Abstract
Background
Residential segregation, a geospatial manifestation of structural racism, is a fundamental driver of racial and ethnic health inequities, and longitudinal studies examining segregation’s influence on cardiovascular health are limited. This study investigates the impact of segregation on hypertension in a multiracial and multiethnic cohort and explores whether neighborhood environment modifies this association.
Methods and Results
Leveraging data from a diverse cohort of adults recruited from 6 sites in the United States with 2 decades of follow‐up, we used race‐ and ethnicity‐stratified Cox models to examine the association between time‐varying segregation with incident hypertension in 1937 adults free of hypertension at baseline. Participants were categorized as residing in segregated and nonsegregated neighborhoods using a spatial‐weighted measure. We used a robust covariance matrix estimator to account for clustering within neighborhoods and assessed effect measure modification by neighborhood social or physical environment. Over an average follow‐up of 7.35 years, 65.5% non‐Hispanic Black, 48.1% Chinese, and 53.7% Hispanic participants developed hypertension. Net of confounders, Black and Hispanic residents in segregated neighborhoods were more likely to develop hypertension relative to residents in nonsegregated neighborhoods (Black residents: hazard ratio [HR], 1.33; 95% CI, 1.09–1.62; Hispanic residents: HR, 1.33; 95% CI, 1.04–1.70). Results were similar but not significant among Chinese residents (HR, 1.20; 95% CI, 0.83–1.73). Among Black residents, neighborhood social environment significantly modified this association such that better social environment was associated with less pronounced impact of segregation on hypertension.
Conclusions
This study underscores the importance of continued investigations of groups affected by the health consequences of racial residential segregation while taking contextual neighborhood factors, such as social environment, into account.
Keywords: health equity, hypertension, neighborhood environment, racial residential segregation
Subject Categories: Epidemiology, Hypertension, Race and Ethnicity
Nonstandard Abbreviations and Acronyms
- MESA
Multi‐Ethnic Study of Atherosclerosis
Clinical Perspective
What Is New?
A cohort study with 2 decades of follow‐up found that Black and Hispanic adults living in racially segregated neighborhoods were more likely to develop hypertension, adjusting for individual sociodemographic and health factors.
Among Black participants, the impact of segregation on hypertension was more pronounced in neighborhoods with worse social environment quality (eg less social cohesion, reduced sense of safety), highlighting the importance of understanding structural processes that negatively influence neighborhood social conditions.
What Are the Clinical Implications?
Addressing sociopolitical mechanisms that uphold structural racism, such as racial residential segregation, may be important to reduce racial and ethnic inequities in incident hypertension.
Hypertension is a major risk factor for cardiovascular diseases such as stroke, coronary artery disease, heart failure, and atrial fibrillation as well as all‐cause mortality. 1 , 2 Persistent racial and ethnic inequities in hypertension remain an urgent public health challenge. According to the American Heart Association, the prevalence of hypertension among Black people in the United States is among the highest in the world at 56.6% for men and 55.3% for women. 3 Hypertension control‐related behaviors, including hypertension treatment and management, are also significantly less common among Hispanic, Asian, and non‐Hispanic Black populations. 1 , 4 , 5 Individual‐level factors have failed to account for these persistent inequities, highlighting the need to understand contextual‐level factors that may explain these differences.
Extensive research has documented that place may help explain the inequities in hypertension and other cardiometabolic factors. 6 , 7 , 8 , 9 , 10 One multidimensional aspect of place is racial residential segregation, or “the physical separation of the races in residential contexts,” which was systematically created through sociopolitical policies and economic programs such as mortgage redlining, urban renewal, and barriers to educational and economic opportunities. 11 Structural racism, a fundamental cause of racial and ethnic health inequities, operates through residential segregation to produce differential socioeconomic conditions, neighborhood environment, and access to health care across space. 12 , 13 Understanding the influence of residential segregation can contribute to hypertension prevention and control in Black populations and other minoritized racial and ethnic groups, reducing racial and ethnic inequities in hypertension and the disproportionate burden of cardiovascular diseases on minoritized populations.
Studies investigating the link between residential segregation and hypertension have focused primarily on Black populations and reported mixed findings. Kershaw et al. found that Black participants had higher odds of hypertension compared with their White counterparts, and this disparity increased in highly segregated metropolitan areas compared with low segregation areas. 14 A geospatial analysis in Durham, North Carolina showed that census block‐level racial isolation of non‐Hispanic Black patients was associated with increased odds of hypertension for both non‐Hispanic Black and White participants. 15 Other studies examining segregation and hypertension conducted in Black populations found null results or associations only in specific subgroups. 16 , 17 , 18 For example, one study in New York City found that neighborhood‐level segregation was protective against hypertension among foreign‐born Black older adults but not among younger or US‐born Black adults. 18 There has been only 1 longitudinal study to date that documented the associations between changes in segregation and blood pressure over time. This analysis showed that increased exposure to segregation was associated with a small but significant increase in systolic blood pressure among Black participants. 19 Overall, these studies have demonstrated mixed results and suggest that further investigation of the relationship between segregation and hypertension is needed.
There are also other major limitations in the current literature on segregation and hypertension that need to be addressed. First, there have been few studies examining segregation and hypertension in other minoritized racial and ethnic groups, and these existing studies were cross‐sectional and reported mixed findings. Whereas one study in Chicago found that Latino participants living in neighborhoods with higher concentration of immigrant and Latino residents had lower odds of hypertension but also worse access to hypertension control, another study found that high Latino ethnic density was associated with higher risk of hypertension. 10 , 20 A study examining Asian populations documented no association between living in an Asian ethnic enclave in New York City and self‐reported hypertension. 21 Additionally, only 2 studies have examined the cross‐sectional associations between segregation and hypertension in samples with multiple minoritized racial and ethnic groups; both studies documented associations between economic or racial segregation and hypertension in the overall, multiracial study population. 22 , 23 Although Black Americans experience unique and most pervasive forms of structural racism that manifest in persistent and severe residential segregation, residential segregation, and its correlates in housing and access to other resources, may also have consequences for other minoritized racial and ethnic groups. 24 , 25 , 26 It is important to evaluate whether associations between segregation and hypertension vary across minoritized racial and ethnic groups in order to elucidate the ways in which structural racism drives racial and ethnic health inequities.
Second, given that there are both positive and negative aspects of racial and ethnic spatial clustering, studies should examine the neighborhood‐level factors through which segregation may influence hypertension. Segregation is usually used to capture the negative aspects of this spatial clustering, which create vastly different economic, social, and physical neighborhood conditions through differential exposure to poor housing quality, concentrated poverty, and lack of access to education and economic opportunities. 11 , 27 , 28 On the other hand, the ethnic density hypothesis posits that living in ethnic enclaves—neighborhoods with higher concentration of residents from the same ethnic background—is health promoting because of social support, social cohesion, provision of a buffer against racism, and access to culturally appropriate resources. 29 , 30 , 31 Owing to the mixed nature of study findings on spatial clustering of minoritized racial and ethnic groups and hypertension, it is possible that both the harmful aspects and the protective effects of segregation are operating simultaneously. For instance, the type of social support usually associated with ethnic enclaves may also exist in segregated, predominantly Black neighborhoods but fails to offset the effects caused by poor neighborhood environment and systematic barriers to resources. In order to consider both the harmful and protective aspects of segregation, it is necessary for studies to evaluate whether neighborhood physical and social environments modify the association between segregation and hypertension.
