Abstract
The gut microbiota plays a central role in regulating host metabolism. While substantial progress has been made in discerning how the microbiota influences host functions post birth and beyond, little is known about how key members of the maternal gut microbiota can influence feto-placental growth. Notably, in pregnant women, Bifidobacterium represents a key beneficial microbiota genus, with levels observed to increase across pregnancy. Here, using germ-free and specific-pathogen-free mice, we demonstrate that the bacterium Bifidobacterium breve UCC2003 modulates maternal body adaptations, placental structure and nutrient transporter capacity, with implications for fetal metabolism and growth. Maternal and placental metabolome were affected by maternal gut microbiota (i.e. acetate, formate and carnitine). Histological analysis of the placenta confirmed that Bifidobacterium modifies placental structure via changes in Igf2P0, Dlk1, Mapk1 and Mapk14 expression. Additionally, B. breve UCC2003, acting through Slc2a1 and Fatp1-4 transporters, was shown to restore fetal glycaemia and fetal growth in association with changes in the fetal hepatic transcriptome. Our work emphasizes the importance of the maternal gut microbiota on feto-placental development and sets a foundation for future research towards the use of probiotics during pregnancy.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00018-022-04379-y.
Keywords: Pregnancy, Metabolism, Microbiota, Fetus, Bifidobacterium
Introduction
All nutrients and metabolites required for feto-placental growth are provided by the mother, which in turn is thought to be influenced by the maternal gut microbiota through the breakdown of complex dietary components [1]. During gestation, liberated metabolites may be used by the placenta for morphogenesis, and transported across the placenta for use by the fetus for growth and development [2, 3]. This is highly important across gestation, particularly at later stages, when fetal growth is maximal. Notably, there are also alterations in the maternal microbiota throughout pregnancy with levels of the bacterial genus Bifidobacterium rising from trimester 1 onwards [4–6]. Failure of the mother to provide nutrients and metabolites to the fetus can result in pregnancy complications including small for gestational age, fetal loss and stillbirth. However, the contribution of the maternal gut microbiota in determining fetal outcomes is largely unexplored. Knowledge in this area would be highly valuable for developing treatments to improve fetal growth, with benefits for population health.
Studies performed with germ-free (GF) mice have identified that the microbiota is a key regulator for adequate development, early immune education and metabolism [7–11]. However, little is known about how maternal gut microbiota influences feto-placental growth and placental structure and function. Here, we hypothesized that the maternal gut microbiota, and specific microbiota members, regulate fetal growth by modulating placental development and nutrient supply. We tested this hypothesis by comparing conceptus growth across a range of microbiome complexity; using conventional specific-pathogen-free (SPF) mice as a model for standard microbial colonization, and as a baseline to define correct feto-placental growth [11]; GF mice which represent a completely clean and naïve microbiome system; and a mono-colonized maternal GF model—GF mice colonized with Bifidobacterium breve UCC2003 (group referred throughout the manuscript as BIF) [12]. Bifidobacterium, including B. breve UCC2003, is known to beneficially modulate the wider gut microbiota and host responses [13–15]. Certain species and strains are defined as probiotics “live microorganisms, which when ingested or locally applied in sufficient numbers confer one or more specified demonstrated health benefits for the host” (FAO/WHO; [16]). Therefore, B. breve may represent a suitable option for treating pregnancy complications by exerting metabolic effects on maternal physiology and associated feto-placental growth. Indeed, B. breve induced changes in placental morphogenesis and the abundance of placental glucose and lipid transporters, which were associated with improvements in the growth and metabolism of the fetus.
Materials and methods
Bifidobacterium breve UCC2003/pCheMC
B. breve UCC2003/pCheMC was generated by introducing the plasmid pCheMC to electrocompetent B. breve UCC2003 as described previously to allow antibiotic tagging of B. breve for subsequent culture studies [17]. In brief, B. breve UCC2003 was grown until mid-log phase, chilled on ice and washed twice with ice-cold sucrose citrate buffer (1 mM citrate, 0.5 M sucrose, pH5.8) and then electroporation of cells was carried out under the following conditions; 25MF, 200Ohms, 2 kV. Transformed cells were incubated for 2 h in reinforced clostridial medium (RCM) at 37 °C in a controlled anaerobic chamber then plated [18] on RCM agar plates with selective antibiotics. Colonies were sub-cultured 3 times on RCM agar plates with selective antibiotics. Antibiotics were used at the following final concentrations erythromycin 2 μg/mL.
Lyophilised B. breve
B. breve was grown in De Man, Rogosa and Sharpe agar (MRS) under anaerobic conditions overnight. The bacterial cell pellet was resuspended in 10% milk powder and lyophilised in 200 mL quantities. Lyophilised B. breve was reconstituted with 500 μL PBS. Concentration of B. breve was 1010 CFU/mL. All batches were tested for contamination upon the reconstitution of Luria–Bertani (LB) and brain–heart infusion (BHI) plates under anaerobic and aerobic conditions at 37 °C. No contamination of B. breve was detected.
Mice
All mouse experiments were performed under the UK Regulation of Animals (Scientific Procedures) Act of 1986. The project license PDADA1B0C under which these studies were carried out was approved by the UK Home Office and the UEA Ethical Review Committee. All mice were housed in the Disease Modelling Unit at the University of East Anglia, UK. Animals were housed in a 12:12 h light/dark, temperature-controlled room and allowed food and water ad libitum (food/water intake was not recorded). Female germ-free C57BL/6J (GF) and specific pathogen free (SPF) mice aged 6–8 weeks were used for the study. GF mice were bred in germ-free isolators (2 females to 1 male) and on gestational day (GD) GD9.5, pregnant mice (confirmed by weight gain) were removed from the GF isolator and transferred to individually ventilated cages. The sterility of these cages was previously tested and found to be suitable for housing GF mice for 1 week. Sterile water was changed every 2 days. We assessed responses at 2 gestational phases—the majority of studies were carried out at GD16.5, whilst the RNASeq studies utilized fetal livers harvested at GD18.5. A total of 6 SPF mice were used for GD16.5 assessments (no SPF mice were studied on GD18.5). For the GF group, a total of 5 (GD16.5) and 3 (GD18.5) dams were used. For the BIF mice, a total of 6 (GD16.5) and 4 (GD18.5) dams were used.
B. breve colonisation levels
Mice were given 100 µL of reconstituted lyophilised B. breve UCC2003 by oral gavage (containing 1010 CFU/mL) at GD10, GD12 and GD14 or 100 μL vehicle control (PBS, 4% skimmed milk powder), with this dosing regimen reflecting a more realistic time frame for women who are more likely to take probiotics once their pregnancy is confirmed. At GD16.5 and GD18.5, mice were sacrificed by cervical dislocation and samples collected for molecular and histological analysis. The experimental design can be found in Fig. 1A.
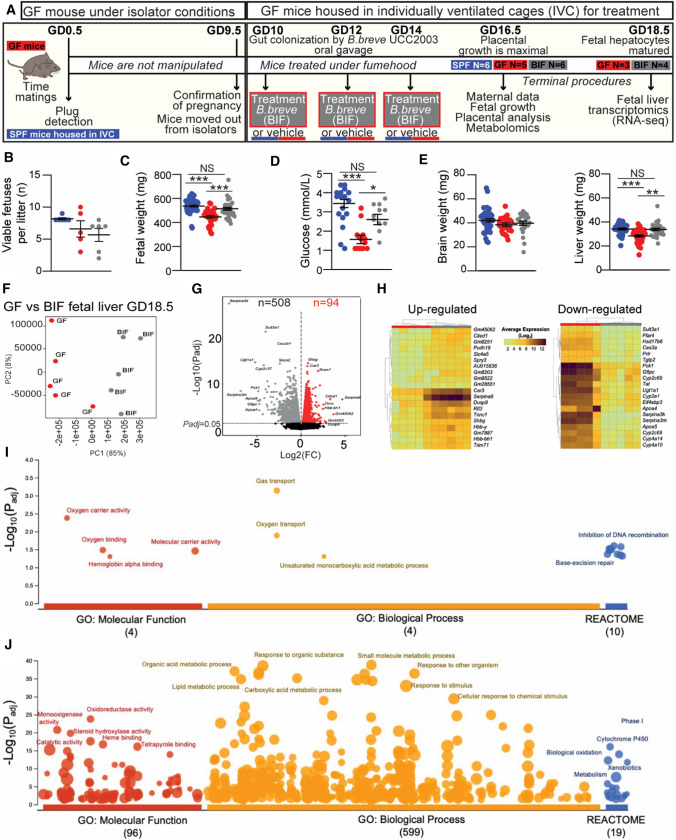
Fig. 1.
Effects of the maternal gut microbiome and B. breve supplementation during pregnancy on fetal viability, growth and hepatic transcriptome. A Experimental design. B Number of viable fetuses per litter (One-way ANOVA with Tukey’s multiple comparison). C Fetal weight. D Circulating glucose concentrations in fetal blood. E Fetal organ weights. F–G RNA-Seq analysis of fetal liver samples obtained at GD18.5. F PCA plot and G volcano plots showing up and down-regulated differentially expressed genes (DEGs) in BIF group (compared to GF group). H Heat map of the 20 most up and down-regulated DEGs (BIF group). I, J Functional profiling (g:Profiler) on 602 DEGs. Key enriched GO terms and REACTOME pathways are shown in the figure. Fetal data are obtained on GD16.5 from: SPF (49 fetuses/6 dams), GF (33 fetuses/5 dams), BIF (34 fetuses/6 dams). Dots represent raw data for each variable assessed (individual values). However, the statistical analysis and the mean ± SEM reported in the graphs were obtained with a general linear mixed model taking into account viable litter size as a covariate and taking each fetus as a repeated measure followed by Tukey multiple comparisons test (further explanations can be found in the Materials and Methods, statistical analysis section). Identification of outliers was performed with the ROUT Method. RNA-seq was performed on fetal livers obtained at GD18.5 from a total of 3 GF and 4 BIF pregnant dams/litters. RNA-Seq data analysis is described in the material and methods section (NS, not significant; *P < 0.05; **P < 0.01; ***P < 0.001)
Faecal samples were checked for contamination and B. breve colonization at GD12 and GD14 and GD16. Briefly, faecal samples from GF and BIF mice were diluted in 500 µL of PBS and agitated for 30 min at 4 °C on an Eppendorf MixMate 5353 Digital Mixer Plate Shaker. The faecal solution was passed through a 0.45 µm syringe filter. Faecal solution was diluted 1 in 100 and 20 µL was added to a De Man, Rogosa and Sharpe agar plate with erythromycin and incubated for 48 h in an anaerobic chamber at 37 °C. Colony-forming units were counted using a click counter. In SPF animals housed in the same animal facility we have previously shown that Bifidobacterium represents ~ 1% of the total gut microbiota [19].
