Abstract
Background
We investigated associations of childhood abuse with 4 cardiovascular disease risk factors in adulthood, and whether exposure to nurturing and household organization in childhood mitigated these associations.
Methods and Results
The CARDIA (Coronary Artery Risk Development in Young Adults) study (baseline examination, 1985–1986) was used to examine associations of childhood exposures (measured retrospectively at the year 15 examination) with incident obesity, type 2 diabetes, hypertension, and hyperlipidemia (assessed from baseline to year 30). Race‐ and sex‐stratified Cox proportional hazards models were used to examine associations of exposure to childhood abuse with incident cardiovascular disease risk factors. Interaction terms between exposure to abuse and exposure to nurturing relationship and household organization were included to test for effect modifications. Exposure to occasional/frequent abuse (versus no abuse) was associated with incident type 2 diabetes among White men (hazard ratio [HR], 1.81; 95% CI, 1.06–3.08). Exposure to low versus no abuse was associated with incident hyperlipidemia among White men (HR, 1.35; 95% CI, 1.09–1.67) and White women (HR, 1.26; 95% CI, 1.01–1.56). Risks of incident hyperlipidemia were higher for White women who experienced abuse and lived in dysfunctional households (HR, 3.61; 95% CI, 1.62–8.05) or households with low levels of organization (HR, 2.05; 95% CI, 1.25–3.36) compared with White women who experienced abuse but lived in well‐organized households (HR, 0.66; 95% CI, 0.41–1.06). Similar patterns were seen for Black men who lived in dysfunctional households (HR, 3.62; 95% CI, 1.29–10.12) or households with low organization (HR, 2.01; 95% CI, 1.08–3.72).
Conclusions
We identified race‐ and sex‐specific associations of childhood exposures with incident cardiovascular disease risk factors. The associations of household organization and dysfunction with cardiovascular disease risks merits further investigation.
Keywords: childhood, childhood exposures, hyperlipidemia, hypertension, obesity, type 2 diabetes
Subject Categories: Pediatrics, Obesity, Primary Prevention, Race and Ethnicity, Risk Factors
Nonstandard Abbreviations and Acronyms
- ACEs
adverse childhood experiences
- CARDIA
Coronary Artery Risk Development in Young Adults
- T2DM
type 2 diabetes
Clinical Perspective
What Is New?
We found race and sex differences in the associations of childhood abuse with future risk of incident type 2 diabetes, hypertension, and hyperlipidemia.
Among White men, exposure to abuse in childhood was associated with higher risk of incident type 2 diabetes and hyperlipidemia.
Among White women and Black men, higher risk of incident hyperlipidemia associated with exposure to abuse in childhood was attenuated by exposure to well‐organized households.
What Are the Clinical Implications?
Our findings highlight the need to further investigate the differential association of abuse in childhood and cardiometabolic health by race and sex to better understand the early life factors associated with known health disparities in cardiovascular disease.
Identification and better understanding of the factors that mitigate the development of major cardiovascular disease risk factors for children exposed to abuse could inform cardiovascular disease prevention efforts.
Early life experiences can initiate behavioral and cardiometabolic processes that increase the risks for cardiovascular events in adulthood, including myocardial infarction, stroke, and death. 1 , 2 , 3 , 4 , 5 Exposure to childhood physical and psychological abuse is associated with the development of obesity, type 2 diabetes (T2DM), hypertension, and hyperlipidemia. 4 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 In contrast, exposure to nurturing relationships in childhood is associated with optimal self‐reported physical and mental health and lower odds of smoking and depression in adulthood. 16 , 17 Similarly, growing up in a well‐organized household environment during childhood is associated with secure attachment, cognitive functioning, healthier eating behaviors, and lower risk of obesity. 18 , 19 , 20
Findings from a limited number of studies suggest that beyond these direct benefits, exposure to nurturing relationships and well‐organized household environments during childhood may mitigate the negative health effects associated with experiencing different forms of abuse or adversity in childhood. Previous studies among children who experienced abuse or neglect found that exposure to nurturing and responsive relationships (with caregivers or mentors) introduced substantial cognitive improvements and attenuated the toxic effects abuse had on children’s odds of developing resilience, reporting mental distress, and likelihood of smoking in adulthood. 5 , 17 , 21 , 22 Among participants from the CARDIA (Coronary Artery Risk Development in Young Adults) study cohort, a previous study found that exposure to higher warmth and affection during childhood from a parent or other adult (ie, nurturing relationships) was associated with the lowest increase in multiple biomarkers of cardiovascular disease (CVD) among participants who experienced abuse in childhood. 6
Although research is limited, there is evidence showing the associations of childhood exposures with CVD risks vary by race and sex. 23 For example, researchers found parental psychological abuse and parental monitoring were associated with mean carotid intima‐media thickness, a subclinical measurement of atherosclerosis, but only among White men. 23 Parental nurture was associated with lower carotid intima‐media thickness in White men and women. 23 No associations were found between childhood exposures and carotid intima‐media thickness among Black male or female participants. 23 Because of systemic racism, Black and White individuals have different access to adaptive and maladaptive coping resources and strategies. 24 Thus, it can be suggested that race and sex differences in coping options available for children who experienced abuse may lead to divergent mechanisms linking similar childhood exposures with different CVD risk. However, race and sex differences in the influence of exposure to childhood abuse on major CVD risk factors are largely understudied.
In this study, we examined the associations of exposure to abuse in childhood (physical and psychological) with the incidence of 4 major risk factors of CVD: obesity, T2DM, hypertension, and hyperlipidemia, and whether exposure to nurturing relationships and well‐organized households in childhood moderates these associations. In the context of this study, nurturing relationships refer to relationships in which a parent or other adult in the household responds sensitively to meet the needs of the child by making the child feel loved, supported, and cared for, and/or expressing physical affection, as opposed to feeling neglected. Household organization refers to a household that was regarded as organized and well managed, where family members were involved in children’s lives and knew what they were up to. The concept of household organization is contrasted with household dysfunction. Several studies have estimated the cumulative prevalence of abuse, neglect and household dysfunction in childhood, in part because adverse experiences co‐occur among >13% of children. 25 Although this approach is useful, it has been noted that it fails to capture the individual contribution of each type of childhood adversity to future health. 26 As a consequence, less is also known about the co‐occurrence of abuse with nurturing and household organization and whether these positive exposures can limit the vulnerability to chronic disease in adulthood.
