Abstract
Background
Outpatient endocrinology care delivered by telehealth is likely to remain common after the pandemic. There are few data to guide endocrinologists’ judgments of clinical appropriateness (safety and effectiveness) for telehealth by synchronous video. We examined how, in the absence of guidelines, endocrinologists determine clinical appropriateness for telehealth, and we identified their strategies to navigate barriers to safe and effective use.
Methods
We conducted qualitative, semi-structuredinterviews with 26 purposively selected US endocrinologists. We used a directed content analysis to characterize participant perceptions of which patients and situations were clinically appropriate for telehealth and to identify adaptations they made to accommodate telehealth visits.
Results
Endocrinologists’ perspectives about appropriateness for telehealth were influenced by clinical considerations, nonclinical patient factors, and the type and timing of the visit. These factors were weighed differently across individual participants according to their risk tolerance, values related to the physical examination and patient relationships, and impressions of patient capabilities and preferences. Some participants made practice adaptations that increased their comfort offering telehealth to a wider swath of patients.
Conclusions
Endocrinologists’ judgments about clinical appropriateness of telehealth for different patient situations varied widely across participants. The risk of such divergent approaches to determining appropriateness is unintended and clinically unwarranted variation in use of telehealth, compromising quality of care. Expert consensus is needed to guide endocrinologists now, along with studies to anchor future evidence-based guidelines for determining clinical appropriateness of telehealth in endocrinology.
Keywords: telehealth, telemedicine, virtual care, endocrinology
Use of telehealth for outpatient endocrinology care skyrocketed early in the coronavirus disease 2019 (COVID-19) pandemic [1, 2]. Telehealth enabled continued access to health care while avoiding the risk of infection from in-person visits. Simultaneously, health care systems developed information technology infrastructures and clinical policies, endocrinologists made workflow adjustments and learned how to use the technology, and patients became more familiar with and now expect telehealth as a continued option for care [3]. In this paper, we focus on a specific form of telehealth, which is synchronous patient-clinician video for outpatient care. During the pandemic, payers largely covered these visits [4-6], and there is political momentum to extend telehealth benefits even after the public health emergency ends [7]. Subsequently, the level of telehealth use in endocrinology is likely to remain much higher than prepandemic levels. A pressing question, then, is how to ensure endocrinology patients are offered telehealth in a manner that enables equitable access to specialist expertise, aligns with their values and preferences for how their care is delivered, and provides safe and effective clinical care [8].
Endocrinologists are central players in the achievement of this goal because they routinely assess the safety and efficacy (i.e., clinical appropriateness) of telehealth. In the absence of evidence-based guidelines, there is scant research on how endocrinologists weigh clinical appropriateness of telehealth for individual patients. This knowledge gap makes it difficult to understand the ways in which endocrinologists’ judgments may affect overall quality of telehealth care. The goal of this study was to understand how endocrinologists evaluate which patient situations are clinically appropriate for telehealth and the ways that they overcome barriers to appropriate telehealth care.
Methods
Study Design
We conducted qualitative interviews with 26 endocrinologists ranging from 1 to 7 per state, over 9 states. Our team included a medical anthropologist (K.S.), a qualitative health services researcher (R.B.), and 2 endocrinologists (D.W., V.V.), 1 of whom is a health services researcher (V.V.). Our methods were consistent with the COREQ framework, which details specific components of study design that should be reported in qualitative research [9]. The VA Bedford Healthcare System institutional review board approved the study.
Participants
We sought a purposive sample of US-based endocrinologists to maximize variation in geographic location, years in practice, and practice setting (e.g., academic, private, public clinics). As a qualitative study, we sought a wide range of perspectives and experiences. To develop the sample, we first interviewed 10 endocrinologists known at arm’s length to study team members. We then asked each participant to identify additional endocrinologists who might be recruited, and we contacted those who would contribute to our goal of variation in experience. We continued recruitment and interviewing until we reached thematic saturation, which is the point at which no new themes are being identified in the data [10, 11].
