Abstract
Objective
To estimate the costs of scaling up the HEARTS pilot project for hypertension management and risk-based cardiovascular disease (CVD) prevention at the full population level in the four subdistricts (upazilas) in Bangladesh.
Settings
Two intervention scenarios in subdistrict health complexes: hypertension management only, and risk-based integrated hypertension, diabetes, and cholesterol management.
Design
Data obtained during July–August 2020 from subdistrict health complexes on the cost of medications, diagnostic materials, staff salaries and other programme components.
Methods
Programme costs were assessed using the HEARTS costing tool, an Excel-based instrument to collect, track and evaluate the incremental annual costs of implementing the HEARTS programme from the health system perspective.
Primary and secondary outcome measures
Programme cost, provider time.
Results
The total annual cost for the hypertension control programme was estimated at US$3.2 million, equivalent to US$2.8 per capita or US$8.9 per eligible patient. The largest cost share (US$1.35 million; 43%) was attributed to the cost of medications, followed by the cost of provider time to administer treatment (38%). The total annual cost of the risk-based integrated management programme was projected at US$14.4 million, entailing US$12.9 per capita or US$40.2 per eligible patient. The estimated annual costs per patient treated with medications for hypertension, diabetes and cholesterol were US$18, US$29 and US$37, respectively.
Conclusion
Expanding the HEARTS hypertension management and CVD prevention programme to provide services to the entire eligible population in the catchment area may face constraints in physician capacity. A task-sharing model involving shifting of select tasks from doctors to nurses and local community health workers would be essential for the eventual scale-up of primary care services to prevent CVD in Bangladesh.
Keywords: program cost, hearts hypertension management and cvd prevention program, scale-up of primary care services, bangladesh
Strengths and limitations of this study.
This study uses the HEARTS costing tool to assess the expected cost of scaling up the programme to all eligible adults in the participating subdistricts (upazila).
The study assesses two programme scenarios: a hypertension management programme and an integrated risk-based hypertension, diabetes and cholesterol management programme.
The study disaggregates costs by function, identifying areas for efficiency improvements, such as task-sharing and bridging programme delivery from the upazila level to more localised community facilities.
Due to lack of data at a local level, the cost projections rely on assumptions regarding population coverage, risk factor prevalence, primary care attendance rate, distribution of cardiovascular disease (CVD) risk among the population, distribution of patients by treatment protocols and frequency of patient visits by CVD risk.
The study uses average medicine prices, unit costs of supplies, wages and provider time, which may vary across subdistricts depending on the procurement arrangements and operational efficiency.
Background
Hypertension is a major and preventable risk factor for cardiovascular disease (CVD). An estimated 1.13 billion people (1 in 4 men and 1 in 5 women) worldwide have hypertension.1 Among people with hypertension worldwide, fewer than one in five have it under control.1 High blood pressure (BP) is a leading global risk factor for premature death and disability, accounting for about 10 million (or 1 in 6) deaths worldwide each year.2 3 Uncontrolled hypertension significantly increases the risk of stroke, myocardial infarction, heart failure, dementia, renal failure, retinopathy and other diseases.4–7 Almost half of all CVD events are attributable to uncontrolled hypertension.2 3
Reducing the prevalence of hypertension is a standing global health objective.8–11 This objective complements the 2030 Sustainable Development Goal of reducing premature deaths from non-communicable diseases (NCDs) by 25%.12 Low-income and middle-income countries (LMICs), where two-thirds of all hypertension cases reside, are increasingly cognizant of the long-term benefits of addressing hypertension in their populations. However, implementing population-level measures targeting hypertension may present challenges for many LMICs where health systems have traditionally focused on infectious diseases and where the capacity for NCD care may be limited.
Bangladesh is among lower-middle-income countries with a high burden of hypertension. In 2018, the prevalence of elevated BP (SBP and/or DBP ≥ 140/90 mm Hg) among adults in Bangladesh was 21%.13–15 According to the 2011 Bangladesh National Demographic and Health Survey, of 14.4 million hypertensive people (adults aged 35 and above), only 7.3 million (51%) were aware of their condition, 41% were treated and 18% had their BP levels under control.16 The burden of hypertension in Bangladesh is expected to grow alongside increased population ageing, rapid urbanisation with commensurate increases in sedentary lifestyle and processed food consumption, and other socioeconomic and lifestyle changes. However, only less than 5% of the health sector programme budget is allocated for NCDs control.16 This demonstrates the need for an effective, low-cost and efficient population-level approach in addressing hypertension.
In 2016, WHO introduced the HEARTS technical package as a framework for CVD prevention at the primary care level.17 The HEARTS technical package consists of guidelines for implementing a primary care approach to CVD management, focusing on screening and management of CVD risk factors, including lifestyle modification and pharmacological treatment of metabolic risk factors such as hypertension, diabetes and hyperlipidaemia. In this paper, we describe the local budgetary impact of implementing the HEARTS programme at the population level for four subdistricts in Bangladesh, based on programme cost data obtained from a representative healthcare facility in each subdistrict. Although the initial focus of the programme in the four subdistricts is presently limited to hypertension control, scaling-up of the initiative may include screening, diagnosis and treatment of diabetes and high cholesterol. Understanding the cost drivers of CVD prevention approaches in the Bangladesh primary care system can support budgeting, procurement, evaluation and planning for scale-up.
Methods
Setting
In 2018, the Directorate General of Health Services and the National Heart Foundation of Bangladesh collaborated with Resolve to Save Lives (an initiative of Vital Strategies, a non-profit global public health organisation) to implement a pilot programme to strengthen the detection, treatment and follow-up management of hypertension in primary care. The programme was introduced in four health complexes in four subdistricts (upazilas) in the Sylhet district: Golapganj, Fenchuganj, Beanibazar and Bishwanath. In Bangladesh, hospitals and health facilities that are in the subdistrict (upazila) level or below are termed as primary health complexes. A typical upazila health complex is a 50-bed hospital with service coverage in the range of 100 000–400 000 population and plays a pivotal role in the provision of primary healthcare through a three-tier system consisting of the ward level, union level and upazila level. The upazila health complex performs a wide range of functions that includes prevention, promotion, treatment (inpatient, outpatient, limited diagnostic services), management, technical support, training, coordination and patient referral services. The outpatient service is usually staffed with five outpatient general practitioners including one resident medical officer, two medical officers and two medical assistants. An ‘NCD corner’ was set up in the outpatient with necessary logistics and personnel for screening and treatment. We project programme costs under two intervention scenarios: a hypertension-focused programme, and a risk-based integrated hypertension, diabetes and cholesterol management programme.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
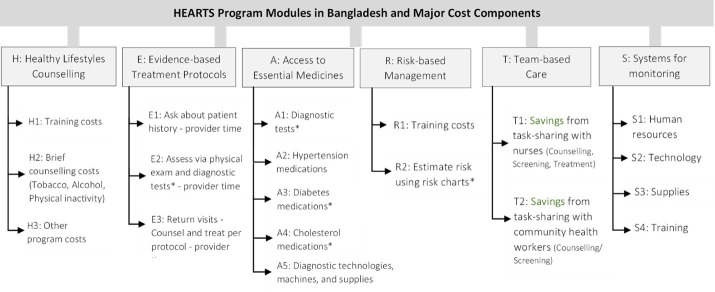
Hypertension management program
The HEARTS Technical Package for CVD prevention in primary care is organised around six modules: H–Healthy-lifestyle counselling, E—Evidence-based treatment protocols, A—Access to essential medicines and technology, R—Risk-based CVD management, T—Team-based Care and S—Systems for monitoring.18 Components of these modules are described in figure 1. In the four upazila primary care complexes in Bangladesh, programmed activities included: training of staff in following a standard treatment protocol, record keeping and reporting; ensuring adequate supply of necessary drugs; community outreach to increase awareness of the need for hypertension screening; introduction of patient monitoring tools and a monthly reporting system; and establishing a mechanism for patient referral from primary care to secondary care and tertiary care at MAG Osmani Medical College. The clinical management protocol for adults with hypertension (defined as systolic blood pressure (SBP)/diastolic blood pressure (DBP)≥140/90 mm Hg, or SBP/DBP≥130/80 mm Hg with comorbidity or high CVD-risk) entailed a first line of treatment with amlodipine 5 mg daily; a second line of treatment using amlodipine 5 mg plus losartan 50 mg daily; and a third line of treatment using amlodipine 5 mg plus losartan 50 mg plus hydrochlorothiazide 12.5 mg daily. Online supplemental appendix 1 depicts the hypertension treatment protocol. The prescribed medicines are typically obtained by public health facilities, generic, domestically manufactured and provided free of charge to patients. The national drug policy recommends that 70% of the public sector medicines be purchased from the state-owned Essential Drug Company Limited (EDCL), 25% from the Central Medical Stores Depot (CMSD) and 5% from local sources.19 20 In order to provide continuous care more sustainably and to reduce burden on physicians, a team-based care strategy was implemented. The healthcare providers were trained to acquire the necessary skills to provide brief interventions to record patients’ medical history, measuring BP, point-of-care testing to assess fasting blood glucose and cholesterol levels and urine dipstick for proteinuria, encourage behaviour change, assess CVD risk or initiate treatment protocol. The training sessions were conducted in one setup with a pool of selected doctors, nurses and community health workers (CHWs) trained with relevant modules. In this approach, CHWs were trained to provide counselling and some screening services along with the doctors and nurses. For the costing estimate, equal burden sharing in terms of provider time was assumed.
