Abstract
Background
Arrhythmia is a significant clinical modifier in COVID‐19 patient outcomes. Currently, data on arrhythmia and ECG characteristics in COVID‐19 from lower middle‐income countries are limited.
Methods
COVID‐19 was confirmed by polymerase chain reaction testing of a nasopharyngeal sample. All clinical records were systematically evaluated to obtain demographic characteristics and medical comorbidities. The ECG was recorded on admission, in‐hospital, and at discharge.
Results
Total documented arrhythmia events account for 22% of patients, comprising 6% of new‐onset arrhythmia and 16% of existing arrhythmia. Atrial fibrillation is the most common arrhythmia. The ECG changes were a decrease in heart rate (91 ± 22 vs. 83 ± 20, p < .001) and an increase in the QT interval (354.7 ± 53.70 vs. 371.4 ± 59.48 msec, p < .001) from hospital admission to hospital discharge, respectively. The in‐hospital HR of 85 bpm or higher increases the risk of death (OR = 2.69, p = .019).
Conclusion
The incidence of arrhythmias in COVID‐19 patients at COVID‐19 referral hospitals in Indonesia is 22%. Atrial fibrillation is the most common arrhythmia in COVID‐19 patients. Prolongation of QRS duration from admission to discharge was related to the occurrence of new‐onset arrhythmia. The in‐hospital HR of 85 bpm or higher increased the risk of death.
Keywords: arrhythmia, Covid‐19, ECG, heart rate
The incidence of arrhythmias in Covid‐19 patient at Covid‐19 referral hospital in Indonesia is 22%. Atrial fibrillation is the most common arrhythmia in Covid‐19 patient. Prolongation of QRS duration from admission to discharge was related to occurrence of new onset arrhythmia. The in‐hospital HR of 85 bpm or higher increase the risk of death.
1. INTRODUCTION
The Covid‐19 pandemic lasted for almost 2 years since the first case in December 2019 at Wuhan. Although the main symptoms of Covid‐19 are related to the respiratory system, heart involvement, especially arrhythmias, has been previously identified. Initial work by Wang et al. 1 revealed that arrhythmia occurrence was about 17% among hospitalized Covid‐19 patients. Currently, only limited data on arrhythmia characteristics in Covid‐19 patients have been published, and most of them come from developed countries equipped with sophisticated medical facilities.
This study aims to elaborate on arrhythmia and ECG characteristics of Covid‐19 patients hospitalized in a lower middle‐income country with fewer medical facilities and budgets.
2. METHODS
2.1. Study population
A total of 200 confirmed Covid‐19 patients by polymerase chain reaction testing of a nasopharyngeal sample participated in this study. A retrospective cohort was done in Covid‐19 referral hospitals of Pertamina Jaya Hospital, Fatmawati General Hospital, and National Cardiovascular Center Harapan Kita. The study received approval from the Institutional Review Board at National Cardiovascular Center Harapan Kita, Jakarta.
2.2. Clinical variables
All clinical records were systematically evaluated to obtain demographic characteristics and medical comorbidities. All the comorbidities were based on the final diagnosis recorded in medical records made by the physicians at discharge. The ECGs were recorded on admission and at discharge. If any arrhythmias occurred during hospitalization, additional ECG was recorded. Subjects with arrhythmia events were divided into new‐onset and preexisting arrhythmia groups. Patients with normal sinus rhythm during admission who had arrhythmia events during hospitalization were classified as new‐onset arrhythmia group. Meanwhile, patients who had arrhythmias during admission were classified into the preexisting arrhythmia group. The outcomes of this study were mechanical ventilation requirement, ICU admission, hospital length of stay, and mortality. In addition, the outcomes were analyzed in relation to the patient's grouping.
2.3. Statistical analysis
Statistical analyses were performed using SPSS, version 25. We compared the clinical and ECG characteristics of patients with and without arrhythmias. The proportion of arrhythmias was calculated against the total number of patients who participated during the study period. The ECG characteristics and type of arrhythmia were analyzed using Pearson regression for correlation with clinical outcome. The categorical variables were analyzed using the Chi‐square test, while an independent sample t test/Mann–Whitney U test was used for continuous data. Nominal variables will be displayed as means and standard deviations. Various confounding variables will be tested by bivariate followed by multivariate. Statistical significance was considered significant if the p value was <.05.
