Abstract
Purpose
To assess visual results (including the Lapid-Kushlin defocus coefficient), and satisfaction, following the implantation of PanOptix® a trifocal intraocular lens.
Methods
Observational, retrospective cohort study. 130 eyes of 65 subjects with bilateral implantation were included. Binocular uncorrected visual acuities [distance (Binocular UDVA), intermediate (Binocular UIVA) and near (Binocular UNVA)] were measured. Also, the manifest refraction, binocular defocus curve and binocular contrast sensitivity were determined. The Lapid-Kushlin defocus coefficient, a new single numerical parameter based on the area under the curve of the defocus curve, was calculated. The validated Spanish CATQUEST-9SF satisfaction survey was applied.
Results
Postoperative visual acuity ranges were: binocular UDVA 0.18 to 0.0 LogMAR, binocular UIVA 0.30 to 0.0 LogMAR and Binocular UNVA 0.18 to 0.0 LogMAR. The levels of contrast sensitivity both in bright light conditions (with and without glare) and low light conditions with glare, remained within the limits of normality. Under scotopic conditions without glare values below normality were found at lower spatial frequencies. The binocular defocus curve showed a plateau without a clearly evident peak. The Lapid-Kushlin defocus coefficient was 0.199. Two patients (3.1%) needed glasses after the procedure for near and intermediate vision. No patient manifested great visual difficulties or was dissatisfied with the results.
Conclusions
The trifocal platform showed very good results in this series of patients. 96.9% of the patients achieved independence of the glasses and expressed a high degree of satisfaction. The Lapid-Kushlin defocus coefficient was better than those calculated from literature, for other multifocal intraocular lenses.
Keywords: Cataract surgery, Multifocal intraocular lens, Trifocal intraocular lens
Introduction
Cataract is a condition of high prevalence in humans older than sixty years of age, and since no preventive therapy is available, and life expectancy is increasing globally, cataract extraction is among the most common surgeries in the world, and will increase in frequency during the next years1,2. In addition, currently, due to higher patients' visual demands cataract surgeries are performed in less advanced cases, at younger ages, and phacoemulsification is also indicated with refractive purposes more frequently. More patients seek independence from glasses for distance and also for near vision, after the implantation of the intraocular lens, a need that has been fulfilled by bifocal intraocular lenses (IOLs) and, more recently, by trifocals. Bifocal platforms of IOLs have been in the market since the 1980s, and with the models marketed during the last decade have provided satisfactory visual acuity for distant and near distances but not for intermediate vision3, 4, 5. Trifocal IOLs of different models are set to solve this weakness, and satisfactory results have been reported with them6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18.
Acrysof PanOptix® (Alcon Inc., Fort Worth, Texas, USA) is a trifocal IOL model launched in recent years, whose design is aimed at improving intermediate vision tasks to increase patient satisfaction, by creating a third focal point at an intermediate distance (60 cm), although with an acceptable range of vision around this point (i.e. from 40–80 cm)6, 7, 8, 9, 10, 11, 12,15, 16, 17, 18. Because of its design, the Panoptix® theoretically is not dependent on pupillary size12.
The purpose of this work was to establish the binocular visual outcomes, including also the quality of vision (evaluated by contrast sensitivity, including the recently described Lapid-Kushlin defocus coefficient) and subjective satisfaction in adult individuals who underwent bilateral implantation of trifocal PanOptix® intraocular lens.
Materials and methods
This was a retrospective, observational study involving patients from an existing database, who underwent bilateral crystalline lens surgery and implantation of trifocal IOL, the AcrySof IQ PanOptix® IOL (TFNT00). The implantation of these lenses was performed after the extraction of cataract with phacoemulsification technique and they were calculated for emmetropia. The inclusion criteria for this database were: age ≥ 50 years, diagnosis of cataract, corneal astigmatism ≤ 0.75 D, bilateral implantation of Panoptix® trifocal lens, and minimum follow-up of 6 weeks. The criteria of exclusion were: glaucoma, age-related macular degeneration, diabetic retinopathy, maculopathies, amblyopia, vascular alterations of the retina, past history of corneal or intraocular surgery, epiretinal membranes, and complications during or after the phacoemulsification procedure.
The database contained patients from two institutions: Clínica Oftalmológica del Caribe COFCA (Barranquilla, Colombia) and Fundación Oftalmológica de Santander FOSCAL (Floridablanca, Colombia). The patients of this database underwent the same surgical technique: phacoemulsification through incision of 2.2–2.5 mm in the cornea, under topical anesthesia combined with intravenous sedation by five expert surgeons (VG, LJE, NIC, RDB, CAN).
