Abstract
BACKGROUND
Percutaneous endoscopic lumbar decompression is gaining attention as a minimally invasive surgery. Here, the authors report a rare complication of pneumocephalus caused by vacuum drain after biportal endoscopic spinal surgery (BESS) for lumbar stenosis.
OBSERVATIONS
A 79-year-old woman with spinal stenosis over the L4–5 level received BESS. No visible dural tear was encountered during surgery, and a vacuum drain was placed after surgery. Approximately 150 mL of cerebrospinal fluid was drained on postoperative day 1. Simultaneously, symptoms of intracranial hypotension were noted. Brain computed tomography (CT) revealed pneumocephalus. The patient was advised to have bed rest and hydration, and her symptoms improved subsequently. Follow-up brain CT indicated the resolution of pneumocephalus.
LESSONS
Pneumocephalus after endoscopic lumbar surgery is rare. Dural tear, high rate of normal saline irrigation, and vacuum drain placement are the associated risk factors.
Keywords: pneumocephalus, endoscopic spine surgery, dural tear, vacuum drain
ABBREVIATIONS : BESS = biportal endoscopic spinal surgery, CSF = cerebrospinal fluid, CT = computed tomography, GCS = Glasgow Coma Scale, ICP = intracranial pressure, MRI = magnetic resonance imaging, N2O = nitrous oxide, PELD = percutaneous endoscopic lumbar decompression, POD = postoperative day
Pneumocephalus is defined as the presence of air or gas within the cranial cavity.1 The first case of pneumocephalus was described by Lecat in 1866,2 but the term “pneumocephalus” was first used by Wolff in 1914 to describe this unusual condition.3 The leading causes of pneumocephalus are head trauma and disruption of the skull or skull base from cranial surgery, thereby trapping air in the cranial vault.4 Dural injury is another important etiology of pneumocephalus. Although it is uncommon, pneumocephalus could occur after invasive spinal procedures, such as spine surgery, lumbar puncture, and spinal anesthesia.5
Percutaneous endoscopic lumbar decompression (PELD), both uniport and biport, is gaining increasing attention. PELD allows the spine surgeon to treat patients through smaller incisions, unlike traditional surgery. One of the major differences between PELD and traditional microsurgery decompression is the surgical field. The surgical field of traditional microsurgery lumbar decompression is kept clean by suction, and the tissues are directly exposed to air while the surgical field of PELD is maintained by continuous normal saline irrigation. The working space of PELD is soaked with water, which acts as a barrier between tissue and air. Complications of PELD are inevitably the same as those of traditional microsurgery decompression, such as inadequate decompression, nerve root injury, and dural tear. However, pneumocephalus after endoscopic decompression is rare and unexpected. We present a case of pneumocephalus that occurred because of vacuum drain placement after biportal endoscopic spine surgery (BESS) without intraoperative dural tear.
Illustrative Case
A 79-year-old woman with a history of hypertension reported to our pain clinic for low back pain. She had been experiencing low back pain for more than 3 years. She had undergone physical therapy, acupuncture, and pharmacotherapy; however, the results were unsatisfactory. Her symptoms had worsened with claudication and decreasing muscle power before she visited our clinic. Neurological examination revealed L5 dermatome paresthesia and decreased muscle power over the extensor longus. These signs and symptoms were dominant on the right side. Plain film radiography indicated some degeneration over several levels of the lumbar spine with spurs. No obvious spondylolisthesis was noted on the flexion-extension view. Magnetic resonance imaging (MRI) reported a hypertrophic flavum ligament with dural sac compression at the L4–5 level. The compression was categorized as grade C according to the Schizas grading system, indicating severe stenosis (Fig. 1A).
FIG. 1.
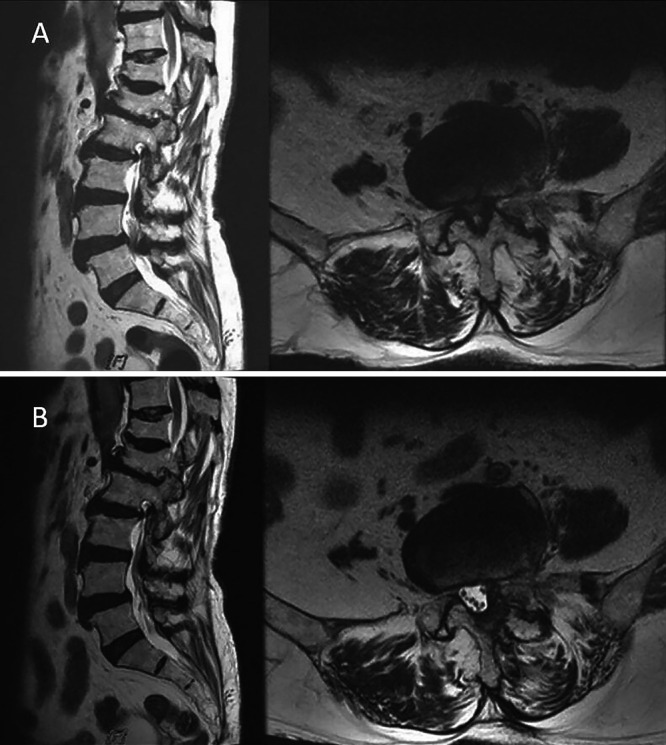
A: Sagittal and axial views of MRI indicated Schizas grade C stenosis. B: MRI performed 4 months later indicated no fluid accumulation over the decompression area.
