Abstract
Background
Prior studies have reported disparities by race in the management of acute myocardial infarction (MI), with many studies having limited covariates or now dated. We examined racial and ethnic differences in the management of MI, specifically non–ST‐segment‐elevation MI (NSTEMI), in a large, socially diverse cohort of insured patients. We hypothesized that the racial and ethnic disparities in the receipt of coronary angiography or percutaneous coronary intervention would persist in contemporary data.
Methods and Results
We identified individuals presenting with incident, type I NSTEMI from 2017 to 2019 captured by a health claims database. Race and ethnicity were categorized by the database as Asian, Black, Hispanic, or White. Covariates included demographics (age, sex, race, and ethnicity); Elixhauser variables, including cardiovascular risk factors and other comorbid conditions; and social factors of estimated annual household income and educational attainment. We examined rates of coronary angiography and percutaneous coronary intervention by race and ethnicity and income categories and in multivariable‐adjusted models. We identified 87 094 individuals (age 73.8±11.6 years; 55.6% male; 2.6% Asian, 13.4% Black, 11.2% Hispanic, 72.7% White) with incident NSTEMI events from 2017 to 2019. Individuals of Black race were less likely to undergo coronary angiography (odds ratio [OR], 0.93; [95% CI, 0.89–0.98]) and percutaneous coronary intervention (OR, 0.86; [95% CI, 0.81–0.90]) than those of White race. Hispanic individuals were less likely (OR, 0.88; [95% CI, 0.84–0.93]) to undergo coronary angiography and percutaneous coronary intervention (OR, 0.85; [95% CI, 0.81–0.89]) than those of White race. Higher annual household income attenuated differences in the receipt of coronary angiography across all racial and ethnic groups.
Conclusions
We identified significant racial and ethnic differences in the management of individuals presenting with NSTEMI that were marginally attenuated by higher household income. Our findings suggest continued evidence of health inequities in contemporary NSTEMI treatment.
Keywords: disparities, ethnicity, non–ST‐segment–elevation myocardial infarction, outcome, race
Subject Categories: Epidemiology, Acute Coronary Syndromes, Coronary Artery Disease, Race and Ethnicity, Women
Clinical Perspective.
What Is New?
Individuals of Black race persistently have lower odds of coronary revascularization post non–ST‐segment–elevation myocardial infarction.
Among all patients who underwent coronary angiography, individuals of Black race or Hispanic ethnicity had lower likelihood of percutaneous coronary intervention.
Lower household income was associated with lower odds of coronary revascularization post non–ST‐segment–elevation myocardial infarction.
What Are the Clinical Implications?
We identified contemporary racial and ethnic differences in the management of individuals presenting with non–ST‐segment–elevation myocardial infarction.
Continued efforts to incorporate race and ethnicity and individual‐level social factors are essential to improve health equity in cardiovascular outcomes.
Prior studies have identified racial and ethnic disparities in the management and treatment of acute coronary syndromes (ACS) and have consistently demonstrated that individuals of Black race are less likely than White individuals to receive invasive cardiac procedures such as coronary angiography and percutaneous cutaneous intervention (PCI). 1 , 2 , 3 , 4 , 5 , 6 Professional societies such as the American Heart Association 7 and Centers for Disease Control and Prevention's Healthy People 2030 8 , 9 have asserted that addressing racial disparities is a priority. 4 , 10 , 11 Identifying the extent of differences in ACS treatment by race and ethnicity in contemporary data is essential for documenting progress toward their resolution.
Further, social risk factors such as income level and educational attainment may contribute to racial and ethnic disparities in cardiovascular care. 12 , 13 As social risk factors contribute to health outcomes, understanding how they modify procedural use is likewise a priority for developing appropriate strategies to address racial disparities. 14 , 15 , 16 , 17 Social risk factors, such as income, education, and neighborhood socioeconomic status, have been shown to modify racial differences in cardiovascular risk and disease. 18 , 19 , 20 Limitations of prior studies of ACS and racial and ethnic differences in management include geographic generalizability and absence of inclusion of social risk factors that may contribute to health care access and management.
We studied racial and ethnic differences in the acute management of patients with non–ST‐segment–elevation myocardial infarction (NSTEMI) in a large, geographically representative, and contemporary administrative health claims database. Specifically, we examined rates of coronary angiography and PCI by race or ethnicity and the contributions of social risk factors, particularly annual household income, toward racial and ethnic differences. Our hypotheses were 2 fold: first, we hypothesized that we would identify persistent differences in the acute management of NSTEMI by race and ethnicity using contemporary data. Second, we hypothesized that racial and ethnic differences in NSTEMI management would vary by annual household income, a marker of social capital.
METHODS
Sample Selection
The data employed in this analysis were provided by Optum Clinformatics. As per licensing agreement, the authors cannot make the data available to others or provide the data to them. Interested individuals may seek the data directly from Optum. The authors indicate they did not have access to the data that would not be available to others with a similar licensing agreement. We conducted a retrospective analysis using Optum's de‐identified Clinformatics® Data Mart Database. Optum is a large US database composed of inpatient, outpatient, emergency department, pharmacy. and laboratory health claims. Medical claims include International Classification of Diseases, Ninth Revision and Tenth Revision codes (ICD‐9 and ICD‐10); Current Procedural Terminology codes; Healthcare Common Procedure Coding System procedure codes; and site of service codes. The database includes commercial and Medicare Advantage enrollees and is geographically diverse across the United States. Informed consent was waived as the data are de‐identified. The University of Pittsburgh Institutional Review Board determined this research activity did not constitute human subjects research.
