Abstract
Background
Despite thrombectomy having become the standard of care for large‐vessel occlusion strokes, acute endovascular management in tandem occlusions, especially of the cervical internal carotid artery lesion, remains uncertain. We aimed to compare efficacy and safety of acute carotid artery stenting to balloon angioplasty alone on treating the cervical lesion in tandem occlusions. Similarly, we aimed to explore those outcomes’ associations with technique approaches and use of thrombolysis.
Methods and Results
We performed a systematic review and meta‐analysis to compare functional outcomes (modified Rankin Scale), reperfusion, and symptomatic intracranial hemorrhage and 3‐month mortality. We explored the association of first approach (anterograde/retrograde) and use of thrombolysis with those outcomes as well. Two independent reviewers performed the screening, data extraction, and quality assessment. A random‐effects model was used for analysis. Thirty‐four studies were included in our systematic review and 9 in the meta‐analysis. Acute carotid artery stenting was associated with higher odds of modified Rankin Scale score ≤2 (odds ratio [OR], 1.95 [95% CI, 1.24–3.05]) and successful reperfusion (OR, 1.89 [95% CI, 1.26–2.83]), with no differences in mortality or symptomatic intracranial hemorrhage rates. Moreover, a retrograde approach was significantly associated with modified Rankin Scale score ≤2 (OR, 1.72 [95% CI, 1.05–2.83]), and no differences were found on thrombolysis status.
Conclusions
Carotid artery stenting and a retrograde approach had higher odds of successful reperfusion and good functional outcomes at 3 months than balloon angioplasty and an anterograde approach, respectively, in patients with tandem occlusions. A randomized controlled trial comparing these techniques with structured antithrombotic regimens and safety outcomes will offer definitive guidance in the optimal management of this complex disease.
Keywords: carotid artery, carotid occlusive disease, intervention, reperfusion, stroke
Subject Categories: Ischemic Stroke
Nonstandard Abbreviations and Acronyms
- BA
balloon angioplasty
- CAS
carotid artery stenting
- ICA
internal carotid artery
- IVT
intravenous thrombolysis
- mRS
modified Rankin Scale
- MT
mechanical thrombectomy
- sICH
symptomatic intracranial hemorrhage
- TO
tandem occlusion
Clinical Perspective
What Is New?
Cervical carotid stenting is found to be an effective treatment for tandem occlusions, showing better functional outcomes and reperfusion rates when compared with balloon angioplasty.
Performing mechanical thrombectomy before cervical recanalization was observed to be the most effective approach (retrograde approach).
Moreover, intravenous thrombolysis in patients receiving cervical carotid stenting was observed to be safe, without an increased risk of symptomatic intracranial hemorrhage.
What Are the Clinical Implications?
Acute cervical carotid stenting after cerebral reperfusion is a reasonable therapeutic option for patients with intracranial large‐vessel occlusion and concomitant cervical tandem occlusions.
A multicenter randomized clinical trial is the natural next step to achieve a standard of care paradigm.
Tandem occlusions (TOs) involve high‐grade stenosis or occlusion of the cervical internal carotid artery (ICA) and concomitant intracranial large‐vessel occlusion. These lesions represent 10% to 20% of all strokes, 1 and are associated with poor prognosis, severe disability, and mortality when left untreated. 2 Acute TOs have shown poor response to intravenous thrombolysis (IVT), with recanalization rates <10%. 3 A subgroup analysis of the Highly Effective Reperfusion Using Multiple Endovascular Devices meta‐analysis found mechanical thrombectomy (MT) may be beneficial for LVOs resulting from TOs. However, there was a paucity of data in regard to the management of the concomitant cervical lesion. 4
Endovascular management of TOs widely varies according to clinical and technical considerations and proceduralist’s preference. 5 Revascularization of the cervical lesion could be performed in an acute or a deferred manner. When performed acutely, carotid artery stenting (CAS)±balloon angioplasty (BA) is a definitive treatment strategy, performed before or following intracranial MT. Acute BA, suction aspiration of the cervical segment, or MT alone implicate a deferred treatment with endarterectomy or stenting in the following days or weeks. Each treatment carries potential risks that are taken into consideration when selecting the best treatment method. For instance, acute CAS involves the risk of symptomatic intracranial hemorrhage (sICH) associated with antithrombotic use in freshly reperfused brain tissue and stent thrombosis. 6 , 7 In contrast, deferred cervical revascularization can be done in a more planned and secure setting. 8 Although it avoids the immediate need for antithrombotics and potential sICH risk, 5 it carries the risk of stroke recurrence and/or progression. 9
Recent studies suggest a benefit in functional outcomes and reperfusion rates when CAS and MT are performed emergently, without increased rates of sICH. 10 , 11 , 12 Moreover, Anadani et al found IVT was not associated with an increased risk of hemorrhagic transformation. 11 Nevertheless, data from randomized controlled trials on optimal management, procedural features, and safety outcomes are still missing, and all the above‐mentioned approaches are used in clinical practice. 5
We aimed to compare the efficacy and safety of CAS±angioplasty with BA alone of the cervical ICA in treating TOs through an aggregated data meta‐analysis of the recent literature. Additionally, we aimed to explore the association of the technique approaches (anterograde and retrograde) with the functional and safety outcomes and IVT with sICH.
METHODS
Search Strategy and Selection Criteria
This systematic review and meta‐analysis follows the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines. We executed a comprehensive literature search using a combination of Medical Subject Headings terms and free text for the concepts of “tandem occlusion,” “thrombectomy,” “stent,” “acute stroke,” and “carotid artery disease” in the MEDLINE database, Embase, and the Web of Science from January 2015 through May 2020. We included studies from 2015 that included the randomized controlled trials supporting the benefit of MT as the standard treatment for acute large‐vessel occlusionstarted at that time. Complete search strategy is detailed in Data S1.
We searched for studies assessing patients presenting with acute high‐grade stenosis (70%–99%) or occlusion of the cervical ICA with ipsilateral occlusion of the distal ICA and/or middle cerebral artery treated with MT and endovascular treatment of the extracranial ICA (CAS and/or BA). Inclusion criteria were randomized controlled trials, cohort and cross‐sectional studies, case series with ≥10 patients, and case‐control studies reporting clinical outcomes (modified Rankin Scale [mRS] scores), complications (sICH, embolization, and death), and reperfusion rates. We only included publications with full text in English. We excluded animal models, protocols, reviews, studies with <10 patients, case reports, and other meta‐analyses. When we encountered studies with multiple reports from the same patient cohort, we kept the report with the higher number of patients and longer follow‐up times. Furthermore, we searched the references of all the included studies to find additional studies.