BESS via an interlaminar approach was arranged with the patient under general anesthesia. The patient was placed in the prone position with hip flexion. Two small incisions were made through the deep fascia over the L4–5 level. The smaller incision of approximately 6 mm was made for the endoscope tunnel with continuous normal saline irrigation, and a larger incision of approximately 10 mm served as the instrument portal and the outflow for normal saline. A normal saline bag was set at approximately 20 cm above the operation plane.
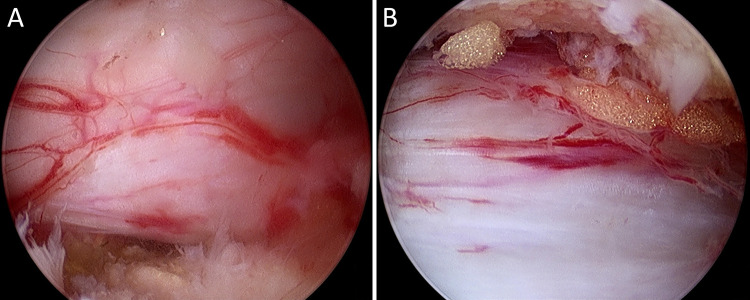
The hypertrophic flavum ligament was removed, and the bilateral lateral recess was decompressed. Neither root injury nor dural tear was found during the operation (Fig. 2). A vacuum drain was inserted through the working tunnel until reaching the epidural space and was fixed. The wound was closed with subcutaneous Vicryl sutures and sterilized strips. The whole operation lasted approximately 170 minutes, and the blood loss was minimal.
FIG. 2.
A: Ipsilateral decompression. B: Contralateral sublaminar decompression.
On postoperative day (POD) 1, the patient felt better with respect to the low back pain and bilateral leg paresthesia. A total of 150 mL of CSF was drained, and the vacuum drain was removed immediately. An occult dural tear with CSF leakage was impressed. Meanwhile, the patient developed a headache with nausea and dizziness, which was aggravated by standing up and relieved by lying down. Intracranial hypotension was suspected, and brain computed tomography (CT) was performed on POD 3, which indicated pneumocephalus with air dispersed in the bilateral ventricles and subarachnoid space (Fig. 3A).
FIG. 3.
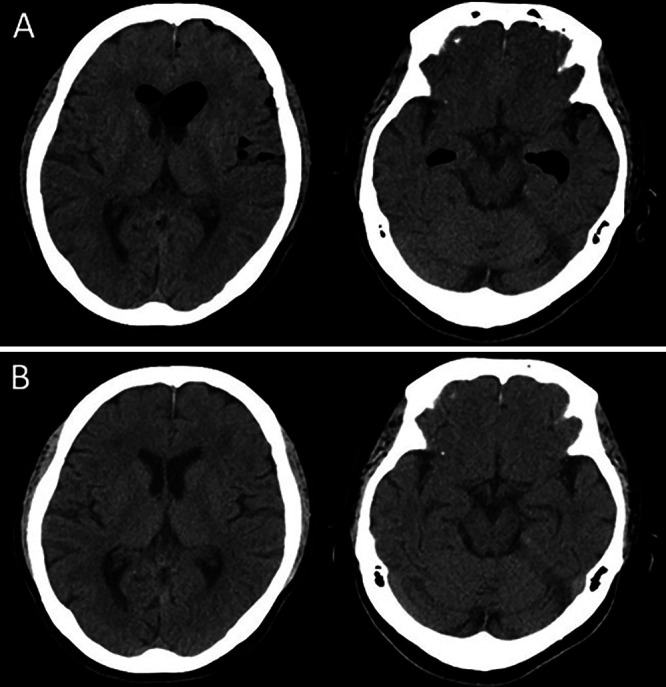
A: CT performed on POD 3 indicated air dispersion within the ventricle and subdural space. B: CT performed 1 month later indicated resolution of the pneumocephalus.
Bed rest (supine position), analgesics, and normal saline hydration were administered as treatment. We constantly monitored the patient’s Glasgow Coma Scale (GCS) scores. Approximately 1 week after the operation, the intensity of headache and sensation of nausea decreased. During these days, the patient’s GCS score was the same, and E4V5M6 and bilateral L5 radiculopathy improved considerably. The patient was discharged and was kept under follow-up.