Blood hormones and circulating metabolites
Maternal blood was obtained by cardiac exsanguination immediately after cervical dislocation. Blood was centrifuged and serum collected and stored at − 80 °C until further analysis. Blood glucose and serum concentrations of leptin, insulin, triglycerides, cholesterol, and free fatty acids were determined as previously reported [20]. Fetal blood glucose levels were measured with a handheld glucometer (One Touch Ultra; LifeScan) immediately after decapitation of the fetus (fetuses were selected at random).
Placental histology
Placentas were cut in half and fixed in 4% paraformaldehyde overnight at 4 °C. Samples were washed 3 times with PBS for 15 min each and storage in 70% ethanol until embedding in wax. Embedded placentas were cut at 5 μm thickness and stained with haematoxylin and eosin for gross morphology. Placental layer volume densities (labyrinth zone, junctional zone and decidua) were calculated using point counting and the Computer Assisted Stereological Toolbox (CAST v2.0) and converted to estimated volumes by multiplying by the weight of the placenta. For analysis of labyrinth components, sections were stained with lectin for the identification of fetal endothelial vessels and with cytokeratin for trophoblasts. Further details of the double-labelling immunohistochemistry can be found elsewhere [21]. Structural analysis of the labyrinth was performed as previously described [22–24]. Briefly, fetal capillaries, maternal blood spaces and trophoblast volume densities were calculated with a point counting system in 16 random fields and their densities were then multiplied by the estimated volume of the labyrinth zone to obtain the estimated component volume. To estimate the surface density of the maternal-facing and fetal-facing interhaemal membranes, we recorded the number of intersection points along cycloid arcs in a total 20 random fields of view. Both interhaemal membrane surfaces were converted to absolute surface areas and the total surface area for exchange calculated by averaging the two absolute surface areas. Fetal capillary length densities were obtained using counting frames with two contiguous forbidden lines [24] and then converted to absolute capillary length by multiplying the volume of the labyrinth zone. Fetal capillary diameter was estimated using the equation; d = 2(mean area/π)1/2. The interhaemal membrane barrier thickness was determined using orthogonal intercepts and measuring the shortest distance between fetal capillaries and the closest maternal blood spaces at random starting locations (at least 99) within the labyrinth zone [24].
For the analysis of placental glycogen, sections were stained with Periodic acid–Schiff (Sigma-Aldrich) previous incubation with 0.5% periodic acid (Thermo Fisher Scientific). Sections were counterstained with Fast-green (Sigma-Aldrich) and digitalized with the nanozoomer scanner (Hamamatsu). Analysis of placental glycogen accumulation was performed with Image J and conducted blinded to experimental groups. TUNEL staining for placental cell death was performed using the TUNEL Assay Kit—HRP-DAB (Abcam, ab206386) following manufacturer instructions except for the counterstaining which was substituted for Nuclear Fast Red (Vector). Sections were digitalized using a nanozoomer scanner (Hamamatsu) and the amount of apoptosis in the labyrinth zone was calculated in 5 random areas (× 20 magnification) and analysed by Image J software.
Western blotting
Protein extraction was performed with RIPA buffer as described previously [25]. Lysates were separated by SDS-PAGE and incubated with antibodies against p-MAPK (Thr202/Tyr204) (Cell Signalling, 4370; 1/1000), t-MAPK 44/42 (Cell Signalling, 4695; 1/1000), DLK-1 antibody (Abcam, ab21682; 1/1000), p-P38MAPK (Cell Signalling, 4511; 1/1000) and t-P38MAPK (Cell Signalling, 8690; 1/1000). Reactive bands were detected by chemiluminescence (Thermo Scientific, Scientific SuperSignal West Femto) and quantified by Image J software. Proteins were normalized to Ponceau S Staining [26].
RNA extraction and qPCR
Extraction of RNA from micro-dissected placental labyrinth zones was performed with RNeasy Plus Mini Kit (Qiagen) and reverse transcribed using the High Capacity cDNA RT Kit minus RT inhibitor (Applied Biosystems) according to manufacturer’s instructions. Samples were analysed using MESA Blue SYBR (Eurogentec) and primers (See Table S1) were synthesized by Sigma-Aldrich. The expression of each gene was normalized to the geometric mean expression of two reference genes Hprt and Ubc, which remained stably expressed across the groups. Analysis was performed using the 2-ΔΔCt method [27].
Sequence pre-processing, differential gene expression (DGE) analysis and functional enrichment analysis
Fetal liver RNA on GD18.5 was extracted using the RNeasy Plus Mini Kit (Qiagen). Purified RNA was quantified, and quality controlled using RNA 6000 Nano kit on a 2100 Bioanalyser (Agilent). Only samples with RIN values above 8 were sequenced. RNA sequencing was performed at the Wellcome Trust Sanger Institute (Hinxton, UK) on paired-end 75 bp inserts on an Illumina HiSeq 2000 platform. Isolated RNA was processed by poly-A selection and/or Ribo-depletion. RNA sequence pre-processing and DGE analysis was performed as previously described with slight modifications [28]. Briefly, FASTQ reads were initially quality-filtered using fastp v0.20.0 with options -q 10 (sequence reads with phred quality < 10 were discarded). Subsequently, sequence reads for each sample were merged (merge-paired-reads.sh) and followed by rRNA sequence filtering via SortMeRNA v2.1 based on SILVA rRNA database optimised for SortMeRNA software [29, 30]. Filtered reads were then unmerged (unmerge-paired-reads.sh) and ready for transcript quantification. Transcript mapping and quantification were then performed using Kallisto v0.44.0 [31]. Mus musculus (C57BL/6 mouse) cDNA sequences (GRCm38.release-98_k31) retrieved from Ensembl database were indexed with Kallisto utility index at default parameter and was used for the following transcript mapping and abundance quantification via Kallisto utility quant at 100 bootstrap replicates (-b 100) [32].
RNA raw counts were subjected (Kallisto outputs) to DGE analysis, which was performed using R library Sleuth (v0.30.0) [33]. Transcripts were then mapped to individual genes using Ensembl BioMart database (GRCm38.p6) with function sleuth_prep and option gene_mode = TRUE. Genes with an absolute log2 (fold change) > 1.0 and q value < 0.05 (p-adjusted value; based on Wald test statistics) were considered to be differentially regulated [34]. DGE statistics were plotted via functions within package Sleuth. Finally, functional enrichment analysis was performed using g:Profiler webtool g:GOst based on organism Mus Musculus species [35]. Briefly, a list of DGEs (Ensembl IDs) was uploaded to g:GOst, then selected ‘GO molecular function’, ‘GO biological process’ and ‘Reactome’ in the ‘data sources’. Significance threshold was set at 0.001 (g:SCS threshold).
Metabolite extraction, nuclear magnetic resonance (NMR) spectroscopy and metabolite quantification
Extraction of metabolites from the fetal liver, placenta and maternal caecum contents were performed as previously described as a standard protocol [36]. For caecal samples, frozen materials (stored at − 80 °C prior to analysis) were weighed ~ 50 mg before the addition of 600 μL of faecal water phosphate buffer solution. The faecal water phosphate buffer was prepared as follows: add 0.51 g NaH2PO4.H2O and 2.82 g K2HPO4 to 200 mL D2O (Deuterium Oxide; Merck). To this, 34.5 mg TSP (Trimethylsilyl propanoic acid; used as NMR standard) and 100 mg NaN3 (Merck) were added [37]. Next, the mixture was centrifuged for 10 min at 17,000×g before transferring the mixture to an NMR tube (Merck) for subsequent NMR analysis.
For liver and placenta samples (stored at − 80 °C prior to analysis), frozen fresh tissue (~ 20–45 mg) was placed into a 2 mL sterile microcentrifuge tube pre-loaded with ~ 15–20 glass beads (Merck) while 200 μL of ice-cold methanol (Fisher Scientific) and 42.5 μL of ultra-pure cold water were added to it and vortexed. Tissue was disrupted via a tissue lyser (Qiagen) for 2 × 2 min. 100 μL of ice-cold chloroform (Merck) was then added and vortexed. 100 μL of ice-cold chloroform and 100 μL of ultra-pure cold water were added to the mixture, and kept on ice for 15 min. Liquid was then transferred into a new sterile microcentrifuge tube and centrifuged for 3 min at 17,000×g. The top aqueous phase was transferred into a new microcentrifuge tube and speed-vacuumed for 30 min at 50 °C and 30 min without heating prior to reconstitution with faecal water phosphate buffer solution at 600 μL. The mixture was then moved to an NMR tube (Merck) for subsequent NMR analysis. Metabolites from culture media Brain Heart Infusion (BHI; Oxoid) and spent media (BHI cultured with B. breve UCC2003 for 48 h) were extracted as follows: 400 μL of the medium was transferred into a sterile microcentrifuge tube with the addition of 200 μL faecal phosphate buffer and mixed well. The mixture was then moved to an NMR tube (Merck) for further NMR analysis.
