if they were: (1) 18 years or older; (2) unsentenced and did not expect to be sentenced to prison or jail time, (3) lived within 20 miles of our research offices and planned to remain in the area for the next 6 months, (4) met DSM-5 criteria (First et al., 2015; Hasin et al., 2013) for alcohol use disorder (AUD) in the last 90 days, (5) did not expect to attend residential alcohol or drug treatment upon release (residential treatment has strong independent effects on abstinence and often does not allow twelve-step volunteers to visit women), and (6) could understand study measures when they were read aloud. Women were excluded if they could not provide names of two locator persons.
We recruited 205 women between October 2013 and September 2018. Research staff screened and consented participants privately. Potential participants were informed of confidentiality of study data and that study participation would not affect their status or length of stay at the jail.
2.2. Randomization
We used permuted block randomization with a minimum block size of 6 and a 1:1 allocation ratio. The randomization sequence was created by the study statistician. Assignment was concealed in numbered envelopes, which were opened in the jail at the time of randomization. To accommodate women’s short jail stays, research assistants recruited, assessed, and randomized participants during a single day. If randomized to CLEAR, participants met with the BTG volunteer the same evening.
2.3. Post-randomization ineligibility
Our target population was unsentenced female pretrial detainees who were returning to the community. Therefore, if a woman was enrolled and randomized but was then (1) sentenced to serve prison or jail time without leaving detention, or (2) not released within 60 days, she was no longer eligible for follow-up and was included in attrition estimates. We followed all remaining participants released from jail to the community after the index incarceration regardless of re-incarceration or continued participation in CLEAR or ESC.
2.4. Interventions
2.4.1. Enhanced Standard Care (ESC).
As is the case in many jails nationally (Solomon, 2008), standard care for women in pretrial jail detention at the study site did not include any alcohol intervention. We enhanced standard care for trial participants by having the randomizing study research assistant give participants a list of local twelve-step meetings and reasons to attend meetings, and community addiction and other resources.
2.4.2. CLEAR
provided a warm handoff for women with AUD who were leaving jail to twelve-step self-help meetings in the community. The intervention is described in detail in Johnson et al (2017). Briefly, CLEAR consisted of a twelve-step volunteer coming into the jail to meet individually with the incarcerated woman. During this meeting, the volunteer developed rapport with the woman, discussed twelve-step meetings and principles (typical of a twelve-step call), and arranged to contact the woman after her discharge to attend a meeting together (Schonbrun et al., 2019). After release, the volunteer contacted the woman to take her to or meet her at her first two twelve-step meetings, and to introduce her to others at the meetings to help her feel comfortable. In partnership with BTG, we provided a brief set of instructions and talking points to volunteers.
In keeping with the twelve-step principle of Nonaffiliation (Alcoholics Anonymous, 1984), which was interpreted by BTG as prohibiting outside organizations (i.e., us) from recruiting or supervising their volunteers, BTG recruited and supervised their own volunteers (see Johnson et al., 2017 for a full discussion). The volunteers were: (1) female, (2) had been sober for at least 2 years; (3) could be cleared for entry into the jail and had attended the jail’s 4-hour volunteer training; (4) could get to the jail and meetings (either in a car or convenient access to public transportation); and (5) were perceived as responsible, invested in twelve-step service to women who were in jail, and had availability to take women to meetings. Because they needed criminal background check clearance to enter the jail, volunteers were typically not formerly incarcerated.
2.5. Assessments
Unblinded research assistants conducted assessments in person at baseline (in jail) and at 1, 3, and 6 months after jail release. They also administered the Timeline Followback interview by phone 1 week after release. Participants did not receive compensation for study baseline interviews, but were remunerated $60 each for follow-up assessments, regardless of post-release incarceration status.
2.5.1. Eligibility.
The alcohol use disorder module from the Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015) was used to determine current AUD.
2.5.2. Outcome assessment.
The Timeline Followback (TLFB) interview (Sobell et al., 1986) was used to assess days abstinent from alcohol (primary) and mean drinks per drinking day at baseline (past 90 days) and during each follow-up period. The TLFB was also used to assess secondary and exploratory outcomes including number of AFTSSG meetings attended, number of unprotected vaginal and anal sexual occasions (USOs), and drug use days (including non-prescription use of heroin/opioids, cocaine, sedatives/benzodiazepines, amphetamines, cannabis, and hallucinogens). We assessed alcohol-related problems using the Short Inventory of Problems (SIP; Miller et al., 1995). Alcohol-focused twelve-step involvement at baseline (lifetime), and during follow-up (since last assessment) was measured with the alcohol-focused twelve-step Affiliation Scale (Humphreys et al., 1998). This 9-item scale assesses a range of twelve-step experiences including having a sponsor, reading twelve-step literature, working the steps, and self-identifying as a twelve-step member. Network support for abstinence (sober support) for the past 3 months (at baseline) or since the last assessment was measured using the revised Behavioral Support for Abstinence scale of the Important People and Activities (IPA; Zywiak et al., 2009) scale.
2.5.3. Moderator assessment.
Baseline depressive symptoms were assessed with the Center for Epidemiologic Studies Short Depression Scale (CESD10; Björgvinsson et al., 2013). Baseline posttraumatic stress disorder (PTSD) symptoms were assessed with the Davidson Trauma Scale (Davidson et al., 1997).