Two independent reviewers initially screened all identified records by reading all titles/abstracts using a free online application for systematic reviews (https://rayyan.qcri.org/). Then, potentially relevant articles were reviewed as full text. The reviewers performed data extraction from these studies and cross‐checked the extracted data. Disagreements in any of these steps were resolved after discussion or with a third senior reviewer when needed.
Identified studies from the literature search were then further evaluated for inclusion in the meta‐analysis. For the main meta‐analysis on the best cervical technique, we only included studies with complete data that compared our outcomes of interest between acute CAS±BA and BA alone. Similarly, for best order of treatment we included studies with acute CAS that compared the outcomes between anterograde and retrograde approaches. Finally, for evaluating the association of IVT status with sICH, we included studies with acute CAS with both IVT groups.
Baseline Data and Outcome Variables
From each study, we collected demographic information, including number of participants, age, sex, race and ethnicity, comorbidities (hypertension, atrial fibrillation, dyslipidemia, diabetes, coronary artery disease, ICA stenosis), smoking status, initial assessment at presentation, use of IVT, stroke workflow metrics (onset to arrival, onset to puncture, onset to revascularization, and puncture to revascularization), location of the intracranial occlusion, type of endovascular interventions, number of patients undergoing each type of treatment, first endovascular approach (anterograde when proximal ICA occlusion was treated first and retrograde when intracranial occlusion was treated first), devices used (stent and balloon type, embolic protection device), concurrent medications (tissue‐type plasminogen activator, anticoagulants, and antiplatelets), procedure‐related complications (new stroke, hemorrhage, hemodynamic impairment, acute stent thrombosis), technical success rates of carotid revascularization, and outcome variables. We separately extracted data of interest about the TO revascularization approach and technique including revascularization order in patients undergoing CAS (anterograde versus retrograde), patients with stenting, and patients with angioplasty only as available.
The primary outcome was functional outcomes scored by mRS at 90 days. We dichotomized the results as good (0–2) and poor (3–6) outcomes. Secondary efficacy outcomes included reperfusion status assessed by the modified Thrombolysis in Cerebral Infarction grading system. Safety outcomes included sICH as defined by each study and mortality at 90 days.
Study Quality and Risk of Bias Assessment
We evaluated the quality of the studies using tools according to the study’s design. For cohorts with control groups, we used the risk of bias in nonrandomized studies of interventions tool, 13 with the overall risk of bias rated as low, moderate, serious, and critical. Single‐arm cohorts were evaluated using the National Institutes of Health quality assessment tool for before–after (pre–post) studies with no control group, 14 with the overall risk of bias rated as good, fair, and poor.
Statistical Analysis
A revised Cochrane risk of bias in randomized trials tool 15 was used for randomized controlled trials with the overall risk of bias rated as low, some concerns, and high risk.
We used a random‐effects model (Mantel‐Haenszel method) for combining cumulative event rates to account for heterogeneity (I 2) between studies to directly compare the efficacy and safety outcomes between CAS and BA alone. Summary effect measures (odds ratios [ORs]) were calculated using data extracted from primary studies and were compared using 95% CIs and prediction intervals. Similarly, we compared the same outcomes after classifying the patients undergoing CAS by first endovascular approach (anterograde versus retrograde) and IVT status (received or not).
Finally, we evaluated the heterogeneity between studies with visual assessment of forest plots, as well as χ2 test. We defined important interstudy heterogeneity as an I 2 test result of >50% and a χ2 test result of <0.1. Analysis was conducted using Review Manager 5. 16 Publication bias was graphically assessed by funnel plot inspection and analyzed by Egger test conducted in R software (R Foundation for Statistical Computing) for Windows version 3.5.2.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
RESULTS
Literature Search and Study Selection
We initially identified 1404 articles through database searching, and 1105 records were screened after duplicates were removed, of which 59 full texts were assessed for eligibility. Twenty‐five studies were excluded, 18 of them reported different endovascular approaches or techniques for treating the cervical ICA grouped (CAS, BA, flow diversion, no CAS, or no acute treatment), 3 analyzed MT of TOs without cervical revascularization, 2 had different outcomes of interest, and 2 grouped TOs and isolated ICA. Finally, 34 studies including 3014 patients with TOs (2482 CAS and 245 BA) were included in our systematic review (Table S1), and 9 were included in our meta‐analysis assessing the best endovascular technique for TOs. Screening and selection of studies are detailed in the flow diagram (Figure 1).
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses flow diagram.
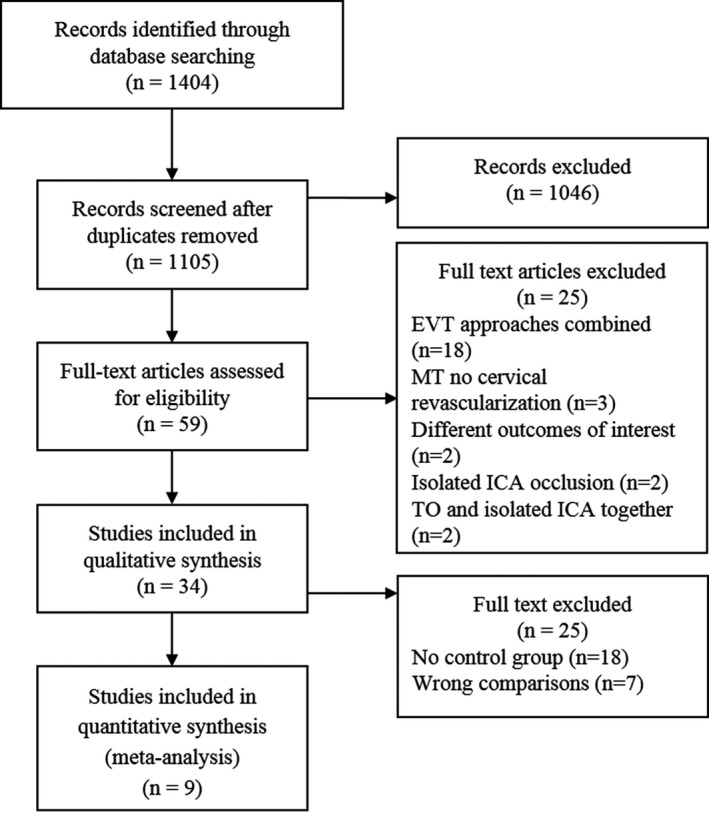
EVT indicates endovascular therapy; ICA, internal carotid artery; MT, mechanical thrombectomy; and TO, tandem occlusion.
