Abstract
Background
Clinical implications of change in the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guideline on the diagnosis and management of hypertension, compared with recommendations by 2014 expert panel and Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7), are not known.
Methods and Results
Using data from the NCDR (National Cardiovascular Data Registry) PINNACLE (Practice Innovation and Clinical Excellence) Registry (January 2013‐Decemver 2016), we compared the proportion and clinical characteristics of patients seen in cardiology practices diagnosed with hypertension, recommended antihypertensive treatment, and achieving blood pressure (BP) goals per each guideline document. In addition, we evaluated the proportion of patients at the level of practices meeting BP targets defined by each guideline. Of 6 042 630 patients evaluated, 5 027 961 (83.2%) were diagnosed with hypertension per the 2017 ACC/AHA guideline, compared with 4 521 272 (74.8%) per the 2014 panel and 4 545 976 (75.2%) per JNC7. The largest increase in hypertension prevalence was seen in younger ages, women, and those with lower cardiovascular risk. Antihypertensive medication was recommended to 70.6% of patients per the ACC/AHA guideline compared with 61.8% and 65.9% per the 2014 panel and JNC7, respectively. Among those on antihypertensive agents, 41.2% achieved BP targets per the ACC/AHA guideline, compared with 79.4% per the 2014 panel and 64.3% per JNC7. Lower proportions of women, non‐White (Black and "other") races, and those at higher cardiovascular risk achieved BP goals. Median practice‐level proportion of patients meeting BP targets per the 2014 panel but not the ACC/AHA guideline was 37.8% (interquartile range, 34.8%–40.7%) and per JNC7 but not the ACC/AHA guideline was 22.9% (interquartile range, 19.8%–25.9%).
Conclusions
Following publication of the 2017 guideline, significantly more people, particularly younger people and those with lower cardiovascular risk, will be diagnosed with hypertension and need antihypertensive treatment compared with previous recommendations. Significant practice‐level variation in BP control also exists. Efforts are needed to improve guideline‐concordant hypertension management in an effort to improve outcomes.
Keywords: cardiovascular disease, guideline, hypertension, prevalence, prevention
Subject Categories: Cardiovascular Disease, Epidemiology
Nonstandard Abbreviations and Acronyms
- ACC
American College of Cardiology
- AHA
American Heart Association
- JNC7
Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
- PCE
pooled cohort risk equation
Clinical Perspective
What Is New?
This study demonstrates that applications of the most recent 2017 American College of Cardiology/American Heart Association hypertension guidelines in cardiology practices will result in a substantially increased number of adults meeting criteria for diagnosis of hypertension.
Moreover, a substantially higher proportion of adults are at risk of being short of the more intensive blood pressure goal set by the 2017 guideline.
This was most pronounced in women, underrepresented races and ethnicities, and those with higher atherosclerotic cardiovascular disease risk.
What Are the Clinical Implications?
This study underscores a greater need to identify patients with hypertension and to initiate lifestyle changes and treatment approaches in appropriate patients to be guideline concordant.
The 2017 American College of Cardiology/American Heart Association guideline, however, may serve as a wake‐up call to identify patients not meeting blood pressure goals.
Although perfect attainment of these goals on a population level will never be achievable, recognition of more patients being further from their goals may spur greater lifestyle and pharmacologic efforts in appropriate patients to control blood pressure.
The 2017 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults 1 provides blood pressure (BP) thresholds for the diagnosis of hypertension, initiation of antihypertensive treatment, and targets for BP control. Compared with recommendations from the 2014 report from the expert panel, composed of members appointed to the intended Eighth Joint National Committee 2 and the 2003 Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7), 3 notable differences in definitions exist (Table 1).
Table 1.
BP Levels to Define Hypertension, Recommend Antihypertensive Therapy, and Provide Treatment Goals, According to the ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7
| Variable | ACC/AHA 1 | 2014 Expert report 2 | JNC7 3 | |
|---|---|---|---|---|
| Definition of hypertension | General population | ≥130/80 | ≥140/90 | ≥140/90 |
| Aged ≥60 y without diabetes or CKD | ≥130/80 | ≥150/90 | ≥140/90 | |
| Initiation of antihypertensive therapy | General | ≥140/90 | ≥140/90 | ≥140/90 |
| Diabetes or CKD | ≥130/80 | ≥140/90 | ≥130/80 | |
| Elevated CVD risk * | ≥130/80 | ≥140/90 | ≥140/90 | |
| Aged ≥65 y | ≥130/80 | ≥150/90 | ≥140/90 | |
| Aged ≥60 y without diabetes or CKD | ≥140/90 | ≥150/90 | ≥140/90 | |
| Goal of BP treatment | General | <130/80 | <140/90 | <140/90 |
| Diabetes or CKD | <130/80 | <140/90 | <130/80 | |
| Aged ≥65 y | <130/80 | <150/90 | <140/90 | |
| Aged ≥60 without diabetes or CKD | <130/80 | <150/90 | <140/90 |
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; CKD, chronic kidney disease; CVD, cardiovascular disease; and JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
*Elevated risk defined as estimated 10‐year CVD risk >10%.
First, the ACC/AHA guideline uses a lower systolic and diastolic BP threshold of 130/80 mm Hg to define hypertension, compared with 140/90 mm Hg used by the previous 2014 expert panel report and JNC7. Although all 3 documents recommend the use of antihypertensive therapy in those with a BP ≥140/90 mm Hg, the most recent guideline also recommends therapy for individuals with a BP ≥130/80 mm Hg and either a 10‐year atherosclerotic cardiovascular disease (ASCVD) risk ≥10% or high‐risk comorbidities (ischemic heart disease, heart failure [HF], diabetes, or chronic kidney disease). Based in part on data from SPRINT (Systolic Blood Pressure Intervention Trial), 4 the 2017 ACC/AHA guideline recommends a more aggressive BP target of <130/80 mm Hg in all adults. In contrast, the 2014 expert panel report recommends a goal of <140/90 mm Hg for all except those aged >60 years, for whom a target of <150/90 mm Hg is recommended. Similarly, the JNC7 set a BP goal of <140/90 mm Hg for the general population, reserving a more intensive goal of <130/80 mm Hg for those with diabetes or chronic kidney disease.
A previous study of 9623 participants in the National Health and Nutrition Examination Survey showed that the application of the 2017 ACC/AHA guideline significantly increased the number of people diagnosed with hypertension as well as those warranting drug therapy. 5 However, the applicability and clinical implications of the ACC/AHA thresholds for diagnosis of hypertension, initiation of antihypertensive therapy, and aggressive treatment targets in a broader population seeking care in cardiology practices and particular subgroups (eg, women, underrepresented races and ethnicities, and those with varying cardiovascular disease [CVD] risk) are not known. It is also unknown whether these findings are consistent across cardiology practices in which patients receive care.
We analyzed data from the NCDR (National Cardiovascular Data Registry) PINNACLE (Practice Innovation and Clinical Excellence) Registry to estimate the number, proportion, and clinical characteristics of patients (1) diagnosed with hypertension, (2) recommended antihypertensive therapy, and (3) on antihypertensive medications who achieved treatment goals according to the ACC/AHA guideline, compared with the 2014 expert panel report and the JNC7. In addition, to understand the impact of guideline changes on hypertension control rates of individual practices, we evaluated practice‐level variation in the proportion of patients meeting BP targets as per either the 2014 expert panel report or JNC7 but not the ACC/AHA criteria. The current analysis is critical to inform the percentage of patients requiring treatment intensification to make their care guideline concordant.
Methods
Data Source
The authors declare that all supporting data are available within the article (and its online supplementary files). The NCDR PINNACLE Registry, established in 2008 by the ACC, is the first national, prospective, office‐based quality improvement registry in the United States with voluntary participation from academic and community‐based cardiology practices. 6 It is the largest outpatient cardiovascular practice registry in the world, with >32 million patient visits to >6000 clinicians at 1954 office locations. The registry is focused on a comprehensive assessment of real‐world management of common chronic cardiovascular conditions, including hypertension, HF, coronary artery disease (CAD), and atrial fibrillation.
A detailed overview of the PINNACLE Registry data collection methods has been published previously. 7 Participation is voluntary; data are extracted from clinical documentation using algorithms mapped to the electronic health record. 8 Data quality is maintained through standardized data collection and transmission protocols, explicit data definitions, uniform data entry, and periodic data quality checks. 9 , 10 Performance metrics for CAD, HF, and atrial fibrillation are endorsed by the ACC, AHA, and the American Medical Association–Physician Consortium for Performance Improvement. 11 , 12 , 13 Given extraction of deidentified data from an electronic medical record under a quality improvement model, approval from an institutional review board and informed consent were waived.
Study Population
For the current analysis, we included all patients, aged ≥18 years, seeking care in practices enrolled in the PINNACLE Registry between January 2013 and December 2016 (n=10 031 431). Patients with missing BP values were excluded from the analysis (n=886 484). Of 9 144 947 with BP values available, we excluded those aged <18 or >100 years (n=118 245) or with <2 BP measurements within the past 2 years (n=2 984 072) of index visit for a total of 6 042 630 patients in our analysis (Figure 1).
