Abstract
Background
Patients resuscitated from out‐of‐hospital circulatory arrest (OHCA) frequently have cardiopulmonary resuscitation injuries identifiable by computed tomography, although the prevalence, types of injury, and effects on clinical outcomes are poorly characterized.
Methods and Results
We assessed the prevalence of resuscitation‐associated injuries in a prospective, observational study of a head‐to‐pelvis sudden‐death computed tomography scan within 6 hours of successful OHCA resuscitation. Primary outcomes included total injuries and time‐critical injuries (such as organ laceration). Exploratory outcomes were injury associations with mechanical cardiopulmonary resuscitation and survival to discharge. Among 104 patients with OHCA (age 56±15 years, 30% women), 58% had bystander cardiopulmonary resuscitation, and total cardiopulmonary resuscitation time was 15±11 minutes. The prevalence of resuscitation‐associated injury was high (81%), including 15 patients (14%) with time‐critical findings. Patients with resuscitation injury were older (58±15 versus 46±13 years; P<0.001), but had otherwise similar baseline characteristics and survival compared with those without. Mechanical chest compression systems (27%) had more frequent sternal fractures (36% versus 12%; P=0.009), including displaced fractures (18% versus 1%; P=0.005), but no difference in survival (46% versus 41%; P=0.66).
Conclusions
In patients resuscitated from OHCA, head‐to‐pelvis sudden‐death computed tomography identified resuscitation injuries in most patients, with nearly 1 in 7 with time‐critical complications, and one‐half with extensive rib‐cage injuries. These data suggest that sudden‐death computed tomography may have additional diagnostic utility and treatment implications beyond evaluating causes of OHCA. These important findings need to also be taken in context of the certain fatal outcome without resuscitation efforts.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT03111043.
Keywords: cardiopulmonary resuscitation, computed tomography, out‐of‐hospital cardiac arrest, out‐of‐hospital circulatory arrest, resuscitation complications, rib fracture, sudden‐death CT
Subject Categories: Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care, Sudden Cardiac Death, Computerized Tomography (CT)
Nonstandard Abbreviations and Acronyms
- OHCA
out‐of‐hospital circulatory arrest
- SDCT
sudden‐death computed tomography
Clinical Perspective
What Is New?
Head‐to‐pelvis sudden‐death computed tomography in patients successfully resuscitated after out‐of‐hospital circulatory arrest was performed early (<6 hours) after hospital arrival and demonstrated a high prevalence of injuries associated with resuscitation, including rib‐cage fractures in most patients, as well as time‐critical or life‐threatening complications (eg, organ laceration, internal hemorrhage).
What Are the Clinical Implications?
These data suggest that sudden‐death computed tomography may have an incremental benefit in the early post–out‐of‐hospital circulatory arrest period by assisting in the prompt identification of resuscitation injury to inform postarrest patient care.
The downstream effect of this diagnostic intervention on clinical outcomes merits further study.
Out‐of‐hospital circulatory arrest (OHCA) occurs in ≈140 per 100 000 adults in the United States annually and is associated with poor outcomes. 1 High‐quality cardiopulmonary resuscitation (CPR) is critical to survival in OHCA. 2 Injuries from chest compressions, defibrillation, intubation, vascular cannulation, and other interventions performed during cardiovascular life support are described. 3 However, the prevalence and types of skeletal and visceral injuries attributable to CPR, as well as their effect on clinical outcome, remain poorly characterized. We have previously reported the findings of a prospective observational study examining the utility of early head‐to‐pelvis sudden‐death computed tomography (SDCT) in patients resuscitated after OHCA to identify the cause of circulatory arrest. 4 SDCT can also evaluate for resuscitation injuries, such as organ laceration, rib fracture, and vascular disruption. Rapid detection of such injuries may allow for early targeted intervention and improvement in outcomes. The aim of the present analysis is to describe the prevalence, severity, and effects on outcomes for injuries associated with resuscitation efforts as detected by SDCT imaging in patients hospitalized after OHCA.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request. The full methods of the study have been previously described (National Clinical Trial number 03111043). 