We selected individuals hospitalized with an NSTEMI from January 1, 2017, to December 31, 2019. Individuals were required to have continuous benefit enrollment for at least 6 months before presentation with a diagnosis of NSTEMI as defined by ICD‐10 codes; all administrative codes used in the analysis are provided in Table S1. We then excluded individuals with (1) missing or unknown income or race or ethnicity; (2) heart assist device or cardiogenic shock present at the time of admission, as indicators of severity of presentation; (3) less than 6 months of enrollment; (4) age <18 years, as the diagnosis of NSTEMI in children would be both unexpected and have different management than that of adults; and (5) unknown or missing sex. Figure S1 summarizes the sequence of steps used for cohort selection. Table S2 summarizes the baseline characteristics of excluded individuals for the missing variables compared with the main cohort.
The approach toward the assignment of race or ethnicity in Optum has been described previously. 20 Briefly, race or ethnicity was derived from individual records obtained from a licensed consumer database and categorized as Asian, Black, Hispanic, or White. Individuals whose race or ethnicity could not be determined based on the described methods were considered unknown and were excluded from this analysis.
Two outcomes were assessed in this study: receipt of coronary angiography and PCI within the index hospitalization. These outcomes were assessed separately, with each dichotomized to indicate whether the procedure had been performed as identified by Current Procedural Terminology codes. An individual was considered to have either outcome of interest if they had a Current Procedural Terminology code for the corresponding procedure on a claim with a date within their inpatient stay. Those individuals with Current Procedural Terminology codes for both coronary angiography and PCI were categorized as having undergone PCI.
We collected baseline characteristics of individuals with NSTEMI, including sex, age, race, ethnicity, and estimated household income and educational attainment. The Elixhauser Comorbidity Index employed here and previously validated for administrative analyses using ICD‐9 and ICD‐10 codes 21 , 22 incorporates over 30 conditions across organ systems and their varying severity. Comorbidities were defined based on the presence of a corresponding ICD‐9 or ICD‐10 diagnosis code in any claim before or at the time of cohort entry (inpatient admission).
Annual household income was estimated by extracting >130 data points (eg, Internal Revenue Service data, address‐level home value, credit and short‐term loans) linked to the ZIP +4, a highly specific geographic indicator, as described previously. 23 Annual household income was categorized as <$40 000, $40 000–$49 999, $50 000–$59 999, $60 000–$74 999, $75 000–$99 999, and ≥$100 000 and validated using household surveys. 23 Educational attainment was similarly estimated using census data at the ZIP +4 level and was categorized as less than 12th grade, high school diploma, less than bachelor's degree, bachelor's degree or higher, or unknown.
Statistical Analysis
We summarized continuous variables by their distributions (mean and SD or median for nonnormally distributed variables) and categorical variables by their frequency. We summarized characteristics across the 4 different racial and ethnic groups (Asian, Black, Hispanic, White) using the ANOVA or Wilcoxon rank‐sum tests for continuous variables and Pearson's chi‐square tests for categorical variables. Additionally, we compared the unadjusted incidence of primary outcomes across racial or ethnicity categories.
We used stepwise multivariable‐adjusted logistic regression to assess the odds of undergoing coronary angiography or PCI across categories of race or ethnicity employing White race as our referent. Our progressive multivariable adjustment included age and sex (Model 1); the covariates included in the Elixhauser Comorbidity Index and Model 1 covariates (Model 2); annual household income, educational attainment, insurance type (Medicare versus commercial insurance), and Model 2 covariates (Model 3). Using Model 2 covariates and educational attainment, we then assessed for the association between race or ethnicity and receipt of coronary angiography by annual household income. We then repeated these steps using PCI as the outcome of interest. Individuals of White race were used as the referent category in all models. To assess the effect by annual household income, we stratified our analysis by income with White race as the referent category. We then plotted the odds ratios (ORs) of the association of race and ethnicity on receipt of interventions by annual household income on a log scale. As a sensitivity analysis, in Table S3, we used Greedy propensity score matching to reduce residual confounding in our regression models. We used 1:2 matching of individuals of Black race, Hispanic and Asian ethnicity to individuals of White race with a caliper of 0.2, and repeated our multivariable‐adjusted logistic regressions described earlier using the matched data. We then repeated our stratified analyses by income with White race as the referent category. All analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC). A 2‐sided P value of 0.05 was considered the threshold for statistical significance.
RESULTS
Following exclusions, we identified a total of 87 094 individuals for inclusion in the analysis as described by Table 1 (age 73.8±11.6 years; 55.6% male; 2.6% Asian, 13.4% Black, 11.2% Hispanic, 72.7% White). Hypertension, diabetes, and stroke were more common among Black and Hispanic individuals than Asian and White individuals. In total, 52.5% of the data set had an annual household income ≥$50 000; of whom 3.4% were Asian, 7.5% were Black, 10.1% were Hispanic, and 79% were White. Among those with Medicare, 2.4% were Asian race, 13.7% Black race, 11.5% Hispanic ethnicity, and 72.3% White race. Among those with a bachelor's degree, 5.4% were Asian race, 4.9% Black race, 7.0% Hispanic ethnicity, and 82.6% White race. Among those who had <12th‐grade education, 4% were Asian race, 4.9% were Black race, 67% were Hispanic ethnicity, and 24% were White race.
Table 1.