Figure 1.
Cost components of the HEARTS programme in Bangladesh.
bmjopen-2022-061467supp001.pdf (565.9KB, pdf)
Risk-based integrated hypertension, diabetes and hyperlipidaemia management programme
To further strengthen CVD prevention, the HEARTS programme in Bangladesh also planned to integrate diabetes and hyperlipidaemia management in addition to hypertension management in primary care patients. The programme entails assessment of target population by total CVD risk estimation to categorise their risk for CVD. The risk stratification is based on WHO and International Society of Hypertension cardiovascular risk prediction charts and expressed as the probability of developing CVD over 10 years: low CVD risk (0 to <10%); medium CVD risk (10% to 20%) and high CVD risk (≥20%).21 The treatment protocol for patients with uncomplicated type two diabetes (defined as fasting plasma glucose ≥ 7.0 mmol/L or routine plasma glucose ≥ 11.1 mmol/L or HbA1C ≥ 6.5%) managed at the primary care level included metformin (500 mg), metformin (1000 mg), then metformin (1000 mg) and gliclazide (80 mg) as the first, second and third lines of treatments, respectively. The protocol is based on the WHO guidance on diagnosis, classification and management of diabetes (HEARTS - D), which is aligned with the WHO Package of Essential Noncommunicable Disease Interventions in Primary Healthcare.22 For managing plasma lipid levels (ie, high cholesterol), the use of statins as the primary therapy is widely recommended, however, the WHO is yet to offer any specific guidance.23 For costing, the local consultants and experts proposed a statin-based treatment protocol for hyperlipidaemia including simvastatin (10 mg) as first, atorvastatin (20 mg) as second and atorvastatin (40 mg) as the third line of treatment. Costs associated with implementing integrated hypertension, diabetes and hyperlipidaemia treatment protocols include provider time spent on estimating CVD risk using risk charts during an annual primary care visit; training in CVD risk estimation, in addition to time spent collecting patient history; medication costs and diagnostic test costs including provider (technician) time, complete blood count panel, fasting blood glucose and blood lipid panel tests.
HEARTS costing tool
Programme costs were assessed using the HEARTS costing tool, an Excel-based instrument to collect, track and evaluate the incremental annual cost of implementing the HEARTS programme from the health system perspective. The tool is organised by HEARTS modules.24 In July–August 2020, we obtained unit costs from four upazila complexes and used these to project annual resource needs for implementing the CVD prevention programme at the subdistrict population level. The researchers completed in-person collection of data from the four facilities on human resource and time costs, diagnostic prices, time-motion on laboratory diagnostics, market price of medicines and others.
Figure 1 shows major cost categories within HEARTS modules. Once programme costs and other inputs such as population coverage, risk factor prevalence and planned provider numbers were entered into the costing tool, the cost calculations were allocated across different HEARTS modules.
The cost elements in the Healthy-lifestyle counselling module ‘H’ included costs of training providers in lifestyle counselling and costs of community awareness programmes and training. Counselling is based on the Assess, Advise, Agree, Assist, Arrange model, which is an evidence-based approach for promoting healthy behavioural changes to prevent NCD risk factors.25 26 Total provider time to administer brief counselling was equal to the average time that the health provider spends to counsel a patient to change behaviour multiplied by the total number of patients who would receive counselling. The cost of total provider time was calculated as the total provider time, multiplied by the weighted average salary of the health providers who have been trained to provide counselling.
The cost elements in module ‘E’ included provider time devoted to assessing patient history, conducting physical exams and diagnostic tests, and return visits. The costs of diagnostic tests (complete blood count panel, blood lipid panel, fasting blood glucose), medications (hypertension, diabetes and cholesterol) and on-site diagnostic technologies and supplies were assessed under module ‘A’. Module ‘R’ reports the costs of training providers in conducting risk-based management and the cost of provider time for estimating patient CVD risk using risk charts. Module ‘T’ reports cost savings from task-sharing by comparing the cost that could have been incurred if the tasks were performed solely by the physicians with costs incurred through task-sharing among physicians, nurses and CHW. Therefore, in the baseline scenario (ie, in the absence of task-sharing allocation), the costing tool assumes a physician-led programme. In our cost projections, we assumed that doctors, nurses and CHWs will equally share the tasks (ie, provider time) when applicable. For instance, CHWs would only provide behavioural counselling and screening service, but they would not assess CVD risk (using risk-cart), or prescribe patients with pharmacologic treatments. Accordingly, the provider time allocated for behaviour counselling and screening will be shared equally among doctors, nurses and CHWs. Nurses will be trained to do major tasks (ie, counselling, screening and assessing CVD risk, and treating according to CVD risk), therefore, providers’ time for performing hypertension/CVD risk-assessment, prescribing suitable treatment and return-visits were allocated equally between doctors and nurses. While the ‘T’ module reports the cost savings from team-based care, the accrued cost of provider time (inclusive of doctors, nurses and CHWs) spent on various tasks is included in the corresponding ‘H’, ‘E’ and ‘R’ modules. Module ‘S’ reports costs related to human resources, technology (software and hardware), supplies and training for patient monitoring.
Data
Data on salaries of government healthcare providers and programme staff were collected from in-person interviews and/or records. Total salary was calculated according to the Government of Bangladesh National pay scale. Size of the population in the examined subdistricts was obtained from census and imputed based on Bangladesh Bureau of Statistics estimates. Other population parameters (eg, primary care attendance rate and risk factor prevalence) were obtained from the nationally representative NCD Risk Factor Survey 2018.15 Medicine prices were collected from the medicine outlets in the public hospitals. The unit prices represent the average price of domestically manufactured generic medicines procured by health facilities from EDCL or CMSD. Prices of laboratory diagnostics were collected from diagnostic labs at the district (Sylhet district) and subdistrict (upazila) levels. Data on time needed to conduct laboratory tests were collected from in-person interviews of laboratory personnel. Training data, including number of training and participants, per-diem costs of staff, costs related to rent, transport, refreshments and other logistics, were collected from the respective project records.
Table 1 presents the prevalence of CVD risk factors as well as cost inputs used to populate the HEARTS costing tool. Fifteen per cent of the adult population was estimated to be at medium and high risk for CVD. The leading risk factors were tobacco use (43.7%), hyperlipidaemia (28.4%) and hypertension (21%), followed by physical inactivity (12.3%), diabetes (8.3%) and alcohol consumption (4.4%); The primary care attendance rate was assumed to be 47.9% in each upazila.15 The distributions of patients by CVD risks and for the pharmacological treatment of hypertension, diabetes and cholesterol by different treatment lines were adopted from the literature and/or based on local physician consensus.27–30 Local currency was converted to US dollars using the Bangladesh Bank official conversion rate in June 2020.
Table 1.