To address the limitations in the existing literature, this study leveraged data from MESA (the Multi‐Ethnic Study of Atherosclerosis) to evaluate the association between residential segregation and incident hypertension with 2 decades of follow‐up, using methods that account for spatial clustering of observations. We conducted analyses within 3 racial or ethnic groups: non‐Hispanic Black, Chinese, and Hispanic. Furthermore, we assessed whether the association between segregation and hypertension is modified by neighborhood physical and social environment quality. We hypothesized that living in a segregated neighborhood would be associated with higher risk of hypertension within each racial or ethnic subgroup. Furthermore, we hypothesized that better neighborhood physical and social environment quality can offset the negative impact or amplify the positive aspects of segregation on health.
Methods
Qualified researchers trained in human subject confidentiality protocols may find information on requesting access to the data used in this study at https://mesa‐nhlbi.org.
Study Population
This study used data from MESA. Details about the study design are described elsewhere. 32 Briefly, MESA is a prospective cohort study designed to examine the determinants of subclinical cardiovascular disease in adults aged 45 to 84 years at baseline. Self‐identified non‐Hispanic Black, White, Chinese, and Hispanic male and female participants free of clinical cardiovascular disease were recruited from 6 sites in the United States: New York, New York; Baltimore City and County, Maryland; Forsyth County, North Carolina; St. Paul, Minnesota; Chicago, Illinois; and Los Angeles County, California. Five additional examinations have been completed since baseline: Exam 2 (2002–2004), Exam 3 (2004–2005), Exam 4 (2005–2007), Exam 5 (2010–2012), and Exam 6 (2016–2018). Analyses in this study also used data from the MESA Neighborhood Ancillary study, designed to assess neighborhood conditions’ impact on cardiovascular disease.
Of the non‐Hispanic Black, Chinese, and Hispanic MESA participants who gave informed consent to participate in the Neighborhood Ancillary Study (n=3758), we excluded participants who had prevalent hypertension at baseline (n=1804), were missing segregation status (n=6), or did not have covariate information (n=11). This resulted in a final analytic sample of 1937 participants. Those excluded from the analytic sample were more likely to be male, older, non‐Hispanic Black, current smoker, insured, US‐born, have lower education attainment level, and lived in neighborhoods with worse physical environment. This study was approved by the institutional review boards at each study site and all participants gave written informed consent.
Incident Hypertension
At each Exam, blood pressure was measured using a standardized protocol: 3 measurements were taken at 2‐minute intervals with an automated oscillometric sphygmomanometer after 5 minutes of seated rest. The analysis used the average of the second and third measurements. To be comparable with existing literature, incident hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or reported use of antihypertensive medication. 33 As a sensitivity analyses, we also evaluated incident hypertension defined as systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥80 mm, or the use of antihypertensive medication, based on the 2017 American College of Cardiology/American Heart Association guidelines. 34 The month of the incident hypertension was set as the midpoint between the last nonhypertensive examination and the first hypertensive examination. Those who did not develop hypertension were censored at their last exam.
Residential Segregation
Using data from the US Census and American Community Survey that corresponded with each Exam, we characterized the residential segregation status of neighborhoods, which were defined as census tracts. Time‐varying neighborhood‐level own‐group racial residential segregation was measured using the Getis‐Ord Local Gi * statistic, based on the census tract of the geocoded addresses of MESA participants during Exam calendar year. The Gi * statistic returned a Z score for each neighborhood, indicating the extent to which the racial composition in that tract and neighboring tracts deviated from the mean racial composition of larger areal unit within which the census tract was located (eg county). We used racial and ethnic census data (% Hispanic, % non‐Hispanic Black, and % non‐Hispanic Asian) to calculate the Gi * statistics, which were then assigned to participants based on their race or ethnicity and residence census tract. Positive Gi * Z‐scores indicated racial and ethnic clustering in the census tract compared with the larger areal unit within which the tract was located. We categorized census tracts with Gi * statistics above 1.96 as segregated. Census tracts with Gi * statistics at or below 1.96, which included both no clustering and statistically significant low clustering (underrepresentation of the racial or ethnic group in the census tract), were categorized as nonsegregated because there were few participants residing in areas where they were underrepresented. 19 , 22 , 35 , 36 Segregation measures were linked to MESA participants at each Exam based on the most comparable dates for the American Community Survey data. Exams 1, 2, and part of Exam 3 used 2000 US Census data, part of Exam 3 and Exam 4 used 2005 to 2009 American Community Survey data, and Exam 5 used 2007 to 2011 American Community Survey data. For Exam 6, we used the segregation measurements from the last wave of the Neighborhood Ancillary study, which corresponded to Exam 5.
Neighborhood Physical and Social Environment
Analyses in this study used data from the MESA Neighborhood Ancillary study, designed to assess neighborhood conditions’ impact on cardiovascular diseases. Corresponding to MESA Exams 1 to 5, the Neighborhood Ancillary study collected survey‐based information on the neighborhood social and physical environments around participants’ home addresses. In addition to MESA participants, individuals residing in the same neighborhoods as MESA participants were recruited as a part of the Community Survey and asked to rate several aspects of their neighborhoods. The Community Survey reduced same‐source bias, increased within‐neighborhood sample size for constructing contextual variables and provided a more representative view of the neighborhoods. 37 , 38 Because the Neighborhood Ancillary study was not conducted paralleling MESA Exam 6, data from the Neighborhood Ancillary study corresponding to Exam 5 was used for Exam 6.
Time‐varying neighborhood physical and social environment measures were created based on responses from MESA participants and Community Survey respondents at MESA sites. Participants were asked to consider the area approximately 1 mile around their homes and indicate the extent to which they agreed with given statements about their neighborhood environment. Neighborhood physical environment was characterized by survey‐based perception of healthy food environment (3 items about the availability of fruits and vegetables and low‐fat products) and walking environment (7 items about the pleasantness, ease, and frequency of walking in the neighborhood). Neighborhood social environment was measured by survey‐based perception of aesthetic quality (5 items about noise, litter, and neighborhood attractiveness), safety (3 items about violence and walking safety), and social cohesion (4 items about relationship with neighbors). Neighborhood physical and social environment scores were summarized from the scale‐based responses and standardized by subtracting the mean and divided by the SD. These scales have been used in prior studies and were shown to have good internal consistency and reliability (Cronbach's α=0.75 and 0.88 for physical and social environment scale, respectively). 6 , 7 , 37 A higher score reflected better neighborhood environment quality.
Covariates
We adjusted for individual‐level sociodemographic covariates, which included age at baseline (years), sex (female, male), education (4 categories), birthplace (born in the United States and its territories, born in another country), and health insurance (insured, uninsured), as well as time‐varying per capita adjusted income (continuous household income/number of people supported per $10 000). Additionally, we adjusted for time‐varying individual‐level health behaviors including cigarette smoking and physical activity, as well as continuous body mass index (BMI). Smoking status was modeled as a categorical variable (never smoker, former smoker, and current smoker). The MESA Typical Week Physical Activity Survey, adapted from the Cross‐Cultural Activity Participation Study, identified the time and frequency spent in various physical activities during a typical week in the past month. 39 We defined physical activity as total intentional exercise, measured in metabolic equivalent ‐minutes per week. Metabolic equivalent is the ratio of the rate of energy expended during an activity to the rate of energy expended at rest. We categorized 1000+ metabolic equivalent‐minutes/week as high physical activity, between 0 and 1000 metabolic equivalent‐minutes/week as intermediate physical activity, and 0 metabolic equivalent‐minutes/week as physically inactive based on the 2008 Physical Activity Guidelines for Americans. 40 For descriptive analysis, we classified BMI into 4 categories following the World Health Organization’s guidelines: Normal (BMI <25), Overweight (BMI 25–30), Obesity Class I and II (BMI 30–40), Obesity Class III (BMI >=40). 41 When a participant had missing covariate value for income, smoking status, BMI, and physical activity at Exams 2 to 6, we carried over the last available value from previous exams.
