Abstract
Introduction
Several studies have demonstrated dysbiosis in irritable bowel syndrome (IBS). Therefore, faecal microbiota transplantation, whose effect and safety have been proven in Clostridioides difficile infections, may hold promise in other conditions, including IBS. Our study will examine the effectiveness of stool transfer with artificially increased microbial diversity in IBS treatment.
Methods and analysis
A three-group, double-blind, randomised, cross-over, placebo-controlled study of two pairs of gut microbiota transfer will be conducted in 99 patients with diarrhoeal or mixed type of IBS. Patients aged 18–65 will be randomised into three equally sized groups: group A will first receive two enemas of study microbiota mixture (deep-frozen stored stool microbiota mixed from eight healthy donors); after 8 weeks, they will receive two enemas with placebo (autoclaved microbiota mixture), whereas group B will first receive placebo, then microbiota mixture. Finally, group C will receive placebos only. The IBS Severity Symptom Score (IBS-SSS) questionnaires will be collected at baseline and then at weeks 3, 5, 8, 11, 13, 32. Faecal bacteriome will be profiled before and regularly after interventions using 16S rDNA next-generation sequencing. Food records, dietary questionnaires, anthropometry, bioimpedance, biochemistry and haematology workup will be obtained at study visits during the follow-up period. The primary outcome is the change in the IBS-SSS between the baseline and 4 weeks after the intervention for each patient compared with placebo. Secondary outcomes are IBS-SSS at 2 weeks after the intervention and 32 weeks compared with placebo and changes in the number of loose stools, Bristol stool scale, abdominal pain and bloating, anthropometric parameters, psychological evaluation and the gut microbiome composition.
Ethics and dissemination
The study was approved by the Ethics Committee of Thomayer University Hospital, Czechia (G-18-26); study results will be published in peer-reviewed journals and presented at international conferences and patient group meetings.
Trial registration number
Keywords: functional bowel disorders, adult gastroenterology, microbiology
Strengths and limitations of this study
Usage of mixed microbiota from multiple donorsinflates the diversity of transferred microbiotaby enriching it for numerous rare species.
All interventions will be carried out using the same active mixed microbiota or the same placebo.
Each intervention consists of two consecutive transfers, which increases the probability that the transferred microbiota engrafts.
Microbiome profiling, food records, anthropometry and bioimpedance data allow detailed monitoring of transfer effectiveness.
Mucosa-associated microbiota will not be assessed because the stool transfer will be performed by enema, not colonoscopy that would allow biopsies.
Introduction
Irritable bowel syndrome (IBS) is characterised as recurrent abdominal pain on average at least oneday/week in the last 3 months, associated with two or more of the following criteria: (1) related to defecation; (2) associated with a change in the frequency of stool and (3) associated with a change in the form (appearance) of stool.1 It is common among the adult Europid population (approx. 10%2), but its aetiology is still unknown. It may, among other causes, include microinflammation, disturbance of the brain–gut axis, inadequate secretion of bile acids, increased permeability of the gut epithelial barrier, or gut dysbiosis. Dysbiosis in IBS has been suggested by several studies.3 There are indications that Firmicutesmay be disturbed, with Dorea, Blautia and Roseburia increased, whereas Veillonella and Faecalibacterium decreased. Among Actinobacteria, a decrease in Bifidobacterium was noted, and among Proteobacteria, Enterobacteriaceaewere increased. Conflicting and heterogeneous results were reported for Bacteroidetes. The major limitation of available studies is their cross-sectional character, which may not be enough in a disease where diarrhoeal episodes alternate with normal stool composition or constipation.
The faecal microbiota transplantation (FMT) has gained popularity by its remarkableeffect in recurrent Clostridioides difficile infections, where it has now become a recognised life-saving therapy.4 The first published randomised, double-blinded study on FMT in IBS, published in 2018 when starting our study,5 used stool intervention from an allogeneic donor or autologous stool. The intervention was centred on a well-defined group of IBS of predominantly diarrhoeal form. The stool was transferred by colonoscopy to the cecum. The primary outcome was an improvement in the IBS-Severity Symptom Score (IBS-SSS). The treatment was associated with a significant effect at 3 months but not at 12 months postintervention.5 This study used single donors and did not assess stool microbiota. Thus, the transferred microbiota likely varied between transfers both in their composition and in their diversity. Since then, more studies focused on FMT in IBS have beencarried out.6–11 They differed in design, but none of them used a mixed microbiota from multiple donors as the active substance. Furthermore, a recent meta-analysis of randomised control trials on FMT in IBS (including the above-mentioned articles) pointed out insufficient evidence quality to support recommending FMT in the treatment of IBS.12
Our study protocol aims to test whether FMT of mixed microbiota from several selected donors can alleviate symptoms of IBSmeasured by IBS-SSS 4 weeks after the intervention, as compared with autoclaved placebo. The secondary study aims to test the acute (after 2 weeks) and the long-term effect (after 6 months)on symptoms relief. We also focus on the number of loose stools, Bristol stool scale, abdominal pain and bloating, body mass index (BMI), fat content, waist circumference, skinfold thickness, psychological evaluation and the gut microbiome composition.