2.5.4. Intervention characterization.
We characterized the intervention using participant self-report of volunteer contacts and topics discussed, the Working Alliance Inventory Short Form (Tracey and Kokotovic, 1989), the Empathy Scale (Burns and Auerbach, 1996), and an adapted End of Intervention Questionnaire (EIQ; Najavits et al., 1998)
2.6. Analytical methods
Primary analyses were intent-to-treat. A 2-sided α = .05 was used for tests of Hypotheses 1–5, specified a priori. Analysis of each outcome included the baseline value of the outcome as a covariate (e.g., baseline days abstinent was a covariate in analyses predicting follow-up days abstinent), intervention condition as a main effect, indicator variables for follow-up time period, and no additional covariates or predictors. A small amount of missing data made sample sizes slightly different for some outcomes.
2.6.1. Hypotheses 1–3.
Count outcomes (days abstinent, twelve-step meetings attended, unsafe sexual encounters, and drug use days) were analyzed using mixed-effects negative binomial regression models. Because it was positively skewed and did not include values less than zero, mean drinks per drinking day was also analyzed using a log link function and negative binomial error distribution. Days at risk for each follow-up period was defined as the number of days since jail release (for the first follow-up assessment) or since the most recent assessment (for subsequent follow-up assessments). Log (days at risk) was entered as an offset for days of alcohol use, times attending AFTSSG meetings, drug use days, and unsafe sexual encounters. Days at risk was adjusted for the number of self-reported nights spent incarcerated or in residential treatment in models evaluating the effect of intervention on days alcohol abstinent, number of unsafe sexual encounters, and drug use days. Days at risk was not adjusted for incarceration/residential treatment days in models predicting number of post-release twelve-step meetings attended because it is possible to attend twelve-step meetings when in jail or residential treatment. Continuous outcomes were analyzed using mixed effects linear models. We used the robust variance estimator (Rosenblum and van der Laan, 2009) for tests of significance.
2.6.2. Mediation Hypotheses (4 and 5).
As recommended by MacKinnon et al. (2002), the statistical significance of the indirect effect was assessed using bias-corrected bootstrapped standard errors.
2.6.3. Moderators.
We tested the following planned moderators of the intervention on days abstinent from alcohol with p < .01 to control for Type I error: (1) AUD severity (as indexed by number of SCID-5 criteria met), (2) past 90-day use of opioids and/or cocaine (yes/no); (3) past-year AFTSSH group attendance (yes/no), (4) network support for abstinence, (5) abstinence goal (yes/no), (6) depressive symptoms (CESD10 score), (7) PTSD symptoms (Davidson Trauma Scale score), and (8) age.
2.6.4. Dose-response analyses
examined the number of contacts with one’s volunteer after release as a predictor of days abstinent from alcohol.
2.6.5. Missing data.
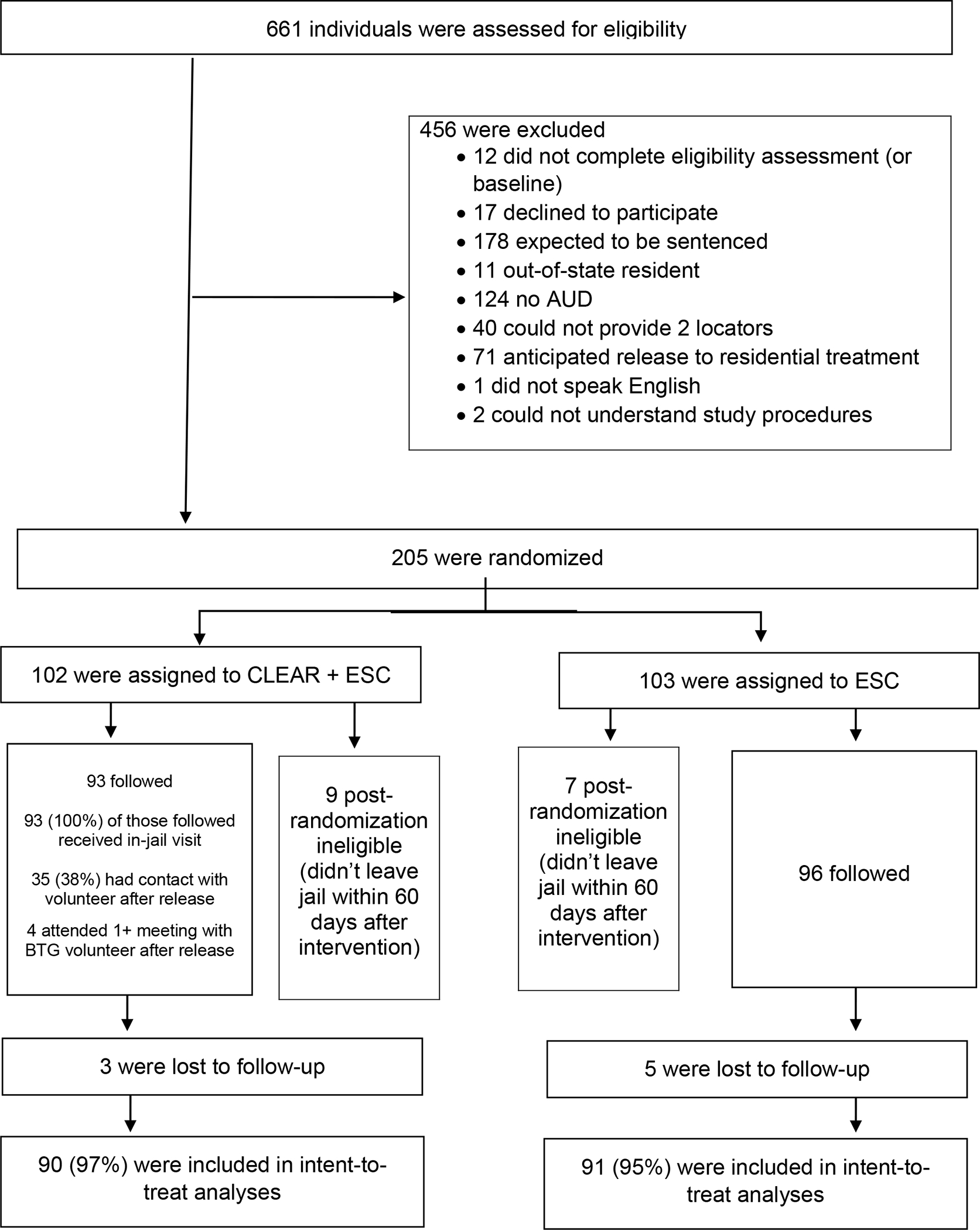
Our analyses used observed data from the 96% of study participants providing at least one follow-up assessment (Figure 1). To evaluate the sensitivity of our findings to subject attrition, we conducted separate analyses assuming that persons lost to follow-up were either alcohol abstinent or were daily drinkers.