Data Collection
A 2-person team (K.S., D.W.) conducted semi-structured interviews over a secure video platform from January through March 2021 and recorded the audio portion. All participants were using telehealth visits in addition to in-person visits when the interviews were conducted. K.S. led the interviews; D.W. took detailed notes that were later checked against the audio. Each interview was 30 to 45 minutes long and we queried participants about what factors they considered in determining which outpatient situations were safe and effective (clinically appropriate) for telehealth and in which situations telehealth worked best. We also obtained information about clinician demographics including what proportions of participants’ weekly visits used telehealth (Table 1). Participants provided verbal consent before the interview.
Table 1.
Participant characteristics (N = 26)
| Characteristics | N (%) |
|---|---|
| Female | 16 (62) |
| Clinical settinga | |
| Academic | 12 (46) |
| Public | 7 (27) |
| Private | 8 (30) |
| Rural-urban settinga | |
| Rural | 7 (27) |
| Suburban | 8 (30) |
| Urban | 12 (46) |
| Proportion of weekly visits using telehealth | |
| 0%-25% | 3 (12) |
| 26%-50% | 11 (42) |
| 51%-75% | 6 (23) |
| 76%-100% | 5 (19) |
| Unreported | 1 (4) |
| US geographic region | |
| Northeast | 12 (46) |
| Midwest | 4 (15) |
| West | 3 (12) |
| Southwest | 5 (19) |
| Southeast | 2 (8) |
| Years in practice, y | |
| <1-4 | 3 (12) |
| 5-14 | 15 (58) |
| 15-24 | 5 (19) |
| >25 | 3 (12) |
a Clinicians may work in more than 1 setting.
Data Analysis
We conducted a directed content analysis to understand the factors endocrinologists weighed in determining which patient situations are clinically appropriate for telehealth. Using a rapid qualitative analysis approach, 2 team members (K.S., D.W.) individually reviewed interview notes and audio-recordings and summarized information within a priori categories across interviews [12]. A priori categories relevant to our study were derived from the clinical component of the CHEATS framework for the evaluation of information communication technologies, including quality of care, changes in work practices, and appropriateness of referral [13]. We met regularly as a full team to build consensus and discuss factors that did not fall into the a priori categories. We remained open to refining, renaming, and adding emergent categories drawn from the data about the factors endocrinologists considered in determining appropriateness for telehealth. As is standard in qualitative data analysis, the content within each category was iteratively examined for internal consistency and differentiation from the other categories by each team member individually and in group discussion, allowing us to reach consensus on the final categories and their content [14-16]. We then synthesized the data within categories, using constant comparison methods to identify and understand the breadth of factors influencing endocrinologists’ evaluation of appropriateness. To minimize bias in data interpretation related to each member’s professional background, we involved all team members in weekly data analysis meetings.
Results
We interviewed 26 endocrinologists (Table 1). Many participants had specific areas of interest or focus: prediabetes and gestational diabetes care; telehealth/telemedicine access and administration; chronic disease and diabetes management; clinical research; thyroid conditions (including cancer); geriatrics; and pediatrics. We did not collect data on which telehealth platforms participants used, but many mentioned that suboptimal telehealth platforms deterred them from using the technology. Some participants, especially those in rural areas or those who serve as sole providers in large coverage areas, reported using telehealth before the COVID-19 pandemic. All reported an uptick in telehealth usage after the COVID-19 pandemic began.