We hypothesisethat the transfer of active microbiota of high diversity can lead to changes in thepatient’s gut microbiome composition and/or function toalleviate IBS symptoms.
Methods and analysis
Study design
This is a three-group, double-blind, placebo-controlled, randomised, cross-over study in adult patients diagnosed with IBS (diarrhoeal or mixed form) according to Rome IV criteria. Each study subject will undergo two pairs of FMT (a total of four enemas for each patient), with the pairs of transfers being 8 weeks apart. The active intervention substance is a mixed stool microbiota derived from healthy individuals who were preselected for high alpha diversity of their microbiome and distance in community ordination from IBS patient’smicrobiota. Placebo is the same mixture, inactivated by autoclaving.
The study subjects are randomly assigned to one of three groups: (A) enema with active substance first and with placebo second or (B) enema with placebo first and active substance second or (C) enemas of placebo only (detailed scheme in figure 1). Eligible participants will be followed up for 32 weeks after the first intervention to monitor symptom severity scoring of IBS (IBS-SSS), with regular profiling of their gut microbiome and other parameters like the number of loose stools, Bristol stool scale, abdominal pain and bloating, BMI, fat content, waist circumference, skinfold thickness and psychological evaluation.
Figure 1.
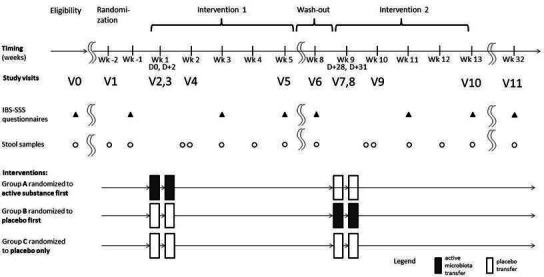
Per-protocol intervention scheme: the visits, questionnaires and samples. IBS-SSS, Irritable Bowel Syndrome Severity Symptom Score.
The placebo group is planned because of the unknown onset and duration of the intervention effect: if the beginning of an effect is delayed, or if it persists for a long time, simple cross-over design would not have sufficient power due to the carry-over effect. In case the FMT was associated with significant but not durable amelioration of the status, the control group would still increase the statistical power.
This study protocol is reported as per the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) guidelines13 (for the SPIRIT checklist see online supplemental appendix 1).
bmjopen-2021-056594supp001.pdf (71.3KB, pdf)
Study setting
The participants are recruited at a single centre, the Department of Internal Medicine, Thomayer University Hospital in Prague, Czech Republic. This hospital has approximately 1000 beds, including 80 in intensive care units, serves approximately 50 000 patients per year. The centre is experienced in treating patients with IBS and other functional gastrointestinal disorders, with about 200 such patients registered and further subjects coming for consultations from other workplaces to this tertiary referral centre.
Recruitment and eligibility criteria
Stool donors
Stool donor candidates were recruited among blood donors at Thomayer University Hospital and medical students in their first year of study (ie, preclinical) from the second Faculty of Medicine, Charles University, Prague. We obtained stool samples from 58 such candidates fulfilling the inclusion criteria (table 1). Based on their high bacterial alpha-diversity and by the position on the ordination plot of the weighted UniFrac distance against 46 patients with IBS-D (figure 2), 14 candidates proceeded to the safety screening, where by 8 passed it (for reasons of candidate’s exclusion, see figure 3.
Table 1.
Inclusion and exclusion criteria for FMT donors
| Inclusion | Adults aged 18–65 years |
| BMI 18.5–27 kg/m2 | |
| Lack of restrictive diets (diet discussed with experienced gastroenterologist) | |
| Bristol stool scale usually between 3 and 4 | |
| High alpha diversity and significant difference in beta-diversity from patients (using 16S rDNA sequencing) | |
| Expected to donate regularly | |
| Consented in writing | |
| Exclusion | Any chronic GI disease in patient’s history (coeliac disease, inflammatory bowel disease, irritable bowel syndrome, colorectal carcinoma) or active acute GI issues (infectious gastroenteritis or enterocolitis, frequent bloating, diarrhoea or vomiting) |
| Chronic disease in ’ ’patient’s history (cancer, autoimmune conditions, type 2 diabetes mellitus, coronary heart disease, hypertension, hypercholesterolaemia, gout) | |
| Clostridiodes difficile infection in patient’s history | |
| Colorectal carcinoma in family history | |
| Any restrictive diet habits (raw-vegans, fruitarians, keto or carnivore) | |
| Any systemic antibiotics in the last 6 months | |
| Using proton-pump inhibitors in the last 6 months | |
| Regular unprotected sex with unknown persons |
BMI, body mass index; FMT, faecal microbiota transplantation; GI, gastrointestinal.