Figure 1: Consort Diagram.
3. Results
The CONSORT Table (Figure 1) shows participant flow through the study. Descriptive statistics for the study sample are shown in Table 1. Follow-up rates were 87%, 76%, and 75% at 1, 3, and 6 months post-release, with 96% of participants completing at least one of these follow-up assessments. Outcomes are shown in Table 2.
Table 1.
Sample descriptors at baseline. Cell entries are means (± SD) or n (%).
| INTERVENTION ARM |
|||
|---|---|---|---|
| Sample (n =189) | Control (n = 96) | CLEAR (n = 93) | |
|
| |||
| Age | 35.7 (± 10.1) | 36.5 (± 10.3) | 34.8 (± 9.7) |
| Race | |||
| White | 131 (69.3%) | 65 (67.7%) | 66 (71.0%) |
| African American/Black | 26 (13.8%) | 17 (17.7%) | 9 (9.7%) |
| Native American/Alaskan Native | 5 (2.7%) | 2 (2.1%) | 3 (3.2%) |
| Asian | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Pacific Islander/Hawaiian | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Other | 17 (9.0%) | 8 (8.3%) | 9 (9.7%) |
| More than one race | 10 (5.3%) | 4 (4.2%) | 6 (6.5%) |
| Hispanic/Latina (Yes) | 19 (10.1%) | 12 (12.5%) | 7 (7.5%) |
| Years of education | 11.8 (± 2.2) | 12.0 (± 2.2) | 11.5 (± 2.2) |
| Employed full-time or part-time (Yes) | 33 (17.5%) | 18 (18.8%) | 15 (16.1%) |
| Past-year legal income | |||
| < $10,000 | 130 (68.8%) | 64 (66.7%) | 66 (71.0%) |
| $10,000 – $19,999 | 34 (18.0%) | 15 (15.6%) | 19 (20.4%) |
| $20,000 – $29.999 | 14 (7.4%) | 9 (9.4%) | 5 (5.4%) |
| $30,000 or more | 11 (5.8%) | 8 (8.3%) | 3 (3.2%) |
| Lives with partner (Yes) | 51 (27.0%) | 25 (26.0%) | 26 (30.0%) |
| Homeless (Yes) | 18 (9.5%) | 10 (10.4%) | 8 (8.6%) |
| Days incarcerated (of past 90a) | 12.5 (± 11.5) | 13.5 (± 13.2) | 11.4 (± 9.3) |
| Number of AUD criteria met (of 11) | 7.4 (± 2.5) | 7.3 (± 2.5) | 7.5 (± 2.5) |
| Non-Prescription past 90-Day Use | |||
| Heroin/Opioids (Yes) | 64 (33.9%) | 31 (32.3%) | 33 (35.5%) |
| Cocaine (Yes) | 82 (43.4%) | 45 (46.9%) | 37 (39.8%) |
| Sedatives/Benzodiazepines (Yes) | 28 (14.8%) | 17 (17.7%) | 11 (11.8%) |
| Amphetamines (Yes) | 14 (7.4%) | 7 (7.3%) | 7 (7.5%) |
| Cannabis (Yes) | 88 (46.6%) | 43 (44.8%) | 45 (48.4%) |
| Any (Yes) | 150 (79.4%) | 75 (78.2%) | 75 (80.7%) |
| Days used alcohol (0–90) | 58.3 (± 23.9) | 60.0(± 23.3) | 56.5 (± 24.4) |
| Heavy (4+ drinks) drinking days (0–90) | 50.9 (± 26.8) | 52.7 (± 25.9) | 49.1 (± 27.8) |
| Mean drinks per drinking day | 12.2 (± 10.4) | 12.4 (± 11.6) | 7.87 (± 7.3) |
| AFTSSG attendance | |||
| Ever attended (Yes) | 144 (76.2%) | 76 (79.2%) | 68 (73.1%) |
| Any past year attendance (Yes) | 85 (45.0%) | 43 (44.8%) | 42 (45.2%) |
| # Unprotected sexual occasions past 90 days | |||
| Mean | 28.7 (± 68.8) | 19.1 (± 26.5) | 38.6 (± 93.5) |
| Median (IQR) | 8 (34) | 5.5 (29.5) | 10 (59) |
| AFTSSG Affiliation Scale score (0–9) | 2.16 (± 2.25) | 2.16 ± (2.20) | 2.17 (± 2.30) |
| Alcohol-related problems (SIP score; 0–3)b | 1.99 (± 0.76) | 1.99 (± 0.77) | 1.99 (± 0.74) |
| Goal after leaving jail | |||
| Make no changes in alcohol use | 6 (3.2%) | 3 (3.1%) | 3 (3.2%) |
| Drink less | 53 (28.0%) | 26 (27.1%) | 27 (29.0%) |
| Abstinence from alcohol | 130 (68.8%) | 67 (69.8%) | 63 (67.7%) |
| CESD10 (0–30) | 18.1 (± 6.4) | 18.0 (± 6.9) | 18.1 (± 6.0) |
| Davidson Trauma Scale score (0–136) | 51.0 (± 19.2) | 51.8 (± 19.6) | 50.2 (± 18.9) |
Days incarcerated includes current and previous jail detentions over the past 90 days
Mean item scores
Table 2.