3. RESULTS
3.1. Clinical characteristics
The majority of cases are male and relatively young. Hypertension and cerebrovascular disease (CVD) are the predominant comorbidities. Table 1 shows demographic and comorbid proportions. All patients took azithromycin 500 mg QD for the initial 5 days of hospitalization, but none took hydrochloroquine. Other medications were antiviral (favipiravir or remdesivir), additional intravenous antibiotic if needed, 1 g vitamin C injection, oral vitamin D 5000 IU, and oral Zinc sulfate. Actemra was rarely given due to undersupply and high cost .
TABLE 1.
Clinical characteristics
| Parameters | Description |
|---|---|
| Age | 52 ± 14 |
| Gender | |
| Male | 134 (67%) |
| Female | 66 (33%) |
| Comorbidities | |
| Hypertension | 88 (44%) |
| CAD | 5 (2.5%) |
| DM | 68 (34%) |
| Chronic respiratory disease | 19 (9.5%) |
| CKD | 23 (11.5%) |
| CVD | 104 (52%) |
| Obesity | 5 (2.5%) |
| LOS (days) | 17 ± 11 |
Abbreviations: CAD, coronary artery disease; CKD, chronic kidney disease; CVD, cerebrovascular disease; DM, diabetes mellitus; LOS, length of stay.
3.2. Rhythm characteristics
Total documented arrhythmia events account for 22% of patients, comprising 6% of new‐onset arrhythmia and 16% of preexisting arrhythmia. Atrial fibrillation was the commonest arrhythmia encountered in our subjects, but there was no documented ventricular arrhythmia event. During the average hospital length of stay of 17.50 ± 11.02 days proportion of most arrhythmias decreases significantly from admission to discharge (Table 2). Total AV block occurred in 1 patient and persisted until 14 days, warrants permanent pacemaker implantation (Figure 1).
TABLE 2.
The arrhythmia types and ECG parameters during admission and discharge
| Rhythm and ECG | Recording time | p value | |
|---|---|---|---|
| Admission (n = 200) | Discharge (n = 200) | ||
| Rhythm types | |||
| Sinus rhythm | 171 (85.5%) | 176 (88%) | <.001 |
| Atrial fibrillation | 21 (10.5%) | 18 (9%) | <.001 |
| Atrial flutter | 2 (1%) | 1 (0.5%) | .01 |
| Junctional rhythm | 1 (0.5%) | 1 (0.5%) | 1.00 |
| Pacing rhythm | 1 (0.5%) | 2 (1%) | .01 |
| AV block | 4 (2%) | 2 (1%) | .04 |
| ECG parameters | |||
| Heart rate (bpm) | 91 ± 22 | 83 ± 20 | <.001 |
| QRS duration (ms) | 88.7 ± 18.5 | 90.3 ± 21.1 | .224 |
| QT interval (ms) | 354.7 ± 53.7 | 371.4 ± 59.5 | <.001 |
| QTc interval (ms) | 431.4 ± 81.7 | 430.9 ± 56.5 | .229 |
| ST‐T changes (%) | 35 | 36 | .695 |
FIGURE 1.
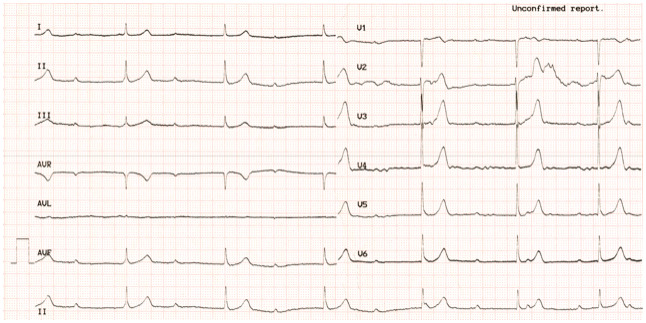
Complete heart block happened at ninth days of hospitalization in one patient
3.3. ECG parameters
Three cardiology fellows manually calculated basic ECG parameters with intra‐ and interobserver agreement of 0.80 and 0.89, respectively. There was a total of 400 ECGs on admission and discharge. The mean heart rate was decreased, whereas the QT interval was slightly increased from admission to discharge (Table 2). The QRS duration, QT corrected (QTc) interval, and ST‐T changes were not statistically different.