Samples in NMR tubes were subsequently subjected to NMR spectroscopy. The 1H NMR spectra were recorded at 600 MHz on a Bruker AVANCE spectrometer (Bruker BioSpin GmbH, Germany) running Topspin 2.0 software. The metabolites were then quantified using the software Chenomx® NMR Suite 7.0™.
Statistical analysis
All statistical analysis and sample size are shown in each figure/table and in the corresponding figure/table legends. Only samples from viable fetuses were analysed. No statistical analysis was used to pre-determine sample size and samples were assigned code numbers and, were possible, analysis was performed in a blinded fashion. Statistical calculations were performed using the GraphPad Prism software (GraphPad v9, San Diego, CA), SAS/STAT 9.0 (Statistical System Institute Inc. Cary, NC, USA) and RStudio Version 1.4.1106 (RStudio Boston, MA) with R Version 4.0.3 (Vienna, Austria). Data reported as mean ± SEM. Morphometric parameters of mother, litter size and western blot data were analysed by one-way ANOVA followed by the Tukey post hoc test. Feto-placental weights, placental stereological measurements and placental Lz gene expression levels were analysed with a general linear mixed model, taking into account viable litter size as a covariate and taking each fetus as a repeated measure of the mother. In this statistical analysis, fetuses and placentas per litter are nested within litters[38]. Identification of outliers was performed with ROUT Method. For metabolomics, differences between individual metabolites between the three groups were tested with a Kruskal–Wallis test using the Kruskal test function with correction for multiple comparisons applied using the Benjamini & Hochberg false discovery rate method using the p.adjust function. Pairwise comparisons between the three groups were carried out with a Dunn's test on individual metabolites significantly different after correction for multiple comparisons using the dunnTest function in the FSA package. The level of significance for all statistical tests used in this study was set at P < 0.05. All figures in the manuscript show individual values (raw data). However, P values and mean ± SEM within the graphs analysed by the general linear mixed model were corrected for repeated measures. Graphs containing the individual dots and graphs with corrected mean ± SEM were generated with Graphpad and merged with Adobe Illustrator.
Results
Germ-free mice treated with B. breve have altered body composition and caecum metabolic profile
To assess whether maternal microbiota can influence feto-placental growth, GF mice were treated orally with B. breve UCC2003 from day 10 of gestation (treatment on days 10, 12 and 14; i.e. BIF group), and compared to GF and SPF dams (for an experimental overview see Fig. 1A). Timing and dosing were based on the fact that levels of Bifidobacterium rise throughout pregnancy [5] (colonization levels during pregnancy can be found in Figure S1). Previous work has indicated three consecutive doses of B. breve UCC2003 facilitates stable gut colonization, with the advantage of also avoiding repeated handling of the mice, which may induce spontaneous abortions [28, 39]. In addition, from a translational point of view, we also wanted to correlate our animal model with potential future supplementation studies in women at the point pregnancy is confirmed.
Maternal body composition differed between groups with GF and BIF mice showing increased digestive tract weight and lower pancreas mass compared to SPF mice. GF and BIF mice had similar circulating concentrations of glucose and insulin to SPF mice (Table 1). Compared to SPF mice, treatment with B. breve reduced maternal gonadal fat depot, liver, and spleen weights in BIF mice. No differences were observed in the circulating concentrations of leptin, cholesterol, triglycerides, or free fatty acids in maternal serum (Table 1).
Table 1.
Effects of maternal gut microbiome and B. breve administration during pregnancy on maternal body composition, circulating metabolites and hormones in maternal serum, and metabolites in caecum on day 16.5 of gestation
| SPF (n = 6) | GF (n = 5) | BIF (n = 6) | SPF vs GF | SPF vs BIF | GF vs BIF | |
|---|---|---|---|---|---|---|
| Hysterectomy weight (g) | 26.01 ± 0.91 | 27.87 ± 0.78 | 27.17 ± 0.80 | NS | NS | NS |
| Digestive tract (g) | 2.76 ± 0.03 | 6.83 ± 0.32 | 7.25 ± 0.63 | < 0.0001 | < 0.0001 | NS |
| Caecum (g) | 0.66 ± 0.03 | 3.47 ± 0.25 | 3.96 ± 0.41 | < 0.0001 | < 0.0001 | NS |
| Small intestine (g) | 1.66 ± 0.03 | 2.65 ± 0.11 | 2.59 ± 0.14 | < 0.0001 | < 0.0001 | NS |
| Pancreas (mg) | 315.40 ± 30.12 | 183.40 ± 24.74 | 190.60 ± 38.71 | 0.041 | 0.044 | NS |
| Gonadal fat (mg) | 433.10 ± 43.20 | 297.0 ± 37.02 | 272.0 ± 27.35 | NS | 0.016 | NS |
| Liver (g) | 2.09 ± 0.10 | 1.79 ± 0.05 | 1.55 ± 0.08 | NS | 0.001 | NS |
| Spleen (mg) | 117.90 ± 2.80 | 91.76 ± 10.60 | 83.03 ± 6.72 | NS | 0.012 | NS |
| Glucose (mmol/L) | 8.08 ± 0.78 | 8.38 ± 1.18 | 8.88 ± 0.74 | NS | NS | NS |
| Insulin (μg/L) | 0.12 ± 0.004 | 0.19 ± 0.05 | 0.20 ± 0.06 | NS | NS | NS |
| Leptin (pg/mL) | 2465 ± 177.1 | 2739 ± 486 | 2425 ± 303 | NS | NS | NS |
| Cholesterol (mmol/L) | 1.33 ± 0.03 | 1.56 ± 0.08 | 1.41 ± 0.09 | NS | NS | NS |
| Triglycerides (mmol/L) | 1.54 ± 0.08 | 1.79 ± 0.14 | 1.50 ± 0.11 | NS | NS | NS |
| Free Fatty Acids (μmol/L) | 890.6 ± 101.3 | 1440 ± 362 | 1092 ± 114.5 | NS | NS | NS |
| SPF (n = 3) | GF (n = 4) | BIF (n = 5) | SPF vs GF | SPF vs BIF | GF vs BIF | |
|---|---|---|---|---|---|---|
| Maternal caecum metabolites | ||||||
| Butyrate (mmol/kg) | 12.47 ± 7.97 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Citrulline (mmol/kg) | 0.30 ± 0.06 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Fucose (mmol/kg) | 0.08 ± 0.01 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Isobutyrate (mmol/kg) | 0.41 ± 0.24 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Isovalerate (mmol/kg) | 0.09 ± 0.01 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Malonate (mmol/kg) | 0.09 ± 0.02 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Methylamine (mmol/kg) | 0.05 ± 0.02 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Propionate (mmol/kg) | 4.48 ± 1.99 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Trimethylamine (mmol/kg) | 0.06 ± 0.007 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Valerate (mmol/kg) | 0.57 ± 0.27 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| 2.methylbutyrate (mmol/kg) | 0.05 ± 0.01 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| 5.Aminopentanoate (mmol/kg) | 0.33 ± 0.14 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.006 | 0.008 | NS |
| Acetate (mmol/kg) | 35.49 ± 20.66 | 0.55 ± 0.06 | 3.22 ± 1.39 | 0.006 | 0.129 | 0.094 |
Body composition and metabolites/hormones in serum were analyzed by one-way ANOVA followed by Tukey multiple comparisons test. Metabolites in maternal caecum were analysed by Kruskal–Wallis test followed by multiple comparisons using the Benjamini & Hochberg false discovery rate method and Dunn's test. ROUT test was used for the identification of outlier values. The level of significance was set at P < 0.05. NS: not significant. Data presented as mean ± SEM. The number of dams used for each group is annotated on the table and only data from dams at day 16.5 of gestation were used
Metabolomics analysis in maternal caecum samples indicated that the concentration of 13 out of 81 metabolites were significantly altered (Table 1 and Table S2). Acetate was influenced by B. breve (Table 1), with BIF dams having intermediate concentrations compared to SPF and GF mice (the low levels of acetate detectable in GF mice, most likely originated from the diet and/or are host-derived). These findings suggest that acetate producing B. breve and the wider gut microbiota may exert selective effects on maternal metabolic (gonadal fat depot and liver) and immune organs (spleen).
Maternal gut microbiota and B. breve regulate fetal growth by controlling fetal glycaemia and hepatic transcriptome
The three experimental groups had similar numbers of viable fetuses per litter, although GF and BIF groups showed a higher variability compared to the SPF group (Fig. 1B). Compared to SPF and BIF mice, GF fetuses were growth restricted, hypoglycaemic and had reduced liver weight, but had preserved brain size (Fig. 1C–E). As the liver is a key organ for glucose storage and production and fetuses from BIF mice had heavier livers and improved glycaemia, we next determined if there were changes in the fetal hepatic transcriptome (livers were collected from a small cohort of mice on GD18.5, when fetal liver function is particularly active prior to term. Indeed, mouse fetal hepatocytes are mature from GD18.5, when they present a similar gene expression pattern to those in the postnatal liver [40]). A total of 602 genes were differentially expressed, with 94 significantly up-regulated and 508 down-regulated genes in BIF group, when compared to GF group (Fig. 1F–H). Functional enrichment analysis indicated that pathways involved in haemoglobin and oxygen transport-binding were significantly upregulated in the fetal livers of BIF mice (Fig. 1I and Table S3). In contrast, many metabolic pathways were downregulated in response to B. breve administration, including carboxylic acid and lipid metabolic processes, steroid hydroxylase activity, fatty acid metabolism and response to glucocorticoid (Fig. 1H; Table S3). Therefore, maternal B. breve appears to exert changes in fetal hepatic function with implications for fetal growth.