Estimated adjusted effects of the intervention on primary and secondary outcomes assessed across 6 months post release.
| Count outcomes | n = a | obs b | IRRc (95%CI)d | z (p =) d |
|
| ||||
| # Days alcohol abstinente | 178 | 567 | 1.04 (0.96; 1.12) | 0.86 (.390) |
| Mean drinks per drinking dayf | 153 | 354 | 0.95 (0.75; 1.20) | −0.47 (.639) |
| # AFTSSG meetings attended | 178 | 567 | 0.81 (0.34; 1.91) | −0.48 (.630) |
| # Unsafe sexual occasions | 178 | 567 | 1.92 (0.95; 3.94) | 1.80 (.071) |
| # Drug use days | 178 | 567 | 1.18 (0.57; 2.47) | 0.44 (.659) |
| Continuous outcomes | n = a | obs b | b (95%CI) d | z (p =) d |
|
| ||||
| AFTSSG Affiliation score | 170 | 433 | −0.07 (−0.48; 0.34) | −0.34 (.735) |
| Network support for abstinence | 168 | 421 | 0.02 (−0.20; 0.25) | 0.23 (.818) |
| Alcohol-related problems (SIP) | 170 | 433 | −0.25 (−0.48; −0.02) | −2.15 (.032) |
Number of participants available for analysis.
Total number of follow-up observations.
Incidence rate ratio estimated by mixed-effects negative binomial regression. Models included indicator variables for month of assessment and the baseline value of the outcome being evaluated.
Confidence interval estimates and tests of significance were based on the robust variance estimator (Rosenblum and van der Laan, 2009).
Observed data.
Excludes observations for which participants reported zero drinking days during assessment period.
3.1. Outcomes
3.1.1. Primary (alcohol) outcomes.
Days abstinent.
Participants randomized to CLEAR had slightly (IRR=1.04, 95%CI 0.96; 1.12, z=0.86, p=0.39) but not significantly higher adjusted mean rates of alcohol abstinence at follow-up (Table 2). Expressed as a 30 day rate, the marginal effect was 0.8 days. In the CLEAR condition, 52.7%, 30.5%, and 31.2% of participants reported abstinence from alcohol for all non-incarcerated, non-residential treatment days (days at risk) at 1-month, 3-month, and 6-month follow-ups. In the control condition, these numbers were 46.4%, 31.3%, and 26.7%, respectively.
Mean drinks per drinking day
was an additional measure of alcohol use. Controlling for baseline mean drinks per drinking day, the estimated effect of CLEAR on drinks per drinking day was not statistically significant. Estimated mean drinks per drinking day post-release were 10.2 and 9.6 in the control and intervention arms, respectively.
3.1.2. Secondary Outcomes.
AFTSSG attendance.
Participants randomized to intervention and control arms did not differ significantly in rates of AFTSSG attendance at follow-up. The median number of meetings attended in each condition was 1; 52% of women in the CLEAR condition and 53% of women in the ESC condition attended at least one AFTSSG meeting in the 6 months post-release.
AFTSSG affiliation. (Alcohol Focused twelve-step Affiliation Scale score).
Intervention arms did not differ significantly with respect to level of AFTSSG affiliation during follow-up.
Network support for abstinence.
Intervention arms did not differ significantly with respect to network support for abstinence during follow-up.
Unprotected sexual occasions (USOs).
Controlling for baseline frequency of unprotected vaginal or anal sex, the effect of intervention on number of USOs during follow-up was not statistically significant. Median USOs over the follow-up period were 6.5 and 2.0 for the CLEAR and ESC conditions, respectively.
3.1.3. Additional Outcomes.
Alcohol-related problems.
Controlling for baseline scores, participants randomized to the intervention arm had significantly less severe alcohol-related problems (SIP total scores) across follow-up assessments (p=0.032). Estimated Cohen’s d is 0.29.
Drug use days.
The intervention arms did not differ with respect to reported number of drug use days.
3.2. Mediation
Number of AFTSSG meetings attended (our hypothesized mediator of effects of CLEAR on days abstinent) predicted more days of alcohol abstinence (covarying baseline abstinence days and condition; IRR=1.004, 95% CI 1.002; 1.006, z=4.26, p<0.001). Alcohol abstinence days (our hypothesized mediator of the effects of CLEAR on USOs) did not predict USOs (IRR=0.992, 95% CI 0.985; 1.013, z=0.96, p=0.34). Our full mediation hypotheses were not tested because CLEAR did not have significant effects on mediating variables or hypothesized outcomes.