Subgroup analysis based on arrhythmia onset showed that in patients with normal sinus rhythm, heart rate was significantly decreased from admission to discharge. On the contrary, the QT interval was increased. Patients in the new‐onset arrhythmia group had a significant increase in QRS duration from admission to discharge. The preexisting arrhythmia group showed no significant differences in all measured ECG parameters (Table 3).
TABLE 3.
The ECG parameters on normal rhythm and arrhythmia
| Variable | Normal rhythm | p value | New‐onset arrhythmia | p value | Existing arrhythmia | p value | |||
|---|---|---|---|---|---|---|---|---|---|
| Admission | Discharge | Admission | Discharge | Admission | Discharge | ||||
| Heart Rate (bpm) | 90 ± 19.7 | 83 ± 17.3 | <.001 | 84 ± 14.02 | 71 ± 28.09 | .080 | 100 ± 31.9 | 88 ± 26.1 | .072 |
| QRS Duration (msec) | 87.5 ± 18.1 | 88.1 ± 19.4 | .583 | 86.3 ± 16.6 | 93.5 ± 23.6 | .041 | 95 ± 20.2 | 99.7 ± 25.7 | .181 |
| QT interval (msec) | 352.3 ± 46.8 | 368.7 ± 56.9 | .001 | 375.5 ± 42.8 | 407.5 ± 70.7 | .155 | 357.7 ± 81.9 | 371.5 ± 64.9 | .372 |
| QTc interval (msec) | 426.3 ± 53.8 | 430.3 ± 52.3 | .324 | 441.4 ± 50.4 | 422.5 ± 65.9 | .318 | 452.9 ± 163.6 | 437 ± 72.2 | .608 |
| ST‐T changes (%) | 32.7 | 35.3 | .373 | 41.7 | 33.3 | .339 | 43.8 | 40.6 | .662 |
The in‐hospital and discharge/last recorded heart rate (HR) were significantly higher in patients who required ICU or died (Table 4). The in‐hospital and discharge/last ECG HR of >85 bpm had an increased risk of death (OR = 2.69, p = .019 and OR = 2.47, p = .035, respectively) (Table 5).
TABLE 4.
The ECG parameters and clinical outcomes
| Survive (n = 169) | Death (n = 31) | p | Non‐ICU (132) | ICU (n = 67) | p | |
|---|---|---|---|---|---|---|
| HR 1 | 90.2 ± 22.4 | 96.8 ± 19.6 | .128 | 91.4 ± 22.6 | 91.2 ± 21.3 | .958 |
| HR 2 | 79.9 ± 17.2 | 88.2 ± 16.3 | .028 | 79.3 ± 17.0 | 84.9 ± 17.1 | .059 |
| HR 3 | 80.4 ± 16.2 | 97.5 ± 30.3 | .001 | 80.9 ± 17.0 | 86.9 ± 24.4 | .046 |
| QRS Dur 1 | 88.9 ± 18.8 | 87.5 ± 16.7 | .709 | 88.8 ± 19.2 | 88.5 ± 17.3 | .89 |
| QRS Dur 2 | 90.1 ± 20.7 | 89.5 ± 18 | .897 | 91.7 ± 22 | 89 ± 16.1 | .175 |
| QRS Dur 3 | 90.2 ± 21.4 | 90.1 ± 19.9 | .943 | 91.2 ± 22.3 | 88.8 ± 18.6 | .446 |
| QT 1 | 356.8 ± 56.1 | 343.582 ± 36.8 | .207 | 359.3 ± 58.1 | 345.6 ± 43.3 | .09 |
| QT 2 | 379.2 ± 57.3 | 364.5 ± 41.6 | .217 | 383.4 ± 59.2 | 364.8 ± 44.1 | .051 |
| QT 3 | 373.8 ± 59.4 | 358.3 ± 59 | .182 | 378.8 ± 62.5 | 357.7 ± 50.7 | .017 |
| QTc 1 | 432.8 ± 86.8 | 423.9 ± 44.3 | .576 | 437.1 ± 92.4 | 420.7 ± 54.4 | .181 |
| QTc 2 | 433.0 ± 51.4 | 432.0 ± 58.5 | .932 | 436.7 ± 53.7 | 425.6 ± 50.3 | .223 |
| QTc 3 | 429.5 ± 54.2 | 439 ± 67.9 | .389 | 434.8 ± 55.4 | 423.4 ± 58.6 | .18 |
Note: 1 = admission, 2 = in‐hospital, 3 = discharge or last ECG.