Figure 1. Flow diagram of PINNACLE (Practice Innovation and Clinical Excellence) Registry patients with hypertension.
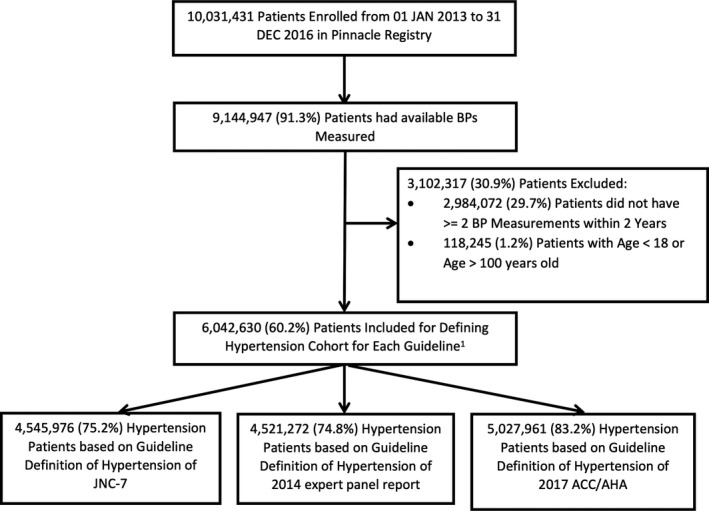
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; and JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Study Outcomes and Statistical Analysis
All baseline demographic data, including comorbidities, were assessed at index event. We first assessed the number and proportion of patients meeting the definition of hypertension according to the 2017 ACC/AHA guideline, 2014 expert panel report, and JNC7 (Table 1) based on available BP measurements for the overall registry and selected subgroups by age (18–44, 45–54, 55–64, 65–74, and ≥75 years), sex (men or women), race (White, Black, or other), ethnicity (Hispanic or non‐Hispanic), 10‐year ASCVD risk categories using (PCEs) (<5%, 5%–<10%, 10%–<20%, or ≥20%), and history of CVD (yes or no). All proportions and 95% CIs were estimated using the Clopper‐Pearson method. Given small number of patients in race categories other than White and Black, ie, Asian, American Indian/Alaskan Native, Native Hawaiin/Pacific Islander in the PINNACLE registry, all other race categories were combined to form “other races.”
In addition to those who met previously noted criteria for hypertension, patients marked as having hypertension in the registry or who were on antihypertensive medication (not solely for left ventricular ejection fraction ≤40%) were also regarded as having hypertension. Patients with ≥2 encounters with BP available within 2 years were included in the analysis. The first encounter was used as an index encounter. BPs were calculated as the mean of systolic BP or diastolic BP values for all encounters occurring within 2 years of the index encounter, including the index event. Patients were defined as having hypertension based on BP definitions for systolic BP, diastolic BP, or both; for example, if a patient had systolic BP of 136 mm Hg and diastolic BP of 72 mm Hg, the patient was considered as having hypertension per the 2017 ACC/AHA guideline.
For each individual study subject in the cohort, individual 10‐year risk for ASCVD was calculated on the basis of the ACC/AHA PCE for estimation of 10‐year risk of ASCVD. For the equation, the values for age, total cholesterol, high‐density lipoprotein cholesterol, and systolic BP are Ln transformed. Interactions between age and lipids or age and systolic BP use the natural log of each variable (eg, Ln[Age]×Ln[Total Cholesterol]). These values are then multiplied by the coefficients from the equation (used from 2013 ACC/AHA Cardiovascular Risk Assessment Guideline) for the specific race‐sex group of the individual. The sum of the “Coefficient×Value” is then calculated for the individual according to race and sex group. The estimated 10‐year risk of a first hard ASCVD event was then calculated for each individual as 1 minus the survival rate at 10 years (also obtained from the above guideline document), raised to the power of the exponent of the “Coefficient×Value” sum minus the race‐ and sex‐specific overall mean “Coefficient×Value” sum or, in equation form: 1−S10(lndX’B–MeanX’B).
We then compared the characteristics of patients meeting each of the 3 definitions of hypertension. This included age (analyzed as a continuous variable and stratified into following groups: 18–44, 45–54, 55–64, 65–74, and ≥75 years), sex (male or female), race (White, Black, or other), ethnicity (Hispanic or non‐Hispanic), documented history of comorbidities, including diabetes, chronic kidney disease (CKD), CAD, stroke/transient ischemic attack, and HF with preserved or reduced ejection fraction in the chart. For patients with hypertension without any of these comorbidities, we calculated and compared 10‐year ASCVD risk using the PCE, with stratification as <5%, 5% to 10%, 10% to <20%, and >20%.
Second, we evaluated the number and proportion of PINNACLE Registry participants meeting criteria for initiation of antihypertensive therapy (Table 1) for the entire registry and across the above‐listed subgroups. We also evaluated the number and proportion of participants recommended antihypertensive therapy per the 2017 ACC/AHA guideline but not the 2014 expert panel report or JNC7. We compared the clinical characteristics of patients recommended antihypertensive therapy by age, sex, race, history of prior transient ischemic attack or stroke, history of ischemic heart disease, diabetes, CKD, HF, and 10‐year ASCVD risk.
Third, we calculated the number and proportion of patients in the PINNACLE Registry meeting BP treatment targets (Table 1) for the entire cohort and above noted subgroups. We compared the clinical characteristics of patients meeting BP treatment targets by age, sex, race, history of prior transient ischemic attack or stroke, history of ischemic heart disease, diabetes, CKD, HF, and 10‐year ASCVD risk. We performed sensitivity analysis to include only visits in which patients on antihypertensive therapy for all visits with each patient having a minimum of at least 2 visits to calculate mean BP for the patient. We then calculated the number and proportions of these patients and compared clinical characteristics of patients on antihypertensive therapy meeting BP targets per each guideline document.
Finally, we assessed the implications of changes in guideline recommendations on hypertension management at the practice level because practices and providers are often incentivized to achieve specific levels of BP control. Accordingly, we calculated median practice‐level rates and interquartile range for the difference in the proportion of patients meeting BP targets per the 2014 expert panel report or JNC7 but not the 2017 ACC/AHA guideline. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
Results
Prevalence of Hypertension
Of the 6 042 630 patients included in the primary analysis, 5 027 961 (83.2%) were diagnosed with hypertension per the 2017 ACC/AHA guideline, 4 521 272 (74.8%) per the 2014 expert panel report, and 4 545 976 (75.2%) per JNC7 (Figure 2). This amounts to an absolute increase in the prevalence of hypertension of 8.4% and 8.0% when the 2017 ACC/AHA guideline is compared with the 2014 expert panel report and JNC7, respectively (Table 2). The proportion of patients meeting criteria of hypertension based on a history of hypertension or being on antihypertensive medications for the 2014 expert panel and JNC7 is shown in Tables S1 and S2, respectively.
Figure 2. Proportion of patients enrolled in the PINNACLE (Practice Innovation and Clinical Excellence) Registry, seeking care in cardiology practices between January 2013 and December 2016 and meeting criteria for the definition of hypertension, recommendations for antihypertensive therapies, and targets for blood pressure based on American College of Cardiology (ACC)/American Heart Association (AHA) guidelines, 2014 expert panel report, and Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7).
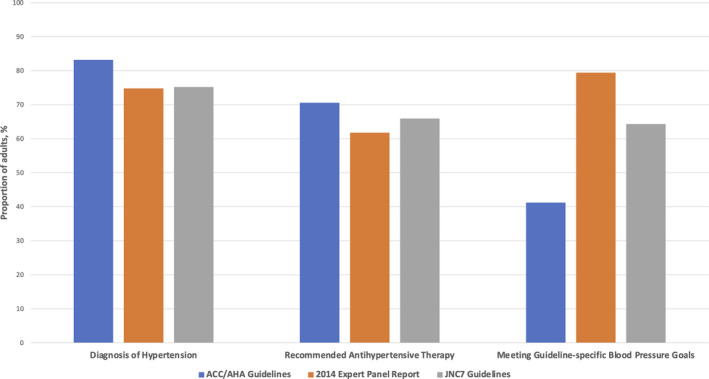
Compared with the 2014 expert panel report and JNC7, a higher proportion of patients are diagnosed with hypertension and meet recommendations for antihypertensive therapy. Moreover, as the blood pressure (BP) treatment goals set by the ACC/AHA guidelines are more intensive, a higher proportion of adults will not meet BP goals.
Table 2.