Figure 2.
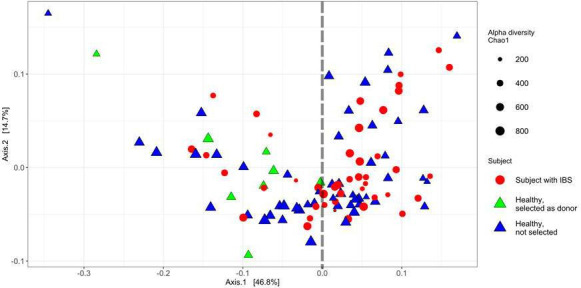
Ordination plot on the weighted UniFrac distance at the genus level for selectionof the donor candidates based on their gut microbiome alpha diversity and beta diversity. These are the results of a comparative microbiome case–control study which helped us to preselect 14 donor candidates. Alpha diversity calculation was based on Chao 1 index. The beta-diversity calculation was based on Non-Metric Dimensional Scaling (NMDS) with weighted UniFrac distance matrix for bacterial genus. NMDS axis 1 captured 46.8% of variability; NMDS axis 2 represents 14.7% of the variability. Healthy subjects were enriched in negative values of the first ordination axis; therefore, we selected donors among healthy subjects in this half of the graph and based on their microbiome’s alpha diversity. The reason for concentrating healthy and enriched subjects in the left part of the plot could be their younger age. IBS, irritable bowel syndrome.
Figure 3.
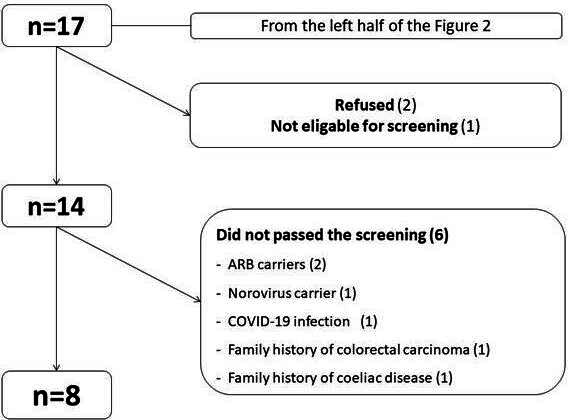
Process of donor selection and reasons for their excluding. ARB, antibiotic resistant bacteria.
After 14 potential donors were selected based on the microbiota composition, they were screened for infectious diseases and clinically examined as indicated by the European consensus conference on FMT in clinical practice guidelines14 (box 1). All subjects were also repeatedly tested for SARS-CoV-2 from both nasopharyngeal swab and stool. Six candidates were excluded (for reasons, see figure 3), whereas eight became regular stool donors. These eight donors were regularly investigated as follows:
Box 1. Laboratory screening of the FMT donors*.
Blood testing
Hepatitis A, hepatitis B, hepatitis C and hepatitis E viruses (serology)
HIV-1 and HIV-2 (p24 antigen)
Treponema pallidum (serology)
Strongyloides stercoralis (serology)
Complete blood cell count with differential
Creatinine, aminotransferases, bilirubin
Stool testing
Clostridioides difficile (cultures, antigen testing)
Common enteric pathogens, including Salmonella, Shigella, Campylobacter, shiga toxin-producing Escherichia coli, Yersinia and Vibrio cholerae (cultures)
Antibiotic-resistant bacteria (ARB), including vancomycin-resistant Enterococci, meticillin-resistant Staphylococcus aureus
Gram-negative ARB including extended-spectrum β-lactamase-producing Enterobacteriaceae, and carbapenem-resistant Enterobacteriaceae/carbapenemase-producing Enterobacteriaceae (cultures)
Norovirus, rotavirus, adenovirus, sapovirus (PCR)
SARS-CoV-2 (reverse transcription-PCR)
Common intestinal parasites, including Giardia intestinalis, Cryptosporidium parvum et hominis (cultures and PCR), Blastocystis hominis**, Dientamoeba fragilis** (both PCR only)
At every donation: by questionnaire for gastrointestinal symptoms, antibiotic usage, unprotected sex, travelling to exotic countries; clinical signs of COVID-19; the presence of SARS-CoV-2 in the donated stool.
Every 4 weeks: for SARS-CoV-2 from nasopharyngeal swab.
Every 8–12 weeks: for all other stool tests mentioned in box 1.
Prospective study participants
Patients diagnosed with IBS-D (diarrhoeal type) or IBS-M (mixed diarrhoeal and constipation type) who fulfil the inclusion and exclusion criteria listed in table 2 are recruited via regular’ patient’s check-ups at the Gastroenterological unit at Thomayer University Hospital, by referrals from their general practitioners, following our newspaper articles or word of mouth.
Table 2.