The main outcomes of this investigation were binocular uncorrected distance visual acuity (Binocular UDVA) measured at 4 meters, binocular uncorrected intermediate visual acuity (Binocular UIVA) measured at 65 cm, binocular uncorrected near visual acuity (Binocular UNVA) measured at 40 cm. Other primary outcomes were: percentage of patients with binocular UDVA, UIVA and UNVA of 20/25 or better and the performance on the curve of defocus. This curve was created in the following way: once obtained the manifest refraction of the eyes (distance of the optotypes = 4 meters), the required distance correction was placed and then both eyes were defocused with different negative lenses, beginning with -4.00 D, in -0.50 D steps until the defocus was zero, and the binocular visual acuity was determined for each amount of negative defocus. Since in the real world there are not objects that generate convergent rays (other than optical lenses), positive defocus steps in these curves was considered to have a very complex interpretation and not a significant utility. On the other hand, it meant subjecting patients to a longer exam time, and consequently were not used. As explained by Gundersen and Potvin the corresponding viewing distances for each negative vergence magnitude evaluated during the defocus curve examination were adjusted accounting for the 4 meters chart distance13,19. Briefly, the principles of adjustment were as follows: since 4 meters charts were used, a patient corrected for this distance is not really being measured at infinity, and the vergence listed as “0” Diopters (D) on the graph was really of an amount of -0.25 D. So, the effective vergences from the defocus charts had to be adjusted in such magnitude. Therefore, for example, -1.00 D became -1.25 D (and the corresponding viewing distance was not calculated as 100 cm/-1.00 D but as 100 cm/-1.25 D, i.e. 80 cm). In the same way -1.50 D, became -1.75 D and its corresponding viewing distance changed from 66.7 cm to 57.1 cm 13,19.
As secondary outcomes were considered: the manifest refraction data, assisted by electronic auto refractometer (KR-800, Topcon Medical Systems, Tokyo, Japan) and subjective refinement by experienced optometrists. In addition, the results of the validated Spanish CATQUEST-9SF satisfaction survey that was applied to the patients 20,21. The ordinal raw data from the CATQUEST-9SF questionnaire were converted into a Rasch person score, with an interval level measurement called logit unit21,22. A logit is the natural log-odds of a respondent's successful completion of an item against failed completion. A negative logit score indicates that the level of capability is above average of the necessary degree of demand for the items 21,22.
In addition, the new Lapid-Kushlin defocus coefficient, which is a single numerical parameter based on a mathematical model in order to compare defocus curves of different multifocal IOLs considering the area under the curve in a given range of vision (defocus amount from plano to -3.50 D), was calculated (Lapid-Gortzak R, Kushlin Y, Lapid O. Area under the graph as a modality for comparing multifocal IOLs. Free Paper. Oral presentation at: XXXVI European Society of Cataract and Refractive Surgeons ESCRS Meeting; September 22-26th, 2018, Vienna, Austria).
A descriptive statistics evaluation of the several variables was performed determining measures of central tendency, position and dispersion fitting to the frequency distribution. The level of significance of the study was 5%.
Conforming to the Helsinki declaration, this protocol was reviewed and approved by the Research Ethics Committee of the Fundación Oftalmológica de Santander FOSCAL (Floridablanca, Colombia).
Results
In total 130 eyes of 65 patients with trifocal platform IOL (PanOptix®) implant in both eyes, were included. Average age was 67.2 ± 10.7 years (range 53 to 90 years). There were 30 men and 35 women. Follow-up time was 12.4 ± 4.6 months (range 1.5 to 25.7 months). Optical power selected to be implanted exhibited a mean of 22.01 ± 2.07 D (range 18.5 to 26 D). The final binocular visual acuity results are shown in Table 1. 41 patients showed binocular UDVA equal to 20/20 (63.1%). 59 of 65 patients (90.8%) achieved binocular UDVA of 20/25 or better. No patient had binocular UDVA lower than 20/30. 47 patients (72.3%) achieved 20/25 or better binocular UIVA measured at 65 cm. 49 patients (75.4%) achieved 20/25 or better binocular UNVA measured at 40 cm. Only one of the individuals presented binocular UIVA lower than 20/30. None of the patients presented binocular UNVA lower than 20/30.
Table 1.
Final binocular visual results.
| Mean± SD (LogMAR) | Mean (Snellen) | Range (LogMAR) | Range (Snellen) | |
|---|---|---|---|---|
| Binocular UDVA | 0.04 ± 0.06 | 20/22 | 0.18 to 0.0 | 20/30 to 20/20 |
| Binocular UIVA* | 0.07 ± 0.08 | 20/24 | 0.30 to 0.0 | 20/40 to 20/20 |
| Binocular UNVA† | 0.05 ± 0.08 | 20/22 | 0.18 to 0.0 | 20/30 to 20/20 |
SD: Standard deviation
UDVA: Uncorrected distance visual acuity
UIVA: Uncorrected intermediate visual acuity
UNVA: Uncorrected near visual acuity
At 65 cm
At 40 cm
The final postoperative refraction at the last follow up visit showed and spherical equivalent of -0.14 ± 0.33 D (range -1.13 to +1.25 D). Defocus equivalent (calculated as the numerical value of the spherical equivalent without regard to its sign, i.e. absolute value, plus half the numerical value of the refractive cylinder without regard to its sign, i.e. absolute value) was 0.39 ± 0.37 D (range 0 to 1.50 D). Cumulative percentages of eyes within a given postoperative spherical equivalent, refractive cylinder and defocus equivalent are shown in Table 2.