Studies included in the review contained the primary outcome and at least 1 of the other outcomes of interest. Thirty‐three studies were retrospective cohort studies (22 single‐center and 11 multicenter), and 1 was a single‐center pilot randomized controlled trial study. 17 Of the 33 cohort studies, 17 were from prospectively collected databases. Fifteen studies evaluated outcomes of CAS±BA, 7 , 10 , 11 , 12 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 and 1 evaluated BA‐alone outcomes without comparison groups. 8 Two studies compared CAS in TOs to isolated proximal ICA stenosis, 6 , 29 2 compared CAS in TOs with MT in isolated LVOs, 30 , 31 3 compared CAS with other endovascular techniques combined in TOs, 32 , 33 , 34 1 compared CAS with carotid endarterectomy, 35 and 9 compared CAS to BA. 9 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43
Characteristics of the studies included in the systematic review are summarized in Table S1. Studies were heterogenous on type of intervention, use of embolic protection device (6/34), antiplatelet regimen, information on concurrent management (heparin and antiplatelets), definition of sICH and any intracranial hemorrhage (8/34), and outcome evaluations (15/34 evaluated in stent thrombosis or reocclusion). The type of endovascular approach was reported in most of the studies, but only 4 studies explored the best first approach (anterograde versus retrograde) and compared our outcomes of interest between both groups. Antiplatelet therapy was inconsistently reported in the included studies, and only 4 studies of patients undergoing CAS reported sICH rates in patients with and without IV tissue‐type plasminogen activator use.
Qualitative Analysis
Of the 20 retrospective studies with control groups included in the systematic review and meta‐analysis assessed by the risk of bias in nonrandomized studies of interventions tool, 11 studies had moderate overall risk of bias assessments, and 9 had serious overall risk of bias assessments (Figure S1A). When the bias was assessed per domain, 6 studies had serious risk because of missing data at the 3‐month follow‐up, 6 had serious risk of confounding bias, and 1 had risk because of the classification of the interventions. Only 1 study 42 mentioned a blinded assessment of mRS score at follow‐up (Figure S1B).
Studies with no comparison group assessed by the pre–post tool were of variable quality rating, most of them were rated fair (10/14) to good (3/14), but 1 was rated poor 27 because of unclear objectives and inclusion criteria, not including all the eligible participants, small sample size, and loss at follow‐up (Table S2). The randomized pilot trial by Poppe et al had some concerns of bias because of deviation from the intended intervention and in the measurement of the outcome (Table S3).
Meta‐Analysis of Included Studies
For assessing the best endovascular technique, we included 9 studies in the meta‐analysis of the primary outcome. Stenting was associated with favorable mRS scores at 3 months (OR, 1.95 [95% CI, 1.24–3.05]) (Figure 2A). 9 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 The 95% prediction interval, however, ranged from 0.69 to 5.48, indicating some uncertainty with the treatment effect of CAS on functional outcome. No significant heterogeneity between studies was found for this outcome (I 2=31.0%, χ2=11.65, P=0.17). Eight studies were included in the meta‐analysis of the reperfusion outcome; CAS was associated with higher odds of Thrombolysis in Cerebral Infarction grade 2b‐3 (OR, 1.89 [95% CI, 1.26–2.83]), with no significant heterogeneity between studies (I 2=30.0%, χ2=10.01, P=0.19), although the 95% prediction interval ranged from 0.55 to 6.66 (Figure 2B). 9 , 36 , 37 , 38 , 40 , 41 , 42 , 43 There were no statistically significant differences in mortality at 3 months (OR, 0.79 [95% CI, 0.50–1.27]) or sICH (OR, 1.31 [95% CI, 0.62–2.77]), although the direction of the association suggested lower odds of death and higher odds of sICH with stenting (Figure 2C and 2D). 9 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43
Figure 2. Meta‐analysis of (A) good functional outcome at 90 days (modified Rankin Scale score of 0–2), (B) good reperfusion status Thrombolysis in Cerebral Infarction grade 2b‐3, (C) symptomatic intracranial hemorrhage, and (D) mortality in patients with acute stenting vs balloon angioplasty.
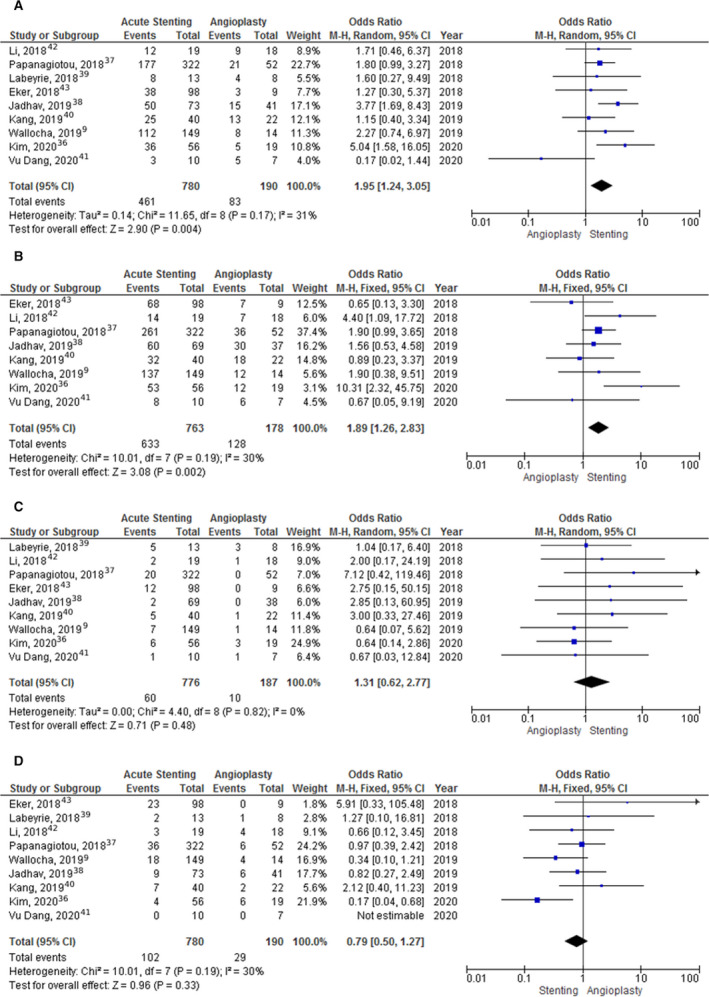
M‐H indicates Mantel‐Haenszel.