Statistical Analysis
We conducted descriptive analyses to examine the distribution of the participants’ characteristics by those who resided in a segregated neighborhood and those who did not at baseline, as well as by those who developed hypertension during the follow‐up period and those who did not.
To assess the association between time‐varying residential segregation and development of incident hypertension in the 3 racial or ethnic minority groups, we used race and ethnicity‐stratified Cox proportional hazards models to estimate hazard ratios comparing those who resided in segregated neighborhoods to those who did not. In Model 1, we adjusted for socioeconomic characteristics, including age at baseline, sex, education, and income. Model 1 included health insurance and nativity when there was sufficient variation in the distribution of these variables within specific racial or ethnic groups. In Model 2, we further adjusted for smoking status, physical activity, and BMI. In Model 3, we additionally adjusted for neighborhood social and physical environment quality. These models used a robust covariance matrix estimator to account for clustering of individuals within census tracts. To assess effect measure modification by the quality of the neighborhood social and physical environments, we created cross‐product interaction terms between segregation and neighborhood environment scores and assessed them separately in Model 2. Significance of interaction terms were assessed using P value <0.1 and 95% CI.
Violations in the proportional hazard assumptions were assessed analytically. We tested for interactions of each covariate with linear and log‐transformed time (days). Using P value <0.05 as the statistically significant threshold, we found violations by age at baseline and smoking with linear time. Hence, we included interaction terms between age at baseline and time as well as smoking status and time in all our models. In sensitivity analyses, we reran all models using the updated definition of hypertension (130/80 mm Hg or usage of antihypertensive medication). In these models, we found proportional hazard assumption violations by age at baseline and BMI with log time; consequently, we also added interactions terms between baseline age and time as well as BMI and time.
For all analyses, we reported estimates and 95% CIs. All statistical analyses were conducted using R (www.r‐project.org). Cox proportional hazards models used R package “survival.”
Results
The final analytic sample included 693 non‐Hispanic Black, 778 Hispanic, and 466 Chinese participants, with an average follow‐up of 7.35 years. The mean age at baseline was between 58.0 and 59.4 years old across groups. Table 1 displays the distribution of participant characteristics by segregation status at Exam 1. During Exam 1, 55.8% of Black, 64.9% of Hispanic, and 77.9% of Chinese residents lived in segregated neighborhoods. Overall, age, sex, and health‐related covariates were fairly evenly distributed between those who resided in a segregated neighborhood and those who did not, in all racial and ethnic groups. Hispanic participants in segregated neighborhoods were more likely to be born outside of the United States and had lower physical activity level, and Black participants in segregated neighborhoods were more likely to be uninsured. For both Black and Hispanic participants, those who lived in segregated neighborhoods had lower education attainment and income, as well as worse neighborhood social and physical environment quality.
Table 1.
Participant Characteristics by Segregation Status at Baseline, Multi‐Ethnic Study of Atherosclerosis, 2000 to 2001
| Non‐Hispanic Black | Hispanic | Chinese | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | Nonsegregated | Segregated | Overall | Nonsegregated | Segregated | Overall | Nonsegregated | Segregated | |
| N | 693 | 306 | 387 | 778 | 273 | 505 | 466 | 103 | 363 |
| Age, y | 58.4 (9.8) | 57.6 | 59.0 | 58.0 (9.7) | 57.7 | 58.1 | 59.4 (9.8) | 60.0 | 59.3 |
| Sex | |||||||||
| Female | 361 (52.1) | 54.2 | 50.4 | 378 (48.6) | 45.8 | 50.1 | 231 (49.6) | 45.6 | 50.7 |
| Male | 332 (47.9) | 45.8 | 49.6 | 400 (51.4) | 54.2 | 49.9 | 235 (50.4) | 54.4 | 49.3 |
| Education | |||||||||
| Bachelor’s/graduate degree | 272 (39.2) | 45.4 | 34.4 | 95 (12.2) | 20.9 | 7.5 | 206 (44.2) | 46.6 | 43.5 |
| Technical school/associate | 256 (36.9) | 31.7 | 41.1 | 213 (27.4) | 33.3 | 24.2 | 94 (20.2) | 20.4 | 20.1 |
| High school | 107 (15.4) | 15.4 | 15.5 | 160 (20.6) | 20.1 | 20.8 | 74 (15.9) | 16.5 | 15.7 |
| Less than high school | 58 (8.4) | 7.5 | 9.0 | 310 (39.8) | 25.6 | 47.5 | 92 (19.7) | 16.5 | 20.7 |
| Health insurance | |||||||||
| Insured | 641 (92.5) | 97.1 | 88.9 | 629 (80.8) | 83.5 | 79.4 | 368 (79.0) | 79.6 | 78.8 |
| Uninsured | 52 (7.5) | 2.9 | 11.1 | 149 (19.2) | 16.5 | 20.6 | 98 (21.0) | 20.4 | 21.2 |
| Physical activity | |||||||||
| None | 152 (21.9) | 19.6 | 23.8 | 239 (30.7) | 23.4 | 34.7 | 135 (29.0) | 34.0 | 27.5 |
| Intermediate | 191 (27.6) | 29.7 | 25.8 | 234 (30.1) | 31.9 | 29.1 | 161 (34.5) | 35.9 | 34.2 |
| High | 350 (50.5) | 50.7 | 50.4 | 305 (39.2) | 44.7 | 36.2 | 170 (36.5) | 30.1 | 38.3 |
| Smoking status | |||||||||
| Never | 306 (44.2) | 49.0 | 40.3 | 405 (52.1) | 49.5 | 53.5 | 355 (76.2) | 74.8 | 76.6 |
| Former | 231 (33.3) | 30.1 | 35.9 | 247 (31.7) | 34.1 | 30.5 | 85 (18.2) | 20.4 | 17.6 |
| Current | 156 (22.5) | 20.9 | 23.8 | 126 (16.2) | 16.5 | 16.0 | 26 (5.6) | 4.9 | 5.8 |
| Body mass index | |||||||||
| Normal | 157 (22.7) | 23.2 | 22.2 | 145 (18.6) | 17.6 | 19.2 | 326 (70.0) | 67.0 | 70.8 |
| Overweight | 266 (38.4) | 38.6 | 38.2 | 364 (46.8) | 49.5 | 45.3 | 126 (27.0) | 29.1 | 26.4 |
| Obesity class I and II | 235 (33.9) | 33.3 | 34.4 | 239 (30.7) | 30.4 | 30.9 | 14 (3.0) | 3.9 | 2.8 |
| Obesity class III | 35 (5.1) | 4.9 | 5.2 | 30 (3.9) | 2.6 | 4.6 | 0 (0.0) | 0.0 | 0.0 |
| Birthplace | |||||||||
| US states and territories | 616 (88.9) | 82.4 | 94.1 | 336 (43.2) | 50.5 | 39.2 | 20 (4.3) | 4.9 | 4.1 |
| Other countries | 77 (11.1) | 17.6 | 5.9 | 442 (56.8) | 49.5 | 60.8 | 446 (95.7) | 95.1 | 95.9 |
| Per capita adjusted income | 2.78 (1.9) | 3.0 | 2.6 | 1.59 (1.5) | 2.1 | 1.3 | 1.71 (1.6) | 1.8 | 1.7 |
| Neighborhood social environment | −0.03 (1.0) | 0.1 | −0.2 | −0.29 (0.9) | 0.2 | −0.6 | 0.38 (0.7) | 0.4 | 0.4 |
| Neighborhood physical environment | −0.31 (1.1) | −0.1 | −0.5 | −0.13 (0.8) | 0.3 | −0.3 | 0.09 (0.8) | 0.1 | 0.1 |
| Developed hypertension (n) | 454 | 184 | 270 | 418 | 131 | 287 | 224 | 49 | 175 |
Categorical variables displayed by count and percentage in parenthesis (overall), displayed by percentage (by segregation status): sex, education, insurance, physical activity, smoking status, body mass index class, and birthplace.