Table 2.
Final postoperative refraction.
| WITHIN (D) | CUMULATIVE NUMBER OF EYES (CUMULATIVE %) | |
|---|---|---|
| SPHERICAL EQUIVALENT | ± 0.25 | 91 (70 %) |
| ± 0.50 | 116 (89.2%) | |
| ± 0.75 | 127 (97.7%) | |
| ± 1.00 | 128 (98.4%) | |
| ± 1.25 | 130 (100%) | |
| REFRACTIVE CYLINDER | ± 0.25 | 81 (62.3 %) |
| ± 0.50 | 106 (81.5%) | |
| ± 0.75 | 123 (94.6%) | |
| ± 1.00 | 128 (98.4%) | |
| ± 1.50 | 130 (100%) | |
| DEFOCUS EQUIVALENT* | ± 0.25 | 71 (54.6 %) |
| ± 0.50 | 102 (78.5%) | |
| ± 0.75 | 116 (89.2%) | |
| ± 1.00 | 123 (94.6%) | |
| ± 1.50 | 130 (100%) |
Defocus equivalent = |Spherical equivalent|+ (|Refractive Cylinder|/2)
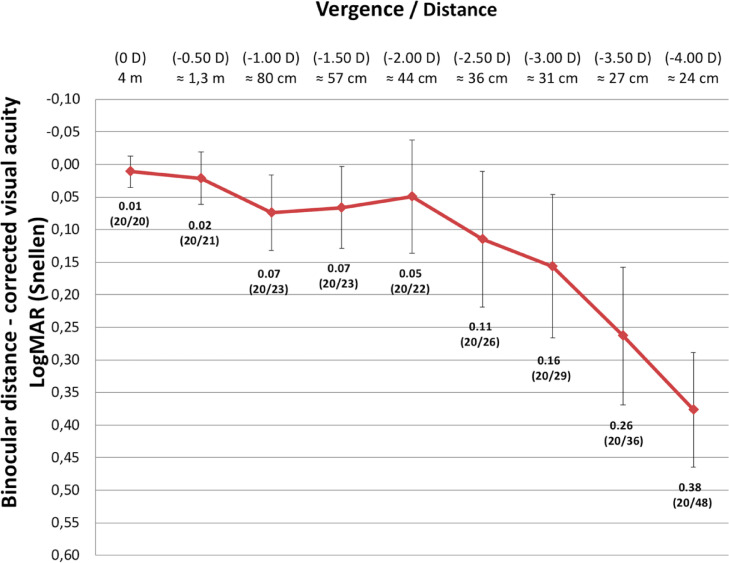
Fig. 1 presents the average distance-corrected binocular defocus curve of the patients. As explained before, an adjustment of the viewing distances for each negative lens presented to the patient was performed accounting for the 4 meters distance of the chart13,19.
Fig. 1.
Binocular defocus curve, with subjects corrected for distance. Viewing distances indicated for each negative lens placed were calculated after adjusting the real negative vergence of each lens, accounting for the 4 meters chart distance (i.e. adding -0.25 D of negative vergence to the power of the lens presented in front of a patient's eye).
The binocular defocus curve showed at vergences corresponding to distances of approximately 1.3 m or further, the best performance, with visions between LogMAR 0.01 and 0.02 (in Snellen 20/20 to 20/21). Then it showed a plateau without a clearly evident peak in visual acuity in the vergences equivalent to intermediate vision (between -1.00 D and -2.00 D, corresponding in distance to the interval between approximately 80 cm and 44 cm,) with visual acuity average between LogMAR 0.05 and 0.07 (in Snellen between 20/22 and 20/23). However, in greater amounts of negative defocus (-2.50 D and -3.00 D, equivalent to distances of around 36 cm and 31 cm) a progressive decrease of the curve was evidenced. The visual acuity in these distances (near vision) was maintained between LogMAR 0.11 and 0.16 (in Snellen between 20/26 and 20/29). Finally, for the vergences -3.50 D and -4.00 D, viewing distance of around 27 cm and 24 cm, the visual acuity diminished to LogMAR 0.26 and 0.38 (Snellen 20/36 and 20/48).