4 , 5 Briefly, CT‐FIRST (CT Feasibility In Resuscitated Patients for Sudden Death Triage) was a prospective, observational study of patients resuscitated after an OHCA event but without obvious cause for the OHCA event (termed idiopathic OHCA). The study was designed to evaluate the incremental diagnostic capability and safety of early (<6 hours from hospital arrival) head‐to‐pelvis SDCT in addition to standard care. Patients who survived an idiopathic OHCA between December 2015 and February 2018 and presented at 1 of 2 academic medical centers were eligible for enrollment if clinically stable to undergo computed tomography (CT) scanning within 6 hours of hospital arrival. Exclusion criteria included ST‐segment–elevation myocardial infarction; known unrevascularized coronary artery disease or stent diameter <2.5 mm; estimated glomerular filtration rate <30 mL/min per 1.73 m2 and serum creatinine >1.7 mg/dL, unless the ordering physician deemed SDCT clinically necessary; implantable defibrillator; known iodinated contrast allergy; and known hospice status or terminal disease (prognosis <3 months). Patients could be enrolled in 1 of 2 ways: (1) prospectively, in which informed consent could be obtained from the patient or legally authorized representative before SDCT followed by SDCT as part of the research protocol; or (2) retrospectively, in which patients who underwent clinically directed SDCT could have eligibility screening and the informed consent process performed post hoc. All patients subsequently underwent clinically directed SDCT, and thus no patients were prospectively prior to SDCT. Patients for whom the study had been ordered clinically and subsequently died with no identifiable legally authorized representative were also enrolled if they satisfied the inclusion criteria. Institutional Review Board/Human Subject Division approval was obtained for consenting and all study procedures. The study adhered to all Health Insurance Portability and Accountability Act requirements. The study was partially supported by a research grant from the Medic One Foundation (Seattle, WA).
The SDCT scan was performed on either a dual‐source CT (FORCE, Siemens Medical Solutions, Forchheim, Germany) or a wide single‐detector CT (REVOLUTION, GE Healthcare, Waukesha, WI), and consisted of (1) a noncontrast head CT from the vertex to below the mandible, (2) an ECG‐gated CT scan of the thorax, and (3) a non–ECG‐gated venous‐phase CT scan extending from the diaphragm to just below the pelvis.
SDCT Evaluation
As previously described, all SDCT data, except for coronary imaging data, were read by an attending radiologist and were released to treating providers in real time. 4 , 5 These data included resuscitation injuries. For the purpose of this research analysis, the SDCT studies were independently reviewed by 2 board‐certified radiologists (M.L.G. and R.M.E.) with 34 combined years of experience in tomographic imaging who were blinded to the patients’ clinical data, including radiology reports. In addition, the chest CT images were independently reviewed by a third radiologist (B.S.) with 15 years of experience in chest CT to describe rib‐cage fractures including location (rib number and angle) and morphology (Data S1). 6
The radiology reports were subsequently independently evaluated by 2 cardiologists who had access to the patients’ clinical data (A.K. and K.R.H.B.) to assess the likelihood the findings were potentially associated to resuscitation (rather than preceding or unrelated to resuscitative efforts) and graded to “time‐critical” if the findings warranted urgent evaluation by specialty services, urgent additional imaging, or urgent treatments. 4 All discrepancies were resolved by consensus. Clinical outcomes studied were death from CPR injury detected by SDCT and survival to hospital discharge.
Statistical Analysis
All data were compiled into a Research Electronic Data Capture 7 , 8 database and summarized as number (percentage [95% CI]) or mean±SD. Continuous data were visually inspected for conformation with the normal distribution and were compared using a 2‐tailed Student t test; categorical variables were compared using Fisher’s exact test. Exploratory analyses were performed to evaluate resuscitation injuries for an association with survival to discharge and mechanical CPR. All analyses were performed using JMP Pro 15.0.0 (SAS, Cary, NC). A P value of <0.05 was considered statistically significant.
Results
A total of 307 patients presented after OHCA to the 2 centers during the enrollment period; 111 underwent head‐to‐pelvis SDCT; 7 patients were subsequently excluded as a result of incorrect SDCT protocol (n=4) or refusing enrollment after awakening (n=3), resulting in a study cohort of 104 patients.
Baseline characteristics of the study population are shown in Table 1. Mean age was 56±15 years, and 30% were women. The majority (43%) of events occurred at home, and most (58%) patients received bystander CPR. The most common initial OHCA rhythm was pulseless electrical activity (38%). Mean CPR duration was 15±11 minutes; a mechanical chest compression system was used in 27% of cases. Compared with patients without injury, patients with injury associated with CPR were older (58±15 versus 46±13 years; P<0.001) but otherwise exhibited similar characteristics (Table 1).