This study uses a life course approach and an intersectionality framework to understand how early‐life experiences at the intersection of race and sex shape adult cardiovascular risks. 27 To identify race‐ and sex‐specific lifelong associations, analyses were stratified by race and sex. We hypothesized that (1) exposure to nurturing relationships would mitigate the association of experiencing abuse in childhood with incidence of obesity, T2DM, hypertension, and hyperlipidemia; (2) exposure to well‐organized household environments during childhood would mitigate the association of experiencing abuse in childhood with incidence of obesity, T2DM, hypertension, and hyperlipidemia; and (3) analyses will evidence race and sex differences by showing stronger associations among White men and women, consistent with previous studies. 23
Methods
Study Design and Data Source
This study uses data from the ongoing CARDIA study. In 1985, the CARDIA study longitudinal cohort began following up 5115 Black and White adults to investigate the evolution of coronary heart disease during young adulthood. 28 , 29 Study design and methods have been previously described. 28 , 29 Briefly, from 1985 to 1986, participants aged 18 to 30 years were recruited in 4 urban areas: Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. 28 , 29 Participants were recruited using stratified random sampling procedures to recruit an equal number of participants by race, sex, age subgroup (18–24 years and 25–30 years), and education. Additional in‐person clinical examinations were held after 2, 5, 7, 10, 15, 20, 25, and 30 years; the retention rates across examinations were 91%, 86%, 81%, 79%, 74%, 72%, 72%, and 71%, respectively. As part of the study, childhood environments (ie, exposure to abuse, nurturing, and well‐organized households) were examined retrospectively during the assessment conducted 15 years after the baseline examination (when participants were aged 33–45 years). Incidence of obesity, T2DM, hypertension, and hyperlipidemia outcomes was examined prospectively from baseline. The data used in this study are available from the CARDIA study (https://www.cardia.dopm.uab.edu/) on reasonable request.
For the present study, each outcome was examined separately. Participants were excluded if they did not complete the year 15 examination, or had obesity, T2DM, hypertension, or hyperlipidemia at baseline. Following exclusions, the study sample sizes for the analyses of each respective outcome were as follows: 3208 participants for obesity, 3492 participants for T2DM, 3458 participants for hypertension, and 2973 participants for hyperlipidemia analyses. Institutional review board approval was obtained by each study site, and participants provided informed consent during each examination.
Measurements
During the year 15 visit, participants were asked to respond to the Childhood Family Environments Questionnaire, an instrument derived from the inventory of adverse childhood experiences (ACEs) by Felitti et al. 30 This instrument is distinct from the ACE questionnaire, and was designed to capture different dimensions of CARDIA study respondent’s family and social environment, including exposure to physical or psychological abuse, nurturing or neglectful relationships, and household organization or dysfunction during childhood and adolescence (before the age of 18 years). 6 , 23 Each question is rated on a 4‐point Likert scale, composed of the responses “rarely or none of the time,” “some or little of the time,” “occasionally or moderate amount of time,” and “most or all of the time.”
Table 1 introduces the specific items included in each dimension. To create the dimension of abuse, we first examined the distribution of this exposure, which revealed that prevalence of abuse in childhood was low among CARDIA study participants and the measure was skewed. Thus, responses to the abuse questions were grouped into 3 categories. Category 1 represents “no abuse” (childhood abuse=0) and includes participants who answered they experienced abuse in childhood “rarely or none of the time.” Category 2 represents “low abuse” (childhood abuse>0 and ≤1) and includes participants who answered they experienced abuse “some or little of the time” to either 1 of the 2 questions or to both. Category 3 represents “occasional or frequent abuse” (childhood abuse>1) and includes participants who answered they experienced abuse “occasionally or moderate amount of time” and/or “most or all of the time.” Nurturing and household organization were not skewed, so they were modeled continuously. The dimensions of nurturing and household organization were calculated by averaging the responses to selected questions included in the Childhood Family Environments Questionnaire scale such that scores for each childhood exposure ranged from 0 (indicating “rarely or none of the time”) to 3 (indicating “most or all of the time”). Respectively, the dimension of nurturing ranged from “no nurturing or neglect” (score of 0) and “low nurturing” (score of 1) to “higher nurturing” (scores of 2–3), and the dimension of household organization ranged from “household dysfunction” (score of 0) and “low organization” (score of 1) to “well‐organized households” (scores of 2–3). Previous research conducted among CARDIA study participants has estimated similar subscales with the same selected items from this instrument to examine childhood abuse and nurturing. 6
Table 1.
Questions From the Childhood Family Environment Questionnaire Used at Year 15 (2000–2001) to Assess Childhood Exposure to Abuse, Nurturing, and Household Organization
| Childhood exposure | Score, mean (SD) | Questions |
|---|---|---|
| Abuse | 0.46 (0.66) | How often did a parent or other adult in the household push, grab, shove, or hit you so hard you had marks or were injured? |
| How often did a parent or other adult in the household swear at you, insult you, put you down, or act in a way that made you feel threatened? | ||
| Nurturing | 2.19 (0.83) | How often did a parent or other adult in the household make you feel that you were loved, supported, and cared for? |
| How often did a parent or other adult in the household express physical affection for you, such as hugging or other physical gesture of warmth and affection? | ||
| Household organization | 2.24 (0.81) | Would you say the household you grew up in was well organized and well managed? |
| Did your family know what you were up to? |
Outcomes
Data on CVD risk factors were collected at each examination. Trained examiners collected measurements of height and weight, waist circumference, resting blood pressure, and a venous blood sample for analysis of fasting glucose and lipids, including total cholesterol, low‐density lipoprotein, high‐density lipoprotein, and triglycerides. Obesity was defined as body mass index (BMI) ≥30 kg/m2. 31 T2DM was defined on the basis of the American Diabetes Association criteria as having measurements of fasting serum glucose of ≥126 mg/dL, 2‐hour‐postload serum glucose of ≥200 mg/dL, a hemoglobin A1c of ≥6.5%, or use of antihyperglycemic medications. 32 Hypertension was defined on the basis of the guidelines that were current at the time of data collection. 33 Individuals with systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or taking antihypertensive medications were considered hypertensive. 33 Hyperlipidemia was defined on the basis of serum total cholesterol levels of ≥240 mg/dL, low‐density lipoprotein cholesterol ≥160 mg/dL, triglycerides ≥200 mg/dL, or high‐density lipoprotein cholesterol of ≤40 mg/dL, and/or taking a cholesterol‐lowering medication. 34 , 35
Covariates
At the time of enrollment, participants self‐reported their age, race, sex at birth, years of education for themselves, and average years of education of both parents. Study site and these demographic characteristics were included as covariates. Average parental education was calculated on the basis of the number of years of education for the number of parents reported. These potential confounders were selected on the basis of previous studies documenting that these factors could influence the association of childhood exposures with incidence of obesity, T2DM, hypertension, and hyperlipidemia. 36 , 37 , 38 , 39 , 40 , 41 Although obesity is a major risk factor for hypertension and T2DM, BMI measurements were not assessed in childhood or adolescence, the time period the exposure refers to. Thus, baseline BMI was examined as a covariate only in supplementary analyses (Table S1). Supplemental analyses also include the assessment of the risks for abdominal adiposity, to document cardiometabolic risks that measurements of BMI may not show. Although BMI is the most widely used measurement of weight status, studies suggest that when compared with waist circumference assessment, this measurement of abdominal adiposity is a better predictor of the CVD and mortality. 42 For the purpose of our analyses, abdominal adiposity was defined as having a waist circumference >94 cm for men and >80 cm for women. 42
Statistical Analysis
Participant demographic characteristics were stratified by race, sex, and categories of abuse. Continuous variables were summarized as mean (SD), and category variables were summarized as count (percentage). Participants were considered at risk of developing CVD risk outcomes (obesity, T2DM, hypertension, and hyperlipidemia) from baseline examination until either the follow‐up examination at which CVD risk outcome was identified or censored at the last attended examination. Participants who died or were lost to follow‐up were censored at the next examination. Cox proportional hazards models with discrete failure time were used to estimate adjusted hazard ratios (HRs) and 95% CIs for the associations of exposure to abuse with incidence of (1) obesity, (2) T2DM, (3) hypertension, and (4) hyperlipidemia. Models adjusted for age, race, sex at birth, years of education for themselves, and average years of education for both parents. Additional models were used to test the interactions of abuse with nurturing relationships and abuse with household organization. Interactions between exposure to abuse and exposure to nurturing relationship and between exposure to abuse with household organization were tested for differences in incidences of CVD risk outcomes. All models were stratified by race and sex and adjusted for all study covariates. Proportional hazard assumptions were tested using Kaplan‐Meier curves and log‐log survival plots. On the basis of the patterns of missing covariates for each major CVD risk outcome (Table S2), we assumed the missing covariates to be missing at random. We used multiple imputation by chained equations to impute data for missing covariates. 43 A total of 10 imputed data sets were created. All statistical analyses were done using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Participant Characteristics
The mean age of participants at baseline was 25.08±3.62 years, 56% of participants were women, and 47% of participants were Black. Overall, most participants experienced no abuse (56%) and were exposed to high levels of nurture (2.19±0.83) and household organization (2.24±0.81) during childhood. Baseline characteristics, stratified by race and sex, are presented by categories of abuse in Table 2.