Abbreviations: HR, heart rate; QRS Dur, QRS duration.
TABLE 5.
Logistic regression test of heart rate for the outcomes
| HR cutoff | HR2 | HR3 | ||||||
|---|---|---|---|---|---|---|---|---|
| Deathn (%) | Surviven (%) | p | OR | Deathn (%) | Surviven (%) | p | OR | |
| ≥ 85 | 16 (51.6) | 48 (28.4) | .013 | 2.69 | 19 (61.3) | 66 (39.1) | .024 | 2.47 |
| < 85 | 15 (48.4) | 121 (71.6) | 12 (38.7) | 103 (60.9) | ||||
| Total | 31 (100) | 169 (100) | 31 (100) | 169 (100) | ||||
Abbreviations: HR2, in‐hospital heart rate; HR3, discharge/last ECG heart rate; OR, odds ratio.
3.4. Arrhythmia outcomes
In patients with sinus rhythm, 20% required a ventilator, 34.8% required ICU care, and 14.7% died during an average of 18 ± 11 days length of stay. Neither existing nor new‐onset arrhythmias changed outcomes in terms of mechanical ventilation requirement, ICU stay, hospital length of stay, and mortality (Table 6).
TABLE 6.
Association of arrhythmia types with clinical outcomes
| Rhythm at admission | Ventilator requirement | p value | ICU admission | p value | Death | p value |
|---|---|---|---|---|---|---|
| Sinus rhythm | Ref | Ref | Ref | |||
| Atrial fibrillation | 4 (19%) | 1.00 | 6 (28.6%) | .85 | 4 (19%) | .53 |
| Atrial flutter | 0 (0%) | 1.00 | 2 (100%) | .12 | 0 (0%) | 1.00 |
| Junctional rhythm | 0 (0%) | 1.00 | 0 (0%) | 1.00 | 0 (0%) | 1.00 |
| Pacing rhythm | 1 (100%) | .21 | 1 (100%) | .34 | 1 (100%) | .15 |
| AV block | 1 (25%) | 1.00 | 1 (25%) | 1.00 | 1 (25%) | .48 |
Atrial fibrillation was not associated with the need for a ventilator, ICU hospitalization, and death. Other documented arrhythmias were not influenced the clinical outcomes as well (Supporting Information Table S1).
3.5. Inflammation markers
In 60 subjects, who had complete laboratory data, we analyzed the relationship of inflammatory markers to the changes in ECG parameters. The admission CRP level showed a significant and moderate correlation with an increase in QRS duration (r = .35, p = .03) and QTc intervals (r = .36, p = .03) at discharge (Table 7). The admission CRP level did not differ between normal rhythm and arrhythmia subjects (33.2 ± 41.4 vs. 28.9 ± 38.1, p = .759, respectively). In addition, the ESR is moderately correlated with discharge QT interval (r = .36, p = .03). However, there is no significant association between inflammation markers and AF in our subset.
TABLE 7.