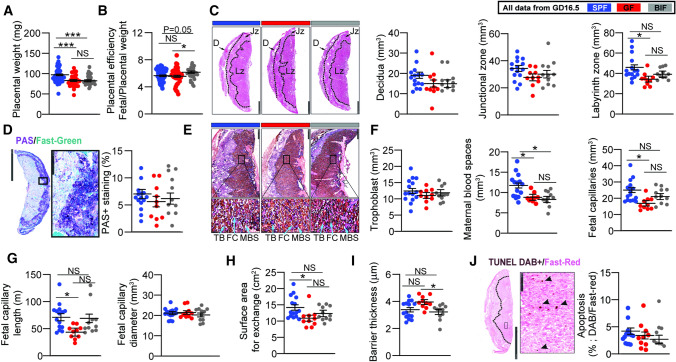
Maternal gut microbiota and B. breve control placental morphogenesis
To further understand the links between the maternal gut microbiota and the regulation of fetal growth, we assessed placental structure (performed on GD16.5, when placental growth in mice is maximal [24]). When compared to SPF mice, placentas were lighter in GF and BIF mice (Fig. 2A). Placental efficiency, defined as the grams of fetus produced per gram of placenta, was significantly improved in the BIF group compared to GF mice (Fig. 2B). Analysis of placental compartments showed that a lack of maternal gut microbiota significantly hampered the growth of the placental labyrinth transport zone (Lz), without compromising the endocrine junctional zone or decidua volumes (Fig. 2C). It also did not affect placental glycogen storage (Fig. 2D) or the volume of the trophoblast (Fig. 2E–F). Analysis of maternal blood spaces revealed that GF and BIF groups had reduced spaces compared to SPF mice, while the volume and the length of fetal capillaries were significantly reduced in the GF compared to SPF (Fig. 2F–G). Similarly, the surface area for exchange of the Lz was significantly decreased in GF compared to SPF mice (Fig. 2H). The barrier between maternal and fetal blood was also determined to be thinner in BIF vs GF mice (Fig. 2I). Lz apoptosis levels were similar between groups (Fig. 2J).
Fig. 2.
Effects of maternal gut microbiome and B. breve supplementation during pregnancy on placental structure on day 16.5 of gestation. A Placenta weight. B Placental efficiency determined by dividing fetal by placental mass. C Placental regional analysis. Scale bar = 1 mm. D Representative staining of placental glycogen with PAS and glycogen abundance. Scale bar = 2.5 mm and 250 μm. E Representative image of lectin and cytokeratin staining for labyrinth zone structural quantification. Scale bar = 500 μm and 50 μm. F–I Stereological parameters determined in placental labyrinth zone. J Representative image of TUNEL staining for apoptosis quantification in labyrinth zone. Scale bar = 2.5 mm and 100 μm. All data were analyzed by a general linear mixed model, taking into account litter size as a covariate and taking each fetus as a repeated measure followed by Tukey multiple comparisons test. ROUT test was used for the identification of outlier values. Dots represent raw data (individual values). However, the statistical analysis and the mean ± SEM reported within the graphs were obtained with the general linear mixed model (further explanations can be found in the Materials and Methods statistical analysis section). Placental weight-efficiency was obtained from: SPF (49 fetuses/6 dams), GF (33 fetuses/5 dams), BIF (34 fetuses/6 dams). Laboratorial analysis was performed with: SPF (14–15 placentas from 6 dams), GF (10 placentas from 5 dams) and BIF (9–11 placentas from 6 dams). Only placentas collected on day 16.5 of gestation were analysed. One to three placentas per litter were randomly selected and used for assessment. Placentas were analysed blind to the experimental groups. (NS, not significant; *P < 0.05; ***P < 0.001). D decidua, Jz junctional zone, Lz labyrinth zone, TB trophoblasts, FC fetal capillaries, MBS maternal blood spaces
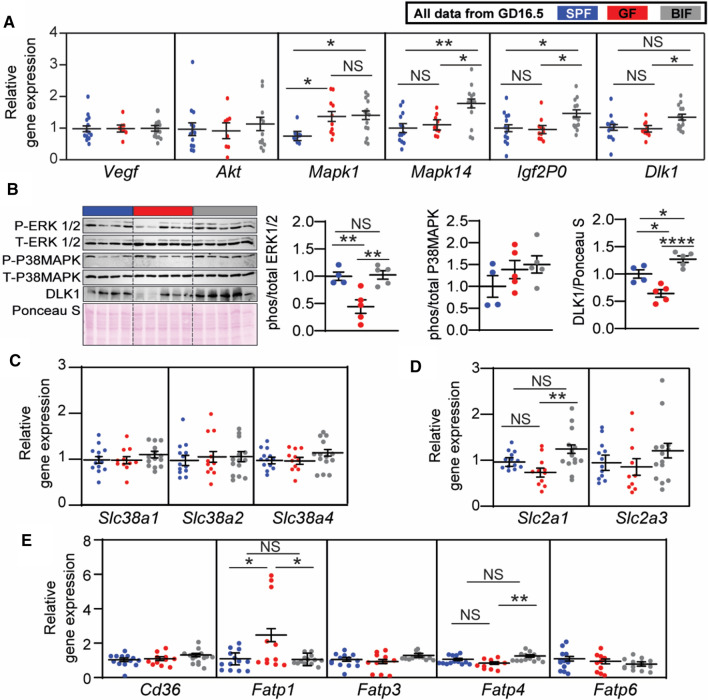
To define the molecular mechanisms behind the changes in the Lz, we quantified the expression of select genes in micro-dissected Lz. The angiogenic factor Vegf was similarly expressed between groups (Fig. 3A). However, the expression of signalling pathways involved in cell proliferation and growth, namely the MAPK pathway, was significantly altered by changes in maternal gut microbiota; Mapk1 was shown to be increased in both GF and BIF, while Mapk14 (also known as p38Mapk) was revealed to be specifically up-regulated in the Lz of BIF mice. In addition, Dlk1 and Igf2P0, which are key genes implicated in metabolism and Lz formation, were significantly up-regulated in the BIF group compared to GF mice. The expression of Akt did not vary between groups (Fig. 3A). As informed by western blotting, activation of ERK was reduced in the placental Lz of GF compared to SPF mice, and this effect was reversed by BIF (Fig. 3B). p38MAPK protein activity was similar between groups. DLK1 protein level was also lower in GF compared to SPF mice. However, BIF increased DLK1 protein levels when compared to both SPF and GF mice (Fig. 3B). Overall, these findings suggest that the maternal gut microbiota, and B. breve, regulate the development of the mouse placental Lz via the modulation of specific cell growth and metabolic genes/pathways.
Fig. 3.
Effects of maternal gut microbiome and B. breve supplementation during pregnancy on placental gene and protein levels on day 16.5 of gestation. A Gene expression levels in micro-dissected labyrinth zones. B Immunoblots and protein quantification by Western blot in micro-dissected labyrinth zones. C–E Gene expression levels in micro-dissected labyrinth zones for amino-acids, glucose and lipid transporters. Western blot data were analysed by one-way ANOVA. qPCR data were analyzed by a general linear mixed model, taking into account litter size as a covariate and taking each fetus as a repeated measure followed by Tukey multiple comparisons test. ROUT test was used for the identification of outlier values. Dots represent raw data (individual values). However, the statistical analysis and the mean ± SEM reported within the graphs (for qPCR data) were obtained with the general linear mixed model (further explanations can be found in the Materials and Methods, statistical analysis section). Gene expression analysis was performed with: SPF (13 placentas from 6 dams), GF (11 placentas from 5 dams) and BIF (14 placentas from 6 dams). Protein quantification was performed with: SPF (4 placentas from 4 dams), GF (5 placentas from 5 dams) and BIF (5 placentas from 5 dams). Only placentas collected on day 16.5 of gestation were analysed. For qPCR, one to three placentas per litter were assessed and selection of the samples was conducted at random. For protein expression analysis, 1 placenta per litter was selected (NS, not significant; *P < 0.05; **P < 0.01; ****P < 0.0001)
Maternal gut microbiota and B. breve controls key placental nutrient transporters
To better understand the changes in fetal growth and glycemia between groups, we quantified the expression of selected amino acid, glucose and lipid transporters in the Lz. We found no difference in the expression of system A amino acid transporters (Slc38a1, Slc38a2, Slc38a4) between groups (Fig. 3C). However, the key glucose transporter Slc2a1 was up-regulated in the Lz of BIF mice compared to GF mice (Slc2a3 mRNA levels were similar between groups; Fig. 3D). Fatty acid transporters were also altered, with increased levels of Fatp1 in the GF group compared to SPF and BIF, while Fatp4 was increased in the BIF group compared to the GF (Fig. 3E; Cd36 and Fatp3,6 expression levels were unaltered). Collectively, these data suggest that maternal gut microbiota, and B. breve, may regulate fetal growth by inducing changes in the expression of key nutrient transporters within the placenta.