Table 1.
Baseline Clinical and Out‐of‐Hospital Circulatory Arrest Characteristics
| Characteristic* |
Patients (n=104) |
CPR injury | P value | |
|---|---|---|---|---|
|
Yes (n=84) |
No (n=20) |
|||
| Age, y | 56±15 | 58±15 | 46±13 | <0.001 |
| Female sex | 31/104 (30) | 25/83 (30) | 6/21 (29) | 1.000 |
| Body mass index, kg/m2 | 25±8 | 24±8 | 27±8 | 0.219 |
| Available medical history | 95 | 77 | 18 | … |
| Hypertension | 38/95 (40) | 32/77 (42) | 6/18 (33) | 0.753 |
| Dyslipidemia | 15/95 (16) | 12/77 (16) | 3/18 (17) | 1.000 |
| Heart failure | 12/95 (13) | 10/77 (13) | 2/18 (11) | 1.000 |
| Diabetes | 19/95 (20) | 17/77 (22) | 2/18 (11) | 0.513 |
| Chronic kidney disease | 12/95 (13) | 10/77 (13) | 2/18 (11) | 1.000 |
| History of coronary artery disease | 11/95 (12) | 9/77 (12) | 2/18 (11) | 1.000 |
| Prior cardiac arrest | 2/95 (2) | 2/77 (3) | 0/18 (0) | 1.000 |
| Prior PCI | 5/95 (5) | 4/77 (5) | 1/18 (6) | 1.000 |
| Prior valvular disease | 5/95 (5) | 4/77 (5) | 1/18 (6) | 1.000 |
| Prior stroke | 6/95 (6) | 3/77 (4) | 3/18 (17) | 0.080 |
| Initial rhythm | 0.778 | |||
| Pulseless electrical activity | 40/104 (38) | 33/84 (40) | 7/20 (35) | |
| VT/VF | 30/104 (29) | 25/84 (30) | 5/20 (25) | |
| Asystole/unknown | 34/104 (33) | 26/84 (31) | 8/20 (40) | |
| Witnessed arrest | 59/99 (59) | 46/79 (58) | 13/20 (65) | 0.621 |
| Bystander CPR | 57/99 (58) | 46/79 (58) | 11/20 (55) | 0.805 |
| Mechanical CPR | 28/104 (27) | 25/84 (30) | 3/20 (15) | 0.263 |
| Mean CPR time, min | 15±11 | 16.1±11.0 | 12.3±8.5 | 0.138 |
Data are shown as number, number/total number (percentage), or mean±SD. CPR indicates cardiopulmonary resuscitation; LV, left ventricle; PCI, percutaneous coronary intervention; VF, ventricular fibrillation; and VT, ventricular tachycardia.
Of 104 (91%) patients, 95 had complete past medical history obtained during the hospitalization, resulting in discrepant numbers of total patients and denominators for the patient characteristics.
The overall prevalence of injury attributable to resuscitation was 81% (95% CI, 72%–87%; 84/104 patients; Figure 1); 37 patients (36% [95% CI, 27%–45%]) had >1 injury. A total of 15 patients (14% [95% CI, 9%–22%]) had 19 total time‐critical findings, including liver/spleen laceration, pneumothorax or pulmonary laceration, or hemorrhage in another site (Figure 2; Table 2). A total of 32 downstream evaluations or treatments occurred in 13/15 (87%; 13% of the overall study population) patients as a result of SDCT identifying time‐critical injuries, including repeat or additional imaging in 11 patients, surgical consultations for 9 patients, blood transfusions in 5 patients (per our institutional protocol, 2 “massive” transfusions and 3 standard transfusions), chest/abdominal drains placed in 5 patients, and endotracheal tube repositioning in 2 patients.
Figure 1. Resuscitation‐associated injuries including time‐critical injuries.