Continuous variables displayed by mean value and SD in parenthesis (overall), displayed by mean (by segregation status): age, per capita adjusted income, neighborhood social and physical environment scores.
Table 2 provides the distribution of baseline participant characteristics by hypertension status. By the end of follow‐up, 65.5% of Black, 53.7% of Hispanic, and 48.1% of Chinese participants developed hypertension. Generally, participants who developed hypertension were more likely to be older and have higher BMI. Black participants who developed hypertension were more likely to reside in neighborhoods with worse physical environment quality, and Asian participants who developed hypertension were more likely to live in neighborhood with worse social environment.
Table 2.
Participant Characteristics at Baseline by Hypertension Status by 2018, Multi‐Ethnic Study of Atherosclerosis, 2000 to 2018
| Non‐Hispanic Black | Hispanic | Chinese | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall |
No hypertension |
Incident hypertension |
Overall |
No hypertension |
Incident hypertension |
Overall |
No hypertension |
Incident hypertension |
|
| N | 693 | 239 | 454 | 778 | 360 | 418 | 466 | 242 | 224 |
| Age, y | 58.4 (9.8) | 56.7 | 59.3 | 58.0 (9.7) | 56.01 | 59.7 | 59.4 (9.8) | 57.4 | 61.6 |
| Sex | |||||||||
| Female | 361 (52.1) | 50.6 | 52.9 | 378 (48.6) | 49.4 | 47.8 | 231 (49.6) | 52.9 | 46.0 |
| Male | 332 (47.9) | 49.4 | 47.1 | 400 (51.4) | 50.6 | 52.2 | 235 (50.4) | 47.1 | 54.0 |
| Education | |||||||||
| Bachelor’s/graduate degree | 272 (39.2) | 43.1 | 37.2 | 95 (12.2) | 13.6 | 11.0 | 206 (44.2) | 46.3 | 42.0 |
| Technical school or associate | 256 (36.9) | 33.9 | 38.5 | 213 (27.4) | 30.3 | 24.9 | 94 (20.2) | 22.3 | 17.9 |
| High school | 107 (15.4) | 15.1 | 15.6 | 160 (20.6) | 18.3 | 22.5 | 74 (15.9) | 12.0 | 20.1 |
| Less than high school | 58 (8.4) | 7.9 | 8.6 | 310 (39.8) | 37.8 | 41.6 | 92 (19.7) | 19.4 | 20.1 |
| Health insurance | |||||||||
| Insured | 641 (92.5) | 93.3 | 92.1 | 629 (80.8) | 76.1 | 84.9 | 368 (79.0) | 80.6 | 77.2 |
| Uninsured | 52 (7.5) | 6.7 | 7.9 | 149 (19.2) | 23.9 | 15.1 | 98 (21.0) | 19.4 | 22.8 |
| Physical activity | |||||||||
| None | 152 (21.9) | 17.6 | 24.2 | 239 (30.7) | 31.9 | 29.7 | 135 (29.0) | 30.2 | 27.7 |
| Intermediate | 191 (27.6) | 30.5 | 26.0 | 234 (30.1) | 27.8 | 32.1 | 161 (34.5) | 36.8 | 32.1 |
| High | 350 (50.5) | 51.9 | 49.8 | 305 (39.2) | 40.3 | 38.3 | 170 (36.5) | 33.1 | 40.2 |
| Smoking status | |||||||||
| Never | 306 (44.2) | 41.4 | 45.6 | 405 (52.1) | 52.5 | 51.7 | 355 (76.2) | 79.8 | 72.3 |
| Former | 231 (33.3) | 33.5 | 33.3 | 247 (31.7) | 30.6 | 32.8 | 85 (18.2) | 16.1 | 20.5 |
| Current | 156 (22.5) | 25.1 | 21.1 | 126 (16.2) | 16.9 | 15.6 | 26 (5.6) | 4.1 | 7.1 |
| Body mass index | |||||||||
| Normal | 157 (22.7) | 27.2 | 20.3 | 145 (18.6) | 20.8 | 16.7 | 326 (70.0) | 75.2 | 64.3 |
| Overweight | 266 (38.4) | 41.4 | 36.8 | 364 (46.8) | 53.1 | 41.4 | 126 (27.0) | 21.5 | 33.0 |
| Obesity class I and II | 235 (33.9) | 29.3 | 36.3 | 239 (30.7) | 23.9 | 36.6 | 14 (3.0) | 3.3 | 2.7 |
| Obesity class III | 35 (5.1) | 2.1 | 6.6 | 30 (3.9) | 2.2 | 5.3 | 0 (0.0) | 0.0 | 0.0 |
| Birthplace | |||||||||
| US states and territories | 616 (88.9) | 87.9 | 89.4 | 336 (43.2) | 40.3 | 45.7 | 20 (4.3) | 5.8 | 2.7 |
| Other countries | 77 (11.1) | 12.1 | 10.6 | 442 (56.8) | 59.7 | 54.3 | 446 (95.7) | 94.2 | 97.3 |
| Per capita adjusted income | 2.8 (1.9) | 2.7 | 2.8 | 1.6 (1.5) | 1.53 | 1.64 | 1.7 (1.6) | 1.8 | 1.6 |
| Neighborhood social environment | −0.0 (1.0) | 0.1 | −0.1 | −0.3 (0.9) | −0.25 | −0.33 | 0.4 (0.7) | 0.5 | 0.3 |
| Neighborhood physical environment | −0.3 (1.1) | −0.2 | −0.4 | −0.1 (0.8) | −0.09 | −0.16 | 0.1 (0.8) | 0.1 | 0.1 |
| Resided in segregated neighborhood | 387 | 117 | 270 | 505 | 218 | 287 | 363 | 188 | 175 |
Categorical variables displayed by count and percentage in parenthesis (overall) and displayed by percentage (by hypertension status): sex, education, insurance, physical activity, smoking status, body mass index class, and birthplace.
Continuous variables displayed by mean value and SD in parenthesis (overall) and displayed by mean (by hypertension status): age, per capita adjusted income, neighborhood social and physical environment scores.