Baseline Characteristics by Race and Ethnicity
| Race and ethnicity | All eligible patients (n=87 094) | Asian (n=2303) | Black (n=11 659) | Hispanic (n=9780) | White (n=63 352) |
|---|---|---|---|---|---|
| Age, y, mean (SD) | 73.8 (11.6) | 73.3 (12.5) | 72.1 (11.6) | 73.5 (11.8) | 74.2 (11.4) |
| Sex, n (%) | |||||
| Female | 38 683 (44.4%) | 887 (38.5%) | 6255 (53.7%) | 4228 (43.2%) | 27 313 (43.1%) |
| Male | 48 411 (55.6%) | 1416 (61.5%) | 5404 (46.4%) | 5552 (56.8%) | 36 039 (56.9%) |
| Education level, n (%) | |||||
| <12th grade | 526 (0.6%) | 21 (0.9%) | 26 (0.2%) | 354 (3.6%) | 125 (0.2%) |
| High school diploma | 30 164 (34.6%) | 485 (21.1%) | 6316 (54.2%) | 4644 (47.5%) | 18 719 (29.6%) |
| <Bachelor's degree | 46 614 (53.5%) | 1261 (54.8%) | 4831 (41.4%) | 4091 (41.8%) | 36 431 (57.5%) |
| ≥Bachelor's degree | 9715 (11.2%) | 534 (23.2%) | 477 (4.1%) | 681 (7%) | 8023 (12.7%) |
| Unknown | 75 (0.1%) | 2 (0.1%) | 9 (0.1%) | 10 (0.1%) | 54 (0.1%) |
| Household income, n (%) | |||||
| <$40 000 | 32 781 (37.6%) | 556 (24.1%) | 6931 (59.5%) | 4050 (41.4%) | 21 244 (33.5%) |
| $40 000‐$49 999 | 8536 (9.8%) | 172 (7.5%) | 1282 (11%) | 1123 (11.5%) | 5959 (9.4%) |
| $50 000‐$59 999 | 8568 (9.8%) | 193 (8.4%) | 1092 (9.4%) | 1167 (11.9%) | 6116 (9.7%) |
| $60 000–$74 999 | 10 269 (11.8%) | 273 (11.9%) | 950 (8.2%) | 1157 (11.8%) | 7889 (12.5%) |
| $75 000–$99 999 | 12 345 (14.2%) | 413 (17.9%) | 800 (6.9%) | 1137 (11.6%) | 9995 (15.8%) |
| $100 000 | 14 595 (16.8%) | 696 (30.2%) | 604 (5.2%) | 1146 (11.7%) | 12 149 (19.2%) |
| Medicare, n (%) | 72 681 (83.5%) | 1847 (80.2%) | 9981 (85.6%) | 8320 (85.1% | 52 533 (82.9%) |
| Number of Elixhauser comorbidities, median (Q1, Q3) | 9 (5, 12) | 8 (5, 11) | 9 (6, 13) | 9 (6, 12) | 8 (5, 12) |
| Hypertension | 82 381 (94.6%) | 2155 (93.6%) | 11 299 (96.9%) | 9352 (95.6%) | 59 575 (94%) |
| Diabetes | 49 168 (56.5%) | 1460 (63.4%) | 7664 (65.7%) | 6730 (68.8%) | 33 314 (52.6%) |
| Stroke | 28 134 (32.3%) | 734 (31.9%) | 4056 (34.8%) | 3129 (32%) | 20 215 (31.9%) |
| Continuous enrollment time, median (Q1, Q3) | 60.7 (34.4, 106.5) | 60.8 (35.5, 109.5) | 48.6 (28.3, 87.1) | 57.8 (31.4, 117.6) | 60.8 (36.4, 108.5) |
Table 2 presents the incidence of coronary angiography and PCI by race and ethnicity and annual household income strata. In the overall cohort, Black and Hispanic individuals had a significantly lower incidence of coronary angiography than White individuals. Asian individuals (554 per 1000 inpatient events, 95% CI, 523–584) had a trend toward a lower incidence of coronary angiography when compared with White individuals (562 per 1000 inpatient events, 95% CI, 557–568). With increasing annual household income strata, individuals of Black race and Hispanic ethnicity had had similar incidence rates of coronary angiography compared with individuals of White race. Within the overall cohort, Asian (306 per 1000 inpatient events, 95% CI, 283–328), Black (256 per 1000 inpatient events, 95% CI, 247–265) and Hispanic (273 per 1000 inpatient events, 95% CI, 263–284) individuals had a lower incidence of PCI compared with individuals of White race (307 per 1000 inpatient events, 95% CI, 303–312). With increasing annual income, individuals of Asian race (for income ≥$100 000, 337 per 1000 inpatient events, 95% CI, 294–380) had a similar incidence of PCI to individuals of White race (for income ≥$100 000, 339 per 1000 inpatient events, 95% CI, 329–349). With increasing annual household income, individuals of Black race and Hispanic ethnicity had lower incidence rates of PCI than individuals of White race.
Table 2.
Incidence Rates of Coronary Angiography and Percutaneous Coronary Intervention per 1000 Individuals by Race or Ethnicity and Income Strata
| Coronary angiography | ||||
|---|---|---|---|---|
| Asian | Black | Hispanic | White | |
| Overall cohort | 553.6 (523.2, 584.0) | 528.1 (514.9, 541.3) | 535.3 (520.8, 549.8) | 562.4 (556.6, 568.2) |
| <$40 000 | 489.6 (431.4, 547.8) | 494.9 (478.6, 511.2) | 510.8 (488.6, 532.9) | 559.6 (549.2, 570) |
| $40 000–$49 999 | 598.4 (482.9, 714.0) | 508.6 (469.5, 547.6) | 516.2 (474.2, 558.2) | 551.8 (532.8, 570.8) |
| $50 000–$59 999 | 585.3 (477.4, 693.3) | 538.2 (494.6, 581.8) | 539.2 (497, 581.4) | 550.4 (532, 568.8) |
| $60 000–$74 999 | 490.4 (407.4, 573.5) | 571.2 (523.2, 619.2) | 540.1 (497.8, 582.3) | 582.5 (565.5, 599.6) |
| $75 000–$99 999 | 580.8 (507.3, 654.3) | 577.5 (524.8, 630.2) | 579.9 (535.6, 624.2) | 584.0 (569.0, 599.0) |
| ≥$100 000 | 594.7 (537.4, 652.1) | 629.1 (565.8, 692.5) | 607.3 (562.2, 652.3) | 594.4 (580.9, 607.9) |
| Percutaneous coronary intervention | ||||
| Overall cohort | 305.7 (283.1, 328.3) | 255.8 (246.6, 264.9) | 273.3 (263.0, 283.7) | 307.3 (303.0, 311.6) |
| <$40 000 | 250.2 (208.6, 291.8) | 229.6 (218.5, 240.7) | 252.8 (237.2, 268.3) | 297.8 (290.2, 305.4) |
| $40 000–$49 999 | 337.0 (250.2, 423.7) | 257.4 (229.6, 285.2) | 276.8 (246, 307.5) | 295.8 (281.9, 309.7) |