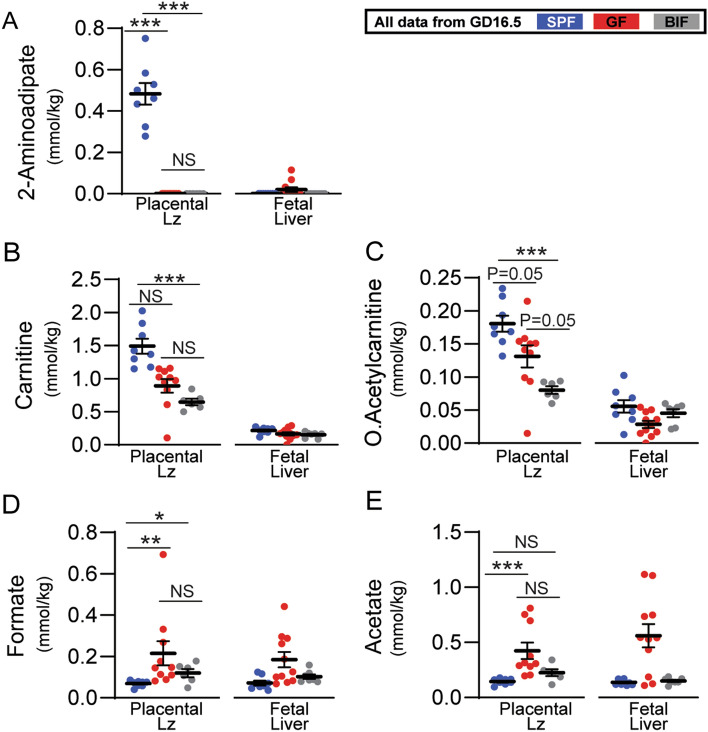
Differences in placental labyrinth growth are linked to an altered placental metabolome
To gain a further mechanistic understanding of the changes observed in the placental Lz and fetal liver, we analysed > 80 metabolites at GD16.5 (Fig. 4 and Table S2). We found 5 metabolites significantly altered in the placental Lz (Fig. 4). 2-Aminoadipate in the Lz was very low in GF/BIF groups as well as in fetal livers (Fig. 4A). Treatment with B. breve significantly reduced the concentrations of acetylcarnitine and carnitine in Lz tissue compared to SPF placentas, but not in fetal livers (Fig. 4B, C). Levels of formate in placental Lz were significantly elevated in both GF and BIF compared to SPF mice (Fig. 4D), with a similar trend (although not significant) in fetal liver samples. Acetate was also altered in the Lz (Fig. 4E), with concentrations significantly lower in the SPF compared to the GF group, whilst BIF samples showed intermediate levels (although these levels were much lower than observed in the maternal caecum). Similar to formate, concentrations of acetate in fetal liver followed similar directions to the Lz, yet were not statistically different between groups. These data suggest that maternal gut microbiota, and B. breve, regulate the fetal and placental growth via modulation of the placental Lz metabolome.
Fig. 4.
Metabolomic profiling of placental labyrinth zone and fetal liver on day 16.5 of gestation. Data were analysed by Kruskal–Wallis test followed by multiple comparisons using the Benjamini & Hochberg false discovery rate method and Dunn's test. ROUT test was used for the identification of outlier values. Data presented as mean ± SEM. Number of litters analysed per group: SPF (8 placentas-livers from 4 dams), GF (8–7 placentas-livers from 4–5 dams), BIF (6–7 placentas-livers from 5 dams). Only tissues collected at GD16.5 were analysed. Selection of the samples was conducted at random (NS, not significant; *P < 0.05; **P < 0.01; ***P < 0.001)
Discussion
In this study, we demonstrate that the maternal gut microbiota and the microbiota member B. breve regulate feto-placental growth. To the best of our knowledge, this is the first demonstration of a maternal gut bacterium remotely controlling placental structure and nutrient transporters, with important implications for fetal glycaemia and fetal growth. We observed that the effects of Bifidobacterium are partially mediated by altered metabolites in the maternal caecum and in placental Lz tissue, with alterations in the expression of key genes in the placental Lz and fetal liver.
Bifidobacterium is the dominant microbiota member in vaginally delivered, breast-fed infants, with certain species and strains known to stimulate and aid in maturation of the immune system [41]. B. breve UCC2003 also regulates responses at the gut barrier, inducing homeostatic epithelial cell programming, and protecting against inflammatory insults [28, 42]. Importantly, pregnancy is accompanied by increasing Bifidobacterium abundance in the gut of women and mice [5] and alterations in the abundance of Bifidobacterium are linked to the development of serious pregnancy complications like preeclampsia [43]. Recently, it has been demonstrated that the maternal gut microbiota regulate embryonic organ growth by promoting fetal neurodevelopment [44]. Our study shows that maternal gut microbiota induces changes in fetal organogenesis and that B. breve supplementation restored fetal glycaemia and liver weight. In this regard, fetal brain weight was unaltered in the three experimental groups, whilst liver mass was drastically reduced only in the GF group. Together, these results suggest that untreated GF fetuses prioritize the growth of the brain at expense of the liver. This fetal strategy, known as the ‘brain sparing effect’, is a protective mechanism to preserve oxygenation and nutrient delivery to the brain in situations of placental insufficiency [45–48]. Our RNAseq analysis shows an upregulation of genes involved in oxygen transport and haemoglobin binding, and downregulation of metabolic pathways such as steroid hydroxylase activity, carboxylic acid binding or fatty acid metabolism in the BIF group. These data, therefore, suggest that fetal defenses against growth retardation were better in the BIF group compared to the GF group and that the downregulation of the metabolic pathways could be due to the fact that BIF fetuses already achieved their hepatocyte maturation or their maximum liver growth potential earlier than the GF group. In fact, B. breve supplementation restored fetal glycaemia and weight, achieving similar values to that seen for SPF fetuses.
Previous in vivo studies show different strains of Bifidobacterium (including B. breve) modulate glucose handling [49], with this genus consistently associated with potential protection against human metabolic disorders e.g. type 2 diabetes [50, 51]. Our observations of reduced maternal gonadal fat mass and maternal liver weight in B. breve-treated dams compared to SPF dams, suggest that Bifidobacterium, or B. breve metabolites, could affect responses of key organs in the mother, and subsequently impact fetal resource allocation. B. breve UCC2003 appeared to induce changes in the metabolite milieu, including carnitine and acetate in the maternal caecum and/or placenta, which could be determinant of the effects observed on fetal growth. Carnitine is well known for mediating the transport of fatty acids into the mitochondrial matrix for fatty acid β-oxidation and BIF placentas had lower concentrations of acetylcarnitine and carnitine compared to SPF. These results suggest a potential greater reliance on these compounds for energy production or enhanced transfer of these fatty acids to the fetus [52]. On the other hand, acetate is a major bifidobacterial fermentation by-product, which directly mediates glucose homeostasis through the free fatty acid receptor 2 [53] and epithelial cell responses. Previous work in adult mice suggests that the elevation of gut acetate levels due to Bifidobacterium treatment plays a key role in regulating glucose handling systemically and reduces visceral fat accumulation [54]. Acetate also exerts systemic metabolic [55, 56] and immunological effects [57]. More generally, microbial-derived short-chain fatty acids (SCFAs) modulate multiple host physiological systems and during pregnancy are associated with maternal gestational weight, neonatal length and body weight, and protection against allergic airway disease in the developing fetus [58, 59]. Acetate crosses the placenta [59], so in our model, the elevated maternal B. breve-derived acetate may exert effects on feto-placental growth in three potential ways. First, higher maternal caecum acetate concentrations in SPF and B. breve supplemented dams vs GF dams could indicate maternal effects, through interactions within the maternal gut mucosa and subsequent impact on maternal organs (liver, adipose and spleen). Second, effects on the placenta, through the potential use of acetate for cellular metabolism, growth and function. Finally, effects on fetal metabolism following transport of acetate across the placenta to the fetus. Compared to the maternal caecum, levels of acetate were relatively low in the placental Lz and fetal liver (for all 3 groups). This suggests that B. breve (and SPF microbiota-derived acetate) may be used to support anabolic processes in utero (hence the very low levels detected). Moreover, the observed modulation of immune-associated pathways in the fetal liver, including those associated with G protein-coupled receptor signalling (e.g. Dusp9), also indicates a role in direct acetate-associated responses [60]. Further work is required to fully understand the mechanisms behind the differences observed in maternal organs between the SPF and BIF groups (liver, adipose and spleen) and how these changes impact materno-fetal resource allocation. Thus, future studies should assess the ontogeny of these changes and incorporate an additional pregnant SPF group treated with B. breve to fully understand the chemical, endocrine and metabolic interactions occurring between B. breve, maternal organs (gut, liver, adipose and spleen) and fetal metabolism.
Administration of B. breve significantly reduced the interhaemal membrane barrier thickness of the placenta (compared to GF group), which may facilitate the exchange of nutrients and gases. Previous work has shown that the barrier thickness is regulated by Igf2P0, as Igf2P0/knockout mice have increased thickness of the exchange barrier and reduced passive permeability of the placentas [61]. In our case, Igf2P0 was significantly elevated in the BIF group compared to the SPF and GF groups and although in vivo functional assays evaluating the passive and active transport of solutes are required to verify the implications of this effect on fetal nutrient allocation (e.g. performing unidirectional maternal–fetal transfer assays using 51Cr-EDTA or glucose and amino acid analogues, 3H-MeG or 14C-MeAIB [23, 61, 62]), this result explains, in part, the improvement in fetal weight observed in the BIF group. Moreover, IGFs have been implicated in the regulation of glucose transporters in a variety of organs by utilizing signalling pathways such as PI3K/AKT and MAPK [63], and among the different nutrient transporters evaluated, Slc2a1 mRNA levels were significantly elevated in the BIF group compared to GF group. The other two transporters that were altered, Fatp1 and Fatp4, changed in opposite directions suggesting that B. breve could modulate the expression of these two transporters in different ways depending on the direction and magnitude of fatty acid flux at the placental Lz [64, 65]. The divergent expression of Fatp1 and Fatp4 in the BIF compared to the GF group may also be linked to intracellular carnitine utilization, as Fatp1 can interact with carnitine palmitoyltransferase 1 to promote fatty acid transport into mitochondria [66].