3.3. Moderators
Effects of CLEAR relative to ESC on days abstinent from alcohol did not vary by baseline AUD severity, past 90-day use of opioids or cocaine (yes/no), past-year AFTSSG attendance (yes/no), network support for abstinence, abstinence goal (yes/no), depressive symptoms, PTSD symptoms, or age.
3.4. Intervention characterization and dose-response
A total of 19 BTG volunteers met with CLEAR participants in jail for a mean of 30 (SD=14; range 9–80) minutes each. The following topics were discussed in more than 90% of in-jail meetings: the woman’s recovery story, the volunteer’s recovery story, the woman’s experience with AFTSSGs, the volunteer’s experience with AFTSSGs, and benefits of attending meetings. In more than 80% of meetings, the volunteer asked about the woman’s goals for drinking, and discussed which meetings the volunteer and woman might attend together post-release. Working Alliance Inventory, Empathy Scale, and EIQ scores (Tables 3 and 4) indicated generally positive reactions to the volunteers and intervention, but varied from negative/neutral to enthusiastic.
Table 3.
Participant-rated measures of their interactions with their volunteers*
| Scale and scoring range | M (SD) | Observed range |
|---|---|---|
| Working Alliance Inventory – Short Form total score (12 – 84) | 65.0 (11.8) | 36 – 84 |
| Agreement on goals subscale (4 – 28) | 21.5 (4.2) | 10 – 28 |
| Agreement on tasks subscale (4 – 28) | 21.9 (4.4) | 10 – 28 |
| Therapeutic bond subscale (4 – 28) | 21.6 (4.4) | 4 – 28 |
| Empathy Scale (−15 to +15) | 10.3 (4.5) | −1 to +15 |
n = 73 CLEAR intervention participants who completed the 1-month post-release assessment
Table 4.
Acceptability and fit of CLEAR volunteers and intervention*
| Slightly to very negative (n) | Neutral (n) | Slightly to very positive (n) | NA or did not occur (n) | |
|---|---|---|---|---|
| Questions related to helpfulness | ||||
| Overall, how helpful was your volunteer? | 7 | 8 | 58 | -- |
| Overall, how helpful was your in jail meeting with your volunteer? | 8 | 7 | 58 | -- |
| How helpful were the following: | ||||
| Making a connection to a new sober friend | 2 | 21 | 42 | 8 |
| Finding out more about AFTSSG | 6 | 18 | 45 | 4 |
| Strategizing how to get to an AFTSSG meeting | 5 | 17 | 42 | 9 |
| Working with my volunteer to help me feel ready to attend a meeting | 4 | 14 | 45 | 10 |
| Feeling more motivated to attend an AFTSSG meeting | 5 | 18 | 45 | 5 |
| Getting a better idea of what an AFTSSG meeting is like | 5 | 13 | 52 | 3 |
| Developing a better understanding of the goals of AFTSSG | 3 | 15 | 52 | 3 |
| Learning more about AFTSSG literature | 3 | 17 | 46 | 7 |
| Learning more about the 12 steps or other AFTSSG principles | 3 | 19 | 49 | 12 |
| Finding out more about AFTSSG meetings in my area | 5 | 12 | 50 | 6 |
| Becoming more motivated to make changes to my drinking | 2 | 17 | 50 | 4 |
| Having someone to go to an AFTSSG meeting with | 3 | 14 | 41 | 15 |
| Developing a relationship with my AFTSSG volunteer | 2 | 14 | 44 | 13 |
| Having my volunteer contact me after release | 0 | 12 | 34 | 27 |
| Having my volunteer try to attend meetings with me after release | 1 | 9 | 34 | 28 |
| Attending an AFTSSG meeting with my volunteer after release | 0 | 0 | 3 | 70 |
| Questions related to likelihood or future action | ||||
| How likely are you to go to meetings with your volunteer in the future? | 21 | 7 | 45 | -- |
| How likely are you to contact your volunteer again? | 19 | 10 | 44 | -- |
| How likely would you have been to contact BTG on your own? (NA = had never heard of BTG) | 21 | 4 | 19 | 29 |
| How likely is it that you would have attended an AFTSSG meeting if you hadn’t been in this study? | 35 | 13 | 24 | 1 |
| Do you think we should keep doing this kind of linkage in the future? | 2 | 3 | 68 | -- |
| Questions related to fit and comfort with the volunteer | ||||
| How good a fit was your volunteer for you? | 6 | 16 | 51 | -- |
| How comfortable were you with your volunteer? | 12 | 8 | 53 | -- |
| How did the following affect your comfort with and trust of your volunteer? | ||||
| Hearing the volunteer’s sobriety story or experiences in AFTSSG | 1 | 8 | 62 | 2 |
| Having the volunteer ask me about my goals for drinking | 4 | 10 | 57 | 2 |
| Having the volunteer ask me about myself in general | 4 | 11 | 56 | 2 |
| Feeling that the volunteer cared about me | 4 | 14 | 53 | 2 |
| Knowing that my volunteer was willing to help me get to my first AFTSSG meetings after release | 1 | 9 | 60 | 3 |
| Receiving advice from the volunteer | 1 | 10 | 59 | 3 |
| Being listened to by the volunteer | 1 | 10 | 60 | 2 |
| Feeling criticized by the volunteer | 8 | 12 | 3 | 50 |
| The volunteer telling me things I didn’t want to hear but needed to hear | 6 | 14 | 32 | 21 |
| Having things in common with the volunteer | 2 | 8 | 58 | 5 |
| My volunteer’s age | 4 | 41 | 21 | 7 |
| My volunteer’s race or ethnicity | 3 | 49 | 14 | 7 |
n = 73 CLEAR intervention participants who completed the 1-month post-release assessment
Observed rates of post-release contact with volunteers were low. Only 66% of the 78% of CLEAR participants who completed the one-month follow-up assessment reported being aware that a volunteer had tried to contact them (n=48, per the EIQ), typically rating it as helpful (Table 4). Only 38% of the 96% of participants providing any follow-up data reported making post-release contact with a volunteer (n=34, per the TLFB). Four participants reported meeting a volunteer at a twelve-step meeting (though 52% went to at least one AFTSSG meeting on their own). Total number of contacts (mostly phone) did not predict days of alcohol abstinence (IRR= 1.00, 95%CI 1.00; 1.00, z=0.69, p=0.49).