Percentages of US Adults, Overall and in Selected Subgroups, Meeting the Definition for Hypertension According to the ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Subgroups | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Overall (N=6 042 630) | 83.21 (83.18–83.24) | 74.82 (74.79–74.86) | 8.39 (8.36–8.41) | 75.23 (75.20–75.27) | 7.98 (7.95–8.00) |
| Age group, y | |||||
| 18–44 (N=892 971) | 53.66 (53.55–53.76) | 36.06 (35.96–36.16) | 17.60 (17.52–17.68) | 36.06 (35.96–36.16) | 17.60 (17.52–17.68) |
| 45–54 (N=806 202) | 78.41 (78.32–78.50) | 66.01 (65.91–66.11) | 12.40 (12.33–12.47) | 66.01 (65.91–66.11) | 12.40 (12.33–12.47) |
| 55–64 (N=1 280 248) | 86.13 (86.07–86.19) | 77.77% (77.70–77.84) | 8.36 (8.32–8.41) | 78.16 (78.09–78.23) | 7.97 (7.93–8.02) |
| 65–74 (N=1 569 242) | 90.73 (90.69–90.78) | 85.13 (85.07–85.19) | 5.60 (5.57–5.64) | 85.84 (85.78–85.89) | 4.90 (4.86–4.93) |
| ≥75 (N=1 493 967) | 93.05 (93.01–93.09) | 89.40 (89.35–89.45) | 3.66 (3.63–3.69) | 89.97 (89.93–90.02) | 3.08 (3.05–3.11) |
| Men (N=2 888 411) | 87.49 (87.45–87.52) | 79.38 (79.33–79.43) | 8.11 (8.07–8.14) | 79.76 (79.71–79.80) | 7.73 (7.70–7.76) |
| Women (N=3 148 983) | 79.27 (79.23–79.32) | 70.62 (70.57–70.67) | 8.65 (8.62–8.68) | 71.06 (71.01–71.11) | 8.21 (8.18–8.24) |
| Race or ethnicity | |||||
| White (N=3 933 307) | 82.74 (82.70–82.77) | 74.04 (73.99–74.08) | 8.70 (8.67–8.73) | 74.49 (74.45–74.54) | 8.24 (8.21–8.27) |
| Black (N=432 202) | 87.45 (87.35–87.54) | 79.79 (79.67–79.91) | 7.66 (7.58–7.74) | 80.08 (79.96–80.20) | 7.36 (7.29–7.44) |
| Other (N=28 139) * | 81.31 (80.85–81.77) | 73.12 (72.60–73.64) | 8.19 (7.87–8.52) | 73.44 (72.92–73.96) | 7.87 (7.56–8.19) |
| Hispanic (N=255 374) | 79.91 (79.76–80.07) | 71.50 (71.32–71.67) | 8.42 (8.31–8.53) | 71.78 (71.60–71.95) | 8.14 (8.03–8.24) |
| Non‐Hispanic (N=5 787 256) | 83.35 (83.32–83.38) | 74.97 (74.93–75.01) | 8.38 (8.36–8.41) | 75.38 (75.35–75.42) | 7.97 (7.95–7.99) |
| 10‐y ASCVD risk categories, % | |||||
| <5 (N=30 796) | 70.16 (69.65–70.67) | 55.21 (54.65–55.76) | 14.95 (14.56–15.36) | 55.28 (54.73–55.84) | 14.88 (14.48–15.28) |
| 5–<10 (N=21 241) | 85.39 (84.90–85.86) | 74.49 (73.90–75.08) | 10.89 (10.48–11.32) | 74.93 (74.34–75.51) | 10.46 (10.05–10.88) |
| 10–<20 (N=24 609) | 91.02 (90.65–91.37) | 83.60 (83.13–84.06) | 7.42 (7.09–7.75) | 84.06 (83.60–84.51) | 6.96 (6.64–7.28) |
| ≥20% (N=21 394) | 96.40 (96.14–96.64) | 92.68 (92.33–93.03) | 3.71 (3.46–3.97) | 93.11 (92.77–93.45) | 3.28 (3.05–3.53) |
| History of CVD (N=2 585 483) | 92.82 (92.79–92.85) | 89.49 (89.45–89.52) | 3.33 (3.31–3.35) | 89.68 (89.64–89.72) | 3.14 (3.12–3.16) |
Proportions and 95% Clopper‐Pearson (exact) CIs were reported. In each row, we presented the percentage of patients with hypertension and patients with guideline‐recommended antihypertensive medication in each subgroup. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; and PINNACLE, Practice Innovation and Clinical Excellence.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/Pacific Islander.
The prevalence of hypertension was higher within all age, sex, race and ethnicity, and ASCVD risk categories and CVD subgroups (Figure 3A through 3F). Of the 6 042 630 patients in our analysis, 2 585 483 had history of CVD. Among adults without CVD, 98 040 had available data to calculate ASCVD risk, with 98 040 having complete lipid data. The largest increase was seen in the youngest age groups (aged 18–45 years followed by aged 45‐54 years), women, and those with lower ASCVD risk (<5% and 5%–10%) (Figure 3A and 3E and Table 2).
Figure 3. Proportion of patient enrolled in the PINNACLE (Practice Innovation and Clinical Excellence) Registry, between January 2013 and December 2016, meeting criteria for the definition of hypertension, recommendations for antihypertensive therapies, and targets for blood pressure based on the American Colleoge of Cardiology (ACC)/American Heart Association (AHA) guidelines, 2014 expert panel report, and Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of high blood pressure (JNC7) across age categories (A), sex (B), race (C), ethnicity (D), 10 year atherosclerotic cardiovascular disease (ASCVD) risk categories (E), and presence of CVD (F).
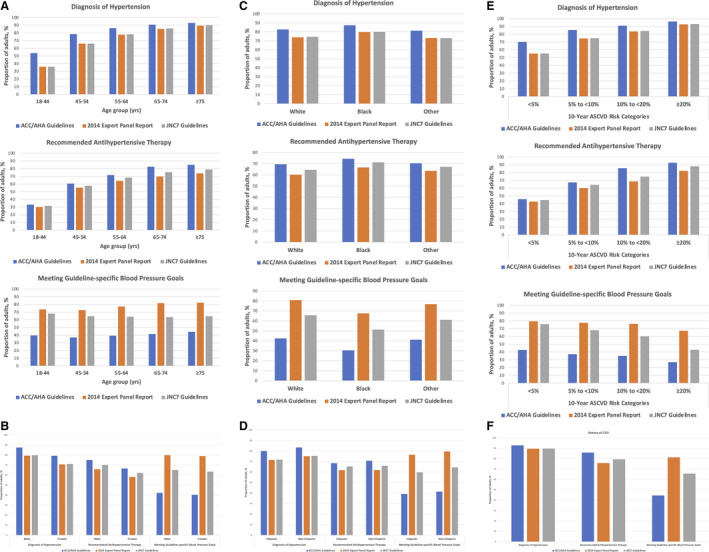
CVD indicates cardiovascular disease.
Baseline characteristics of patients diagnosed with hypertension based on 3 criteria are shown in Table 3. Patients were comparable in terms of age, sex, ASCVD risk, and prevalence of diabetes, CKD, stroke, HF, and CAD. Patients diagnosed with hypertension based on the ACC/AHA guideline alone were more likely to be younger, to be women, and with a lower predicted 10‐year ASCVD risk and prevalence of diabetes, CKD, stroke, CAD, and HF.
Table 3.
