Abstract
Background
As primary total knee arthroplasty volume continues to increase, so will the number of revision total knee arthroplasty (rTKA) procedures. The purpose of this study is to provide an updated perspective on the incidence, indications, and financial burden of rTKA in the United States.
Material and methods
This was a retrospective epidemiologic analysis using the National Inpatient Sample. International Classification of Diseases ninth and tenth revision codes were used to identify patients who underwent rTKA and create cohorts based on rTKA indications from 2012 to 2019. National and regional trends for length of stay, cost, and discharge location were evaluated.
Results
A total of 505,160 rTKA procedures were identified. The annual number of rTKA procedures increased by 29.6% over the study period (56,490 to 73,205). The top 3 indications for rTKA were aseptic loosening (23.1%), periprosthetic joint infection (PJI) (20.4%), and instability (11.0%). Over the study period, the proportion of patients discharged to skilled nursing facility decreased from 31.7% to 24.1% (P < .001). Hospital length of stay decreased from 4.0 days in 2012 to 3.8 days in 2019 (P < .001). Hospital costs increased by $1300 from $25,730 to $27,077 (P < .001). The proportion of rTKA cases performed at urban academic centers increased (52.1% to 74.3%, P < .001) while that at urban nonacademic centers decreased (39.0% to 19.2%, P < .001).
Conclusion
The top 3 indications for rTKA were aseptic loosening, PJI, and instability, with PJI becoming the most common indication in 2019. These cases are increasingly being performed at urban academic centers and away from urban nonacademic centers.
Level of Evidence
3 (Retrospective cohort study).
Keywords: Revision total knee arthroplasty, Clinical epidemiology, National trends, Healthcare resource utilization
Introduction
Total knee arthroplasty (TKA) is a cost-effective means of improving functional ability and quality of life for patients suffering from end-stage osteoarthritis [1]. Case volume for primary TKA is expected to increase substantially in the coming years; by the year 2030, conservative projections estimate that the annual case volume could reach 1.3 million, while more aggressive forecasts predict nearly 3.5 million primary TKAs per year [[2], [3], [4]]. In accordance with the rise in number of primary TKAs, it is estimated that the annual volume of revision TKA (rTKA) will increase by as much as 600% from 2005 to 2030 [[3], [5], [6], [7]]. Revision total joint arthroplasty is an immensely expensive procedure and costs on average 76% more than primary joint replacement, in large part due to longer operative time and hospitalizations, more expensive implants, and higher perioperative costs [[8], [9], [10]]. Furthermore, compared with primary TKA, rTKA is associated with marginal improvements in patient-reported outcome measures, increased cost per unit of patient-reported outcome measure improvement, and higher rates of postoperative complications and mortality [8,11,12].
Past analyses have demonstrated that periprosthetic joint infection (PJI) and aseptic loosening continue to be the most common indications for rTKA and are the underlying cause for nearly half of all rTKAs performed in the United States [[13], [14], [15], [16]]. With the expansion of primary TKA to younger patients, an additional concern is a recent finding that the incidence of rTKA is rising especially quickly among young patients [13]. Given that this subset of patients is more likely to outlive their implants and require rTKA, it is imperative to identify common indications for rTKA with the hopes of further improving implant longevity [17,18].
The introduction of large, nationally representative databases has given physician scientists access to an unprecedented volume of clinical data. The National Inpatient Sample (NIS), created by the Agency for Healthcare Research and Quality (AHRQ), is one such database which includes patient data from an estimated 20% of all hospital discharges in the United States [19]. Efficient use of such large databases relies upon standardized data coding protocols, and the NIS specifically makes use of the International Classification of Diseases (ICD) to allow for streamlined data accession. On October 1, 2015, the coding standard for the ICD was updated, and the ICD, tenth edition, (ICD-10) was introduced. Since the transition from ICD, ninth editon, to ICD-10, there has been a lack of data describing updated trends in indications for rTKA [[20], [21], [22], [23]].
Given the high rate of complications following rTKA, and the increased cost compared with primary TKA, it is imperative that orthopedic surgeons have a comprehensive understanding of the indications for rTKA as it may help to direct further refinement of surgical techniques and prosthetic constructs to improve prosthesis longevity, patient outcomes, and to minimize need for revision surgery. The purpose of this study is to provide an updated perspective on the incidence, indications, financial burden, and healthcare utilization (length of stay [LOS] and nonhome discharge) of rTKA in the United States.
Material and methods
Our study cohort was identified using the NIS over an 8-year period (January 1, 2012, to December 31, 2019). The NIS is a nationally representative database developed from all hospitals participating in the Healthcare Cost and Utilization Project (HCUP) and validated through a federal-state-industry partnership sponsored by the AHRQ. It is based on inpatient data from over 40 states derived from billing and discharge information, covering approximately 96% of the US population using an estimated stratified sample of 20% of all discharges from US hospitals. A stratified formula based on discharge weights reported by participating HCUP institutions was designed to allow an estimation of nationally representative statistics. Available variables include demographic data, diagnoses, procedures, hospital LOS, hospital cost, and hospital characteristics [24]. Since the NIS database has been sufficiently deidentified of any personal health information or identifiers, this study was deemed exempt from approval by the institutional review board at our institution.
Patients older than 18 years who were admitted and underwent an rTKA procedure during the study period were considered for this study. Patients undergoing rTKA were identified using ICD, ninth editon, procedure codes for cases from January 1, 2012, to September 30, 2015, and ICD-10 procedure codes for cases from October 1, 2015, through December 31, 2019, (Table 1). In order to be identified as a revision operation, each patient entry must contain either the revision code or both the removal and replacement codes. Patients with tibia and femur revision procedure codes reported separately were classified as a revision of both components. These patients were then grouped based on the specific indication for rTKA (Table S1) [25]. The first related diagnostic code listed was used as the primary indication for rTKA. The proportion of patients with multiple related diagnoses was summarized. For ICD-10 diagnostic codes, no differentiation was made between modifiers for initial encounter, subsequent encounter, or sequelaesequelae. The number of rTKA procedures per year was tabulated and used to generate trends during the study period.
Table 1.
Procedural codes used to identify rTKA procedure types.
| Location | Operation | ICD-9 | ICD-10 |
|---|---|---|---|
| All components | Revision | 00.80 | 0SWC08Z, 0SWC0EZ, 0SWC0JZ, 0SWD08Z, 0SWD0EZ, 0SWD0JZ |
| Removal | 0SPC08Z, 0SPC0EZ, 0SPC0JZ, 0SPD08Z, 0SPD0EZ, 0SPD0JZ | ||
| Replacement | 0SRC069, 0SRC06A, 0SRC06Z, 0SRC0EZ, 0SRC0J9, 0SRC0JA, 0SRC0JZ, 0SRD069, 0SRD06A, 0SRD06Z, 0SRD0EZ, 0SRD0J9, 0SRD0JA, 0SRD0JZ | ||
| Tibia | Revision | 00.81 | 0SWV0JZ, 0SWW0JZ |
| Removal | 0SPV0JZ, 0SPW0JZ, 0SPC08Z, 0SPC0EZ, 0SPC0JZ, 0SPD08Z, 0SPD0EZ, 0SPD0JZ | ||
| Replacement | 0SRV0J9, 0SRV0JA, 0SRV0JZ, 0SRW0J9, 0SRW0JA, 0SRW0JZ | ||
| Femur | Revision | 00.82 | 0SWT0JZ, 0SWU0JZ |
| Removal | 0SPT0JZ, 0SPU0JZ, 0SPC08Z, 0SPC0EZ, 0SPC0JZ, 0SPD08Z, 0SPD0EZ, 0SPD0JZ | ||
| Replacement | 0SRT0J9, 0SRT0JA, 0SRT0JZ, 0SRU0J9, 0SRU0JA, 0SRU0JZ | ||
| Patella | Revision | 00.83 | 0SWC0JC, 0SWD0JD |
| Removal | 0SPC0JC, 0SPD0JD, 0SPC08Z, 0SPC0EZ, 0SPC0JZ, 0SPD08Z, 0SPD0EZ, 0SPD0JZ | ||
| Replacement | 0SUC09C, 0SUD09C | ||
| Liner | Revision | 00.84 | 0SWC09Z, 0SWD09Z |
| Removal | 0SPC09Z, 0SPD09Z, 0SPV0JZ, 0SPW0JZ, 0SPC08Z, 0SPC0EZ, 0SPC0JZ, 0SPD08Z, 0SPD0EZ, 0SPD0JZ | ||
| Replacement | 0SUC09Z, 0SUD09Z, 0SUV09Z, 0SUW09Z |
Patient demographics, hospital characteristics, hospitalization LOS, hospitalization cost, and discharge locations for rTKA patients were analyzed. Patient demographics included age (years), sex (male and female), race (white, black, Hispanic, Asian, Native American, and other), and insurance (Medicare, Medicaid, private, and self-pay). Discharge locations included home and skilled nursing facility (SNF). Hospital characteristics included hospital type (urban nonteaching, urban teaching, and rural), hospital size based on number of beds (large, medium, and small), and region (Northeast, Midwest, South, and West). Individual hospitalization cost was calculated using diagnosis-related group codes multiplied by hospital-specific cost-to-charge ratios provided by the AHRQ. HCUP indices of the diagnosis-related group were then used to account for differences in hospitalization severity [26]. The cost was subsequently standardized for inflation using rates from the United States Bureau of Labor Statistics and described in December 2019 US dollars.