Maternal gut microbiota affected placental structure and its vascular bed, which is required for adequate fetal growth [23]. The mechanisms governing these structural changes could be partially mediated by changes in the expression Igf2P0 and Dlk1 (two important imprinted genes in placental physiology [67]), and via MAPK upregulation. In addition to the changes above described for barrier thickness, deletion of Igf2P0 results in feto-placental growth restriction in association with reduced placental surface area for exchange and fetal capillary volume (reviewed by [68]); parameters that were significantly affected in the SPF vs GF groups, and partially restored by B breve administration. Dlk1, a non-canonical ligand of the Notch signalling pathway localized to the endothelial cells of fetal capillaries in the placental Lz, regulates placental vascularisation and branching morphogenesis [69] and both, IGF2 and DLK1, can mediate cellular actions via the MAPK pathway [70–72]. We observed no differences in the mRNA levels of Dlk1 between SPF and GF mice. However, at the protein level, DLK1 in the Lz was controlled by the maternal gut microbiota and more specifically by B. breve. Similarly, Mapk1 levels were increased in both GF and BIF groups compared to the SPF, but at the protein level, ERK activity was lower in the GF but not BIF group when compared to the SPF group, suggesting once again that B. breve is involved in the regulation of DLK-MAPK signaling. Another important signaling pathway for embryogenesis and placental Lz angiogenesis and vascular remodeling is p38MAPK (encoded by the gene Mapk14) [73]. This pathway has been linked to environmental stresses and inflammatory cytokines [74]. However, p38MAPK also regulates many normal cellular processes, including proliferation and cytoskeletal organisation. We observed that exposure to B. breve increases the mRNA abundance of Mapk14 and carnitine, a metabolite that was found to be altered in the Lz of the BIF group compared to the SPF group, can also promote p38MAPK signalling activation in cardiac tissue [75]. Taken together, our findings reveal that (1) maternal gut microbiota promotes fetal and placental growth in mice and (2) B. breve UCC2003 treatment may link to the altered metabolites/nutrient milieu in the mother, affecting placental nutrient transporter abundance and placental barrier thickness for exchange, with effects on fetal growth and development (when compared to GF).
Limitations of the study
While our study has clear strengths and strong translational implications for pregnancy complication treatments, it has limitations that are important to consider as they impact the conclusions drawn. First, our study only addresses the effects of B. breve UCC2003 in a completely clean and naïve microbiome system (GF model). This is not representative of the human gut environment, and therefore future experiments could include the addition of a SPF group treated with B. breve UCC2003 and also a similar group treated with another probiotic species (e.g. Lactobacillus acidophilus), or a combination of species. This would help to define Bifidobacterium-specific effects (driven by key metabolites), including their efficacy, safety and potential use of probiotics during pregnancy. Moreover, it could be argued that the SPF group interferes in the interpretations of the B. breve effects. However, there is a lack of fundamental knowledge on what is considered “normal or abnormal” in the GF system, as very little research has been done in understanding the role of the maternal gut microbiota on placental development (SPF vs GF). Therefore, the addition of the SPF group is required to define a baseline for adequate feto-placental growth, and it would also be important to understand how reconstitution of GF mice with SPF microbiota also modulates these responses. As previously mentioned, future work should evaluate the response of pregnant SPF mice to B. breve UCC2003 supplementation (using microbial profiling [e.g. shotgun metagenomics] to follow microbiota changes), as well as the efficiency of B. breve UCC2003 using other types of mouse models such as antibiotic-treated mice. These animal models may also reduce issues with the immune naïve physiology of the GF system [8]. Unsurprisingly, we did not see a full ‘rescue’ of placental phenotype in the monocolonised GF B. breve (BIF) group, compared to the complex microbiota found in SPF dams. However, structural and functional adaptations of these placentas exposed to B. breve were adequate enough to ‘rescue’ fetal weight and fetal glycaemia. An array of gut-associated signaling and a diverse metabolite pool are expected to provide more complete placental development. Indeed, other or additional Bifidobacterium species and/or strains may be required for placental and fetal development, given strain-specific host physiology responses [42, 76]. Further studies should allow the relative contributions of other microbial- and Bifidobacterium-derived factors to be elucidated. Moreover, ideally, future work should analyze fetal and placental growth each day of the supplementation period and use larger cohorts of pregnant mice. It would also be valuable to assess the impact of B. breve supplementation from prior to, and/or during the whole pregnancy.
Exploring three different compartments (i.e. mother, placenta and fetus) with respect to metabolites and elucidating their role is a complex process, and makes interpretations and drawing definitive conclusions difficult. Further studies using e.g. 13C labeled Bifidobacterium or specific metabolites for tracking experiments may allow more nuanced interactions to be uncovered in future work. Nonetheless, this study has revealed novel roles for the gut microbiota and specifically Bifidobacterium and provides the bases for future therapeutic strategies for treating pregnancy complications. These data suggest an opportunity for in utero programming through maternal Bifidobacterium and associated metabolites. Overall, although our study was performed in mice and is not representative of a clinical scenario, our study highlights the importance of the maternal gut microbiota during gestation and demonstrates that B. breve modulates maternal physiology, placental structure and nutrient transporter capacity with an impact on fetal glycaemia and fetal growth (Fig. 5). Our findings prompt an in-depth investigation into how additional members of the maternal gut microbiota impact on pregnancy outcomes. These future studies are important for the design of novel therapies to combat fetal growth restriction and other pregnancy complications.
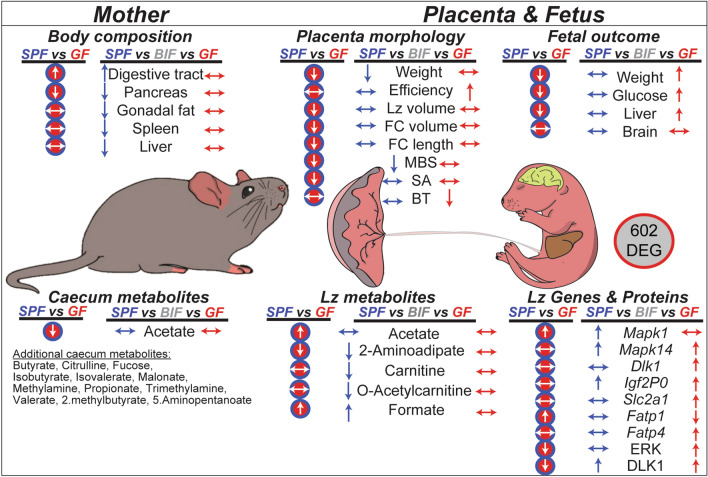
Fig. 5.
Summary illustration showing the most relevant results on how the maternal gut microbiota and B. breve affects mother, placenta and fetus during gestation. The effects of lacking maternal gut microbiota on maternal, placental and fetal phenotype are shown in red circles (SPF vs GF comparisons). Our results suggest that lacking maternal gut microbiota aside from inducing changes in the maternal digestive tract, pancreas and caecum metabolites, has important implications for the correct growth of the fetus and its placenta. The effects of B. breve administration compared to the SPF and GF groups are shown in blue and red arrows, respectively. Overall, B. breve induces changes in the maternal compartment that affect the structure, metabolome and function of the placenta in association with alterations in fetal metabolism, growth and hepatic transcriptome. SPF specific-pathogen-free mouse, GF germ-free mouse, BIF germ-free mouse treated with B. breve UCC2003, Lz labyrinth zone, MBS maternal blood spaces, FC fetal capillaries, SA surface area for exchange, BT barrier thickness, DEG differentially expressed genes
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Figure 1. Colonization levels of B. breve determined in maternal faecal samples on gestational day (GD), 12 and 14. Analysis performed by two-ways ANOVA (****P<0.0001). Data displayed as mean ± SEM. Number of dams for GF and BIF groups are 5 and 6, respectively. Assessment was performed only on dams sacrificed at GD16.5 (TIF 740 KB)
Supplementary Table 1. List of primers used for placental labyrinth zone qPCR (DOCX 15 KB)
Supplementary Table 2. List of metabolites analysed in maternal caecum, placental labyrinth zone and fetal liver on day 16.5 of gestation (XLSX 45 KB)
Supplementary Table 3. List of differentially expressed genes and pathways detected in the liver RNA-Seq on day 18.5 of gestation (XLSX 4301 KB)
Acknowledgements
Authors would like to thank Dr Ruben Bermejo-Poza (Complutense University of Madrid) for statistical advice and the Ferguson-Smith laboratory (University of Cambridge) for providing the DLK1 antibody.
Author contributions
JL-T, ZS, ANS-P, LJH designed research; JL-T, ZS, RK, GLG conducted research, JL-T, ZS, RK, MJD contributed analytic tools and performed analysis; DvS contributed reagents; JL-T, ZS, ANS-P, LJH wrote the paper with feedback from all the authors.
Funding
JL-T currently holds a Sir Henry Wellcome Postdoctoral Fellowship (220456/Z/20/Z) and previously a Newton International Fellowship from the Royal Society (NF170988 / RG90199). LJH is supported by Wellcome Trust Investigator Awards (100974/C/13/Z and 220876/Z/20/Z); the Biotechnology and Biological Sciences Research Council (BBSRC), Institute Strategic Programme Gut Microbes and Health (BB/R012490/1), and its constituent projects BBS/E/F/000PR10353 and BBS/E/F/000PR10356. ANS-P is supported by a Lister Institute of Preventative Medicine Research Prize (RG93692).
Data availability
The fetal liver RNA-Seq raw sequencing data are deposited at the National Center for Biotechnology Information (NCBI) under BioProject PRJNA748000. Relevant data are within the manuscript, individual figures and its Supporting Information files. Additionally, data are available from the corresponding authors on reasonable request. Scripts for differential gene expression analysis can be accessed at GitHub, https://github.com/raymondkiu/Maternal-foetal-microbiota-paper/.
Declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All mouse experiments were performed under the UK Regulation of Animals (Scientific Procedures) Act of 1986. The project license PDADA1B0C under which these studies were carried out was approved by the UK Home Office and the UEA Ethical Review Committee.
Consent for publication
For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jorge Lopez-Tello and Zoe Schofield contributed equally to this work.
Amanda N. Sferruzzi-Perri and Lindsay J. Hall contributed equally to this work.
Contributor Information
Jorge Lopez-Tello, Email: jl898@cam.ac.uk.