| $50 000–$59 999 | 326.3 (245.7, 406.9) | 277.8 (246.5, 309.2) | 268.3 (238.5, 298.1) | 286.4 (273.1, 299.7) |
| $60 000–$74 999 | 285.5 (222.1, 348.8) | 279.3 (245.7, 312.9) | 283.8 (253.2, 314.4) | 323.1 (310.3, 335.8) |
| $75 000–$99 999 | 319.4 (264.9, 373.9) | 307.5 (269.1, 345.9) | 290.4 (259.1, 321.7) | 325.9 (314.7, 337.1) |
| ≥$100 000 | 337.0 (293.8, 380.1) | 328.7 (282.9, 374.5) | 329.7 (296.5, 362.9) | 339 (328.8, 349.2) |
Table 3 summarizes the association between race and ethnicity and the odds of coronary angiography and PCI receipt following presentation with NSTEMI in multivariable‐adjusted models. In Model 1 (adjusted for age and sex), individuals of Black race (OR, 0.79; [95% CI, 0.76–0.82]) and Hispanic ethnicity (OR, 0.86; [95% CI, 0.82–0.90]) significantly had lower odds of receipt of coronary angiography compared with individuals of White race. In Model 3 (fully adjusted), individuals of Black race (OR, 0.93; [95% CI, 0.89–0.98]) and Hispanic ethnicity (OR, 0.88; [95% CI, 0.84–0.92]) persistently had lower odds of receipt of coronary angiography. A similar trend was observed among individuals receiving PCI. In Model 1, individuals of Black race (OR, 0.74; [95% CI, 0.71–0.78]) and Hispanic ethnicity (OR, 0.82; [95% CI, 0.78–0.86]) had lower odds of receiving PCI than individuals of White race. In Model 3, individuals of Black race (OR, 0.86; [95% CI, 0.81–0.90]) and Hispanic ethnicity (OR, 0.85; [95% CI, 0.81–0.89]) persistently had lower odds of PCI than individuals of White race. As summarized in Table S4, among individuals who have received coronary angiography, individuals of Black race (OR, 0.85; [95% CI, 0.80–0.90]) and Hispanic ethnicity (OR, 0.88; [95% CI, 0.83–0.94]) persistently had lower odds of PCI compared with Individuals of White race. We also found a significant interaction between sex, race, and income, as summarized in Table S5 and S6 and Figure S2.
Table 3.
Association of Race and Ethnicity With Coronary Angiography and Percutaneous Coronary Intervention (n=87 094) After Presentation With Non–ST‐Segment–Elevation Myocardial Infarction
| Race or ethnicity | Model 1, OR (95% CI)* | P value | Model 2, OR (95% CI)† | P value | Model 3, OR (95% CI)‡ | P value |
|---|---|---|---|---|---|---|
| Coronary angiography | ||||||
| Asian | 0.91 (0.84–1.00) | 0.04 | 0.95 (0.87–1.05) | 0.31 | 0.95 (0.87–1.05) | 0.30 |
| Black | 0.79 (0.76–0.82) | <0.01 | 0.92 (0.88–0.96) | <0.01 | 0.93 (0.89–0.98) | <0.01 |
| Hispanic | 0.86 (0.82–0.90) | <0.01 | 0.89 (0.85–0.93) | <0.01 | 0.88 (0.84–0.92) | <0.01 |
| White | Referent | … | Referent | … | Referent | … |
| Percutaneous coronary intervention | ||||||
| Asian | 0.94 (0.86–1.04) | 0.22 | 0.96 (0.87–1.05) | 0.38 | 0.96 (0.87–1.05) | 0.36 |
| Black | 0.74 (0.71–0.78) | <0.01 | 0.84 (0.80–0.88) | <0.01 | 0.86 (0.81–0.90) | <0.01 |
| Hispanic | 0.82 (0.78–0.86) | <0.01 | 0.84 (0.80–0.88) | <0.01 | 0.85 (0.81–0.89) | <0.01 |
| White | Referent | … | Referent | … | Referent | … |
Modeling the odds of receipt of coronary angiography or percutaneous coronary intervention.
Model 1 adjusted for age and/or age and sex in the overall categories.
Model 2 adjusted for Model 1 plus Elixhauser Comorbidities Index.
Model 3 adjusted for Model 2 plus income and education level.
OR indicates odds ratio.
Table 4 and Figure 1 summarize the association of race and ethnicity with coronary angiography and PCI after presentation with NSTEMI by annual household income. Among individuals with an annual household income <$40 000, Black race (OR, 0.92; [95% CI, 0.87–0.98]) and Hispanic ethnicity (OR, 0.84; [95% CI, 0.78–0.90]) were associated with significantly lower receipt of coronary angiography than White race. Similarly, individuals of Black race (OR, 0.81; [95% CI, 0.76–0.87]) and Hispanic ethnicity (OR, 0.81; [95% CI, 0.75–0.88]) had lower odds of PCI than individuals of White race. Among individuals with an annual household income ≥$100 000, the differences in the receipt of coronary angiography and PCI were attenuated across all other racial and ethnic groups compared with individuals of White race. Higher income attenuated the observed racial differences in the receipt of coronary angiography and PCI among individuals of Asian, Black, and White race compared to individuals of White race with an annual household income ≥$100 000. Using propensity matching, results were similar, whereby individuals of Black race and Hispanic ethnicity with an annual household income <$40 000 had lower odds of receipt of both coronary angiography and PCI (Table S7). Additionally, we observed effect modification between annual household income and race and ethnicity. As summarized in Table S8, relative to White individuals with an annual household income ≥$100 000, individuals with an annual household income <$40 000 and categorized as Asian, Black, or Hispanic were less likely to undergo coronary angiography and PCI.