All result sample sizes represented national annual estimates, accounting for individual discharge-level weights from the NIS's stratified two-stage cluster design using R’s survey package [27]. This package allows for summary statistics, two-sample tests, rank tests, and generalized linear models to be estimated incorporating the survey weights provided by HCUP to ensure that all results are nationally representative. As NIS samples 20% of all hospital discharges nationally, survey weights on average are approximately 5. Descriptive statistics were used to describe both baseline characteristics and outcome parameters within each comparison group. Continuous variables were reported using mean and standard error. Proportions were reported using mean and 95% confidence interval. Analysis was done using a two-tailed Student’s t-test after ensuring normal distributions. For skewed, nonparametric distributions, continuous variables are presented as median (interquartile range) and analyzed using the Wilcoxon rank-sum test. Chi-squared tests were used for categorical analysis. Trend analysis was performed using univariate regression evaluating a linear relationship for year. Statistical significance was defined as P < .05. Statistical analyses were performed using R 3.6.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 505,160 rTKA procedures were identified during the 8-year study period. From 2012 to 2019, the number of rTKA procedures per year increased by 29.6% (56,490 to 73,205; Table 2). All component revisions were the most common rTKA procedure (59.9%), followed by isolate liner exchanges (19.6%), tibial component only (11.1%), femoral component only (4.7%), and patellar component only (4.7%). The proportion of type of procedure varied over time, with 58.3% all component rTKAs in 2012 increasing to 62.7% in 2019 (P < .001), the proportion of isolated patellar component revision decreasing from 6.3% in 2012 to 1.5% in 2019 (P < .001), and the proportion of isolated liner exchanges increasing from 18.6% to 21.3% (Table 2).
Table 2.
Annual numbers of rTKA procedures by procedure type.
| Component | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| All | 32920 (58.3%) | 33935 (58.5%) | 35350 (58.5%) | 37650 (60.3%) | 37910 (61.1%) | 36910 (57.5%) | 42165 (61.7%) | 45870 (62.7%) | 302710 (59.9%) |
| Tibia | 6540 (11.6%) | 6070 (10.5%) | 6675 (11%) | 6350 (10.2%) | 7635 (12.3%) | 7805 (12.2%) | 7295 (10.7%) | 7705 (10.5%) | 56075 (11.1%) |
| Femur | 2960 (5.2%) | 3240 (5.6%) | 3135 (5.2%) | 2775 (4.4%) | 2790 (4.5%) | 3175 (4.9%) | 2675 (3.9%) | 2900 (4%) | 23650 (4.7%) |
| Liner | 10485 (18.6%) | 11325 (19.5%) | 11835 (19.6%) | 12250 (19.6%) | 10595 (17.1%) | 13145 (20.5%) | 13940 (20.4%) | 15620 (21.3%) | 99195 (19.6%) |
| Patella | 3585 (6.3%) | 3415 (5.9%) | 3455 (5.7%) | 3430 (5.5%) | 3120 (5%) | 3130 (4.9%) | 2285 (3.3%) | 1110 (1.5%) | 23530 (4.7%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Demographics
Of all rTKA patients, 20.9% were aged 75 years or older, while 14.3% of patients were younger than 55 years (Table S2). The proportion of patients younger than 55 years decreased from 17.8% in 2012 to 11.2% in 2019 (P < .001). The proportion of patients aged 65 to 74 years undergoing rTKA increased from 30.8% to 36.9% (P < .001). Insurance type varied over the study period with patients opting for Medicare increasing from 57.0% to 62.1% (P < .001) and those opting for private insurance decreasing from 32.1% to 27.5% (Table S3).
Indications
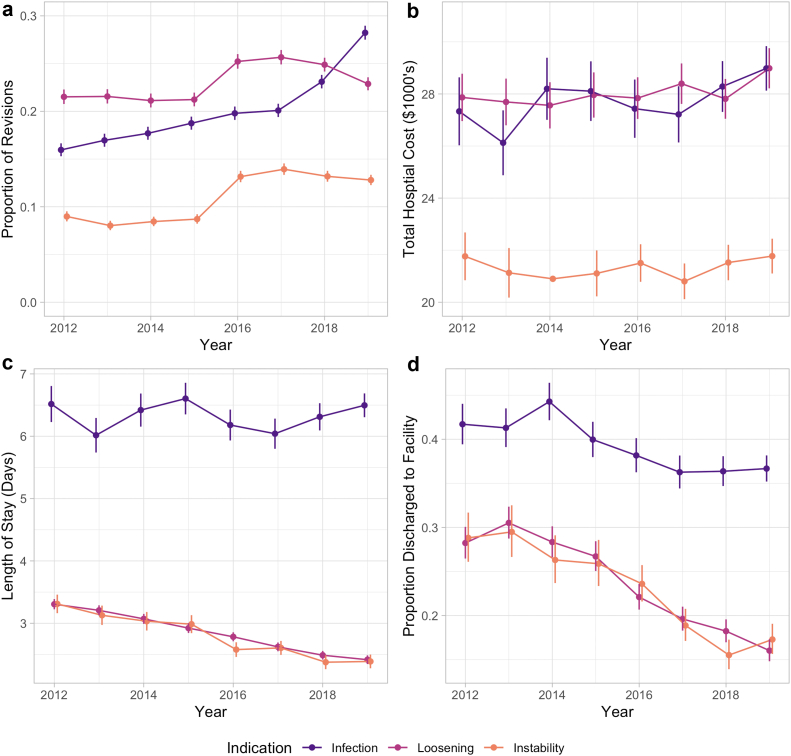
The top 3 associated primary indications for rTKA were aseptic loosening (23.1%), PJI (20.4%), and instability (11.0%) (Table 3, Fig. 1A). Over time, the proportion of rTKA procedures associated with aseptic loosening increased from 21.5% in 2012 to 25.7% in 2017, before decreasing to 22.9% in 2019 (increasing trend overall, P < .001). The proportion of procedures associated with PJI increased from 16.0% in 2012 to 28.2% in 2019 (P < .001), and the proportion associated with instability increased from 9% to 12.8% (P < .001) from 2012 to 2019. Importantly, the proportion of cases with a nonspecific diagnostic code classified as “other” decreased from 34.7% in 2012 to 19.0% in 2019 (P < .001). In 2019, PJI became the most common indication accounting for 28.2% of cases, surpassing aseptic loosening with 22.9% and instability with 12.8% (Fig. 1A). A total of 13.1% of cases were not associated with any associated diagnosis codes, while 13.3% of patients had multiple diagnosis codes listed.
Table 3.
Primary diagnosis for patients undergoing rTKA.
| Indication | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Loosening | 12,155 (21.5%) | 12,500 (21.6%) | 12,770 (21.1%) | 13,260 (21.2%) | 15,650 (25.2%) | 16,465 (25.7%) | 17,010 (24.9%) | 16,745 (22.9%) | 116,555 (23.1%) |
| PJI | 9015 (16%) | 9835 (17%) | 10,695 (17.7%) | 11,710 (18.7%) | 12,280 (19.8%) | 12,890 (20.1%) | 15,790 (23.1%) | 20,665 (28.2%) | 102,880 (20.4%) |
| Instability | 5075 (9%) | 4655 (8%) | 5110 (8.5%) | 5440 (8.7%) | 8165 (13.2%) | 8940 (13.9%) | 9015 (13.2%) | 9370 (12.8%) | 55,770 (11%) |
| Bearing surface wear | 1555 (2.8%) | 1390 (2.4%) | 1380 (2.3%) | 1425 (2.3%) | 1550 (2.5%) | 1580 (2.5%) | 1515 (2.2%) | 1310 (1.8%) | 11,705 (2.3%) |
| Periprosthetic fracture | 680 (1.2%) | 755 (1.3%) | 760 (1.3%) | 740 (1.2%) | 295 (0.5%) | 1490 (2.3%) | 1635 (2.4%) | 1835 (2.5%) | 8190 (1.6%) |
| Osteolysis | 550 (1%) | 500 (0.9%) | 350 (0.6%) | 480 (0.8%) | 415 (0.7%) | 375 (0.6%) | 365 (0.5%) | 350 (0.5%) | 3385 (0.7%) |
| Breakage | 585 (1%) | 675 (1.2%) | 590 (1%) | 545 (0.9%) | 930 (1.5%) | 865 (1.3%) | 865 (1.3%) | 870 (1.2%) | 5925 (1.2%) |
| Other | 19,575 (34.7%) | 19,770 (34.1%) | 20,590 (34.1%) | 19,775 (31.7%) | 13,845 (22.3%) | 13,285 (20.7%) | 13,925 (20.4%) | 13,930 (19%) | 134,695 (26.7%) |
| Missing | 7300 (12.9%) | 7905 (13.6%) | 8205 (13.6%) | 9080 (14.5%) | 8920 (14.4%) | 8275 (12.9%) | 8240 (12.1%) | 8130 (11.1%) | 66,055 (13.1%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Figure 1.