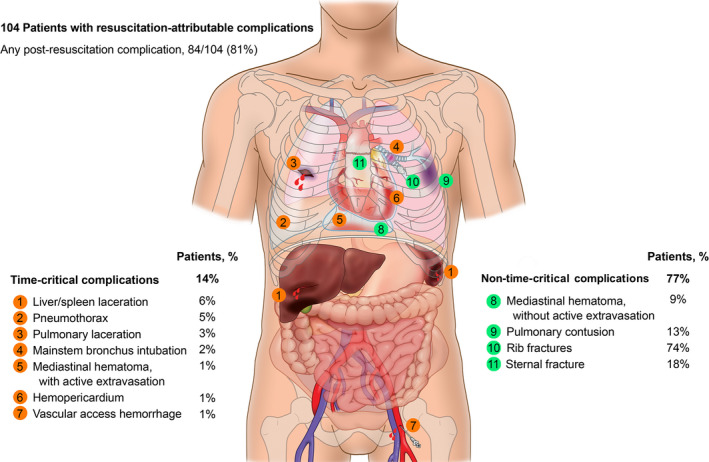
Figure 2. Illustrative radiographic examples of cardiopulmonary resuscitation complications.
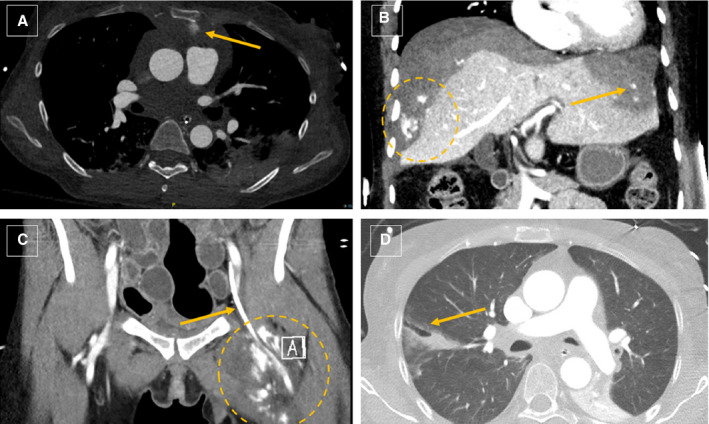
(A and C) Anterior mediastinal hematoma (arrow, A) and left thigh medial compartment hematoma (circle) associated with a femoral artery catheter (arrow, C), both exhibiting active extravasation in a patient with disseminated intravascular coagulation treated with massive transfusion. (B) Extensive subcapsular liver hematoma with multiple foci of active extravasation (circle, arrow) and several lacerations treated conservatively because of a poor prognosis with multiple transfusions and eventual autotamponade of bleeding. (D) Right lower lobe pulmonary laceration (arrow) associated with bilateral rib and sternal fractures in a patient with hereditary pheochromocytoma/paraganglioma syndrome who underwent prolonged resuscitation.
Table 2.
Resuscitation‐Associated Injuries (n=104 Patients)
| Type of resuscitation‐associated injury | Patients |
|---|---|
| Any postresuscitation injury | 84/104 (81 [72–87]) |
| Time critical* | 15/104 (14 [9–22]) |
| Liver/spleen laceration | 6 (6 [3–12]) |
| Pneumothorax | 5 (5 [2–11]) |
| Mediastinal hemorrhage, active extravasation | 1 (1 [0–5]) |
| Hemopericardium | 1 (1 [0–5]) |
| Pulmonary laceration | 3 (3 [1–8]) |
| Vascular access hemorrhage | 1 (1 [0–5]) |
| Mainstem bronchus intubation | 2 (2 [1–7]) |
| Not time critical* | 80/104 (77 [68–84]) |
| Mediastinal hematoma without active extravasation | 9 (9 [5–16]) |
| Pulmonary contusion | 14 (13 [8–21]) |
| Rib fractures | 77 (74 [65–82]) |
| Displaced | 16 (15 [10–24]) |
| Meets surgical stabilization screening criteria | 45 (43 [34–53]) |
| Displaced rib fractures, ≥3 | 3 (3 [1–8]) |
| Flail chest | 1 (1 [0–5]) |
| Flail sternal segment | 42 (40 [31–50]) |
| Number of rib fractures per patient | 5.0±4.6 |
| Sternal fracture | 19 (18 [12–27]) |
| Displaced | 6 (6 [3–12]) |
Data are shown as number (percentage [95% CI]), number/total number (percentage [95% CI]), or mean±SD of patients with each injury type; some patients had >1 injury.
The anatomical distribution of rib fractures (N=519; 5.0±4.6 fractures per patient) is shown in Figure 3. The majority (80% [95% CI, 76%–83%]) of fractures were anterolateral, and more than half (58% [95% CI, 54%–62%]) were on the third, fourth, or fifth ribs.
