Abstract
Background
Adolescence is a critical period in human life, associated with reduced physical activity and increased sedentary behaviors. In this systematic review and dose-response meta-analysis, we evaluated the association between screen time and risk of overweight/obesity among adolescents.
Methods
A systematic search in electronic databases, including PubMed, Embase, and Scopus was performed up to September 2021. All published studies evaluating the association between screen time and risk of overweight/obesity among adolescents were retrieved. Finally, a total of 44 eligible studies were included in the meta-analysis.
Results
The results of the two-class meta-analysis showed that adolescents at the highest category of screen time were 1.27 times more likely to develop overweight/obesity (OR = 1.273; 95% CI = 1.166–1.390; P < 0.001; I-squared (variation in ES attributable to heterogeneity) = 82.1%). The results of subgrouping showed that continent and setting were the possible sources of heterogeneity. Moreover, no evidence of non-linear association between increased screen time and risk of overweight/obesity among adolescents was observed (P-nonlinearity = 0.311).
Conclusion
For the first time, the current systematic review and meta-analysis revealed a positive association between screen time and overweight/obesity among adolescents without any dose-response evidence.
Trial registration
The protocol of the current work has been registered in the PROSPERO system (Registration number: CRD42021233899).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-022-01761-4.
Keywords: Screen time, Overweight, Obesity, Dose-response, Adiposity, Meta-analysis
Background
Adolescence is a critical period regarding physical activity-related behaviors since regular physical activity decreases and sedentary behavior increases in this period [1, 2]. Screen-related physical activities like television watching are very common among adolescents particularly in modern societies; it is reported that adolescents spend about 3h per day on screen activities [3]. Screen time constitutes an important part of adolescents’ life, and they are major TV users [4, 5]. In a study, 57% of adolescents reported watching TV every day (average time in a day: 109 minutes) [6]. According to some recent evidence, increased screen-related sedentary behaviors led not only to obesity growth [7], but also to mental problems among adolescents [8–12].
Sedentary behavior guidelines recommend less than 2h per day of recreational screen time for the youth [13]. However, it has been estimated that more than 50% of adolescents exceed this time [14]. In a report from the Health Behavior in School-Age Children (HBSC), which was performed among adolescents aged 11, 13, and 15 years in 41 European and North American countries, 56–65% of the adolescents spent 2h or more per day watching television [15, 16].
Sedentary behaviors are characterized by activities with low energy expenditure (< 1.5 metabolic equivalents) in a sitting position like television watching or other screen behaviors [17]. Such behaviors are an important risk factor for cardio-metabolic disease in adulthood [18–21]. In adolescents, obesity is associated with dyslipidemia, glucose intolerance, and hypertension [22]. In several population-based studies [23–25], high screen time was positively associated with high blood pressure (BP), high low-density lipoprotein (LDL) cholesterol, and triglyceride (TG) (P < 0.05).
Numerous studies have reported the association between screen time and adiposity among adolescents; however, the results are inconsistent. Some studies reported increased odds of obesity by increasing screen time [22, 26, 27]. For example, Cheng [26] included 2201 Chinese adolescents and reported increased odds of obesity for those with more than 2h of screen time per day (1.53; 95%CI = 0.95–2.09; P < 0.001). In contrary, in another population-based study in the school setting, Lopez-Gonzalez evaluated 1,319,293 adolescents aged 12–14 years old and reported no significant association between obesity and screen time [28]. Several other studies also reported no association between obesity and screen time [28–31]. Meanwhile, in some other studies, only watching television or playing video games for more than 3h per day increased the risk of obesity among adolescents [32–34]. More surprisingly, in a study by De-Lima et al. [35], a non-significant reduced risk of excess weight was observed by increased screen time of more than 4h per day (P = 0.87; 95% CI = 0.59–1.30).
As mentioned, there is an inconsistency between the results of different studies regarding the association between screen time and overweight/obesity among adolescents. In today’s digital age, screen time is almost unavoidable and it has drastically increased among children and adolescents, especially during the coronavirus disease 2019 (COVID-19) pandemic. Excessive screen time may have adverse health consequences because it replaces healthy behaviors and habits like physical activity and sleep routine [36, 37]. However, currently, there is no systematic review and meta-analysis evaluating the association between screen time and obesity among adolescents. More importantly, no study in this filed has focused on such dimensions as the type of screen (TV, PC, DVD, video games, etc.), duration of screen use, and several other factors affecting the association between overweight/obesity and screen time.
Therefore, in this systematic review and meta-analysis, we systematically searched and analyzed all the available literature evaluating the association between overweight/obesity and screen time among adolescents. We also classified the results according to numerous factors, including geographical distribution, screen type, setting, obesity status, as well as the quality and sample size of studies to identify the possible determinants of these associations.
Methods
The results were reported according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist (Sup. Table 1) [38]. The protocol’s registration code in PROSPERO is CRD42021233899.
Search strategy, selection of studies, inclusion and exclusion criteria
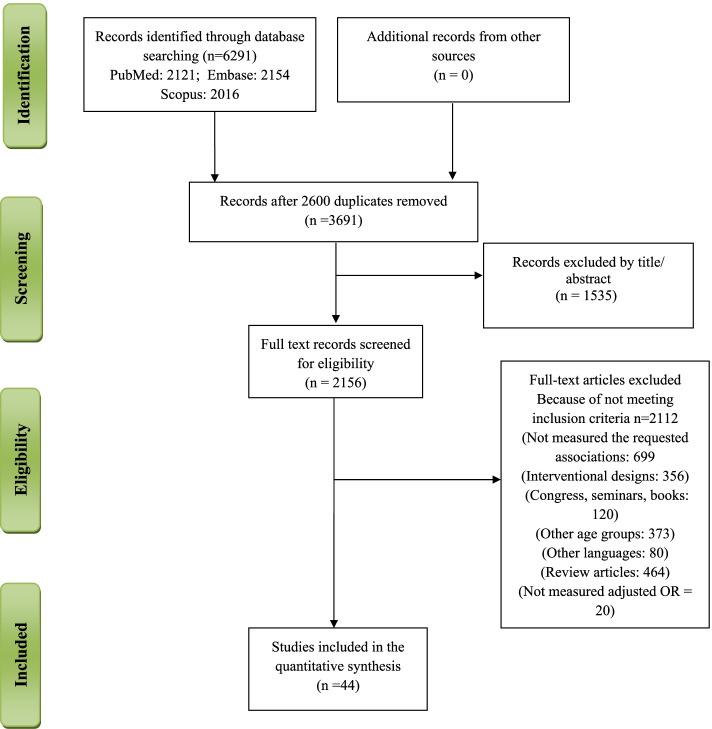
A total of 6291 articles were retrieved through searching electronic databases, including PubMed, Embase, and Scopus up to September 2021 (Fig. 1). The search strategy for PubMed is provided in Sup. Table 2, and it has been adopted for each electronic database. A total of 44 manuscripts were eligible to be included in the final meta-synthesis.
Fig. 1.
Study Flowchart
The inclusion criteria were as follows: 1) studies with observational designs (case control, cross-sectional or cohort studies with the baseline or cross-sectional measurement of study parameters), 2) studies evaluating the relationship (OR, RR, or HR) between screen time and risk of overweight/obesity, and (3) studies conducted only among adolescents (age ≥ 10–20 years). The studeis that did not provide an OR, RR, or HR or those with adjustment for confounders were excluded from the analysis.
The PICO model (patients, intervention, comparison, outcome), which is one of the most widely used models for formulating clinical questions, was used for selecting the studies (Table 1).
Table 1.
The PICO criteria used for the systematic review
| PICO criteria | Description |
|---|---|
| Participants | Adolescents population |
| Exposure (Interventions) | Highest category of screen time |
| Comparisons | Lowest category of screen time |
| Outcome | Overweight/ obesity |
| Study design | Observational studies with the design of cross-sectional, case control or cohort |
Data extraction and quality assessment
Data extraction was done by two authors in a standard EXCELL datasheet. The data sheet included the following information: name of first author and journal, publication year, country, setting, age range, number of participants, study design, adjusted covariate, gender, definition of overweight/obesity and screen time, overweight/obesity status, weight, height, screen time measurement tools, and main results. Any disagreements between reviewers were resolved by discussion. The methodological quality of studies were assessed using the Agency for Healthcare Research and Quality (AHRQ) checklist [54] (Table 2).
Table 2.