Trends in annual rTKA by primary associated indication for overall proportion (a), mean hospital costs (b), length of stay (c), and proportion of discharge to facility (d). Vertical bars represent 95% confidence intervals.
The breakdown of indications by revision procedure performed are summarized in Table S4. For patients with PJI, 44.1% underwent an all-component revision while another 41.6% underwent an isolated liner exchange. This differs from aseptic loosening where 70.8% of patients underwent an all-component revision, and only 3.1% underwent and isolated liner exchange.
Cost
While average hospital charges increased significantly from $87,394 to $113,158 over the study period (adjusted for inflation in December 2019 US dollars, P < .001, Table S5), hospital costs also increased by a substantially smaller margin from $25,730 in $2012 to $27,077 in 2019 (P < .001, Table 4). Periprosthetic fractures ($41,078) had the highest average cost followed by aseptic loosening ($28.051) and PJI ($27,874). The average hospital cost associated with PJI (P = .004), aseptic loosening (P = .04), and periprosthetic fracture (P = .001) increased slightly but significantly over the study period, while the mean hospital cost associated with instability did not change (P = .53).
Table 4.
Total hospital costs in USD, adjusted for inflation, by primary rTKA indication.
| Indication | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Loosening | 27,867 (345) | 27,693 (305) | 27,562 (289) | 27,960 (295) | 27,840 (259) | 28,395 (825) | 27,812 (247) | 28,986 (277) | 28,051 (149) |
| PJI | 27,333 (581) | 26,125 (398) | 28,199 (564) | 28,108 (451) | 27,435 (459) | 27,216 (399) | 28,286 (817) | 28,982 (412) | 27,874 (196) |
| Instability | 21,763 (459) | 21,130 (465) | 20,900 (509) | 21,108 (450) | 21,506 (360) | 20,804 (339) | 21,526 (357) | 21,773 (338) | 21,339 (140) |
| Bearing surface wear | 18,604 (663) | 17,148 (680) | 17,664 (693) | 17,480 (596) | 18,248 (704) | 16,717 (620) | 16,408 (633) | 16,386 (689) | 17,344 (234) |
| Periprosthetic fracture | 40,854 (2487) | 37,110 (1638) | 36,777 (1504) | 41,307 (2019) | 37,948 (2427) | 40,354 (1251) | 41,518 (1512) | 45,087 (1348) | 41,078 (605) |
| Osteolysis | 35,020 (2304) | 29,218 (1331) | 28,699 (2060) | 34,351 (1679) | 32,960 (1689) | 30,130 (1935) | 32,591 (1908) | 30,850 (1718) | 31,896 (666) |
| Breakage | 23,751 (1366) | 24,653 (1600) | 23,333 (1602) | 22,580 (1547) | 25,671 (1219) | 24,487 (1201) | 23,932 (1251) | 24,300 (1177) | 24,216 (478) |
| Other | 22,822 (230) | 23,085 (231) | 22,302 (207) | 22,683 (215) | 21,764 (245) | 22,429 (266) | 22,604 (264) | 23,235 (284) | 22,634 (85) |
| Missing | 30,343 (469) | 30,916 (507) | 29,455 (423) | 28,558 (412) | 28,807 (469) | 29,017 (545) | 28,087 (426) | 28,785 (514) | 29,206 (167) |
| Total | 25,730 (170) | 25,620 (153) | 25,434 (161) | 25,731 (152) | 25,523 (155) | 25,893 (253) | 26,117 (224) | 27,077 (169) | 25,927 (66) |
Standard error in parentheses.
Length of stay
Hospital LOS decreased over the study period for all rTKAs from 3.96 in 2012 to 3.49 in 2017 and then increased to 3.78 days in 2019 (P < .001 for overall decrease, Table 5). Periprosthetic fracture had the highest average LOS (6.39 days) followed by PJI (6.33 days). Over the study period, LOS decreased significantly for rTKA associated with instability (P < .001) and aseptic loosening (P < .001, Fig. 1C). Change in LOS was not significant for PJI (P = .75) and periprosthetic fracture (P = .05).
Table 5.
Mean length of stay by primary rTKA indication.
| Indication | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Loosening | 3.31 (0.04) | 3.21 (0.04) | 3.07 (0.04) | 2.92 (0.04) | 2.78 (0.03) | 2.62 (0.04) | 2.49 (0.04) | 2.42 (0.04) | 2.81 (0.01) |
| PJI | 6.52 (0.15) | 6.02 (0.11) | 6.42 (0.14) | 6.6 (0.15) | 6.18 (0.12) | 6.04 (0.1) | 6.31 (0.1) | 6.5 (0.12) | 6.33 (0.04) |
| Instability | 3.31 (0.08) | 3.13 (0.07) | 3.03 (0.07) | 2.99 (0.08) | 2.58 (0.06) | 2.6 (0.07) | 2.37 (0.05) | 2.39 (0.06) | 2.71 (0.02) |
| Bearing surface wear | 3.13 (0.1) | 2.75 (0.09) | 2.73 (0.1) | 2.41 (0.1) | 2.42 (0.08) | 2.23 (0.09) | 2.07 (0.08) | 2.03 (0.12) | 2.47 (0.03) |
| Periprosthetic fracture | 6.46 (0.45) | 5.79 (0.29) | 5.58 (0.31) | 6.94 (0.45) | 5.64 (0.5) | 6.24 (0.29) | 6.63 (0.32) | 6.77 (0.25) | 6.39 (0.12) |
| Osteolysis | 3.49 (0.18) | 3.37 (0.17) | 2.79 (0.12) | 3.32 (0.33) | 2.82 (0.15) | 2.97 (0.27) | 2.37 (0.15) | 2.0 (0.16) | 2.96 (0.08) |
| Breakage | 3.62 (0.22) | 3.46 (0.2) | 3.49 (0.25) | 3.48 (0.29) | 3.07 (0.17) | 2.75 (0.16) | 2.61 (0.16) | 2.66 (0.18) | 3.08 (0.07) |
| Other | 3.26 (0.04) | 3.13 (0.03) | 3 (0.03) | 2.82 (0.03) | 2.59 (0.03) | 2.51 (0.04) | 2.36 (0.04) | 2.27 (0.04) | 2.8 (0.01) |
| Missing | 4.19 (0.08) | 4.24 (0.1) | 4.05 (0.08) | 3.91 (0.08) | 3.92 (0.09) | 3.64 (0.08) | 3.47 (0.08) | 3.69 (0.12) | 3.88 (0.03) |
| Total | 3.96 (0.03) | 3.82 (0.03) | 3.79 (0.03) | 3.77 (0.04) | 3.56 (0.03) | 3.49 (0.03) | 3.54 (0.03) | 3.78 (0.04) | 3.71 (0.01) |
Standard error in parentheses.
Discharge destination
Overall, the proportion of patients discharged to SNF decreased from 31.7% to 24.1% (P < .001) over the study period (Table 6, Fig. 1D). Patients treated for periprosthetic fractures (67.8%) and PJI (38.1%) were more likely to be discharged to SNF. Over the study period, the proportion of patients discharged to SNF decreased significantly for those with aseptic loosening, instability, and PJI (P < .001 for all, Fig. 1D), while it increased significantly for periprosthetic fracture (P < .001).
Table 6.