Table 4.
Association of Race and Ethnicity with Coronary Angiography and Percutaneous Coronary Intervention (n=87094) following presentation with non‐ST segment elevation myocardial infarction, by annual household income (95% Confidence Intervals)
| Coronary angiography | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <$40 000 | P value | $40‐<$50 000 | P value | $50‐<$60 000 | P value | $60‐<$75 000 | P value | $75‐<$100 000 | P value | $ ≥ 100 000 | P value | |
| Asian | 0.84 (0.70–1.01) | 0.06 | 1.34 (0.95–1.88) | 0.10 | 1.18 (0.86–1.62) | 0.31 | 0.71 (0.54–0.92) | 0.01 | 1.07 (0.85–1.34) | 0.56 | 0.97 (0.81–1.16) | 0.73 |
| Black | 0.92 (0.87–0.98) | 0.01 | 0.89 (0.78–1.02) | 0.10 | 0.93 (0.80–1.07) | 0.30 | 0.94 (0.81–1.10) | 0.46 | 0.94 (0.80–1.11) | 0.45 | 1.01 (0.84–1.22) | 0.89 |
| Hispanic | 0.84 (0.78–0.90) | <0.01 | 0.88 (0.76–1.01) | 0.07 | 0.87 (0.76–1.01) | 0.06 | 0.89 (0.78–1.03) | 0.11 | 0.94 (0.82–1.07) | 0.36 | 0.97 (0.85–1.12) | 0.68 |
| White | Referent | Referent | Referent | Referent | Referent | Referent | ||||||
| Percutaneous coronary intervention | ||||||||||||
| Asian | 0.82 (0.67–1.01) | 0.06 | 1.28 (0.91–1.80) | 0.15 | 1.22 (0.89–1.69) | 0.22 | 0.86 (0.65–1.14) | 0.31 | 0.99 (0.79–1.24) | 0.92 | 0.95 (0.80–1.13) | 0.56 |
| Black | 0.81 (0.76–0.87) | <0.01 | 0.90 (0.78–1.04) | 0.14 | 0.99 (0.85–1.15) | 0.85 | 0.83 (0.71–0.97) | 0.02 | 0.93 (0.79–1.09) | 0.38 | 0.90 (0.75–1.08) | 0.25 |
| Hispanic | 0.81 (0.75–0.88) | <0.01 | 0.93 (0.80–1.08) | 0.32 | 0.87 (0.75–1.01) | 0.07 | 0.87 (0.75–1.00) | 0.05 | 0.81 (0.71–0.94) | <0.01 | 0.90 (0.78–1.03) | 0.12 |
| White | Referent | Referent | Referent | Referent | Referent | Referent | ||||||
Modeling the odds of receipt of coronary angiography or percutaneous coronary intervention.
Adjusted for age, sex, Elixhauser Comorbidities Index, educational level, and insurance type.
Figure 1.
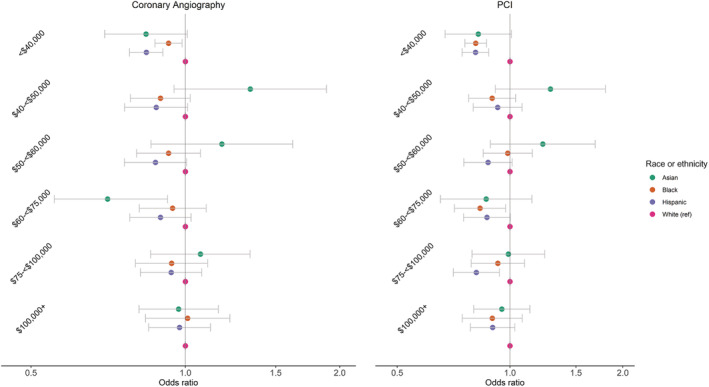
Odds ratio of coronary angiography or percutaneous coronary intervention by income and race or ethnicity (Asian – Green; Black –Orange, Hispanic – Purple, and White – Pink). PCI indicates percutaneous coronary intervention.
DISCUSSION
In a large, highly representative, administrative health claims database of insured individuals, we examined racial and ethnic differences in standard interventional treatment for individuals presenting with NSTEMI. Specifically, we identified that among individuals presenting with NSTEMI, those of Black race and Hispanic ethnicity were less likely to undergo coronary angiography and PCI than individuals of White race. Interestingly, among patients with NSTEMI who underwent coronary angiography, individuals of Black race and Hispanic ethnicity subsequently had lower odds of PCI than individuals of White race who underwent coronary angiography. Individuals of Asian race have a similar likelihood of coronary angiography and PCI as individuals of White race. We further identified a graded association between annual household income and the likelihood of coronary angiography and PCI. Specifically, we determined that lower annual household income was associated with decreased likelihood of coronary angiography and PCI in Asian, Black, and Hispanic individuals.
Extensive research has demonstrated the association between race and ethnicity and ACS management. 3 , 24 , 25 There are significant differences in the preventive care received by individuals of Black race compared with those of White race. 26 The differences in care likely indicate suboptimal preventative medical therapy and underdiagnosed coronary artery disease among individuals of Black race. Individuals of Black race are less likely to receive guideline‐based NSTEMI therapies, including coronary angiography and revascularization. 27 , 28 , 29 Notably, a prior study 27 demonstrated that racial differences in the management of NSTEMI persisted across the span of 15 years (2000–2014). Similarly, racial disparities in coronary revascularization have been noted in the management of ST‐segment–elevation myocardial infarction, with Black race and Hispanic ethnicity associated with lower likelihood of coronary intervention. 4 Our study extends this literature as we report that despite increasing awareness of health inequities, we identified persistent racial and ethnic disparities in NSTEMI management in highly generalizable contemporary data. Our analyses were further strengthened by accounting for social risk factors, thereby facilitating our examination of whether annual household income, a fundamental indicator of social capital, may modify the association between race and ethnicity and interventional strategy. Multiple mechanisms likely contribute to our findings including (1) implicit and explicit bias; (2) intersectionality of race, ethnicity, and income; and (3) individual‐level factors.