Agency for Healthcare Research and Quality (AHRQ) checklist to assess quality of the cross-sectional studies
| ARHQ Methodology Checklist items for Cross-Sectional study | Zhang Y [39] | De-Lima TR [35] | Zulfiqar T [33] | Kerkadi A [30] | Hu J [99] | De-Jong E [40] | Franceschin MJ [22] | Dalamaria, T [27] | Cheng L [100] | ||
| 1) Define the source of information (survey, record review) | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 3) Indicate time period used for identifying patients | ⊕ | ⊕ | ⊕ | _ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 4) Indicate whether or not subjects were consecutive if not population-based | ⊕ | – | – | ⊕ | – | – | – | – | – | ||
| 5) Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants | – | – | – | U | – | – | – | – | – | ||
| 6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | – | – | U | U | U | U | U | U | ⊕ | ||
| 7) Explain any patient exclusions from analysis | ⊕ | ⊕ | ⊕ | _ | ⊕ | – | ⊕ | – | ⊕ | ||
| 8) Describe how confounding was assessed and/or controlled. | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | – | ⊕ | ⊕ | ||
| 9) If applicable, explain how missing data were handled in the analysis | ⊕ | – | ⊕ | ⊕ | ⊕ | – | ⊕ | ⊕ | ⊕ | ||
| 10) Summarize patient response rates and completeness of data collection | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | – | ⊕ | ⊕ | ⊕ | ||
| 11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | – | – | – | ⊕ | – | – | – | – | – | ||
| Total score | 8 | 6 | 7 | 7 | 7 | 4 | 6 | 6 | 8 | ||
| ARHQ Methodology Checklist items for Cross-Sectional study | Lopez-GonzalezD [28] | Pabón D [41] | Haidar A [29] | Saha M [31] | Mansoori M [42] | Godakanda I [43] | Talat MA [44] | Piryani MA [44] | Moradi G [45] | ||
| 1) Define the source of information (survey, record review) | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 3) Indicate time period used for identifying patients | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 4) Indicate whether or not subjects were consecutive if not population-based | ⊕ | – | – | – | – | – | ⊕ | – | – | ||
| 5) Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants | U | U | U | – | – | U | U | U | – | ||
| 6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | U | U | U | – | ⊕ | U | U | U | – | ||
| 7) Explain any patient exclusions from analysis | _ | _ | _ | – | ⊕ | ⊕ | _ | _ | – | ||
| 8) Describe how confounding was assessed and/or controlled. | ⊕ | ⊕ | – | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ||
| 9) If applicable, explain how missing data were handled in the analysis | ⊕ | ⊕ | ⊕ | – | – | ⊕ | – | – | – | ||
| 10) Summarize patient response rates and completeness of data collection | ⊕ | – | – | – | ⊕ | – | – | – | – | ||
| 11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | ⊕ | – | – | – | – | ⊕ | – | – | – | ||
| Total score | 8 | 5 | 4 | 4 | 7 | 7 | 5 | 4 | 4 | ||
| ARHQ Methodology Checklist items for Cross-Sectional study | Watharkar A [46] | De- Lucena JMS [47] | Velásquez-Rodríguez CM [48] | De Jong E [40] | Ercan S [49] | Collins AE [34] | Drake KM [50] | Sun Y [32] | Adesina AF [51] | El-Gilany AH [52] | Byun W [53] |
| 1) Define the source of information (survey, record review) | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| 2) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| 3) Indicate time period used for identifying patients | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| 4) Indicate whether or not subjects were consecutive if not population-based | – | ⊕ | – | ⊕ | – | – | ⊕ | – | – | ⊕ | ⊕ |
| 5) Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants | – | – | – | – | – | – | – | – | – | – | – |
| 6) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) | – | U | – | U | – | – | – | U | – | ⊕ | ⊕ |
| 7) Explain any patient exclusions from analysis | – | ⊕ | ⊕ | ⊕ | – | – | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| 8) Describe how confounding was assessed and/or controlled. | U | ⊕ | – | ⊕ | U | U | ⊕ | ⊕ | U | ⊕ | ⊕ |
| 9) If applicable, explain how missing data were handled in the analysis | – | – | ⊕ | – | – | – | ⊕ | – | – | ⊕ | ⊕ |
| 10) Summarize patient response rates and completeness of data collection | – | ⊕ | – | ⊕ | – | – | ⊕ | ⊕ | – | ⊕ | ⊕ |
| 11) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained | – | – | – | – | – | – | ⊕ | – | – | – | – |
| Total score | 3 | 7 | 5 | 7 | 3 | 3 | 8 | 6 | 4 | 8 | 8 |
Definitions
The Oxford English Dictionary defines screen time as “the time spent using a device such as a computer, or games” [55]. In the current meta-analysis, according to the World Health Organization (WHO), screen time was defined as “the time spent passively watching screen-based entertainment (TV, computer, and mobile devices); this does not include active screen-based games where physical activity or movement is required” [56]. Therefore, TV watching, smart phone use, internet and computer use, and video games that are played in sedentary position are considered as screen time. As previously described by the WHO, adolescence is defined as the age range of 10–19 years old [57]. Overweight and obesity were defined as follows: (a) as Z score for the body mass index (BMI) for age with the cut-off points of > 1 to ≤2 standard deviations for overweight and values > 2 standard deviations for obesity [58]; (b) as the international age and sex specific cut-offs of BMI [≥85th percentile and less than 95th percentile for overweight and ≥ 95th for obesity [46]; and (c) as BMI cut-off of overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 [59].
Statistical analysis
STATA version 13 (STATA Corp, College Station, TX, USA) was used for data analysis and P-values less than 0.05 were considered as statistically significant. The studies reporting the odds ratio (OR) of overweight/obesity in people with highest versus lowest screen time were included in the two-class dose-response meta-analysis. In the two-class meta-analysis, the pooled OR with 95% confidence intervals (CI) were estimated using a weighted random-effect model (the DerSimonian-Laird approach). If the number of participants in the categories were not provided, equal number of participants in each category was assumed. Cochran’s Q and I-squared tests were used to identify between-study heterogeneity as follows: I2 <25%, no heterogeneity; I2 = 25–50%, moderate heterogeneity; and I2 > 50%, high heterogeneity [60].
The possible sources of heterogeneity were identified using subgrouping approach. For subgrouping, the possible confounders were chosen (e.g., continent, screen type, age group, setting, overweight/obesity status, sample size, and quality of study). Begg’s funnel plot was used to evaluate the publication bias followed by the Egger’s regression asymmetry test and Begg’s adjusted rank correlation for formal statistical assessment of funnel plot asymmetry. Because of an evidence of publication bias, trim-and-fill method was used for estimating potentially missing studies due to publication bias in the funnel plot and adjusting the overall effect estimate. For dose-response meta-analysis, only the studies that reported at least three categories for screen time and the odds of overweight/obesity were included in the dose-response meta-analysis. Accordingly, 13 different studies published in five articles were included [61–73]. The median point in each screen time category was identified; when medians were not reported, approximate medians were estimated using the midpoint of the lower and upper limits. When the lowest or highest screen time categories were open-ended, the screen time was calculated by assuming the similar interval for those categories and estimating the mid-point. The reference category was the lowest one, assuming OR and CIs of 1 for it. The potential non-linear associations were assessed using random-effects dose-response meta-analysis by defining the restricted cubic splines with three knots at fixed percentiles (10, 50, and 90%) of distribution, and were used to calculate study-specific ORs.
Results
Study characteristics
General characteristics of included studies are represented in Table 3. In the meta-analysis of the odds of overweight/obesity among high screen-user adolescents, a total of 44 studies were included. Also, some of the studies reported the results separately for both genders [28], or reported the separate results for each of the screen types [31, 33, 43, 46, 74], or according to overweight/obesity status [29, 41]. The study by Velásquez-Rodríguez [48] reported separate results for healthy adolescents and adolescents with insulin resistance. Generally, the studies had a cross-sectional design, or cross-sectional data from cohort studies were used for data analysis [32]. The age range of the participants in the included studies was 10–19 years old. The studies had been performed in the United States [29, 41, 43, 74], Brazil [22, 27, 35, 47], Egypt [44, 52], China [26, 39], Iran [45], Indonesia [34], Japan [32], Nigeria [51], Pakistan [42], Nepal [75], Bangladesh [31], Qatar [30], Australia [33], Mexico [28], India [46], Finland [48], Netherland [40], Turkey [49], England [50], and South Korea [53]. The screen time was assessed by validated questionnaires and overweight and obesity definitions were according to (a) as Z score for the BMI for age with the cut-off points of > 1 to ≤2 standard deviations for overweight and values > 2 standard deviations for obesity [58]; (b) as the international age and sex specific cut- offs of BMI [≥ 85th percentile and less than 95th percentile for overweight and ≥ 95th for obesity [46] and (c) as BMI cut-off of overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 [59]. All the studies included in the meta-analysis reported an adjusted OR that was adjusted according to the confounders, including age, gender, race, nationality, dietary behaviors, parents’ education, occupation, and socio-economic status.
Table 3.