Proportion of rTKA patients discharged to facility by primary indication.
| Indication | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Loosening | 28% (3405) | 30.3% (3790) | 28.2% (3595) | 26.5% (3515) | 22% (3445) | 19.6% (3220) | 18.2% (3095) | 16% (2675) | 22.9% (26,740) |
| PJI | 40.9% (3685) | 40.6% (3995) | 43.4% (4640) | 39.2% (4590) | 37.6% (4615) | 35.8% (4615) | 35.8% (5650) | 36% (7445) | 38.1% (39,235) |
| Instability | 28.7% (1455) | 29.4% (1370) | 26.1% (1335) | 25.6% (1395) | 23.5% (1915) | 18.8% (1680) | 15.5% (1395) | 17.3% (1620) | 21.8% (12,165) |
| Bearing surface wear | 28.6% (445) | 22.7% (315) | 18.8% (260) | 18.2% (260) | 21.6% (335) | 15.5% (245) | 15.2% (230) | 13.7% (180) | 19.4% (2270) |
| Periprosthetic fracture | 55.1% (375) | 67.5% (510) | 63.8% (485) | 67.6% (500) | 57.6% (170) | 66.1% (985) | 71.9% (1175) | 73.6% (1350) | 67.8% (5550) |
| Osteolysis | 36.4% (200) | 34% (170) | 27.1% (95) | 37.5% (180) | 22.9% (95) | 25.3% (95) | 11% (40) | 12.9% (45) | 27.2% (920) |
| Breakage | 29.9% (175) | 29.6% (200) | 32.2% (190) | 32.1% (175) | 25.8% (240) | 25.4% (220) | 21.4% (185) | 20.7% (180) | 26.4% (1565) |
| Other | 27.6% (5400) | 29.1% (5750) | 25.5% (5245) | 23.9% (4735) | 20.4% (2830) | 17.7% (2350) | 15.4% (2145) | 14.9% (2075) | 22.7% (30,530) |
| Missing | 38.1% (2780) | 38% (3000) | 36.3% (2975) | 36.7% (3330) | 33.6% (3000) | 25.7% (2130) | 25.8% (2130) | 25.6% (2085) | 32.4% (21,430) |
| Total | 31.7% (17,920) | 32.9% (19,100) | 31.1% (18,820) | 29.9% (18,680) | 26.8% (16,645) | 24.2% (15,540) | 23.5% (16,045) | 24.1% (17,655) | 27.8% (140,405) |
Regional analyses
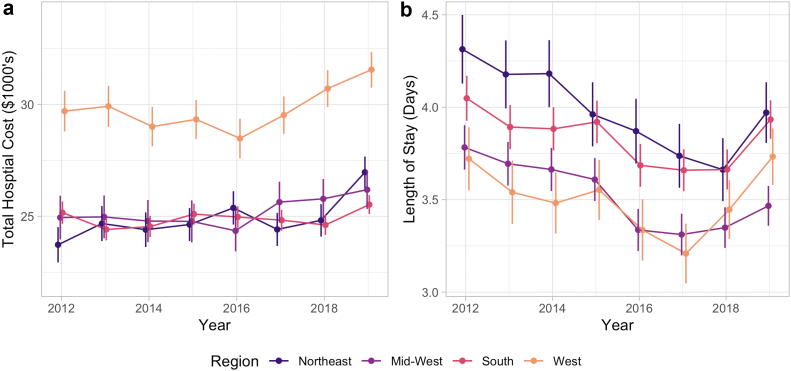
The distribution of rTKA cases by census region was roughly constant over the study period, with the highest proportion of cases in the Southern region (38.5%), followed by the Midwest (26.3%), the West (19.5%), and the Northeast (16.9%) (Table S6). rTKA Procedures performed in the West were associated with the lowest average LOS of 3.5 days but the highest average cost of $29,838 (Table S7, Table S8, Fig. 2). The mean total hospital costs increased significantly in the West (P < .001), Northeast (P < .001), and Midwest (P = .01), but costs did not change significantly in the South (P = .11). Meanwhile, the mean LOS decreased significantly in the Northeast, Midwest, and Southern regions (P < .001 for all) but did not change significantly in the Western region (P = .31).
Figure 2.
Total hospital costs (a) and length of stay (b) by US census region. Vertical bars represent 95% CI. US dollars adjusted for inflation, represented as December 2019 US dollars.
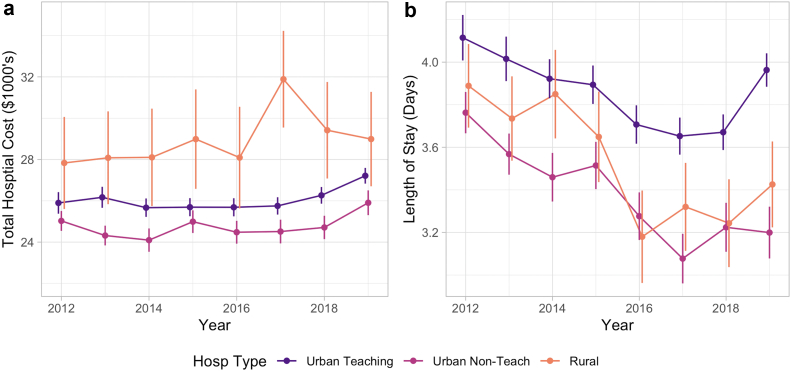
Hospital type analyses
The proportion of rTKA cases performed at urban academic centers significantly increased from 52.1% in 2012 to 74.3% in 2019 (P < .001), while the proportion performed at urban nonacademic centers (39.0% to 19.2%, P < .001) and rural centers (8.9% to 6.5%, P < .001) decreased over the study period (Table 7). Hospital costs increased for urban teaching hospitals (P < .001) and urban nonteaching hospitals (P = .04), but did not change for rural hospitals (P = .10) over the study period (Table S9, Fig. 3). Compared with urban teaching hospitals, costs were lower at urban nonteaching hospitals (P < .001) and higher in rural hospitals (P < .001). LOS decreased significantly in all hospital types (Table S10, P < .001 for all) and was significantly shorter in urban nonteaching (P < .001) and rural hospitals (P < .001) than in teaching hospitals. The indications for rTKA by hospital type are summarized in Table S11. Rural hospitals had the highest relative rate of rTKA for aseptic loosening (P < .001), while urban academic centers had the highest rate of rTKA for PJI (P < .001).
Table 7.
Number of rTKA cases by hospital type.
| Hospital | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Urban teaching | 29,420 (52.1%) | 30,755 (53%) | 40,005 (66.2%) | 41,285 (66.1%) | 41,325 (66.6%) | 44,345 (69.1%) | 48,105 (70.4%) | 54,395 (74.3%) | 329,635 (65.3%) |
| Urban nonteaching | 22,040 (39%) | 22,285 (38.4%) | 15,955 (26.4%) | 16,870 (27%) | 16,610 (26.8%) | 15,275 (23.8%) | 15,695 (23%) | 14,040 (19.2%) | 138,770 (27.5%) |
| Rural | 5030 (8.9%) | 4945 (8.5%) | 4490 (7.4%) | 4300 (6.9%) | 4115 (6.6%) | 4545 (7.1%) | 4560 (6.7%) | 4770 (6.5%) | 36,755 (7.3%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Figure 3.
Total hospital costs (a) and length of stay (b) by hospital type. Vertical bars represent 95% CI. US dollars adjusted for inflation, represented as December 2019 US dollars.
Discussion
TKA is one of the most commonly performed procedures in the United States and is associated with excellent overall outcomes. The number of TKA procedures performed annually in the US is expected to reach 1.3 to 3.5 million by the year 2030 [[2], [3], [4]]. During this same time period, the number of rTKAs performed is predicted to increase to 120,000 to 200,000 annually [13]. With the growing volume of rTKA, it becomes increasingly important to study the shifts in various trends to evaluate the efficacy and financial prudency of new developments in the field. Additionally, analysis of the causes and patterns associated with rTKA can assess current systems and guide future research.
Aseptic loosening is the most common cause of rTKA, with 23.1% of rTKAs attributed to aseptic loosening over the study period. The etiology of aseptic loosening is multifactorial and may be a result of implant, surgical, or patient factors [28,29]. From an implant perspective, wear debris from the polyethylene, cement, and metal can lead to particulate disease, inflammation, and loosening. Implant design and degree of constraint can also contribute. From a surgical perspective, malalignment, imbalance, and poor cement technique can increase rates of loosening, while patient factors such as osteoporosis, activity level, and elevated body mass index may also increase this risk. Contrary to THA, the adoption of highly cross-linked polyethylene (HXLPE) in TKA has been slower and more heterogenous over concerns for greater risk of wear delamination, pitting, and fatigue failure [[30], [31], [32]]. Although HXLPE has not shown any difference in the short term, the use of HXLPE has been shown to result in lower rates of rTKA for aseptic loosening in long-term registry studies [[33], [34], [35]]. While aseptic loosening secondary to polyethylene wear may be decreasing, other factors such as component alignment, cementation technique, or patient-specific factors (such as increasing rates of rTKA in high-body mass index individuals) may continue to contribute to the high prevalence of aseptic loosening [29,36,37]. In Australian and British joint registries, aseptic loosening remains the most common indication for rTKA accounting for 24.3% and 29.6% of rTKA, respectively, slightly higher than our findings here [38,39]. The rate of aseptic loosening in this study is slightly higher than that in prior epidemiological studies in the United States through 2013, which find roughly 20% of rTKAs attributed to PJI and aseptic loosening [14].
Similar to recent trends in TKA, we find a significant decrease in average LOS for rTKA patients over the study period from 4.0 to 3.8 days [40]. On subgroup analysis, however, LOS did not change for periprosthetic fracture and PJI rTKA patients, likely a result of increased time needed for preoperative planning and administration of intravenous antibiotics. Similarly, the proportion of patients discharged to facility also decreased significantly over the study period from 32% to 24%. This is in line with trends for primary TKA patients as well, with rates of nonhome discharge decreasing substantially over the past decade [41,42]. Increased LOS and nonhome discharges have been associated with worse patient outcomes including increased readmission, reoperations, and total costs [[43], [44], [45]].