First, race and ethnicity are nuanced social constructs, incorporating institutional and individual discrimination. 30 , 31 Explicit and implicit biases may contribute to the differences in coronary interventions. For instance, many individuals bear negative attitudes toward individuals of Black race. 32 Explicit bias may manifest as miscommunication between patients and providers, lower likelihood of recommendations for guideline‐directed treatments, 28 , 33 and other practices that further racial discrimination. Compared with the presentation of an ST‐segment–elevation myocardial infarction, for which the standard of care is urgent revascularization, care differences may be amplified with regard to the approach for treating an NSTEMI. 28 Management of an NSTEMI may consequently be more susceptible to implicit biases because provider recommendations for intervention (coronary angiography or PCI) may bear more weight in low‐ to moderate‐risk patients. Prior studies have demonstrated that individuals of Black race and Hispanic ethnicity were less likely to receive counseling about referral for advanced therapies, which can have dire consequences on patient health outcomes. 34 , 35 Standardized approaches to patients with respect to guideline‐directed treatment may assist with ameliorating racial and ethnic differences in referral for invasive cardiovascular treatments.
Second, the intersectionality of race or ethnicity and income with respect to health outcomes has been demonstrated in the literature, whereby lower income has been associated with a decreased likelihood of coronary revascularization for acute myocardial infarction. 34 , 35 Lower‐income individuals have less access to high‐quality hospitals, inconsistent patient‐provider relationships, and an increased likelihood of limited health literacy, which could contribute to decreased rates of revascularization among these patients. 16 , 36 Our findings show that income level further amplifies the noted racial disparities in receipt of coronary angiography and PCI for NSTEMI. 27 , 28 We found that individuals with an income <$40 000 consistently had lower likelihood of coronary angiography and lower likelihood of PCI when compared with White individuals with an annual household income ≥$100 000. Race and ethnicity and income, correlated but by no means equivalent, have joint contributions to cardiovascular health risk and outcomes. 31 Therefore, attention must be given to both race or ethnicity and social risk factors, such as income, to overcome racial and ethnic disparities in management of ACS.
Lastly, at the individual level, prior research indicates that individuals of Black race and Hispanic ethnicity may be less likely to consent to invasive cardiovascular procedures. 37 The distrust and fear at the level of the individual may be rooted in the historical and current experiences of disadvantaged individuals within the health care system. Distrust of providers or the health care delivery system, given prior experience with discrimination, may limit patients' acceptance of treatment for ACS. 38 Further research is needed to identify and implement interventions to dismantle individual‐level barriers reinforced by structural racism. Dismantling these barriers will allow disadvantaged individuals to benefit from standard, guideline‐based therapies.
Our findings that insured individuals of Black race or Hispanic ethnicity had decreased likelihood of coronary revascularization in NSTEMI compared with those of White race are noteworthy. The decreased likelihood of coronary revascularization persisted despite adjusting for social risk factors such as income and education. Additionally, we noted that income modified the association of race and ethnicity and the likelihood of coronary interventions, such that decreasing income was associated with lower likelihood of receiving the procedures studied here across all racial and ethnic groups. The evident racial and ethnic disparities in the management of NSTEMI identified here are concerning, as coronary angiography and PCI are standard and potentially life‐saving therapies for treating ACS. 39 The persistent racial and ethnic disparities in cardiovascular disease care emphasize the critical importance of addressing obstacles toward health equity.
Our findings underscore the importance of intentionally addressing the well‐established racial and ethnic disparities in cardiovascular disease management and outcomes. A systematic review of 16 studies revealed that a diverse workforce improved clinical outcomes and health care quality. 40 Studies have shown that a more diverse cardiology workforce could lead to better patient care and health outcomes among marginalized populations, such as Black and Hispanic individuals. 41 , 42 A workforce with more minority physicians could result in more marginalized patients receiving improved preventative care, essential health care screenings, and guideline‐directed care for ACS. Training a more diverse workforce will have extensive benefits for addressing both institutionalized racism and reluctance of patients to accept interventions.
Our analysis had several strengths, most notably the availability of contemporary nationwide health claims data from over 80 000 individuals diagnosed with NSTEMI. Optum is a geographically, racially, and ethnically diverse cohort of individuals, which facilitates the generalizability of our findings to both private and Medicare Advantage‐insured individuals with NSTEMI. The demographic representation, including sex, region, age, and race and ethnicity, is consistent with the overall privately insured population in the United States. Our study has several important limitations. First, these data represent only individuals with private health insurance or Medicare Advantage. We recognize that the use of health claims data introduces a selection bias. Our inability to include uninsured patients in our analysis likely underestimates the effects of social risk factors such as income and education on receiving revascularization for ACS, specifically NSTEMI. As such, we recognize that consistent with other administrate health claims data, our results are not generalizable to those without insurance. Individuals of Black race, for example, are less likely to have insurance and therefore less represented by claims data such as used in our current analysis. Second, we recognize that administrative data are subject to misclassification of diagnoses. Third, we likewise cannot rule out misclassification of demographics such as race, ethnicity, or the social risk factors used in the current analysis. We also recognize that race and ethnicity are highly heterogeneous and may not be adequately captured by the categories used in this analysis. Similarly, we recognize that administrative data are an indirect estimation, and as such, the racial and ethnic groups may not be consistent with those identified as self‐report. Fourth, we cannot determine the appropriateness of revascularization, as we do not have data on the extent of coronary artery disease, in the current data; however, we identified consistent differences in PCI after coronary angiography by race and ethnicity. Finally, we recognize that other factors, such as neighborhood segregation, may influence the racial and ethnic differences observed here. Likewise, we cannot exclude residual confounding from unmeasured drivers of structural racism and health inequities that are beyond our capacity to include in this analysis.
