Short abstract
We present the case of a 68‐year‐old man with a cardiac resynchronization therapy‐defibrillator Medtronic device implanted 3 years ago, admitted to our hospital due to a wide complex tachycardia with unexpected pacing spikes inside QRS complexes. Although that could be easily attributed to ventricular undersensing, more complicated mechanisms are involved, including the origin of the tachycardia, the parameters of the device, and the position of the device and the leads.
Keywords: defibrillator function, paradoxical pacing, resynchronization therapy, wide complex tachycardia
One of the most common causes of unexpected pacing spikes inside QRS complexes is ventricular undersensing. Sometimes, more complicated mechanisms occur that can be elucidated by the knowledge of tachycardia and bradycardia parameters of the device, the position of the device and leads, and the morphologic characteristics of the tachycardia. We present an interesting case of paradoxical pacing spikes during a wide complex tachycardia.
A 68‐year‐old man presented with palpitation, shortness of breath, and progressively worsening dyspnea. He had a past medical history of coronary artery bypass grafting surgery 25 years ago, peripheral artery disease with stent implantation in the left popliteal artery 2 years ago, psoriatic arthritis, and diabetes mellitus type I. A cardiac resynchronization therapy‐defibrillator (CRT‐D) was implanted 3 years ago as secondary prevention due to sustained monomorphic ventricular tachycardia in a 24‐h Holter. Baseline electrocardiogram (ECG) showed sinus rhythm, PR interval 220 ms, and QRS 155 ms with a left bundle branch block morphology. Left ventricular function was severely impaired with an estimated ejection fraction of 25%–30%.
On arrival, he was hemodynamically stable with a blood pressure of 90/70 mm Hg and a heart rate of 115 beats/min. The ECG revealed a wide complex tachycardia (WCT) of 115 beats/min with a QRS duration of 165 msec. The tachycardia was self‐terminated with the restoration of sinus rhythm and biventricular (BiV) pacing at 65 beats/min with a QRS interval of 160 ms. What kind of WCT is this? (Figure 1).
FIGURE 1.

The 12‐lead electrocardiogram of the patient shows a wide complex tachycardia at the rate of 115 bpm. Leads I, II, and III are in zoom. A small deflection—the P wave—is seen regularly before some QRS and is marked with red vertical arrows
The diagnostic dilemma that a regular, monomorphic wide QRS complex tachycardia poses, is very important not only for acute arrhythmia management but also for further workup and prognosis. ECG remains the cornerstone of WCT differential diagnosis and many algorithms have been developed, based on a few simple principles. According to Brugada criteria (Step 3) and Vereckei algorithm (Step 1), the presence of AV dissociation, which is obvious in our patient's ECG, indicates ventricular tachycardia (VT). 1 , 2 In our ECG, the new algorithm's criteria for differential diagnosis of wide QRS complex tachycardia based only on aVR lead is also met, as the width of the initial r wave is >40 ms. 3 Superior axis, left bundle branch block morphology in V1, and QS in V4 suggest an exit site at the inferoapical segment of the left ventricle. 4 Is there any correlation between the visible spikes and the P waves? (Figure 2).
FIGURE 2.
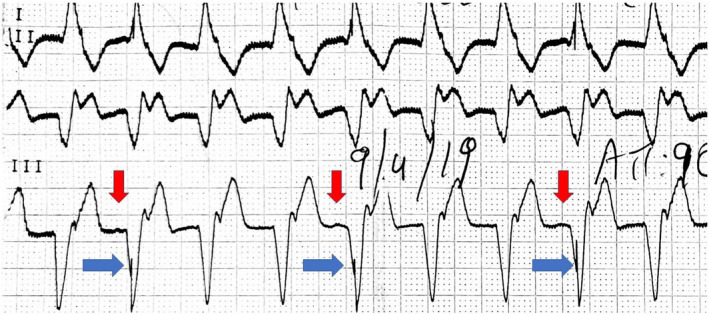
Leads I, II, and III during the wide complex tachycardia. It is apparent that the presence of a P wave is related to the pacing spike inscribed in the QRS. Red vertical arrows refer to the P waves and blue horizontal to the pacing spikes, respectively
It is known that a VT detected by an implantable cardioverter‐defibrillator or a CRT‐D can be classified into three or more zones including the monitor zone. Each zone has a separate therapeutic protocol. 5 In this patient, the slower zone had been set as a monitor zone at the nominal rate of 133 bpm. The tachycardia cycle length is very slow measured at 520 ms, which corresponds to 115 bpm. As a result, tachycardia remains undetected as its cycle length stands below the monitor zone and at the same time every P wave can still be tracked due to the fact that heart rate was also below the upper rate limit. Therefore, atrial sensed (As)activity triggers BiV pacing at the end of the sensed AV interval. P waves are more visible in III limb lead and the P–P intervals (red vertical arrows) are regular.