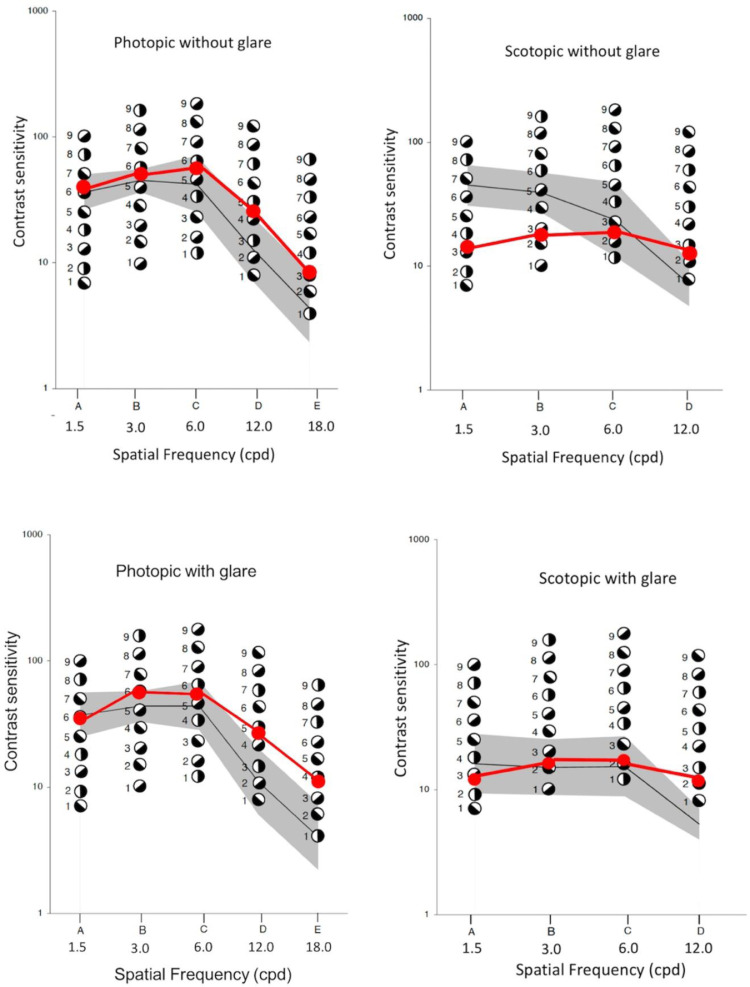
Regarding the reciprocal of the contrast threshold (i.e. contrast sensitivity) in photopic (bright light) conditions, both without and with glare, and also in scotopic conditions (low light) with glare, the values remained within the limit of normality (for patients aged 60 years or more)23, or even a little above normal in conditions with glare and at the higher spatial frequencies. However, when examining contrast sensitivity under scotopic conditions without glare values below normality were found at lower spatial frequencies. Fig. 2.
Fig. 2.
Contrast sensitivity test results (Optec 6500P) compared with the normality for the age group (according to Hohberger et al)23.
The results of the satisfaction survey with the Spanish CATQUEST-9SF questionnaire are summarized in Table 3.Only 6.1% responded that their vision after the procedure did cause some difficulties in their everyday life and none responded that they had great or very great difficulties. Additionally, 100% of the individuals surveyed manifested that they felt satisfied with their vision (84.8% very satisfied and 15.2% fairly satisfied). None of the patients answered that they were rather or very dissatisfied with the results
Table 3.
CATQUEST-9SF questionnaire results.
| No difficulty (Score 1) | Some difficulties (Score 2) | Great difficulties (Score 3) | Very great difficulties (score 4) | |
|---|---|---|---|---|
| Do you consider that your current vision causes you in some way difficulties in your daily life? | 62 (93,9%) | 4 (6,1%) | 0 (0%) | 0 (0%) |
| Very satisfied (Score 1) | Fairly satisfied (Score 2) | Rather dissatisfied (Score 3) |
Very dissatisfied (Score 4) |
|
| Are you satisfied or dissatisfied with your current vision? | 56 (84.8%) | 10 (15.2%) | 0 (0%) | 0 (0%) |
| Do you have difficulties when performing the following activities because of your vision? If your answer is yes, with what intensity? |
No difficulty (score 1) |
Some difficulties (score 2) | Great difficulties (score 3) |
Very great difficulties (score 4) |
| Read the texts of the newspapers | 58 (87.9%) | 8 (12.1%) | 0 (0%) | 0 (0%) |
| Recognize the faces of the people who known | 61 (92.4%) | 5 (7.6%) | 0 (0%) | 0 (0%) |
| See prices of things when will you buy | 57 (86.4%) | 9 (13.6%) | 0 (0%) | 0 (0%) |
| Walking for irregular surfaces. For example: roadway with cobblestones (cobblestone street) |
64 (97%) | 2 (3%) | 0 (0%) | 0 (0%) |
| Make jobs manuals For example: works of carpentry |
64 (97%) | 2 (3%) | 0 (0%) | 0 (0%) |
| Read subtitles on television | 63(95.5%) | 3(4.5%) | 0 (0%) | 0 (0%) |
| When you perform some activity / hobby in which you are interested | 62 (93.9%) | 4 (6.1%) | 0 (0%) | 0 (0%) |
The mean postoperative Rasch-revised Catquest-9SF person score was -3.74 ± 0.4 logits (range -3.94 to -2.09) and showed a median of -3.94 (IQR 0.3).
When patients were enquired if they wore glasses for any activity, whether in distant, near or intermediate vision, we found that 2 of them (3.1%) wore glasses for near and intermediate vision.
The Lapid-Kushlin defocus coefficient calculated from the defocus curve, based on the are under the curve, resulted 0.199.
No patient required refractive surgery for correction of a residual ametropia.