A total of 4 studies provided data to compare safety and efficacy outcomes based on anterograde and retrograde approaches. 12 , 22 , 25 , 40 The meta‐analysis of the primary outcome showed the retrograde approach was associated with higher odds of favorable mRS scores at 3 months (OR, 1.72 [95% CI, 1.05–2.83]) with no heterogeneity (I 2=0%, χ2=0.79, P=0.85) and Thrombolysis in Cerebral Infarction grade 2b‐3 (OR, 3.18 [95% CI, 1.50–6.74]) with no significant heterogeneity (I 2=18%, χ2=3.66, P=0.30). There were no statistically significant differences on mortality at 3 months (OR, 0.84 [95% CI, 0.40–1.77]) or sICH (OR, 0.81 [95% CI, 0.29–2.33]) between approaches (Figure 3A through 3D). 12 , 22 , 25 , 40
Figure 3. Meta‐analysis of (A) functional outcome at 90 days (modified Rankin Scale score of 0–2), (B) good reperfusion status Thrombolysis in Cerebral Infarction grade 2b‐3, (C) symptomatic intracranial hemorrhage, and (D) mortality in patients with an anterograde vs retrograde approach.
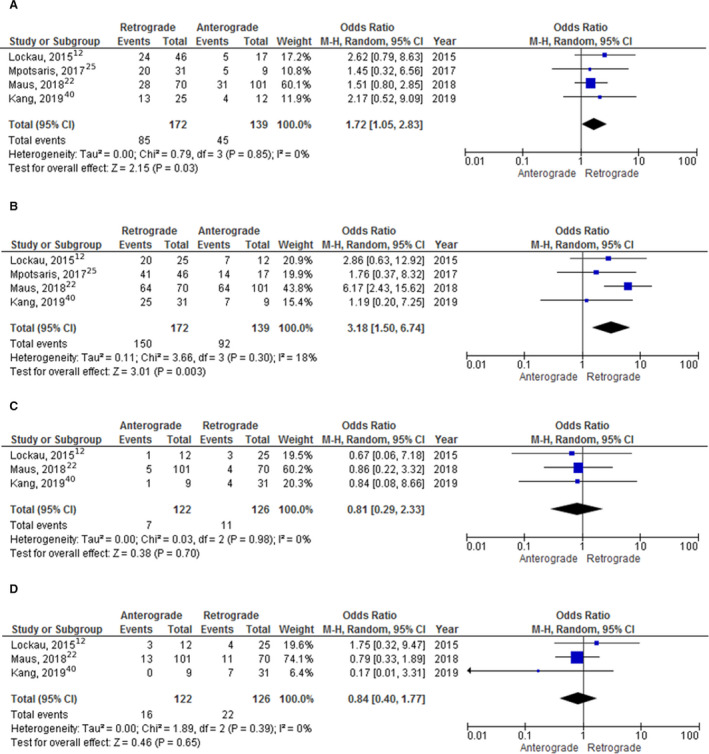
M‐H indicates Mantel‐Haenszel.
A total of 4 studies provided data for comparing our safety outcome in patients treated with CAS, MT, and IV tissue‐type plasminogen activator to patients treated with CAS and MT alone. 10 , 11 , 19 , 23 The meta‐analysis showed no statistically significant difference in the rates of sICH between both groups (OR, 0.66 [95% CI, 0.19–2.30]) (Figure S2).
No evidence of publication bias was found by inspecting the funnel plots and Egger test in most of the outcomes, except for the comparison on successful reperfusion stratified by the best first approach, which demonstrated a significant asymmetry by Egger test (P=0.02) (Figures S3 through S5).
DISCUSSION
This systematic review and meta‐analysis demonstrates that acute cervical CAS in patients presenting with TOs is effective and safe in the setting of MT. Patients treated with CAS have significantly better reperfusion rates and 3‐month functional outcomes, without a significant increase in the rates of sICH or mortality. A retrograde approach might have better functional outcomes and reperfusion rates as well. Finally, receiving IVT does not increase the sICH rates in patients who undergo CAS.