Figure 3. Anatomical distribution of rib fractures.
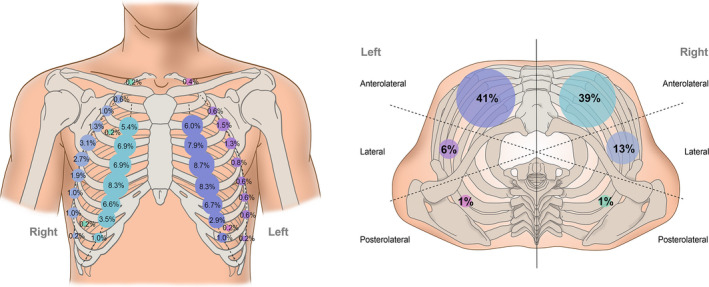
Distribution of rib fractures by transverse sector (anterolateral, 0–72 °; lateral 73–108 °; posterolateral, 109–180 °) shown by rib number (left) and for the overall sector (right). Numbers are shown as percentage of total rib fractures (N=519); circle size is proportionate to frequency in respective anatomic location.
In exploratory analyses, 44 (42%) patients survived to discharge, and there was no significant difference in survival between those with or without overall resuscitation‐associated injury (39% versus 55%; P=0.22). Patients who did not survive had more rib fractures (5.7±4.7 versus 4.0±4.4; P=0.03; Table S1) and sternal fractures (25% versus 9%; P=0.04) than survivors. No patient died as a direct consequence of time‐critical injuries. Those who underwent mechanical CPR (n=28, 27%) had similar rates of overall (89% versus 78%; P=0.26) and time‐critical (21% versus 12%; P=0.22) resuscitation‐associated injuries compared with patients who only received manual CPR (Table S2). Mechanical CPR was associated with more frequent sternal fractures (36% versus 12%; P=0.009), including displaced fractures (18% versus 1%; P=0.005), compared with nonmechanical CPR, but this did not adversely impact survival to discharge (46% versus 41%; P=0.66).
Discussion
Our study demonstrated that resuscitation‐associated injuries after an OHCA event are common and are identified by SDCT scanning in ≈80% (95% CI, 72%–87%) of survivors of OHCA. Although the most prevalent complication was rib fracture, radiographic flail chest or sternum occurred in a significant proportion (40% [95% CI, 31%–50%]) of patients, and time‐critical resuscitation injuries occurred in 14% (95% CI, 9%–22%) of patients, including organ laceration and significant bleeding requiring massive transfusion. These data support the use of a head‐to‐pelvis SDCT protocol to provide important diagnostic information in patients successfully resuscitated from OHCA.
Thoracic and abdominal injury are relatively common after CPR and cardiovascular life support. Injuries can range from relatively benign, such as nondisplaced rib fractures, to life‐threatening, including hemorrhage from organ injury. Autopsy series identified thoracic and abdominal complications at a high frequency, including rib and sternal fractures in up to 89% and 47%, respectively. Laceration or rupture of either the liver or spleen occurred in up to 21% and 10%, respectively. 3 , 9 , 10 Current guidelines for postresuscitative care suggest only ECG, chest radiograph, and echocardiography as routine diagnostic modalities in the early resuscitation period, 2 , 11 , 12 but these cannot evaluate for all resuscitation injuries. Chest radiography alone substantially underestimates thoracic injuries and only identified 50% of total rib or sternal fractures at autopsy in patients with OHCA. 9 CT scanning, on the other hand, has the capabilities to simultaneously evaluate bony structures, thoracic and abdominal organs and soft tissue, and intravascular line and endotracheal tube placement. Kashiwagi et al. evaluated 223 patients after OHCA with whole‐body CT (65% postmortem; 35% within 72 hours after the return of spontaneous circulation) and found a similarly high prevalence of rib fractures (70%), sternal fractures (8.1%), and pneumothorax (7.6%) 13 ; our findings are more clinically relevant given that all scans in our study were performed in alive patients within 6 hours (mean, 1.9±1.0 hours) of arrival. Seung et al. published a retrospective CT study of 148 patients and showed a high overall prevalence of complications (rib fractures in 75%, “serious complications” in 7.4%) as well as a higher prevalence of complications in survivors of OHCA compared with in‐hospital cardiac arrest. 14 However, only a chest CT was required for inclusion, which would not reveal resuscitation complications in the nonvisualized portions of the abdomen and the pelvis, several of which were identified with our head‐to‐pelvis CT protocol.