Baseline Characteristics of US Adults Meeting the Definition for Hypertension According to the ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Characteristics | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Total No. | 5 027 961 | 4 521 272 | 506 689 | 4 545 976 | 481 985 |
| Age, y | |||||
| Mean±SD | 65.0±14.7 | 66.3±13.9 | 53.4±16.9 | 66.3±13.9 | 52.4±16.7 |
| Median (Q1–Q3) | 67.0 (56.0–76.0) | 67.0 (58.0–76.0) | 54.0 (41.0–66.0) | 68.0 (58.0–76.0) | 53.0 (40.0–65.0) |
| Range (minimum–maximum) | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 |
| 18–44 | 9.5 | 7.1 | 31.0 | 7.1 | 32.6 |
| 45–54 | 12.6 | 11.8 | 19.7 | 11.7 | 20.7 |
| 55–64 | 21.9 | 22.0 | 21.1 | 22.0 | 21.2 |
| 65–74 | 28.3 | 29.5 | 17.4 | 29.6 | 15.9 |
| ≥75 | 27.6 | 29.5 | 10.8 | 29.6 | 9.5 |
| Sex | |||||
| Men | 50.3 | 50.8 | 46.2 | 50.7 | 46.3 |
| Women | 49.7 | 49.2 | 53.8 | 49.3 | 53.7 |
| Race | |||||
| White | 64.7 | 64.4 | 67.5 | 64.5 | 67.3 |
| Black | 7.5 | 7.6 | 6.5 | 7.6 | 6.6 |
| Other * | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
| Missing | 27.3 | 27.5 | 25.5 | 27.5 | 25.7 |
| History of stroke/TIA | 10.9 | 11.5 | 5.9 | 11.4 | 5.8 |
| History of stroke | 8.5 | 8.9 | 4.9 | 8.8 | 4.9 |
| History of TIA | 3.4 | 3.7 | 1.4 | 3.7 | 1.4 |
| Coronary artery disease | 38.3 | 41.4 | 10.7 | 41.2 | 10.5 |
| History of MI | 9.1 | 9.9 | 2.3 | 9.8 | 2.3 |
| History of PCI | 13.0 | 14.1 | 2.9 | 14.1 | 2.9 |
| History of CABG | 6.5 | 7.1 | 1.2 | 7.1 | 1.2 |
| Diabetes | 22.4 | 24.0 | 7.8 | 23.9 | 8.2 |
| Chronic kidney disease | 3.9 | 4.3 | 0.6 | 4.3 | 0.6 |
| Heart failure | 15.1 | 16.3 | 4.7 | 16.2 | 4.7 |
| 10‐y Predicted ASCVD risk, % | |||||
| Mean±SD (N) | 14.0±12.0 (82 765) | 14.8±12.3 (73 227) | 7.8±7.7 (9538) | 14.8±12.3 (73 548) | 7.6±7.5 (9217) |
| Median (Q1–Q3) | 10.6 (4.8–20.0) | 11.5 (5.4–21.1) | 5.3 (2.3–10.7) | 11.5 (5.4–21.1) | 5.0 (2.3–10.4) |
| Range (minimum–maximum) | 0.0–95.1 | 0.0–95.1 | 0.1–63.1 | 0.0–95.1 | 0.1–63.1 |
| <5 | 26.1 | 23.2 | 48.3 | 23.1 | 49.7 |
| 5–<10 | 21.9 | 21.6 | 24.3 | 21.6 | 24.1 |
| 10–<20 | 27.1 | 28.1 | 19.1 | 28.1 | 18.6 |
| ≥20 | 24.9 | 27.1 | 8.3 | 27.1 | 7.6 |
| History of CVD | 47.7 | 51.2 | 17.0 | 51.0 | 16.8 |
Data are given as percentages, unless otherwise indicated. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; CABG, coronary artery bypass grafting; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; MI, myocardial infarction; PCI, percutaneous coronary intervention; Q1, quartile 1; Q3, quartile 3; PINNACLE, Practice Innovation and Clinical Excellence; and TIA, transient ischemic attack.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/Pacific Islander.
Eligibility for Antihypertensive Therapy
Overall, 70.6%, 61.8%, and 65.9% qualified for antihypertensive pharmacotherapy according to the 2017 ACC/AHA guideline, 2014 expert panel report, and JNC7, respectively (Figure 2). This results in an additional 8.8% and 4.7% qualifying for BP‐lowering therapy when the 2017 ACC/AHA guideline was compared with the 2014 expert panel report and JNC7 (Table 4). These findings were consistent for patients regardless of age, sex, race and ethnicity, and ASCVD risk (Figure 3A through 3E). The largest increase, however, was seen in older age groups (aged >65 years), those with an intermediate 10‐year ASCVD risk (10%–<20%), and those with a history of CVD (Figure 3A, 3E, and 3F and Table 4).
Table 4.
Percentage of US Adults, Overall and in Selected Subgroups, Recommended Antihypertensive Medication According to the ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Subgroups | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Overall (N=6 042 630) | 70.60 (70.56–70.64) | 61.80 (61.76–61.84) | 8.80 (8.78–8.83) | 65.93 (65.89–65.96) | 4.67 (4.66–4.69) |
| Age group, y | |||||
| 18–44 (N=892 971) | 33.16 (33.06–33.26) | 30.14 (30.05–30.24) | 3.02 (2.99–3.06) | 31.56 (31.47–31.66) | 1.60 (1.57–1.62) |
| 45–54 (N=806 202) | 60.68 (60.58–60.79) | 55.20 (55.09–55.31) | 5.48 (5.43–5.53) | 57.75 (57.64–57.86) | 2.93 (2.90–2.97) |
| 55–64 (N=1 280 248) | 71.61 (71.53–71.69) | 64.20 (64.12–64.28) | 7.41 (7.36–7.45) | 68.40 (68.32–68.48) | 3.20 (3.17–3.23) |
| 65–74 (N=1 569 242) | 82.51 (82.45–82.57) | 69.68 (69.61–69.75) | 12.83 (12.78–12.88) | 75.30 (75.23–75.36) | 7.21 (7.17–7.25) |
| ≥75 (N=1 493 967) | 84.96 (84.90–85.01) | 73.94 (73.87–74.01) | 11.02 (10.97–11.07) | 78.91 (78.84–78.97) | 6.05 (6.01–6.09) |
| Men (N=2 888 411) | 75.05 (75.00–75.10) | 65.84 (65.78–65.89) | 9.21 (9.17–9.24) | 70.04 (69.99–70.09) | 5.01 (4.98–5.03) |
| Women (N=3 148 983) | 66.51 (66.46–66.56) | 58.08 (58.02–58.13) | 8.43 (8.40–8.46) | 62.14 (62.09–62.20) | 4.37 (4.34–4.39) |
| Race and ethnicity | |||||
| White (N=3 933 307) | 69.52 (69.48–69.57) | 60.18 (60.13–60.23) | 9.35 (9.32–9.37) | 64.56 (64.51–64.60) | 4.97 (4.94–4.99) |
| Black (N=432 202) | 74.40 (74.27–74.53) | 66.64 (66.50–66.78) | 7.76% (7.68–7.84) | 71.17 (71.04–71.31) | 3.23 (3.18–3.28) |
| Other * (N=28 139) | 70.44 (69.90–70.97) | 63.61 (63.04–64.17) | 6.83 (6.54–7.14) | 67.22 (66.66–67.76) | 3.22 (3.02–3.44) |
| Hispanic (N=255 374) | 68.35 (68.17–68.53) | 61.67 (61.48–61.85) | 6.69 (6.59–6.78) | 65.23 (65.05–65.42) | 3.12 (3.05–3.19) |
| Non‐Hispanic (N=5 787 256) | 70.70 (70.66–70.74) | 61.80 (61.76–61.84) | 8.90 (8.87–8.92) | 65.96 (65.92–65.99) | 4.74 (4.73–4.76) |
| 10‐y ASCVD risk categories, % | |||||
| <5 (N=30 796) | 45.82 (45.26–46.38) | 42.84 (42.29–43.40) | 2.97 (2.79–3.17) | 44.79 (44.23–45.35) | 1.03 (0.92–1.15) |
| 5–<10 (N=21 241) | 67.42 (66.78–68.05) | 59.97 (59.31–60.63) | 7.44 (7.09–7.80) | 64.20 (63.55–64.85) | 3.22 (2.98–3.46) |
| 10–<20 (N=24 609) | 85.56 (85.12–86.00) | 68.71 (68.13–69.29) | 16.85 (16.38–17.32) | 74.90 (74.35–75.44) | 10.67 (10.28–11.06) |
| ≥20 (N=21 394) | 92.59 (92.23–92.93) | 82.14 (81.62–82.65) | 10.45 (10.04–10.86) | 88.04 (87.60–88.48) | 4.54 (4.27–4.83) |
| History of CVD (N=2 585 483) | 85.82 (85.78–85.87) | 75.72 (75.67–75.77) | 10.10 (10.07–10.14) | 79.33 (79.28–79.38) | 6.49 (6.46–6.52) |
Proportions and 95% Clopper‐Pearson (exact) CIs were reported. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; and PINNACLE, Practice Innovation and Clinical Excellence.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/ Pacific Islander.
Baseline characteristics of individuals recommended antihypertensive therapy according to the 2017 ACC/AHA guideline, the 2014 expert panel report, and the JNC7 are shown in Table 5. Individuals recommended antihypertensive therapy according to the 2017 ACC/AHA guideline alone were more likely to be older, to be men, to be White race, to have less CKD, and to have a 10‐year predicted ASCVD risk of 10% to <20% compared with counterparts in other risk categories.
Table 5.