The characteristics of studies that evaluated the association between overweight and obesity risk by increased screen time among adolescents
| Journal/ Year/ First author | Country | Setting/ num | Design | Age (y)/ gender | Overweight/ obesity status and definition | ST definition | Adjusted variables | Main findings |
|---|---|---|---|---|---|---|---|---|
| Revista Paulista de Pediatria/ 2021/ Dalamaria T [27] | Brazil | School/ 1387 | Cross-sectional | 14–18/ both | Obesity/ ≥85th percentile of age | Internet addiction | None | Increased odds of obesity in internet addicted adolescents [OR = 1.1; CI = 0.9–3.18]. Not adjusted |
| BMC Public Health/ 2020/ Zhang Y [39] | China | School/ 2264 | Cross-sectional | 12–15/ both | Obesity/ ≥85th percentile of age | TV, VG, PC | Age, sex, being the single child, ethnic minority, fruit and vegetable intake, sleep time, parents’ Education, fathers’ occupation. | Non-significant association between screen time and odds of obesity. |
| Nutrients/ 2020/ Lopez-Gonzalez D [28] | Mexico | School/309 girl; 340 boys | Cross-sectional | 12–17/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV, electronic games | Stratified by age and sex | Non-significant association between obesity and screen time. |
| Rev Bras Cineantropometri Desempenho Hum/ 2020/ Franceschin MJ [22] | Brazil | School/ 1015 | Cross-sectional | 15.3/ both | Overweight/ obesity defined as 1 ≤ BMI Z-score < 2 | TV, Video game or PC | Sex, age, type of school attended and dietary energy intake | A significant increased odds of overweight/ obesity in those with more than 2 hours per day TV watching (1.73 (1.24–2.42). The OR for PC and video games was 1.01 (0.71–1.45). |
| Revista Paulista de Pediatria/ 2020/ De Lima TR [35] | Brazil | School/ 583 | Cross-sectional | 11–17/ both | Overweight defined as BMI Z-score ≥ 1 | TV, Video game or PC | Gender, maternal schooling, alcohol consumption, smoking, screen time-sedentary behavior | Non-significant reduced risk of excess weight by increased screen time of more than 4 hours/day (0.87 CI = 0.59–1.30) |
| Public Health Nutrition/ 2020/ Cheng L [26] | China | School/ 2201 | Cross-sectional | 10/ both | Obesity/ ≥95th percentile of age | TV/video games/ PC/iPad/ phone | Sex, age and school location (rural or urban) with school as a random effect | Increased odds of obesity for those with more than 2 hours/ d screen time (1.53; CI = 0.95–2.09) |
| J Immigrant Minor health/ 2019/ Zulfiqar T [33] | Australia | Community/ 2115 girls and 2000 boys | Cross-sectional | 10–11/ both | Overweight/ obesity +BMI ≥ 25 kg/m2 | TV, electronic games | Sleep issues, breastfeeding, birth weight, siblings, foreign language spoken at home, maternal work status, family SEP, maternal partnership status | TV watching of more than 3 hours/ day in weekends was associated with odds of obesity in boys (1.4 (1.0,1.9) and girls (1.5 (1.1,1.9) P < 0.05 |
| In J Environ Res Pub Health/ 2019/ Kerkadi A [30] | Qatar | Community/ 1161 | Cross-sectional | 14–18/ both | Overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 | TV, Video game or PC | Age, nationality | No significant association between screen time of more than 2 hours/ day and risk of overweight/ obesity (OR = 1; CI = 0.7–1.4) |
| Plos One/ 2019/ Pabon et al. [41] | USA | Community/ 2358 + 546 | Cross-sectional | 13–17/ both | Overweight/ obesity defined as 1 ≤ BMI Z-score < 2 | TV, Video game | Age, sex, socioeconomic level, geographic area, ethnic group and exposure to television and / or video games. | No significant association between increased screen time and risk of overweight or obesity. |
| BMC Public Health/ 2019/ Haidar A [29] | USA | School/ 6716 | Cross-sectional | 14.88/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV, DVD, movies | Grade, gender, ethnicity, weight, SES, parents’ education level | No significant association between increased screen time and risk of overweight or obesity. |
| J Nepal Health Res Counc/ 2018/ Saha M [31] | Bangladesh | School/ 288 | Cross-sectional | 10–14/ both | Obesity defined as ≥95th percentile of age | TV, Video game, PC | None | No significant association between increased screen time and risk of overweight or obesity. |
| Tropical Doctor/ 2018/ Mansouri N [42] | Pakistan | School/ 887 | Cross-sectional | 11–15/ both | Overweight defined as ≤95th and ≥ 85th percentile of age | TV | Age, sex, type of school, sleeping soft drink consumption | Watching TV more than 2 hours/ day was associated with increased risk of overweight (6.42 (4.32–9.54) P < 0.0001) |
| Prev Chronic Dis/ 2018/ Hu EY [74] | USA | School/ 15,624 | Cross-sectional | 14–18/ both | Obesity defined as ≥95th percentile of age | TV, Video or computer game, PC use | Age, sex, and race/ethnicity | Increased risk of obesity for those with more than 3 hours/ day TV watching (1.38 (1.09–1.76) and more than 3 hours video game or PC use (1.19 (0.98–1.43) |
| BMC Res Notes/ 2018/ Godakanda I [43] | USA | School/ 880 | Cross-sectional | 14–15/ both | Overweight defined as BMI Z-score ≥ 1 | TV, Video/ DVD | Age, sex, ethnicity, schooling years | Television watching time ≥ 2 h/day (2.6 (1.7–3.8) and Video/DVD watching ≥2 h/day (3.1 (1.8–5.3) were associated with increased risk of overweight. |
| Egypt Ped Assoc Gazette/ 2016/ Talat MA [44] | Egypt | School/ 900 | Cross-sectional | 12–15/both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV | Age, gender, SES | More than 2 hours TV watching was associated with increased risk of obesity (1.36 CI = 0.45–6.8; P = 0.048) |
| BMJ Open/ 2016/ Piryani S [75] | Nepal | School/ 360 | Cross-sectional | 16–19/ both | Overweight defined as BMI Z-score ≥ 1 | TV | Age, sex, ethnicity, type of school, mother’s educational and occupation, family type, number of siblings, SES, watching TV and fruit consumption | Watching TV more than 2 hours/ day was associated with increased risk of obesity (OR = 8.86 (3.90 to 20.11) < 0.001 |
| Med J Islamic Rep Iran/ 2016/ Moradi G [45] | Iran | School/ 2506 | Cross-sectional | 10–12/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV, VG | Age, sex, SES | Screen time was associated with increased risk of overweight and obesity (1.41 (1.17–1.69) |
| Indian J Comm Health/ 2015/ Watharkar A [46] | India | School/ 806 | Cross-sectional | 12–15/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV, PC, cell phone | None | Increased risk of overweight obesity for those with more than 2 hours TV watching (OR = 3.72; CI = 2.38–5.83) or more than 2 hours computer or mobile phone use (OR = 1.68; CI = 1.09–2.57) |
| Revista Paulista de Pediatria/ 2015/ De Lucena JMS [47] | Brazil | School/ 2874 | Cross-sectional | 14–19/ both | Overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 | TV, PC, VG | None | Excessive screen time was associated with increased risk of overweight/ obesity (1.25 (0.93–1.67) |
| BMC Pediatr/ 2014/ Velásquez-Rodríguez CM [48] | Finland | Community/ 120 | Cross-sectional | 10–18/ both | Overweight defined as ≤95th and ≥ 85th percentile of age | TV | None | Increased risk of overweight in excessive TV watchers among adolescents with insulin resistance (OR = 2.39; CI = 0.94–6.05) but not among healthy adolescents. |
| Int J Obes/ 2013/ De Jong E [40] | Netherland | School/ 2004 + 2068 | Cross-sectional | 10–13/ both | Overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 | TV, PC | Family characteristics and lifestyle nutrition behaviours | No significant association between TV watching more than 1.5 hours or PC use of more than 30 minutes and overweight/ obesity. |
| JCRPE/ 2012/ Ercan S [49] | Turkey | School/ 8848 | Cross- sectional | 11–18/ both | Overweight 25 ≤ BMI ≤ 30 kg/m2 and obesity BMI ≥ 30 kg/m2 | TV, PC | None | Increased risk of overweight and obesity for those with more than 2 hours TV watching or PC use. |
| Pediatrics/ 2012/ Drake KM [50] | England | School/ 1718 | Cross-sectional | 12–18/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV, DVD, video game | Adolescent demographics (gender, grade in school, race [white/nonwhite]);screen time; academic performance; employment status; diet quality (fast food, fruit and vegetable consumption over the past week) | Screen time of 7.1–14 and > 14 hours/week was associated with increased obesity risk of OR = 1.28 CI = 1.06, 1.55; P < 0.05 and OR = 1.37 CI = 1.09, 1.71; P < 0.01 respectively. |
| J Korean Med Sci/ 2012/ Byun W [53] | Korea | Community/ 1033 | Cross-sectional | 12–18/ both | Overweight/ obesity defined as ≥95th percentile of age | TV, PC, video game | Age, sex, annual household income, and moderate-to-vigorous physical activity | Increased risk of overweight and obesity was observed by increased screen time |
| Ital J Pediatr / 2012/ Adesina AF [51] | Nigeria | School/ 690 | Cross-sectional | 10–19/ both | Overweight/ obesity defined as ≤95th and ≥ 85th and ≥ 95th percentile of age respectively | TV | None | Increased risk of overweight and obesity was observed by increased screen time |
| Childhood Obesity/ 2011/ El-Gilany AH [52] | Egypt | School/ 953 | Cross-sectional | 14–19/ both | Overweight defined as ≤95th and ≥ 85th percentile of age | TV, PC | Age, sex, socioeconomic level, geographic area, ethnicity | Increased risk of overweight/ obesity for those with more than 2 hours TV watching (2.6 (1.7–3.9) or more than 2 hours computer use (1.8 (1.3–2.5) |
| J Epidemiol/ 2009/ Sun Y [32] | Japan | School/ 2842 | Cross-sectional data of an original cohort | 12–13/ both | Overweight 25 ≤ BMI ≤ 30 kg/m2 | TV, VG | Age, parental overweight, and other lifestyle variables | Watching TV more than 3 hours/ d was associated with increased risk of overweight in boys (OR = 1.79; CI = 1.21–2.67 and girls OR = 2.37; CI = 1.55–3.62; P < 0.001 |
| Int J Pediatr Obes/ 2008/ Collins AE [34] | Indonesia | School/ 1758 | Cross-sectional | 12–15/ both | Obesity defined as BMI ≥ 25 kg/m2 | PC, PS | None | Increased risk of obesity in those with more than 3 hours/ d PC use (OR = 1.85; CI = 1.04–3.29) or play station use (OR = 1.94; CI = 1.23–3.05) |
Abbreviations: BMI Body mass index, TV Television, ST Screen time, SBP Systolic blood pressure, DBP Diastolic blood pressure, PC Personal computer, DVD Digital video discs, VCDs Video compact disc digital, SEP Socioeconomic position, SES Socioeconomic status, ST Measurement in all of the studies was performed by questionnaire. All of the included participants were apparently healthy
The results of the meta-analysis
In the current meta-analysis, after searching the electronic databases, a total of 6291 articles were retrieved (Fig. 1). After removing 2600 duplicated studies and 1535 records according to title/abstarct irrelevancy, 2156 artciles remained for final full-text screening. Then, 2112 manuscripts were removed due to not meeting the inclusion criteria. Finally, 44 manuscripts with a total number of 112,489 participants were included in the final meta-analysis. The included stdueis had a cross-sectional design and recruitted both genders.