Discussion
Multifocal (both bifocal and trifocal) IOLs´ platforms were designed to increase near vision, maintaining a good distance vision, and thus leading to independence from the glasses. This approach however has an intrinsic inherent problem: when dividing the light in the different focus, the quality of the image on the retina, of each of the two or three focus, is affected. Even so, the results attained with new IOL platforms have been progressively better, and overall satisfaction is high3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18. The initial models were bifocal, with a distant focus and the other for near (35 or 40 cm). However, with the demands of modern life, patients increasingly require the use of intermediate vision (to work on computer screens, for example) and therefore trifocal intraocular lenses were developed. In a meta-analysis recently published, the authors concluded that the uncorrected intermediate visual acuity (UIVA) was significantly lower in the group with the bifocal IOLs than in those patients with trifocal IOLs. On the other hand, no differences were found with respect to the need of spectacles independence, and satisfaction of the patients, when comparing bifocal against trifocal IOLs. In that study by Jin et al., however, the PanOptix® IOL was not included14.
The AcrySof IQ PanOptix® lens (TFNT00) (Alcon Laboratories, Fort Worth, Texas, USA) is a single-piece lens, with a trifocal platform, with a hybrid diffractive-refractive design, with contains a diffractive structure in the most central 4.5 mm of the anterior surface, with 15 diffractive rings that surround a small central refractive zone (≈ 1.16 mm in diameter). In addition, it has another refractive peripheral zone beyond the diffractive rings. At the IOL plane this platform has an addition for intermediate distance of +2.17 D and a maximum add of + 3.25 D for vision at near distance, representing approximately +1.65 D and +2.35 D at the corneal plane after implantation, respectively, for the average pseudophakic anterior chamber depth of a human eye 24.
Optical studies of this lens by performing contrast modulation transfer measurements in an optical bench with an eye model showed that the PanOptix® lens is equivalent to bifocal IOLs in near and far photopic performance, while additionally providing a substantial range of intermediate vision with an optimal intermediate focus close to 60 cm 12. The published clinical results seem to support these experimental findings8, 9, 10, 11,15, 16, 17, 18.
In this series, the percentage of patients who achieved UDVA ≥ 20/25 was remarkably high, 90.8%. García-Perez et al also reported that 96.6% achieved this level of UDVA10. The difference between these proportions did not reach statistically significant difference (p = 0.06).
As predicted by the theoretical performance of the PanOptix® trifocal platform, the visual acuities without correction at the three distances (far, intermediate, 65 cm, and near, 40 cm) were very good: 0.04 ± 0.06 LogMAR (Snellen 20/22), 0.07 ± 0.08 LogMAR (Snellen 20/24) and 0.05± 0.08 LogMAR (Snellen 20/22), respectively. These values were similar to those reported by some groups8, 9, 10, but a little lower than the results published by other groups (p = 0.014)11.
The contrast sensitivity was not altered in photopic (high luminance) conditions, maintaining its average within the limits of normality for the age group23. However, when examined under scotopic (low luminance) conditions without glare, a decrease was evident, being located below the normal, especially at low spatial frequencies. Strikingly, under scotopic conditions with glare there was no diminution of contrast sensitivity compared with normal values for the age group. Escandón-García et al found a reduction in the contrast sensitivity under low luminance (scotopic) conditions with glare, and not only for the PanOptix® lens, but for another trifocal lens (FineVision, PhysIOL, Liege, Belgium)9. However, they performed the test with a different system, and they did not clarify if the normality values were adjusted for the age of the group of patients. On the other hand, García-Perez and co-authors did not find this lessened contrast sensitivity in individuals with PanOptix® platform. They also used a different device than the one employed in this study and the one used by Escandón-García and co-authors, which could somehow influence the results10.
The binocular defocus curve showed a plateau without a clearly evident peak, in visual acuity in the blurs corresponding to intermediate vision (from -2.00 D to -1.00 D, corresponding in distance to the interval between 44 cm and 80 cm) with an average visual acuity LogMAR 0.05 and LodMAR 0.07 (in Snellen between 20/22 and 20/23). Although in larger defocuses (-2.50 D and -3.00 D, corresponding to distances of 36 cm and 31 cm) a progressive decrease of the curve was evidenced, the visual acuity in these distances (near vision) was maintained between LogMAR 0.11 and LogMAR 0.16 (in Snellen between 20/26 and 20/29). On the other hand, by reducing the negative defocus and thus increasing the simulated distance of the object (-0.50 D to 0 D, equivalent to distance between 1.3 m and 4 m), the curve showed an even better performance, with visions of between LogMAR 0.02 and LogMAR 0.01 (in Snellen 20/21 and 20/20).
A similar behavior has been evidenced in other researchers, and because of this, i.e. to the absence of peaks and valleys of visual acuity along the different distances, is that some (as Böhm and coauthors of Kohnen's group) recently suggested naming the PanOptix® IOL as "panfocal" instead of “trifocal” 7,15.