In multivariate models, residency in racially segregated neighborhoods compared with nonsegregated neighborhoods was associated with greater hazard of developing hypertension for Black and Hispanic residents, adjusted for individual sociodemographic characteristics including age at baseline, sex, education, birthplace, insurance, and per capita adjusted income (Table 3, Model 1). These associations persisted after further adjusting for BMI, physical activity, and smoking. Black and Hispanic participants residing in segregated neighborhoods were 33% more likely to develop hypertension (Black participants: HR, 1.33; 95% CI, 1.09–1.62; Hispanic participants: HR, 1.33; 95% CI, 1.04–1.70). Results were similar but not significant among Chinese residents (HR, 1.20; 95% CI, 0.83–1.73). Lastly, after adjusting for neighborhood social and physical environment, the association between segregation and hypertension in Black participants persisted, but the association was attenuated among Hispanic participants. In sensitivity analysis using the updated guidelines for hypertension, the direction of the association remained the same in the fully adjusted Model 2, but the magnitude was smaller and only remained statistically significant for the Hispanic population (Black participants: HR, 1.12; 95% CI, 0.95–1.33; Hispanic participants: HR, 1.22; 95% CI, 1.01–1.46; Chinese participants: HR, 1.21; 95% CI, 0.88–1.65).
Table 3.
Adjusted Hazard Ratios of Hypertension Incidence by Segregation Status, Multi‐Ethnic Study of Atherosclerosis, 2000 to 2018
| Non‐Hispanic Black | Hispanic | Chinese | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Segregation |
1.31 (1.08–1.58) |
1.33 (1.09–1.62) |
1.24 (1.01–1.54) |
1.32 (1.05–1.66) |
1.33 (1.04–1.70) |
1.13 (0.87–1.46) |
1.12 (0.78–1.61) |
1.20 (0.83–1.73) |
1.30 (0.87–1.93) |
| Age |
1.04 (1.03–1.05) |
1.04 (1.03–1.06) |
1.04 (1.03–1.06) |
1.05 (1.04–1.07) |
1.06 (1.04–1.07) |
1.06 (1.04–1.07) |
1.07 (1.04–1.09) |
1.07 (1.05–1.10) |
1.08 (1.05–1.10) |
| Sex (male) |
1.04 (0.87–1.26) |
1.14 (0.95–1.38) |
1.14 (0.94–1.39) |
1.08 (0.88–1.32) |
1.17 (0.95–1.45) |
1.20 (0.97–1.49) |
1.30 (1.00–1.70) |
1.21 (0.87–1.68) |
1.14 (0.81–1.62) |
| Education | |||||||||
| Technical/associate |
1.20 (0.97–1.49) |
1.12 (0.91–1.38) |
1.09 (0.88–1.34) |
1.01 (0.70–1.44) |
0.95 (0.66–1.37) |
1.03 (0.71–1.50) |
0.97 (0.63–1.51) |
1.01 (0.64–1.58) |
1.00 (0.63–1.60) |
| High school |
1.24 (0.95–1.64) |
1.20 (0.90–1.60) |
1.14 (0.85–1.53) |
1.12 (0.77–1.62) |
1.10 (0.76–1.59) |
1.14 (0.79–1.67) |
1.49 (1.03–2.17) |
1.44 (0.97–2.15) |
1.38 (0.91–2.09) |
| <High school |
1.32 (0.87–2.02) |
1.40 (0.92–2.13) |
1.26 (0.82–1.94) |
1.30 (0.89–1.88) |
1.26 (0.87–1.82) |
1.31 (0.89–1.93) |
1.02 (0.68–1.54) |
1.00 (0.64–1.55) |
0.94 (0.59–1.51) |
| Per capita adjusted income |
1.02 (0.97–1.07) |
1.02 (0.97–1.07) |
1.03 (0.98–1.09) |
1.04 (0.97–1.11) |
1.06 (0.98–1.14) |
1.07 (1.00–1.16) |
0.90 (0.79–1.02) |
0.90 (0.78–1.02) |
0.92 (0.80–1.05) |
| Born outside of the United States | N/A | N/A | N/A |
0.90 (0.73–1.11) |
0.99 (0.80–1.23) |
0.97 (0.78–1.21) |
N/A | N/A | N/A |
| Uninsured | N/A | N/A | N/A |
0.78 (0.58–1.05) |
0.80 (0.59–1.08) |
0.79 (0.58–1.07) |
0.89 (0.61–1.29) |
0.87 (0.60–1.26) |
0.96 (0.66–1.39) |
| Body mass index |
1.05 (1.03–1.06) |
1.05 (1.03–1.06) |
1.07 (1.05–1.09) |
1.07 (1.05–1.09) |
1.07 (1.02–1.13) |
1.07 (1.01–1.12) |
|||
| Physical activity | |||||||||
| Intermediate |
1.00 (0.76–1.32) |
1.01 (0.76–1.34) |
1.06 (0.80–1.41) |
1.08 (0.81–1.45) |
0.93 (0.59–1.47) |
0.90 (0.56–1.44) |
|||
| High |
1.09 (0.84–1.40) |
1.09 (0.85–1.41) |
1.00 (0.76–1.31) |
1.03 (0.78–1.36) |
0.93 (0.61–1.41) |
0.91 (0.58–1.42) |
|||
| Smoking status | |||||||||
| Former |
1.25 (0.92–1.69) |
1.25 (0.92–1.68) |
0.99 (0.71–1.39) |
1.00 (0.70–1.41) |
1.28 (0.74–2.23) |
1.34 (0.74–2.44) |
|||
| Current |
1.02 (0.70–1.48) |
1.03 (0.71–1.48) |
0.90 (0.57–1.41) |
0.87 (0.55–1.37) |
1.77 (0.86–3.65) |
1.87 (0.85–4.10) |
|||
| Physical environment |
0.89 (0.81–0.97) |
0.90 (0.78–1.05) |
0.90 (0.72–1.13) |
||||||
| Social environment |
0.94 (0.85–1.04) |
0.87 (0.75–1.00) |
1.03 (0.81–1.29) |
||||||
95% CI displayed in parentheses.
Model 1 adjusted for sociodemographic characteristics. Model 2 adjusted for Model 1 covariates + health factors. Model 3 adjusted for Model 2 covariates + neighborhood environment.
All models included an interaction term between age and time, and Model 2 and 3 also included an interaction term between smoking and time (not shown).
Referent level: sex=female; education=bachelor’s or graduate degree; physical activity=none; smoking status=never; uninsured=no; birthplace=United States; Age, per capita adjusted income, body mass index, and neighborhood environment were modeled continuously.
N/A: covariate not included in model owing to lack of variation in variable distribution in specific racial or ethnic group.
The association between residential segregation and incident hypertension was significantly modified by neighborhood social environment quality among Black participants (Figure 1). As neighborhood social environment quality score increases, the difference between the hazard of hypertension for Black participants who resided in segregated neighborhoods and the hazard of Black participants who did not live in segregated neighborhoods was smaller (P value=0.0108). For example, at the 25th percentile of the neighborhood social environment, Black participants in segregated neighborhoods had 1.63 (95% CI, 1.26–2.10) times the hazard of hypertension compared with those not living in segregated neighborhoods. As the social environment improves to the 75th percentile, the HR associated with segregation was 1.06 (95% CI, 0.81–1.37), suggesting that better neighborhood social environment may buffer the deleterious influence of segregation on hypertension. There was no statistically significant interaction with social environment quality score in Hispanic or Chinese groups, although the interaction terms were in the opposite direction compared with Black participants such that better social environment score was associated with a widening gap in the hazard of hypertension between segregated and nonsegregated residents (Hispanic participants: 25th percentile: HR, 1.11; 95% CI, 0.76–1.62; 75th percentile: HR, 1.20; 95% CI, 0.88–1.62; Chinese participants: 25th percentile: HR, 1.22; 95% CI, 0.80–1.87; 75th percentile: HR, 1.42; 95% CI, 0.91–2.20). There was no statistically significant interaction with physical environment quality score in any racial or ethnic group.