Inclusion and exclusion criteria for recipients of FMT
| Inclusion | Adults 18–65 years |
| Diagnosed with IBS-D or IBS-M according to the rome IV criteria | |
| Expected adherence to following the protocol | |
| Written consent to the study | |
| Exclusion | The use of antibiotics and probiotics within 1 month prior to faecal microbiota transplantation |
| History of inflammatory bowel disease or gastrointestinal malignancy, systemic autoimmune diseases (ongoing or in history) | |
| Previous abdominal surgery (other than appendectomy or cholecystectomyor hernioplasty or caesarean section) | |
| HIV infection or other active infection | |
| Renal or hepatic disease (both defined by biochemistry workup) | |
| Diabetes mellitus, abnormal thyroid functions not controlled by thyroid medications | |
| Bipolar disorder or schizophrenia (ongoing or history thereof), moderately severe depression defined by Patient Health Questionnaire-9 score >15 | |
| Anxiety defined by a Generalised Anxiety Disorder 7 score >10, with any organic causes that can explain the symptoms of IBS | |
| Current pregnancy and lactation |
FMT, faecal microbiota transplantation; IBS, irritable bowel syndrome.
Study microbiota mixture for intervention
The intervention microbiotais a mixture of regular stool donations from the eight regular donors. The collection of stools for this purpose is already completed. The donors were advised to regularly defecate at their home toilet into a clean plastic bag placed in Fecotainer (Excretas Medical, NL) with an Anaerogen bag (Thermo Scientific, USA). This bag generated an anaerobic atmosphere during transport to ensure anaerobes survival. The stool was transported to the laboratory with the maximum allowable time until processing being 6 hours; the actual time was approximately 1.5 hours. The stool was weighed on arrival, inspected for blood admixture and immediately processed by blending with a solution consisting of sterile 0.9% saline (160 mL per 100 g of stool), sterile phosphate buffer saline at pH 7.4 (20 mL per 100 g of stool) and sterile 99.5% glycerol (20 mL per 100 g stool, which is approximately 10% of solution’s volume; therefore, it is unlikely to have laxative properties on administration). From our experience, ~105 mL of the study mixture represents ~40 g of stool. The mixture was then filtered through a sterilestainless steel mesh of 0.8 mm pore size into a sterile plastic bottle, which was then immediately frozen at −80°C. Whenever possible (blending or postfiltration), the procedure was performed under a nitrogen atmosphere to protect obligate anaerobes. All stool portions were remixed together in a large stainless steel bucket using an electric mortar mixer under anaerobic conditions and at low temperature (on ice).
Based on the recommendation from the Nanjing consensus,15 the bacterial cell content of the study microbiota mixture was quantified. We performed a real-time PCR of the 16S rRNA gene with a standard curve derived from bacterial culture and controls from previously used stool transplants from another centre. It was estimated that the cell count in the transfer ranged between 2e+12 and 1e+13 (depending on the expected composition of the microbiota as to the 16S gene count per an average bacterial cell). Unfortunately, the Nanjing consensus15 provides neither reference to the cell counting method (box 1 therein) nor to control materials. Therefore more exact direct comparison of the requested quantities is not possible.
The mixed microbiotasubstance wasdivided into aliquots of 13–14 g (which is ~35 mL). Two-thirds of the tubes served as a placebo: they wereimmediately autoclaved at 121°C for 30 min with slow cooling. Presterilised tubes were used to ensure that autoclaved placebos would not be visually distinguishable from tubes with the active substance. Assignation of tubes to the autoclave, numbering, sealing and labelling were done under the guidance of a statistical unit member (see below).
All aliquot tubes are kept frozen at −80°C in the same type of plastic tubes, labelled by codes. Three such aliquots represent one dose for FMT (~40 g of stool, in ~105 mL). Aliquoting into multiple 50 mL tubes instead of one larger volume was decided because of the availability of durable plastic, which must be both autoclavable and deep frost resistant.
Before administering, the study microbiota mixture will be thawed in a warm (37°C) water bath, with intermittent mixing by inverting the tubes.
Randomisation, allocation and blinding
At visit 1, each patient is randomised into one of three equally sized groups (figure 1) as described in the Study design section. Randomisation assignments is generated in advance in blocks of nine and stored in a protected database. For each patient, anonymous codes for tubes containing either active study microbiota mixture or placebo is received. Thus, the true assignment will remain concealed for the patients and the study staff until the end of the study observation period. The investigator is encouraged to maintain the blind as far as possible. The actual allocation must not be disclosed to the patient and/or other study personnel including other site personnel, monitors, corporate sponsors or project office staff; nor should there be any written or verbal disclosure of the code in any of the corresponding patient documents.
Study intervention
Study substance is administered during visit 2+3 and then again 7+8 as a retention colon enema and will be held optimally for at least 30 min. Bowel preparation is applied the day before the intervention (prior to visit 2 and visit 7) (natrii picosulfas 10 mg, magnesii oxidum leve 3, 5 g, acidum citricum 12 g). No preparation is performed before the second enema in the pair (visits 3 and 8).