Costing inputs and unit costs
| Input description | Units | Value |
| Eligible population (adult population, age 18+) | ||
| Golapganj | Persons | 261 098 |
| Fenchuganj | Persons | 86 503 |
| Beanibazar | Persons | 209 454 |
| Bishwanath | Persons | 192 075 |
| Primary healthcare attendance rate (annual) | Per cent | 47.9% |
| Adult population with risk factors | ||
| Use of tobacco products | Per cent | 43.7% |
| Hazardous or harmful use of alcohol | Per cent | 4.4% |
| Physical inactivity | Per cent | 12.3% |
| Hypertension (≥140/90 mm Hg) | Per cent | 21.0% |
| Diabetes (≥7.0 mmol/L or 126 mg/dL) | Per cent | 8.3% |
| Hyperlipidaemia (≥6 mmol/L or 190 mg/dL) | Per cent | 28.4% |
| Low CVD risk (0 to <10%) | Per cent | 85.1% |
| Medium CVD risk (10 to <20%) | Per cent | 14.4% |
| High CVD risk (≥20%) | Per cent | 0.5% |
| Annual wage (in LCU (BDT) and USD, including benefits) | ||
| Doctors | BDT (USD)/year | 1 399 452 (16 484) |
| Nurses | BDT (USD)/year | 726 360 (8555) |
| CHWs | BDT (USD)/year | 486 568 (5731) |
| Lab technicians | BDT (USD)/year | 576 720 (6793) |
| Accountant | BDT (USD)/year | 576 720 (6793) |
| Administrative assistant | BDT (USD)/year | 446 242 (5256) |
| Clerical officer | BDT (USD)/year | 446 242 (5256) |
| Custodian | BDT (USD)/year | 446 242 (5256) |
| IT personnel | BDT (USD)/year | 446 242 (5256) |
| Programme director | BDT (USD)/year | 1 399 452 (16 484) |
| Programme manager | BDT (USD)/year | 726 300 (8555) |
| Secretary | BDT (USD)/year | 446 242 (5256) |
| Security officer | BDT (USD)/year | 400 196 (4714) |
| Pharmacist/chemist | BDT (USD)/year | 576 720 (6,793) |
| Statistician | BDT (USD)/year | 576 720 (6793) |
| Supplies manager | BDT (USD)/year | 486 568 (5731) |
| Purchasing price (in LCU (BDT) and USD) of pharmaceutical drugs | ||
| Hypertension medicine | ||
| Amlodipine 5 mg | BDT (USD)/tablet | 1 (0.012) |
| Losartan 50 mg | BDT (USD)/tablet | 8 (0.094) |
| Hydrochlorothiazide | BDT (USD)/tablet | 0.35 (0.004) |
| Diabetes medicine | ||
| Metformin 500 mg | BDT (USD)/tablet | 4 (0.047) |
| Metformin 1000 mg | BDT (USD)/tablet | 9 (0.106) |
| Gliclazide | BDT (USD)/tablet | 3.5 (0.041) |
| Cholesteror medicine | ||
| Simvastatin 10 mg | BDT (USD)/tablet | 7 (0.082) |
| Atorvastatin 20 mg | BDT (USD)/tablet | 10 (0.118) |
| Atorvastatin 40 mg | BDT (USD)/tablet | 28 (0.330) |
| Purchasing price (in LCU) of diagnostic tests | ||
| Diabetes (complete blood count panel) | BDT (USD)/test | 400 (4.71) |
| Diabetes (fasting blood glucose) | BDT (USD)/test | 120 (1.41) |
| Diabetes and cholesterol (blood lipid panel) | BDT (USD)/test | 800 (9.42) |
| Counselling patients to change behaviour | ||
| Time to counsel a patient to change behaviour | Minutes | 10 |
| # of 'How to quit' informational materials disseminated per person, annually (print) | 5 | |
| Cost of 'How to quit' informational materials, per unit (print materials) | BDT (USD)/print | 20 (0.24) |
| LCU to USD exchange rate | BDT/USD | 84.9 |
| ‘Safety stock’ required to be on hand for medicines | Percent | 3.0 |
| No of health providers in need of training | ||
| Counsel patients to change behaviour | Persons | 30 |
| Assess patients' total CVD risk | Persons | 10 |
| Training to counsel patients to change behaviour (5A’s)* | ||
| Classroom size | Persons | 30 |
| Hours of training needed | Persons | 16 |
| Training to screen/diagnosis/treat patients hypertension/CVD patients | ||
| Classroom size | Persons | 30 |
| Hours of training needed | Persons | 8 |
| No of trainers | ||
| Professional trainer(s) | Persons | 2 |
| Administrative staff | Persons | 1 |
| Input costs for training | ||
| Hourly wage | ||
| Professional trainer | BDT (USD)/hour | 500 (5.89) |
| Administrative staff | BDT (USD)/hour | 250 (2.94) |
| Per unit cost of materials | ||
| Instructive handbooks | BDT (USD)/book | 1000 (11.8) |
| Facility rental for training (1 day) | BDT (USD)/day | 9000 (106) |
| Refreshments | BDT (USD)/day | 6000 (70.7) |
| Per diem for staff | BDT (USD)/day | 3500 (41.2) |
| Per diem and/or salary of trainees | BDT (USD)/day | 5000 (58.9) |
| Transportation stipend for staff | BDT (USD)/training | 3165 (37.3) |
| CVD risk screening and diagnosis | ||
| Time (in minutes) a health provider spends to: | ||
| Screen patients for total CVD risk | Minutes | 5 |
| Provide a physical exam to assess patients' total CVD risk | Minutes | 5 |
| Assess patient risk using a CVD risk chart | Minutes | 5 |
| Time (in minutes) a lab technician spends to: | ||
| Administer and analyse a blood test | Minutes | 10 |
| Administer and analyse a urine test | Minutes | 10 |
| Treatment for high CVD risk | ||
| # follow-up visits for a person annually with the following levels of CVD risk annually | ||
| Low CVD risk (≥0% to <10%) | Visits | 2 |
| Medium CVD risk (≥10% to <20%) | Visits | 3 |
| High CVD risk (≥20%) | Visits | 4 |
| Time health providers spend with a patient during a visit? | ||
| Generalists/primary care doctors | Minutes | 5 |
| Nurses | Minutes | 5 |
| Screen for CVD risk: Diagnostics cost in LCU (BDT) and USD | ||
| Diabetes (compete blood count panel) | BDT (USD)/test | 400 (4.7) |
| Diabetes (fasting blood glucose) | BDT (USD)/test | 120 (1.4) |
| Diabetes and cholesterol (blood lipid panel) | BDT (USD)/test | 80 (0.9) |
| Pharmacological treatment for hypertension | ||
| Hypertension Protocol Step #1 (Amlodipine 5 mg, 1 per day, 365 days) | ||
| % of all individuals with high blood pressure who receive this treatment regimen | Percent | 62% |
| Hypertension protocol step #2 (Amlodipine 5 mg+Losartan 50 mg) | ||
| % of all individuals with high blood pressure who receive this treatment regimen | Percent | 34% |
| Hypertension protocol step #3 (Amlodipine +Losartan+ Hydrochlorothiazide) | ||
| % of all individuals with high blood pressure who receive this treatment regimen | Percent | 4% |
| Unit price of amlodipine 5 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 1 (0.012) |
| Unit price of losartan 50 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 8 (0.094) |
| Unit price of hydrochlorothiazide in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 0.35 (0.004) |
| Pharmacological treatment for diabetes | ||
| Diabetes protocol step #1 (metformin 500 mg) | ||
| % of all individuals with diabetes who receive this treatment regimen | Percent | 75% |
| Diabetes protocol step #2 (metformin 1000 mg) | ||
| % of all individuals with diabetes who receive this treatment regimen | Percent | 15% |
| Diabetes protocol step #3 (metformin 1000 mg+gliclazide 8 mg) | ||
| % of all individuals with diabetes who receive this treatment regimen | Percent | 10% |
| Unit price of metformin 500 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 4 (0.047) |
| Unit price of metformin 1000 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 9 (0.106) |
| Unit price of gliclazide 80 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 3.5 (0.041) |
| Pharmacological treatment for high cholesterol (default regimens) | ||
| High cholesterol protocol step #1 (low intensity, simvastatin 10 mg) | ||
| Percent of all individuals with high cholesterol who receive this treatment | Percent | 85% |
| High cholesterol protocol step #2 (moderate intensity, atorvastatin 20 mg) | ||
| Percent of all individuals with high cholesterol who receive this treatment | Percent | 10% |
| High cholesterol protocol step #3 (high intensity, atorvastatin 40 mg) | ||
| Percent of all individuals with high cholesterol who receive this treatment | Percent | 5% |
| Unit price of simvastatin 10 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 7 (0.082) |
| Unit price of simvastatin 20 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 10 (0.118) |
| Unit price of atorvastatin 40 mg in LCU (Taka or BDT) and USD | BDT (USD)/tablet | 28 (0.330) |
*The ‘5A’ model is an evidence-based approach entailing health behaviour change counselling to prevent NCD risk factors in primary care setting.25 26
5A’s, Assess, Advise, Agree, Assist, Arrange; BDT, Bangladesh Taka; CHWs, community health workers; CVD, cardiovascular disease; LCU, Local currency unit; NCD, non-communicable disease.
Results
Population coverage
The total population in the four subdistricts was 1.12 million, of which 749 000 were adults aged 18 and above (table 2). The total number of people eligible to receive counselling, screening, diagnosis and treatment under the two types of HEARTS intervention packages (ie, hypertension control and risk-based integrated approach) in the four subdistricts was determined by the primary care attendance rate, the prevalence of low-CVD, medium-CVD and high-CVD risk in the population, the prevalence of hypertension, diabetes and high cholesterol. The estimated number of eligible persons in the catchment area of the four subdistricts was 359 000, of which 305 000, 52 000 and 1800 were projected to be low-CVD, medium-CVD and high-CVD risk patients. The estimated number of persons undergoing treatment for hypertension, diabetes and high cholesterol was 75 000, 30 000 and 102 000, respectively (table 2). Unit costs and other cost inputs were applied to these population parameters to project total programme costs.
Table 2.
Population coverage: care cascade for counselling, screening, diagnosis and treatment
| Golapganj | Fenchuganj | Beanibazar | Bishwanath | Total | |
| Total population | 390 688 | 129 436 | 313 412 | 287 404 | 1 120 940 |
| Adult population in need (18+ years) | 261 098 | 86 503 | 209 454 | 192 075 | 749 130 |
| Adults who present at the health centre | 125 066 | 41 435 | 100 328 | 92 004 | 358 833 |
| Providing brief counselling | |||||
| Eligible to receive brief advice | 125 066 | 41 435 | 100 328 | 92 004 | 358 833 |
| Tobacco user | 54 654 | 18 107 | 43 844 | 40 206 | 156 810 |
| Harmful alcohol | 5503 | 1823 | 4414 | 4048 | 15 789 |
| Physical inactivity | 15 383 | 5096 | 12 340 | 11 316 | 44 136 |
| Screening and diagnosis of 10 year CVD risk | |||||
| Low CVD risk | 106 431 | 35 261 | 85 380 | 78 295 | 305 367 |
| Medium CVD risk | 18 009 | 5967 | 14 447 | 13 249 | 51 672 |
| High CVD risk | 625 | 207 | 502 | 460 | 1794 |
| Treatment of 10-year CVD risk | |||||
| Low CVD risk | 106 431 | 35 261 | 85 380 | 78 295 | 305 367 |
| Hypertension | 22 351 | 7405 | 17 930 | 16 442 | 64 127 |
| Diabetes | 8834 | 2927 | 7087 | 6499 | 25 345 |
| Cholesterol | 30 226 | 10 014 | 24 248 | 22 236 | 86 724 |
| Medium CVD risk | 18 009 | 5967 | 14 447 | 13 249 | 51 672 |
| Hypertension | 3782 | 1253 | 3034 | 2782 | 10 851 |
| Diabetes | 1495 | 495 | 1199 | 1100 | 4289 |
| Cholesterol | 5115 | 1695 | 4103 | 3763 | 14 675 |
| High CVD risk | 625 | 207 | 502 | 460 | 1794 |
| Hypertension | 131 | 44 | 105 | 97 | 377 |
| Diabetes | 52 | 17 | 42 | 38 | 149 |
| Cholesterol | 178 | 59 | 142 | 131 | 510 |
Risk factors and disease prevalence rates were assumed uniform across subdistricts.