Our study supports the high prevalence of resuscitation‐associated injury in a prospective cohort of survivors of OHCA, adds granularity, and confirms the feasibility and utility of an early (<6 hours) SDCT protocol to identify resuscitation complications. In particular, the extent of rib‐cage injuries was striking, with an estimated 40% meeting institutional criteria for consideration of surgical stabilization. This included a 3‐fold increase in sternal fractures in the 27% of patients who received mechanical chest compressions, consistent with prior studies showing sternal fractures, 15 and other thoracic injuries such as myocardial rupture. 16 Thoracic injuries after resuscitation have been associated with prolonged mechanical ventilation, tracheostomy, pneumonia, acute respiratory distress syndrome, and increased mortality among others. 17 Interestingly, severe injuries that could be missed by plain radiography and echocardiography (such as life‐threatening hemorrhage or organ laceration) were frequent in our study, and SDCT significantly affected downstream clinical evaluations and treatments in at least 13% of cases. These data suggest that SDCT may have additional diagnostic utility and treatment implications beyond evaluating causes of OHCA, a hypothesis that merits further study in a larger, randomized trial. 4 Fortunately, despite their high frequency, only a small minority of patients required invasive procedures to treat resuscitation‐associated injury, and no patients died as a direct consequence thereof.
The current study is limited by total number of patients as well as selection bias of the prospective cohort studied as all patients underwent a clinically ordered SDCT at 1 of 2 academic medical centers. We did not collect data on survivors of OHCA presenting at the participating centers during the study period who were eligible for the study but did not undergo SDCT (n=196), and thus we cannot assess for systematic differences between this group and the present study cohort. Thus, data from this cohort may not be generalizable to all survivors of OHCA. There also is no standard for identification and of injuries potentially associated with resuscitation in survivors of OHCA such that SDCT acts as its own standard. SDCT readings were blinded to clinical data and performed by 2 board certified radiologists to reduce observer bias. We also cannot definitively assess the effect of SDCT imaging on clinical outcomes as all scan data were available clinically and there was no comparator group. Whether clinical outcomes would have been altered with or without SDCT remains unclear. Outcomes may be confounded by the small sample size and patient characteristics (eg, frailty) such that further prospective study is needed to define the role of early SDCT in assisting with clinical care. Finally, while not being dismissive of injuries potentially related to resuscitation from OHCA, one must bear in mind that the alternative to efforts that might result in such complications from urgently needed treatment is certain death.
In conclusion, in patients who survived an OHCA event as a result of resuscitation protocols, resuscitation‐associated injuries are common and are identifiable by a head‐to‐pelvis SDCT. Resuscitation injury has a range of diagnoses and severities, but in our study nearly 1 in 7 had time‐critical diagnoses by SDCT that required further evaluation or intervention, and up to half had extensive rib‐cage injuries that might have impacted clinical care. Thus, although resuscitation injuries were not associated with survival to discharge in our study, SDCT scanning can identify clinically important and actionable complications of resuscitation as well as causes for OHCA. Importantly, these findings need to be taken in the context of the certain fatal outcome were resuscitation to not be performed after OHCA.
Sources of Funding
This work is supported by the Medic One Foundation, Seattle, WA.
Disclosures
Dr Branch reports receiving research grants from Bayer, Sanofi, Eli Lilly, Kestra, and the Medic One Foundation and consulting for Bayer, Janssen, Amgen, Kestra, and Hanmi. Dr Gunn reports receiving research grants from Annalise.ai and Philips Healthcare. The remaining authors have no disclosures to report.
Supporting information
Data S1
Tables S1–S2
Acknowledgments
We thank our research coordinators Deborah Fly, RN, and Michele Olsufka, RN, for their assistance in contacting patients and family members as well as data abstraction and imaging supervisor technologist Mena Flemon and all the computed tomography technicians for their assistance with the sudden‐death computed tomography protocol. We also thank Dennis Mathias for his illustrations. We thank each of the departments and divisions within the University of Washington for their ongoing support of this research endeavor. Finally, we offer special thanks to the Medic One Foundation for their financial support.
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.023949
For Sources of Funding and Disclosures, see page 7.