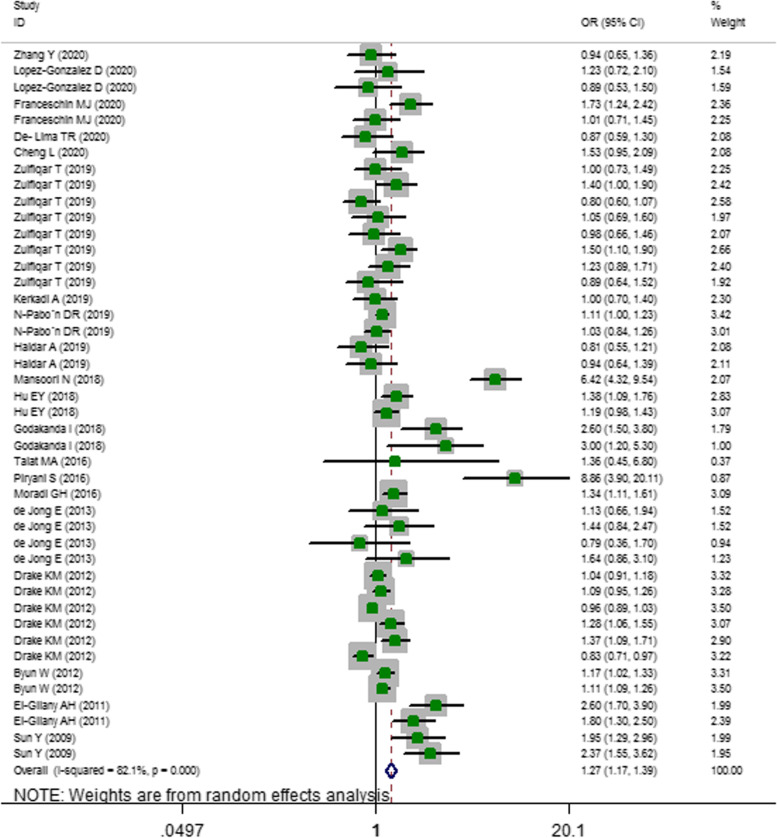
The results of the two-class meta-analysis is presented in Fig. 2. As can be seen, adolescents in the highest category of screen time were 1.27 times more likely to develop overweight/obesity compared to those in the lowest category (OR = 1.273; 95%CI = 1.166–1.390; P < 0.001; I-squared = 82.1%).
Fig. 2.
Odds ratio (OR) with 95% confidence interval (CI) of overweight/ obesity in highest versus lowest screen user adolescents. I2 represents the degree of heterogeneity
The results of subgrouping is shown in Table 4. Subgrouping according to continent reduced heterogeneity to some degree. For example, in the studies carried out in the United States, the heterogeneity reduced to 39.9%. Similarly, setting also was a possible source of heterogenity since subgropuing by setting reduced the heterogenity of community-based studies to 21.2%. However, other parameters were not potent sources of heterogeneity.
Table 4.
Subgroup analysis for the odds of overweight/ obesity in highest versus lowest screen-user adolescents
| Group | No. of studies* | OR (95% CI) | P within group | P between group * | P heterogeneity | I2, % |
|---|---|---|---|---|---|---|
| Total | 44 | 1.273 1.166 1.390 | < 0.001 | < 0.001 | 82.1 | |
| Continent | < 0.001 | |||||
| America | 11 | 1.115 1.002 1.241 | 0.046 | 0.083 | 39.9 | |
| Europe | 10 | 1.080 0.966 1.208 | 0.276 | 0.002 | 66.2 | |
| Asia | 11 | 2.014 1.450 2.798 | < 0.001 | < 0.001 | 90.9 | |
| Oceania | 8 | 1.099 0.927 1.304 | 0.278 | 0.056 | 49.1 | |
| Africa | 4 | 1.646 1.018 2.660 | 0.042 | < 0.001 | 86.9 | |
| Screen type | < 0.001 | |||||
| TV | 16 | 1.813 1.420 2.315 | < 0.001 | < 0.001 | 86.7 | |
| PC | 3 | 1.467 0.950 2.265 | 0.509 | 0.159 | 45.7 | |
| VG | 5 | 1.114 0.808 1.536 | 0.084 | 0.014 | 67.9 | |
| TV + VG | 5 | 1.094 0.959 1.248 | 0.184 | 0.107 | 47.5 | |
| VG + PC | 2 | 1.106 1.030 1.187 | 0.005 | 0.612 | 0 | |
| TV + VG + PC | 13 | 1.068 0.974 1.172 | 0.163 | 0.002 | 60.7 | |
| Age group | < 0.001 | |||||
| < 15 | 23 | 1.375 1.131 1.672 | 0.001 | < 0.001 | 81.9 | |
| ≥ 15 | 6 | 1.470 1.076 2.008 | 0.016 | < 0.001 | 82.8 | |
| Both | 15 | 1.126 1.032 1.228 | 0.008 | < 0.001 | 76.4 | |
| Setting | < 0.001 | |||||
| School | 31 | 1.405 1.228 1.608 | < 0.001 | < 0.001 | 86.6 | |
| Community | 13 | 1.109 1.040 1.182 | 0.002 | 0.229 | 21.2 | |
| Obesity status | < 0.001 | |||||
| Obesity | 11 | 1.109 0.964 1.275 | 0.150 | 0.001 | 67.0 | |
| Overweight | 9 | 1.567 1.282 1.916 | < 0.001 | < 0.001 | 84.1 | |
| Overweight/ obesity | 24 | 1.271 1.105 1.463 | 0.001 | < 0.001 | 87 | |
| Sample size | < 0.001 | |||||
| 1000 > | 11 | 2.024 1.303 3.144 | 0.002 | < 0.001 | 90.9 | |
| 1000–5000 | 27 | 1.121 1.049 1.198 | 0.001 | < 0.001 | 59.9 | |
| ≥ 5000 | 6 | 1.323 1.017 1.722 | 0.037 | 0.001 | 75.7 | |
| Study quality * | < 0.001 | |||||
| Low | 0 | – | – | – | – | |
| Moderate | 31 | 1.259 1.085 1.461 | < 0.001 | < 0.001 | 80.3 | |
| High | 13 | 1.282 1.146 1.435 | 0.002 | < 0.001 | 84.4 | |
| Adjusted covariates | < 0.001 | |||||
| Age, sex, nationality, SES | 7 | 1.239 1.116 1.377 | < 0.001 | 0.586 | 0 | |
| Age, sex, nationality, SES, other demographic variables | 14 | 1.454 1.251 1.690 | < 0.001 | < 0.001 | 87.3 | |
| Age, sex, nationality, SES, other demographic variables, dietary habits | 23 | 1.091 0.982 1.212 | 0.107 | < 0.001 | 64.8 |
*low quality = 0–3; moderate quality = 4–7; high quality ≥8; all of the included studies were in moderate quality group therefore, subgrouping was not performed
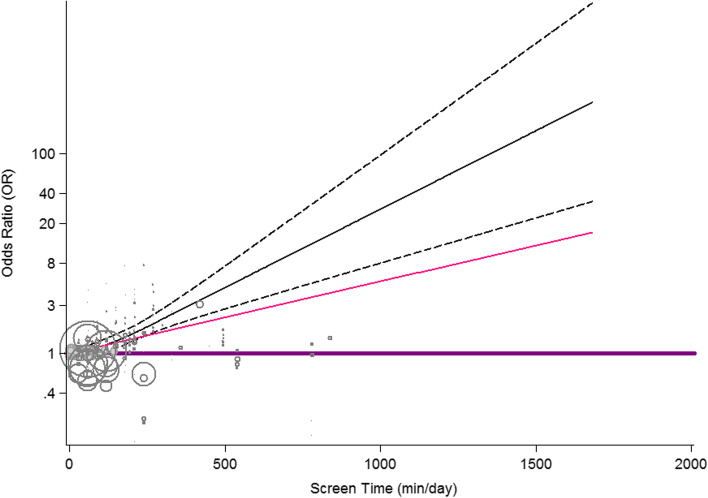
The results of dose-response relationship between screen time and overweight/obesity is presented in Fig. 3. There was no evidence of non-linear association between increased screen time and risk of overweight/obesity (P-nonlinearity = 0.311).