One month after the operation, no pneumocephalus was observed on brain CT (Fig. 3B). Postoperative lumbar MRI was performed 4 months later and indicated proper decompression and no fluid accumulation in the spinal canal (Fig. 1B) or any other location.
Discussion
Observations
In this report, we used the PubMed database for our literature review. The following keywords were used: (endoscopic) AND (lumbar) AND (pneumocephalus). Only two cases of pneumocephalus after endoscopic lumbar decompression were reported (Table 1).6,7 Compared with two other cases, our case is different in terms of an invisible intraoperative dural tear and the placement of a vacuum drain.
TABLE 1.
Characteristics of the three cases
| Authors & Year | Age (yr)/ Sex | Time Until Development of PNC | Type of Op | Signs & Symptoms | Image | Treatment | Dural Tear | Drain |
|---|---|---|---|---|---|---|---|---|
| Lin et al., 20196 |
63/M |
Immediately after op |
PELD for L3/4 |
Seizure (GTC) & conscious disturbance |
CT |
HBO2 |
+ |
− |
| Kim et al., 20117 |
67/F |
Immediately after op |
PELD for L3/4 |
Seizure (GTC) & conscious disturbance |
CT/MRI |
Conservative |
+ |
− |
| Present case | 79/F | 1 day | PELD for L4/5 | Headache & nausea | CT | Conservative | − | + |
CT = computed tomography; GTC = generalized tonic-clonic; HBO2 = hyperbaric oxygen therapy; MRI = magnetic resonance imaging; PELD = percutaneous endoscopic lumbar decompression; PNC = pneumocephalus.
Most of the pneumocephalus after lumbar spine surgery could be explained by two major theories:8 the inverted bottle theory and the ball valve theory.9,10 The inverted bottle theory deduces that the negative pressure caused by CSF leakage is replaced by air until the intracranial pressure and extracranial pressure reach equilibrium. The ball valve theory speculates that the air enters the intracranial cavity through a dural defect, which also acts as a one-way valve and traps the air. The dural defect plays a key role in both theories. The dura could be violated directly and indirectly. The direct dural injury, encountered in the other two cases, is caused by surgical instruments during the operation, whereas indirect dural injury may result from a high-pressure gradient produced by a settled vacuum drain. Furthermore, the high-pressure gradient aggravates the CSF leakage. We speculate that the worn dura or the violated dura with intact arachnoid membrane is vulnerable to the indirect injury. In our case, we believe both direct injury and indirect injury played roles in an invisible dural tear and vacuum drain aspiration.
Normally, the whole surgical field of endoscopic spine surgery is soaked with water and is separated from air. How did the air get into the intrathecal space through the dural defect under this water-filled environment? There are two possible mechanisms. First, the air is trapped by normal saline and is introduced into the surgical field and subarachnoid space by repetitive entry and exit of tools through the working channel.6 This is the theory proposed by Lin et al.6 Second, when the CSF is drained out, the pressure of the intrathecal space is relatively lower. Once the vacuum bottle was disconnected from the drain tube, the air flowed in through the drain tube. We believe that the second mechanism accounts for the air inflow in our case and explains why pneumocephalus was not noted immediately after the operation in comparison with other two cases.
Under the situation of an intact dura, Joh et al.11 proposed that the massive use of normal saline irrigation during the operation is somehow related to the increase in epidural pressure and intracranial pressure (ICP). If an inadvertent dural tear occurs, a connecting pipe is formed. We suppose that ICP is gravely impacted not only by normal saline epidural compression but also by normal saline entering the intrathecal space via the dural defect. It is reasonable to deduce that the increase in ICP is positively correlated with the size of the dural tear and the pressure provided by normal saline irrigation. Intraoperatively, a clear surgical field was maintained by continuous normal saline irrigation. The height of a normal saline bag is approximately 20–30 cm above the surgical field. If bleeding is confronted, the pressure of irrigation can be elevated by compressing the normal saline bag or adjusting the height of the normal saline bag. Uchida et al.12 described that the increase in ICP reduced the frequency of seizures in a case of status epilepticus. The relationship between seizures and ICP has been proposed but not clearly identified. Whether changes in ICP can evoke seizures remains controversial.12 Lin et al.13 proposed that the appearance of the Cushing triad during the operation is a prodrome of seizure after PELD. After reviewing anesthesia records, no Cushing triad occurred during the operation. In addition, the normal saline outflow is less impeded in BESS than in uniport endoscopic spine surgery. It is unclear which type of endoscope was used in the other two cases because it is not mentioned in the literature. The major difference between our case and the other two case lies in the size of the dural defect during the operation, and we assume that is why seizure and coma did not occur in our case.