CONCLUSIONS
In this retrospective analysis of a large US health care use database, we found that, compared with those of White race, individuals of Black race and Hispanic ethnicity had a persistently lower likelihood of receiving coronary angiography or PCI when presenting with NSTEMI, even when accounting for demographics, comorbidities, and social risk factors. We observed a graded association between annual household income and likelihood of coronary intervention. Our analysis used real‐world, contemporary claims data demonstrating that racial and ethnic disparities in ACS management continue to be endemic in clinical practice. Additional investigation must address how to incorporate data regarding race, ethnicity, and income into the management of patients with ACS, specifically NSTEMI, to improve the overall cardiovascular outcomes across diverse patient populations.
Sources of Funding
Dr. Jared W. Magnani – This work was supported by the following grants: National Institutes of Health/National Heart, Lung, and Blood Institute R01HL143010 and R33HL144669. Dr. Essien is supported by this award. This work was not supported specifically by this award.
Disclosures
None.
Supporting information
Tables S1‐S8
Figures S1‐S2
Supplementary Material for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.025758
For Sources of Funding and Disclosures, see page 9.
REFERENCES
- 1. Simon S, Ho PM. Ethnic and racial disparities in acute myocardial infarction. Curr Cardiol Rep. 2020;22:88. doi: 10.1007/s11886-020-01351-9 [DOI] [PubMed] [Google Scholar]
- 2. Graham G, Xiao Y‐YK, Rappoport D, Siddiqi S. Population‐level differences in revascularization treatment and outcomes among various United States subpopulations. World . J Cardiol. 2016;8:24–40. doi: 10.4330/wjc.v8.i1.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Singh JA, Lu X, Ibrahim S, Cram P. Trends in and disparities for acute myocardial infarction: an analysis of Medicare claims data from 1992 to 2010. BMC Med. 2014;12:190. doi: 10.1186/s12916-014-0190-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bolorunduro OB, Kiladejo AV, Animashaun IB, Akinboboye OO. Disparities in revascularization after ST elevation myocardial infarction (STEMI) before and after the 2002 IOM report. J Natl Med Assoc. 2016;108:119–123. doi: 10.1016/j.jnma.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 5. Rashid M, Timmis A, Kinnaird T, Curzen N, Zaman A, Shoaib A, Mohamed MO, Belder MA, Deanfield J, Martin GP, et al. Racial differences in management and outcomes of acute myocardial infarction during COVID‐19 pandemic. Heart. 2021;107:734–740. doi: 10.1136/heartjnl-2020-318356 [DOI] [PubMed] [Google Scholar]
- 6. Hess N, Seese L, Sultan I, Mulukutla S, Marroquin O, Gleason T, Fallert M, Wang Y, Thoma F, Kilic A. The impact of race on outcomes of revascularization for multivessel coronary artery disease. The Annals of Thoracic Surgery. 2020;111:1983–1990. doi: 10.1016/j.athoracsur.2020.08.005 [DOI] [PubMed] [Google Scholar]
- 7. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 8. Johnson S, Gold MR, Baciu A. Rethinking the leading health indicators for Healthy People 2030. Am Med Asso. 2020;1:e200426. doi: 10.1001/jamahealthforum.2020.0426 [DOI] [PubMed] [Google Scholar]
- 9. Jackson DN, Trivedi N, Baur C. Re‐prioritizing digital health and health literacy in healthy people 2030 to affect health equity. Health Commun. 2021;36:1155–1162. doi: 10.1080/10410236.2020.1748828 [DOI] [PubMed] [Google Scholar]
- 10. Pahigiannis K, Thompson‐Paul AM, Barfield W, Ochiai E, Loustalot F, Shero S, Hong Y. Progress toward improved cardiovascular health in the United States: healthy people 2020 heart disease and stroke objectives. Circulation. 2019;139:1957–1973. doi: 10.1161/CIRCULATIONAHA.118.035408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yancy CW, Kirtane AJ. Race/ethnicity–based outcomes in cardiovascular medicine. JAMA Cardiol. 2017;2:1313–1314. doi: 10.1001/jamacardio.2017.3826 [DOI] [PubMed] [Google Scholar]
- 12. Graham G. Racial and ethnic differences in acute coronary syndrome and myocardial infarction within the United States: from demographics to outcomes. Clinical Cardiol. 2016;39:299–306. doi: 10.1002/clc.22524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tertulien T, Chen Y, Althouse AD, Essien UR, Johnson A, Magnani JW. Association of income and educational attainment in hospitalization events in atrial fibrillation. American Journal of Preventive Cardiol. 2021;100201:100201. doi: 10.1016/j.ajpc.2021.100201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kucharska‐Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population‐based data from the United States and Finland. Ann Epidemiol. 2011;21:572–579. doi: 10.1016/j.annepidem.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu K, Cedres LB, Stamler J, Dyer A, Stamler R, Nanas S, Berkson DM, Paul O, Lepper M, Lindberg HA, et al. Relationship of education to major risk factors and death from coronary heart disease, cardiovascular diseases and all causes, Findings of three Chicago epidemiologic studies. Circulation. 1982;66:1308–1314. doi: 10.1161/01.CIR.66.6.1308 [DOI] [PubMed] [Google Scholar]