Fig. 3.
Dose–response association between screen time and odds of overweight/ obesity. Linear relation (solid line) and 95% CI (dashed lines) of pooled OR of obesity by 1 min/day increment of screen time (p- nonlinearity = 0.310) among adolescents
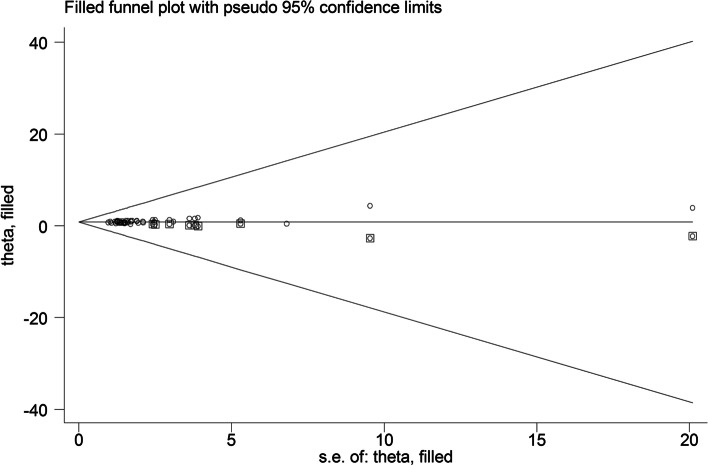
Funnel plots indicating publication bias are presented in Fig. 4. The results of Begg’s and Egger’s tests showed some evidence of publication bias (Egger’s P-value = 0.001; Begg’s P-value = 0.001). Therefore, trim-and-fill analysis was performed (Fig. 5) and the obtained results were reported (95%OR = 1.472; 95% CI = 1.083–2.068; P < 0.001).
Fig. 4.
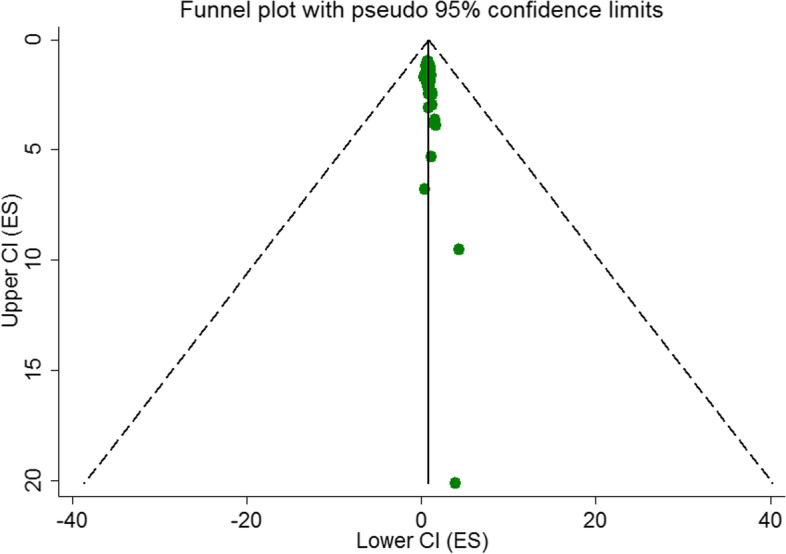
Begg’s funnel plot (with pseudo 95% CIs) of the odds of overweight/ obesity in highest versus lowest screen time categories among adolescents
Fig. 5.
Filled funnel plot with pseudo 95% confidence limits for studies evaluating the association between screen time and overweight/ obesity among adolescents [OR = 1.472; CI = 1.083, 2.068; P < 0.001]
Discussion
In the current meta-analysis, for the first time, we summarized the results of studies that evaluated the association between screen time and overweight/obesity risk among adolescents. In addition, in a large sample size (n = 112,489), we witnessed that high screen time was associated with 1.27-time higher chance of overweight/obesity among adolescents. No evidence of non-linear association was observed in the dose-response analysis.
Previous population-based studies have revealed the obesity-promoting effects of high screen time. Lopez-Gonzalez [28] evaluated more than 7511 registered schools and reported that high screen time was considered as an obesogenic factor. Several other studies also revealed that screen time more than two or 3h per day increased the risk of obesity [26, 33]. Internet addicted adolescents had also elevated risk of obesity in one study [27]. However, several other studies reported no significant association between obesity and screen time [30, 35, 41]. The possible strong reason for this inconsistency might be attributed to the type of screen (e.g., TV, video games, PCs, etc.) used in different studies.
In this study, we also performed subgroup analysis. According to the results, the studies that defined video games as their screen failed to reveal a positive association between screen time and obesity [31, 39, 41]. In our meta-analysis, video games alone or in combination with other screen types failed to show a positive obesity-promoting effect. In the study by Sun et al. [32], the positive association between video game playing and risk of obesity was only observed among girls and not boys. Zulfiqar et al. [33], also reported the positive association between obesity and TV watching, but not for video games. Several studies even showed the negative association between active video games and obesity. In the study by Strahan et al. [76], active video games reduced the chance of obesity among adolescents. This is possibly because some video games can increase physical activity and physical health. In a meta-analysis by Primack et al., video games were associated with 69% improve in psychological therapy outcomes and 50% improve in physical activity outcomes [77]. In another study by Williams, active video games were introduced as effective tools to improve physical activity among adolescents and were considered as a more acceptable and sustainable approach than many conventional methods [78].
In our meta-analysis, the most important obesogenic screen was TV (OR = 1.813; 95%CI: 1.420–2.315, P < 0.001). In the study by Franceschin et al. [22], adolescents watching TV for more than 2h per day had almost doubled chance of being obese compared to those watching TV for less than 2h per day (OR = 1.73; 95% CI = 1.24–2.42); but the association was not significant for playing video games or using the PC. Therefore, it seems that TV watching is a stronger motivator of obesity among adolescents. Also, the age group is a determinant of screen type use and the consequent obesity. In our study, most of the included studies had been performed in adolescents less than 15 years old and the association between screen time and overweight/obesity in this age group was stronger (P < 0.001) because at lower ages, children and adolescents have less structured time than older adolescents and most of this unstructured time is filled by watching TV [51, 79]. Another important finding in our subgrouping was the role of setting. In school-based studies, the association between screen time and overweight/obesity was more pronounced than other study types (OR = 1.405; 95% CI: 1.228–1.608; P < 0.001) because adolescents usually have more tendency to eat calorie foods in restaurants. Most of the adolescents buy lunch at school canteen and restaurants and are more likely to develop overweight and obesity [80].
High screen time, as a sedentary behavior, reduces lipoprotein lipase activity (LPL) and leads to reduced plasma triglycerides’ absorption by skeletal muscles, reduced HDL level and postprandial increase in serum lipids, that consequently results in fat deposition in vessels or adipose tissue [81–83]. Moreover, increased screen time increases food intake. Previous studies revealed that television watching increases motivated response to food intake and snacking behavior among children and adolescents [4, 84–87]; this is also true for video games [88–90] and personal computer use [91, 92]. More importantly, several TV food advertisements promote the consumption of junk food and fast foods and increase the risk of obesity [93–98]. Therefore, the association between obesity and screen use is a multi-dimensional factor. Also, the results of included studies in our meta-analysis were reported for both genders; therefore, it was not possible to give gender-specific results.
This study had some limitations. First, this study had a cross-sectional design, which precludes causal inference. Second, the data collection method for screen time measurement was self-reported questionnaires that might be biased. Third, we were not able to perform subgroup analysis for some important confounders, such as eating food while watching screen, type of video games (active or non-active), and gender because the articles had not mentioned such information.