CVD, cardiovascular disease.
Hypertension management programme cost
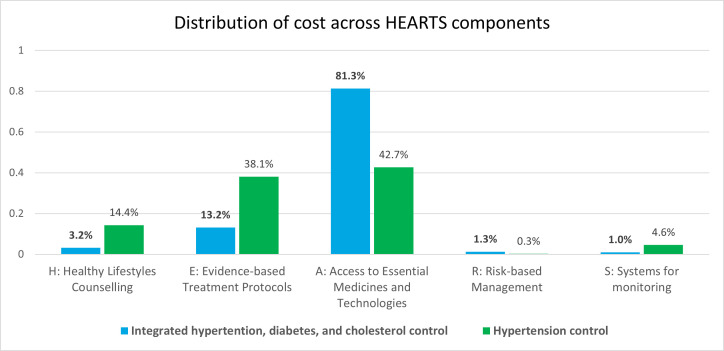
Table 3 reports the estimated annual costs, in 2020 USD and Bangladesh Taka (BDT), of implementing the HEARTS hypertension management programme in four upazilas at the population level (adults aged 18 and above). Figure 2 presents the distribution of costs by HEARTS components and subcomponents. The total annual cost was estimated at US$3.2 million, equivalent to US$2.8 per capita, US$4.3 per adult and US$8.9 per eligible participant. Module ‘A’ (Access to medicines and technology) constitutes the largest cost share (US$1.36 million; 43%), followed by module ‘E’ (Evidence-based treatment protocols; US$1.22 million; 38%). The projected medication expenditure per patient treated with medications for hypertension was US$18.
Table 3.
Total annual cost of HEARTS hypertension control programme in four subdistricts
| Golapganj | Fenchuganj | Beanibazar | Bishwanath | Total | ||||||
| BDT | USD | BDT | USD | BDT | USD | BDT | USD | BDT | USD | |
| H: Healthy lifestyles | 13 335 339 | 157 071 | 4 765 107 | 56 126 | 10 800 324 | 127 212 | 9 947 252 | 117 164 | 38 848 022 | 457 574 |
| H1: Training costs | 418 990 | 4935 | 418 990 | 4935 | 418 990 | 4935 | 418 990 | 4935 | 1 675 960 | 19 740 |
| H1.1: Facility rental (% of H1) | 18 000 | 212 | 18 000 | 212 | 18 000 | 212 | 18 000 | 212 | 72 000 | 848 |
| H1.2: Human resources | 20 000 | 236 | 20 000 | 236 | 20 000 | 236 | 20 000 | 236 | 80 000 | 942 |
| H1.3: Instructive handbooks | 35 000 | 412 | 35 000 | 412 | 35 000 | 412 | 35 000 | 412 | 140 000 | 1649 |
| H1.4: Per diem/transportation | 339 990 | 4005 | 339 990 | 4005 | 339 990 | 4005 | 339 990 | 4005 | 1 359 960 | 16 018 |
| H1.5: Refreshments | 6000 | 71 | 6000 | 71 | 6000 | 71 | 6000 | 71 | 24 000 | 283 |
| H2: Brief counselling costs | 12 816 349 | 150 958 | 4 246 117 | 50 013 | 10 281 334 | 121 099 | 9 428 262 | 111 051 | 36 772 062 | 433 122 |
| H2.1: Tobacco | 9 272 756 | 109 220 | 3 072 108 | 36 185 | 7 438 647 | 87 617 | 6 821 441 | 80 347 | 26 604 952 | 313 368 |
| Provider time to administer 5A’s | 3 807 374 | 44 845 | 1 261 401 | 14 857 | 3 054 293 | 35 975 | 2 800 870 | 32 990 | 10 923 938 | 128 668 |
| Informational materials (print) | 5 465 382 | 64 374 | 1 810 707 | 21 328 | 4 384 354 | 51 641 | 4 020 572 | 47 357 | 15 681 014 | 184 700 |
| H2.2: Alcohol | 933 641 | 10 997 | 309 320 | 3643 | 748 971 | 8822 | 686 827 | 8090 | 2 678 759 | 31 552 |
| Provider time to administer 5A’s | 383 351 | 4515 | 127 006 | 1496 | 307 526 | 3622 | 282 010 | 3322 | 1 099 893 | 12 955 |
| Informational materials (print) | 550 290 | 6482 | 182 314 | 2147 | 441 445 | 5200 | 404 817 | 4768 | 1 578 866 | 18 597 |
| H2.3: Physical inactivity | 2 609 952 | 30 741 | 864 689 | 10 185 | 2 093 715 | 24 661 | 1 919 994 | 22 615 | 7 488 350 | 88 202 |
| Provider time to administer 5A’s | 1 071 641 | 12 622 | 355 040 | 4182 | 859 675 | 10 126 | 788 345 | 9286 | 3 074 701 | 36 216 |
| Informational materials (print) | 1 538 311 | 18 119 | 509 650 | 6003 | 1 234 040 | 14 535 | 1 131 648 | 13 329 | 4 413 649 | 51 986 |
| H3: Other programme costs | 100 000 | 1178 | 100 000 | 1178 | 100 000 | 1178 | 100 000 | 1178 | 400 000 | 4711 |
| Community awareness meetings | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 200 000 | 2356 |
| Community health workers training | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 200 000 | 2356 |
| E: Evidence-based treatment protocols | 35 959 415 | 423 550 | 11 913 524 | 140 324 | 28 846 806 | 339 774 | 26 453 304 | 311 582 | 103 173 049 | 1 215 230 |
| E1: Ask about patient history - provider time | 5 317 334 | 62 631 | 1 761 658 | 20 750 | 4 265 589 | 50 243 | 3 911 661 | 46 074 | 15 256 241 | 179 697 |
| E2: Assess via physical exam and diagnostic tests - provider time | 5 317 334 | 62 631 | 1 761 658 | 20 750 | 4 265 589 | 50 243 | 3 911 661 | 46 074 | 15 256 241 | 179 697 |
| E3: Return visits - Counsel and treat per protocol - provider time | 25 324 748 | 298 289 | 8 390 209 | 98 825 | 20 315 628 | 239 289 | 18 629 982 | 219 434 | 72 660 567 | 855 837 |
| A: Access to Essential Medicines and Technologies | 40 197 017 | 473 463 | 13 429 971 | 158 186 | 32 279 509 | 380 206 | 29 615 146 | 348 824 | 115 521 643 | 1 360 679 |
| A1: Hypertension medications | 40 028 765 | 471 481 | 13 261 719 | 156 204 | 32 111 257 | 378 224 | 29 446 893 | 346 842 | 114 848 633 | 1 352 752 |
| Amlodipine 5 mg | 9 873 894 | 116 300 | 3 271 268 | 38 531 | 7 920 882 | 93 297 | 7 263 664 | 85 556 | 28 329 707 | 333 683 |
| Losartan 50 mg | 30 016 637 | 353 553 | 9 944 653 | 117 134 | 24 079 482 | 283 622 | 22 081 538 | 260 089 | 86 122 310 | 1 014 397 |
| Hydrochlorothiazide 12.5 mg | 138 235 | 1628 | 45 798 | 539 | 110 892 | 1306 | 101 691 | 1198 | 396 616 | 4672 |
| A2: Diagnostic technologies, machines and supplies | 168 253 | 1982 | 168 253 | 1982 | 168 253 | 1982 | 168 253 | 1982 | 673 010 | 7927 |
| R: Risk-based management | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 689 336 | 8119 |
| R1: Training costs | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 689 336 | 8119 |
| T: Team-based care Savings from training nurses and CHWs to do tasks customarily performed by doctors | 13 815 043 | 162 721 | 4 576 989 | 53 910 | 11 082 490 | 130 536 | 10 162 944 | 119 705 | 39 637 467 | 466 872 |
| T1: Savings from training nurses | 11 976 134 | 141 062 | 3 967 750 | 46 734 | 9 607 309 | 113 160 | 8 810 163 | 103 771 | 34 361 355 | 404 727 |
| Savings from counselling to change behaviour | 1 355 873 | 15 970 | 449 207 | 5291 | 1 087 688 | 12 811 | 997 439 | 11 748 | 3 890 208 | 45 821 |
| Savings from screening for--and assess--CVD risk | 3 367 235 | 39 661 | 1 115 581 | 13 140 | 2 701 212 | 31 816 | 2 477 084 | 29 176 | 9 661 112 | 113 794 |
| Savings from treating CVD risk | 7 253 025 | 85 430 | 2 402 961 | 28 303 | 5 818 410 | 68 533 | 5 335 639 | 62 846 | 20 810 036 | 245 112 |
| T2: Savings from training CHWs | 1 838 909 | 21 660 | 609 239 | 7176 | 1 475 181 | 17 376 | 1 352 781 | 15 934 | 5 276 112 | 62 145 |
| Savings from counselling to change behaviour | 1 838 909 | 21 660 | 609 239 | 7176 | 1 475 181 | 17 376 | 1 352 781 | 15 934 | 5 276 112 | 62 145 |
| S: Systems for monitoring | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 12 458 546 | 146 744 |
| S1: Human resources | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 11 878 546 | 139 912 |
| S2: Technology | 110 000 | 1296 | 110 000 | 1296 | 110 000 | 1296 | 110 000 | 1296 | 440 000 | 5183 |
| S3: Supplies | 10 000 | 118 | 10 000 | 118 | 10 000 | 118 | 10 000 | 118 | 40 000 | 471 |
| S4: Training | 25 000 | 294 | 25 000 | 294 | 25 000 | 294 | 25 000 | 294 | 100 000 | 1178 |
| Total Programme Cost (H+E+A+R+T+S) | 92 778 742 | 1 092 800 | 33 395 573 | 393 352 | 75 213 609 | 885 908 | 69 302 672 | 816 286 | 270 690 596 | 3 188 346 |
BDT, Bangladesh Taka; CHWs, community health worker; CVD, cardiovascular disease.