- 16. Yong CM, Abnousi F, Asch SM, Heidenreich PA. Socioeconomic inequalities in quality of care and outcomes among patients with acute coronary syndrome in the modern era of drug eluting stents. J Am Heart Assoc. 2014;3:e001029. doi: 10.1161/JAHA.114.001029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hanley GE, Morgan S, Reid RJ. Income‐related inequity in initiation of evidence‐based therapies among patients with acute myocardial infarction. J Gen Intern Med. 2011;26:1329–1335. doi: 10.1007/s11606-011-1799-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Merkin SS, Karlamangla A, Roux AD, Shrager S, Watson K, Seeman T. Race/ethnicity, neighborhood socioeconomic status and cardio‐metabolic risk. SSM Popul Health. 2020;11:100634. doi: 10.1016/j.ssmph.2020.100634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Havranek EP, Mujahid MS, Barr DA, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 20. Islam SJ, Hwan Kim J, Joseph E, Topel M, Baltrus P, Liu C, Ko YA, Almuwaqqat Z, Mujahid MS, Sims M, et al. Association between early trauma and ideal cardiovascular health among black Americans: results from the morehouse‐emory cardiovascular (MECA) center for health equity. Circulation. 2021;14:e007904. doi: 10.1161/CIRCOUTCOMES.121.007904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li B, Evans D, Faris P, Dean S, Quan H. Risk adjustment performance of Charlson and Elixhauser comorbidities in ICD‐9 and ICD‐10 administrative databases. BMC Health Serv Res. 2008;8:1–7. doi: 10.1186/1472-6963-8-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 23. LaRosa AR, T O'Neal W, Lutsey PL, Chen LY, Bengtson L, Chamberlain AM, Alonso A, Magnani JW. Association of household income and adverse outcomes in patients with atrial fibrillation. Heart. 2020;106:1679–1685. doi: 10.1136/heartjnl-2019-316065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269:2642–2646. doi: 10.1001/jama.1993.03500200056033 [DOI] [PubMed] [Google Scholar]
- 25. Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary‐revascularization procedures—are the differences real? Do they matter? New Engl J Med. 1997;336:480–486. doi: 10.1056/NEJM199702133360706 [DOI] [PubMed] [Google Scholar]
- 26. Iantorno M, Rogers T, Torguson R, Kolm P, Gajanana D, Khalid N, Shlofmitz E, Khan JM, Chen Y, Musallam A, et al. Racial disparities in clinical characteristics and outcomes of women undergoing percutaneous coronary intervention. Cardiovasc Revasc Med. 2019;20:1039–1042. doi: 10.1016/j.carrev.2019.09.020 [DOI] [PubMed] [Google Scholar]
- 27. Arora S, Stouffer GA, Kucharska‐Newton A, Vaduganathan M, Qamar A, Matsushita K, Kolte D, Reynolds HR, Bangalore S, Rosamond WD, et al. Fifteen‐year trends in management and outcomes of non‐ST‐segment‐elevation myocardial infarction among black and white patients: the ARIC community surveillance study, 2000–2014. J Am Heart Assoc. 2018;7:e010203. doi: 10.1161/JAHA.118.010203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Anstey DE, Li S, Thomas L, Wang TY, Wiviott SD. Race and sex differences in management and outcomes of patients after ST‐elevation and non–ST‐elevation myocardial infarct: results from the NCDR. Clinical Cardiol. 2016;39:585–595. doi: 10.1002/clc.22570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yong CM, Ungar L, Abnousi F, Asch SM, Heidenreich PA. Racial differences in quality of care and outcomes after acute coronary syndrome. Am J Cardiol. 2018;121:1489–1495. doi: 10.1016/j.amjcard.2018.02.036 [DOI] [PubMed] [Google Scholar]
- 30. Feagin JR, McKinney KD. The many costs of racism. Lanham, MD: Rowman & Littlefield Publishers; 2003. [Google Scholar]
- 31. Williams DR, Sternthal M. Understanding racial‐ethnic disparities in health: sociological contributions. J Health Soc Behav 2010;51 Suppl:S15‐27. doi: 10.1177/0022146510383838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Social Sci Med. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019 [DOI] [PubMed] [Google Scholar]
- 33. Breathett K, Knapp SM, Carnes M, Calhoun E, Sweitzer NK. Imbalance in heart transplant to heart failure mortality ratio among African American, hispanic, and white patients. Circulation. 2021;143:2412–2414. doi: 10.1161/CIRCULATIONAHA.120.052254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rose KM, Foraker RE, Heiss G, Rosamond WD, Suchindran CM, Whitsel EA. Neighborhood socioeconomic and racial disparities in angiography and coronary revascularization: the ARIC surveillance study. Annals Epidemiol. 2012;22:623–629. doi: 10.1016/j.annepidem.2012.06.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kilpi F, Silventoinen K, Konttinen H, Martikainen P. Early‐life and adult socioeconomic determinants of myocardial infarction incidence and fatality. Soc Sci Med. 2017;177:100–109. doi: 10.1016/j.socscimed.2017.01.055 [DOI] [PubMed] [Google Scholar]
- 36. Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.CIR.88.4.1973 [DOI] [PubMed] [Google Scholar]
- 37. Groeneveld PW, Sonnad SS, Lee AK, Asch DA, Shea JE. Racial differences in attitudes toward innovative medical technology. J Gen Intern Med. 2006;21:559–563. doi: 10.1111/j.1525-1497.2006.00453.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Purnell TS, Simpson DC, Callender CO, Boulware LE. Dismantling structural racism as a root cause of racial disparities in COVID‐19 and transplantation. Am J Transpl. 2021;21:2327–2332. doi: 10.1111/ajt.16543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore‐Mensah Y, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 40. Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019;111:383–392. doi: 10.1016/j.jnma.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 41. Johnson AE, Birru Talabi M, Bonifacino E, Culyba AJ, Jonassaint NL, Nance MA, Napoé GS, Olafiranye O, Owusu‐Ansah S, Suber TL. Considerations for racial diversity in the cardiology workforce in The United States of America. J Am Coll Cardiol. 2021;77:1934–1937. doi: 10.1016/j.jacc.2021.02.043 [DOI] [PubMed] [Google Scholar]
- 42. QT C, Johnson A, Berlacher K, Douglas PS. The urgent and ongoing need for diversity, inclusion, and equity in the cardiology workforce in the United States. J Am Heart Assoc. 2021;10:e018893. doi: 10.1161/JAHA.120.018893 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1‐S8
Figures S1‐S2