Of note, the sensed AV interval during tachycardia (130 ms) is shorter than the sensed AV delay during sinus rhythm (180 ms). This can be explained by the rate‐adaptive sensed AV interval of Medtronic devices, which is desirable at higher rates to avoid symptomatic 2:1 block during exercise. A short AV interval is also desirable at higher rates to promote consistent BiV pacing. Further studies are necessary to determine the clinical impact of these rate‐adaptive algorithms. But why ventricular sensed events do not inhibit ventricular spikes? (Figure 3).
FIGURE 3.
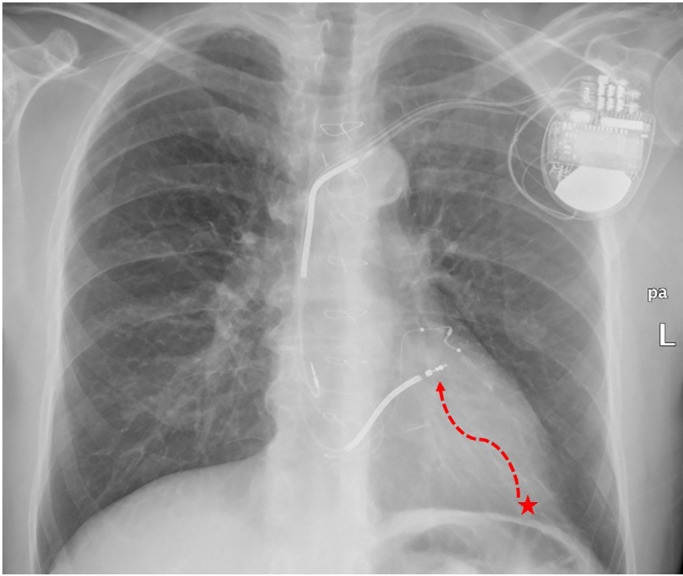
Chest X‐ray showing the position of the defibrillator lead at a high septal position far away from the exit site of the tachycardia (red asterisk). A red asterisk illustrates the exit of the ventricular tachycardia circuit on the cardiac silhouette. The dotted red line refers to the distance the electrical impulse covers from the exit site till being sensed by the tip of the defibrillator lead. This propagation time is prolonged and in the meanwhile sensed AV interval has expired. As a result, ventricular pacing ensues despite QRS onset
So far, it is explained why the dissociated P waves are tracked by the device, as the slow ventricular rate is below the upper tracking rate. Normally, we would expect that the intrinsic ventricular activation would inhibit ventricular pacing after each atrial sensed event. However, in our case, pacing spikes are observed after the onset of the QRS. This could be explained by the relative distance of the tachycardia exit to the defibrillator lead tip. It is known that the exit site of ventricular tachycardia is reflected by the QRS onset. As mentioned before, the tachycardia exit seems to be at the inferoapical segment of the LV at a relative distance to the sensing tip of the RV lead. The time required for the electrical stimulus to cover this distance—between the exit site of the tachycardia (QRS onset) and the tip of the right ventricular lead—is quite long. As a result, the sensed AV interval has already expired leading to a ventricular spike inside the QRS of the tachycardia.
Briefly, the slow rate of the ventricular tachycardia below the upper tracking rate limit and the location of the ventricular sensing lead with regard to the exit site of the tachycardia can explain the periodical presence of fused paced beats during the VT. Checking the device parameters and the position of the leads at the chest X‐ray shed light on this unexpected appearance of pacing spikes.
CONFLICT OF INTEREST
The authors declare no conflict of interest in this article.
Leventopoulos G, Koufou E‐E, Koros R, Perperis A, Davlouros P. Paradoxical pacing spikes during a wide complex tachycardia in biventricular defibrillator. What is the mechanism? Is it undersensing due to troubleshooting? J Arrhythmia. 2022;38:462–464. 10.1002/joa3.12688
REFERENCES
- 1. Brugada P, Brugada J, Mont L, Smeets J, Andries EW. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991;83(5):1649–59. [DOI] [PubMed] [Google Scholar]
- 2. Vereckei A. Current algorithms for the diagnosis of wide QRS complex tachycardias. Curr Cardiol Rev. 2014;10(3):262–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vereckei A, Duray G, Szénási G, Altemose GT, Miller JM. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. 2007;28(5):589–600. [DOI] [PubMed] [Google Scholar]
- 4. Josephson M, Horowitz L, Waxman H, et al. Sustained ventricular tachycardia: role of the 12‐lead electrocardiogram in localizing site of origin. Circulation. 1981;64(2):257–72. [DOI] [PubMed] [Google Scholar]
- 5. Mansour F, Khairy P. 568 ICD monitoring zones: intricacies, pitfalls, and programming. J Cardiovasc Electrophysiol. 2008;19(5):568–74. [DOI] [PubMed] [Google Scholar]