Baseline Characteristics of US Adults Recommended Antihypertensive Medication According to the ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Characteristics | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Total No. | 4 266 118 | 3 734 134 | 531 984 | 3 983 633 | 282 485 |
| Age, y | |||||
| Mean±SD | 66.5±13.8 | 66.3±13.9 | 68.1±12.6 | 66.3±13.8 | 68.5±12.7 |
| Median (Q1–Q3) | 68.0 (58.0–76.0) | 67.0 (58.0–76.0) | 69.0 (62.0–77.0) | 68.0 (58.0–76.0) | 70.0 (63.0–77.0) |
| Range (minimum–maximum) | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 |
| 18–44 | 6.9 | 7.2 | 5.1 | 7.1 | 5.1 |
| 45–54 | 11.5 | 11.9 | 8.3 | 11.7 | 8.4 |
| 55–64 | 21.5 | 22.0 | 17.8 | 22.0 | 14.5 |
| 65–74 | 30.3 | 29.3 | 37.8 | 29.7 | 40.1 |
| ≥75 | 29.8 | 29.6 | 30.9 | 29.6 | 32.0 |
| Sex | |||||
| Men | 50.9 | 51.0 | 50.0 | 50.8 | 51.3 |
| Women | 49.1 | 49.0 | 50.0 | 49.2 | 48.7 |
| Race | |||||
| White | 64.1 | 63.4 | 69.1 | 63.7 | 69.2 |
| Black | 7.5 | 7.7 | 6.3 | 7.7 | 4.9 |
| Other * | 0.5 | 0.5 | 0.4 | 0.5 | 0.3 |
| Missing | 27.9 | 28.4 | 24.2 | 28.1 | 25.6 |
| History of stroke/TIA | 12.0 | 11.9 | 12.1 | 11.8 | 14.8 |
| History of stroke | 9.3 | 9.3 | 10.0 | 9.1 | 12.8 |
| History of TIA | 3.7 | 3.8 | 3.2 | 3.7 | 3.3 |
| Coronary artery disease | 41.6 | 42.3 | 36.8 | 41.5 | 42.9 |
| History of MI | 9.9 | 10.3 | 7.6 | 10.0 | 9.4 |
| History of PCI | 14.2 | 14.6 | 11.3 | 14.3 | 12.8 |
| History of CABG | 7.1 | 7.4 | 4.9 | 7.2 | 5.2 |
| Diabetes | 24.0 | 24.1 | 23.1 | 25.7 | 0.0 |
| Chronic kidney disease | 4.2 | 4.5 | 2.7 | 4.5 | 0.0 |
| Heart failure | 16.4 | 16.7 | 14.0 | 16.4 | 16.5 |
| 10‐y Predicted ASCVD risk, % | |||||
| Mean±SD (N) | 15.5±12.3 (69 294) | 15.5±12.6 (60 416) | 15.3±9.2 (8878) | 15.5±12.5 (64 697) | 14.7±7.1 (4597) |
| Median (Q1–Q3) | 12.4 (6.1–21.7) | 12.1 (5.7–22.0) | 13.6 (9.0–20.1) | 12.2 (5.8–22.0) | 13.6 (10.3–18.9) |
| Range (minimum–maximum) | 0.1–95.1 | 0.1–95.1 | 0.2–86.8 | 0.1–95.1 | 0.2–56.2 |
| <5 | 20.4 | 21.8 | 10.3 | 21.3 | 6.9 |
| 5–<10 | 20.7 | 21.1 | 17.8 | 21.1 | 14.9 |
| 10–<20 | 30.4 | 28.0 | 46.7 | 28.5 | 57.1 |
| ≥20 | 28.6 | 29.1 | 25.2 | 29.1 | 21.1 |
| History of CVD | 52.0 | 52.4 | 49.1 | 51.5 | 59.4 |
Data are given as percentages, unless otherwise indicated. Please note that all adults with hypertension, according to the 2014 expert panel member report definition of hypertension, are recommended treatment with antihypertensive medications. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; CABG, coronary artery bypass grafting; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; MI, myocardial infarction; PCI, percutaneous coronary intervention; PINNACLE, Practice Innovation and Clinical Excellence; Q1, quartile 1; Q3, quartile 3; and TIA, transient ischemic attack.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/ Pacific Islander.
Achievement of BP Treatment Goals According to Different Guidelines
Among the patients taking antihypertensive medication, 41.2%, 79.4%, and 64.3% of patients achieved BP targets per the 2017 ACC/AHA guideline, the 2014 expert panel report, and the JNC7, respectively (Figure 2 and Table 6). Similar trend was observed in additional sensitivity analysis, including only visits for each in which they were on antihypertensive therapy, where 41.6%, 79.8%, and 64.3% of patients achieved BP targets per the 2017 ACC/AHA guideline, the 2014 expert panel report, and the JNC7, respectively (Table S3).
Table 6.
Percentage of US Adults, Overall and in Selected Subgroups, Taking Antihypertensive Medication Who Meet BP Treatment Goal per ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Subgroups | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Overall (N=3 405 189) | 41.24 (41.19–41.30) | 79.41 (79.36–79.45) | 38.16 (38.11–38.21) | 64.30 (64.25–64.35) | 23.06 (23.01–23.10) |
| Age group, y | |||||
| 18–44 (N=205 638) | 39.64 (39.43–39.86) | 73.46 (73.27–73.65) | 33.81 (33.61–34.02) | 67.96 (67.76–68.16) | 28.32 (28.12–28.51) |
| 45–54 (N=376 824) | 37.03 (36.88–37.19) | 72.52 (72.38–72.66) | 35.49 (35.34–35.64) | 64.56 (64.41–64.72) | 27.53 (27.39–27.67) |
| 55–64 (N=742 428) | 39.34 (39.23–39.45) | 77.31 (77.21–77.40) | 37.97 (37.86–38.08) | 63.97 (63.86–64.08) | 24.63 (24.53–24.73) |
| 65–74 (N=1 027 950) | 41.38 (41.29–41.48) | 81.68 (81.60–81.75) | 40.29 (40.20–40.39) | 63.40 (63.30–63.49) | 22.01 (21.93–22.09) |
| ≥75 (N=1 052 349) | 44.27 (44.18–44.37) | 82.30 (82.22–82.37) | 38.03 (37.93–38.12) | 64.61 (64.52–64.70) | 20.34 (20.26–20.42) |
| Men (N=1 747 780) | 42.15 (42.07–42.22%) | 79.88 (79.82–79.94) | 37.73 (37.66–37.81) | 65.10 (65.03–65.17) | 22.96 (22.89–23.02) |
| Women (N=1 654 071) | 40.29 (40.21–40.36) | 78.90 (78.84–78.96) | 38.61 (38.54–38.69) | 63.46 (63.38–63.53) | 23.17 (23.10–23.23) |
| Race and ethnicity | |||||
| White (N=2 150 367) | 42.35 (42.28–42.41) | 80.86 (80.81–80.91) | 38.51 (38.45–38.58) | 65.74 (65.67–65.80) | 23.39 (23.33–23.44) |
| Black (N=250 690) | 30.38 (30.20–30.56) | 67.57 (67.39–67.75) | 37.19 (37.00–37.38) | 51.31 (51.12–51.51) | 20.93 (20.77–21.09) |
| Other * (N=16 685) | 41.14 (40.40–41.90) | 76.82 (76.17–77.46) | 35.67 (34.95–36.41) | 61.07 (60.33–61.81) | 19.93 (19.32–20.54) |
| Hispanic (N=145 086) | 39.08 (38.83–39.33) | 76.43 (76.21–76.64) | 37.34 (37.10–37.59) | 59.67 (59.42–59.92) | 20.59 (20.38–20.80) |
| Non‐Hispanic (N=3 260 103) | 41.34 (41.29–41.39) | 79.54 (79.50–79.58) | 38.20 (38.15–38.25) | 64.51 (64.46–64.56) | 23.17 (23.12–23.21) |
| 10‐y ASCVD risk categories, % | |||||
| <5 (N=11 128) | 42.57 (41.65–43.49) | 79.46 (78.69–80.20) | 36.89 (35.99–37.79) | 75.66 (74.85–76.45) | 33.09 (32.21–33.97) |
| 5–<10 (N=11 207) | 37.06 (36.16–37.96) | 77.43 (76.65–78.20) | 40.38 (39.47–41.29) | 67.90 (67.02–68.76) | 30.84 (29.98–31.70) |
| 10–<20 (N=15 449) | 34.91 (34.16–35.67) | 76.20 (75.52–76.87) | 41.28 (40.51–42.07) | 60.11 (59.33–60.88) | 25.19 (24.51–25.88) |
| ≥20 (N=16 053) | 26.82 (26.14–27.52) | 67.28 (66.55–68.00) | 40.45 (39.69–41.22) | 42.85 (42.08–43.62) | 16.02 (15.46–16.60) |
| History of CVD (N=1 896 465) | 44.47 (44.40–44.54) | 81.26 (81.21–81.32) | 36.79 (36.72–36.86) | 65.57 (65.51–65.64) | 21.10 (21.05–21.16) |
Proportions and 95% Clopper‐Pearson (exact) CIs were reported. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; BP, blood pressure; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; and PINNACLE, Practice Innovation and Clinical Excellence.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/ Pacific Islander.
When stratified by age, sex, and race and ethnicity, the percentage of patients reaching BP targets per the ACC/AHA guideline was higher among men, White race, and those with prevalent CVD compared with the overall population (Figure 3A through 3F). Among the ASCVD risk subgroups, the proportion of patients who achieved BP targets was highest for those with a 10‐year ASCVD risk <5%, and BP control decreased as 10‐year ASCVD risk increased (Figure 3E). Similar trend was observed in sensitivity analysis, including only visits when patients were on antihypertensive therapy (Table S4).
Baseline characteristics of patients who achieved their target BP according to the 2017 ACC/AHA guideline, 2014 expert panel report, and JNC7 are shown in Table 7. Patients were comparable in terms of ASCVD risk and prevalence of diabetes, CKD, and CVD. Patients achieving their BP targets according to the 2014 expert panel report and JNC7 but not the 2017 ACC/AHA guideline were more likely to be middle‐aged (aged 45–64 years), women, and Black race, and less likely to have CAD, stroke/transient ischemic attack, or HF.