The degree of patient satisfaction and assessment of visual function using a questionnaire in the present research was very high with a median Rasch person score of -3.94 logit. Notice that a more negative logit score indicates a better self-assessed visual function. 93.9% responded that their vision with PanOptix® IOLs did not cause any difficulty in their everyday life and none responded that they had great or very great difficulties. Additionally, 84.8% of the individuals surveyed manifested that they felt very satisfied with their vision and the remaining 15.2% felt fairly satisfied. None responded that he/she was dissatisfied to any degree. Only 2 of the patients included in the present study, (3.1% of the total group) reported that he or she required glasses for intermediate or near vision, after surgery. No patient referred needing eyeglasses for distance vision.
Interestingly, in a study published by Kohnen and coauthors in 2017, despite reporting a higher visual acuity without correction on average (UDVA LogMAR 0.0 +/- 0.1, UIVA LogMAR 0.0 +/- 0.1 and UNVA to LogMAR 0.0 + / - 0.1), one out of 27 patients required glasses for distant vision, and 5 patients (18.5%) indicated that they would not choose that same intraocular lens. They did not indicate what was the distance vision of the patient who required glasses. As for the dissatisfaction with the type of lens, there is no clear explanation, because they had no worse visual acuity or contrast sensitivity than the patients in the present study. In that research, on the other hand, they interrogated directly by halos vision, and 89% of the patients reported them. It is possible that these symptoms were more bothersome in the group of patients in that study conducted in Germany, with patients whose iris color was possibly lighter and the scotopic pupils larger. It is also possible that the visual requirements, especially in intermediate vision, of older adults in Germany were greater than those of our patients in Colombia (where the need to drive at night or the use of computer screens in that age group is not so high). It would be interesting in a future study to investigate more specifically about this type of activity in our patients. These factors could partly explain the greater index of dissatisfaction in the European study15.
We did not interrogate directly by vision of halos or glare, but the patients were asked whether or not they presented any difficulty with their vision, so if they had noticed significant symptoms, they would have answered affirmatively. In that question only 6.1% of the patients indicated that they had some difficulties and none indicated that they had great or very great difficulties. It is noteworthy that it has been suggested that directly inquiring about halos or glare could generate a bias due to the reactivity of patients to the direct questions (also known as the Hawthorne effect / observer effect)11,25.
As already mentioned, this trifocal platform (PanOptix® IOL) has also been described as panfocal, due to the relative plateau in the defocus curve in the intermediate vision, without a clear valley between the peaks of vision7,15. The PanOptix® uses a particular technology, quadrifocal, with 3 different focal points located at 40 cm, 60 cm and 120 cm plus a remote focus (≥ 6 meters). However, this technology was adapted so that the farthermost intermediate focal point (i.e. 120 cm) was redistributed to the focal point of distance to optimize the use of light (Enlighten Optical Technology®). The light is distributed at 25% for near, 25% for intermediate and 50% for far distance.
This behavior was confirmed in the present research, where a plateau between 44 cm and 80 cm was evidenced in the defocus curve, with a slight decrease at the distance of 36 cm. In nearer distances it was evident that performance was lower in the binocular defocus curve, but patients did not complain about this, which is explainable because such short distances are rarely used. Recently similar good results were reported by Lapid-Gortzak et al 16.
The comparison between Panoptix and other platforms have been reported by several authors.
Gundersen & Potvin reported better intermediate uncorrected visual acuity at 60 cm in the individuals with PanOptix IOL than in those with FineVision IOL, six months after surgery, but they did not find discrepancies at other distances 13. Lapid-Gortzak et al. in the defocus curve found an approximately 1-line difference between -1.50 D and -2.0 D defocus in favor Panoptix over ATLIsa Tri (Carl Zeiss AG, Oberkochen, Germany). Panoptix platform was also better than ATLisa tri in binocular uncorrected visual acuity at both intermediate and near distances, while the two trifocal platforms were similar in binocular uncorrected distance visual acuity. They also calculated a new parameter: Acuity reserve, as the proportion of print size to visual acuity limit, by superimposing the defocus curve with the visual acuity requirement for a target size corresponding to 0.1 LogMAR (20/25) at far distance. They applied the definite integral of a curve to determine the area under the curve (AUC), and this parameter was then employed to establish approximately the useful functional range of acuity reserve between 1 m (-1.0 D) and 40 cm (-2.5 D). The mean overall AUC between -1.0 D and -2.50 D was significantly higher for the Panoptix group than for the ATLisa Tri group16.
The Lapid-Kushlin defocus coefficient, which is a recently described new parameter, comes from an abstract model that uses a mathematical model, was created to permit comparing the curves of defocus of different multifocal platforms of IOLs by means of a single measurable number, based on a consideration of the area under the curve of a functional range of vision (defocus amount from plano to -3.50 D). Since this value is based on the LogMAR visual acuity for each defocus step, the lower the quantity, the better the performance of the intraocular lens. This Lapid-Kushlin defocus coefficient was calculated for the group of eyes in the present study and was found to be 0.199. This value was a little less good than to the one calculated by Lapid-Gortzak et al. from published studies (2009–2017) and also including groups of eyes studied by them, which was 0.11 for the Panoptix IOL. However, similar to that shown by Lapid-Gortzak et al., the Lapid-Kushlin coefficient calculated for the group of eyes from the present study with the PanOptix IOL, was better than that calculated for them for other intraocular lens models. For example, for both LISA AT 839MP (Zeiss) and FineVision (Physiol) these researchers calculated a coefficient of 0.27 (Lapid-Gortzak R, Kushlin Y, Lapid O. Area under the graph as a modality for comparing multifocal IOLs. Free Paper. Oral presentation at: XXXVI European Society of Cataract and Refractive Surgeons ESCRS Meeting; September 22–26th, 2018, Vienna, Austria).