Table 2.
Baseline Characteristics of White CARDIA Study Participants by Sex, and Categories of Exposure to Abuse in Childhood
| Demographic characteristics | White race | |||||
|---|---|---|---|---|---|---|
| White men | White women | |||||
| No abuse | Low abuse | Occasional/frequent abuse | No abuse | Low abuse | Occasional/frequent abuse | |
| (n=541) | (n=271) | (n=94) | (n=553) | (n=322) | (n=147) | |
| Age, y | 25.61±3.29 | 25.47±3.32 | 25.70±3.45 | 25.54±3.44 | 25.65±3.47 | 25.71±3.22 |
| Study center | ||||||
| Oakland, CA | 106 (19.59) | 55 (20.30) | 24 (25.53) | 147 (26.58) | 95 (29.50) | 46 (31.29) |
| Birmingham, AL | 129 (23.84) | 54 (19.93) | 14 (14.89) | 112 (20.25) | 47 (14.60) | 19 (12.93) |
| Chicago, IL | 133 (24.58) | 64 (23.62) | 24 (25.53) | 123 (22.24) | 72 (22.36) | 29 (19.73) |
| Minneapolis, MN | 173 (31.98) | 98 (36.16) | 32 (34.04) | 171 (30.92) | 108 (33.54) | 53 (36.05) |
| Participant’s years of education | 15.08±0.10 | 14.51±0.15 | 13.73±0.26 | 15.00±0.09 | 14.47±0.12 | 14.25±0.19 |
| Parental years of education | 14.32±0.12 | 13.63±0.17 | 13.36±0.31 | 14.12±0.12 | 13.52±0.17 | 13.27±0.24 |
| Clinical characteristics | ||||||
| Body mass index, kg/m2 | 24.35±0.14 | 24.39±0.22 | 24.34±0.41 | 22.88±0.18 | 23.34±0.25 | 23.42±0.37 |
| Blood pressure, mm Hg | ||||||
| Diastolic | 71.17±9.23 | 70.15±9.68 | 70.95±9.80 | 66.72±8.33 | 65.57±7.70 | 66.80±8.37 |
| Systolic | 114.46±9.79 | 114.37±11.18 | 114.22±11.48 | 105.07±9.21 | 104.20±8.90 | 105.45±8.90 |
| Glucose | ||||||
| Fasting glucose, mg/dL | 84.42±0.45 | 85.44±0.61 | 84.05±0.77 | 80.67±0.33 | 81.55±0.83 | 80.82±0.60 |
| Lipids, mg/dL | ||||||
| Total cholesterol | 176.36±1.38 | 179.05±2.18 | 175.74±3.29 | 174.94±1.30 | 178.07±1.82 | 173.59±2.42 |
| HDL cholesterol | 47.17±0.45 | 47.57±0.74 | 47.17±1.17 | 56.26±0.52 | 56.00±0.76 | 57.03±1.03 |
| LDL cholesterol | 111.56±1.31 | 113.92±1.95 | 110.46±3.02 | 104.80±1.19 | 108.36±1.68 | 102.84±2.33 |
| Triglycerides | 88.10±2.99 | 87.88±3.77 | 90.69±7.85 | 69.55±1.57 | 68.61±1.98 | 68.45±2.74 |
| Childhood experiences | ||||||
| Abuse | 0.00±0.00 | 0.68±0.24 | 1.77±0.40 | 0.00±0.00 | 0.74±0.25 | 1.95±0.50 |
| Nurturing relationships | 2.45±0.62 | 2.03±0.76 | 1.46±0.87 | 2.51±0.64 | 1.88±0.89 | 1.32±0.98 |
| Household organization | 2.50±0.63 | 2.11±0.77 | 1.56±0.84 | 2.60±0.58 | 2.05±0.87 | 1.55±0.93 |
| Baseline Characteristics of Black CARDIA Study Participants by Sex, and Categories of Exposure to Abuse in Childhood | ||||||
|---|---|---|---|---|---|---|
| Demographic characteristics | Black race | |||||
| Black men | Black women | |||||
| No abuse | Low abuse | Occasional/frequent abuse | No abuse | Low abuse | Occasional/frequent abuse | |
| (n=377) | (n=255) | (n=74) | (n=568) | (n=300) | (n=140) | |
| Age, y | 24.38±3.65 | 24.43±3.76 | 24.83±3.89 | 24.37±3.86 | 24.74±3.71 | 24.83±4.23 |
| Study center | ||||||
| Oakland, CA | 96 (25.46) | 68 (26.67) | 24 (32.43) | 184 (32.39) | 102 (34.00) | 48 (34.29) |
| Birmingham, AL | 121 (32.10) | 75 (29.41) | 12 (16.22) | 167 (29.40) | 68 (22.67) | 31 (22.14) |
| Chicago, IL | 73 (19.36) | 55 (21.57) | 18 (24.32) | 114 (20.07) | 69 (23.00) | 38 (27.14) |
| Minneapolis, MN | 87 (23.08) | 57 (22.35) | 20 (27.03) | 103 (18.13) | 61 (20.33) | 23 (16.43) |
| Participant’s years of education | 13.21±0.10 | 12.91±0.12 | 12.91±0.22 | 13.32±0.07 | 13.04±0.10 | 12.99±0.17 |
| Parental years of education | 12.10±0.14 | 12.10±0.15 | 12.05±0.31 | 12.05±0.11 | 11.67±0.16 | 11.49±0.22 |
| Clinical characteristics | ||||||
| Body mass index, kg/m2 | 24.76±0.23 | 24.37±0.25 | 25.60±0.61 | 25.52±0.27 | 26.42±0.37 | 27.04±0.58 |
| Blood pressure, mm Hg | ||||||
| Diastolic | 70.63±10.21 | 71.11±10.84 | 70.45±11.61 | 67.63±8.81 | 67.67±9.27 | 67.39±11.59 |
| Systolic | 115.60±10.18 | 115.96±10.57 | 116.00±11.80 | 108.45±9.73 | 108.27±10.20 | 109.04±10.39 |
| Glucose | ||||||
| Fasting glucose, mg/dL | 84.08±1.10 | 84.11±0.82 | 83.41±0.85 | 79.70±0.41 | 80.82±0.82 | 79.45±0.74 |
| Lipids, mg/dL | ||||||
| Total cholesterol | 177.69±1.84 | 175.97±2.16 | 181.07±4.10 | 179.76±1.41 | 177.05±1.92 | 183.10±2.56 |
| HDL cholesterol | 53.23±0.66 | 54.07±0.88 | 54.47±1.70 | 56.17±0.54 | 54.97±0.71 | 53.74±1.12 |
| LDL cholesterol | 110.19±1.75 | 108.16±2.04 | 113.26±3.65 | 111.22±1.32 | 108.98±1.82 | 116.20±2.52 |
| Triglycerides | 71.38±2.22 | 68.63±2.29 | 66.81±4.33 | 61.91±1.32 | 65.47±2.12 | 65.50±2.61 |
| Childhood experiences | ||||||
| Abuse | 0.00±0.00 | 0.71±0.25 | 1.82±0.42 | 0.00±0.00 | 0.73±0.25 | 1.95±0.53 |
| Nurturing relationships | 2.39±0.72 | 2.12±0.79 | 1.83±0.90 | 2.46±0.71 | 2.03±0.84 | 1.51±0.98 |
| Household organization | 2.31±0.76 | 1.96±0.83 | 1.78±0.89 | 2.45±0.69 | 2.09±0.84 | 1.71±0.97 |