3.5. Sensitivity analyses
Analysis of abstinent days finds similar results under the assumption that those lost to follow-up were alcohol abstinent (OR=1.05, 95%CI 0.98; 1.12, p=0.20) or were daily drinkers (IRR=1.02, 95%CI 0.87; 1.19, p=0.82), suggesting that missing data did not influence results for this outcome.
4. Discussion
4.1. Findings in context
Because: (1) AFTSSG meetings and BTG volunteers are widely available and free, and (2) regular post-release AFTSSG attendance has been associated with better alcohol outcomes for women (Schonbrun et al., 2011), the CLEAR warm handoff intervention was a potentially disseminable and low-cost method to improve alcohol and related outcomes among women being released from pretrial jail detention. However, unlike our small pilot study (Johnson, Schonbrun, and Stein, 2013) and despite primarily positive reactions to volunteers and to the CLEAR intervention (Schonbrun et al., 2019, Table 3, Table 4), post-release connection between BTG volunteers and participants did not regularly occur in this larger trial. Given that the modal dose of CLEAR was a single in-jail individual meeting, it is unsurprising that CLEAR had little effect on post-release outcomes. Although post-release AFTSSG attendance (our hypothesized mechanism by which CLEAR would improve post-release alcohol outcomes) did predict alcohol abstinence, CLEAR did not increase post-release AFTSSG attendance relative to ESC (~50% of women in each condition attended at least one meeting).
Some interpret the twelve-step tradition of Attraction (“Our public relations policy is based on attraction rather than promotion;” Alcoholics Anonymous, 1984) as a prohibition on active outreach. However, our previous qualitative work showed that many re-entering women preferred not to make the first call post-release (even to someone they know), and interpreted being called by providers or BTG volunteers as proving they care (Johnson, Schonbrun, and Stein, 2013; Johnson, Williams, et al., 2015). Volunteers were initially hesitant about making the first post-release call, but agreed to try because of the high need in our target population. Ultimately, our research assistants were able to reach 96% of participants for at least one of the post-release assessments. In contrast, only 66% of participants who completed the 1-month follow-up assessment reported being aware that their volunteer had tried to reach them and only 38% of participants reported making contact with a volunteer post-release. The project coordinator observed that many more volunteers reported trying to reach women than women reported hearing from their volunteers. Given that phone numbers change and women may not receive messages left with others, participants may not have received volunteers’ messages, which the volunteers may have interpreted as lack of interest. Remuneration ($60) for follow-up assessments (but not baseline assessments or meetings with volunteers) might explain some of the difference between rates of research assistant versus volunteer contact with participants post-release. However, we have had good compliance with other (unpaid) post-release interventions (Johnson et al., 2020; Johnson, Peabody, et al., 2015; Johnson, Williams, et al., 2015; Johnson and Zlotnick, 2012) making this explanation less likely. We conclude that there is a mismatch between a level of outreach that was extremely active by twelve-step standards and the level of outreach required to follow up with women after jail release. As a result, a twelve-step volunteer-led warm handoff at jail release seems unlikely to happen routinely if CLEAR was standard practice.
About 70% of women in our study sample said that their post-jail goal was alcohol abstinence (Table 1). It is possible that a warm handoff to a volunteer from a twelve step background (which focuses on abstinence) did not fit the goals of the other 30% of participants. However, all participants understood the nature of the study and volunteered. Given that more women in CLEAR reported an abstinence goal (69%) than reported contact with their volunteers (38%), it seems unlikely that non-abstinence goals were the primary factor impeding contact between participants and volunteers after release. Effects of CLEAR on days abstinent did not differ for women with and without an abstinence goal.
Many women with AUD who become justice-involved experience co-occurring drug use and/or mental health problems. This sample was no exception (Table 1). Although women with co-occurring drug use and/or mental health problems often have additional intervention needs (Johnson et al., 2014), this study did not find evidence that effects of CLEAR relative to ESC on days abstinent from alcohol varied by drug use or mental health symptoms.
It was important to test the effectiveness of a twelve-step volunteer led warm handoff because twelve step groups are free and widely available, and many jails lack resources for paid substance use treatment. A non-volunteer, more professionalized intervention (e.g., peer support specialists, recovery coaches, or forensic peer specialists) whose role is active outreach may work better in providing a twelve-step focused warm handoff. However, these are typically paid positions receiving professional training and supervision, rather than twelve-step volunteers.