Figure 1. Association between residential segregation and incident hypertension among non‐Hispanic Black participants, by percentile of neighborhood social environment: the Multi‐Ethnic Study of Atherosclerosis, 2000 to 2018.
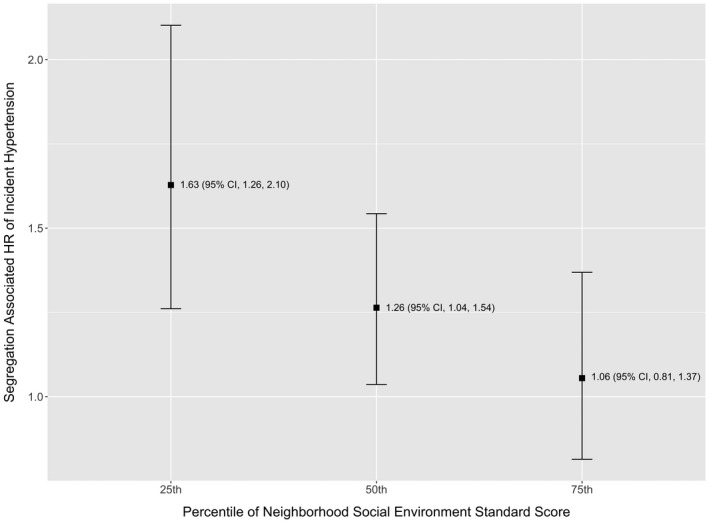
Model adjusted for age, sex, education, per capita adjusted income, body mass index, and physical activity. P value for interaction between segregation and social environment=0.0108. Standardized social environment is displayed from worse (25th percentile) to better (75th percentile). HR indicates hazard ratio.
Discussion
This study examined the associations between neighborhood‐level racial residential segregation, a prominent mechanism of structural racism that produces racial and ethnic health inequities through unequal distribution of resources and harms across neighborhoods, and development of incident hypertension. Using data from a sample of racially and ethnically diverse group of middle‐aged and older adults in the United States with 2 decades of follow‐up, we found that residency in a racially segregated neighborhood was associated with increased hazard of incident hypertension among Black and Hispanic participants, adjusting for time‐varying individual sociodemographic characteristics and health‐related covariates and accounting for spatial clustering of participants within neighborhoods. Adjusting for neighborhood physical and social environment quality attenuated this association among Hispanic participants but not among non‐Hispanic Black participants. Results were similar for Chinese participants but not statistically significant. Lastly, neighborhood social environment quality modified the relationship between segregation and incident hypertension for Black participants.
To our knowledge, our study is the first to document longitudinal associations between residential segregation and incident hypertension and examine effect measure modification of this relationship by neighborhood environment in Black, Hispanic, and Chinese populations. These results aligned with cross‐sectional evidence on the negative impact of residential segregation on hypertension prevalence, as well as on other cardiovascular outcomes and risk factors, among Black and Hispanic participants. 14 , 18 , 19 , 20 , 42 , 43 Our findings were also consistent with an existing longitudinal study documenting that reduction in exposure to segregation was associated with a decrease in systolic blood pressure among Black participants over 25 years of follow‐up. 19 Furthermore, adjusting for neighborhood environment resulted in a smaller but still significant hazard ratio, suggesting that although neighborhood context may matter, it does not fully attenuate the associations between segregation and hypertension among Black participants. Compared with other studies that documented null associations between segregation and hypertension, our study may have produced different findings owing to use of longitudinal data, measurement of segregation at the census tract level rather than at larger geographic scales such as metropolitan area, and rigorous assessment of outcome and time‐varying individual covariates. Building on this study’s evidence of consistent associations between segregation and hypertension, future studies can leverage longitudinal data, robust individual and neighborhood information, and rigorous assessment and analytic methods to understand the causal effects of segregation on cardiovascular health racial and ethnic inequities.
Our study also examined this relationship in Hispanic and Asian populations. The results among Hispanic participants contradicted a cross‐sectional study that reported lower odds of hypertension associated with segregation for Latino residents, suggesting that the benefits associated with living in areas with a high concentration of co‐ethnic populations may not be protective enough against the development of incident hypertension. 10 A previous MESA study found that a higher percentage of immigrant population in the neighborhood was associated with better diet but worse level of physical activity, both risk factors for hypertension, among Hispanic participants. This difference from our results highlighted that the operationalization and measurement of neighborhood segregation and ethnic enclave warrant careful consideration, because our study used an exposure assessment method that considered the racial composition of the larger contextual area within which the neighborhood was situated, which differed from other studies' measurement methods. 44 Furthermore, segregation was associated with hypertension after adjusting for participants’ birthplace, suggesting that segregation may matter for both immigrants and US‐born Hispanic populations. Findings from this study were consistent with other cross‐sectional evidence that residential segregation is a strong contextual factor in the development of incident hypertension among Hispanic participants. 20 Although this study did not find statistically significant associations among Chinese participants, possibly because of the small sample size of Chinese participants in this study sample, the direction of the association was similar to results for Black and Hispanic participants. Other studies have examined the associations between residing in segregated Asian neighborhoods or ethnic enclaves and other factors related to cardiovascular health such as smoking, BMI, diabetes, and diet, which also yielded mixed and inconclusive results. 21 , 31 , 45 , 46 Our findings suggest that the influence of segregation on cardiovascular health in Hispanic and Asian populations warrants further examination.
Another novel contribution of this study is the examination of the role neighborhood social and physical environment quality plays in the relationships between residential segregation and hypertension. Greater social cohesion and sense of safety in a good neighborhood social environment may lessen chronic stressors, buffer the health consequences of experiencing interpersonal discrimination, and provide more access to community resources, which have been documented to be associated with hypertension risk and may be pathways through which segregation influences health. 47 , 48 , 49 Studies of minoritized and immigrant populations have emphasized that close social ties and less potential of experiencing racial discrimination in a racially homogenous place can be protective for health. 30 , 44 First, the association between residential segregation and incident hypertension persisted after adjusting for neighborhood environment quality only among Black participants, suggesting that segregation, as a manifestation of structural racism, may affect Black populations in ways that extend above and beyond the neighborhood environment. Second, this investigation, by examining effect measure modification by neighborhood environment, elucidates how the health impacts of segregation vary depending on neighborhood social and physical environment quality. Epidemiologic studies that examine the relationships between segregation and cardiovascular health among Black populations have focused more on the negative neighborhood features such as concentrated poverty, social disorder, and other unjust material conditions. Although it is important to draw attention to this structural deprivation, this framing can also overlook the support network and community assets that exist in Black neighborhoods and may offset the deleterious effect of structural racism. 50 , 51 , 52 Our findings suggest that improving neighborhood social environment in segregated Black neighborhoods can potentially remedy the harmful impact of residential segregation and reduce racial and ethnic inequities in cardiovascular health among Black adults. Notably, neighborhoods that have experienced disinvestment are more vulnerable to gentrification, a process in which neighborhoods with affordable cost of development experience an influx of capital that improves physical amenities and access to resources. This process can displace lower‐income residents and disintegrate communities through increased property value and rent. Given our finding that neighborhood social environment can buffer the associations between segregation and hypertension among Black participants, future studies should examine how structural processes such as gentrification may affect community‐level social support and cohesion to further exacerbate cardiovascular health inequities. 53 , 54 , 55 , 56 Although we did not document similar findings in other racial or ethnic groups, future studies with larger sample size may be necessary to detect these associations.