Data are given as mean±SD or number (percentage). CARDIA indicates Coronary Artery Risk Development in Young Adults; HDL, high‐density lipoprotein; and LDL, low‐density lipoprotein.
Obesity
Over a median follow‐up of 25.49 years, there were a total of 1419 participants who developed obesity (200.72 per 10 000 years). Multivariate adjusted HR and 95% CI of the associations of abuse in childhood with incident obesity, stratified by race and sex, are presented in Table 3. After adjustments for age, study site, participants’ years of education, and average years of parental education, having experienced abuse in childhood was not associated with an increased risk of developing obesity. Childhood exposure to nurturing relationships and household organization did not modify the null associations of abuse with incidence of obesity. Furthermore, the obesity risks associated with exposure to abuse in childhood did not vary when examined with measurement of abdominal obesity (Table S1).
Table 3.
Multivariate Adjusted HRs and 95% CIs of CVD Risk Factors Associated With Exposure to Abuse in Childhood, by Race and Sex
| White race † | Black race † | |||
|---|---|---|---|---|
| Variable | White men | White women | Black men | Black women |
| Obesity* | ||||
| No abuse | Reference | Reference | Reference | Reference |
| Low abuse | 1.14 (0.90–1.45) | 1.06 (0.82–1.37) | 1.12 (0.87–1.43) | 1.14 (0.94–1.40) |
| Occasional/frequent abuse | 1.02 (0.70–1.48) | 1.02 (0.73–1.42) | 0.94 (0.61–1.44) | 1.03 (0.78–1.36) |
| Type 2 diabetes* | ||||
| No abuse | Reference | Reference | Reference | Reference |
| Low abuse | 0.92 (0.58–1.45) | 0.88 (0.56–1.39) | 1.11 (0.76–1.61) | 1.09 (0.80–1.49) |
| Occasional/frequent abuse | 1.81 (1.06–3.08) | 0.91 (0.51–1.62) | 1.14 (0.64–2.03) | 1.22 (0.83–1.80) |
| Hypertension* | ||||
| No abuse | Reference | Reference | Reference | Reference |
| Low abuse | 0.90 (0.69–1.17) | 0.87 (0.65–1.17) | 1.23 (0.99–1.53) | 1.03 (0.85–1.25) |
| Occasional/frequent abuse | 1.00 (0.68–1.47) | 1.00 (0.70–1.43) | 0.88 (0.60–1.29) | 1.09 (0.85–1.40) |
| Hyperlipidemia* | ||||
| No abuse | Reference | Reference | Reference | Reference |
| Low abuse | 1.35 (1.09–1.67) | 1.26 (1.01–1.56) | 1.09 (0.87–1.37) | 0.87 (0.69–1.10) |
| Occasional/frequent abuse | 1.21 (0.89–1.66) | 0.91 (0.68–1.22) | 0.91 (0.62–1.32) | 1.02 (0.75–1.37) |
Data are given as HR (95% CI). CVD indicates cardiovascular disease; and HR, hazard ratio.
Incident obesity events examined from baseline (year 0 [1985–1986]) to year 30 (2015–2016).
Models adjusted for age, study site, participant’s years of education, and average parental years of education at baseline.
Type 2 Diabetes
There were 539 T2DM cases over 29.80 median follow‐up years (57.46 per 10 000 years). Analyses of the associations of abuse in childhood with incident T2DM are presented in Table 3. Among White men, exposure to occasional/frequent abuse in childhood was associated with higher risk of incident T2DM (HR, 1.81; 95% CI, 1.06–3.08) than no abuse exposure in childhood. Among White women and Black men and women, exposure to abuse in childhood did not associate with incident T2DM. Nurturing relationships and household organization in childhood did not modify the association of abuse with incidence of TD2M among CARDIA study participants.
Hypertension
Over 29.47 median follow‐up years, 1452 people developed hypertension (167.96 per 10 000 years). Exposure to abuse in childhood was not significantly associated with incident hypertension (Table 3). Nurturing relationships and household organization in childhood did not modify these associations of abuse with incidence of hypertension among CARDIA study participants.
Hyperlipidemia
During 20.67 median follow‐up years, 1570 people developed hyperlipidemia (276.02 per 10 000 years). Table 3 introduces the adjusted multivariable Cox models that examine the associations of childhood experiences with incident hyperlipidemia. When compared with no abuse in childhood, exposure to low abuse was associated with higher risk of incident hyperlipidemia among White men (HR, 1.35; 95% CI, 1.09–1.67) and White women (HR, 1.26; 95% CI, 1.01–1.56). The association of exposure to childhood abuse with incident hyperlipidemia was not significant for Black men and women. Among White women, there was a significant interaction between exposure to abuse and household organization (P=0.008). Figure 1 shows that experiencing occasional/frequent abuse in childhood associated with higher risk of incident hyperlipidemia among White women who grew up in households rated as dysfunctional (score of 0; HR, 3.60; 95% CI, 1.62–8.02), or with low organization (score of 1; HR, 2.04; 95% CI, 1.24–3.35), but not among White women who grew up in more organized (score of 2; HR, 1.16; 95% CI, 0.88–1.61) or well‐organized households (score of 3; HR, 0.66; 95% CI, 0.41–1.06).