Table 7.
Baseline Characteristics of US Adults Taking Antihypertensive Medication Who Meet BP Treatment Goal per ACC/AHA Guideline, 2014 Expert Panel Report, and JNC7 Based on the 2013 to 2016 PINNACLE Registry Data
| Characteristics | ACC/AHA guideline | 2014 Report | Difference between ACC/AHA guideline and 2014 report | JNC7 | Difference between ACC/AHA guideline and JNC7 |
|---|---|---|---|---|---|
| Total No. | 1 404 435 | 2 703 939 | 1 299 504 | 2 189 612 | 785 177 |
| Age, y | |||||
| Mean±SD | 67.7±13.7 | 67.6±13.4 | 67.4±13.0 | 67.0±13.7 | 68.5±13.8 |
| Median (Q1–Q3) | 69.0 (60.0–78.0) | 69.0 (60.0–77.0) | 69.0 (60.0–77.0) | 69.0 (58.0–77.0) | 67.0 (57.0–75.0) |
| Range (minimum–maximum) | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 | 18.0–100.0 |
| 18–44 | 5.8 | 5.6 | 5.4 | 6.4 | 7.4 |
| 45–54 | 9.9 | 10.1 | 10.3 | 11.1 | 13.2 |
| 55–64 | 20.8 | 21.2 | 21.7 | 21.7 | 23.3 |
| 65–74 | 30.3 | 31.1 | 31.9 | 29.8 | 28.8 |
| ≥75 | 33.2 | 32.0 | 30.8 | 31.1 | 27.3 |
| Sex | |||||
| Men | 52.5 | 51.7 | 50.8 | 52.0 | 51.1 |
| Women | 47.5 | 48.3 | 49.2 | 48.0 | 48.9 |
| Race | |||||
| White | 64.8 | 64.3 | 63.7 | 64.6 | 64.1 |
| Black | 5.4 | 6.3 | 7.2 | 5.9 | 6.7 |
| Other * | 0.5 | 0.5 | 0.5 | 0.5 | 0.4 |
| Missing | 29.2 | 29.0 | 28.6 | 29.1 | 28.8 |
| History of stroke/TIA | 12.7 | 12.5 | 12.2 | 12.1 | 11.1 |
| History of stroke | 9.8 | 9.6 | 9.4 | 9.4 | 8.6 |
| History of TIA | 4.0 | 3.9 | 3.9 | 3.8 | 3.4 |
| Coronary artery disease | 49.1 | 46.4 | 43.4 | 46.1 | 40.7 |
| History of MI | 13.2 | 11.8 | 10.3 | 12.1 | 10.3 |
| History of PCI | 17.5 | 16.3 | 15.0 | 16.2 | 14.0 |
| History of CABG | 9.3 | 8.4 | 7.4 | 8.2 | 6.3 |
| Diabetes | 23.9 | 21.6 | 19.1 | 15.3 | 0.0 |
| Chronic kidney disease | 4.7 | 4.0 | 3.3 | 3.0 | 0.0 |
| Heart failure | 21.5 | 18.9 | 16.0 | 19.2 | 14.9 |
| 10‐y Predicted ASCVD risk, % | |||||
| Mean±SD (N) | 13.3±10.8 (18 590) | 14.6±11.4 (40 092) | 15.6±11.7 (21 502) | 12.7±10.1 (32 192) | 11.9±9.1 (13 602) |
| Median (Q1–Q3) | 10.6 (4.9–19.1) | 11.8 (5.6–20.9) | 12.8 (6.4–22.4) | 10.1 (4.8–18,3) | 9.4 (4.7–17.1) |
| Range (minimum–maximum) | 0.1–80.7 | 0.1–80.7 | 0.1–72.2 | 0.1–80.7 | 0.1–63.1 |
| <5 | 25.5 | 22.1 | 19.1 | 26.2 | 27.1 |
| 5–<10 | 22.3 | 21.6 | 21.0 | 23.6 | 25.4 |
| 10–<20 | 29.0 | 29.4 | 29.7 | 28.8 | 28.6 |
| ≥20 | 23.2 | 26.9 | 30.2 | 21.4 | 18.9 |
| History of CVD | 60.1 | 57.0 | 53.7 | 56.8 | 51.0 |
Proportions and 95% Clopper‐Pearson (exact) CIs were reported. ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic CVD; BP, blood pressure; CABG, coronary artery bypass grafting; CVD, cardiovascular disease; JNC7, Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; MI, myocardial infarction; PCI, percutaneous coronary intervention; PINNACLE, Practice Innovation and Clinical Excellence; Q1, quartile 1; Q3, quartile 3; and TIA, transient ischemic attack.
*Defined as combination of any race other than White or Black, including Asian, American Indian/Alaskan Native, Native Hawaiin/ Pacific Islander.
Median practice‐level difference in the proportion of patients meeting their BP target according to the 2014 panel but not the 2017 ACC/AHA guideline was 37.8% (interquartile range, 34.8%–40.7%) (Figure 4). The practice‐level rates ranged widely, with several practices having <20% of patients with hypertension meeting BP goals per the 2014 panel report but not the 2017 ACC/AHA guideline and few having a >50% difference. Most practices demonstrated a difference of around 30% to 40%.
Figure 4. Differences in the proportion of patients meeting blood pressure (BP) targets as per 2014 expert panel report but not as per American College of Cardiology (ACC)/American Heart Association (AHA) guideline across participating practices in the PINNACLE (Practice Innovation and Clinical Excellence) Registry.
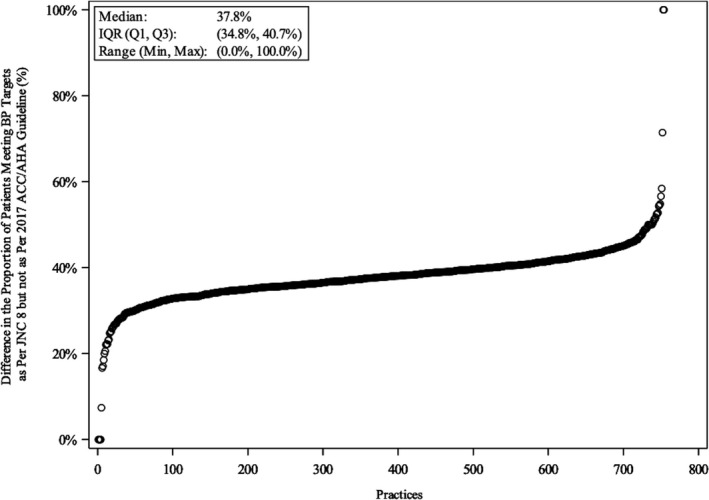
The x axis shows random practice identifier; the y axis shows difference in the proportion of patients meeting BP target per 2014 expert panel report but not ACC/AHA guidelines. IQR indicates interquartile range; JNC8, Eighth Joint National Committee; Max, maximum; Min, minimum; Q1, quartile 1; and Q3, quartile 3.
Similarly, the median practice‐level rate in the proportion of patients with hypertension meeting BP targets according to the JNC7 but not the 2017 ACC/AHA guideline was 22.9% (interquartile range, 19.8%–25.9%) (Figure 5).
Figure 5. Difference in the proportion of patients meeting blood pressure (BP) targets as per Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) but not as per American College of Cardiology (ACC)/American Heart Association (AHA) guideline across participating practices in the PINNACLE (Practice Innovation and Clinical Excellence) Registry.
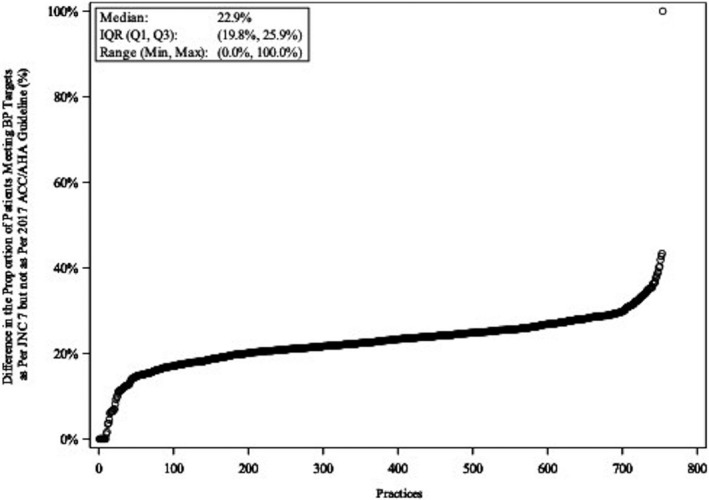
The x axis shows random practice identifier; the y axis shows difference in the proportion of patients meeting BP target per JNC7 but not ACC/AHA guidelines. IQR indicates interquartile range; Max, maximum; Min, minimum; Q1, quartile 1; Q3, quartile 3.