Böhm et al. made a study comparing four presbyopia-correcting platforms with regard to their defocus curves: Panoptix, AT Lisa tri (Zeiss), Mplus X (Oculentis), and the so-called “extended depth of focus” Tecnics Symfony (Abbott Medical Optics)15. They found several differences at specific distances. The researchers established that the Tecnics Symfony IOL displayed slightly better distance corrected intermediate visual acuity, but on the other hand it presented worse distance corrected near visual acuity with respect to the other designs. The Panoptix IOL exhibited better distance corrected intermediate visual acuity at 50 cm15.
Recently (2019) in a literature review Sudhir et al. established that the existing evidence suggested that in general good visual results, along with a high degree of independence of spectacles, were attained with the FineVision, PanOptix, AT LISA and Tecnis Symfony IOLs. However, with regard to UIVA (at 60 cm), PanOptix platform exhibited better results than Tecnis Symfony, FineVision and AT LISA. And furthermore, PanOptix exhibited considerably better results for near vision compared with Tecnis Symfony, FineVision, and AT LISA tri 17.
A weakness of the present study was that the measurements of visual acuity (both uncorrected and corrected during manifest refraction examination, and distance-corrected during defocus curve determination) were not done beyond the 20/20 line. Therefore, many patients who possibly could read the 20/15 line were not detected, and the average of visual acuity could be in fact better than shown. In addition, other factors that may affect visual quality were not analyzed (i.e. IOL centration, kappa angle, alpha angle). Additional studies are warranted26, 27, 28.
In conclusion, the trifocal intraocular lens PanOptix® showed very satisfactory results in this group of patients, who achieved independence of the glasses and expressed a high level of satisfaction.
Sources of funding
This study did not receive any specific funding.
Disclosures
None.
Compliance with ethical standards
Ethical approval
All procedures performed in studies involving human subjects were in harmony with the ethical standards of the institutional and/or national research committee (place name of institute/committee) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This study was reviewed and approved by the Research Ethics Committee of the Fundación Oftalmológica de Santander FOSCAL (Floridablanca, Colombia). For this type of study, formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
References
- 1.Galvis V, Tello A, Carreño N. [The crystalline lens for the general practitioner] MedUNAB. 2008;11:225–230. [Google Scholar]
- 2.GBD 2017 Mortality Collaborators Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;10:1684–1735. doi: 10.1016/S0140-6736(18)31891-9. 392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2012;9 doi: 10.1002/14651858.CD003169.pub3. cd003169. [DOI] [PubMed] [Google Scholar]
- 4.Alió JL, Plaza-Puche AB, Férnandez-Buenaga R, Pikkel J, Maldonado M. Multifocal intraocular lenses: an overview. Surv Ophthalmol. 2017;62:611–634. doi: 10.1016/j.survophthal.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 5.Rangel CM, Galvis V, Tello A, Fierro A. [Visual results of toric multifocal intraocular lenses at Fundación Oftalmológica de Santander] Rev Sociedad Colombiana de Oftalmologia. 2014;47:118–126. [Google Scholar]
- 6.Kohnen T, Titke C, Bohm M. Trifocal intraocular lens implantation to treat visual demands in various distances following lens removal. Am J Ophthalmol. 2016;161:71–77. doi: 10.1016/j.ajo.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 7.Böhm M, Hemkeppler E, Herzog M, Schönbrunn S, de'Lorenzo N, Petermann K, Kohnen T. Comparison of a panfocal and trifocal diffractive intraocular lens after femtosecond laser-assisted lens surgery. J Cataract Refract Surg. 2018;44:1454–1462. doi: 10.1016/j.jcrs.2018.07.060. [DOI] [PubMed] [Google Scholar]
- 8.Alió JL, Plaza-Puche AB, Alió Del Barrio JL, Amat-Peral P, Ortuño V, Yébana P, Al-Shymali O, Vega-Estrada A. Clinical outcomes with a diffractive trifocal intraocular lens. Eur J Ophthalmol. 2018;28:419–424. doi: 10.1177/1120672118762231. [DOI] [PubMed] [Google Scholar]