Figure 1. Risk of incident hyperlipidemia associated with the exposure to occasional/frequent abuse across different levels of household organization among White women.
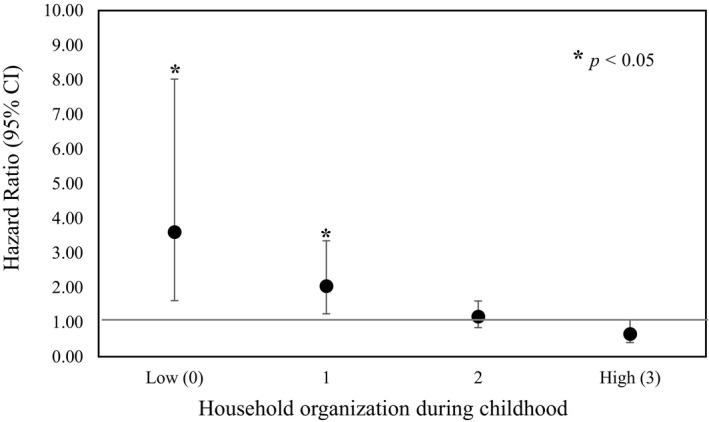
Effect that exposure to occasional/frequent abuse during childhood has on incident hyperlipidemia by different levels of exposure to household organization in childhood among White women. Hyperlipidemia events were examined from baseline (year 0 [1985–1986]) to year 30 (2015–2016). Models adjusted for age, study site, participant’s years of education, and average parental years of education at baseline.
Among Black men, there was a similar interaction between exposure to abuse and household organization (P=0.037). Figure 2 shows that when compared with Black men who grew up in organized households (HR, 0.62; 95% CI, 0.34–1.11), risk of incident hyperlipidemia was higher for Black men who experienced occasional/frequent abuse in childhood and grew up in dysfunctional households (score of 0; HR, 3.62; 95% CI, 1.29–10.12) or households with low organization (score of 1; HR, 2.01; 95% CI, 1.08–3.72). Childhood abuse was not associated with risks of developing hyperlipidemia among Black female participants, and exposures to nurturing relationships or household organization did not modify these null associations of abuse with incident hyperlipidemia.
Figure 2. Risk of incident hyperlipidemia associated with the exposure to occasional/frequent abuse across different levels of household organization among Black men.
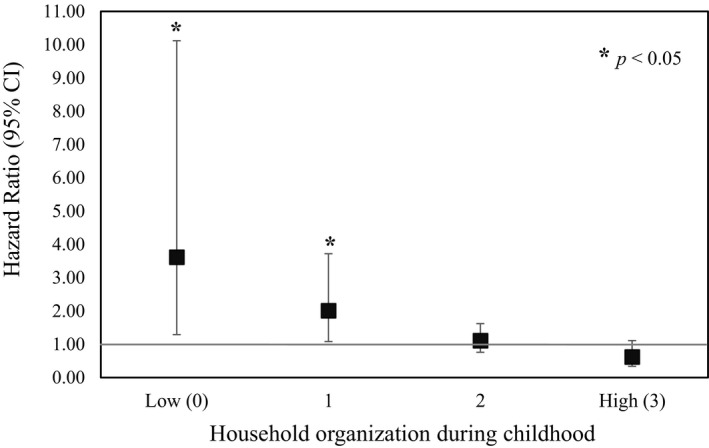
Figure shows the effect that exposure to occasional/frequent abuse during childhood has on incident hyperlipidemia by different levels of exposure to household organization in childhood among Black men. Hyperlipidemia events were examined from baseline (year 0 [1985–1986]) to year 30 (2015–2016). Models adjusted for age, study site, participant’s years of education, and average parental years of education at baseline.
Discussion
We found that, among CARDIA study participants, the risks of developing T2DM and hyperlipidemia associated with experiencing abuse in childhood varied by race and sex. White men who experienced occasional/frequent abuse in childhood had higher risks of developing T2DM than White men who experienced no abuse. Higher risks for hyperlipidemia were associated with exposure to low abuse among White men and women. However, when compared with same sex and race participants who experienced abuse in childhood, interaction tests show that among White women, higher risks of incident hyperlipidemia were attenuated if they grew up in well‐organized households. Similarly, for Black men who experienced occasional/frequent abuse, risks of incident hyperlipidemia were attenuated if they grew up in well‐organized households. White men and women did not exhibit stronger associations with exposure to abuse, nurturing relationships, or household organizations, as originally hypothesized. Exposure to higher levels of household organization during childhood mitigated the association of childhood abuse with hyperlipidemia, but not other major CVD risk factors in adulthood.
