Sir,
Managing a difficult tracheal intubation is a challenge for any airway operator. The McCoy laryngoscope was developed in 1993 to manage difficult intubations. This device improves the glottic view during difficult laryngoscopy because of its levering tip, making it an important gadget for difficult airway management, especially in patients with cervical spine injury.[1,2] Video laryngoscopes are relatively newer devices which have better glottic visualisation and first pass success rate as compared to Macintosh and McCoy laryngoscopes in studies simulating cervical spine injury.[3,4] Video laryngoscopes are recommended for difficult airway management, however they are not available universally, especially in resource limited settings.[5,6]Also, video laryngoscope does not have a levering tip to elevate the epiglottis like the McCoy laryngoscope. Combining the favourable features of both these devices, we developed an affordable levering video laryngoscope, which was tested in a manikin study.
With the help of our biomedical engineering team we attached a waterproof wireless borescope examination camera with six light-emitting diode lights into the groove of a Macintosh laryngoscope, 40 mm proximal to the tip of laryngoscope. The laryngoscope was further modified by cutting it obliquely 2 cm proximal to the tip and welded it with a hinge to make it a levering tip which can be flexed to 70° by pushing the proximal lever forward with a spring loaded drum attached to the left side of flange [Figure 1a]. This video laryngoscope can be used in a way similar to a conventional laryngoscope. The levering tip helps to elevate the epiglottis and improves the glottic view [Figures 1b and c]. The image captured from the camera can be seen on a smartphone or tablet connected using a cable, using the Inskam application (freely downloadable from google play store). The real time video laryngoscopic image can also be transmitted to a control room from where an experienced airway operator can monitor and guide junior staff performing the procedure. The images of laryngoscopic view and the tracheal tube passage into the glottis can also be saved for documentation and training purposes.
Figure 1.
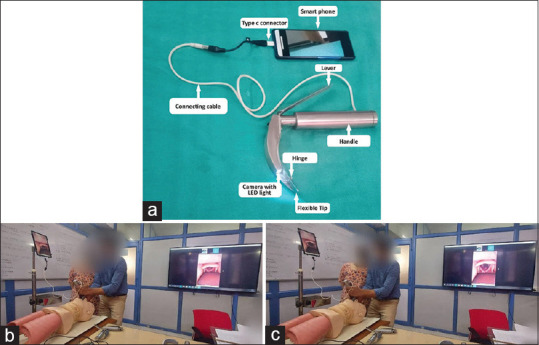
(a) MLVL with its tip in neutral position. (b) Glottic view without pushing the lever of MLVL. (c) Improvement in glottic view by pushing the lever forward. MLVL: Modified levering video laryngoscope
To test this improvised video laryngoscope, we performed a manikin study. The device was found to be easy to use having the advantages of both a McCoy laryngoscope and a conventional video laryngoscope. We compared our modified levering video laryngoscope (MLVL) with McCoy laryngoscope in a manikin (Laerdal Medical™). Ten certified anaesthesiologists who had completed 3 years of anaesthesia training performed intubations. Two intubations with each device were performed by each anaesthesiologist with or without cervical collar in place. The intubation time and percentage of glottic opening (POGO) scores were recorded. The data were compared using a one way analysis of variance (ANOVA). Subgroup analysis was done using Tukey’s honestly significant difference (HSD) test. All intubations were successful at the first attempt. Although there was no statistically significant difference in intubation times (P = 0.143), there was a significant improvement in glottic view when MLVL was used [Table 1]. The intergroup differences in mean POGO scores were significant (F = 28.77; P < 0.001). The laryngoscopic view improved when the lever was pushed forward in 60% of the patients.
Table 1.