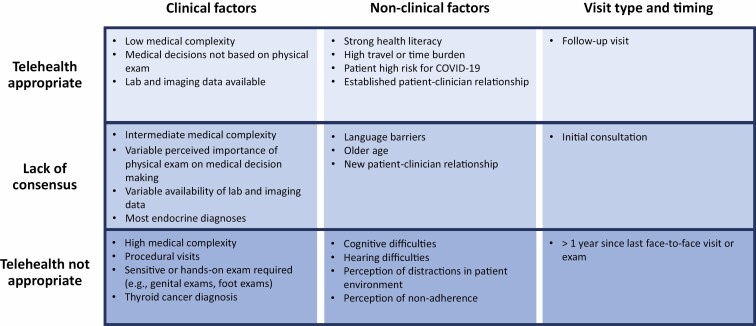
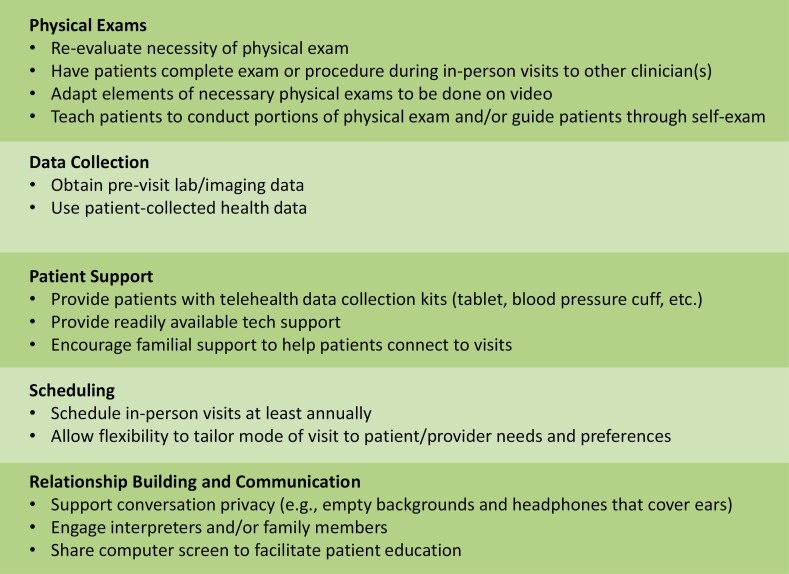
Participants expressed that endocrinology as a field is well-suited to telehealth because clinical decisions can often be made through history, medication review, lab/imaging results, review of patient-collected data (e.g., vital signs, blood glucose), and discussion with the patient, which can all be evaluated remotely. We identified 4 broad themes that described the factors participants weighed in making decisions about clinical appropriateness of specific situations for telehealth: clinical considerations, nonclinical patient factors, considerations related to the type and timing of the visit, and adaptations to overcome limitations of telehealth (Figs. 1 and 2).
Figure 1.
Endocrinologists’ perceptions of factors affecting clinical appropriateness of telehealth.
Figure 2.
Adaptations to increase perceived appropriateness of telehealth in endocrinology.
Clinical Factors
Conditions consistently described as amenable to telehealth were those that were low complexity or for which management relies little on the physical examination, such as osteoporosis, calcium disorders, and adrenal disorders, and where decisions are mostly based on vitals, laboratory data, and imaging data. Procedural visits such as thyroid ultrasound and fine-needle aspiration biopsy were identified as never appropriate for telehealth. Physical examinations that included sensitive components such as a genital examination, or where hands-on examination was required, such as a foot examination, were also considered inappropriate. Thyroid cancer was a specific condition commonly offered as not suitable for telehealth because of the frequent need for a physical examination and/or ultrasound: “The patients for whom a physical exam is really important [include] thyroid cancer patients—I’d really want to do a thorough neck exam on [them]” (Participant 5).
There were mixed opinions about suitability of most other diagnoses for telehealth. These judgments were based on individual participants’ degrees of concern about missing certain issues by telehealth, the perceived importance of the physical examination, the availability of imaging or laboratory data, and the perceived complexity of the individual patient’s diagnosis. Some participants were comfortable managing diabetes via telehealth if it was well-controlled, using whatever blood glucose data were available and accepting that a foot examination would be limited. However, others were not comfortable managing diabetes via telehealth without cloud-based glucose data or with a limited foot examination: “There are not many [diabetes] patients that I think are perfect for virtual care . . . We know we can miss things. We miss foot ulcers . . . skin integrity . . . hydration status . . . mobility—which in diabetes is really important for tracking” (Participant 8).