Amanda N. Sferruzzi-Perri, Email: ans48@cam.ac.uk
Lindsay J. Hall, Email: Lindsay.Hall@tum.de, Email: Lindsay.Hall@quadram.ac.uk
References
- 1.Krajmalnik-Brown R, Ilhan Z-E, Kang D-W, DiBaise JK. Effects of gut microbes on nutrient absorption and energy regulation. Nutr Clin Pract. 2012;27:201–214. doi: 10.1177/0884533611436116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonald B, McCoy KD. Maternal microbiota in pregnancy and early life. Science. 2019;365:984–985. doi: 10.1126/science.aay0618. [DOI] [PubMed] [Google Scholar]
- 3.de Agüero MG, Ganal-Vonarburg SC, Fuhrer T, et al. The maternal microbiota drives early postnatal innate immune development. Science. 2016;351:1296–1302. doi: 10.1126/science.aad2571. [DOI] [PubMed] [Google Scholar]
- 4.Koren O, Goodrich JK, Cullender TC, et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell. 2012;150:470–480. doi: 10.1016/j.cell.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nuriel-Ohayon M, Neuman H, Ziv O, et al. Progesterone increases bifidobacterium relative abundance during late pregnancy. Cell Rep. 2019;27:730–736.e3. doi: 10.1016/j.celrep.2019.03.075. [DOI] [PubMed] [Google Scholar]
- 6.Napso T, Yong H, Lopez-Tello J, Sferruzzi-Perri AN. The role of placental hormones in mediating maternal adaptations to support pregnancy and lactation. Front Physiol. 2018 doi: 10.3389/fphys.2018.01091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamousé-Smith ES, Tzeng A, Starnbach MN. The intestinal flora is required to support antibody responses to systemic immunization in infant and germ free mice. PLoS ONE. 2011;6:e27662. doi: 10.1371/journal.pone.0027662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kennedy EA, King KY, Baldridge MT. Mouse microbiota models: comparing germ-free mice and antibiotics treatment as tools for modifying gut bacteria. Front Physiol. 2018;9:1534. doi: 10.3389/fphys.2018.01534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lu J, Synowiec S, Lu L, et al. Microbiota influence the development of the brain and behaviors in C57BL/6J mice. PLoS ONE. 2018;13:e0201829. doi: 10.1371/journal.pone.0201829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martin AM, Yabut JM, Choo JM, et al. The gut microbiome regulates host glucose homeostasis via peripheral serotonin. PNAS. 2019;116:19802–19804. doi: 10.1073/pnas.1909311116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faas MM, Liu Y, Borghuis T, et al. Microbiota induced changes in the immune response in pregnant mice. Front Immunol. 2019;10:2976. doi: 10.3389/fimmu.2019.02976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pokusaeva K, Fitzgerald GF, van Sinderen D. Carbohydrate metabolism in bifidobacteria. Genes Nutr. 2011;6:285–306. doi: 10.1007/s12263-010-0206-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turroni F, Ventura M, Buttó LF, et al. Molecular dialogue between the human gut microbiota and the host: a Lactobacillus and Bifidobacterium perspective. Cell Mol Life Sci. 2014;71:183–203. doi: 10.1007/s00018-013-1318-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turroni F, Milani C, Duranti S, et al. Bifidobacteria and the infant gut: an example of co-evolution and natural selection. Cell Mol Life Sci. 2018;75:103–118. doi: 10.1007/s00018-017-2672-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.James K, O’Connell Motherway M, Penno C, et al. Bifidobacterium breve UCC2003 employs multiple transcriptional regulators to control metabolism of particular human milk oligosaccharides. Appl Environ Microbiol. 2018;84:e02774–e2817. doi: 10.1128/AEM.02774-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Food and Agriculture Organization of the United Nations, World Health Organization (2006) Probiotics in food: health and nutritional properties and guidelines for evaluation. Food and Agriculture Organization of the United Nations : World Health Organization, Rome
- 17.Mazé A, O’Connell-Motherway M, Fitzgerald GF, et al. Identification and characterization of a fructose phosphotransferase system in Bifidobacterium breve UCC2003. Appl Environ Microbiol. 2007;73:545. doi: 10.1128/AEM.01496-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cronin M, Akin AR, Collins SA, et al. High Resolution in vivo bioluminescent imaging for the study of bacterial tumour targeting. PLoS ONE. 2012;7:e30940. doi: 10.1371/journal.pone.0030940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes KR, Schofield Z, Dalby MJ, et al. The early life microbiota protects neonatal mice from pathological small intestinal epithelial cell shedding. FASEB J. 2020;34:7075–7088. doi: 10.1096/fj.202000042R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Musial B, Fernandez-Twinn DS, Vaughan OR, et al. Proximity to delivery alters insulin sensitivity and glucose metabolism in pregnant mice. Diabetes. 2016;65:851–860. doi: 10.2337/db15-1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Clercq K, Lopez-Tello J, Vriens J, Sferruzzi-Perri AN. Double-label immunohistochemistry to assess labyrinth structure of the mouse placenta with stereology. Placenta. 2020;94:44–47. doi: 10.1016/j.placenta.2020.03.014. [DOI] [PubMed] [Google Scholar]
- 22.Sferruzzi-Perri AN, López-Tello J, Fowden AL, Constancia M. Maternal and fetal genomes interplay through phosphoinositol 3-kinase(PI3K)-p110α signaling to modify placental resource allocation. Proc Natl Acad Sci. 2016;113:11255–11260. doi: 10.1073/pnas.1602012113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.López-Tello J, Pérez-García V, Khaira J, et al. Fetal and trophoblast PI3K p110α have distinct roles in regulating resource supply to the growing fetus in mice. Elife. 2019 doi: 10.7554/eLife.45282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coan PM, Ferguson-Smith AC, Burton GJ. Developmental dynamics of the definitive mouse placenta assessed by stereology. Biol Reprod. 2004;70:1806–1813. doi: 10.1095/biolreprod.103.024166. [DOI] [PubMed] [Google Scholar]
- 25.Salazar-Petres E, Carvalho DP, Lopez-Tello J, Sferruzzi-Perri AN (2021) Placental mitochondrial function, nutrient transporters, metabolic signalling and steroid metabolism relate to fetal size and sex in mice
- 26.Romero-Calvo I, Ocón B, Martínez-Moya P, et al. Reversible Ponceau staining as a loading control alternative to actin in Western blots. Anal Biochem. 2010;401:318–320. doi: 10.1016/j.ab.2010.02.036. [DOI] [PubMed] [Google Scholar]
- 27.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(− Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 28.Kiu R, Treveil A, Harnisch LC, et al. Bifidobacterium breve UCC2003 induces a distinct global transcriptomic program in neonatal murine intestinal epithelial cells. Science. 2020;23:101336. doi: 10.1016/j.isci.2020.101336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen S, Zhou Y, Chen Y, Gu J. fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics. 2018;34:i884–i890. doi: 10.1093/bioinformatics/bty560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kopylova E, Noé L, Touzet H. SortMeRNA: fast and accurate filtering of ribosomal RNAs in metatranscriptomic data. Bioinformatics. 2012;28:3211–3217. doi: 10.1093/bioinformatics/bts611. [DOI] [PubMed] [Google Scholar]
- 31.Bray NL, Pimentel H, Melsted P, Pachter L. Near-optimal probabilistic RNA-seq quantification. Nat Biotechnol. 2016;34:525–527. doi: 10.1038/nbt.3519. [DOI] [PubMed] [Google Scholar]
- 32.Zerbino DR, Achuthan P, Akanni W, et al. Ensembl 2018. Nucleic Acids Res. 2018;46:D754–D761. doi: 10.1093/nar/gkx1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pimentel H, Bray NL, Puente S, et al. Differential analysis of RNA-seq incorporating quantification uncertainty. Nat Methods. 2017;14:687–690. doi: 10.1038/nmeth.4324. [DOI] [PubMed] [Google Scholar]
- 34.Kinsella RJ, Kähäri A, Haider S, et al. Ensembl BioMarts: a hub for data retrieval across taxonomic space. Database (Oxford) 2011;2011:bar030. doi: 10.1093/database/bar030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raudvere U, Kolberg L, Kuzmin I, et al. g:Profiler: a web server for functional enrichment analysis and conversions of gene lists (2019 update) Nucleic Acids Res. 2019;47:W191–W198. doi: 10.1093/nar/gkz369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Le Gall G. Sample collection and preparation of biofluids and extracts for NMR spectroscopy. Methods Mol Biol. 2015;1277:15–28. doi: 10.1007/978-1-4939-2377-9_2. [DOI] [PubMed] [Google Scholar]
- 37.Wu J, An Y, Yao J, et al. An optimised sample preparation method for NMR-based faecal metabonomic analysis. Analyst. 2010;135:1023–1030. doi: 10.1039/b927543f. [DOI] [PubMed] [Google Scholar]
- 38.Lazic SE, Essioux L. Improving basic and translational science by accounting for litter-to-litter variation in animal models. BMC Neurosci. 2013;14:37. doi: 10.1186/1471-2202-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fanning S, Hall LJ, Cronin M, et al. Bifidobacterial surface-exopolysaccharide facilitates commensal-host interaction through immune modulation and pathogen protection. PNAS. 2012;109:2108–2113. doi: 10.1073/pnas.1115621109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Single-cell RNA-Seq analysis reveals dynamic trajectories during mouse liver development—PubMed. https://pubmed.ncbi.nlm.nih.gov/29202695/. Accessed 27 Jan 2022 [DOI] [PMC free article] [PubMed]
- 41.Dalby MJ, Hall LJ (2020) Recent advances in understanding the neonatal microbiome. F1000Res 9:F1000 Faculty Rev-422. 10.12688/f1000research.22355.1