We find that hospital costs increased significantly by roughly $1300 after adjusting for inflation despite a slight decrease in LOS. Inflation-adjusted hospital charges did increase significantly to nearly $115,000 in 2019. Bundled payment models through the Centers for Medicare and Medicaid [46] have resulted in an emphasis on cost containment by hospital systems in the treatment of arthroplasty patients [[47], [48], [49]]. This emphasis has driven decreased LOS and rates of nonhome discharge. The cost-savings of these changes may be offset by increased implant costs for rTKAs over the study period. Implant costs cannot be specifically isolated in NIS, and little has been published on rTKA implant costs although the variation seen in primary TKAs is likely to be amplified by the use of implants often required in a revision setting, such as condylar constrained knee or rotating hinge knee system, with modular stems, cones, and augments to treat ligamentous insufficiency and bone loss associated with rTKA [50]. There was significant regional variability in hospital costs, with the Western census region having the highest rTKA hospital costs but the lowest associated LOS. Further studies are needed to analyze the geographic disparities in LOS and costs for comparable procedures performed in other regions of the United States.
rTKAs Are often complex procedures requiring additional training, surgical expertise, and multidisciplinary care, which may be more commonly found at academic institutions. Between 2002 and 2008, just over 50% of rTKAs were performed in academic centers [51]. This proportion further increased from 52.1% to 74.3% in 2019 in our study. There was a corresponding drop in rTKA at urban nonacademic centers from 39% to 19.2%. The proportion of rTKA procedures performed at rural centers also decreased between 2012 and 2019. In a recent study utilizing the American Joints Replacement Registry, Lawson et al. found 78.3% of rTKAs were performed at academic institutions between 2012 and 2020 [50]. Patients undergoing rTKA for PJI were more likely to transfer care from a nonacademic to academic institution for their revision procedure. Academic medical centers often care for patients of increased medical complexity and serve as tertiary referral centers. Given the complexity of rTKA management, especially in the treatment of PJI, the establishment of centers of excellence focused on arthroplasty infection has been proposed [51].
The present study is not without its limitations. First, we recognize the inherent weaknesses in a large database study including potential for errors in coding and data entry. The transition to using ICD-10 codes in October 2015 was likely associated with increased variations in coding as new norms were being established [20]. However, our study is one of the first to utilize ICD-10 codes in a database study evaluating rTKA. We hope that future studies can continue to clarify and improve upon the procedure and diagnostic codes used in order to accurately capture and evaluate these patients. Given the limited granularity of ICD codes and coding errors, it is possible that types of conversion TKAs are included in our analysis of rTKA despite our best efforts to exclude them. This study did not evaluate any outcomes following the initial rTKA admission because the NIS does not include readmission data. Given the increased risk of complications after rTKA, it would be useful to evaluate how outcomes following rTKA have changed over the last decade. Furthermore, no information on functional outcomes after rTKA is available for analysis. Based on inability to link records in NIS, we were unable to determine when the implant being revised was initially placed. Lastly, information regarding surgical details such as implants used, procedure duration, intraoperative complications, and blood loss was unavailable in the NIS. Thus, we were unable to comment on changes in these variables over time.
Conclusions
Despite the above limitations, our study, to the best of our knowledge, reports on the largest number of rTKA patients to date in the United States and provides the most recent national epidemiological analysis. Our findings highlight some of the most recent trends in rTKA, which will be important to consider as the number of rTKA procedures continues to increase in the coming years. Importantly, while we find that aseptic loosening is the most common indication overall, PJI eclipsed aseptic loosening as the most common rTKA indication in 2019. All component revisions account for 60% of rTKA procedures, and isolated liner exchanges account for another 20%. Overall, costs have increased marginally, while charges have increased substantially. Significant regional variation exists with regard to LOS and costs associated with rTKA. Finally, rTKA procedures are increasingly being performed in urban academic centers.
Conflicts of interest
The authors declare that there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2022.03.004.
Supplementary Tables
Table S1.
Categorized rTKA diagnostic codes for ICD-9 and ICD-10.
| Group | ICD-9 | ICD-10 | ICD-10 text |
|---|---|---|---|
| Loosening | 996.41 | T84.03 | Mechanical loosening of internal prosthetic joint |
| T84.032 | Mechanical loosening of internal right knee prosthetic joint | ||
| T84.033 | Mechanical loosening of internal left knee prosthetic joint | ||
| T84.038 | Mechanical loosening of other internal prosthetic joint | ||
| T84.039 | Mechanical loosening of unspecified internal prosthetic joint | ||
| Infection | 996.66 | T84.5 | Infection and inflammatory reaction due to internal joint prosthesis |
| T84.50 | Infection and inflammatory reaction due to unspecified internal joint prosthesis | ||
| T84.53 | Infection and inflammatory reaction due to internal right knee prosthesis | ||
| T84.54 | Infection and inflammatory reaction due to internal left knee prosthesis | ||
| T84.59 | Infection and inflammatory reaction due to other internal joint prosthesis | ||
| 996.69 | T84.7 | Infection and inflammatory reaction due to other internal orthopedic prosthetic devices, implants and grafts | |
| Instability | 996.42 | T84.022 | Instability of internal right knee prosthesis |
| T84.023 | Instability of internal left knee prosthesis | ||
| T84.028 | Dislocation of other internal joint prosthesis | ||
| T84.029 | Dislocation of unspecified internal joint prosthesis | ||
| M24.3 | Pathological dislocation of joint, not elsewhere classified | ||
| M24.36 | Pathological dislocation of knee, not elsewhere classified | ||
| M24.40 | Recurrent dislocation, unspecified joint | ||
| M24.46 | Recurrent dislocation, knee | ||
| S83.00 | Unspecified subluxation and dislocation of patella | ||
| S83.01 | Lateral subluxation and dislocation of patella | ||
| S83.09 | Other subluxation and dislocation of patella | ||
| S83.10 | Unspecified subluxation and dislocation of knee | ||
| S83.11 | Anterior subluxation and dislocation of proximal end of tibia | ||
| S83.12 | Posterior subluxation and dislocation of proximal end of tibia | ||
| S83.13 | Medial subluxation and dislocation of proximal end of tibia | ||
| S83.14 | Lateral subluxation and dislocation of proximal end of tibia | ||
| S83.19 | Other subluxation and dislocation of knee | ||
| Breakage | 996.43 | T84.01 | Broken internal joint prosthesis |
| T84.012 | Broken internal right knee prosthesis | ||
| T84.013 | Broken internal left knee prosthesis | ||
| T84.018 | Broken internal joint prosthesis, other site | ||
| T84.019 | Broken internal joint prosthesis, unspecified site | ||
| Periprosthetic fracture | 996.44 | M97 | Periprosthetic fracture around internal prosthetic joint |
| M97.1 | Periprosthetic fracture around internal prosthetic knee joint | ||
| M97.11 | Periprosthetic fracture around internal prosthetic right knee joint | ||
| M97.12 | Periprosthetic fracture around internal prosthetic left knee joint | ||
| M97.8 | Periprosthetic fracture around other internal prosthetic joint | ||
| M97.9 | Periprosthetic fracture around unspecified internal prosthetic joint | ||
| Osteolysis | 996.45 | T84.05 | Periprosthetic osteolysis of internal prosthetic joint |
| T84.052 | Periprosthetic osteolysis of internal prosthetic right knee joint | ||
| T84.053 | Periprosthetic osteolysis of internal prosthetic left knee joint | ||
| T84.058 | Periprosthetic osteolysis of other internal prosthetic joint | ||
| T84.059 | Periprosthetic osteolysis of unspecified internal prosthetic joint | ||
| M89.5 | Osteolysis | ||
| Bearing surface wear | 996.46 | T84.06 | Wear of articular bearing surface of internal prosthetic joint |
| T84.062 | Wear of articular bearing surface of internal prosthetic right knee joint | ||
| T84.063 | Wear of articular bearing surface of internal prosthetic left knee joint | ||
| T84.068 | Wear of articular bearing surface of other internal prosthetic joint | ||
| T84.069 | Wear of articular bearing surface of unspecified internal prosthetic joint | ||
| Other Mechanical | 996.47 | T84.09 | Other mechanical complication of internal joint prosthesis |
| T84.092 | Other mechanical complication of internal right knee prosthesis | ||
| T84.093 | Other mechanical complication of internal left knee prosthesis | ||
| T84.098 | Other mechanical complication of other internal joint prosthesis | ||
| T84.099 | Other mechanical complication of unspecified internal joint prosthesis | ||
| 996.49 | T84.4 | Mechanical complication of other internal orthopedic devices, implants, and grafts | |
| T84.41 | Breakdown (mechanical) of other internal orthopedic devices, implants and grafts | ||
| T84.42 | Displacement of other internal orthopedic devices, implants and grafts | ||
| T84.49 | Other mechanical complication of other internal orthopedic devices, implants and grafts | ||
| T84.3 | Mechanical complication of other bone devices, implants and grafts | ||
| T84.32 | Displacement of other bone devices, implants and grafts | ||
| T84.39 | Other mechanical complication of other bone devices, implants and grafts | ||
| Other | 996.77 | T84.8 | Other specified complications of internal orthopedic prosthetic devices, implants and grafts |
| T84.81 | Embolism due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.82 | Fibrosis due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.83 | Hemorrhage due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.84 | Pain due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.85 | Stenosis due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.86 | Thrombosis due to internal orthopedic prosthetic devices, implants and grafts | ||
| T84.89 | Other specified complication of internal orthopedic prosthetic devices, implants and grafts | ||
| T84.9 | Unspecified complication of internal orthopedic prosthetic device, implant and graft |
Table S2.