Some participants felt that hypothyroidism or hyperthyroidism would generally be appropriate for telehealth, whereas others preferred face-to-face visits to obtain vitals, palpate the thyroid, and ascertain subtle physical examination findings that may not be easily visible on video such as skin quality, reflexes, or tremors. One participant reported that they were comfortable with telehealth for thyroid dysfunction, knowing it did not preclude a subsequent face-to-face visit if the assessment over video indicated that was needed:
“So I think you just always have to have in your mind that…they’re much sicker than you think, you always have to have a back-up plan and be willing to say ‘Hey, you know what? I’m sorry, this visit is not standard of care for your sickness level. We need to get you either into us or into someone near you’” (Participant 3).
Nonclinical Patient Factors
There was agreement across participants that patients with strong health literacy were better candidates for telehealth visits. Participants favored telehealth to support patients who lived at a distance or were unable to travel because of physical limitations or lack of transport. One participant, who was the sole endocrinology provider for many rural areas of her state, described the struggle her patients faced getting to her for appointments:
“Because so many people have to travel it’s like a 3-day trip…to come see me for 45 minutes. For some people…it’s like a 4- or 5-day visit because planes only fly certain days of the week so they have to wait two days until they can fly home or take a ferry and a plane and drive…which makes it really hard. Allowing people to do video [visits] is super valuable” (Participant 7).
Many participants also acknowledged that the benefits of telehealth might be significant for patients who would otherwise need to take time off from work, juggle caregiving duties to travel for a face-to-face visit, or put themselves at risk for COVID-19 exposure.
There was also agreement on other characteristics that made telehealth impracticable, such as cognitive and hearing difficulties, or patients’ inability to attend telehealth visits in an undistracting, private, and quiet space. Many participants felt the additional effort of a face-to-face visit strengthened patients’ perceptions of the importance of the treatment plan and thus encouraged otherwise nonadherent patients to participate more in care.
There was a lack of consensus about how language barriers and patients' older age influenced clinical appropriateness. Although language barriers led some participants to prefer face-to-face visits, others were satisfied using interpreters available over video. Some participants perceived older individuals to be poorly suited to telehealth appointments because of their assumed lack of experience and competence with technology. In contrast, several other participants asserted that, despite their initial assumptions, the generalization that older patients are unable to use telehealth had proven incorrect in their experience. One participant describes her frustration with others labeling elderly patients as unfit for telehealth:
“One of my biggest pet peeves…is when [a doctor] assumes because of [a patient’s] age that they can’t do telehealth…I think it’s a double standard for me not to fight for [older patients] and I can tell you that I have 92-year-old patients who can run circles around me with technology. I have an 83-year-old [patient] who teaches computer classes…I try not to use age as a limiting factor or barrier” (Participant 16).
Visit Type and Interval Between Visits
Participants weighed whether the visit was for a follow-up or initial consultation, as well as the interval between visits. There was general agreement that follow-up care was often appropriate for telehealth. One participant explained this in terms of having a preexisting relationship: “I’ve known this patient for the last three years and that made a huge difference because we knew each other, and we knew what to expect from a follow-up visit . . .” (Participant 21). Another explained it in terms of the likelihood of a change in clinical status: “In [endocrinology] you follow people longitudinally. They don’t change a tremendous amount. When you’re talking on the phone . . . there’s not an awful lot, other than a personal connection you’re missing [compared to in-person visits]” (Participant 17).
Opinions varied about initial consultations. Several participants felt strongly that consultations should occur in person: “For new patients, I do think you’re able to get . . . a whole view of the patient when you see them in person, and you’re not able to do that with telehealth” (Participant 1). Perceived benefits to a face-to-face consultation included the ability to conduct at least one physical examination, an opportunity to establish better rapport and stronger relationships, and reinforcement of the importance of the visit that could in turn encourage patients to take the condition more seriously. One participant described how face-to-face visits strengthen the patient-clinician relationship and communication, thus increasing the likelihood of developing an effective treatment plan:
“It was harder to transition new patients and consults [to telehealth] because those are people you’ve never met before…It’s a little bit harder to establish that connection. […] Just getting a sense of [type 2 diabetes patients] is important…because people need to buy into what their treatment plan is and agree to it. You can write all the prescriptions in the world, but if they’re not willing to take them or they have some fear they want to tell you but they don’t feel like telling a new person over the phone, usually that will come out in the office” (Participant 19).