In addition to the compression and influx of normal saline irrigation, Kim et al.7 proposed that the inhalation of nitrous oxide (N2O) could also increase ICP. N2O is used for maintaining general anesthesia, and the partial pressure of N2O in the air is low. Once the dissolved N2O contacts the entrapped air, the N2O escapes from solution and expands the pneumocephalus. There is no record of N2O use in our case.
Lessons
Percutaneous endoscopic lumbar decompression is a minimally invasive technique that has been proved to be effective and safe. However, pneumocephalus, a rare complication, can occur even without dural tear during the procedure. Hence, it is crucial to avoid dural tear during the operation. Second, it is important to maintain adequate homeostasis without pumping normal saline or elevating the normal saline bag to a higher level. Third, the operation time should be shortened. Finally, as seen in this case, the placement of a vacuum drain should be avoided.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Wu, Yang. Acquisition of data: Wu, Yang. Analysis and interpretation of data: Wu, Yang. Drafting the article: Wu, Yang. Critically revising the article: Wu, Yang. Reviewed submitted version of manuscript: Wu, Yang. Approved the final version of the manuscript on behalf of all authors: Wu. Statistical analysis: Yang. Administrative/technical/material support: Wu. Study supervision: Wu, Chiu.
References
- 1. An BK, Hyun DK, Kim KC, Park CO, Ha YS. A case of anterior sacral meningocele with pneumocephalus and meningitis. J Korean Neurosurg Soc. 1999;28:997–1000. [Google Scholar]
- 2. Jelsma F, Moore DF. Cranial aerocele. Am J Surg. 1954;87(3):437–451. doi: 10.1016/s0002-9610(54)90147-6. [DOI] [PubMed] [Google Scholar]
- 3. Wolff E. Luftansammlung im rechten Seitenventrikel des Gehirns (Pneumozephalus) Munch Med Wochenschr. 1914;61:899. [Google Scholar]
- 4. Kizilay Z, Yilmaz A, Ismailoglu O. The effect of the previous craniectomy on the formation of tension pneumocephalus after spinal dural injury: a case report and review of the literature. Interdiscip Neurosurg. 2017;8:60–63. [Google Scholar]
- 5. Eltorai IM, Montroy RE, Kaplan SL, Ho WH. Pneumocephalus secondary to cerebrospinal fluid leak associated with a lumbar pressure ulcer in a man with paraplegia. J Spinal Cord Med. 2003;26(3):262–269. doi: 10.1080/10790268.2003.11753695. [DOI] [PubMed] [Google Scholar]
- 6. Lin CH, Lin SM, Lan TY, Pao JL. Pneumocephalus with conscious disturbance after full endoscopic lumbar diskectomy. World Neurosurg. 2019;131:112–115. doi: 10.1016/j.wneu.2019.07.200. [DOI] [PubMed] [Google Scholar]
- 7. Kim SH, Song GS, Sung SK, Son DW. A case of seizure in a patient following percutaneous endoscopic lumbar discectomy. Korean J Spine. 2011;8(1):55–58. [Google Scholar]
- 8. Abu-Hamdiyah OJ, Al Sharie S, Awadi S, Khamees A, Athamneh MJ. Pneumocephalus secondary to a spinal surgery: a literature review and a case report. Int J Surg Case Rep. 2021;86:106342. doi: 10.1016/j.ijscr.2021.106342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Horowitz M. Intracranial pneumocoele: an unusual complication following mastoid surgery. J Laryngol Otol. 1964;78(2):128–134. doi: 10.1017/s0022215100061910. [DOI] [PubMed] [Google Scholar]
- 10. Dandy WE. Pneumocephalus (intracranial penumatocele or aerocele) Arch Surg. 1926;12(5):949–982. [Google Scholar]
- 11. Joh JY, Choi G, Kong BJ, Park HS, Lee SH, Chang SH. Comparative study of neck pain in relation to increase of cervical epidural pressure during percutaneous endoscopic lumbar discectomy. Spine (Phila Pa 1976) 2009;34(19):2033–2038. doi: 10.1097/BRS.0b013e3181b20250. [DOI] [PubMed] [Google Scholar]
- 12. Uchida D, Fujimoto A, Yamazoe T, Yamamoto T, Enoki H. Seizure frequency can be reduced by changing intracranial pressure: a case report in drug-resistant epilepsy. Epilepsy Behav Case Rep. 2018;10:14–17. doi: 10.1016/j.ebcr.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin CY, Chang CC, Tseng C, et al. Seizure after percutaneous endoscopic surgery-incidence, risk factors, prevention, and management. World Neurosurg. 2020;138:411–417. doi: 10.1016/j.wneu.2020.03.121. [DOI] [PubMed] [Google Scholar]