Figure 2.
Distribution of annual cost by HEARTS components.
Most of the projected annual cost (95%) of implementing module ‘H’ (Healthy-lifestyles counselling) was attributable to the cost of provider time and information materials for counselling patients (US$433 000). The estimated cost for module ‘E’ (Evidence-based treatment protocols) was attributable to provider time across three major activities: asking patient history (US$180 000; 15%), patient assessment via physical exam and diagnostic tests (US$180 000; 15%), and conducting return visits (US$856 000, 70%). The projected cost to implement module ‘S’ (Systems for monitoring) was US$147 000, primarily attributed to administration staff labour costs (95%), with the remaining cost allocated to technology (software/hardware).
Table 4 highlights an important programmatic aspect by describing health providers’ time needed to implement the hypertension control programme. Implementing the programme at the full population level in all four subdistricts was estimated to require the full-time equivalent of 51 doctors, 51 nurses and 6 CHWs. The largest time requirement activities included providing initial screening and diagnosis and conducting return visits.
Table 4.
Hypertension control programme: estimated health provider time for counselling, screening, diagnosis and treatment
| Activity | Golapganj | Fenchugonj | Beanibazar | Bishwanath | Total | ||||
| Workdays | FTE | Workdays | FTE | Workdays | FTE | Workdays | FTE | FTE | |
| Counselling to change behaviour | |||||||||
| Doctor | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| Nurses | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| CHW | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| Screening and diagnosis | |||||||||
| Doctor | 1302 days, 1 hours | 5.0 | 431 days, 6 hours | 1.7 | 1045 days, 2 hours | 4.0 | 958 days, 3 hours | 3.7 | 14.4 |
| Nurses | 1302 days, 1 hours | 5.0 | 431 days, 6 hours | 1.7 | 1045 days, 2 hours | 4.0 | 958 days, 3 hours | 3.7 | 14.4 |
| Return visits - counsel and treat per protocol | |||||||||
| Doctor | 2806 days, 0 hours | 10.8 | 929 days, 6 hours | 3.6 | 2251 days, 1 hours | 8.7 | 2064 days, 2 hours | 7.9 | 31.0 |
| Nurses | 2806 days, 0 hours | 10.8 | 929 days, 6 hours | 3.6 | 2251 days, 1 hours | 8.7 | 2064 days, 2 hours | 7.9 | 31.0 |
Annual: total minutes/124 800.
CHW, community health worker; FTE, full-time equivalent.
Risk-based integrated hypertension, diabetes and high cholesterol management programme cost
Table 5 reports the estimated costs of implementing the risk-based hypertension, diabetes and high cholesterol management programme in four upazilas at the population level (adults aged 18 and above). Figure 2 presents the distribution of costs by HEARTS components. The total annual cost was estimated at US$14.4 million, equivalent to US$12.9 per capita, US$19.3 per adult and US$40.2 per eligible participant. Module ‘A’ (Access to medicines and technology) constitutes the largest cost share (US$11.7 million; 81%), followed by module ‘E’ (Evidence-based treatment protocols, US$1.9 million; 13%). Within module ‘A’, the projected costs of diagnostic tests, hypertension medications, diabetes medications and cholesterol medications were US$5.7 million (49% of module costs), US$1.4 million (12%), US$0.9 million (7%) and US$3.8 million (32%), respectively. The projected medication expenditure per patient treated with medications for hypertension, diabetes and cholesterol was US$18, US$29 and US$37, respectively.
Table 5.
Annual cost of implementing risk-based hypertension, diabetes and high cholesterol management programme in four subdistricts
| Golapganj | Fenchuganj | Beanibazar | Bishwanath | Total | ||||||
| BDT | USD | BDT | USD | BDT | USD | BDT | USD | BDT | USD | |
| H: Healthy lifestyles counselling | 13 335 339 | 157 071 | 4 765 107 | 56 126 | 10 800 324 | 127 212 | 9 947 252 | 117 164 | 38 848 022 | 457 574 |
| H1: Training costs | 418 990 | 4935 | 418 990 | 4935 | 418 990 | 4935 | 418 990 | 4935 | 1 675 960 | 19 740 |
| H1.1: Facility rental (% of H1) | 18 000 | 212 | 18 000 | 212 | 18 000 | 212 | 18 000 | 212 | 72 000 | 848 |
| H1.2: Human resources | 20 000 | 236 | 20 000 | 236 | 20 000 | 236 | 20 000 | 236 | 80 000 | 942 |
| H1.3: Instructive handbooks | 35 000 | 412 | 35 000 | 412 | 35 000 | 412 | 35 000 | 412 | 140 000 | 1649 |
| H1.4: Per diem/transportation | 339 990 | 4005 | 339 990 | 4005 | 339 990 | 4005 | 339 990 | 4005 | 1 359 960 | 16 018 |
| H1.5: Refreshments | 6000 | 71 | 6000 | 71 | 6000 | 71 | 6000 | 71 | 24 000 | 283 |
| H2: Brief counselling costs | 12 816 349 | 150 958 | 4 246 117 | 50 013 | 10 281 334 | 121 099 | 9 428 262 | 111 051 | 36 772 062 | 433 122 |
| H2.1: Tobacco | 9 272 756 | 109 220 | 3 072 108 | 36 185 | 7 438 647 | 87 617 | 6 821 441 | 80 347 | 26 604 952 | 313 368 |
| Provider time to administer 5A’s | 3 807 374 | 44 845 | 1 261 401 | 14 857 | 3 054 293 | 35 975 | 2 800 870 | 32 990 | 10 923 938 | 128 668 |
| Informational materials (print) | 5 465 382 | 64 374 | 1 810 707 | 21 328 | 4 384 354 | 51 641 | 4 020 572 | 47 357 | 1,5681,014 | 184 700 |
| H2.2: Alcohol | 933 641 | 10 997 | 309 320 | 3643 | 748 971 | 8822 | 686 827 | 8090 | 2 678 759 | 31 552 |
| Provider time to administer 5A’s | 383 351 | 4515 | 127 006 | 1496 | 307 526 | 3622 | 282 010 | 3322 | 1 099 893 | 12 955 |
| Informational materials (print) | 550 290 | 6482 | 182 314 | 2147 | 441 445 | 5200 | 404 817 | 4768 | 1 578 866 | 18 597 |
| H2.3: Physical inactivity | 2 609 952 | 30 741 | 864 689 | 10 185 | 2 093 715 | 24 661 | 1 919 994 | 22 615 | 7 488 350 | 88 202 |
| Provider time to administer 5A’s | 1 071 641 | 12 622 | 355 040 | 4182 | 859 675 | 10 126 | 788 345 | 9286 | 3 074 701 | 36 216 |
| Informational materials (print) | 1 538 311 | 18 119 | 509 650 | 6003 | 1 234 040 | 14 535 | 1 131 648 | 13 329 | 4 413 649 | 51 986 |
| H3: Other programme costs | 100 000 | 1178 | 100 000 | 1178 | 100 000 | 1178 | 100 000 | 1178 | 400 000 | 4711 |
| Community awareness meetings | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 200 000 | 2356 |
| Community health workers training | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 50 000 | 589 | 200 000 | 2356 |
