Clinical vignette
A 70-year-old patient, with a past medical history of liver cirrhosis (Child-Pugh B8) with multiple episodes of encephalopathy, ascites, and oesophageal varices (grade I–II), presented to the emergency department complaining of progressive dyspnoea and asthenia over the past month. He admitted to have had three episodes of dizziness and blurry vision when standing up from a sitting position in the last 2 weeks, without having had any loss of consciousness.
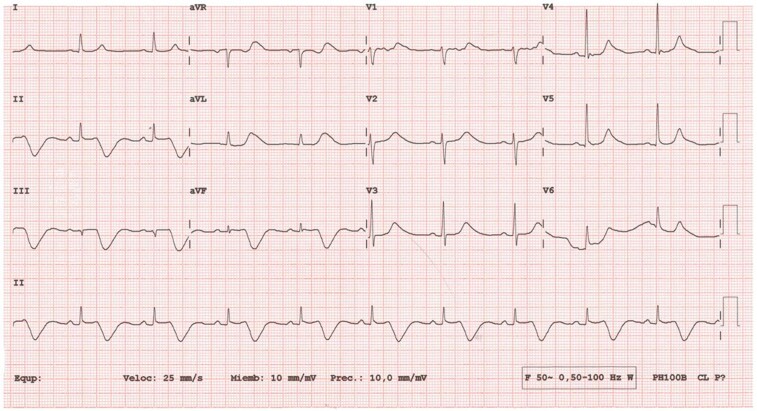
The patient was taking 50 mg of propranolol every 12 hours due to primary prophylaxis for variceal bleeding. Another electrocardiogram (ECG) was ordered to reassess the underlying rhythm, which is displayed in the Figure.
During the acquisition of the tracing, the nurse did not report any difficulty with the placement of the self-adhesive electrodes; no cardiologist was present when the tracing was obtained. This ECG finding led to an immediate clinical exam of the patient. A complete biochemical blood test, with ionogram and cardiac biomarkers, was extracted; without any pathological result, the ECG was repeated, and it was completely normal.
What is the explanation for the new ECG changes?
Single ECG figure
Multiple-choice questions and explanations
Question 1
-
(1) Judging by the ECG T wave morphology, what’s the most likely diagnosis?
Wellens T waves
Inferior myocardial infarction
Propranolol toxicity
Electromechanical association artifact
Hepatotoxicity
Correct answer: D
This ECG displays a prolonged QT interval at the expense of a deep T wave inversion in inferior leads. Wellens T waves consist of a symmetrical and anterior negativization of T waves, which is not the case. While an inferior myocardial infarction is a possible diagnosis, the clinical vignette (without pain) and the absence of reciprocal changes in I and aVL make it very unlikely in this setting.
Sparing of lead I raises the suspicion for an electromechanical association artifact, probably because of a pulsatile left posterior artery since the artifact has a fixed relation with the QRS (lead I is formed between right and left arm, thus being spared).
Question 2
-
(2) What’s the correct management in this setting?
Immediately stop propranolol
Emergency transvenous pacemaker
Repeat the ECG with new electrodes
Start isoproterenol drip
Consult hepatologist
Correct answer: C
As discussed, the sparing of lead I makes it likely an electromechanical artifact. The repeated ECG is normal afterwards (included in thesupplemental material). The rest of the options exhibit potential harmful effects of not recognizing this pattern and unnecessarily stopping/starting therapies (e.g. if propranolol is stopped long enough, it could precipitate variceal bleeding).
Question 3
-
(3) Why are the precordial leads affected in a left lower limb artifact?
Wilson central terminal
QT prolongation normally occurs in all leads
Precordial leads are not affected
Precordial leads are calculated from the right lower limb
Not affected, as no T inversion is observed
Correct answer: A
The explanation of the artifactual T wave in aVR and aVL is sustained by the fact that most of the electrocardiography devices record leads I and II and then calculate other limb derivations from these two derivations.1 When one of this limb electrodes is affected, it distorts not only the corresponding lead but also leads III, aVR, aVL, and aVF, which are all calculated by mathematical equations from the first two derivations, including the distorted one.2
As in our case, it should be noted that limb artifacts do also affect the precordial leads because of the Wilson central terminal, which involves the three unipolar limb leads and constitutes the negative pole.3
Supplementary Material
Contributor Information
Ravi Vazirani Ballesteros, Department of Cardiology, Hospital Clínico San Carlos (Madrid), Instituto Cardiovascular, Calle Profesor Martín Lagos s/n, 28040 Madrid, Spain.
Zaira Gómez Álvarez, Department of Cardiology, Hospital Clínico San Carlos (Madrid), Instituto Cardiovascular, Calle Profesor Martín Lagos s/n, 28040 Madrid, Spain.
Carmen Olmos Blanco, Department of Cardiology, Hospital Clínico San Carlos (Madrid), Instituto Cardiovascular, Calle Profesor Martín Lagos s/n, 28040 Madrid, Spain.
Supplementary material
Supplementary material is available at European Heart Journal—Case Reports online.
Acknowledgements
All authors have contributed equally to the work.
Consent: the patient expressed written consent for the ECG and anonymized clinical case in accordance with COPE guidelines.
Conflict of interest: None declared.
Funding: None declared.
References
- 1. Aslanger E. An unusual electrocardiogram artifact in a patient with near syncope. J Electrocardiol 2010;43:686–688. [DOI] [PubMed] [Google Scholar]
- 2. Aslanger E. Maybe a dazzle but not puzzle. J Electrocardiol 2010;43:682–684. [DOI] [PubMed] [Google Scholar]
- 3. Rudiger A, Hellermann JP, Mukherjee R, Follath F, Turina J. Electrocardiographic artifacts due to electrode misplacement and their frequency in different clinical settings. Am J Emerg Med 2007;25:174–178. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.