However, this is the first meta-analysis reporting the association between screen time and overweight/obesity among adolescents. We raised concerns among parents, health care professionals, educators, and researchers about the effects of screen time on the health of adolescents. Our study has some important clinical and health implications for policy makers to develop strategies to encourage adolescents to be more physically active and to apply some restrictions for school-based meal servings. They can also improve access of adolescents to opportunities for physical activity, as is the case with state laws related to the quantity and quality of physical education. Also, parents should pay more attention to the adolescents’ screen-based behaviors and apply some at-home restrictions. Setting restrictions on screen use at certain times is a great way to protect adolescents from potentially harmful online activities and encourages them to use their time appropriately.
Conclusion
The current meta-analysis is the first study providing quantitative results for the association between different screen types and overweight/obesity among adolescents. Further studies are warranted to focus on the effects of gender, different screen types and video games to better explain the discrepancies in the obtained results.
Supplementary Information
Acknowledgements
The research protocol was approved and supported by Student Research Committee, Tabriz University of Medical Sciences (Grant Number: 68712).
Authors’ contributions
All authors have read and approved the manuscript; MAF and PH, supervised the project, performed the search, extraction and wrote the first draft of the manuscript, MAF also analyzed the data. GS was involved in search, extraction and revision of the paper. GS and ES, were involved in data extraction and SA was involved in data analysis and manuscript revision.
Funding
None.
Availability of data and materials
The data that support the findings of this study are available from Tabriz University of Medical Sciences but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of corresponding author.
Declarations
Ethics approval and consent to participate
The protocol of the current work has been registered in the PROSPERO system (Registration number: CRD42021233899). Also, the research has been approved by the ethics committee of Tabriz University of Medical Sciences (Code: IR.TBZMED.VCR.REC.1400.374; Grant number: 68712).
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Suchert V, Hanewinkel R, Isensee B. Screen time, weight status and the self-concept of physical attractiveness in adolescents. J Adolesc. 2016;48:11–17. doi: 10.1016/j.adolescence.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Pate RR, Mitchell J, Byun W, Dowda M. Sedentary behaviour in youth. Br J Sports Med. 2011;45(11):906e913. doi: 10.1136/bjsports-2011-090192. [DOI] [PubMed] [Google Scholar]
- 3.Hardy LL, Dobbins T, Booth ML, Denney-Wilson E, Okely AD. Sedentary behaviours among Australian adolescents. Aust New Zealand. J Public Health. 2006;30(6):534e540. doi: 10.1111/j.1467-842x.2006.tb00782.x. [DOI] [PubMed] [Google Scholar]
- 4.Domoff SE, Sutherland E, Yokum S, Gearhardt AN. The association of adolescents’ television viewing with body mass index percentile, food addiction, and addictive phone use. Appetite. 2021:157;104990. [DOI] [PMC free article] [PubMed]
- 5.Fairman RT, Weaver SR, Akani BC, Dixon K, Popova L. “You have to vape to make it through”: E-cigarette outcome expectancies among youth and parents. Am J Health Behav. 2021;45(5):933–946. doi: 10.5993/AJHB.45.5.13. [DOI] [PubMed] [Google Scholar]
- 6.Rideout V, Robb M. The common sense census: media use by tweens and teens. Common Sense ; 2021. pp. 1–104. [Google Scholar]
- 7.Throuvala MA, Griffiths MD, Rennoldson M, Kuss DJ. The role of recreational online activities in school-based screen time sedentary behaviour interventions for adolescents: a systematic and critical literature review. Int J Ment Heal Addict. 2021;19:1065–115.
- 8.Twenge JM, Martin GN, Campbell WK. Decreases in psychological well-being among American adolescents after 2012 and links to screen time during the rise of smartphone technology. Emotion. 2018;18(6):765–780. doi: 10.1037/emo0000403. [DOI] [PubMed] [Google Scholar]
- 9.Zhou J, Li Z, Meng H, Chang Y-C, Peng N-H, Wei B. Chinese parental awareness of Children's COVID-19 protective measures. Am J Health Behav. 2021;45(4):657–664. doi: 10.5993/AJHB.45.4.5. [DOI] [PubMed] [Google Scholar]
- 10.Schroeder K, Kubik MY, Sirard JR, Lee J, Fulkerson JA. Sleep is inversely associated with sedentary time among youth with obesity. Am J Health Behav. 2020;44(6):756–764. doi: 10.5993/AJHB.44.6.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamolthip R, Fung XC, Lin C-Y, Latner JD, O'Brien KS. Relationships among physical activity, health-related quality of life, and weight stigma in children in Hong Kong. Am J Health Behav. 2021;45(5):828–842. doi: 10.5993/AJHB.45.5.3. [DOI] [PubMed] [Google Scholar]
- 12.Lutz M, Vargas C, Stojanova J, Arancibia M. Diet and depressive disorders. Arch Clin Psychiatry (São Paulo) 2021;48:117–122. [Google Scholar]
- 13.Tremblay MS, LeBlanc AG, Janssen I, Kho ME, Hicks A, Murumets K, et al. Canadian sedentary behaviour guidelines for children and youth. Appl Physiol Nutr Metab. 2011;36(1):59–64. doi: 10.1139/H11-012. [DOI] [PubMed] [Google Scholar]
- 14.Sisson SB, Church TS, Martin CK, Tudor-Locke C, Smith SR, Bouchard C, et al. Profiles of sedentary behavior in children and adolescents: the US National Health and nutrition examination survey, 20012006. Int J Pediatr Obes. 2009;4(4):353–359. doi: 10.3109/17477160902934777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Currie C, Zanotti C, Morgan A. Health policy for children and adolescents. WHO Regional Office for Europe; 2012. Social determinants of health and well-being among young people health behaviour in school-aged children (HBSC): international report from the 2009/2010 survey; pp. 1–252. [Google Scholar]
- 16.Tang D, Bu T, Feng Q, Liu Y, Dong X. Differences in overweight and obesity between the north and south of China. Am J Health Behav. 2020;44(6):780–793. doi: 10.5993/AJHB.44.6.4. [DOI] [PubMed] [Google Scholar]
- 17.Coombs NA, Stamatakis E. Associations between objectively assessed and questionnaire-based sedentary behaviour with BMI-defined obesity among general population children and adolescents living in England. BMJ Open. 2015;5(6):e007172. doi: 10.1136/bmjopen-2014-007172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guillaume M, Lapidus L, Björntorp P, Lambert A. Physical activity, obesity, and cardiovascular risk factors in children. The Belgian Luxembourg child study II. Obes Res. 1997;5(6):549–556. doi: 10.1002/j.1550-8528.1997.tb00576.x. [DOI] [PubMed] [Google Scholar]
- 19.Burke V, Beilin LJ, Simmer K, Oddy WH, Blake KV, Doherty D, et al. Predictors of body mass index and associations with cardiovascular risk factors in Australian children: a prospective cohort study. Int J Obes. 2005;29(1):15–23. doi: 10.1038/sj.ijo.0802750. [DOI] [PubMed] [Google Scholar]
- 20.Martinez-Gomez D, Rey-López JP, Chillón P, Gómez-Martínez S, Vicente-Rodríguez G, Martín-Matillas M, et al. Excessive TV viewing and cardiovascular disease risk factors in adolescents. The AVENA cross-sectional study. BMC Public Health. 2010;10:274. doi: 10.1186/1471-2458-10-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mota J, Ribeiro JC, Carvalho J, Santos MP, Martins J. Television viewing and changes in body mass index and cardiorespiratory fitness over a two-year period in schoolchildren. Pediatr Exerc Sci. 2010;22(2):245–253. doi: 10.1123/pes.22.2.245. [DOI] [PubMed] [Google Scholar]
- 22.Franceschin MJ, da Veiga GV. Association of cardiorespiratory fitness, physical activity level, and sedentary behaviour with overweight in adolescents. Revista Brasileira de Cineantropometria e Desempenho Humano. 2020;22:1–12. [Google Scholar]
- 23.Safiri S, Kelishadi R, Qorbani M, Abbasi-Ghah-Ramanloo A, Motlagh ME, Ardalan G, et al. Screen time and its relation to cardiometabolic risk among children and adolescents: the CASPIAN-III study. Iran J Public Health. 2015;44(1):35–44. [Google Scholar]
- 24.Ulaganathan V, Kandiah M, Shariff ZM. A case–control study on the association of abdominal obesity and hypercholesterolemia with the risk of colorectal cancer. J Carcinogenesis. 2018;17. [DOI] [PMC free article] [PubMed]
- 25.Putrawan HA, Antariksa B, Yunus F, Basalamah MA, Nurwidya F. Prevalence of pulmonary hypertension in indonesian patients with stable chronic obstructive pulmonary disease. J Nat Sci Biol Med. 2019;10(1):49. [Google Scholar]