Findings suggest that the pathways linking childhood experiences with CVD events and all‐cause mortality in adulthood differ by race, sex, and level of household organization or dysfunction in childhood. Among CARDIA study participants, exposure to adverse childhood family environments has been associated with higher risk of carotid intima‐media thickness, myocardial infarction, stroke, all CVD events, and all‐cause mortality in adulthood. 23 , 44 , 45 , 46 Several psychosocial (eg, depressive symptoms, anger expressions, and socioeconomic position) and behavioral factors (eg, smoking) have been identified as mediators in these associations of childhood exposures with adult cardiometabolic problems. 23 , 46 For example, a previous study among CARDIA study participants found that adverse family environments were associated with less adaptive psychosocial functioning. 45 Psychosocial functioning was, in turn, associated with elevated CRP (C‐reactive protein). 45 The associations of CRP with T2DM, hypertension, and lipids, particularly with low‐density lipoprotein cholesterol, have been previously recognized. 47 , 48 , 49 , 50 A different study among CARDIA study participants showed that childhood abuse was associated with chronic inflammation. 6 Chronic inflammation can be induced by persistent stress, and can trigger a variety of alterations in lipid metabolisms, such as decreases in high‐density lipoprotein and increases in low‐density lipoprotein and triglycerides. These pathways may explain the increased risk of incident hyperlipidemia among White men and women, and Black men who experienced frequent abuse. 47 , 51
Miller and colleagues proposed 3 mechanisms through which adversity in early life influences the development of cardiometabolic disease in adulthood. According to their Biological Embedding Model, epigenetic markings, posttranslational modifications, and tissue remodeling combine to explain how adversity experienced in early childhood “gets under the skin,” incubates during decades, and manifests through cardiometabolic diseases in adulthood. 52 Others have shown that the stress from experiencing physical or psychological abuse in early life can trigger mitochondrial dysfunction and increased vascular reactive oxygen species production. 53 Miller and colleagues advance this and propose that stress particularly affects the proinflammatory phenotype of the monocyte/macrophage lineage, triggering excessive inflammatory responses and the resistance to hormonal anti‐inflammatory signals. 52 Beyond these molecular and biological processes, the adoption of unhealthy behaviors, such as smoking or excessive drinking, also associated with experiencing abuse in childhood, will contribute to exacerbate the chronic inflammatory state. 52 Over time, chronic inflammation will promote the development of high blood pressure, insulin resistance, and plaque growth. 52 In the context of this study, it is likely that the abuse experienced in childhood contributes to the development of T2DM among White men, and hyperlipidemia among White men and women, and Black men. Furthermore, although the model does not address the role of nurturing, authors acknowledge that maternal nurturance may offset some of the hormonal, metabolic, inflammatory, and cardiovascular risks associated with childhood adversity. 52 Lower inflammatory responses have been documented among participants in the CARDIA study who experienced higher levels of nurturing in childhood. 6
Beyond the associations of exposures to physical or psychological abuse in childhood with CVD risk factors in adulthood, our results advance the literature by showing that exposure to well‐organized households may attenuate CVD risks. Previous studies have shown that exposure to abuse and household dysfunction in childhood is associated with chronic inflammation. 6 In a recent review, authors found that exposure to household dysfunction in childhood was associated with elevated cortisol, and higher prevalence of obesity and psychosocial stress. 54 However, the mechanisms through which protective exposures attenuate CVD risks are less understood. Exposure to physical or psychological abuse in childhood can affect cardiometabolic health through behavioral, mental health, and biological mechanisms. 4 Drawing from the literature of psychosocial factors and chronic diseases, it can be suggested that the associations of childhood environments with major cardiovascular risk factors followed divergent mechanisms. Divergent pathways may have been facilitated by childhood exposures to household organization and social implications of race and sex differences. For example, researchers have proposed that as a consequence of the barriers of access to mental health care, Black individuals may be more likely than White individuals to rely on negative behavioral coping strategies (eg, smoking or binge drinking or eating) associated with lower psychological damage, but higher cardiometabolic harm. 55 These differences are introduced to explain why, when compared with White participants, Black participants have higher prevalence of chronic medical conditions but lower than expected prevalence of depression. 55
Sex differences in coping strategies have been previously identified. A study found that when compared with men, women reported depressive symptoms more frequently and were more likely to use emotional support and positive reframing as coping mechanisms. 56 Higher levels of positive reframing were, in turn, associated with lower depression scores among women, but not among men. 56 In the current study, race and sex differences in coping strategies may explain why household organization was associated with lower risks for hyperlipidemia among White women and Black men who experienced abuse. However, the lack of information on the temporality and source of abuse or dysfunction experienced in childhood or adolescence precludes us from further investigating any behavioral pathways. A better understanding of the resilience‐promoting mechanisms implemented by White women and Black men who grew up in more organized households could inform future CVD prevention efforts.
It is important to consider the associations identified could be attributed to limited statistical power and the lower prevalence of abuse in childhood among CARDIA study participants rather than any differences in biological, behavioral, or psychological responses to childhood experiences. In the landmark ACE study among 17 337 adults, Felitti et al found that >50% of participants had at least one adverse experience in childhood. 30 Participants who had ≥4 ACEs had higher odds of T2DM, stroke, and ischemic heart disease than participants who had no ACEs. 30 , 57 When compared with the study by Felitti et al, in our study, occasional/frequent abuse was experienced by about 30% of participants. However, the lower prevalence may be explained because we limited our examination to physical and psychological abuse in childhood. Instead, Felitti et al explored 10 categories of abuse and dysfunction. 30 Similar prevalence of abuse in childhood has been reported in previous studies. In a prospective study of 972 participants from New Zealand followed up from age 3 to 32 years, researchers found that one potential category of abuse was experienced by 27% of children and 9% experienced ≥2 indicators of abuse. 58 Findings from this study demonstrated that exposure to ≥1 categories of abuse was not associated with more cardiovascular risk factors. 58 In a sample of 2510 German adults, Clemens et al found that 30% of participants experienced child maltreatment. 59 In this retrospective cross‐sectional study, participants who experienced child maltreatment had increased odds of having obesity, diabetes, hypertension, and myocardial infraction. 59 Additional studies have also found exposure to childhood abuse is associated with cardiometabolic outcomes. 4 , 7 However, findings from a meta‐analysis suggest the associations of abuse in childhood with obesity and T2DM are overall weak or modest. 7 On the basis of our findings, it can be suggested that these modest findings could be driven by race and sex differences in the associations or in the coping mechanisms adopted. Research is needed to better understand the mediating factors that may explain race and sex disparities in the associations of abuse in childhood with CVD risk factors in adulthood, particularly among diverse children. The lack of research that examines the contribution from unique social and historical positions to CVD risks is an important gap in the literature.
The findings of this study should be interpreted within the context of its limitations. The relatively small size of the associations caution against overinterpretation of the study findings. Data on childhood family environments were collected retrospectively among participants who were aged 33 to 45 years. As a result, the true magnitude of the exposures could be underestimated because of recall bias or the sensitivity of the questions. To the extent that respondents did not recall or chose not to reveal childhood abuse, the power to detect significant associations may have been reduced or the strength of our findings may have been underestimated. In addition, as shown in the supplementary analyses of T2DM and hypertension, we were only able to adjust for BMI measured at baseline, rather than during childhood or adolescence. This limits our ability to determine the extent to which BMI was a confounder or a potential mediator of these associations. Furthermore, although we adjusted our analyses by including variables related to childhood exposures associated with cardiovascular risks, we cannot exclude the possibility of residual confounding. It is important to recognize that the source and timing of abuse, nurture, and household organization or dysfunction were not identified in the CARDIA study cohort. These preclude our ability to investigate how the source or temporality could have influenced our study findings. In addition, data on coping strategies adopted following the exposure to abuse in childhood were not collected as part of the CARDIA study. We are not able to evaluate the different coping mechanisms adopted and their cardiometabolic consequences. Future epidemiological prospective studies should investigate the long‐term consequences to cardiovascular health associated with different sources of physical or psychological abuse, nurturing, and household organization or dysfunction in childhood and how these associations differ by race and sex in samples of diverse children.
In conclusion, this study demonstrated that among CARDIA study participants, the association of exposure to abuse in childhood with risks of incident T2DM and hyperlipidemia differs by race and sex. Significant interactions suggested that for White women and Black men, risks of hyperlipidemia were attenuated by exposure to well‐organized households. Together, these findings demonstrate childhood negative and positive experiences have long‐term consequences for adult cardiovascular health and may explain key disparities by race and sex in CVD risks. Further research is needed to better understand the mechanisms that drive the race‐ and sex‐specific associations identified.