| E: Evidence-based treatment protocols | 56 155 264 | 661 428 | 18 604 504 | 219 134 | 45 048 007 | 530 601 | 41 310 245 | 486 575 | 161 118 020 | 1 897 739 |
| E1: Ask about patient history—provider time | 5 317 334 | 62 631 | 1 761 658 | 20 750 | 4 265 589 | 50 243 | 3 911 661 | 46 074 | 15 256 241 | 179 697 |
| E2: Assess via physical exam and diagnostic tests——provider time | 25 513 182 | 300 509 | 8 452 638 | 99 560 | 20 466 790 | 241 069 | 18 768 602 | 221 067 | 73 201 212 | 862 205 |
| E3: Return visits - Counsel and treat per protocol—provider time | 25 324 748 | 298 289 | 8 390 209 | 98 825 | 20 315 628 | 239 289 | 18 629 982 | 219 434 | 72 660 567 | 855 837 |
| A: Access to Essential Medicines and tech. | 347 102 943 | 4 088 374 | 115 109 353 | 1 355 823 | 278 480 835 | 3 280 104 | 255 388 440 | 3 008 109 | 996 081 571 | 11 732 410 |
| A1: Diagnostic tests | 170 039 655 | 2 002 823 | 56 334 940 | 663 545 | 136 406 582 | 1 606 674 | 125 088 536 | 1 473 363 | 487 869 714 | 5 746 404 |
| Complete blood count (panel) | 51 527 168 | 606 916 | 17 071 194 | 201 074 | 41 335 328 | 486 871 | 37 905 617 | 446 474 | 147 839 307 | 1 741 335 |
| Blood lipid panel | 103 054 336 | 1 213 832 | 34 142 388 | 402 148 | 82 670 656 | 973 742 | 75 811 234 | 892 947 | 295 678 614 | 3 482 669 |
| Fasting blood glucose | 15 458 150 | 182 075 | 5 121 358 | 60 322 | 12 400 598 | 146 061 | 11 371 685 | 133 942 | 44 351 792 | 522 400 |
| A2: Hypertension medications | 40 028 765 | 471 481 | 13 261 719 | 156 204 | 32 111 257 | 378 224 | 29 446 893 | 346 842 | 114 848 633 | 1 352 752 |
| Amlodipine 5 mg | 9 873 894 | 116 300 | 3 271 268 | 38 531 | 7 920 882 | 93 297 | 7 263 664 | 85 556 | 28 329 707 | 333 683 |
| Losartan 50 mg | 30 016 637 | 353 553 | 9 944 653 | 117 134 | 24 079 482 | 283 622 | 22 081 538 | 260 089 | 86 122 310 | 1 014 397 |
| Hydrochlorothiazide 12.5 mg | 138 235 | 1628 | 45 798 | 539 | 110 892 | 1306 | 101 691 | 1198 | 396 616 | 4672 |
| A3: Diabetes medications | 25 366 503 | 298 781 | 8 404 042 | 98 988 | 20 349 124 | 239 683 | 18 660 698 | 219 796 | 72 780 367 | 857 248 |
| Metformin 500 mg | 11 707 617 | 137 899 | 3 878 789 | 45 687 | 9 391 903 | 110 623 | 8 612 630 | 101 444 | 33 590 939 | 395 653 |
| Metformin 1000 mg | 12 292 998 | 144 794 | 4 072 728 | 47 971 | 9 861 498 | 116 154 | 9 043 262 | 106 517 | 35 270 486 | 415 436 |
| Gliclazide | 1 365 889 | 16 088 | 452 525 | 5330 | 1 095 722 | 12 906 | 1 004 807 | 11 835 | 3 918 943 | 46 160 |
| A4: Cholesterol medications | 111 499 768 | 1 313 307 | 36 940 399 | 435 105 | 89 445 620 | 1 053 541 | 82 024 060 | 966 126 | 319 909 847 | 3 768 078 |
| Simvastatin 10 mg | 79 451 930 | 935 830 | 26 322 800 | 310 045 | 63 736 699 | 750 727 | 58 448 282 | 688 437 | 227 959 711 | 2 685 038 |
| Atorvastatin 20 mg | 13 353 266 | 157 282 | 4 424 000 | 52 108 | 10 712 050 | 126 173 | 9 823 241 | 115 704 | 38 312 556 | 451 267 |
| Atorvastatin 40 mg | 18 694 572 | 220 195 | 6 193 600 | 72 952 | 14 996 870 | 176 642 | 13 752 537 | 161 985 | 53 637 579 | 631 774 |
| A5: Diagnostic tech. machines and supplies | 168 253 | 1982 | 168 253 | 1982 | 168 253 | 1982 | 168 253 | 1982 | 673 010 | 7927 |
| R: Risk-based management | 5 489 668 | 64 660 | 1 933 992 | 22 780 | 4 437 923 | 52 272 | 4 083 995 | 48 104 | 15 945 577 | 187 816 |
| R1: Training costs | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 172 334 | 2030 | 689 336 | 8119 |
| R2: Estimate risk using risk charts | 5 317 334 | 62 631 | 1 761 658 | 20 750 | 4 265 589 | 50 243 | 3 911 661 | 46 074 | 15 256 241 | 179 697 |
| T: Team-based care: Savings from training nurses and CHWs to do tasks customarily performed by doctors | 25 600 367 | 301 536 | 8 481 523 | 99 900 | 20 536 731 | 241 893 | 18 832 739 | 221 823 | 73 451 360 | 865 151 |
| T1: Savings from training nurses | 23 761 458 | 279 876 | 7 872 283 | 92 724 | 19 061 549 | 224 518 | 17 479 958 | 205 889 | 68 175 248 | 803 006 |
| Savings from counselling to change behaviour | 1 355 873 | 15 970 | 449 207 | 5291 | 1 087 688 | 12 811 | 997 439 | 11 748 | 3 890 208 | 45 821 |
| Savings from screening for—and assess—CVD risk | 15 152 559 | 178 475 | 5 020 114 | 59 130 | 12 155 452 | 143 174 | 11 146 879 | 131 294 | 43 475 005 | 512 073 |
| Savings from treating CVD risk | 7 253 025 | 85 430 | 2 402 961 | 28 303 | 5 818 410 | 68 533 | 5 335 639 | 62 846 | 20 810 036 | 245 112 |
| T2: Savings from training CHWs | 1 838 909 | 21 660 | 609 239 | 7176 | 1 475 181 | 17 376 | 1 352 781 | 15 934 | 5 276 112 | 62 145 |
| Savings from counselling to change behaviour | 1 838 909 | 21 660 | 609 239 | 7176 | 1 475 181 | 17 376 | 1 352 781 | 15 934 | 5 276 112 | 62 145 |
| S: Systems for monitoring | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 3 114 636 | 36 686 | 12 458 546 | 146 744 |
| S1: Human resources | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 2 969 636 | 34 978 | 11 878 546 | 139 912 |
| S2: Technology | 110 000 | 1296 | 110 000 | 1296 | 110 000 | 1296 | 110 000 | 1296 | 440 000 | 5183 |
| S3: Supplies | 10 000 | 118 | 10 000 | 118 | 10 000 | 118 | 10 000 | 118 | 40 000 | 471 |
| S4: Training | 25 000 | 294 | 25 000 | 294 | 25 000 | 294 | 25 000 | 294 | 100 000 | 1178 |
| Total programme cost (H+E+A+R+T+S) | 425 197 850 | 5 008 220 | 143 527 592 | 1 690 549 | 341 881 725 | 4 026 875 | 313 844 568 | 3 696 638 | 1,224,451,735 | 14 422 282 |
5 A’s, Assess, Advise, Agree, Assist, Arrange; BDT, Bangladesh Taka; CHW, community health worker; CVD, cardiovascular disease.
The adoption of task-sharing approach would save US$865 000, of which US$803 000 comes from using nurses to complete tasks customarily performed by doctors (ie, counselling, screening and assessing CVD risk, and treating according to CVD risk) and US$62 000 comes from using CHWs to provide counselling to change behaviour. Implementing the risk-based hypertension, diabetes and high cholesterol management programme at the full population level in all four subdistricts was estimated to require the full-time equivalent of 58 doctors, 58 nurses, 6 CHWs and 101 lab technicians (table 6). The largest time requirement activities included providing initial screening and diagnosis and conducting return visits.
Table 6.