Comparison of POGO score and intubation time using McCoy laryngoscopy vs levering video laryngoscopy in a manikin with or without cervical collar in place
| McCoy | Modified levering VL (MLVL) | McCoy with cervical collar | Modified Levering VL with cervical collar | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| POGO score (%) | Intubation time$ (s) | POGO score (%) | Intubation time (s) | POGO score (%) | Intubation time (s) | POGO score (%) | Intubation time (s) | |
| Anaesthesiologist 1 | 60 | 11.9 | 90 | 11.7 | 40 | 14.3 | 90 | 13.7 |
| Anaesthesiologist 2 | 50 | 10.2 | 80 | 15.3 | 50 | 11.9 | 70 | 18.9 |
| Anaesthesiologist 3 | 70 | 12.7 | 90 | 12.5 | 70 | 15.6 | 90 | 17.7 |
| Anaesthesiologist 4 | 80 | 16.2 | 100 | 15.4 | 50 | 11.8 | 90 | 28.2 |
| Anaesthesiologist 5 | 60 | 10.2 | 90 | 16.4 | 40 | 17.3 | 80 | 21.0 |
| Anaesthesiologist 6 | 40 | 9.87 | 90 | 10.3 | 40 | 11.3 | 90 | 17.9 |
| Anaesthesiologist 7 | 80 | 16.6 | 100 | 19.9 | 40 | 20.1 | 60 | 11.2 |
| Anaesthesiologist 8 | 70 | 10.6 | 100 | 11.8 | 70 | 15.7 | 100 | 15.2 |
| Anaesthesiologist 9 | 60 | 7.3 | 90 | 11.6 | 60 | 7.7 | 90 | 9.87 |
| Anaesthesiologist 10 | 50 | 10.3 | 100 | 11.7 | 40 | 10.3 | 70 | 20.1 |
| Mean (SD) | 62±13.2 | 11.6±2.9 | 93.0±6.7 | 13.7±3.0 | 50.0±12.5 | 13.6±3.7 | 83.0±12.5 | 17.4±5.3 |
ANOVA F for POGO score=28.77; P<0.001; ANOVA F for intubation time=3.954; P=0.016. Between group comparisons (Tukey’s HSD) ‘P’ values: McCoy vs MLVL: POGO score (P=<0.001), intubation time (P=0.626); McCoy vs MLVL (with cervical collar): POGO score (P=<0.001), intubation time (P=0.143). POGO=percentage of glottic opening from 0% (no part of glottis is visible) to 100% (whole glottis with anterior commissure is visible). $Intubation time is the time between insertion of laryngoscope until cuff of tracheal tube just passes the vocal cords. ANOVA: Analysis of variance; VL: Video laryngoscope; MLVL: Modified levering video laryngoscope; SD: Standard deviation
Our initial observations in manikins suggest that the MLVL provides the dual advantage of a superior glottic view like a video laryngoscope, with further possibility of improvement of the view due to its levering tip which elevates the epiglottis. Further studies on human subjects are required to establish the safety and efficacy of this device in humans. This device has the potential to be a future affordable alternative to video laryngoscopes for difficult airway management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to acknowledge Dr. Tahira K. Ansari for helping in the preparation of the manuscript. We would like to thank our biomedical team for their support.
REFERENCES
- 1.Szarpak L. Laryngoscopes for difficult airway scenarios:A comparison of the available devices. Expert Rev Med Devices. 2018;15:631–43. doi: 10.1080/17434440.2018.1511423. [DOI] [PubMed] [Google Scholar]
- 2.Bansal T, Taxak S, Yadav A, Singh S. McCoy laryngoscope:A savior in patient with limited mouth opening. J Anaesthesiol Clin Pharmacol. 2019;35:406–7. doi: 10.4103/joacp.JOACP_210_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seo KH, Kim KM, John H, Jun JH, Han M, Kim S. Comparison of C-MAC D-blade videolaryngoscope and McCoy laryngoscope efficacy for nasotracheal intubation in simulated cervical spinal injury:A prospective randomized comparative study. BMC Anesthesiol. 14(20):114. doi: 10.1186/s12871-020-01021-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choudhary J, Barai AK, Das S, Mukherjee N. Evaluation of the use of the channeled King Vision video laryngoscope in improving glottic visualisation in patients with limited glottic view with the Macintosh laryngoscope:A prospective observational study. Indian J Anaesth. 2021;65:874–9. doi: 10.4103/ija.ija_905_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shruthi AH, Dinakara D, Chandrika YR. Role of videolaryngoscope in the management of difficult airway in adults:A survey. Indian J Anaesth. 2020;64:855–62. doi: 10.4103/ija.IJA_211_20. [DOI] [PMC free article] [PubMed] [Google Scholar]