- 42.Hughes KR, Harnisch LC, Alcon-Giner C, et al. Bifidobacterium breve reduces apoptotic epithelial cell shedding in an exopolysaccharide and MyD88-dependent manner. Open Biol. 2017;7:160155. doi: 10.1098/rsob.160155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miao T, Yu Y, Sun J, et al. Decrease in abundance of bacteria of the genus Bifidobacterium in gut microbiota may be related to pre-eclampsia progression in women from East China. Food Nutr Res. 2021 doi: 10.29219/fnr.v65.5781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vuong HE, Pronovost GN, Williams DW, et al. The maternal microbiome modulates fetal neurodevelopment in mice. Nature. 2020;586:281–286. doi: 10.1038/s41586-020-2745-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Godfrey KM, Haugen G, Kiserud T, et al. Fetal liver blood flow distribution: role in human developmental strategy to prioritize fat deposition versus brain development. PLoS ONE. 2012;7:e41759. doi: 10.1371/journal.pone.0041759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.López-Tello J, Arias-Álvarez M, Jiménez-Martínez M-Á, et al. The effects of sildenafil citrate on feto-placental development and haemodynamics in a rabbit model of intrauterine growth restriction. Reprod Fertil Dev. 2017;29:1239–1248. doi: 10.1071/RD15330. [DOI] [PubMed] [Google Scholar]
- 47.López-Tello J, Arias-Alvarez M, Jimenez-Martinez MA, et al. Competition for materno-fetal resource partitioning in a rabbit model of undernourished pregnancy. PLoS ONE. 2017;12:e0169194. doi: 10.1371/journal.pone.0169194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Giussani DA. The fetal brain sparing response to hypoxia: physiological mechanisms. J Physiol (Lond) 2016;594:1215–1230. doi: 10.1113/JP271099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kikuchi K, Ben Othman M, Sakamoto K. Sterilized bifidobacteria suppressed fat accumulation and blood glucose level. Biochem Biophys Res Commun. 2018;501:1041–1047. doi: 10.1016/j.bbrc.2018.05.105. [DOI] [PubMed] [Google Scholar]
- 50.Wu H, Esteve E, Tremaroli V, et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug. Nat Med. 2017;23:850–858. doi: 10.1038/nm.4345. [DOI] [PubMed] [Google Scholar]
- 51.Solito A, Bozzi Cionci N, Calgaro M, et al. Supplementation with Bifidobacterium breve BR03 and B632 strains improved insulin sensitivity in children and adolescents with obesity in a cross-over, randomized double-blind placebo-controlled trial. Clin Nutr. 2021;40:4585–4594. doi: 10.1016/j.clnu.2021.06.002. [DOI] [PubMed] [Google Scholar]
- 52.Sferruzzi-Perri AN, Higgins JS, Vaughan OR, et al. Placental mitochondria adapt developmentally and in response to hypoxia to support fetal growth. Proc Natl Acad Sci USA. 2019;116:1621–1626. doi: 10.1073/pnas.1816056116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fuller M, Priyadarshini M, Gibbons SM, et al. The short-chain fatty acid receptor, FFA2, contributes to gestational glucose homeostasis. Am J Physiol Endocrinol Metab. 2015;309:E840–E851. doi: 10.1152/ajpendo.00171.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aoki R, Kamikado K, Suda W, et al. A proliferative probiotic Bifidobacterium strain in the gut ameliorates progression of metabolic disorders via microbiota modulation and acetate elevation. Sci Rep. 2017;7:43522. doi: 10.1038/srep43522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fukuda S, Toh H, Hase K, et al. Bifidobacteria can protect from enteropathogenic infection through production of acetate. Nature. 2011;469:543–547. doi: 10.1038/nature09646. [DOI] [PubMed] [Google Scholar]
- 56.González Hernández MA, Canfora EE, Jocken JWE, Blaak EE. The short-chain fatty acid acetate in body weight control and insulin sensitivity. Nutrients. 2019;11:1943. doi: 10.3390/nu11081943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hu M, Eviston D, Hsu P, et al. Decreased maternal serum acetate and impaired fetal thymic and regulatory T cell development in preeclampsia. Nat Commun. 2019;10:3031. doi: 10.1038/s41467-019-10703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Priyadarshini M, Thomas A, Reisetter AC, et al. Maternal short-chain fatty acids are associated with metabolic parameters in mothers and newborns. Transl Res. 2014;164:153–157. doi: 10.1016/j.trsl.2014.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thorburn AN, McKenzie CI, Shen S, et al. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nat Commun. 2015;6:7320. doi: 10.1038/ncomms8320. [DOI] [PubMed] [Google Scholar]
- 60.Kim CH. Control of lymphocyte functions by gut microbiota-derived short-chain fatty acids. Cell Mol Immunol. 2021;18:1161–1171. doi: 10.1038/s41423-020-00625-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Placental-specific insulin-like growth factor 2 (Igf2) regulates the diffusional exchange characteristics of the mouse placenta | PNAS. 10.1073/pnas.0402508101. Accessed 8 May 2022 [DOI] [PMC free article] [PubMed]
- 62.Constância M, Hemberger M, Hughes J, et al. Placental-specific IGF-II is a major modulator of placental and fetal growth. Nature. 2002;417:945–948. doi: 10.1038/nature00819. [DOI] [PubMed] [Google Scholar]
- 63.Baumann MU, Deborde S, Illsley NP. Placental glucose transfer and fetal growth. Endocrine. 2002;19:13–22. doi: 10.1385/ENDO:19:1:13. [DOI] [PubMed] [Google Scholar]
- 64.Dutta-Roy AK. Transport mechanisms for long-chain polyunsaturated fatty acids in the human placenta. Am J Clin Nutr. 2000;71:315S–S322. doi: 10.1093/ajcn/71.1.315s. [DOI] [PubMed] [Google Scholar]
- 65.Larqué E, Demmelmair H, Klingler M, et al. Expression pattern of fatty acid transport protein-1 (FATP-1), FATP-4 and heart-fatty acid binding protein (H-FABP) genes in human term placenta. Early Hum Dev. 2006;82:697–701. doi: 10.1016/j.earlhumdev.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 66.Sebastián D, Guitart M, García-Martínez C, et al. Novel role of FATP1 in mitochondrial fatty acid oxidation in skeletal muscle cells. J Lipid Res. 2009;50:1789–1799. doi: 10.1194/jlr.M800535-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Frost JM, Moore GE. The importance of imprinting in the human placenta. PLoS Genet. 2010;6:e1001015. doi: 10.1371/journal.pgen.1001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sferruzzi-Perri AN, Sandovici I, Constancia M, Fowden AL. Placental phenotype and the insulin-like growth factors: resource allocation to fetal growth. J Physiol. 2017;595:5057–5093. doi: 10.1113/JP273330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yevtodiyenko A, Schmidt JV. Dlk1 expression marks developing endothelium and sites of branching morphogenesis in the mouse embryo and placenta. Dev Dyn. 2006;235:1115–1123. doi: 10.1002/dvdy.20705. [DOI] [PubMed] [Google Scholar]
- 70.Huang C-C, Kuo H-M, Wu P-C, et al. Soluble delta-like 1 homolog (DLK1) stimulates angiogenesis through Notch1/Akt/eNOS signaling in endothelial cells. Angiogenesis. 2018;21:299–312. doi: 10.1007/s10456-018-9596-7. [DOI] [PubMed] [Google Scholar]
- 71.Forbes K, Westwood M, Baker PN, Aplin JD. Insulin-like growth factor I and II regulate the life cycle of trophoblast in the developing human placenta. Am J Physiol Cell Physiol. 2008;294:C1313–C1322. doi: 10.1152/ajpcell.00035.2008. [DOI] [PubMed] [Google Scholar]
- 72.Sandovici I, Georgopoulou A, Pérez-García V et al (2022) The imprinted Igf2-Igf2r axis is critical for matching placental microvasculature expansion to fetal growth. Dev Cell 57:63–79.e8. 10.1016/j.devcel.2021.12.005 [DOI] [PMC free article] [PubMed]
- 73.Mudgett JS, Ding J, Guh-Siesel L, et al. Essential role for p38α mitogen-activated protein kinase in placental angiogenesis. PNAS. 2000;97:10454–10459. doi: 10.1073/pnas.180316397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cuenda A, Rousseau S. p38 MAP-Kinases pathway regulation, function and role in human diseases. Biochimica Biophysica Acta Mol Cell Res. 2007;1773:1358–1375. doi: 10.1016/j.bbamcr.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 75.Fan Z, Han Y, Ye Y, et al. l-carnitine preserves cardiac function by activating p38 MAPK/Nrf2 signalling in hearts exposed to irradiation. Eur J Pharmacol. 2017;804:7–12. doi: 10.1016/j.ejphar.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 76.Ruiz L, Delgado S, Ruas-Madiedo P, et al. Bifidobacteria and their molecular communication with the immune system. Front Microbiol. 2017;8:2345. doi: 10.3389/fmicb.2017.02345. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Colonization levels of B. breve determined in maternal faecal samples on gestational day (GD), 12 and 14. Analysis performed by two-ways ANOVA (****P<0.0001). Data displayed as mean ± SEM. Number of dams for GF and BIF groups are 5 and 6, respectively. Assessment was performed only on dams sacrificed at GD16.5 (TIF 740 KB)
Supplementary Table 1. List of primers used for placental labyrinth zone qPCR (DOCX 15 KB)
Supplementary Table 2. List of metabolites analysed in maternal caecum, placental labyrinth zone and fetal liver on day 16.5 of gestation (XLSX 45 KB)
Supplementary Table 3. List of differentially expressed genes and pathways detected in the liver RNA-Seq on day 18.5 of gestation (XLSX 4301 KB)
Data Availability Statement
The fetal liver RNA-Seq raw sequencing data are deposited at the National Center for Biotechnology Information (NCBI) under BioProject PRJNA748000. Relevant data are within the manuscript, individual figures and its Supporting Information files. Additionally, data are available from the corresponding authors on reasonable request. Scripts for differential gene expression analysis can be accessed at GitHub, https://github.com/raymondkiu/Maternal-foetal-microbiota-paper/.