Integrated risk-based approach: estimated health provider time for counselling, screening, diagnosis and treatment
| Activity | Golapganj | Fenchugonj | Beanibazar | Bishwanath | Total | ||||
| Workdays | FTE | Workdays | FTE | Workdays | FTE | Workdays | FTE | FTE | |
| Counselling to change behaviour | |||||||||
| Doctor | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| Nurses | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| CHW | 524 days, 7 hours | 2.0 | 173 days, 6 hours | 0.7 | 420 days, 2 hours | 1.6 | 385 days, 2 hours | 1.5 | 5.8 |
| Screening and diagnosis | |||||||||
| Doctor | 1302 days, 1 hours | 5.0 | 431 days, 6 hours | 1.7 | 1045 days, 2 hours | 4.0 | 958 days, 3 hours | 3.7 | 14.4 |
| Nurses | 1302 days, 1 hours | 5.0 | 431 days, 6 hours | 1.7 | 1045 days, 2 hours | 4.0 | 958 days, 3 hours | 3.7 | 14.4 |
| Screening and diagnosis by Lab technicians | 9119 days, 3 hours | 35.1 | 3021 days, 6 hours | 11.6 | 7315 days, 0 hours | 28.1 | 6708 days, 1 hours | 25.8 | 100.6 |
| Estimating CVD risk using risk charts | |||||||||
| Doctor | 2 658 667 | 2.5 | 880 829 | 0.8 | 2 132 795 | 2.0 | 1 955 830 | 1.8 | 7.2 |
| Nurses | 2 658 667 | 2.5 | 880 829 | 0.8 | 2 132 795 | 2.0 | 1 955 830 | 1.8 | 7.2 |
| Return visits—counsel and treat per protocol | |||||||||
| Doctor | 2806 days, 0 hours | 10.8 | 929 days, 6 hours | 3.6 | 2251 days, 1 hours | 8.7 | 2064 days, 2 hours | 7.9 | 31.0 |
| Nurses | 2806 days, 0 hours | 10.8 | 929 days, 6 hours | 3.6 | 2251 days, 1 hours | 8.7 | 2064 days, 2 hours | 7.9 | 31.0 |
CHW, community health worker; CVD, cardiovascular disease; FTE, full-time equivalent.
Discussion
The HEARTS pilot project in four Bangladesh subdistricts launched a framework for hypertension management in primary care, with a potential for expanding into a comprehensive CVD prevention approach that incorporates hypertension, diabetes and cholesterol management. This study projects the expected cost of scaling up the programme to all eligible adults in the participating subdistricts. We assessed two programme scenarios: a hypertension management programme and an integrated risk-based hypertension, diabetes and cholesterol management programme. The total annual cost was estimated at US$3.2 and US$14.4 million for the hypertension and risk-based comprehensive approach, respectively. The overall per capita cost was approximately US$2.8 per capita for the hypertension control programme and US$12.9 per capita for the risk-based comprehensive approach. These estimates correspond to 0.14% and 0.7% of the 2020 gross domestic product per capita in Bangladesh, respectively. The main cost drivers for the hypertension control programme were medication expenditures (43%) and the cost of provider time for providing care during multiple visits (38%). In the risk-based integrated approach, the combined costs of hypertension, diabetes and cholesterol medications and diagnostic tests make up the largest share of the overall programme cost (81%). Although the main driver of projected programme costs for the integrated approach was expenditure on essential medicines and diagnostic tests, hypertension and diabetes medications contributed a relatively small portion (19%) to this expenditure (ie, module A), whereas cholesterol medications contributed nearly 32%. Hypertension treatment remains among the leading cost-effective ways to combat heart disease. In this study, the annual medication expenditure per patient treated with medications for hypertension, diabetes and cholesterol was US$18, US$29 and US$37, respectively.
Though based on observations gathered in one district of Bangladesh, our results are consistent with those reported by past studies. A previous study on Bangladesh by Nugent et al31 estimated that hypertension treatment would cost about US$13 (BDT1070) per patient per year.31 WHO (2011) has estimated the average hypertension screening cost for LMICs at approximately US$4 for LMICs, not including treatment but including the cost of performing CVD risk assessment and BP measurement in primary care settings.32 Haque33 estimated the average cost of diabetes screening in Bangladesh at approximately US$5 (BDT411), including glucose screening in primary care, documentation, setting up referrals and organising screening events but excluding treatment.33 In this study, the cost elements in the Bangladesh HEARTS programme are wide-ranging including screening, diagnosis and treatment for multiple CVD risk conditions (hypertension, diabetes, hyperlipidaemia) and counselling for CVD risk factors (tobacco use, alcohol use and physical inactivity).
The analysis revealed that scaling up the hypertension management programme within the four subdistricts would require an additional full-time equivalent of 51 doctors, 51 nurses and 6 CHWs. Population-level scale-up of the risk-based hypertension, diabetes and high cholesterol management programme in the four subdistricts was estimated to require the full-time equivalent of 58 doctors, 58 nurses, 6 CHWs and 101 lab technicians. To put this in context, a typical 50-bed subdistrict public health complex in Bangladesh employs 20 doctors, 16 nurses and 1 medical assistant. Oftentimes, not all health provider posts are filled. This gap in provider capacity poses a significant barrier to programme expansion. Team-based care using task-sharing among doctors, nurses and CHWs and volunteers can accomplish the activities required by the HEARTS package more affordably, including NCD-related health promotion, prevention, screening and patient navigation through the health system. A systematic review of intervention trials in LMICs by Joshi et al34 found that team-based care, including task sharing was effective in improving process outcomes (eg, hypertension and diabetes screening) and health outcomes (eg, hypertension and diabetes control) and achieving treatment concordance with doctors.16 34 Krishnan et al35 conducted a study on a community-based hypertension management programme of BP monitoring and lifestyle counselling intervention undertaken by female community health volunteers in Nepal, and assessed the intervention to be highly cost-effective.35 However, there are several barriers to team-based care with task sharing, including staff attrition and turnover, retention of training, patient perception and acceptance toward non-physician health workers, lack of delegation of work by physicians, legislation and policy etc.36
In Bangladesh, of the four entities (ie, the government, for-profit private sector, non-profit nongovernmental organisation and donor agencies) involved in the primary healthcare provision, the government plays the leading role, mainly in rural areas. There are six tiers of public healthcare infrastructure: national, divisional, district, upazila (subdistrict), union and ward levels. To tackle NCDs, the government of Bangladesh introduced ‘NCD Corners’ initiative in 2012 dedicated to providing prevention and care services for common NCDs and related conditions. The government has plans to expand ‘NCD corners’ at the upazila level, and the upazila primary care setting is well positioned to bridge the link the healthcare providers down to the union, ward (and community) levels by harnessing community support and delegating suitable activities under task-sharing principles.16 37 38 This will enhance healthcare access among disadvantaged populations and mitigate health disparities. Further, in Bangladesh, according to the 2016 Household Income Expenditure Survey and 2014 Health and Morbidity Status Survey, one in three patients received treatment from a pharmacy or medical shop, while about one in five received treatment from public health providers.39 40 This emphasises the need for partnerships with various types of public–private health providers.
The models of care introduced in the Bangladesh national hypertension guidelines and NCD operational plan are encouraging; however, there are capacity challenges to the scaling-up of NCD care in Bangladesh.41 42 The fiscal year 2021 budget allocation to the health sector stands just above 5%, which is less than 1% of GDP. Further, less than 5% of public sector funding for health covers NCDs, despite NCDs being responsible for almost two-thirds (63% in 2016) of disability-adjusted life-years in Bangladesh.16 The per capita NCD allocation is only US$0.08.16 There is a need for better coordination of non-state stakeholders in NCD control with the public sector with a stronger focus of the public sector on NCD prevention and health promotion.16 The health sector in Bangladesh is financed 93% from domestic sources (74% out-of-pocket, 17% government health expenditure and 3% other private sources) and 7% from external health expenditures. Domestic general government health expenditure per capita is only US$7 (0.4% of GDP per capita).43 Due to insufficient public sector funding, out-of-pocket expenditure for NCD care is large in Bangladesh, contributing to the impoverishment of patients and their families. Moreover, a recent policy review by Biswas et al44 highlights the lack of proper planning, implementation and monitoring of NCD health initiatives.44 However, the Bangladesh Copenhagen Project assessed the benefits of managing hypertension through targeted investment and reported a high level of return on investment (BDT17 benefit for every BDT spent).31
This report has several limitations. Due to lack of data at a local level, the cost projections rely on assumptions regarding population coverage, risk factor prevalence, primary care attendance rate, distribution of CVD risk among the population, distribution of patients by treatment protocols, and frequency of patient visits by CVD risk, which were assumed to be uniform for the four subdistricts and across age or sex groups. Similarly, unit costs of supplies, wages and provider time allocations were assumed to be the same across subdistricts. Since the examined subdistricts are adjacent to each other, these unit costs may not be considerably different. While we used average medicine prices, they may vary in different subdistricts depending on the procurement arrangement and sources. However, in Bangladesh, the price variations are minimal or low in the public health facilities, given the medicines are procured mainly from EDCL and/or CMSD.19 20 The strength of the study lies in its ability to disaggregate costs by function, identifying areas for efficiency improvements, such as task-sharing and bridging programme delivery from the upazila level to more localised community facilities.
In 2018, the Government of Bangladesh introduced a multisectoral action plan for NCD prevention and control, which emphasises NCD risk factors including tobacco use, unhealthy diet, physical inactivity and harmful use of alcohol.42 This study can inform approaches to scaling up this action plan nationally, with the goal of increasing population outreach for CVD prevention at the primary care level. Using the costs reported in this study for future cost-effectiveness analyses can further support evidence-based decision making for CVD prevention programmes in Bangladesh.
Conclusion
Expanding the HEARTS hypertension management and CVD prevention programme to provide services to the entire eligible population in the catchment area may face constraints in physician capacity. A task-sharing model involving shifting of select tasks from doctors to nurses and local CHWs would be essential for the eventual scale-up of primary care services to prevent CVD in Bangladesh.