Age groups of patients undergoing rTKA.
| Age | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | All |
|---|---|---|---|---|---|---|---|---|---|
| <55 | 10,055 (17.8%) | 9235 (15.9%) | 9630 (15.9%) | 9510 (15.2%) | 8990 (14.5%) | 8310 (13%) | 8505 (12.4%) | 8230 (11.2%) | 72,465 (14.3%) |
| 55-64 | 17,200 (30.4%) | 17,990 (31%) | 18,720 (31%) | 19,050 (30.5%) | 19,270 (31.1%) | 19,510 (30.4%) | 20,415 (29.9%) | 21,550 (29.4%) | 153,705 (30.4%) |
| 65-74 | 17,380 (30.8%) | 18,795 (32.4%) | 20,005 (33.1%) | 20,635 (33%) | 21,200 (34.2%) | 23,370 (36.4%) | 25,055 (36.7%) | 27,025 (36.9%) | 173,465 (34.3%) |
| 75+ | 11,855 (21%) | 11,965 (20.6%) | 12,095 (20%) | 13,260 (21.2%) | 12,590 (20.3%) | 12,975 (20.2%) | 14,385 (21%) | 16,400 (22.4%) | 105,525 (20.9%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Table S3.
Payor for patients undergoing rTKA.
| Payor | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | All |
|---|---|---|---|---|---|---|---|---|---|
| Medicare | 32,185 (57%) | 33,615 (58%) | 35,165 (58.2%) | 36,595 (58.6%) | 36,645 (59.1%) | 38,090 (59.4%) | 41,590 (60.8%) | 45,490 (62.1%) | 299,375 (59.3%) |
| Private | 18,135 (32.1%) | 18,385 (31.7%) | 18,965 (31.4%) | 19,300 (30.9%) | 18,830 (30.3%) | 19,265 (30%) | 19,500 (28.5%) | 20,125 (27.5%) | 152,505 (30.2%) |
| Medicaid | 2420 (4.3%) | 2390 (4.1%) | 2750 (4.5%) | 3075 (4.9%) | 3410 (5.5%) | 3370 (5.3%) | 3665 (5.4%) | 3600 (4.9%) | 24,680 (4.9%) |
| Other | 3615 (6.4%) | 3535 (6.1%) | 3465 (5.7%) | 3445 (5.5%) | 3105 (5%) | 3320 (5.2%) | 3555 (5.2%) | 3920 (5.4%) | 27,960 (5.5%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Table S4.
Indication by specific components revised.
| Indication | All components | Tibia | Femur | Liner | Patella | Total |
|---|---|---|---|---|---|---|
| Loosening | 82,510 (70.8%) | 20,060 (17.2%) | 6615 (5.7%) | 3625 (3.1%) | 3745 (3.2%) | 116,555 |
| PJI | 45,340 (44.1%) | 8450 (8.2%) | 2535 (2.5%) | 42,805 (41.6%) | 3750 (3.6%) | 102,880 |
| Instability | 26,470 (47.5%) | 6620 (11.9%) | 3435 (6.2%) | 15,955 (28.6%) | 3290 (5.9%) | 55,770 |
| Bearing surface wear | 4335 (37%) | 1590 (13.6%) | 255 (2.2%) | 4345 (37.1%) | 1180 (10.1%) | 11,705 |
| Periprosthetic fracture | 5655 (69%) | 620 (7.6%) | 1245 (15.2%) | 415 (5.1%) | 255 (3.1%) | 8190 |
| Osteolysis | 2655 (78.4%) | 270 (8%) | 170 (5%) | 220 (6.5%) | 70 (2.1%) | 3385 |
| Breakage | 3135 (52.9%) | 840 (14.2%) | 510 (8.6%) | 815 (13.8%) | 625 (10.5%) | 5925 |
| Other | 84,800 (63%) | 14,140 (10.5%) | 6915 (5.1%) | 20,705 (15.4%) | 8135 (6%) | 134,695 |
| Missing | 47,810 (72.4%) | 3485 (5.3%) | 1970 (3%) | 10,310 (15.6%) | 2480 (3.8%) | 66,055 |
| Total | 302,710 (59.9%) | 56,075 (11.1%) | 23,650 (4.7%) | 99,195 (19.6%) | 23,530 (4.7%) | 505,160 |
Table S5.
Average total hospital charges by rTKA indication.
| Indication | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Loosening | 93,074 (1283) | 98,135 (1217) | 101,558 (1251) | 105,455 (1357) | 107,520 (1246) | 110,800 (2095) | 114,797 (1272) | 119,081 (1436) | 107,341 (523) |
| PJI | 95,828 (2154) | 96,357 (1788) | 106,569 (2327) | 110,197 (2072) | 111,458 (2461) | 112,281 (1889) | 122,795 (3692) | 123,334 (1902) | 112,286 (893) |
| Dislocation | 74,336 (1717) | 75,537 (1934) | 76,217 (1974) | 80,483 (1977) | 84,193 (1654) | 82,802 (1513) | 90,422 (1808) | 91,994 (1833) | 83,609 (650) |
| Bearing surface wear | 57,811 (2395) | 60,337 (2877) | 56,329 (2479) | 59,542 (2287) | 65,465 (3017) | 64,414 (2660) | 62,000 (2735) | 59,836 (3042) | 60,835 (957) |
| Periprosthetic fracture | 143,103 (9064) | 146,638 (8549) | 144,935 (6802) | 164,021 (9135) | 152,571 (12410) | 166,012 (6710) | 180,749 (7857) | 192,055 (7447) | 168,633 (3073) |
| Osteolysis | 107,634 (7330) | 105,900 (5732) | 115,786 (11775) | 117,625 (7466) | 114,888 (6545) | 110,918 (7758) | 130,225 (10119) | 112,757 (7180) | 113,959 (2822) |
| Breakage | 80,594 (5691) | 87,678 (5857) | 93,013 (10610) | 87,214 (7356) | 100,728 (6679) | 92,392 (5411) | 94,984 (5170) | 94,380 (5555) | 92,251 (2304) |
| Other | 78,619 (896) | 84,617 (934) | 83,772 (898) | 87,769 (1000) | 85,436 (1125) | 89,361 (1244) | 94,086 (1275) | 97,438 (1475) | 86,963 (383) |
| Missing | 100,314 (1734) | 108,003 (1904) | 108,020 (1813) | 109,196 (1855) | 113,110 (2236) | 114,333 (2251) | 115,099 (2094) | 119,214 (2491) | 111,096 (735) |
| Total | 87,394 (634) | 92,435 (625) | 94,637 (681) | 98,697 (689) | 100,218 (764) | 103,107 (828) | 109,490 (1042) | 113,158 (821) | 100,580 (281) |
Standard error in parentheses.
Table S6.
Number of rTKA operations by census region.
| Region | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | All |
|---|---|---|---|---|---|---|---|---|---|
| Northeast | 9545 (16.9%) | 9710 (16.7%) | 10,010 (16.6%) | 10,925 (17.5%) | 10,725 (17.3%) | 10,995 (17.1%) | 11,325 (16.6%) | 12,190 (16.7%) | 85,425 (16.9%) |
| Midwest | 14,985 (26.5%) | 15,530 (26.8%) | 15,970 (26.4%) | 16,095 (25.8%) | 16,595 (26.7%) | 16,980 (26.5%) | 17,825 (26.1%) | 18,800 (25.7%) | 132,780 (26.3%) |
| South | 20,630 (36.5%) | 21,570 (37.2%) | 22,425 (37.1%) | 23,040 (36.9%) | 22,755 (36.7%) | 23,600 (36.8%) | 26,165 (38.3%) | 28,220 (38.5%) | 188,405 (37.3%) |
| West | 11,330 (20.1%) | 11,175 (19.3%) | 12,045 (19.9%) | 12,395 (19.8%) | 11,975 (19.3%) | 12,590 (19.6%) | 13,045 (19.1%) | 13,995 (19.1%) | 98,550 (19.5%) |
| Total | 56,490 | 57,985 | 60,450 | 62,455 | 62,050 | 64,165 | 68,360 | 73,205 | 505,160 |
Table S7.