Our meta‐analysis attempted to address a common and controversial matter during the endovascular treatment of the proximal ICA in TOs. 44 As previously shown by our published international survey, emergent CAS±angioplasty and BA with local aspiration seem to be equally preferred techniques (41% versus 38%). 5 Certainly, both CAS and BA have advantages and risks to consider when facing a TO. Because of the wide variety of factors to weigh, proceduralists currently retain full discretion over individual case technique selections, which leads to wide practice variability. 45 CAS seems more effective in treating the cervical ICA lesion and directly treating the cause of the stroke when atherosclerotic plaques or dissections are the culprits. Thus, it decreases the risk of stroke recurrence immediately 9 while improving cerebral reperfusion, clot lysis, or even allowing spontaneous intracranial reperfusion, 22 , 24 , 46 at the expenses of a potential risk for acute stent thrombosis and the need for early antithrombotic therapy. 47 On the other hand, BA may prevent futile stenting in patients with poor outcomes 8 and the need of antithrombotics, but with the shortcoming of a potential risk of thrombus formation and stroke recurrence. 37 , 48 , 49 In our analysis, CAS demonstrated an association with better functional outcomes at 3 months, and despite the concerns about increased risk of sICH in association with CAS, we did not find an increase in its rates or mortality. Similarly, our results showed no statistical difference in sICH rates between patients undergoing CAS with and without IVT. Our results are in agreement with previous TITAN (Thrombectomy In Tandem Lesion) study reports of hemorrhagic transformation and support a more aggressive treatment using acute stenting with dual antithrombotic regimen. 37 , 50
Initial studies reported pooled data of patients with TOs treated with MT±CAS and compared the recanalization rates and functional and safety outcomes with outcomes from patients with isolated intracranial large‐vessel occlusiontreated with MT, which confirmed the benefit of MT in TOs, as previously published in the Goyal et al collaboration. 4 , 28 , 51 , 52 Other meta‐analyses compared patients undergoing CAS with patients with no stenting, including in the latter several modalities angioplasty±aspiration, suction alone, flow diversion, and clot wire‐disruption as treatment modalities. 1 , 53 For instance, Dufort et al combined multiple cervical treatment regimens (BA, aspiration, and CAS) and patients with no acute treatment in the nonstenting cohort. Despite this heterogeneity, they found similar results to ours, favoring CAS over no stenting in regard to functional independence (OR, 1.43 [95% CI, 1.07–1.91]); however, BA effect size could not be evaluated separately. 53 Interestingly, the Wilson et al meta‐analysis compared CAS with BA, but they found no differences in efficacy and safety outcomes. The discrepancy with our study might be explained by the fact that they did not incorporate 2 recent studies, 1 of them a large single‐center cohort of 163 patients that showed early neurological improvements in their CAS group. 9 Furthermore, they included noncomparative retrospective studies that only assessed 1 of the techniques without comparison groups (13 CAS and 3 BA studies), which might have introduced additional heterogeneity (I 2 ≥50% for each technique and functional outcome). 51 In our meta‐analysis, we exclusively included studies that defined the endovascular revascularization procedures performed in the proximal ICA (CAS or BA) and compared both techniques on our outcomes of interest. Similarly, the studies defined the degree of ICA stenosis (70%–99%) in their methodology, all of these to decrease heterogeneity. More importantly and considering that MT became the standard of care in 2015, our meta‐analysis comprises all large recent studies to account for the expected acquired improvement in endovascular treatment techniques over time that might have favored outcomes for CAS.
The order in which the cervical and intracranial lesions should be treated has been under investigation because of the various reasons for preferring one approach over the other. 12 , 54 Favorable outcomes in the retrograde approach might relate to faster reperfusion times of the intracranial LVO. Additionally, it involves a decreased risk of distal embolization and hemodynamic instability. Yet the steno‐occlusive lesion may be difficult to access intracranially and restrict technical success of the intracranial MT. Our meta‐analysis is the first to demonstrate an association of the retrograde approach with good functional outcomes and successful reperfusion in patients undergoing CAS. Previously, Wilson et al reported no statistical differences between the approaches; however, their approach groups included studies with BA, aspiration, or CAS as neck recanalization techniques and were not directly comparing each technique, resulting in significant heterogeneity (I 2=63%). 51 We included 4 studies of only patients undergoing CAS in evaluating this subject and reported revascularization rates and good functional outcome. 12 , 22 , 25 , 40 Despite our significant results, it is important to recognized that many confounders play a role in the outcomes of interest, such as infarct core, collateral vasculature, time to reperfusion, and grade of stenosis of the proximal ICA, which were not collected in all the aforementioned studies. Maus et al in their international multicenter study found a successful reperfusion rate of 92% in their retrograde cohort; however, the rate of favorable outcome was only 44%. 22
Our study has several limitations. First, almost all the studies included in our systematic review (33/34) have a retrospective design. Allocation to intervention and concomitant management were decided by treating physicians. Factors that may have influenced both decisions, including premorbid functional state, stroke severity, type of antiplatelet agents used, and cause of stroke were not systematically reported in the included series. Additionally, more patients were treated with CAS than BA alone, which makes the studies heterogeneous and potentially biased. Furthermore, the definition of outcomes and protocols varied across the different studies. We also observed wide PIs when analyzing the primary outcomes. This may have been favored by the small number of studies reflecting some uncertainty about the effects of the techniques. Moreover, they may indicate the existence of settings where stenting has a suboptimal effect. The antithrombotic regimen was not regularly reported in most of the studies. Some multicenter studies even differed between their center’s protocols.
All these aspects should be considered when interpreting the results of our analysis. However, our meta‐analysis has the strength of comparing acute stenting versus BA only and includes the most recent TO cohorts with severe stenosis ≥70%. We suggest a prospective evaluation of both techniques, and an optimal antithrombotic regimen before and after emergent CAS in the acute stroke setting should be further evaluated.
CONCLUSIONS
Acute CAS of the proximal ICA lesion in TOs is effective and safe. CAS and a retrograde approach have higher odds of successful reperfusion and good functional outcomes at 3 months than BA and an anterograde approach, respectively. CAS seems safe even in patients who received IVT, with no increase of sICH rates. Hence, an aggressive management of TOs should be considered in clinical practice. However, there are still insufficient data about stent patency and antithrombotic therapy that might influence the evaluated outcomes. The limitations of this meta‐analysis may pave the way for a definitive, multicenter, high‐quality randomized controlled trial evaluating both techniques, where structured antithrombotic regimens and systematically measured efficacy and safety outcomes will provide more guidance in the optimal management of this complex disease.
Sources of Funding
None.
Disclosures
Dr Ortega‐Gutierrez reports consulting for Medtronic and Stryker Neurovascular. Dr Zaidat reports consulting and speaking for Cerenovus, Stryker, Penumbra, and Medtronic. The remaining authors have no disclosures to report.
Supporting information
Data S1
Tables S1–S3
Figures S1–S5
This article was sent to Sean Savitz, MD, PhD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.022335
For Sources of Funding and Disclosures, see page 8.