Other participants felt less strongly about the need for face-to-face initial consultations, remarking that, in fact, the ability to see a patient in their home context over video helped understand them as a whole person and thus enriched the patient-clinician relationship.
Interval between visits also influenced perceived clinical appropriateness of a visit. Many participants voiced a general discomfort about not having seen some patients for more than a year because of the COVID-19 pandemic. One said, “I would want to see [people with diabetes] at least once a year for a [thorough] exam. The rest [of the visits] can be virtual” (Participant 15). The range of concerns included diminished relationships over long-term telehealth, missing new clinical issues, and medicolegal concerns.
Adapting Individual Practice for Telehealth
Many participants expressed frustration at the logistical challenges of telehealth, which reduced the number of patients for whom they thought telehealth would be safe and effective. However, not all were stymied by logistical challenges. In several instances, participants had modified their practice to enable clinically appropriate care over telehealth for patients they would otherwise want to see face-to-face (Fig. 2).
Some had reconsidered what elements of a physical examination were truly necessary at a given visit, noting that if relevant data could be obtained via other means than hands-on examination, then a face-to-face visit may not be needed. One participant pointed out how home equipment could be used by patients for data collection, which could be shared during or uploaded before the visit: “One of my questions . . . is ‘Do they have a weigh scale or blood pressure cuff at home?’ Because that makes it very easy . . . a lot of people don’t have weigh scales at home, which makes it very difficult” (Participant 19). Participants said they were more likely to offer telehealth visits to patients who could collect and share their vitals and health readings, such as glucose values, at home. Another participant described how the clinic provided patient support and technology support for telehealth by equipping patients with blood pressure cuffs, Bluetooth equipment to upload data, tablets, and other hardware to improve access to telehealth and ensure endocrinologists had patient data to guide care decisions. For older patients who struggled to use the technology or hear adequately, some participants mentioned recruiting family members to assist with the telehealth visit.
Even if a hands-on physical examination or procedure was needed, participants mentioned they could work around this by having the patient see another clinician for those elements after the telehealth visit. Another participant offered an example of using imaging data along with patient maneuvers over video: “If I have bone density data, I can get them to stand up, if they’re stable. I can see the shape of their spine. I can get a feeling for how well they’re moving” (Participant 11). Patient self-examination was also described:
“I show [patients]…how to feel their neck. And I ask them, “Do you feel anything that’s…different on one side than another? Do you feel a lump… something that feels like a marble…[or] that feels like a rubber eraser? … I make sure they go all along their collar bones and the front of their neck and sternal notch. [Two of my patients] found metastatic disease in their neck…I was totally impressed that people were finding their own stuff” (Participant 14).
Scheduling annual face-to-face visits relieved the anxiety for many participants about long-term telehealth. These visits were considered sufficiently frequent for maintaining the patient-clinician relationship, for many required physical examination components, and to avoid any liability incurred by the risks of telehealth-only care. In fact, some participants expressed that they would offer telehealth to patients with any medical condition provided there was an annual face-to-face visit: “If it stretched for a whole year without having [patients] in the office, that would start to be not good medicine for me—especially for [diabetes] or [a] thyroid patient, because I can’t feel the thyroid. With these two, I feel vulnerable that something could go wrong because of just visual communication” (Participant 11).
Several adaptations were mentioned to improve relationship-building and overcome challenges to patient-clinician communication. To address privacy concerns and support more frank conversations, some participants wore over-the-ear headphones to clearly convey that no one else could hear and maintained an empty or virtual background on video calls. Many participants mentioned the ease of involving interpreters and family for video calls. To share information that could not be passed between hands or for patients who were hard of hearing, some participants drew pictures and held them up to the camera, or shared computer screens if the platform allowed.