Sources of Funding
The CARDIA (Coronary Artery Risk Development in Young Adults) study is conducted and supported by the National Heart, Lung, and Blood Institute in collaboration with the University of Alabama at Birmingham (HHSN268201800005I and HHSN268 201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). Dr Aguayo was supported by the American Heart Association during the completion of this project (17SFRN33660752) and is currently supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01 115937‐03S2). Dr Aguayo’s work was assisted in part by a grant from the National Institutes of Health–funded Emory Specialized Center of Research Excellence in Sex Differences (U54AG062334). Dr Heard‐Garris is currently supported by the National Heart, Lung, and Blood Institute (K01 HL147995‐01).
Disclosures
None.
Supporting information
Table S1–S2
For Sources of Funding and Disclosures, see page 11.
References
- 1. Umer A, Kelley GA, Cottrell LE, Giacobbi P Jr, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta‐analysis. BMC Public Health. 2017;17:683. doi: 10.1186/s12889-017-4691-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ohlsson C, Bygdell M, Sondén A, Jern C, Rosengren A, Kindblom JM. BMI increase through puberty and adolescence is associated with risk of adult stroke. Neurology. 2017;89:363. doi: 10.1212/WNL.0000000000004158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Heshmati A, Chaparro MP, Goodman A, Koupil I. Early life characteristics, social mobility during childhood and risk of stroke in later life: findings from a Swedish cohort. Scand J Public Health. 2017;45:419–427. doi: 10.1177/1403494817696600 [DOI] [PubMed] [Google Scholar]
- 4. Suglia SF, Koenen KC, Boynton‐Jarrett R, Chan PS, Clark CJ, Danese A, Faith MS, Goldstein BI, Hayman LL, Isasi CR, et al. Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation. 2018;137:e15–e28. doi: 10.1161/CIR.0000000000000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Srivastav A, Strompolis M, Kipp C, Richard CL, Thrasher JF. Moderating the effects of adverse childhood experiences to address inequities in tobacco‐related risk behaviors. Health Promot Pract. 2020;21:139S–147S. doi: 10.1177/1524839919882383 [DOI] [PubMed] [Google Scholar]
- 6. Carroll JE, Gruenewald TL, Taylor SE, Janicki‐Deverts D, Matthews KA, Seeman TE. Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proc Natl Acad Sci. 2013;110:17149–17153. doi: 10.1073/pnas.1315458110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The effect of multiple adverse childhood experiences on health: a systematic review and meta‐analysis. Lancet Public Health. 2017;2:e356–e366. doi: 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- 8. Smith L, Jacob L, Grabovac I, López‐Sánchez GF, Yang L, Carvalho AF, Shin JI, Sigman A, Zou L, Koyanagi A. Violence and obesogenic behavior among adolescents aged 12–15 years from 62 countries: a global perspective. Prev Med. 2020;137:106123. doi: 10.1016/j.ypmed.2020.106123 [DOI] [PubMed] [Google Scholar]
- 9. Komulainen K, Mittleman MA, Ruohonen S, Laitinen TT, Pahkala K, Elovainio M, Tammelin T, Kähönen M, Juonala M, Keltikangas‐Järvinen L, et al. Childhood psychosocial environment and adult cardiac health: a causal mediation approach. Am J Prev Med. 2019;57:e195–e202. doi: 10.1016/j.amepre.2019.08.018 [DOI] [PubMed] [Google Scholar]
- 10. Boynton‐Jarrett R, Rosenberg L, Palmer JR, Boggs DA, Wise LA. Child and adolescent abuse in relation to obesity in adulthood: the Black Women’s Health Study. Pediatrics. 2012;130:245–253. doi: 10.1542/peds.2011-1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high‐income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- 12. Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121:e1240–e1249. doi: 10.1542/peds.2007-2403 [DOI] [PubMed] [Google Scholar]
- 13. Johnson JG, Cohen P, Kasen S, Brook JS. Childhood adversities associated with risk for eating disorders or weight problems during adolescence or early adulthood. Am J Psychiatry. 2002;159:394–400. doi: 10.1176/appi.ajp.159.3.394 [DOI] [PubMed] [Google Scholar]
- 14. Lissau I, Sørensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343:324–327. doi: 10.1016/S0140-6736(94)91163-0 [DOI] [PubMed] [Google Scholar]
- 15. Riley EH, Wright RJ, Jun HJ, Hibert EN, Rich‐Edwards JW. Hypertension in adult survivors of child abuse: observations from the Nurses' Health Study II. J Epidemiol Community Health. 2010;64:413–418. doi: 10.1136/jech.2009.095109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: associations across adverse childhood experiences levels. JAMA Pediatr. 2019;173:e193007. doi: 10.1001/jamapediatrics.2019.3007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Crouch E, Radcliff E, Strompolis M, Srivastav A. Safe, stable, and nurtured: protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs). J Child Adolesc Trauma. 2018;12:165–173. doi: 10.1007/s40653-018-0217-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bates CR, Bohnert AM, Buscemi J, Vandell DL, Lee KTH, Bryant FB. Family entropy: understanding the organization of the family home environment and impact on child health behaviors and weight. Transl Behav Med. 2019;9:413–421. doi: 10.1093/tbm/ibz042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bates CR, Buscemi J, Nicholson LM, Cory M, Jagpal A, Bohnert AM. Links between the organization of the family home environment and child obesity: a systematic review. Obes Rev. 2018;19:716–727. doi: 10.1111/obr.12662 [DOI] [PubMed] [Google Scholar]
- 20. Saltzman JA, Bost KK, McBride BA, Fiese BH. Household chaos, maternal emotional responsiveness, and child eating behavior: a moderation analysis. J Dev Behav. 2019;40:622–632. doi: 10.1097/DBP.0000000000000701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nelson CA, Zeanah CH, Fox NA, Marshall PJ, Smyke AT, Guthrie D. Cognitive recovery in socially deprived young children: the Bucharest early intervention project. Science. 2007;318:1937–1940. doi: 10.1126/science.1143921 [DOI] [PubMed] [Google Scholar]
- 22. Heard‐Garris N, Davis MM, Szilagyi M, Kan K. Childhood adversity and parent perceptions of child resilience. BMC Pediatr. 2018;18:204. doi: 10.1186/s12887-018-1170-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Loucks EB, Taylor SE, Polak JF, Wilhelm A, Kalra P, Matthews KA. Childhood family psychosocial environment and carotid intima media thickness: the CARDIA study. Soc Sci Med. 2014;104:15–22. doi: 10.1016/j.socscimed.2013.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Beatty Moody DL, Leibel DK, Pantesco EJ, Wendell CR, Waldstein SR, Evans MK, Zonderman AB. Interactive relations across dimensions of interpersonal‐level discrimination and depressive symptoms to carotid intimal‐medial thickening in African Americans. Psychosom Med. 2020;82:234–246. doi: 10.1097/PSY.0000000000000765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Giano Z, Wheeler DL, Hubach RD. The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health. 2020;20:1327. doi: 10.1186/s12889-020-09411-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Negriff S. ACEs are not equal: examining the relative impact of household dysfunction versus childhood maltreatment on mental health in adolescence. Soc Sci Med. 2020;245:112696. doi: 10.1016/j.socscimed.2019.112696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- 28. Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. doi: 10.1016/0895-4356(88)90080-7 [DOI] [PubMed] [Google Scholar]