References
- 1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, et al. Heart disease and stroke statistics‐2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 2. Panchal AR, Bartos JA, Cabanas JG, Donnino MW, Drennan IR, Hirsch KG, Kudenchuk PJ, Kurz MC, Lavonas EJ, Morley PT, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142:S366–S468. doi: 10.1161/CIR.0000000000000916 [DOI] [PubMed] [Google Scholar]
- 3. Krischer JP, Fine EG, Davis JH, Nagel EL. Complications of cardiac resuscitation. Chest. 1987;92:287–291. doi: 10.1378/chest.92.2.287 [DOI] [PubMed] [Google Scholar]
- 4. Branch KRH, Strote J, Gunn M, Maynard C, Kudenchuk PJ, Brusen R, Petek BJ, Sayre MR, Edwards R, Carlbom D, et al. Early head‐to‐pelvis computed tomography in out‐of‐hospital circulatory arrest without obvious etiology. Acad Emerg Med. 2021;28:394–403. doi: 10.1111/acem.14228 [DOI] [PubMed] [Google Scholar]
- 5. Branch KR, Hira R, Brusen R, Maynard C, Kudenchuk PJ, Petek BJ, Strote J, Sayre MR, Gatewood M, Carlbom D, et al. Diagnostic accuracy of early computed tomographic coronary angiography to detect coronary artery disease after out‐of‐hospital circulatory arrest. Resuscitation. 2020;153:243–250. doi: 10.1016/j.resuscitation.2020.04.033 [DOI] [PubMed] [Google Scholar]
- 6. Ritchie N, Wang S, Sochor M, Schneider L. A method for documenting locations of rib fractures for occupants in real‐world crashes using medical computed tomography (CT) scans. SAE Technical Paper. 2006;2006‐01‐0250. doi: 10.4271/2006-01-0250 [DOI] [Google Scholar]
- 7. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lederer W, Mair D, Rabl W, Baubin M. Frequency of rib and sternum fractures associated with out‐of‐hospital cardiopulmonary resuscitation is underestimated by conventional chest X‐ray. Resuscitation. 2004;60:157–162. doi: 10.1016/j.resuscitation.2003.10.003 [DOI] [PubMed] [Google Scholar]
- 10. Buschmann CT, Tsokos M. Frequent and rare complications of resuscitation attempts. Intensive Care Med. 2009;35:397–404. doi: 10.1007/s00134-008-1255-9 [DOI] [PubMed] [Google Scholar]
- 11. Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H, Genbrugge C, Haywood K, Lilja G, Moulaert VRM, et al. European resuscitation council and European society of intensive care medicine guidelines 2021: post‐resuscitation care. Resuscitation. 2021;161:220–269. doi: 10.1016/j.resuscitation.2021.02.012 [DOI] [PubMed] [Google Scholar]
- 12. Soar J, Berg KM, Andersen LW, Böttiger BW, Cacciola S, Callaway CW, Couper K, Cronberg T, D’Arrigo S, Deakin CD, et al. Adult advanced life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A80–A119. doi: 10.1016/j.resuscitation.2020.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kashiwagi Y, Sasakawa T, Tampo A, Kawata D, Nishiura T, Kokita N, Iwasaki H, Fujita S. Computed tomography findings of complications resulting from cardiopulmonary resuscitation. Resuscitation. 2015;88:86–91. doi: 10.1016/j.resuscitation.2014.12.022 [DOI] [PubMed] [Google Scholar]
- 14. Seung MK, You JS, Lee HS, Park YS, Chung SP, Park I. Comparison of complications secondary to cardiopulmonary resuscitation between out‐of‐hospital cardiac arrest and in‐hospital cardiac arrest. Resuscitation. 2016;98:64–72. doi: 10.1016/j.resuscitation.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 15. Baubin M, Sumann G, Rabl W, Eibl G, Wenzel V, Mair P. Increased frequency of thorax injuries with ACD‐CPR. Resuscitation. 1999;41:33–38. doi: 10.1016/S0300-9572(99)00033-7 [DOI] [PubMed] [Google Scholar]
- 16. Machii M, Inaba H, Nakae H, Suzuki I, Tanaka H. Cardiac rupture by penetration of fractured sternum: a rare complication of cardiopulmonary resuscitation. Resuscitation. 2000;43:151–153. doi: 10.1016/S0300-9572(99)00137-9 [DOI] [PubMed] [Google Scholar]
- 17. Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76:462–468. doi: 10.1097/TA.0000000000000086 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Tables S1–S2