Discussion
This study examined how endocrinologists evaluate clinical appropriateness (safety and efficacy) of telehealth for outpatient care. Participants weighed a combination of clinical considerations, nonclinical patient factors, and the type and timing of the visit in determining whether a telehealth visit would be clinically appropriate. Many factors were consistently perceived as supporting appropriateness of telehealth: low medical complexity, lack of need for a physical examination, excessive time or travel burden for a face-to-face visit, established patient-clinician relationship, strong health literacy, and follow-up care. Factors generally perceived as barriers to appropriate telehealth care included a requirement for hands-on care, cognitive and hearing difficulties, distracted or nonadherent patients, and prolonged interval since the last face-to-face visit. There was a lack of consensus regarding several other factors and the degree to which they supported selection of telehealth or rendered it clinically inappropriate. In the absence of expert consensus or provisional guidance, judgments of appropriateness were colored by individual participants’ level of risk tolerance, experience with different demographic groups, perception of the value of hands-on physical examination and face-to-face relationship-building, and willingness and ability to adapt one’s expectations and practice to overcome challenges posed by the remote format. Accordingly, we found wide variation across participants in their judgments about clinically appropriateness of telehealth for many of the same situations in endocrinology. Some participants in our study made determinations of unacceptable safety and efficacy of telehealth based on concerns that other participants overcame with practice workarounds. Participants who used these adaptations were able to render more visits appropriate for telehealth, but such practices were not uniformly implemented.
Wide differences in how endocrinologists determine clinical appropriateness of telehealth, as observed in our study, are problematic because they could result in clinically unwarranted variation in access to telehealth. Studies of other health services demonstrate that variation in individual clinician practice patterns can explain a considerable portion of variation in service use [17-19], even when accounting for factors at the patient and organizational level. Often, clinician-level variation represents deviations of practice from evidence-based approaches; such deviations can in turn lead to disparities in access to care. In the case of endocrinology telehealth, there are not yet evidence-based approaches to judging clinical appropriateness because the evidence is still emerging. The combination of practice variation and a limited evidence base highlights the need for an expert consensus statement on clinically appropriate use of telehealth for endocrine care.
Consensus statements, representing the collective opinions of an expert panel on evolving areas of clinical care, can guide practice where there is both a lack of rigorous evidence and an opportunity to reduce uncertainty and improve quality of care. Findings from this study and others can help inform the opinions of experts in endocrinology clinical care, telehealth, and health services research by showing where there is existing consensus on appropriateness and worthy practice adaptations, and where further information is needed. Expert consensus can thus supply provisional guidance in the near term on the factors to consider in determining clinical appropriateness of telehealth in endocrinology.
There is also a pressing need for research that can inform evidence-based guidelines for clinically appropriate use of telehealth in endocrinology. Several studies suggest that endocrinology care via telehealth can improve glycemic control [20-23] and can achieve comparable glycemic control [24] and weight loss [25] compared with face-to-face care. However, for endocrine conditions other than diabetes, a question of whether clinical outcomes differ if care is delivered face-to-face vs telehealth remains. Studies also show that disparities in social determinants of health cause worsen clinical outcomes and negatively affect patient access to telehealth [26]. Thus, important research questions remain. What other patient characteristics drive any differences in care and differences in outcomes, and why? How often do patients with specific characteristics need to be seen face-to-face to ensure high-quality care? To what extent does a hands-on physical examination contribute to accurate diagnosis and treatment decisions for a given problem? Such questions will need to be examined for specific conditions, and account for differences in patient case mix.
Existing literature should be amplified among the endocrinology community and expanded to include other endocrine conditions beyond diabetes. Even more informative would be for studies to account for patients’ capacity for self-management and ability to navigate the health care system—both may be major factors in outcomes since telehealth-delivered care also means fewer opportunities to interface directly with others in the health system. Because clinical outcomes may take many years to measure, more proximal outcomes such as patients’ experience of patient-centered care or coordinated care can provide data that relate to quality of care. Evidence-based guidelines will build on expert consensus and are likely to reduce clinician-level variation in use of telehealth [27, 28].