There were several strengths in this study. First, the data we used came from a prospective, multiracial and multiethnic cohort study that clinically and rigorously collected outcome data and other covariates, with 2 decades of follow‐up time. The survey scales for neighborhood quality were previously validated and showed good consistency and reliability. We were able to include multiple domains of time‐varying confounders including sociodemographic indicators, health behaviors, and neighborhood environment, in order to elucidate the association of segregation independent of individual‐ and neighborhood‐level characteristics. There were also important limitations in our study. First, we examined only own‐group segregation, which did not capture the experience of a racially and ethnically minoritized participant living in a neighborhood with a high proportion of minoritized populations not sharing their racial or ethnic background. We also did not account for more complex dimensions of segregation, such as the joint effect of racial and economic segregation or graded levels of segregation (ie medium versus high level of segregation). Although we statistically adjusted for an extensive range of confounders, from individual sociodemographic and health risk factors to neighborhood environment quality, residual confounding may still remain because of measurement error of the confounders as well as omission of other key confounders. Furthermore, we carried over missing covariate values from previous exams for Exams 2 to 6; averaging across all Exams, 8.1% of the records had at least 1 missing value imputed this way, which may introduce bias. Hispanic and Chinese MESA participants were recruited from a small number of sites. Hispanic participants were enrolled only in New York, St. Paul, and Los Angeles, and Chinese participants were enrolled only from Chicago and Los Angeles. Because segregation in different racial and ethnic groups may have originated from housing, education, and economic policies that varied across cities and states, residential segregation may operate differently depending on the metropolitan region within which the population is residing. Thus, findings based on this study may not be generalizable to the regions outside of the study sites.
Conclusions
Our results provide strong empirical evidence that racial residential segregation, a manifestation of structural racism, is a fundamental driver of hypertension among non‐Hispanic Black and Hispanic adults, independent of individual socioeconomic and health factors. 11 , 57 , 58 Furthermore, neighborhood social environment may buffer the impact of residential segregation on hypertension incidence in Black populations. Future studies should consider neighborhood context in order to inform place‐based interventions that can address racial and ethnic cardiovascular health inequities produced by residential segregation.
Sources of Funding
This research was supported by contracts 75N92020D00001, HHSN268201500003I, N01‐HC‐95159, 75N92020D00005, N01‐HC‐95160, 75N92020D00002, N01‐HC‐95161, 75N92020D00003, N01‐HC‐95162, 75N92020D00006, N01‐HC‐95163, 75N92020D00004, N01‐HC‐95164, 75N92020D00007, N01‐HC‐95165, N01‐HC‐95166, N01‐HC‐95167, N01‐HC‐95168 and N01‐HC‐95169 from the National Heart, Lung, and Blood Institute and by grants UL1‐TR‐000040, UL1‐TR‐001079, and UL1‐TR‐001420 from the National Center for Advancing Translational Sciences.
Disclosures
None.
Acknowledgments
We thank the investigators, staff, and participants of the MESA study for their contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa‐nhlbi.org.
For Sources of Funding and Disclosures, see page 11.
References
- 1. Dorans KS, Mills KT, Liu Y, He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J Am Heart Assoc. 2017;2018:7. doi: 10.1161/JAHA.118.008888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rapsomaniki E, Timmis A, George J, Pujades‐Rodriguez M, Shah AD, Denaxas S, White IR, Caulfield MJ, Deanfield JE, Smeeth L, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life‐years lost, and age‐specific associations in 1·25 million people. Lancet. 2014;383:1899–1911. doi: 10.1016/S0140-6736(14)60685-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950 [DOI] [PubMed] [Google Scholar]
- 4. Yoon SSS, Carroll MD, Fryar CD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief. 2015;1–8. [PubMed] [Google Scholar]
- 5. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. Blood Press. 1988;303:2043–2050. doi: 10.1001/jama.2010.650 [DOI] [PubMed] [Google Scholar]
- 6. Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, Shea S. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2 [DOI] [PubMed] [Google Scholar]
- 7. Kaiser P, Diez Roux AV, Mujahid M, Carnethon M, Bertoni A, Adar SD, Shea S, McClelland R, Lisabeth L. Neighborhood environments and incident hypertension in the multi‐ethnic study of atherosclerosis. Am J Epidemiol. 2016;183:988–997. doi: 10.1093/aje/kwv296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12:217–230. doi: 10.1111/j.1467-789X.2010.00726.x [DOI] [PubMed] [Google Scholar]
- 9. Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65:1853–1866. doi: 10.1016/j.socscimed.2007.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Viruell‐Fuentes EA, Ponce NA, Alegría M. Neighborhood context and hypertension outcomes among Latinos in Chicago. J Immigr Minor Health. 2012;14:959–967. doi: 10.1007/s10903-012-9608-4 [DOI] [PubMed] [Google Scholar]
- 11. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389:1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 13. Barber S. Racial residential segregation and health inequities in the United States. In: Lovasi GS, Roux AVD, Kolker J, eds. Urban Public Health: A Research Toolkit for Practice and Impact. Oxford University Press; 2020:87–91. [Google Scholar]
- 14. Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan‐level racial residential segregation and black‐white disparities in hypertension. Am J Epidemiol. 2011;174:537–545. doi: 10.1093/aje/kwr116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bravo MA, Batch BC, Miranda ML. Residential racial isolation and spatial patterning of hypertension in Durham, North Carolina. Prev Chronic Dis. 2019;16:E36. doi: 10.5888/pcd16.180445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cole H, Duncan DT, Ogedegbe G, Bennett S, Ravenell J. Neighborhood socioeconomic disadvantage; neighborhood racial composition; and hypertension stage, awareness, and treatment among hypertensive black men in New York City: Does nativity matter? J Racial and Ethnic Health Disparities. 2017;4:866–875. doi: 10.1007/s40615-016-0289-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gilbert KL, Elder K, Lyons S, Kaphingst K, Blanchard M, Goodman M. Racial composition over the life course: examining separate and unequal environments and the risk for heart disease for African American men. Ethn Dis. 2015;25:295–304. doi: 10.18865/ed.25.3.295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. White K, Borrell LN, Wong DW, Galea S, Ogedegbe G, Glymour MM. Racial/Ethnic residential segregation and self‐reported hypertension among US‐ and foreign‐born blacks in New York City. Am J Hypertens. 2011;24:904–910. doi: 10.1038/ajh.2011.69 [DOI] [PubMed] [Google Scholar]