Supplementary Material
Footnotes
Contributors: MJH and MSH conceptualised the study, led the formal analysis, implemented the methodology and the excel-based costing tool, and wrote the draft manuscript. DK, SRC, MRB and AEM contributed to the study concept, analytical aspects, manuscript write-up and critical review. RT and SJ contributed to data collection and critical review of the manuscript. MJH, MSH, SRC, RT, SJ and MRB contributed to data collection. MJH and MSH are responsible for the overall content as guarantor. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Funding: This analysis was conducted on behalf of Resolve to Save Lives, an initiative of Vital Strategies. Resolve to Save Lives is funded by grants from Bloomberg Philanthropies; the Bill & Melinda Gates Foundation; and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation.
Disclaimer: The findings and conclusions of this report are those of authors only and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Organization . Improving hypertension control in 3 million people country experiences of programme development and implementation. Geneva; 2020. [Google Scholar]
- 2.World Health Organization . A global brief on hypertension: silent killer, global public health crisis: World health day; 2013.
- 3.Lily A, Ross HA, GBD . Risk factors collaborators. global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 2013;2015:2287–323. 10.1016/S0140-6736(15)00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 2014;383:1899–911. 10.1016/S0140-6736(14)60685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaes B, Beke E, Truyers C, et al. The correlation between blood pressure and kidney function decline in older people: a registry-based cohort study. BMJ Open 2015;5:e007571. 10.1136/bmjopen-2015-007571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tzourio C. Hypertension, cognitive decline, and dementia: an epidemiological perspective. Dialogues Clin Neurosci 2007;9:61–70. 10.31887/DCNS.2007.9.1/ctzourio [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bloch MJ, FASH F, Basile FJ. Cardiovascular risks of hypertension. In: UpToDate, 2018. [Google Scholar]
- 8.World Health Organization . Sixty-Fifth World health assembly resolutions, decisions, annexes; 2012: 21–6. http://www.who.int/mediacentre/events/2012/wha65/en/ [Accessed 2012].
- 9.World Health Organization . Global action plan for the prevention and control of noncommunicable diseases. Geneva, Switzerland; 2013. http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf [Google Scholar]
- 10.World Health Organization . Global status report on noncommunicable diseases; 2014.
- 11.World Health Organization . Thirteenth general programme of work (GPW13): methods for impact measurement. Geneva; 2020. file:///C:/Research/BangladeshHEARTSCostingtool/gpw13-methodology-nov9-online-version.pdf [Google Scholar]
- 12.General Assembley 70 session . Transforming our world: the 2030 agenda for sustainable development. United Nations; 2015. [Google Scholar]
- 13.Riaz BK, Islam MZ, Islam ANMS, et al. Risk factors for non-communicable diseases in Bangladesh: findings of the population-based cross-sectional national survey 2018. BMJ Open 2020;10:e041334. 10.1136/bmjopen-2020-041334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chowdhury MZI, Rahman M, Akter T, et al. Hypertension prevalence and its trend in Bangladesh: evidence from a systematic review and meta-analysis. Clin Hypertens 2020;26:1–19. 10.1186/s40885-020-00143-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization . National steps survey for non-communicable diseases risk factors in Bangladesh Country Office for Bangladesh; 2018. https://apps.who.int/iris/handle/10665/332886 [Google Scholar]
- 16.The World Bank . Hypertension and type-2 diabetes in Bangladesh: continuum of care assessment and opportunities for action. Washington DC; 2019. [Google Scholar]
- 17.World Health Organization . Hearts: technical package for cardiovascular disease management in primary health care; 2020.
- 18.World Health Organization . Hearts: technical package for cardiovascular disease management in primary health care. Geneva, Switzerland; 2016. https://apps.who.int/iris/bitstream/handle/10665/252661/9789241511377-en [Google Scholar]
- 19.World Health Organization . Medicines in health care delivery Bangladesh: situational analysis: 13 – 25 September 2014 report prepared using the WHO/SEARO workbook tool for undertaking a situational analysis of medicines in health care delivery in low and middle income countries. New Delhi, India: Regional Office for South East Asia; 2014. [Google Scholar]
- 20.Kasonde L, Tordrup D, Naheed A, et al. Evaluating medicine prices, availability and affordability in Bangladesh using World health organisation and health action international methodology. BMC Health Serv Res 2019;19:1–12. 10.1186/s12913-019-4221-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization . Hearts technical package for cardiovascular disease management in primary health care: risk based CVD management. Geneva; 2020. [Google Scholar]
- 22.World Health Organization . Diagnosis and management of type 2 diabetes (HEARTS-D). Geneva, Switzerland; 2020. [Google Scholar]
- 23.Brown RE, Welsh P, Logue J. Systematic review of clinical guidelines for lipid lowering in the secondary prevention of cardiovascular disease events. Open Heart 2020;7:e001396. 10.1136/openhrt-2020-001396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Husain MJ, Allaire BT, Hutchinson B, et al. Assessing costs of a hypertension management program: an application of the hearts costing tool in a program planning workshop in Thailand. J Clin Hypertens 2020;22:111–7. 10.1111/jch.13773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glasgow RE, Emont S, Miller DC. Assessing delivery of the five as for patient-centered counseling. Health Promot Int 2006;21:245–55. 10.1093/heapro/dal017 [DOI] [PubMed] [Google Scholar]
- 26.Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions: an evidence-based approach. Am J Prev Med 2002;22:267–84. 10.1016/S0749-3797(02)00415-4 [DOI] [PubMed] [Google Scholar]
- 27.Islam JY, Zaman MM, Moniruzzaman M, et al. Estimation of total cardiovascular risk using the 2019 WHO CVD prediction charts and comparison of population-level costs based on alternative drug therapy guidelines: a population-based study of adults in Bangladesh. BMJ Open 2020;10:e035842. 10.1136/bmjopen-2019-035842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasan MJ. Pattern of drugs prescribed for treatment of hypertensive patients: Bangladesh. Afr J Pharmacy Pharmacol 2016;10:521–5. 10.5897/AJPP2016.4549 [DOI] [Google Scholar]
- 29.Chowdhury A, SEN N, Banik S. Prescribing pattern of antidiabetic drugs in type 2 diabetic patients of Noakhali city in Bangladesh. Marmara Pharm J 2017;21:1010–4. 10.12991/mpj.2017.24 [DOI] [Google Scholar]
- 30.Elnaem MH, Mohamed MHN, Huri HZ, et al. Effectiveness and prescription pattern of lipid-lowering therapy and its associated factors among patients with type 2 diabetes mellitus in Malaysian primary care settings. Ther Clin Risk Manag 2019;15:137–45. 10.2147/TCRM.S182716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nugent R, Brower E, Cravioto A, et al. A cost-benefit analysis of a national hypertension treatment program in Bangladesh. Prev Med 2017;105:S56–61. 10.1016/j.ypmed.2017.08.014 [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . Scaling up action against non-communicable diseases: how much will it cost; 2011.
- 33.Haque R. Costs and benefits of addressing diabetes and smokeless tobacco consumption via community clinics. Bangladesh Priorities: Copenhagen Consensus Center, 2016. [Google Scholar]
- 34.Joshi R, Alim M, Kengne AP, et al. Task shifting for non communicable disease management in low and middle income countries a systematic review. PLoS One 2014;9:e103754. 10.1371/journal.pone.0103754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krishnan A, Finkelstein EA, Kallestrup P, et al. Cost-effectiveness and budget impact of the community-based management of hypertension in Nepal study (COBIN): a retrospective analysis. Lancet Glob Health 2019;7:e1367–74. 10.1016/S2214-109X(19)30338-9 [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization . Hearts technical package for cardiovascular disease management in primary health care: team-based care. Geneva; 2018. [Google Scholar]
- 37.Rawal LB, Kanda K, Biswas T, et al. Non-communicable disease (Ncd) corners in public sector health facilities in Bangladesh: a qualitative study assessing challenges and opportunities for improving ncd services at the primary healthcare level. BMJ Open 2019;9:e029562. 10.1136/bmjopen-2019-029562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Directorate General of Health Services . Management information system, director General of health services, Ministry of health and family welfare Government of the People’s Republic of Bangladesh Health Bulletin; 2020. [Google Scholar]
- 39.Bangladesh Bureau of Statistics (BBS) . Statisics and informatics division (SID), Ministry of planning. Government of the People’s Republic of Bangladesh: Preliminary report on Household Income and Expenditure Survey; 2017. [Google Scholar]
- 40.Bangladesh Bureau of Statistics (BBS) . Report on Health and Morbidity Status Survey 2014. In: Statisics and informatics division (SID), Ministry of planning. Government of the People’s Republic of Bangladesh, 2015. [Google Scholar]
- 41.World Health Organization . National guidelines for management of hypertension in Bangladesh; 2013.
- 42.Director General of Health Services . Multi-sectoral action plan for prevention and control of non-communicable diseases 2018-2025. Dhaka: Non-communicable Disease Control Programme; 2018. [Google Scholar]
- 43.Who global health expenditure database. Available: https://apps.who.int/nha/database/ViewData/Indicators/en
- 44.Biswas T, Pervin S, Tanim MIA, et al. Bangladesh policy on prevention and control of non-communicable diseases: a policy analysis. BMC Public Health 2017;17:582. 10.1186/s12889-017-4494-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061467supp001.pdf (565.9KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.