Even when clinically appropriate, other contextual factors affect which patients end up with telehealth visits. Patient preference should be a driving factor among these, though telehealth laws and reimbursement constraints may override any patient or clinician wishes. Even if telehealth is demonstrated to be clinically equivalent or better than face-to-face care for certain situations, and patient preference and policy support telehealth, many clinicians and patients may prefer face-to-face communication and choose this route. However, careful assessments of clinical appropriateness provide an ethically sound vantage point from which to evaluate the role and impact of these other factors.
This study has limitations. Some participants we interviewed knew each other from training or as past/current colleagues because of our recruitment strategy. This approach may have introduced selection bias and raises concerns that we interviewed a group with a narrow range of perspectives. However, our data demonstrate that we were successful in eliciting a broad range of approaches to judging appropriateness that highlight the problem of significant variation in clinical judgments about use of telehealth. We interviewed 26 endocrinologists, and although almost half were from the Northeast, all geographic regions in the United States were represented by at least 2 participants. We did not have a sufficient number of participants in each demographic category to learn how this information may affect participants’ evaluations of telehealth's appropriateness, but we did reach thematic saturation within our sample. This strengthens our confidence that we captured the full range of opinions and experiences, as was our goal in this qualitative study.
Conclusions
Although the use of synchronous clinical telehealth for outpatient endocrinology care has proliferated, guidelines to inform decision-making about clinically appropriate telehealth use have lagged. In this context, endocrinologists in our study negotiated and weighed a complex mix of factors to determine appropriateness, often reaching different conclusions about similar situations. A few factors were generally agreed to support or argue against use of telehealth, but there was disagreement on many other factors and wide differences in how individuals adapted their practice to support safe and effective telehealth. Variation in how endocrinologists determine clinical appropriateness increases the risk of clinically unwarranted variation in access to telehealth. In the near term, a consensus statement is needed to reduce clinician uncertainty and improve quality of care. At the same time, research is needed to undergird evidence-based guidelines for use of telehealth in endocrinology.
Acknowledgments
The authors thank B. Graeme Fincke, MD, for his feedback on early drafts of this paper. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Glossary
Abbreviations
- COVID-19
coronavirus disease 2019
Contributor Information
Kailyn E Sitter, Email: Kailyn.Sitter@va.gov, Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA 01730, USA.
Denise H Wong, Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA 01730, USA; Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston University School of Medicine, Boston, MA 02118, USA.
Rendelle E Bolton, Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA 01730, USA; The Heller School for Social Policy and Management, Brandeis University, Waltham, MA 02453, USA.
Varsha G Vimalananda, Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA 01730, USA; Section of Endocrinology, Diabetes, Nutrition and Weight Management, Boston University School of Medicine, Boston, MA 02118, USA.
Funding
This work was funded by a Field Originated Project (FOP 20-190) from the Department of Veterans Affairs, Health Services Research and Development Service (V.V.).
Disclosures
The authors have nothing to disclose.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
References
- 1. Madduri S, Chowdhary PT, Reddy SS. Telehealth adoption among endocrinologists during the COVID-19 pandemic. Endocr Pract. 2020;26(8):846-856. Doi: 10.4158/ep-2020-0237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation in telemedicine use and outpatient care during the COVID-19 pandemic in the United States. Health Aff. 2021;40(2):349-358. Doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andrews E, Berghofer K, Long J, Prescott A, Caboral-Stevens M. Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. 2020;2:100008. Doi: 10.1016/j.ijnsa.2020.100008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Medicare & Medicaid Services. Medicare and medicaid programs; policy and regulatory revisions in response to the COVID-19 public health emergency. Fed Regist. 2020;85(66):19230-19292. [Google Scholar]