Pearson correlation between inflammatory markers and ECG parameters (n = 60)
| Inflammatory markers | QRS duration | QT interval | QTc interval | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Admission | Discharge | Admission | Discharge | Admission | Discharge | |||||||
| r | p value | r | p value | r | p value | r | p value | r | p value | r | p value | |
| ESR | .07 | .67 | .08 | .62 | −.13 | .41 | .34 | .03 | −.16 | .29 | .20 | .21 |
| WBC | .06 | .70 | −.14 | .36 | .06 | .72 | −.06 | .72 | .02 | .91 | −.54 | .73 |
| CRP | .22 | .19 | .35 | .03 | −.22 | .19 | .31 | .06 | −.11 | .52 | .36 | .03 |
4. DISCUSSION
Our study found that the prevalence of arrhythmia events in Covid‐19 patients was 22% in total. The arrhythmias occurred in 18% of patients during admission and remained found in 15% of patients at discharge. Previous work reported the incidence of cardiac arrhythmias in COVID‐19 patients was about 17%. 1 However, we found no difference in clinical outcome between patients who developed arrhythmias during hospitalization and patients who already had arrhythmias on admission compared with patients without arrhythmias. This happened because the Covid‐19 mortality in our series was high (15.5%), which was higher than in previous reports. 1 Patients with existing arrhythmias tend to have a higher mortality rate. Wang et al. 1 found more frequent ICU admission in arrhythmia patients than in patients with a normal rhythm.
We found that atrial fibrillation is the most common arrhythmia during Covid‐19 hospitalization among documented arrhythmia events. However, there is no correlation between atrial fibrillation and clinical outcomes of Covid‐19 patients in our series. As an emerging disease, data on clinical factors associated with Covid‐19 are evolving and conflicting. Bhatla et al. found a 25% incidence of atrial fibrillation, the most common arrhythmia in their cohort. Their data showed atrial fibrillation was associated with mortality but was not an independent factor in multivariate analysis. 2 In recent publications from developed countries, Paris et al. and Mountantonakis et al. reported that AF was found in 15%–17.6% of Covid‐19 cases and significantly had higher hospital mortality compared with patients without atrial fibrillation. 3 , 4 In‐hospital death occurred in 38.7% of the patients with a history for AF vs. 20.8% of those without. The association between AF and mortality remained significant after adjustment for variables associated with COVID‐19 severity, such as comorbidities, previous anticoagulant use, oxygen saturation, red blood cells count, hemoglobin, CRP, plasma troponin, and HF history. Of note, the mean age of patients in this study was 67.4 ± 13.2 years old and even older in AF patients (75.8 ± 10.9 and 73.1 ± 13.5 years old, respectively). 3 , 4 They did not adjust to the age, even though age is a prominent risk factor of AF. Our patients were younger (51.9 ± 13.7 years old) with lower AF incidence (10.5%). Furthermore, in our study, arrhythmia documentation was based on the 12‐lead ECG of patients treated in a regular ward and witnessed ECG monitoring during ICU treatment. This method potentially underestimates actual AF events. However, it generally shows the importance of routine ECG screening to avoid undetectable AF events.
Our study found significant ECG changes in Covid‐19 patients: a decrease in heart rate and an increase in the QT interval from hospital admission to hospital discharge. Fever and inflammation due to moderate to severe Covid‐19 infection may cause an increase in heart rate at admission, which gradually normalized at discharge.
A recent publication by Thakore et al. 5 found that the admission QTc interval in 828 Covid‐19 patients was prolonged compared with discharged patients (450.1 ± 30.2 ms vs. 423.4 ± 21.7 ms, p < .0001). Our study found that the QTc interval did not differ from admission to discharge. On the contrary, the discharge QT interval in our study was longer than its admission value. As the QTc was calculated using Bazett's formula, it depends mainly on changes in RR intervals or HR, affecting the QTc values. In addition, smaller sample size in our study might also influence the results. Furthermore, the QT interval is influenced by several factors. A population‐based survey, which was conducted on 11,209 participants over the age of 35 in China, found that older age, abdominal obesity, hypertension, diabetes, hypokalemia, and any medicine used in the past 2 weeks were associated independently with increased risk for prolonged QTc interval (all p < .05 in the fully adjusted logistic regression model). 6 The younger subjects in our study population might cause a different pattern of QTc interval change.