Average total hospital costs by US census region.
| Region | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Midwest | 24,944 (287) | 24,973 (269) | 24,788 (322) | 24,773 (266) | 24,354 (236) | 25,635 (835) | 25,781 (721) | 26,188 (252) | 25,213 (166) |
| Northeast | 23,728 (359) | 24,676 (392) | 24,402 (428) | 24,632 (357) | 25,376 (419) | 24,414 (350) | 24,820 (350) | 26,969 (387) | 24,932 (135) |
| South | 25,165 (287) | 24,410 (231) | 24,542 (230) | 25,098 (235) | 24,969 (230) | 24,826 (233) | 24,613 (203) | 25,524 (245) | 24,907 (84) |
| West | 29,701 (454) | 29,918 (417) | 29,010 (395) | 29,331 (416) | 28,482 (459) | 29,525 (365) | 30,710 (393) | 31,554 (547) | 29,838 (156) |
| Total | 25,730 (170) | 25,620 (153) | 25,434 (161) | 25,731 (152) | 25,523 (155) | 25,893 (253) | 26,117 (224) | 27,077 (169) | 25,927 (66) |
Standard error in parentheses.
Table S8.
Average length of stay for rTKA patients by US census region.
| Region | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Midwest | 3.78 (0.06) | 3.69 (0.05) | 3.66 (0.06) | 3.61 (0.06) | 3.34 (0.05) | 3.31 (0.06) | 3.35 (0.06) | 3.47 (0.06) | 3.52 (0.02) |
| Northeast | 4.31 (0.09) | 4.18 (0.09) | 4.18 (0.11) | 3.96 (0.08) | 3.87 (0.09) | 3.74 (0.08) | 3.66 (0.08) | 3.97 (0.09) | 3.97 (0.03) |
| South | 4.05 (0.06) | 3.89 (0.05) | 3.88 (0.05) | 3.92 (0.06) | 3.69 (0.05) | 3.66 (0.06) | 3.66 (0.05) | 3.93 (0.07) | 3.83 (0.02) |
| West | 3.72 (0.07) | 3.54 (0.06) | 3.48 (0.06) | 3.55 (0.1) | 3.34 (0.08) | 3.21 (0.06) | 3.45 (0.07) | 3.73 (0.12) | 3.5 (0.03) |
| Total | 3.96 (0.03) | 3.82 (0.03) | 3.79 (0.03) | 3.77 (0.04) | 3.56 (0.03) | 3.49 (0.03) | 3.54 (0.03) | 3.78 (0.04) | 3.71 (0.01) |
Standard error in parentheses.
Table S9.
Average hospital costs for rTKA treatment by hospital type.
| Hospital | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Urban teaching | 25,898 (245) | 26,170 (216) | 25,668 (206) | 25,691 (182) | 25,686 (198) | 25,753 (174) | 26,265 (298) | 27,213 (203) | 26,097 (79) |
| Urban nonteaching | 25,027 (259) | 24,318 (231) | 24,096 (264) | 24,990 (303) | 24,479 (267) | 24,512 (298) | 24,710 (283) | 25,905 (321) | 24,733 (98) |
| Rural | 27,833 (557) | 28,083 (585) | 28,105 (656) | 28,987 (605) | 28,093 (601) | 31,888 (2963) | 29,417 (663) | 28,989 (648) | 28,913 (420) |
| Total | 25,730 (170) | 25,620 (153) | 25,434 (161) | 25,731 (152) | 25,523 (155) | 25,893 (253) | 26,117 (224) | 27,077 (169) | 25,927 (66) |
Standard error in parentheses.
Table S10.
Average length of stay for rTKA patients by hospital type.
| Hospital | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Urban teaching | 4.11 (0.05) | 4.02 (0.05) | 3.92 (0.04) | 3.89 (0.04) | 3.71 (0.04) | 3.65 (0.04) | 3.67 (0.04) | 3.96 (0.05) | 3.85 (0.02) |
| Urban nonteaching | 3.76 (0.05) | 3.57 (0.04) | 3.46 (0.05) | 3.51 (0.08) | 3.28 (0.05) | 3.08 (0.05) | 3.22 (0.07) | 3.2 (0.07) | 3.41 (0.02) |
| Rural | 3.89 (0.09) | 3.74 (0.08) | 3.85 (0.12) | 3.65 (0.12) | 3.18 (0.07) | 3.32 (0.09) | 3.24 (0.1) | 3.43 (0.15) | 3.55 (0.04) |
| Total | 3.96 (0.03) | 3.82 (0.03) | 3.79 (0.03) | 3.77 (0.04) | 3.56 (0.03) | 3.49 (0.03) | 3.54 (0.03) | 3.78 (0.04) | 3.71 (0.01) |
Standard error in parentheses.
Table S11.
Primary revision indication by hospital type.
| Indication | Urban teaching | Urban nonteaching | Rural | Total |
|---|---|---|---|---|
| Loosening | 74,060 (22.5%) | 32,680 (23.5%) | 9815 (26.7%) | 116,555 (23.1%) |
| PJI | 70,740 (21.5%) | 25,065 (18.1%) | 7075 (19.2%) | 102,880 (20.4%) |
| Instability | 36,630 (11.1%) | 15,475 (11.2%) | 3665 (10%) | 55,770 (11%) |
| Bearing surface wear | 7110 (2.2%) | 3660 (2.6%) | 935 (2.5%) | 11,705 (2.3%) |
| Periprosthetic fracture | 5970 (1.8%) | 1805 (1.3%) | 415 (1.1%) | 8190 (1.6%) |
| Osteolysis | 2160 (0.7%) | 980 (0.7%) | 245 (0.7%) | 3385 (0.7%) |
| Breakage | 4055 (1.2%) | 1545 (1.1%) | 325 (0.9%) | 5925 (1.2) |
| Other | 86,210 (26.2%) | 39,660 (28.6%) | 8825 (24%) | 134,695 (26.7%) |
| Missing | 42,700 (13%) | 17,900 (12.9%) | 5455 (14.8%) | 66,055 (13.1%) |
| Total | 329,635 | 138,770 | 36,755 | 505,160 |
Appendix A. Supplementary data
References
- 1.Jenkins P.J., Clement N.D., Hamilton D.F., Gaston P., Patton J.T., Howie C.R. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013;95-b:115–121. doi: 10.1302/0301-620x.95b1.29835. [DOI] [PubMed] [Google Scholar]
- 2.Inacio M.C.S., Paxton E.W., Graves S.E., Namba R.S., Nemes S. Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage. 2017;25:1797–1803. doi: 10.1016/j.joca.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 3.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/jbjs.F.00222. [DOI] [PubMed] [Google Scholar]
- 4.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455–1460. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz S.M., Ong K.L., Lau E., Bozic K.J. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–630. doi: 10.2106/jbjs.M.00285. [DOI] [PubMed] [Google Scholar]
- 6.Patel A., Pavlou G., Mújica-Mota R.E., Toms A.D. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J. 2015;97-b:1076–1081. doi: 10.1302/0301-620x.97b8.35170. [DOI] [PubMed] [Google Scholar]
- 7.Guerrero-Ludueña R.E., Comas M., Espallargues M., et al. Predicting the burden of revision knee arthroplasty: simulation of a 20-year horizon. Value Health. 2016;19:680–687. doi: 10.1016/j.jval.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 8.Weber M., Renkawitz T., Voellner F., et al. Revision surgery in total joint replacement is cost-intensive. Biomed Res Int. 2018;2018:8987104. doi: 10.1155/2018/8987104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bunn K.J., Isaacson M.J., Ismaily S.K., Noble P.C., Incavo S.J. Quantifying and predicting surgeon work effort for primary and revision total knee arthroplasty. J Arthroplasty. 2016;31:59–62. doi: 10.1016/j.arth.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Nichols C.I., Vose J.G. Comparative risk of transfusion and incremental total hospitalization cost for primary unilateral, bilateral, and revision total knee arthroplasty procedures. J Arthroplasty. 2016;31:583.e1. doi: 10.1016/j.arth.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Burns A.W., Bourne R.B., Chesworth B.M., MacDonald S.J., Rorabeck C.H. Cost effectiveness of revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:29–33. doi: 10.1097/01.blo.0000214420.14088.76. [DOI] [PubMed] [Google Scholar]
- 12.Pugely A.J., Martin C.T., Gao Y., Schweizer M.L., Callaghan J.J. The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty. 2015;30:47–50. doi: 10.1016/j.arth.2015.01.063. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz A.M., Farley K.X., Guild G.N., Bradbury T.L. Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty. 2020;35:S79–S85. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delanois R.E., Mistry J.B., Gwam C.U., Mohamed N.S., Choksi U.S., Mont M.A. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017;32:2663–2668. doi: 10.1016/j.arth.2017.03.066. [DOI] [PubMed] [Google Scholar]
- 15.Bozic K.J., Kurtz S.M., Lau E., et al. The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res. 2010;468:45–51. doi: 10.1007/s11999-009-0945-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kamath A.F., Ong K.L., Lau E., et al. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015;30:1492–1497. doi: 10.1016/j.arth.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 17.Bohl D.D., Samuel A.M., Basques B.A., Della Valle C.J., Levine B.R., Grauer J.N. How much do adverse event rates differ between primary and revision total joint arthroplasty? J Arthroplasty. 2016;31:596–602. doi: 10.1016/j.arth.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 18.Nichols C.I., Vose J.G. Clinical outcomes and costs within 90 Days of primary or revision total joint arthroplasty. J Arthroplasty. 2016;31:1400–1406.e3. doi: 10.1016/j.arth.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality Healthcare cost and utilization Project (HCUP) databases 2020. www.hcup-us.ahrq.gov/nisoverview.jsp [accessed 7.07.21] [PubMed]