REFERENCES
- 1. Coelho AP, Lobo M, Gouveia R, Silveira D, Campos J, Augusto R, Coelho N, Canedo A. Overview of evidence on emergency carotid stenting in patients with acute ischemic stroke due to tandem occlusions: a systematic review and meta‐analysis. J Cardiovasc Surg. 2019;60:693–702. doi: 10.23736/S0021-9509.18.10312-0 [DOI] [PubMed] [Google Scholar]
- 2. Seet RCS, Wijdicks EFM, Rabinstein AA. Stroke from acute cervical internal carotid artery occlusion: treatment results and predictors of outcome. Arch Neurol. 2012;69:1615–1620. doi: 10.1001/archneurol.2012.2569 [DOI] [PubMed] [Google Scholar]
- 3. Rubiera M, Ribo M, Delgado‐Mederos R, Santamarina E, Delgado P, Montaner J, Alvarez‐Sabin J, Molina CA. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006;37:2301–2305. doi: 10.1161/01.STR.0000237070.80133.1d [DOI] [PubMed] [Google Scholar]
- 4. Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, van der Lugt A, de Miquel MA, et al. Endovascular thrombectomy after large‐vessel ischaemic stroke: a meta‐analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 5. Zevallos CB, Farooqui M, Quispe‐Orozco D, Mendez‐Ruiz A, Patterson M, Below K, Martins SO, Mansour OY, Mont’Alverne F, Nguyen TN, et al. Proximal internal carotid artery acute stroke secondary to tandem occlusions (PICASSO) international survey. J Neurointerv Surg. 2021;13:1106–1110. doi: 10.1136/neurintsurg-2020-017025 [DOI] [PubMed] [Google Scholar]
- 6. Steglich‐Arnholm H, Holtmannspötter M, Kondziella D, Wagner A, Stavngaard T, Cronqvist ME, Hansen K, Højgaard J, Taudorf S, Krieger DW. Thrombectomy assisted by carotid stenting in acute ischemic stroke management: benefits and harms. J Neurol. 2015;262:2668–2675. doi: 10.1007/s00415-015-7895-0 [DOI] [PubMed] [Google Scholar]
- 7. Heck DV, Brown MD. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. J Neurointerv Surg. 2015;7:170–175. doi: 10.1136/neurintsurg-2014-011224 [DOI] [PubMed] [Google Scholar]
- 8. Akpinar CK, Gürkaş E, Aytac E. Carotid angioplasty‐assisted mechanical thrombectomy without urgent stenting may be a better option in acute tandem occlusions. Interv Neuroradiol. 2017;23:405–411. doi: 10.1177/1591019917701113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wallocha M, Chapot R, Nordmeyer H, Fiehler J, Weber R, Stracke CP. Treatment methods and early neurologic improvement after endovascular treatment of tandem occlusions in acute ischemic stroke. Front Neurol. 2019;10:127. doi: 10.3389/fneur.2019.00127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lucena AF, Castro‐Afonso LH, Monsignore LM, Nakiri GS, Fábio SR, Pontes Neto O, Abud DG. Carotid artery stenting in the context of endovascular treatment of acute ischemic stroke. Arq Neuropsiquiatr. 2016;74:212–218. doi: 10.1590/0004-282X20150213 [DOI] [PubMed] [Google Scholar]
- 11. Anadani M, Spiotta AM, Alawieh A, Turjman F, Piotin M, Haussen DC, Nogueira RG, Papanagiotou P, Siddiqui AH, Lapergue B, et al. Emergent carotid stenting plus thrombectomy after thrombolysis in tandem strokes: analysis of the TITAN registry. Stroke. 2019;50:2250–2252. doi: 10.1161/STROKEAHA.118.024733 [DOI] [PubMed] [Google Scholar]
- 12. Lockau H, Liebig T, Henning T, Neuschmelting V, Stetefeld H, Kabbasch C, Dorn F. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology. 2015;57:589–598. doi: 10.1007/s00234-014-1465-5 [DOI] [PubMed] [Google Scholar]
- 13. Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, et al. ROBINS‐I: a tool for assessing risk of bias in non‐randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. US Department of Health and Human Services–National Institute of Health (NIH) . Quality assessment tool for before‐after (pre‐post) studies with no control group. 2014.
- 15. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H‐Y, Corbett MS, Eldridge SM, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 16. Review Manager (RevMan). The Nordic Cochrane Centre; 2014. [Google Scholar]
- 17. Poppe AY, Jacquin G, Stapf C, Daneault N, Deschaintre Y, Gioia LC, Odier C, Labrie M, Nehme A, Nico L, et al. A randomized pilot study of patients with tandem carotid lesions undergoing thrombectomy. J Neuroradiol. 2020;47:416–420. doi: 10.1016/j.neurad.2019.08.003 [DOI] [PubMed] [Google Scholar]
- 18. Yilmaz U, Körner H, Mühl‐Benninghaus R, Simgen A, Kraus C, Walter S, Behnke S, Faßbender K, Reith W, Unger MM. Acute occlusions of dual‐layer carotid stents after endovascular emergency treatment of tandem lesions. Stroke. 2017;48:2171–2175. doi: 10.1161/STROKEAHA.116.015965 [DOI] [PubMed] [Google Scholar]
- 19. Pfaff JAR, Maurer C, Broussalis E, Janssen H, Blanc R, Dargazanli C, Costalat V, Piotin M, Runck F, Berlis A, et al. Acute thromboses and occlusions of dual layer carotid stents in endovascular treatment of tandem occlusions. J Neurointerv Surg. 2020;12:33–37. doi: 10.1136/neurintsurg-2019-015032 [DOI] [PubMed] [Google Scholar]
- 20. Park SE, Choi DS, Baek HJ, Kim CH, Choi HC, Cho SB, Lee S, Ahn JH. Endovascular therapy of acute ischemic stroke related to tandem occlusion: comparison of occlusion and severe stenosis of the proximal cervical internal carotid artery. Br J Radiol. 2019;92:20180051. doi: 10.1259/bjr.20180051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maus V, Behme D, Borggrefe J, Kabbasch C, Seker F, Hüseyin C, Barnikol U, Yeo L, Brouwer P, Söderman M, et al. Carotid artery stenosis contralateral to acute tandem occlusion: an independent predictor of poor clinical outcome after mechanical thrombectomy with concomitant carotid artery stenting. Cerebrovasc Dis. 2018;45:10–17. doi: 10.1159/000484719 [DOI] [PubMed] [Google Scholar]