A rectal tube is inserted into the rectum, and the enema is applied. Application kit (Irrigator PN 0462/E/93, Erilens, Czechia) is used. After the enema is applied, the patient position is changed to enable the study substance to be spread within the colon. The exact time of the enema completion is recorded as well as the enema retention time.
Outcomes
Primary outcome
The primary outcome is the change in the IBS-SSS in the active microbiota group relative to the placebo group. The change will be evaluated as the difference between the score at 4 weeks after the intervention (study weeks 5 or 13, respectively, see figure 1) and the baseline score (week −1 in group A or week 8 in group B).
Secondary outcomes
The acute change in the IBS severity symptom score (IBS-SSS) between baseline and two weeks after intervention (study weeks 3 and 11, respectively, see Figure 1).
The long-term change in the IBS severity symptom score (IBS-SSS) between baseline (week -1) and week 32 (see Figure 1). The long term change will compare group C (placebo only) to merged groups A+B (active study microbiota mixture).
-
Following outcomes compare changes in the active microbiota group relative to the placebo group between baseline and study week 32:
Quantity of loose stools per day
Stool consistency evaluated by the Bristol Stool Scale.
Abdominal pain measured by the Visual Analogue Scale.
Frequency of bloating per week.
Body mass index in kg/m2.
Body fat mass estimated by measuring combined skinfold thickness in millimetres at given locations (biceps, triceps, subscapular, suprailiac).
Percentage of body fat mass measured by bioelectrical impedance analysis.
Waist circumference in centimetres.
The psychological and well-being effects of the therapy scored by IBS-QoL questionnaires.
The faecal microbiome’s alpha diversity measured by the Chao index.
The faecal microbiome’s beta diversity assessed by the quantitative Bray-Curtis index ordinated by non-metric multidimensional scaling.
Quantity of Blastocystis sp. assessed by a specific quantitative PCR assay measured in genomic equivalents per µL DNA.
Data collection and follow-up
Timing of assessments
At visit 1 (the randomisation), the patient is given detailed instructions and thoroughly instructed by the study team. The patients are asked to keep the identical type of diet throughout the observation. They are asked to regularly (once a week) fill the study questionnaire. A study team member sends that via the Survey Monkey smartphone application, an online survey development cloud-based software. Relevant data are entered in a structured manner (frequency of defecation, Bristol stool scale, pain measures, other symptoms, dietary records, etc). This member also frequently communicate with study participants and answer any questions regarding the study to keep the patient’s adherence. An overview of the examinations at each visit and the timing of the study visits could be seen in table 3.
Table 3.
The study visits with planned activities
| Visit | 0 | * | X | 2+3 | 4 | X | 5 | 6 | 7+8 | 9 | X | 10 | 11 |
| Study week | ? | −2 | −1 | * | † | 3 | 5 | 8 | 9 | 10 | 11 | 13 | 32 |
| Eligibility evaluation (E)/randomisation (R)/wrap-up visit (W)* | E | R | W | ||||||||||
| Colon enema with the study substance (active microbiota or placebo) | XX | XX | |||||||||||
| Irritable bowel syndrome severity scale score | X | X | X | X | X | X | X | X | |||||
| Weight, height, bioimpedance | X | X | X | X | X | X | |||||||
| Detailed anthropometry | X | X | X | X | |||||||||
| Serum workup, archiving serum+plasma | X | X | X | X | |||||||||
| Psychological evaluation | X | X | |||||||||||
| Dietary questionnaire and advice, evaluation of food records† | X | X | |||||||||||
| Stool samples for microbiome analysis | X | X | X | X | X | X | X | X | X | X | X |
*Here, the patient is offered a roll-over into an observational study with active microbiota administration. The patients will be informed of this option at the start of the study and regularly reminded.
†For IBS-SSS questionnaires assessing the primary outcome, please see the intervention scheme in figure 2. Their administering is not linked to study visits.
IBS-SSS, Irritable Bowel Syndrome Severity Symptom Score.
Irritable Bowel Syndrome Severity Scale Score
The IBS-SSS is a five-question survey that reflects (1) the severity of abdominal pain, (2) frequency of abdominal pain, (3) severity of abdominal distention, (4) satisfaction with bowel habits and (5) interference with quality of life over the past 10 days. Subjects respond to each question on a 100-point Analogue Scale; thus, the score can range from 0 to 500, with higher scores indicating more severe symptoms.16
At eligibility screening, the patients is given instructions on how to fill the IBS-SSS questionnaires (via the Survey Monkey application). The questionnaires are filled in at eligibility screening and then at week −1, 3, 5 (before the first intervention, at the presumed peak of its effect, and after further 2 weeks), then at weeks 8, 11, 13 (similarly with the second intervention), and finally at week 32.