Discussion
These analyses from the ACC's NCDR PINNACLE Registry demonstrate that application of the 2017 ACC/AHA guideline recommendations in a cohort of patients treated at cardiology practices resulted in 83.2% of patients meeting criteria for hypertension, 70.6% being recommended antihypertensive medication, and 41.2% achieving their BP goal before the publication and uptake of the 2017 guidelines into cardiology practices (Figure 2). Compared with the criteria put forth in the 2014 expert panel report and JNC7, there is a significant increase in the prevalence of hypertension and the proportion of patients needing antihypertensive therapy. Moreover, there was an absolute decrease of 38.2% and 23.1% in the proportion of patients taking antihypertensive treatment who achieved the 2017 ACC/AHA guideline‐recommended BP goal compared with the 2014 expert panel report and JNC7, respectively. Women, patients belonging to underrepresented racial and ethnic groups, and those with higher 10‐year ASCVD risk demonstrated the lowest degree of BP control. Finally, there was significant practice‐level variation in BP control. Collectively, these findings underscore a greater need to identify patients with hypertension and to initiate lifestyle changes and treatment approaches to be guideline concordant.
Compared with the prior 2014 expert panel report and JNC7, there was an absolute increase in the prevalence of hypertension by about 8% Much of the increase in the prevalence of hypertension stems from adults with a systolic BP of 130 to 139 mm Hg or a diastolic BP of 80 to 89 mm Hg (stage 1 hypertension), consistent with findings from other US and international studies. 4 , 14 , 15 , 16 , 17 , 18 , 19 The largest increase in hypertension was noted in young patients referred to cardiology practices with low cardiovascular risk (ie, 10‐year predicted CVD risk <10%) and without CKD, diabetes, CAD, and HF. A substantial proportion of these individuals would not be recommended drug therapy outright based on their lower baseline cardiovascular risk. 20 , 21 , 22 Correspondingly, we observed a smaller increase in number warranting antihypertensive therapy. Therefore, the application of the 2017 ACC/AHA guideline provides an opportunity to discuss and implement healthy nonpharmacological lifestyle interventions, such as weight loss, a healthy diet, sodium restriction, physical activity, and moderation in alcohol consumption, particularly in those who are young and relatively healthy, but with hypertension.
Failure to achieve BP targets has been a common issue based on prior BP goals; however, with the 2017 ACC/AHA guideline, BP control was lower. About 60% of patients on antihypertensive therapy did not achieve their BP goal per the 2017 ACC/AHA guideline. Lack of BP control was most pronounced in women, Black and Hispanic individuals, and those with higher CVD risk. Previous studies have shown that women have consistently lower BPs compared with men of the same age group. 23 In this analysis, women were less likely to achieve their BP goal. The difference in awareness and behavior of both patients and clinicians 24 may explain this sex disparity. Women are less likely to recognize CVD and CVD risk factors as a health problem, 25 with Hispanic women demonstrating lower hypertension awareness than their Black or White counterparts. Clinicians are also less likely to identify and diagnose CVD and CVD risk factors in women, 26 , 27 and women with CVD or CVD risk factors are less likely to receive guideline‐recommended preventive therapies because of therapeutic inertia. 27 , 28 , 29 , 30
We also observed significant differences in hypertension management based on race and ethnicity, with a lower proportion of Black and Hispanic patients achieving their BP goal. A previous study from the US National Health and Nutrition Examination Survey also highlighted similar differences, with lower BP control rates in non‐Hispanic Black, non‐Hispanic Asian, and Hispanic adults compared with non‐Hispanic White adults. 31 Causes of racial and ethnic disparities are multifactorial and, in part, relate to insurance coverage and access to health care, socioeconomic status, patient‐provider communication, and medication adherence. 32 , 33 In addition, the 2017 ACC/AHA guideline recommends the use of the PCE to estimate 10‐year cardiovascular risk. Because the PCE calculation attributes higher risk to Black than White individuals in its calculation, more Black individuals will have higher 10‐year cardiovascular risk scores and with a BP of 130 to 139/80 to 89 mm Hg will be in need of pharmacotherapy. On the other hand, the PCE may underestimate risk for certain races and ethnicities, including some Asian Americans (eg, South Asian ancestry), American Indians/Alaska Natives, and some Hispanics (eg, Puerto Ricans), 34 potentially resulting in underuse of antihypertensive therapy in these populations. Taken together, the clinically important differences in BP treatment and control among different sexes and races and ethnicities highlighted in our study may in fact be markers of true health disparities that could have important downstream effects, including a higher risk of stroke, myocardial infarction, and renal failure in these specific population groups.
Many practical issues and challenges may limit the widespread implementation of guideline recommendations, accounting for the lack of hypertension control, and substantial practice‐level variation seen in this registry. Globally, a considerable proportion of adults with hypertension are either unaware of their diagnosis or do not achieve BP control per previous guideline recommendations. 35 , 36 , 37 , 38 In our study, more than one third of patients with hypertension did not achieve their BP goal, as defined by the JNC7 criteria. Application of the 2017 ACC/AHA guideline recommendations will result in significant up‐front health care costs to care for the substantially greater number of hypertensive patients, but potentially lower long‐term costs with reduced cardiovascular complications.
Second, the disproportionate increase in people diagnosed with hypertension compared with those recommended antihypertensive therapies 5 , 14 will require a greater emphasis on lifestyle modification to achieve BP reduction. Cardiology practices across the United States need a coordinated effort and multidisciplinary approach to achieve improved hypertension treatment and control. Doing so will most certainly require more time and resources, which may deter the implementation of recommendations in the 2017 ACC/AHA guideline. Moreover, the uneven distribution of patients meeting BP targets across practices seen in our study is likely to result in significant variation in the quality of care if more stringent BP targets were to be approved as performance measures or quality metrics.
The 2017 ACC/AHA guideline, however, may serve as a wake‐up call to identify patients not meeting BP goals. Although perfect attainment of these goals on a population level will never be achievable, recognition of more patients being further from their goals may spur greater lifestyle and pharmacologic efforts in appropriate patients to control BP.
Study Limitations
First, our study population has selected to be seen in outpatient US cardiology practices that participate in the PINNACLE Registry. Accordingly, a higher proportion of patients in our study have cardiovascular comorbidities and, consequently, hypertension compared with the general population. 39 This limits the generalizability of these findings to primary care setting and requires future studies in different cohorts. Second, the results were based on data between 2013 and 2016, which reflects a time before guideline changes and may predate broad uptake into practice. Third, use of average BP values derived from multiple measurements in registry visits may not be accurate to arrive at a clinical diagnosis of hypertension as defined by the guidelines, beyond patients who have a documented diagnosis or are on antihypertensive treatment. However, these may be sufficient to highlight between‐group differences but not to estimate prevalence of hypertension or antihypertensive therapy within the cohort. Furthermore, BP measurement protocols were not standardized across practices and, as such, may account for variability in the measurement of BP.
In addition, assessment of the proportion of patients achieving their BP goal based on an average BP measurement of all visits over a 2‐year period does not reflect real‐life practice. Because some may have been initiated on pharmacotherapy on follow‐up, we may have underestimated BP control. Last, our study assessed outpatient care for patients receiving care in cardiology practices enrolled in the PINNACLE Registry. These results, therefore, may not apply to other cardiology or primary care practices.
Conclusions
In conclusion, our study illustrates that implementation of the 2017 ACC/AHA hypertension guideline results in a substantially increased number of adults referred to cardiology practices meeting criteria for hypertension, particularly among young patients with low cardiovascular risk and without history of diabetes, CKD, and CAD. The increase in number of individuals likely to be recommended antihypertensive therapy from the outset will be smaller, as pharmacological treatment is reserved for those with higher ASCVD risk. Moreover, based on this cross‐sectional analysis predating the 2017 ACC/AHA guideline, a substantially higher proportion of adults are at risk of being short of the more intensive BP goal set by the 2017 guideline. This was most pronounced in women, underrepresented races and ethnicities, and those with higher ASCVD risk. Outreach efforts should be targeted at the practice level, given the significant practice‐level variation observed in the proportion of patients meeting BP targets.
Sources of Funding
This research was supported by the American College of Cardiology Foundation’s NCDR (National Cardiovascular Data Registry). The views expressed in this article represent those of the authors and do not necessarily represent the official views of the NCDR or its associated professional societies identified at http://www.ncdr.com. Dr Virani has grant support from: Department of Veterans Affairs, World Health Federation, Tahir, and Jooma Family. Dr Maddox discloses current grant funding from the National Institutes of Health National Center for Advancing Translational Sciences (1u24tr002306‐01: A National Center for Digital Health Informatics Innovation).
Disclosures
Dr Virani receives honorarium from the America College of Cardiology (Associate Editor for the Innovations, acc.org). Dr Masoudi has a contract with the American College of Cardiology for his role as Chief Scientific Advisor, NCDR (National Cardiovascular Data Registry). Dr Maddox receives honoraria and/or expense reimbursement in the past 3 years from the Henry Ford health system (March 2019), the University of California San Diego (January 2020), the University of Chicago (January 2021), and George Washington University (January 2021). He has also received compensation and travel expense reimbursement for American College of Cardiology leadership roles and meetings. He is currently employed as a cardiologist and the executive director of the Healthcare Innovation Lab at BJC HealthCare/Washington University School of Medicine. In this capacity, he is advising Myia Labs, for which his employer is receiving equity compensation in the company. He is receiving no individual compensation from the company. He is also a compensated director for a New Mexico–based foundation, the J.F. Maddox Foundation. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S4
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.024107
For Sources of Funding and Disclosures, see page 16.