- 5. CMS News and Media Group. Medicare Telemedicine Health Care Provider Fact Sheet. CMS News and Media Group. Accessed January 11, 2021. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 6. AHIP. Health Insurance Providers Respond to Coronavirus (COVID-19). AHIP. Accessed January 18, 2021. https://www.ahip.org/health-insurance-providers-respond-to-coronavirus-covid-19/
- 7. Volk J, Palanker D, O’Brien M, Goe CL. States’ Actions to Expand Telemedicine Access During COVID-19 and Future Policy Considerations; 2021. Improving Health Care Quality. June 23. https://www.commonwealthfund.org/publications/issue-briefs/2021/jun/states-actions-expand-telemedicine-access-covid-19
- 8. Herzer KR, Pronovost PJ. Ensuring quality in the era of virtual care. JAMA. 2021;325(5):429-430. Doi: 10.1001/jama.2020.24955 [DOI] [PubMed] [Google Scholar]
- 9. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. Doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 10. Green J, Thorogood N.. Qualitative Methods for Health Research. Sage, Thousand Oaks, California; 2004. [Google Scholar]
- 11. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59-82. Doi: 10.1177/1525822x05279903 [DOI] [Google Scholar]
- 12. Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423-442. Doi: 10.1146/annurev-publhealth-040218-044215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shaw NT. “CHEATS”: a generic information communication technology (ICT) evaluation framework. Comput Biol Med. 2002;32:209-220. Doi: 10.1016/s0010-4825(02)00016-1 [DOI] [PubMed] [Google Scholar]
- 14. Creswell JW, Creswell JD.. Research Design. 5th ed. Sage Publications, Thousand Oaks, California; 2018. [Google Scholar]
- 15. Patton MQ. Qualitative Research and Evaluation Methods. Sage Publications, Thousand Oaks, California; 2002. [Google Scholar]
- 16. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277-1288. Doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 17. Smulowitz PB, O’Malley AJ, Zaborski L, McWilliams JM, Landon BE. Variation in emergency department admission rates among medicare patients: does the physician matter? Health Aff (Millwood). 2021;40(2):251-257. Doi: 10.1377/hlthaff.2020.00670 [DOI] [PubMed] [Google Scholar]
- 18. Chen CL, Lin GA, Bardach NS, et al. Preoperative medical testing in Medicare patients undergoing cataract surgery. N Engl J Med. 2015;372(16):1530-1538. Doi: 10.1056/NEJMsa1410846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Obermeyer Z, Powers BW, Makar M, Keating NL, Cutler DM. Physician characteristics strongly predict patient enrollment in hospice. Health Aff (Millwood). 2015;34(6):993-1000. Doi: 10.1377/hlthaff.2014.1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Crowley MJ, Endelman D, McAndrew AT. Practical telemedicine for veterans with persistently poor diabetes control: a randomized pilot trial. Telemed J E Health. 2016;22:376-384. Doi: 10.1089/tmj.2015.0145 [DOI] [PubMed] [Google Scholar]
- 21. Kobe EA, Lewinski AA, Jeffreys AS, et al. Implementation of an intensive telehealth intervention for rural patients with clinic-refractory diabetes. J Gen Intern Med. 2022. Doi: 10.1007/s11606-021-07281-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wu C, Wu ZX, Yang LF, et al. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine (Baltim). 2018;97(43):e12962. Doi: 10.1097/MD.0000000000012962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lu AD, Gunzburger E, Glorioso TJ, et al. Impact of longitudinal virtual primary care on diabetes quality of care. J Gen Intern Med. 2021;36(9):2585-2592. Doi: 10.1007/s11606-020-06547-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu W, Saxon DR, McNair B, Sanagorski R, Rasouli N. Endocrinology telehealth consultation improved glycemic control similar to face-to-face visits in veterans. J Diabetes Sci Technol. 2016;10(5):1079-1086. Doi: 10.1177/1932296816648343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shibuya K, Pantalone KM, Burguera B. Virtual shared medical appointments: a novel tool to treat obesity. Endocr Pract. 2018;24:1108-1109. Doi: 10.4158/1934-2403-24.12.1108 [DOI] [PubMed] [Google Scholar]
- 26. Eberly LA, Kallan MJ, Julien HM. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2031640. Doi: 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288(15):1909-1914. Doi: 10.1001/jama.288.15.1909 [DOI] [PubMed] [Google Scholar]
- 28. Lesho EP, Myers CP, Ott M, Winslow C, Brown JE. Do clinical practice guidelines improve processes or outcomes in primary care? Mil Med. 2005;170(3):243-246. Doi: 10.7205/milmed.170.3.243 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.