Weight, height, bioimpedance
Bodyweight, height and bioimpedance is examined during visit 0, 1, 4, 5, 9 and 11. Medical Body Composition Analyzer Seca mBCA 515, (Seca, Germany) is used to measure changes in body composition (8-point bioelectric impedance analysis at a frequency of 5–50 kHz with a current of 100 µA), scanning performed with threepairs of hand electrodes and two pairs of leg electrodes, measurements performed with light clothing and without metal objects (jewellery, keys). The weight is determined in patients wearing underwear using the Seca mBCA 515. The height is determined by a standardised technique with a metal stadiometer with an accuracy of 1 mm. Seca analytics V.115 software is used to analyse the obtained data (Seca, Hamburg, Germany). The measurements is performed according to the NIHR (National Institute for Health and Care Research) Southampton Biomedical Research Centre standard protocol (Seca mBCA, NIHR Southampton Biomedical Research Centre, 2014).
Detailed anthropometry
It is performed by nutritional therapists in visit 1, 5, 10 and 11. It involvesweight, abdominal (waist) circumference, buttocks (hip) circumference, thigh circumference and skinfolds (thigh, triceps, subscapular, suprailiacal).
Serum workup, archiving serum +plasma
Blood is sampled at visits 0, 4, 9, 11 and will include: (A) serum+plasma archiving, (B) serum workup. Laboratory panel testing will comprise sodium, potassium, chloride, urea, creatinine, glucose, calcium, phosphate, total protein and albumin, AST (aspartate transaminase), ALT (alanine transaminase), ALP (alkaline phosphatase), GGT (gamma-glutamyl transferase), bilirubin, lipid panel, HS-CRP (high-sensitive C-reactive protein), blood cell count with differential count, INR (international normalized ratio), urine analysis (sediment and biochemistry). One plasma and one serum aliquots are made at these visits and frozen for forensic reasons.
Psychological evaluation
It is performed during visit 0 and visit 11 using a structured questionnaire evaluated by a qualified psychologist.
Dietary questionnaire and advice, evaluation of food records
It is performed by nutritional therapists at visit 4 and 9 and includes: evaluation of food records will include: overall daily energy intake, proteins, carbohydrates and lipids calculations and dietary fibre.
Gut microbiome composition
Faecal samples are collected at home by the subjects in the same way as described for donors above and at time points indicated in the sections above. If not immediately brought to the visit, the stool is frozen in a home freezer and then transported in a frozen tube container. DNA extraction is performed using the PowerSoil kit (Qiagen), and the bacteriome is characterised by 16S rDNA amplicon profiling using the tagged primers according to Schloss protocol17 and sequencing on a MiSeq instrument with the 2×250 bases sequencing kit (both Illumina, USA).
The first steps of bioinformatic analysis will be performed in the DADA2 package.18 Statistical analyses and visualisation will be then performed in R with its Phyloseq package. The functional potential of the bacteriome will be assessed using the PICRUST software, which predicts functional capabilities based on the 16S rDNA profiles.
The virome is assessed in a total of four stool samples per patient at visit 0, 4,9 and 11. The aim of this analysis is to assess the repertoire of major bacteriophages. The virome analysis is based on metagenomic sequencing of total DNA from a virus-enriched stool sample, according to the previously published protocol.19
Finally, a simple PCR-based semiquantitative parasite screening aims to identify several mostly benign unicellular parasites (eg, Blastocystis, Dientamoeba, Entamoeba, Endolimax).
Safety monitoring
All data are regularly monitored by the research team for any adverse events, and all potential adverse events are recorded. Contacts to study coordinators active 24/7 are provided in case adverse effects occur. If any concerns are identified during the screening or clinical assessment of donors or recipients, further clinical evaluation and/or examination is immediatelyrealised. All the concerns during the study are assessed, and the recipient will be withdrawn if this is thought to be in his best interest. A data monitoring and safety committee (DMSC) has been established and based on the data from the planned interim analysis, has the right to terminate the study if the frequency of severe adverse events crosses the 5% line (for a closer description of DMSC, its responsibilities and premature termination of the study see online supplemental appendix 2.
bmjopen-2021-056594supp002.pdf (177.5KB, pdf)
Sample size and power calculation
The study is powered to detect an absolute improvementof 62.5 points in IBS-SSS score over 8 weeks (which is 25% of the expected mean baseline score 250) between the active microbiota intervention compared with placebo. With asample size of 33 per group (99 total), the probability of detecting such an improvement is at least 0.9. This calculation assumes 20% drop-out rates, variance inIBS-SSS scores 100 (see the results in Palsson et al20), a correlation between the final and baseline IBS-SSS scores 0 (with a positive correlation, the power is higher), and no carry-over or temporal effect.