- 26.Cheng L, Li Q, Hebestreit A, Song Y, Wang D, Cheng Y, et al. The associations of specific school-and individual-level characteristics with obesity among primary school children in Beijing, China. Public Health Nutrition. 2020;23(10):1838–1845. doi: 10.1017/S1368980019004592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dalamaria T, De Jesus Pinto W, Dos Santos Farias E, De Souza OF. Internet addiction among adolescents in a western brazilian amazonian city. Revista Paulista de. Pediatria. 2021;39. [DOI] [PMC free article] [PubMed]
- 28.Lopez-Gonzalez D, Partida-Gaytán A, Wells JC, Reyes-Delpech P, Avila-Rosano F, Ortiz-Obregon M, et al. Obesogenic lifestyle and its influence on adiposity in children and adolescents, evidence from mexico. Nutrients. 2020;12(3). [DOI] [PMC free article] [PubMed]
- 29.Haidar A, Ranjit N, Archer N, Hoelscher DM. Parental and peer social support is associated with healthier physical activity behaviors in adolescents: a cross-sectional analysis of Texas school physical activity and nutrition (TX SPAN) data. BMC Public Health. 2019;19(1). [DOI] [PMC free article] [PubMed]
- 30.Kerkadi A, Sadig AH, Bawadi H, Thani AAMA, Chetachi WA, Akram H, et al. The relationship between lifestyle factors and obesity indices among adolescents in Qatar. Int J Environ Res Public Health. 2019;16(22). [DOI] [PMC free article] [PubMed]
- 31.Saha M, Adhikary DK, Parvin I, Sharma YR, Akhter F, Majumder M. Obesity and its risk factors of among school children in Sylhet, Bangladesh. J Nepal Health Res Counc. 2018;16(2):205–208. [PubMed] [Google Scholar]
- 32.Sun Y, Sekine M, Kagamimori S. Lifestyle and overweight among Japanese adolescents: the Toyama birth cohort study. J Epidemiol. 2009;19(6):303–310. doi: 10.2188/jea.JE20080095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zulfiqar T, Strazdins L, Dinh H, Banwell C, D'Este C. Drivers of overweight/obesity in 4-11 year old children of Australians and immigrants; evidence from growing up in Australia. J Immigr Minor Health. 2019;21(4):737–750. doi: 10.1007/s10903-018-0841-3. [DOI] [PubMed] [Google Scholar]
- 34.Collins AE, Pakiz B, Rock CL. Factors associated with obesity in Indonesian adolescents. Int J Pediatr Obes. 2008;3(1):58–64. doi: 10.1080/17477160701520132. [DOI] [PubMed] [Google Scholar]
- 35.De Lima TR, Moraes MS, Andrade JHC, De Farias JM, Silva DAS. Associated factors with the isolated and simultaneous presence of overweight and abdominal obesity in adolescents. Revista Paulista de Pediatria. 2020;38. [DOI] [PMC free article] [PubMed]
- 36.Alyoubi RA, Kobeisy SA, Souror HN, Alkhaldi FA, Aldajam MA, Allebdi KS, et al. Active screen time habits and headache features among adolescents and young adults in Saudi Arabia. Int J Pharm Res Allied Sci. 2020;9(4):81–86. [Google Scholar]
- 37.Amigo I, Peña E, Errasti JM, Busto R. Sedentary versus active leisure activities and their relationship with sleeping habits and body mass index in children of 9 and 10 years of age. J Health Psychol. 2016;21(7):1472–1480. doi: 10.1177/1359105314556161. [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 39.Zhang Y, Zhang X, Li J, Zhong H, Pan CW. Associations of outdoor activity and screen time with adiposity: findings from rural Chinese adolescents with relatively low adiposity risks. BMC Public Health. 2020;20(1). [DOI] [PMC free article] [PubMed]
- 40.De Jong E, Visscher TLS, Hirasing RA, Heymans MW, Seidell JC, Renders CM. Association between TV viewing, computer use and overweight, determinants and competing activities of screen time in 4- to 13-year-old children. Int J Obes. 2013;37(1):47–53. doi: 10.1038/ijo.2011.244. [DOI] [PubMed] [Google Scholar]
- 41.Rincón-Pabón D, Urazán-Hernández Y, González-Santamaría J. Association between the time spent watching television and the sociodemographic characteristics with the presence of overweight and obesity in Colombian adolescents (secondary analysis of the ENSIN 2010) Plos One. 2019;14(5):e0216455. doi: 10.1371/journal.pone.0216455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mansoori N, Nisar N, Shahid N, Mubeen SM, Ahsan S. Prevalence of obesity and its risk factors among school children in Karachi, Pakistan. Trop Doct. 2018;48(4):266–269. doi: 10.1177/0049475518786664. [DOI] [PubMed] [Google Scholar]
- 43.Godakanda I, Abeysena C, Lokubalasooriya A. Sedentary behavior during leisure time, physical activity and dietary habits as risk factors of overweight among school children aged 14-15 years: case control study. BMC Res Notes. 2018;11(1):186. doi: 10.1186/s13104-018-3292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Talat MA, El Shahat E. Prevalence of overweight and obesity among preparatory school adolescents in urban Sharkia governorate, Egypt. Egypt Pediatr Assoc Gaz. 2016;64(1):20–25. [Google Scholar]
- 45.Moradi G, Mostafavi F, Azadi N, Esmaeilnasab N, Nouri B. Evaluation of screen time activities and their relationship with physical activity, overweight and socioeconomic status in children 10-12 years of age in Sanandaj, Iran: a cross-sectional study in 2015. Med J Islam Repub Iran. 2016;30(1). [PMC free article] [PubMed]
- 46.Watharkar A, Nigam S, Martolia DS, Varma P, Barman SK, Sharma RP. Assessment of risk factors for overweight and obesity among school going children in Kanpur, Uttar Pradesh. Indian J Community Health. 2015;27(2):216–222. [Google Scholar]
- 47.De Lucena JMS, Cheng LA, Cavalcante TLM, Da Silva VA, De Farias JC. Prevalence of excessive screen time and associated factors in adolescents. Revista Paulista de Pediatria. 2015;33(4):407–414. doi: 10.1016/j.rpped.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Velásquez-Rodríguez CM, Velásquez-Villa M, Gómez-Ocampo L, Bermúdez-Cardona J. Abdominal obesity and low physical activity are associated with insulin resistance in overweight adolescents: a cross-sectional study. BMC Pediatr. 2014;14:258. doi: 10.1186/1471-2431-14-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ercan S, Dallar YB, Önen S, Engiz O. Prevalence of obesity and associated risk factors among adolescents in Ankara, Turkey. J Clin Res Pediatr Endocrinol. 2012;4(4):204–207. doi: 10.4274/Jcrpe.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drake KM, Beach ML, Longacre MR, MacKenzie T, Titus LJ, Rundle AG, et al. Influence of sports, physical education, and active commuting to school on adolescent weight status. Pediatrics. 2012;130(2):e296–e304. doi: 10.1542/peds.2011-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Adesina AF, Peterside O, Anochie I, Akani NA. Weight status of adolescents in secondary schools in port Harcourt using body mass index (BMI) Ital J Pediatr. 2012;38:31. doi: 10.1186/1824-7288-38-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.El-Gilany AH, El-Masry R. Overweight and obesity among adolescent school students in Mansoura, Egypt. Child Obes. 2011;7(3):215–222. [Google Scholar]
- 53.Byun W, Dowda M, Pate RR. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27(4):388–394. doi: 10.3346/jkms.2012.27.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cho CE, Taesuwan S, Malysheva OV, Bender E, Tulchinsky NF, Yan J. Trimethylamine-N-oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res. 2017;61:1600324. doi: 10.1002/mnfr.201600324. [DOI] [PubMed] [Google Scholar]
- 55.Oxford University Press . Oxford English Dictionary. Oxford: Oxford University Press; 2020. [Google Scholar]
- 56.World Health Organization . Guidelines on physical activity, sedentary behaviour and sleep for children under 5 years of age. 2020. [PubMed] [Google Scholar]
- 57.Organization, W.H . Adolescent health in the South-East Asia region. 2020. [Google Scholar]
- 58.DO., M The new WHO child growth standards. Paediatr Croat Suppl. 2008;52(SUPP.1):13–17. [Google Scholar]
- 59.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Anandam A, Akinnusi M, Kufel T, Porhomayon J, El-Solh AA. Effects of dietary weight loss on obstructive sleep apnea: a meta-analysis. Sleep Breath. 2013;17:227–234. doi: 10.1007/s11325-012-0677-3. [DOI] [PubMed] [Google Scholar]
- 61.Li L, Shen T, Wen LM, Wu M, He P, Wang Y, et al. Lifestyle factors associated with childhood obesity: a cross-sectional study in Shanghai, China. BMC Res Notes. 2015;8(1). [DOI] [PMC free article] [PubMed]
- 62.Bhadoria AS, Kapil U, Kaur S. Association of duration of time spent on television, computer and video games with obesity amongst children in national capital territory of Delhi. Int J Prev Med. 2015. [DOI] [PMC free article] [PubMed]