- 22. Maus V, Borggrefe J, Behme D, Kabbasch C, Abdullayev N, Barnikol U, Yeo L, Brouwer P, Söderman M, Möhlenbruch M, et al. Order of treatment matters in ischemic stroke: mechanical thrombectomy first, then carotid artery stenting for tandem lesions of the anterior circulation. Cerebrovasc Dis. 2018;46:59–65. doi: 10.1159/000492158 [DOI] [PubMed] [Google Scholar]
- 23. Spiotta AM, Lena J, Vargas J, Hawk H, Turner RD, Chaudry MI, Turk AS. Proximal to distal approach in the treatment of tandem occlusions causing an acute stroke. J Neurointerv Surg. 2015;7:164–169. doi: 10.1136/neurintsurg-2013-011040 [DOI] [PubMed] [Google Scholar]
- 24. Yoon W, Kim BM, Kim DJ, Kim DI, Kim SK. Outcomes and prognostic factors after emergent carotid artery stenting for hyperacute stroke within 6 hours of symptom onset. Neurosurgery. 2015;76:321–329. doi: 10.1227/NEU.0000000000000610 [DOI] [PubMed] [Google Scholar]
- 25. Mpotsaris A, Kabbasch C, Borggrefe J, Gontu V, Soderman M. Stenting of the cervical internal carotid artery in acute stroke management: the Karolinska experience. Interv Neuroradiol. 2017;23:159–165. doi: 10.1177/1591019916681983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Behme D, Mpotsaris A, Zeyen P, Psychogios MN, Kowoll A, Maurer CJ, Joachimski F, Liman J, Wasser K, Kabbasch C, et al. Emergency stenting of the extracranial internal carotid artery in combination with anterior circulation thrombectomy in acute ischemic stroke: a retrospective multicenter study. AJNR Am J Neuroradiol. 2015;36:2340–2345. doi: 10.3174/ajnr.A4459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR. Extracranial carotid artery stenting followed by intracranial stent‐based thrombectomy for acute tandem occlusive disease. J Neurointerv Surg. 2015;7:412–417. doi: 10.1136/neurintsurg-2014-011175 [DOI] [PubMed] [Google Scholar]
- 28. Sadeh‐Gonik U, Tau N, Friehmann T, Bracard S, Anxionnat R, Derelle A‐L, Tonnelet R, Liao L, Richard S, Armoiry X, et al. Thrombectomy outcomes for acute stroke patients with anterior circulation tandem lesions: a clinical registry and an update of a systematic review with meta‐analysis. Eur J Neurol. 2018;25:693–700. doi: 10.1111/ene.13577 [DOI] [PubMed] [Google Scholar]
- 29. Runck F, Maurer CJ, Berlis A. Complication rates using CASPER dual‐layer stents for carotid artery stenting in acute stroke: a 3‐year single center experience. Neuroradiology. 2021;31:173–179. doi: 10.1007/s00062-019-00860-7 [DOI] [PubMed] [Google Scholar]
- 30. Bücke P, Pérez MA, AlMatter M, Hellstern V, Bäzner H, Henkes H. Functional outcome and safety of intracranial thrombectomy after emergent extracranial stenting in acute ischemic stroke due to tandem occlusions. Front Neurol. 2018;9:940. doi: 10.3389/fneur.2018.00940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rodriguez‐Lopez C, Marco FB, Guzman JD. Prognosis of tandem occlusions versus isolated intracranial occlusions. J Stroke Cerebrovasc Dis. 2018;27:3652–3656. doi: 10.1016/j.jstrokecerebrovasdis.2018.08.039 [DOI] [PubMed] [Google Scholar]
- 32. Fahed R, Redjem H, Blanc R, Labreuche J, Robert T, Ciccio G, Smadja D, Smajda S, Piotin M. Endovascular management of acute ischemic strokes with tandem occlusions. Cerebrovasc Dis. 2016;41:298–305. doi: 10.1159/000444068 [DOI] [PubMed] [Google Scholar]
- 33. Lescher S, Czeppan K, Porto L, Singer OC, Berkefeld J. Acute stroke and obstruction of the extracranial carotid artery combined with intracranial tandem occlusion: results of interventional revascularization. Cardiovasc Intervent Radiol. 2015;38:304–313. doi: 10.1007/s00270-014-1047-2 [DOI] [PubMed] [Google Scholar]
- 34. Maurer CJ, Joachimski F, Berlis A. Two in one: endovascular treatment of acute tandem occlusions in the anterior circulation. Clin Neuroradiol. 2015;25:397–402. doi: 10.1007/s00062-014-0318-2 [DOI] [PubMed] [Google Scholar]
- 35. Slawski DE, Jumaa MA, Salahuddin H, Shawver J, Humayun MJ, Russell T, Seiwert A, Paolini D, Abbas J, Nazzal M, et al. Emergent carotid endarterectomy versus stenting in acute stroke patients with tandem occlusion. J Vasc Surg. 2018;68:1047–1053. doi: 10.1016/j.jvs.2017.12.077 [DOI] [PubMed] [Google Scholar]
- 36. Kim B, Kim BM, Bang OY, Baek J‐H, Heo JH, Nam HS, Kim YD, Yoo J, Kim DJ, Jeon P, et al. Carotid artery stenting and intracranial thrombectomy for tandem cervical and intracranial artery occlusions. Neurosurgery. 2020;86:213–220. doi: 10.1093/neuros/nyz026 [DOI] [PubMed] [Google Scholar]
- 37. Papanagiotou P, Haussen DC, Turjman F, Labreuche J, Piotin M, Kastrup A, Steglich‐Arnholm H, Holtmannspötter M, Taschner C, Eiden S, et al. Carotid stenting with antithrombotic agents and intracranial thrombectomy leads to the highest recanalization rate in patients with acute stroke with tandem lesions. JACC Cardiovasc Interv. 2018;11:1290–1299. doi: 10.1016/j.jcin.2018.05.036 [DOI] [PubMed] [Google Scholar]
- 38. Jadhav AP, Zaidat OO, Liebeskind DS, Yavagal DR, Haussen DC, Hellinger FR, Jahan R, Jumaa MA, Szeder V, Nogueira RG, et al. Emergent management of tandem lesions in acute ischemic stroke: analysis of the STRATIS registry. Stroke. 2019;50:428–433. doi: 10.1161/STROKEAHA.118.021893 [DOI] [PubMed] [Google Scholar]