- 19. Kershaw KN, Robinson WR, Gordon‐Larsen P, Hicken MT, Goff DC, Carnethon MR, Kiefe CI, Sidney S, Diez Roux AV. Association of changes in neighborhood‐level racial residential segregation with changes in blood pressure among black adults: the CARDIA Study. JAMA Intern Med. 2017;177:996. doi: 10.1001/jamainternmed.2017.1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Li K, Wen M, Henry KA. Ethnic density, immigrant enclaves, and Latino health risks: a propensity score matching approach. Soc Sci Med. 2017;189:44–52. doi: 10.1016/j.socscimed.2017.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lim S, Yi SS, Lundy De La Cruz N, Trinh‐Shevrin C. Defining ethnic enclave and its associations with self‐reported health outcomes among Asian American adults in New York City. J Immigr Minor Health. 2017;19:138–146. doi: 10.1007/s10903-015-0334-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barber S, Diez Roux AV, Cardoso L, Santos S, Toste V, James S, Barreto S, Schmidt M, Giatti L, Chor D. At the intersection of place, race, and health in Brazil: Residential segregation and cardio‐metabolic risk factors in the Brazilian Longitudinal Study of Adult Health (ELSA‐Brasil). Soc Sci Med. 2018;199:67–76. doi: 10.1016/j.socscimed.2017.05.047 [DOI] [PubMed] [Google Scholar]
- 23. Jones A. Segregation and cardiovascular illness: the role of individual and metropolitan socioeconomic status. Health & Place. 2013;22:56–67. doi: 10.1016/j.healthplace.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 24. Brooks C. Alien Neighbors, Foreign Friends: Asian Americans, Housing, and the Transformation of Urban California. Chicago, IL: University of Chicago Press; 2009. [Google Scholar]
- 25. Molina N. Fit to be Citizens?: Public Health and Race in Los Angeles. Oakland, CA: Univ of California Press; 2006:1879–1939. [Google Scholar]
- 26. Pager D, Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Ann Rev Sociol. 2008;34:181–209. doi: 10.1146/annurev.soc.33.040406.131740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & Place. 2011;17:438–448. doi: 10.1016/j.healthplace.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31:178–194. doi: 10.1093/epirev/mxp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Viruell‐Fuentes EA, Miranda PY, Abdulrahim S. More than culture: Structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75:2099–2106. doi: 10.1016/j.socscimed.2011.12.037 [DOI] [PubMed] [Google Scholar]
- 30. Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health & Place. 2009;15:700–708. doi: 10.1016/j.healthplace.2008.10.008 [DOI] [PubMed] [Google Scholar]
- 31. Yang T‐C, Zhao Y, Song Q. Residential segregation and racial disparities in self‐rated health: how do dimensions of residential segregation matter? Soc Sci Res. 2017;61:29–42. doi: 10.1016/j.ssresearch.2016.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bild DE. Multi‐ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113 [DOI] [PubMed] [Google Scholar]
- 33. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 34. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Sl G, Jamerson KA, Jones Daniel W, et al. Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension. 2018;71:1269–1324. doi: 10.1161/HYP.0000000000000066 [DOI] [PubMed] [Google Scholar]
- 35. Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geographical Analysis. 2010;24:189–206. doi: 10.1111/j.1538-4632.1992.tb00261.x [DOI] [Google Scholar]
- 36. Kershaw KN, Osypuk TL, Do DP, De Chavez PJ, Roux AVD. Neighborhood‐level racial/ethnic residential segregation and incident cardiovascular disease the multi‐ethnic study of atherosclerosis. Circulation. 2015;131:141–U59. doi: 10.1161/CIRCULATIONAHA.114.011345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–867. doi: 10.1093/aje/kwm040 [DOI] [PubMed] [Google Scholar]
- 38. Echeverria SE. Reliability of self‐reported neighborhood characteristics. J Urban Health. 2004;81:682–701. doi: 10.1093/jurban/jth151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ainsworth BE, Irwin ML, Addy CL, Whitt MC, Stolarczyk LM. Moderate physical activity patterns of minority women: the cross‐cultural activity participation study. J Womens Health Gend Based Med. 1999;8:805–813. doi: 10.1089/152460999319129 [DOI] [PubMed] [Google Scholar]
- 40. U.S. Department of Health and Human Services . 2008 Physical Activity Guidelines for Americans. 2008;76. [Google Scholar]
- 41. World Health Organ Tech Rep Ser . Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995;854:1–452. [PubMed] [Google Scholar]
- 42. Borrell LN, Menendez BS, Joseph SP. Racial/ethnic disparities on self‐reported hypertension in New York City: examining disparities among Hispanic subgroups. Ethn Dis. 2011;21:429–436. [PubMed] [Google Scholar]
- 43. Kershaw KN, Albrecht SS. Racial/ethnic residential segregation and cardiovascular disease risk. Curr. Cardiovasc. Risk Rep. 2015;9:10. doi: 10.1007/s12170-015-0436-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The Multi‐ethnic Study of Atherosclerosis. Soc Sci Med. 2009;69:110–120. doi: 10.1016/j.socscimed.2009.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Janevic T, Borrell LN, Savitz DA, Echeverria SE, Rundle A. Ethnic enclaves and gestational diabetes among immigrant women in New York City. Soc Sci Med. 2014;120:180–189. doi: 10.1016/j.socscimed.2014.09.026 [DOI] [PubMed] [Google Scholar]
- 46. Yi SS, Ruff RR, Jung M, Waddell EN. Racial/ethnic residential segregation, neighborhood poverty and urinary biomarkers of diet in New York City adults. Soc Sci Med. 2014;122:122–129. doi: 10.1016/j.socscimed.2014.10.030 [DOI] [PubMed] [Google Scholar]
- 47. Forde AT, Lewis TT, Kershaw KN, Bellamy SL, Diez Roux AV. Perceived discrimination and hypertension risk among participants in the multi‐ethnic study of atherosclerosis. J Am Heart Assoc. 2021;10:e019541. doi: 10.1161/JAHA.120.019541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Mujahid MS, Roux AVD, Cooper RC, Shea S, Williams DR. Neighborhood stressors and race/ethnic differences in hypertension prevalence (The Multi‐Ethnic Study of Atherosclerosis). Am J Hypertens. 2011;24:187–193. doi: 10.1038/ajh.2010.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cozier YC, Palmer JR, Horton NJ, Fredman L, Wise LA, Rosenberg L. Relation between neighborhood median housing value and hypertension risk among black women in the United States. Am J Public Health. 2007;97:718–724. doi: 10.2105/AJPH.2005.074740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Woods GL Creating Resilient Black Neighborhoods in Urban Environments Through Effective Community Planning. 2018.
- 51. Mullings L, Wali A. Stress and Resilience. Boston, MA: Springer US; 2001. doi: 10.1007/978-1-4615-1369-8 [DOI] [Google Scholar]
- 52. Blank MB, Mahmood M, Fox JC, Guterbock T. Alternative mental health services: the role of the black church in the south. Am J Public Health. 2002;92:1668–1672. doi: 10.2105/AJPH.92.10.1668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mujahid MS, Sohn EK, Izenberg J, Gao X, Tulier ME, Lee MM, Yen IH. Gentrification and displacement in the san francisco bay area: a comparison of measurement approaches. Int J Environ Res Public Health. 2019;16:2246. doi: 10.3390/ijerph16122246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Schnake‐Mahl AS, Jahn JL, Subramanian SV, Waters MC, Arcaya M. Gentrification, neighborhood change, and population health: a systematic review. J Urban Health. 2020;97:1–25. doi: 10.1007/s11524-019-00400-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gentrification SN. The Encyclopedia of Housing, Van Vliet, W(Ed). London: Taylor & Francis; 1998:198–201. [Google Scholar]
- 56. Iyanda AE, Lu Y. ‘Gentrification is not improving my health’: a mixed‐method investigation of chronic health conditions in rapidly changing urban neighborhoods in Austin, Texas. J Hous Built Environ. 2021;1–24. doi: 10.1007/s10901-021-09847-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Boyd RW, Lindo EG, Weeks LD, McLemore MR. On racism: a new standard for publishing on racial health inequities. Health Affairs Blog. 2020;10. doi: 10.1377/hblog20200630.939347 [DOI] [Google Scholar]
- 58. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]