- 9.Escandón-García S, Ribeiro FJ, McAlinden C, Queirós A, González-Méijome JM. Through-focus vision performance and light disturbances of 3 new intraocular lenses for presbyopia correction. J Ophthalmol. 2018;2018 doi: 10.1155/2018/6165493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, Blázquez V, Contreras I. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17:72. doi: 10.1186/s12886-017-0462-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kohnen T, Herzog M, Hemkeppler E, Schönbrunn S, De Lorenzo N, Petermann K, Böhm M. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52–62. doi: 10.1016/j.ajo.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Lee S, Choi M, Xu Z, Zhao Z, Alexander E, Liu Y. Optical bench performance of a novel trifocal intraocular lens compared with a multifocal intraocular lens. Clin Ophthalmol. 2016;10:1031–1038. doi: 10.2147/OPTH.S106646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gundersen KG, Potvin R. Trifocal intraocular lenses: a comparison of the visual performance and quality of vision provided by two different lens designs. Clin Ophthalmol. 2017;11:1081–1087. doi: 10.2147/OPTH.S136164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jin S, Friedman DS, Cao K, Yusufu M, Zhang J, Wang J, Hou S, Zhu G, Wang B, Xiong Y, Li J, Li X, He H, Wan X. Comparison of postoperative visual performance between bifocal and trifocal intraocular lens based on randomized controlled trails: a meta-analysis. BMC Ophthalmol. 2019;19:78. doi: 10.1186/s12886-019-1078-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Böhm M, Petermann K, Hemkeppler E, Kohnen T. Comparative analysis of defocus curves of four presbyopia-correcting intraocular lenses with four designs: diffractive panfocal, diffractive trifocal, segmental refractive and extended depth of focus. J Cataract Refract Surg. 2019;45:1625–1636. doi: 10.1016/j.jcrs.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 16.Lapid-Gortzak R, Bhatt U, Sanchez JG, et al. Multicenter visual outcomes comparison of 2 trifocal presbyopia-correcting intraocular lenses: 6-month postoperative results. J Cataract Refract Surg. 2020;46:1534–1542. doi: 10.1097/j.jcrs.0000000000000274. [DOI] [PubMed] [Google Scholar]
- 17.Sudhir RR, Dey A, Bhattacharrya S, Bahulayan A. AcrySof IQ PanOptix intraocular lens versus extended depth of focus intraocular lens and trifocal intraocular lens: a clinical overview. Asia Pac J Ophthalmol (Phila) 2019;8:335–349. doi: 10.1097/APO.0000000000000253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rementería-Capelo LA, Contreras I, García-Pérez JL, Blázquez V, Ruiz-Alcocer J. Visual quality and patient satisfaction with a trifocal intraocular lens and its new toric version. J Cataract Refract Surg. 2019;45:1584–1590. doi: 10.1016/j.jcrs.2019.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Galvis V, Tello A, Carreño NI, Berrospi RD, Niño CA, Serna VH. Defocus curve and vergence related to viewing distance. J Cataract Refract Surg. 2020;46(5):803. doi: 10.1097/j.jcrs.0000000000000158. Maydoi:PMID: 32358289.] [DOI] [PubMed] [Google Scholar]
- 20.Lundstrom M, Pesudovs K. Catquest-9SF patient outcomes questionnaire: nine-item short-form Rasch-scaled revision of the Catquest questionnaire. J Cataract Refract Surg. 2009;35:504–513. doi: 10.1016/j.jcrs.2008.11.038. [DOI] [PubMed] [Google Scholar]
- 21.Lundström M, Llovet F, Llovet A, Martinez Del Pozo M, Mompean B, González JV, Pesudovs K. Validation of the Spanish Catquest-9SF in patients with a monofocal or trifocal intraocular lens. J Cataract Refract Surg. 2016;42:1791–1796. doi: 10.1016/j.jcrs.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Viberg A, Liv P, Behndig A, Lundström M, Byström B. The impact of corneal guttata on the results of cataract surgery. J Cataract Refract Surg. 2019;45:803–809. doi: 10.1016/j.jcrs.2018.12.023. [DOI] [PubMed] [Google Scholar]
- 23.Hohberger B, Laemmer R, Adler W, Juenemann AG, Horn FK. Measuring contrast sensitivity in normal subjects with OPTEC 6500: influence of age and glare. Graefes Arch Clin Exp Ophthalmol. 2007;245:1805–1814. doi: 10.1007/s00417-007-0662-x. [DOI] [PubMed] [Google Scholar]
- 24.Product information, Alcon Laboratories, Inc. AcrySof® IQ PanOptix® Trifocal IOLs. Available at https://www.accessdata.fda.gov/cdrh_docs/pdf4/P040020S087D.pdf. Consulted 4 November 2020.
- 25.McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67:267–277. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fuentes-Mendoza V, Galvis V, Tello A, Aparicio JP, Sánchez B. [Spherical acrysof restor vs. aspherical acrysof restor: centering and effect on the objective and subjective visual quality of the patient] Rev. Sociedad Colombiana de Oftalmologia. 2009;42:887–900. [Google Scholar]
- 27.Chang DH, 4th Waring GO. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158:863–874. doi: 10.1016/j.ajo.2014.06.028. [DOI] [PubMed] [Google Scholar]
- 28.Zhu X, He W, Zhang Y, Chen M, Du Y, Lu Y. Inferior decentration of multifocal intraocular lenses in myopic eyes. Am J Ophthalmol. 2018;188:1–8. doi: 10.1016/j.ajo.2018.01.007. [DOI] [PubMed] [Google Scholar]