- 63.Bingham DD, Varela-Silva MI, Ferrão MM, Augusta G, Mourão MI, Nogueira H, et al. Socio-demographic and behavioral risk factors associated with the high prevalence of overweight and obesity in portuguese children. Am J Hum Biol. 2013;25(6):733–742. doi: 10.1002/ajhb.22440. [DOI] [PubMed] [Google Scholar]
- 64.Koleilat M, Harrison GG, Whaley S, McGregor S, Jenks E, Afifi A. Preschool enrollment is associated with lower odds of childhood obesity among WIC participants in LA County. Matern Child Health J. 2012;16(3):706–712. doi: 10.1007/s10995-011-0774-0. [DOI] [PubMed] [Google Scholar]
- 65.Taylor AW, Winefield H, Kettler L, Roberts R, Gill TK. A population study of 5 to 15 year olds: full time maternal employment not associated with high BMI. The importance of screen-based activity, reading for pleasure and sleep duration in children's BMI. Matern Child Health J. 2012;16(3):587–599. doi: 10.1007/s10995-011-0792-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Balaban G, Motta ME, Silva GA. Early weaning and other potential risk factors for overweight among preschool children. Clinics (Sao Paulo) 2010;65(2):181–187. doi: 10.1590/S1807-59322010000200010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ. Television viewing, computer use, and BMI among U.S. children and adolescents. J Phys Act Health. 2009;6(Suppl 1):S28–S35. doi: 10.1123/jpah.6.s1.s28. [DOI] [PubMed] [Google Scholar]
- 68.Khader Y, Irshaidat O, Khasawneh M, Amarin Z, Alomari M, Batieha A. Overweight and obesity among school children in Jordan: prevalence and associated factors. Matern Child Health J. 2009;13(3):424–431. doi: 10.1007/s10995-008-0362-0. [DOI] [PubMed] [Google Scholar]
- 69.Steele RM, Van Sluijs EMF, Cassidy A, Griffin SJ, Ekelund U. Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old British children. Am J Clin Nutr. 2009;90(5):1185–1192. doi: 10.3945/ajcn.2009.28153. [DOI] [PubMed] [Google Scholar]
- 70.Da Costa Ribeiro I, Taddei JAAC, Colugnatti F. Obesity among children attending elementary public schools in Sao Paulo, Brazil: a case-control study. Public Health Nutr. 2003;6(7):659–663. doi: 10.1079/phn2003473. [DOI] [PubMed] [Google Scholar]
- 71.Lagiou A, Parava M. Correlates of childhood obesity in Athens, Greece. Public Health Nutr. 2008;11(9):940–945. doi: 10.1017/S1368980008002462. [DOI] [PubMed] [Google Scholar]
- 72.Stettler N, Signer TM, Suter PM. Electronic games and environmental factors associated with childhood obesity in Switzerland. Obes Res. 2004;12(6):896–903. doi: 10.1038/oby.2004.109. [DOI] [PubMed] [Google Scholar]
- 73.Utter J, Scragg R, Schaaf D. Associations between television viewing and consumption of commonly advertised foods among New Zealand children and young adolescents. Public Health Nutr. 2006;9(5):606–612. doi: 10.1079/phn2005899. [DOI] [PubMed] [Google Scholar]
- 74.Hu EY, Ramachandran S, Bhattacharya K, Nunna S. Obesity among high school students in the United States: risk factors and their population attributable fraction. Prev Chronic Dis. 2018;15:E137. doi: 10.5888/pcd15.180122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Piryani S, Baral KP, Pradhan B, Poudyal AK, Piryani RM. Overweight and its associated risk factors among urban school adolescents in Nepal: a cross-sectional study. BMJ Open. 2016;6(5):e010335. doi: 10.1136/bmjopen-2015-010335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Strahan BE, Elder JH. Video game playing effects on obesity in an adolescent with autism spectrum disorder: a case study. Autism Res Treat. 2015;2015. [DOI] [PMC free article] [PubMed]
- 77.Primack BA, Carroll MV, McNamara M, Klem ML, King B, Rich M, et al. Role of video games in improving health-related outcomes: a systematic review. Am J Prev Med. 2012;42(6):630–638. doi: 10.1016/j.amepre.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Williams WM, Ayres CG. Can active video games improve physical activity in adolescents? A review of RCT. Int J Environ Res Public Health. 2020;17(2):669. doi: 10.3390/ijerph17020669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rivera IR, Silva MA, Silva RD, Oliveira BA, Carvalho AC. Physical inactivity, TV-watching hours and body composition in children and adolescents. Arq Bras Cardiol. 2010;95(2):159–165. doi: 10.1590/s0066-782x2010005000065. [DOI] [PubMed] [Google Scholar]
- 80.Goyal JP, Kumar N, Parmar I, Shah VB, Patel B. Determinants of overweight and obesity in affluent adolescent in Surat city, South Gujarat region, India. Indian J Commun Med. 2011;36(4):296–300. doi: 10.4103/0970-0218.91418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pitanga FJG, Alves CFA, Pamponet ML, Medina MG, Aquino R. Screen time as discriminator for overweight, obesity and abdominal obesity in adolescents. Revista Brasileira de Cineantropometria e Desempenho Humano. 2016;18(5):539–547. [Google Scholar]
- 82.Edwardson CL, Gorely T, Davies MJ, Gray LJ, Khunti K, Wilmot EG. Association of sedentary behaviour with metabolic syndrome: a meta-analysis. Plos One. 2012;7(4):e34916. doi: 10.1371/journal.pone.0034916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Storz MA. The role of vegan diets in lipotoxicity-induced beta-cell dysfunction in type-2-diabetes. J Popul Ther Clin Pharmacol. 2020;27(SP2):e22–e38. doi: 10.15586/jptcp.v27SP2.744. [DOI] [PubMed] [Google Scholar]
- 84.Temple JL, Giacomelli AM, Kent KM, Roemmich JN, Epstein LH. Television watching increases motivated responding for food and energy intake in children. Am J Clin Nutr. 2007;85(2):355–361. doi: 10.1093/ajcn/85.2.355. [DOI] [PubMed] [Google Scholar]
- 85.Borghese M, Tremblay M, Leduc G, Boyer C, Belanger P, LeBlanc A, et al. Television viewing and food intake pattern of normal weight, overweight, and obese 9-11 year-old Canadian children. Obes Rev. 2014;15:232. doi: 10.1017/jns.2014.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Taveras EM, Sandora TJ, Shih MC, Ross-Degnan D, Goldmann DA, Gillman MW. The association of television and video viewing with fast food intake by preschool-age children. Obesity (Silver Spring) 2006;14(11):2034–2041. doi: 10.1038/oby.2006.238. [DOI] [PubMed] [Google Scholar]
- 87.Mariona P, Roy A. Survey on lifestyle and food habits of patients with PCOS and obesity. J Complement Med Res. 2021;11(5):93. [Google Scholar]
- 88.Chaput JP, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93(6):1196–1203. doi: 10.3945/ajcn.110.008680. [DOI] [PubMed] [Google Scholar]
- 89.Cessna T, Raudenbush B, Reed A, Hunker R. Effects of video game play on snacking behavior. Appetite. 2007;49(1):282. [Google Scholar]
- 90.Chaput JP, Tremblay A, Pereira B, Boirie Y, Duclos M, Thivel D. Food intake response to exercise and active video gaming in adolescents: effect of weight status. Br J Nutr. 2015;115(3):547–553. doi: 10.1017/S0007114515004602. [DOI] [PubMed] [Google Scholar]
- 91.Shi L, Mao Y. Excessive recreational computer use and food consumption behaviour among adolescents. Ital J Pediatr. 2010;36(1):1–4. doi: 10.1186/1824-7288-36-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fulton JE, Wang X, Yore MM, Carlson SA, Galuska DA, Caspersen CJ. Television viewing, computer use, and BMI among US children and adolescents. J Phys Act Health. 2009;6(s1):S28–S35. doi: 10.1123/jpah.6.s1.s28. [DOI] [PubMed] [Google Scholar]
- 93.Gilbert-Diamond D, Emond JA, Lansigan RK, Rapuano KM, Kelley WM, Heatherton TF, et al. Television food advertisement exposure and FTO rs9939609 genotype in relation to excess consumption in children. Int J Obes. 2017;41(1):23–29. doi: 10.1038/ijo.2016.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ustjanauskas AE, Harris JL, Schwartz MB. Food and beverage advertising on children's web sites. Pediatr Obes. 2014;9(5):362–372. doi: 10.1111/j.2047-6310.2013.00185.x. [DOI] [PubMed] [Google Scholar]
- 95.Lee B, Kim H, Lee SK, Yoon J, Chung SJ. Effects of exposure to television advertising for energy-dense/nutrient-poor food on children's food intake and obesity in South Korea. Appetite. 2014;81:305–311. doi: 10.1016/j.appet.2014.06.103. [DOI] [PubMed] [Google Scholar]
- 96.Dibildox J. Analysis of TV, advertising and other behavioral determinants of overweight and obesity in childhood. Salud Publica Mex. 2014;56(Suppl 2):s162–s166. [PubMed] [Google Scholar]
- 97.Kar S, Khandelwal B. Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J Nat Sci Biol Med. 2015;6(2):356. doi: 10.4103/0976-9668.160004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Leman MA, Claramita M, Rahayu GR. Predicting factors on modeling health behavior: a systematic review. Am J Health Behav. 2021;45(2):268–278. doi: 10.5993/AJHB.45.2.7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from Tabriz University of Medical Sciences but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of corresponding author.