- 20.Lygrisse K.A., Roof M.A., Keitel L.N., Callaghan J.J., Schwarzkopf R., Bedard N.A. The inaccuracy of ICD-10 coding in revision total hip arthroplasty and its implication on revision data. J Arthroplasty. 2020;35:2960–2965.e3. doi: 10.1016/j.arth.2020.05.013. [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez T., Chiodo C. ICD 10: a primer for the orthopedic foot and ankle surgeon. Foot Ankle Int. 2015;36:1110–1116. doi: 10.1177/1071100715600286. [DOI] [PubMed] [Google Scholar]
- 22.Marsh R.S., Hatic S.O., 2nd, Curless B., et al. ICD-10 and its impact on our practice. Foot Ankle Spec. 2015;8:289–291. doi: 10.1177/1938640015595044. [DOI] [PubMed] [Google Scholar]
- 23.Henley M.B. ICD 10: “what orthopedic surgeons should know, how it will affect them and the cost of implementation?”. Sport Med Arthrosc Rev. 2013;21:142–147. doi: 10.1097/JSA.0b013e3182991370. [DOI] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality Healthcare cost and utilization Project (HCUP) introduction to the NIS 2016. www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2014.jsp [accessed 7.07.21] [PubMed]
- 25.Upfill-Brown A., Hsiue P.P., Sekimura T., Patel J.N., Adamson M., Stavrakis A.I. Instability is the most common indication for revision hip arthroplasty in the United States: national trends from 2012 to 2018. Arthroplast Today. 2021;11:88–101. doi: 10.1016/j.artd.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agency for Healthcare Research and Quality Healthcare cost and utilization Project (HCUP) cost-to-charge ratio files 2020. www.hcup-us.ahrq.gov/db/ccr/costtocharge.jsp [accessed 7.07.21] [PubMed]
- 27.Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1–19. doi: 10.18637/jss.v009.i08. [DOI] [Google Scholar]
- 28.Sundfeldt M., Carlsson L.V., Johansson C.B., Thomsen P., Gretzer C. Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop. 2006;77:177–197. doi: 10.1080/17453670610045902. [DOI] [PubMed] [Google Scholar]
- 29.Hampton C.B., Berliner Z.P., Nguyen J.T., et al. Aseptic loosening at the tibia in total knee arthroplasty: a function of cement mantle quality? J Arthroplasty. 2020;35:S190–S196. doi: 10.1016/j.arth.2020.02.028. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen L.C.L., Lehil M.S., Bozic K.J. Trends in total knee arthroplasty implant utilization. J Arthroplasty. 2015;30:739–742. doi: 10.1016/j.arth.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 31.Chakrabarty G., Vashishtha M., Leeder D. Polyethylene in knee arthroplasty: a review. J Clin Orthop Trauma. 2015;6:108–112. doi: 10.1016/j.jcot.2015.01.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lachiewicz P.F., Soileau E.S. Is there a benefit to highly crosslinked polyethylene in posterior-stabilized total knee arthroplasty? A randomized trial. Clin Orthop Relat Res. 2016;474:88–95. doi: 10.1007/s11999-015-4241-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gkiatas I., Karasavvidis T., Sharma A.K., et al. Highly cross-linked polyethylene in primary total knee arthroplasty is associated with a lower rate of revision for aseptic loosening: a meta-analysis of 962,467 cases. Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-021-03887-z. [DOI] [PubMed] [Google Scholar]
- 34.Partridge T.C.J., Baker P.N., Jameson S.S., Mason J., Reed M.R., Deehan D.J. Conventional versus highly cross-linked polyethylene in primary total knee replacement. J Bone Joint Surg Am. 2020;102:119–127. doi: 10.2106/jbjs.19.00031. [DOI] [PubMed] [Google Scholar]
- 35.De Steiger R.N., Muratoglu O., Lorimer M., Cuthbert A.R., Graves S.E. Lower prosthesis-specific 10-year revision rate with crosslinked than with non-crosslinked polyethylene in primary total knee arthroplasty. Acta Orthop. 2015;86:721–727. doi: 10.3109/17453674.2015.1065046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thiele K., Perka C., Matziolis G., Mayr H.O., Sostheim M., Hube R. Wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97:715–720. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 37.Kerkhoffs G.M.M.J., Servien E., Dunn W., Dahm D., Bramer J.A.M., Haverkamp D. The influence of obesity on the complication rate and outcome of total knee arthroplasty. J Bone Joint Surg Am. 2012;94:1839–1844. doi: 10.2106/JBJS.K.00820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.AOANJRR . 2020. Annual 2020. Aust orthop assoc Natl Jt replace regist 2020 Annual Report; p. 289. [Google Scholar]
- 39.Ben-Shlomo Y., Blom A., Boulton C., et al. National Joint Registry Annual Reports; London: 2020. National Joint Registry - 17th Annual Report 2020. [Google Scholar]
- 40.Sarpong N.O., Boddapati V., Herndon C.L., Shah R.P., Cooper H.J., Geller J.A. Trends in length of stay and 30-day complications after total knee arthroplasty: an analysis from 2006 to 2016. J Arthroplasty. 2019;34:1575–1580. doi: 10.1016/j.arth.2019.04.027. [DOI] [PubMed] [Google Scholar]
- 41.DeMik D.E., Carender C.N., Glass N.A., Callaghan J.J., Bedard N.A. More patients are being discharged home after total knee arthroplasty, however rates vary between large databases. J Arthroplasty. 2021;36:173–179. doi: 10.1016/j.arth.2020.07.059. [DOI] [PubMed] [Google Scholar]
- 42.Ramkumar P.N., Gwam C., Navarro S.M., et al. Discharge to the skilled nursing facility: patient risk factors and perioperative outcomes after total knee arthroplasty. Ann Transl Med. 2019;7:65. doi: 10.21037/atm.2018.12.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McLawhorn A.S., Fu M.C., Schairer W.W., Sculco P.K., MacLean C.H., Padgett D.E. Continued inpatient care after primary total knee arthroplasty increases 30-day post-discharge complications: a propensity score-adjusted analysis. J Arthroplasty. 2017;32:S113–S118. doi: 10.1016/j.arth.2017.01.039. [DOI] [PubMed] [Google Scholar]
- 44.Keswani A., Tasi M.C., Fields A., Lovy A.J., Moucha C.S., Bozic K.J. Discharge destination after total joint arthroplasty: an analysis of postdischarge outcomes, placement risk factors, and recent trends. J Arthroplasty. 2016;31:1155–1162. doi: 10.1016/j.arth.2015.11.044. [DOI] [PubMed] [Google Scholar]
- 45.Owens J.M., Callaghan J.J., Duchman K.R., Bedard N.A., Otero J.E. Short-term morbidity and readmissions increase with skilled nursing facility discharge after total joint arthroplasty in a medicare-eligible and skilled nursing facility–eligible patient cohort. J Arthroplasty. 2018;33:1343–1347. doi: 10.1016/j.arth.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 46.Sullivan R., Jarvis L.D., O’Gara T., Langfitt M., Emory C. Bundled payments in total joint arthroplasty and spine surgery. Curr Rev Musculoskelet Med. 2017;10:218–223. doi: 10.1007/s12178-017-9405-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lovald S.T., Ong K.L., Malkani A.L., et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014;29:510–515. doi: 10.1016/j.arth.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 48.Haas D.A., Kaplan R.S. Variation in the cost of care for primary total knee arthroplasties. Arthroplast Today. 2017;3:33–37. doi: 10.1016/j.artd.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Molloy I.B., Martin B.I., Moschetti W.E., Jevsevar D.S. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99:402–407. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lawson K.A., Chen A.F., Springer B.D., et al. Migration patterns for revision total knee arthroplasty in the United States as reported in the American joint replacement registry. J Arthroplasty. 2021;36:3538–3542. doi: 10.1016/j.arth.2021.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barnes C.L., Vail T.P., Takemoto S.K. Where do knee revisions for infection, fracture, and other revisions get treated? J Arthroplasty. 2013;28:423–428. doi: 10.1016/j.arth.2012.06.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.