Data management
Data from IBS-SSS, frequency of urgent defecations, Bristol Stool Scale, abdominal pain and bloatingare collected and stored via the application Survey Monkey. All anthropometric data are entered and stored in password-protected platforms integrated within the hospital information system. Only the researchers involved in the study have access to the final study dataset (IBS-SSS, frequency of urgent defecations, Bristol stool scale, abdominal pain and bloating), which will be shared in an anonymised form via the Zenodo repository. The only data in this manuscript are bacteriome data; their anonymised form will be available on reasonable request.
Statistical analyses
The primary outcome analysis will be based on the difference in IBS-SSS scores over the second treatment period (week 14 vs week 8) minus the change over the first treatment period (week 5 vs week −1). This difference will be used as a response in a linear model, with intercept corresponding to the temporal effect (seen in the placebo group C), an indicator of group A corresponding to the cross-over effect (resulting from administration of placebo after active microbiota) and differences in indicators for groups A and B modelling the effect of active microbiota. A robust sandwich estimator of the variance matrix will be used to adjust for potentially unequal variances between the groups. Analyses of secondary outcomes will proceed by a similar methodology, comparing absolute or relative differences of the postintervention measure of each outcome relative to its baseline value. The Consolidated Standards of Reporting Trials 2010 guidelines will be followed in reporting the main trial results.
Study status
The first patient was recruited on 17 June 2021, and the first intervention was applied on 29 July 2021. As of 17 August 2021, 12 patients have signed the informed consent, and 6 interventions have been applied. It is expected that the study will be completed in December 2023.
Patient and public involvement
Information on the study has been spread at conferences, in newspapers and by local gastroenterologists contacted by researchers. Everyone interested got information material, which allowed the potential subjects to read about the study and reach the researchers if they wanted to participate. Participants were not involved in the development, recruitment of other participants or conduct of the study. All recipients are asked about any possible adverse effects of treatment at regular visits planned according to figure 1; a thorough investigation will be conducted if any occur. After completing the data analysis, all recipients will receive information about their results and be offered a roll-over (receiving an active study microbiota mixture).
Ethics and dissemination
Ethics approval for this study was granted in June 2018 by the Ethics Committee of the Institute for Clinical and Experimental Medicine and Thomayer Hospital (Vídeňská 800, 140 59 Prague 4, Czech Republic). Involvement in this study is completely voluntary; donors and recipients are required to provide written informed consent prior to participation in the study (see online supplemental appendixs 3; 4). Recipients and their caregivers are informed of unexpected findings or unrecognised conditions and by possible future usage of their specimens in ancillary studies by trained physician or nurse; further medical care will be arranged. Study donors received financial compensation to pay for the required travelling costs when donating the stool. The patient will be offered a roll-over into an observational study with the administration of active microbiota. The patients are informed of this option at the start of the study and regularly reminded.
bmjopen-2021-056594supp003.pdf (1.2MB, pdf)
bmjopen-2021-056594supp004.pdf (211.5KB, pdf)
We aim to publish findings in impact peer-reviewed international journals. Gastroenterologists, internists and other careproviders will be informed through the national conference meetings, journals and patient groups meetings.
Protocol amendment number:
01. Modification of the study protocol will be communicated to the ethics committee.
Supplementary Material
Acknowledgments
We thank Peter Holger Johnsen, Linn Skjevling and Hege Hansen from University Hospital of North Norway Harstad, Norway and Rasmus Goll from University Hospital of North Norway Tromsø, Norway, for valuable advice regarding the study design and study microbiota mixture preparation. We also thank Marcela Krutova, Jan Tkadlec, Daniela Lzicarova, Kamila Dundrova, Marie Brajerova, Milena Antuskova, Barbora Dravotova, Jana Prasilova, Jana Sumova and Ales Briksi, all from Department of Medical microbiology, 2nd Faculty of Medicine, Charles University and Motol University Hospital, Prague for their laboratory work for the microbiological screening of the study donors.
Footnotes
Contributors: OC, PK, JH, JV and MK contributed to the conception and design of the study. OC, PK, JH and JV drafted the protocol with input from all other authors. JV and PK contributed to the patients recruitment. JH, LV, LK and OC contributed to the microbiome analysis for donor selection. JH, OC and JV contributed to the donor screening. LV, JH and OC contributed to the study microbiota mixture preparation. MK contributed to the power size calculations and statistical analysis. VL contributed to the randomisation. JH and JV contributed equally to writing this paper, OC and PK are last authorship.