Our study showed that in‐hospital HR of >85 bpm significantly increased the risk of death (OR = 2.47, p = .035). Patients with high HR throughout hospitalization might be associated with prolonged and severe inflammation. In the ICU setting, high HR has been associated with increased mortality. 7 In the general population, a meta‐analysis revealed that higher resting HR was independently associated with increased risks of all‐cause and cardiovascular mortality in the general population. This indicates that resting HR is a predictor of all‐cause and cardiovascular mortality. 8 In this study, an increase in the inflammatory marker CRP was significantly associated with lengthening of QRS duration and QTc intervals. Electrocardiographic changes are related to myocardial injury and higher inflammatory biomarkers in Covid‐19. 9 Inflammation has also been recognized as a pivotal factor in QT interval prolongation. Several studies showed that persistent high‐grade systemic inflammation of rheumatoid arthritis was associated with QTc prolongation 10 , 11 , 12 , 13 , 14 , 15 and increased arrhythmias incidence. 16 , 17 A meta‐analysis of population‐based studies showed the risk of AF in rheumatoid arthritis patients was significantly increased. 18 Earlier reports of QT interval prolongation in Covid‐19 patients were associated with drugs that prolong QT intervals, such as hydroxychloroquine or chloroquine and azithromycin. 19 , 20 , 21 This should encourage clinicians to always pay attention to the side effects of medications that can prolong QT intervals and not underestimate the inflammatory influence on changes in QT intervals and arrhythmia events.
4.1. Limitation
This study has some limitations, such as different hospital discharge times resulting in different discharge ECG recording times. The changes in ECG parameters associated with inflammation might differ regarding recovery time. In addition, we only checked limited ECG parameters. Further studies in this younger age group by adding other ECG parameters such as QTd and QRS diminution 22 may describe changes in the ECG pattern more completely.
5. CONCLUSION
The incidence of arrhythmias in Covid‐19 patients at Covid‐19 referral hospitals in Indonesia is 22%, consisting of 16% at admission and 15% at discharge. Atrial fibrillation is the most common arrhythmia in Covid‐19 patients. Prolongation of QRS duration from admission to discharge was related to the occurrence of new‐onset arrhythmia. The in‐hospital HR of 85 bpm or higher increases the risk of death.
CONFLICT OF INTEREST
The authors declared that they have NO affiliation with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
Supporting information
Table S1
ACKNOWLEDGEMENT
The author would like to thank Zhara Juliane and Salsabila Maulaa Putri for their great contribution to collecting, cleaning, and analyzing data. This study is supported by the National Cardiovascular Center Harapan Kita research grant.
Yuniadi Y, Yugo D, Fajri M, Tejo BA, Widowati DR, Hanafy DA, ECG characteristics of COVID‐19 patient with arrhythmias: Referral hospitals data from Indonesia. J Arrhythmia. 2022;38:432–438. 10.1002/joa3.12718
REFERENCES
- 1. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhatla A, Mayer MM, Adusumalli S, Hyman MC, Oh E, Tierney A, et al. COVID‐19 and cardiac arrhythmias. Heart Rhythm. 2020;17:1439–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mountantonakis SE, Saleh M, Fishbein J, Gandomi A, Lesser M, Chelico J, et al. Atrial fibrillation is an independent predictor for in‐hospital mortality in patients admitted with SARS‐CoV‐2 infection. Heart Rhythm. 2021;18:501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Paris S, Inciardi RM, Lombardi CM, Tomasoni D, Ameri P, Carubelli V, et al. Implications of atrial fibrillation on the clinical course and outcomes of hospitalized COVID‐19 patients: results of the cardio‐COVID‐Italy multicentre study. Europace. 2021. Oct 9;23(10):1603–11. 10.1093/europace/euab146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Thakore A, Nguyen J, Pollack S, Chi B, Knight D, Mehrotra B, et al. Electrocardiographic manifestations of COVID‐19: effect on cardiac activation and repolarization. EClinicalMedicine. 2021;39:101057. 