4.2. Strengths and limitations
This externally valid effectiveness trial tested a twelve-step volunteer-led intervention in the only way it could ever occur in research or in practice given the twelve-step tradition of Non-Affiliation (i.e., without external oversight, supervision, or fidelity monitoring of volunteers; Alcoholics Anonymous, 1984; Johnson et al., 2017). This approach is both a strength and a weakness. The strength is that the study addressed an important topic and acknowledged real-world jail resource constraints by testing a free intervention leveraging an already-existing, widely available volunteer network. The trial is also strengthened by a randomized design, credible control condition, use of standardized measures, transparent power and statistical analyses (Johnson et al., 2017), and a high assessment follow-up rate (96% of participants provided at least one follow-up assessment).
Limitations include less direct influence over interventionists than occurs in many randomized trials. To ensure harmony with the twelve-step traditions, the BTG twelve-step volunteer network, rather than the study team, chose, trained, and supervised BTG volunteers. Study research assistants were not blinded, though this is more of a concern for interpreting significant (rather than non-significant) findings. The study sample (59% non-Hispanic white), though representative of the participating jail, is less diverse than many jails.
4.3. Conclusion
A twelve-step volunteer led warm handoff for women leaving jail did not have a significant effect on post-release twelve-step attendance or drinking, likely because the post-release part of the handoff did not occur. The twelve-step tradition of Attraction may inhibit the active outreach required to connect women to services after jail release.
Acknowledgements.
We thank our project coordinator, Megan Kurth, and our study research assistants, Kristin Anslo and Briana Poole. We would also like to thank BTG and twelve-step volunteers everywhere for their tireless efforts on behalf of those who need them.
Role of Funding Source.
This study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA; R01 AA021732; Stein and Johnson, Principal Investigators). NIAAA had no role in the design or implementation of the study, analysis of the data, or writing of the manuscript.
Footnotes
Conflict of interest. No conflict declared.
Clinical Trials Registration: The trial was registered at clinicaltrials.gov (NCT01970293).
Contributor Information
Jennifer E. Johnson, Division of Public Health, Michigan State University College of Human Medicine, 200 East 1st St, Room 366, Flint, MI 48503, United States.
Yael Chatav Schonbrun, Butler Hospital, Warren Alpert Medical School of Brown University, 345 Blackstone Blvd, Providence, RI 02906, United States.
Bradley Anderson, Butler Hospital, 345 Blackstone Blvd, Providence, RI 02906, United States.
Christine Timko, Department of Veterans Affairs, Stanford University School of Medicine, 795 Willow Rd, Menlo Park, CA 94025, United States.
Michael D. Stein, Boston University School of Public Health, 715 Albany Street, Boston, MA 02118, United States
References
- Alcoholics Anonymous, 1984. This is A.A.: An introduction to the A.A. Recovery Program. Alcoholics Anonymous World Services Inc, New York. [Google Scholar]
- Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM, 2013. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment 20(4), 429–436. [DOI] [PubMed] [Google Scholar]
- Bui HN, Morash M, 2010. The impact of network relationships, prison experiences, and internal transformation on women’s success after prison release. J Offender Rehabil 49(1), 1–22. [Google Scholar]
- Burns D, Auerbach A, 1996. Therapeutic empathy in cognitive-behavioral therapy: Does it really make a difference? In Salkovskis PM (Ed.), Frontiers of cognitive therapy. Guilford Press, New York, pp. 135–164. [Google Scholar]
- Center for Substance Abuse Treatment, 2005. Substance Abuse Treatment for Adults in the Criminal Justice System. Treatment Improvement Protocol (TIP) Series 44. DHHS Publication No. (SMA) 05–4056. Rockville, MD: Substance Abuse and Mental Health Services Administration. [PubMed] [Google Scholar]
- Chandler RK, Fletcher BW, & Volkow ND, 2009. Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. JAMA 301(2), 183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke JG, Anderson BJ, Stein MD, 2011. Hazardously drinking women leaving jail: time to first drink. J Correct Health Care 17(1), 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, Hertzberg M, Mellman T, Beckham JC, Smith RD, Davison RM, Katz R, Feldman ME, 1997. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med 27, 153–160. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL, 2015. Structured Clinical Interview for DSM-5. American Psychiatric Association, Arlington, VA. [Google Scholar]
- Hasin D, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, Grant BF, 2013. DSM-5 criteria for substance use disorders: Recommendations and rationale. Am J Psychiatry 170(8), 834–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, Kaskutas LA, Weisner C, 1998. The Alcoholics Anonymous Affiliation Scale: development, reliability, and norms for diverse treated and untreated populations. Alcohol Clin Exp Res 22(5), 974–978. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Jones R, Miller T, Miller I, Stanley B, Brown G, Arias SA, Cerbo L, Rexroth J, Fitting H, Russell D, Kubiak S, Stein M, Matkovic C, Yen S, Gaudiano B, Weinstock LM (2020). Study protocol: A randomized controlled trial of suicide risk reduction in the year following jail release (the SPIRIT Trial). Cont Clin Trials 94, 106003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J, Schonbrun YC, Anderson B, Kurth M, Timko C, Stein M, 2017. Study protocol: Community Links to Establish Alcohol REcovery (CLEAR) for women leaving jail. Contemp Clin Trials 55, 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J, Schonbrun YC, Peabody ME, Shefner RT, Fernandes KM, Rosen RK, Zlotnick C, 2014. Provider experiences with prison care and aftercare for women with co-occurring mental health and substance use disorder: Treatment, resource, and systems integration challenges. J BehavHealth Serv Res 25 March, 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Peabody ME, Wechsberg WM, Rosen R,K, Fernandes K, Zlotnick C, 2015. Feasibility of an HIV/STI risk reduction program for incarcerated women who have experienced interpersonal violence. J Interpers Violence 30(18), 3244–3266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Schonbrun YC, Stein MD, 2013. Pilot test of twelve-step linkage for alcohol abusing women leaving jail. Substance Abuse DOI: 10.1080/08897077.2013.794760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Schonbrun YC, Nargiso JE, Kuo CC, Shefner RT, Williams CA, & Zlotnick C, 2013. “I know if I drink I won’t feel anything”: Substance use relapse among depressed women leaving prison. Int J Prison Health 9(4), 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Williams C, Zlotnick C, 2015. Development and feasibility of a cell phone-based transitional intervention for women prisoners with comorbid substance use and depression. Prison J 95(3), 330–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Zlotnick C, 2012. Pilot study of treatment for major depression among women prisoners with substance use disorder. J Psychiatric Res 46(9), 1174–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karberg J, James D, 2005. Substance dependence, abuse, and treatment of jail inmates, 2002. Report No. NCJ 209588. Bureau of Justice Statistics, U.S. Department of Justice, Washington, DC. [Google Scholar]
- Langan NP, Pelissier BMM, 2001. Gender differences among prisoners in drug treatment. J Subst Abuse 13(3), 291–301. [DOI] [PubMed] [Google Scholar]
- Lewis C, 2006. Treating incarcerated women: Gender matters. Psychiatr Clin North Am 29(3), 773–789. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V, 2002. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 7(1), 83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller W, Tonigan J, Longabaugh R, 1995. The Drinker Inventory of Consequences: an instrument for assessing adverse consequence of alcohol abuse. Project MATCH Monograph Series, Vol 4, DHHS Publication No. 95–3911 ed. National Institute on Alcohol and Alcoholism, Rockville, MD. [Google Scholar]
- Minton TD, 2011. Jail inmates at midyear 2010 - Statistical tables, in: Bureau of Justice Statistics (Ed.). U.S. Department of Justice, Washington, DC. [Google Scholar]
- Najavits L, Gastfriend D, Barber JP, Reif S, Muenz LR, Blaine J, et al. , 1998. Cocaine dependence with and without PTSD in the NIDA Cocaine Collaborative Study. Am J Psychiatry 155, 214–219. [DOI] [PubMed] [Google Scholar]
- O’Brien P, 2001. Making it a Free World: Women in Transition from Prison. State University of New York Press, New York. [Google Scholar]
- Rosenblum M, van der Laan MJ, 2009. Using regression models to analyze randomized trials: Asymptotically valid hypothesis tests despite incorrectly specified models. Biometrics 65(3), 937–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonbrun Y, Kurth M, Johnson JE, Timko C, Stein M, 2019. Participant evaluation of twelve step group linkage for jailed women with alcohol use disorders. Int J Offender Ther Comp Criminol, 63(4), 610–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonbrun Y, Strong DR, Anderson BJ, Caviness CM, Brown RA, Stein MD, 2011. Alcoholics Anonymous and hazardously drinking women returning to the community after incarceration: Predictors of attendance and outcome. Alcohol Clin Exp Res 35, 532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schonbrun YC, Strong DR, Anderson BJ, Caviness CM, Brown RA, Stein MD, 2011. Alcoholics Anonymous and Hazardously Drinking Women Returning to the Community After Incarceration: Predictors of Attendance and Outcome. Alcohol Clin Exp Res 35(3), 532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott C, Dennis ML, 2012. The first 90 days following release from jail: findings from the Recovery Management Checkups for Women Offenders (RMCWO) experiment. Drug Alcohol Depend 125(1–2), 110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell MB, Sobell LC, Klajner F, Pavan D, Basian E, 1986. The reliability of a timeline method for assessing normal drinker college students’ recent drinking history: utility for alcohol research. Addict Behav 11(2), 149–161. [DOI] [PubMed] [Google Scholar]
- Solomon A, Osborne JWL, LoBuglio SF, Mellow J, Mukamal DA, 2008. Life after lockup: Improving reentry from jail to the community. Urban Institute, Justice Policy Center, Washington, DC. [Google Scholar]
- Staton-Tindall M, Leukefeld C, Palmer J, Oser C, Kaplan A, Krietemeyer J, Saum C, Surratt HL, 2007. Relationships and HIV risk among incarcerated women. Prison J 87(1), 143–165. [Google Scholar]
- Stein M, Caviness CM, Anderson BA, Hebert M, Clarke JG, 2010. A brief alcohol intervention for hazardously-drinking incarcerated women. Addiction 105, 466–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong D, Caviness C, Anderson B, Brown RA, Stein M, 2010. Assessing the severity of hazardous drinking and related consequences among incarcerated women. Alcohol Clin Exp Res 34(5), 907–914. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, 1996. Prevalence of psychiatric disorders among incarcerated women. I. Pretrial jail detainees. Arch Gen Psychiatry 53(6), 505–512. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic A, 1989. Factor structure of hte Working Alliance Inventory. Psychol Assess 1, 207–210. [Google Scholar]
- Zeng Z, 2019. Jail inmates in 2017. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics. [Google Scholar]
- Zywiak W, Neighbors CJ, Martin RA, Johnson JE, Eaton CA, Rohsenow DJ, 2009. The Important People Drug and Alcohol interview: Psychometric properties, predictive validity, and implications for treatment. J Subst Abuse Treat 36, 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]