- 39. Labeyrie MA, Ducroux C, Civelli V, Reiner P, Cognat E, Aymard A, Bisdorff A, Saint‐Maurice JP, Houdart E. Endovascular management of extracranial occlusions at the hyperacute phase of stroke with tandem occlusions. J Neuroradiol. 2018;45:196–201. doi: 10.1016/j.neurad.2017.10.003 [DOI] [PubMed] [Google Scholar]
- 40. Kang DH, Kim YW, Hwang YH, Kim YS. Endovascular recanalization of acute tandem cervical carotid and intracranial occlusions: efficacy of cervical balloon angioplasty alone then intracranial target recanalization strategy. World Neurosurg. 2019;126:e1268–e1275. doi: 10.1016/j.wneu.2019.02.240 [DOI] [PubMed] [Google Scholar]
- 41. Vu‐Dang L, Nguyen QA, Nguyen‐Thi‐Thu T, Tran AT, Le‐Chi C, Le‐Hoang K, Nguyen‐Tat T, Nguyen‐Huu A, Pham‐Minh T, Chu‐Dinh T, et al. Endovascular treatment for acute tandem occlusion stroke: results from case series of 17 patients. Ann Indian Acad Neurol. 2020;23:78–83. doi: 10.4103/aian.AIAN_464_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Li W, Chen Z, Dai Z, Liu R, Yin Q, Wang H, Hao Y, Han Y, Qiu Z, Xiong Y, et al. Management of acute tandem occlusions: stent‐retriever thrombectomy with emergency stenting or angioplasty. J Int Med Res. 2018;46:2578–2586. doi: 10.1177/0300060518765310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Eker OF, Bühlmann M, Dargazanli C, Kaesmacher J, Mourand I, Gralla J, Arquizan C, Fischer UM, Gascou G, Heldner M, et al. Endovascular treatment of atherosclerotic tandem occlusions in anterior circulation stroke: technical aspects and complications compared to isolated intracranial occlusions. Front Neurol. 2018;9:1046. doi: 10.3389/fneur.2018.01046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jacquin G, Poppe AY, Labrie M, Daneault N, Deschaintre Y, Gioia LC, Odier C, Raymond J, Roy D, Weill A, et al. Lack of consensus among stroke experts on the optimal management of patients with acute tandem occlusion. Stroke. 2019;50:1254–1256. doi: 10.1161/STROKEAHA.118.023758 [DOI] [PubMed] [Google Scholar]
- 45. Jacquin G, Labrie M, Daneault N, Deschaintre Y, Gioia L, Odier C, Raymond J, Roy D, Stapf C, Weill A, et al. Management of patients with tandem carotid occlusion undergoing endovascular thrombectomy for anterior circulation stroke: an international survey of stroke physicians. Int J Stroke. 2018;13:123. doi: 10.1161/STROKEAHA.118.023758 [DOI] [Google Scholar]
- 46. Steglich‐Arnholm H, Krieger DW. Carotid stent‐assisted thrombectomy in acute ischemic stroke. Future Cardiol. 2015;11:615–632. doi: 10.2217/fca.15.54 [DOI] [PubMed] [Google Scholar]
- 47. Pop R, Zinchenko I, Quenardelle V, Mihoc D, Manisor M, Richter JS, Severac F, Simu M, Chibbaro S, Rouyer O, et al. Predictors and clinical impact of delayed stent thrombosis after thrombectomy for acute stroke with tandem lesions. AJNR Am J Neuroradiol. 2019;40:533–539. doi: 10.3174/ajnr.A5976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Quispe‐Orozco D, Limaye K, Zevallos CB, Farooqui M, Mendez‐Ruiz A, Ansari S, Dajles A, Samaniego EA, Derdeyn C, Ortega‐Gutierrez S. Safety and efficacy of symptomatic carotid artery stenting performed in an emergency setting. Interv Neuroradiol. 2021;27:411–418. doi: 10.1177/1591019920977552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mendez AA, Quispe‐Orozco D, Dandapat S, Samaniego EA, Tamadonfar E, Zevallos CB, Farooqui M, Derdeyn CP, Ortega‐Gutierrez S. Overestimation of core infarct by computed tomography perfusion in the golden hour. Brain Circ. 2020;6:211–214. doi: 10.4103/bc.bc_7_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zhu F, Labreuche J, Haussen DC, Piotin M, Steglich‐Arnholm H, Taschner C, Papanagiotou P, Lapergue B, Dorn F, Cognard C, et al. Hemorrhagic transformation after thrombectomy for tandem occlusions. Stroke. 2019;50:516–519. doi: 10.1161/STROKEAHA.118.023689 [DOI] [PubMed] [Google Scholar]
- 51. Wilson MP, Murad MH, Krings T, Pereira VM, O'Kelly C, Rempel J, Hilditch CA, Brinjikji W. Management of tandem occlusions in acute ischemic stroke‐intracranial versus extracranial first and extracranial stenting versus angioplasty alone: a systematic review and meta‐analysis. J Neurointerv Surg. 2018;10:721–728. doi: 10.1136/neurintsurg-2017-013707 [DOI] [PubMed] [Google Scholar]
- 52. Sivan‐Hoffmann R, Gory B, Armoiry X, Goyal M, Riva R, Labeyrie PE, Lukaszewicz AC, Lehot JJ, Derex L, Turjman F. Stent‐retriever thrombectomy for acute anterior ischemic stroke with tandem occlusion: a systematic review and meta‐analysis. Eur Radiol. 2017;27:247–254. doi: 10.1007/s00330-016-4338-y [DOI] [PubMed] [Google Scholar]
- 53. Dufort G, Chen BY, Jacquin G, Keezer M, Labrie M, Rioux B, Stapf C, Ziegler D, Poppe AY. Acute carotid stenting in patients undergoing thrombectomy: a systematic review and meta‐analysis. J Neurointerv Surg. 2021;13:141–145. doi: 10.1136/neurintsurg-2020-015817 [DOI] [PubMed] [Google Scholar]
- 54. Haussen D, Turjman F, Piotin M, Labreuche J, Steglich‐Arnholm H, Holtmannspötter M, Taschner C, Eiden S, Nogueira R, Papanagiotou P, et al. Head or neck first? Speed and rates of reperfusion in thrombectomy for tandem large vessel occlusion strokes. Interv Neurol. 2020;8:92–100. doi: 10.1159/000496292 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Tables S1–S3
Figures S1–S5