10.1016/j.eclinm.2021.101057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ma Q, Li Z, Guo X, Guo L, Yu S, Yang H, et al. Prevalence and risk factors of prolonged corrected QT interval in general Chinese population. BMC Cardiovasc Disord. 2019;19:276. 10.1186/s12872-019-1244-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kara D, Akinci SB, Babaoglu G, Aypar U. Increased heart rate on first day in intensive care unit is associated with increased mortality. Pak J Med Sci. 2016;32:1402–7. 10.12669/pjms.326.11507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang D, Shen X, Qi X. Resting heart rate and all‐cause and cardiovascular mortality in the general population: a meta‐analysis. CMAJ. 2016;188:E53–63. 10.1503/cmaj.150535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, et al. Characterization of myocardial injury in patients with COVID‐19. J Am Coll Cardiol. 2020;76:2043–55. 10.1016/j.jacc.2020.08.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lazzerini PE, Acampa M, Capecchi PL, Hammoud M, Maffei S, Bisogno S, et al. Association between high sensitivity C‐reactive protein, heart rate variability and corrected QT interval in patients with chronic inflammatory arthritis. Eur J Intern Med. 2013;24:368–74. [DOI] [PubMed] [Google Scholar]
- 11. Panoulas VF, Toms TE, Douglas KM, Sandoo A, Metsios GS, Stavropoulos‐Kalinoglou A, et al. Prolonged QTc interval predicts all‐cause mortality in arrhythmic risk in rheumatoid arthritis patients with rheumatoid arthritis: an association driven by high inflammatory burden. Rheumatology. 2014;53:131–7. [DOI] [PubMed] [Google Scholar]
- 12. Chauhan K, Ackerman M, Crowson CS, Matteson EL, Gabriel SE. Population‐based study of QT interval prolongation in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2015;33:84–9. [PMC free article] [PubMed] [Google Scholar]
- 13. Adlan AM, Panoulas VF, Smith JP, Fisher JP, Kitas GD. Association between corrected QT interval and inflammatory cytokines in rheumatoid arthritis. J Rheumatol. 2015;42:421–8. [DOI] [PubMed] [Google Scholar]
- 14. Lazzerini PE, Acampa M, Capecchi PL, Fineschi I, Selvi E, Moscadelli V, et al. Antiarrhythmic potential of anti‐cytokine therapy in rheumatoid arthritis: tocilizumab reduces QTc interval by controlling systemic inflammation. Arthritis Care Res. 2015;67:332–9. [DOI] [PubMed] [Google Scholar]
- 15. Medenwald D, Kors JA, Loppnow H, Thiery J, Kluttig A, Nuding S, et al. Inflammation and prolonged QT time: results from the cardiovascular disease, living and ageing in Halle (CARLA) study. PLoS One. 2014;9:e95994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chiu HY, Chang WL, Huang WF, Wen YW, Tsai YW, Tsai TF. Increased risk of arrhythmia in patients with psoriatic disease: a nationwide population‐based matched cohort study. J Am Acad Dermatol. 2015;73:429–38. [DOI] [PubMed] [Google Scholar]
- 17. Hussein AA, Gottdiener JS, Bartz TM, Sotoodehnia N, DeFilippi C, See V, et al. Inflammation and sudden cardiac death in a community‐based population of older adults: the cardiovascular health study. Heart Rhythm. 2013;10:1425–32. [DOI] [PubMed] [Google Scholar]
- 18. Ungprasert P, Srivali N, Kittanamongkolchai W. Risk of incident atrial fibrillation in patients with rheumatoid arthritis: a systematic review and meta‐analysis. Int J Rheum Dis. 2015;20:434–41. 10.1111/1756-185X.12820 [DOI] [PubMed] [Google Scholar]
- 19. Sridhar AR, Chatterjee NA, Saour B, Nguyen D, Starnes EA, Johnston C, et al. QT interval and arrhythmic safety of hydroxychloroquine monotherapy in coronavirus disease 2019. Heart Rhythm. 2020;O2(1):167–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chorin E, Wadhwani L, Magnani S, Dai M, Shulman E, Nadeau‐Routhier C, et al. QT interval prolongation and torsade de pointes in patients with COVID‐19 treated with hydroxychloroquine/azithromycin. Heart Rhythm. 2020;17:1425–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jankelson L, Karam G, Becker ML, Chinitz LA, Tsai MC. QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID‐19: a systematic review. Heart Rhythm. 2020;17:1472–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lampert J, Miller M, Halperin JL, Oates C, Giustino G, Nelson K, et al. Prognostic value of electrocardiographic QRS diminution in patients hospitalized with COVID‐19 or influenza. Am J Cardiol. 2021;159:129–37. 10.1016/j.amjcard.2021.07.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