- 29. Hughes GH, Cutter G, Donahue R, Friedman GD, Hulley S, Hunkeler E, Jacobs DR, Liu K, Orden S, Pirie P, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (CARDIA) Study. Control Clin Trials. 1987;8:68s–73s. doi: 10.1016/0197-2456(87)90008-0 [DOI] [PubMed] [Google Scholar]
- 30. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 31. Centers for Disease Control and Prevention . Defining adult overweight and obesity. 2020; https://www.cdc.gov/obesity/adult/defining.html
- 32. American Diabetes Association . 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43(suppl 1):S14–S31. [DOI] [PubMed] [Google Scholar]
- 33. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 34. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults . Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486 [DOI] [PubMed] [Google Scholar]
- 35. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) . Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 36. Sniderman AD, Furberg CD. Age as a modifiable risk factor for cardiovascular disease. Lancet. 2008;371:1547–1549. doi: 10.1016/S0140-6736(08)60313-X [DOI] [PubMed] [Google Scholar]
- 37. Barrett‐Connor E. Sex differences in coronary heart disease. Circulation. 1997;95:252–264. doi: 10.1161/01.CIR.95.1.252 [DOI] [PubMed] [Google Scholar]
- 38. Kaplan RM, Howard VJ, Manly J, Howard G. Comparison of simple efficient clinical and self‐reported predictors of mortality in a national United States cohort. J Epidemiol Res. 2017;3:23. doi: 10.5430/jer.v3n2p23 [DOI] [Google Scholar]
- 39. Panagiotakos DB, Pitsavos CE, Chrysohoou CA, Skoumas J, Toutouza M, Belegrinos D, Toutouzas PK, Stefanadis C. The association between educational status and risk factors related to cardiovascular disease in healthy individuals: the ATTICA study. Ann Epidemiol. 2004;14:188–194. doi: 10.1016/S1047-2797(03)00117-0 [DOI] [PubMed] [Google Scholar]
- 40. Gebreab SY, Diez Roux AV, Brenner AB, Hickson DA, Sims M, Subramanyam M, Griswold ME, Wyatt SB, James SA. The impact of lifecourse socioeconomic position on cardiovascular disease events in African Americans: the Jackson Heart Study. J Am Heart Assoc. 2015;4:e001553. doi: 10.1161/JAHA.114.001553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Aff. 2008;27:350–360. doi: 10.1377/hlthaff.27.2.350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nalini M, Sharafkhah M, Poustchi H, Sepanlou SG, Pourshams A, Radmard AR, Khoshnia M, Gharavi A, Dawsey SM, Abnet CC, et al. Comparing anthropometric indicators of visceral and general adiposity as determinants of overall and cardiovascular mortality. Arch Iran Med. 2019;1:301–309. [PMC free article] [PubMed] [Google Scholar]
- 43. Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. Br Med J. 2009;339:b2393. doi: 10.1136/bmj.b2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pierce JB, Kershaw KN, Kiefe CI, Jacobs DR Jr, Sidney S, Merkin SS, Feinglass J. Association of childhood psychosocial environment with 30‐year cardiovascular disease incidence and mortality in middle age. J Am Heart Assoc. 2020;9:e015326. doi: 10.1161/JAHA.119.015326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Taylor SE, Lehman BJ, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to adult C‐reactive protein in the coronary artery risk development in young adults study. Biol Psychiatry. 2006;60:819–824. doi: 10.1016/j.biopsych.2006.03.016 [DOI] [PubMed] [Google Scholar]
- 46. Loucks EB, Almeida ND, Taylor SE, Matthews KA. Childhood family psychosocial environment and coronary heart disease risk. Psychosom Med. 2011;73:563–571. doi: 10.1097/PSY.0b013e318228c820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lin G‐M, Liu K, Colangelo LA, Lakoski SG, Tracy RP, Greenland P. Low‐density lipoprotein cholesterol concentrations and association of high‐sensitivity C‐reactive protein concentrations with incident coronary heart disease in the multi‐ethnic study of atherosclerosis. Am J Epidemiol. 2016;183:46–52. doi: 10.1093/aje/kwv144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Veeranna V, Zalawadiya SK, Niraj A, Kumar A, Ference B, Afonso L. Association of novel biomarkers with future cardiovascular events is influenced by ethnicity: results from a multi‐ethnic cohort. Int J Cardiol. 2013;166:487–493. doi: 10.1016/j.ijcard.2011.11.034 [DOI] [PubMed] [Google Scholar]
- 49. Bertoni AG, Burke GL, Owusu JA, Carnethon MR, Vaidya D, Barr RG, Jenny NS, Ouyang P, Rotter JI. Inflammation and the incidence of type 2 diabetes: the Multi‐Ethnic Study of Atherosclerosis (MESA). Diabetes Care. 2010;33:804–810. doi: 10.2337/dc09-1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dauphinot V, Roche F, Kossovsky MP, Schott AM, Pichot V, Gaspoz JM, Gosse P, Barthelemy JC. C‐reactive protein implications in new‐onset hypertension in a healthy population initially aged 65 years: the Proof study. J Hypertens. 2009;27:736–743. doi: 10.1097/HJH.0b013e328326f801 [DOI] [PubMed] [Google Scholar]
- 51. Feingold KR, Grunfeld C. The effect of inflammation and infection on lipids and lipoproteins. In: Feingold KR, Anawalt B, Boyce A, et al., eds. The Effect of Inflammation and Infection on Lipids and Lipoproteins. MDText.com, Inc; 2019. [Google Scholar]
- 52. Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. doi: 10.1037/a0024768. PMID: 21787044; PMCID: PMC3202072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lakshmi SV, Padmaja G, Kuppusamy P, Kutala VK. Oxidative stress in cardiovascular disease. Indian J Biochem Biophys. 2009;46:421–440. [PubMed] [Google Scholar]
- 54. Marsh S, Dobson R, Maddison R. The relationship between household chaos and child, parent, and family outcomes: a systematic scoping review. BMC Public Health. 2020;20:513. doi: 10.1186/s12889-020-08587-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kelly MM, Tyrka AR, Price LH, Carpenter LL. Sex differences in the use of coping strategies: predictors of anxiety and depressive symptoms. Depress Anxiety. 2008;25:839–846. doi: 10.1002/da.20341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, Anda RF. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110:1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F [DOI] [PubMed] [Google Scholar]
- 58. Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Why do children from socioeconomically disadvantaged families suffer from poor health when they reach adulthood? A life‐course study. Am J Epidemiol. 2007;166:966–974. doi: 10.1093/aje/kwm155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Clemens V, Bürgin D, Huber‐Lang M, Plener PL, Brähler E, Fegert JM. The interplay between child maltreatment and stressful life events during adulthood and cardiovascular problems‐a representative study. J Clin Med. 2021;10:2021. doi: 10.3390/jcm10173937 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S2