Funding: This research received funding from the Ministry of Health of the Czech Republic, grant Nr. 19-01-00127. Funding received from this grant support direct research cost. All rights reserved.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
References
- 1.Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology 2016;150:1393–407. 10.1053/j.gastro.2016.02.031 [DOI] [PubMed] [Google Scholar]
- 2.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 2012;10:712–21. 10.1016/j.cgh.2012.02.029 [DOI] [PubMed] [Google Scholar]
- 3.Rajilić-Stojanović M, Jonkers DM, Salonen A, et al. Intestinal microbiota and diet in IBS: causes, consequences, or epiphenomena? Am J Gastroenterol 2015;110:278–87. 10.1038/ajg.2014.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly CP. Fecal microbiota transplantation--an old therapy comes of age. N Engl J Med 2013;368:474–5. 10.1056/NEJMe1214816 [DOI] [PubMed] [Google Scholar]
- 5.Johnsen PH, Hilpüsch F, Cavanagh JP, et al. Faecal microbiota transplantation versus placebo for moderate-to-severe irritable bowel syndrome: a double-blind, randomised, placebo-controlled, parallel-group, single-centre trial. Lancet Gastroenterol Hepatol 2018;3:17–24. 10.1016/S2468-1253(17)30338-2 [DOI] [PubMed] [Google Scholar]
- 6.El-Salhy M, Hatlebakk JG, Gilja OH, et al. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut 2020;69:859–67. 10.1136/gutjnl-2019-319630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halkjær SI, Christensen AH, Lo BZS, et al. Faecal microbiota transplantation alters gut microbiota in patients with irritable bowel syndrome: results from a randomised, double-blind placebo-controlled study. Gut 2018;67:2107–15. 10.1136/gutjnl-2018-316434 [DOI] [PubMed] [Google Scholar]
- 8.Aroniadis OC, Brandt LJ, Oneto C, et al. Faecal microbiota transplantation for diarrhoea-predominant irritable bowel syndrome: a double-blind, randomised, placebo-controlled trial. Lancet Gastroenterol Hepatol 2019;4:675–85. 10.1016/S2468-1253(19)30198-0 [DOI] [PubMed] [Google Scholar]
- 9.Holster S, Lindqvist CM, Repsilber D, et al. The effect of allogenic versus autologous fecal microbiota transfer on symptoms, visceral perception and fecal and mucosal microbiota in irritable bowel syndrome: a randomized controlled study. Clin Transl Gastroenterol 2019;10:e00034. 10.14309/ctg.0000000000000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lahtinen P, Jalanka J, Hartikainen A, et al. Randomised clinical trial: faecal microbiota transplantation versus autologous placebo administered via colonoscopy in irritable bowel syndrome. Aliment Pharmacol Ther 2020;51:1321–31. 10.1111/apt.15740 [DOI] [PubMed] [Google Scholar]
- 11.Holvoet T, Joossens M, Vázquez-Castellanos JF, et al. Fecal microbiota transplantation reduces symptoms in some patients with irritable bowel syndrome with predominant abdominal bloating: short- and long-term results from a placebo-controlled randomized trial. Gastroenterology 2021;160:145–57. 10.1053/j.gastro.2020.07.013 [DOI] [PubMed] [Google Scholar]
- 12.Wu J, Lv L, Wang C. Efficacy of fecal microbiota transplantation in irritable bowel syndrome: a meta-analysis of randomized controlled trials. Front Cell Infect Microbiol 2022;12:827395. 10.3389/fcimb.2022.827395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chan A-W, Tetzlaff JM, Altman DG, et al. Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cammarota G, Ianiro G, Kelly CR, et al. International consensus conference on stool banking for faecal microbiota transplantation in clinical practice. Gut 2019;68:2111–21. 10.1136/gutjnl-2019-319548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nanjing consensus on methodology of washed microbiota transplantation. Chin Med J 2020;133:2330–2. 10.1097/CM9.0000000000000954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. 10.1046/j.1365-2036.1997.142318000.x [DOI] [PubMed] [Google Scholar]
- 17.Kozich JJ, Westcott SL, Baxter NT, et al. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the MiSeq Illumina sequencing platform. Appl Environ Microbiol 2013;79:5112–20. 10.1128/AEM.01043-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Callahan BJ, McMurdie PJ, Rosen MJ, et al. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods 2016;13:581–3. 10.1038/nmeth.3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kramná L, Cinek O. Virome sequencing of stool samples. Methods Mol Biol 2018;1838:59–83. 10.1007/978-1-4939-8682-8_6 [DOI] [PubMed] [Google Scholar]
- 20.Palsson OS, Baggish JS, Turner MJ, et al. Ibs patients show frequent fluctuations between loose/watery and hard/lumpy stools: implications for treatment. Am J Gastroenterol 2012;107:286–95. 10.1038/ajg.2011.358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stensvold CR, van der Giezen M. Associations between gut microbiota and common luminal intestinal parasites. Trends Parasitol 2018;34:369–77. 10.1016/j.pt.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 22.Hurych J, Vodolanova L, Vejmelka J, et al. Freezing of faeces dramatically decreases the viability of Blastocystis sp. and Dientamoeba fragilis. Eur J Gastroenterol Hepatol 2022;34:242–3. 10.1097/MEG.0000000000002327 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056594supp001.pdf (71.3KB, pdf)
bmjopen-2021-056594supp002.pdf (177.5KB, pdf)
bmjopen-2021-056594supp003.pdf (1.2MB, pdf)
bmjopen-2021-056594supp004.pdf (211.5KB, pdf)