References
- 1. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;19:2199–2269. doi: 10.1016/j.jacc.2017.11.005 [DOI] [PubMed] [Google Scholar]
- 2. James PA, Oparil S, Carter BL, Cushman WC, Dennison‐Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 Evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427 [DOI] [PubMed] [Google Scholar]
- 3. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al.; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 4. SPRINT Research Group , Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, Whelton PK. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–118. doi: 10.1161/CIRCULATIONAHA.117.032582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Masoudi FA, Ponirakis A, Yeh RW, Maddox TM, Beachy J, Casale PN, Curtis JP, De Lemos J, Fonarow G, Heidenreich P, et al. Cardiovascular care facts: a report from the National Cardiovascular Data Registry: 2011. J Am Coll Cardiol. 2013;62:1931–1947. doi: 10.1016/j.jacc.2013.05.099 [DOI] [PubMed] [Google Scholar]
- 7. Masoudi FA, Ponirakis A, de Lemos JA, Jollis JG, Kremers M, Messenger JC, Moore JWM, Moussa I, Oetgen WJ, Varosy PD, et al. Trends in U.S. cardiovascular care: 2016 report from 4 ACC national cardiovascular data registries. J Am Coll Cardiol. 2017;69:1427–1450. doi: 10.1016/j.jacc.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 8. Chan PS, Oetgen WJ, Buchanan D, Mitchell K, Fiocchi FF, Tang F, Jones PG, Breeding T, Thrutchley D, Rumsfeld JS, et al. Cardiac performance measure compliance in outpatients: the American College of Cardiology and National Cardiovascular Data Registry's PINNACLE Program™. J Am Coll Cardiol. 2010;56:8–14. doi: 10.1016/j.jacc.2010.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Messenger JC, Ho KKL, Young CH, Slattery LE, Draoui JC, Curtis JP, Dehmer GJ, Grover FL, Mirro MJ, Reynolds MR, et al. The National Cardiovascular Data Registry (NCDR) data quality brief: the NCDR data quality program in 2012. J Am Coll Cardiol. 2012;60:1484–1488. doi: 10.1016/j.jacc.2012.07.020 [DOI] [PubMed] [Google Scholar]
- 10. Masoudi FA, Ponirakis A, Yeh RW, Maddox TM, Beachy J, Casale PN, Curtis JP, De Lemos J, Fonarow G, Heidenreich P, et al. Cardiovascular care facts: a report from the National Cardiovascular Data Registry: 2011. J Am Coll Cardiol. 2013;62:1931–1947. doi: 10.1016/j.jacc.2013.05.09 [DOI] [PubMed] [Google Scholar]
- 11. American College of Cardiology Foundation/American Heart Association/American Medical Association–Physician Consortium for Performance Improvement (2005) Clinical performance measures. Chronic stable coronary artery disease (American Medical Association, Chicago, IL) Available at: http://www.metcare.com/_pdf/cadmeasures.pdf. Accessed December 15, 2020
- 12. Bonow RO, Bennett S, Casey DE, Ganiats TG, Hlatky MA, Konstam MA, Lambrew CT, Normand S‐L, Piña IL, Radford MJ, et al. ACC/AHA clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on performance measures endorsed by the Heart Failure Society of America. J Am Coll Cardiol. 2005;46:1144–1178. doi: 10.1016/j.jacc.2005.07.012 [DOI] [PubMed] [Google Scholar]
- 13. Estes NAM III, Halperin JL, Calkins H, Ezekowitz MD, Gitman P, Go AS, McNamara RL, Messer JV, Ritchie JL, Romeo SJW, et al. ACC/AHA/physician consortium 2008 clinical performance measures for adults with nonvalvular atrial fibrillation or atrial flutter: a report of the American College of Cardiology/American Heart Association Task Force on performance measures and the physician consortium for performance improvement developed in collaboration with the heart rhythm society. J Am Coll Cardiol. 2008;51:865–884. doi: 10.1016/j.jacc.2008.01.006 [DOI] [PubMed] [Google Scholar]
- 14. Lee JH, Kim S‐H, Kang S‐H, Cho JH, Cho Y, Oh I‐Y, Yoon C‐H, Lee H‐Y, Youn T‐J, Chae I‐H, et al. Blood pressure control and cardiovascular outcomes: real‐world implications of the 2017 ACC/AHA hypertension guideline. Sci Rep. 2018;8:13155. doi: 10.1038/s41598-018-31549-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khera R, Lu Y, Lu J, Saxena A, Nasir K, Jiang L, Krumholz HM. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018;362:k2357. doi: 10.1136/bmj.k2357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Venkateshmurthy NS, Geldsetzer P, Jaacks LM, Prabhakaran D. Implications of the New American College of Cardiology guidelines for hypertension prevalence in India. JAMA Intern Med. 2018;178:1416–1418. doi: 10.1001/jamainternmed.2018.3511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kibria GMA, Swasey K, Choudhury A, Burrowes V, Stafford KA, Uddin SMI, Mirbolouk M, Sharmeen A, Kc A, Mitra DK. The new 2017 ACC/AHA guideline for classification of hypertension: changes in prevalence of hypertension among adults in Bangladesh. J Hum Hypertens. 2018;32:608–616. doi: 10.1038/s41371-018-0080-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sarganas G, Knopf H, Grams D, Neuhauser HK. Trends in antihypertensive medication use and blood pressure control among adults with hypertension in Germany. Am J Hypertens. 2016;29:104–113. doi: 10.1093/ajh/hpv067 [DOI] [PubMed] [Google Scholar]
- 19. Harrap SB, Lung T, Chalmers J. New blood pressure guidelines pose difficult choices for Australian physicians. Circ Res. 2019;124:975–977. doi: 10.1161/CIRCRESAHA.118.314637 [DOI] [PubMed] [Google Scholar]
- 20. Lonn EM, Bosch J, López‐Jaramillo P, Zhu J, Liu L, Pais P, Diaz R, Xavier D, Sliwa K, Dans A, et al. Blood‐pressure lowering in intermediate‐risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–2020. doi: 10.1056/NEJMoa1600175 [DOI] [PubMed] [Google Scholar]
- 21. ACCORD Study Group , Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons‐Morton DG, Basile JN, Corson MA, et al. Effects of intensive blood‐pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Diao D, Wright JM, Cundiff DK, Gueyffier F. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev. 2012:CD006742. doi: 10.1002/14651858.CD006742.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Everett B, Zajacova A. Gender differences in hypertension and hypertension awareness among young adults. Biodemography Soc Biol. 2015;61:1–17. doi: 10.1080/19485565.2014.929488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gulati M. Improving the cardiovascular health of women in the nation: moving beyond the bikini boundaries. Circulation. 2017;135:495–498. doi: 10.1161/CIRCULATIONAHA.116.025303 [DOI] [PubMed] [Google Scholar]
- 25. Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, Burdick KA, Simpson SL. National study of women's awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. doi: 10.1161/CIRCULATIONAHA.105.588103 [DOI] [PubMed] [Google Scholar]
- 26. Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Fabunmi RP, Kwan J, Mills T, Simpson SL. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111:499–510. doi: 10.1161/01.CIR.0000154568.43333.82 [DOI] [PubMed] [Google Scholar]
- 27. McSweeney JC, Rosenfeld AG, Abel WM, Braun LT, Burke LE, Daugherty SL, Fletcher GF, Gulati M, Mehta LS, Pettey C, et al. Preventing and experiencing ischemic heart disease as a woman: state of the science: a scientific statement from the American Heart Association. Circulation. 2016;133:1302–1331. doi: 10.1161/CIR.0000000000000381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex disparities in treatment of cardiac risk factors in patients with type 2 diabetes. Diabetes Care. 2005;28:514–520. doi: 10.2337/diacare.28.3.514 [DOI] [PubMed] [Google Scholar]
- 29. Mosca L, Merz NB, Blumenthal RS, Cziraky MJ, Fabunmi RP, Sarawate C, Watson KE, Willey VJ, Stanek EJ. Opportunity for intervention to achieve American Heart Association guidelines for optimal lipid levels in high‐risk women in a managed care setting. Circulation. 2005;111:488–493. doi: 10.1161/01.CIR.0000153859.66086.85 [DOI] [PubMed] [Google Scholar]
- 30. McLaughlin TJ, Soumerai SB, Willison DJ, Gurwitz JH, Borbas C, Guadagnoli E, McLaughlin B, Morris N, Cheng SC, Hauptman PJ, et al. Adherence to national guidelines for drug treatment of suspected acute myocardial infarction: evidence for undertreatment in women and the elderly. Arch Intern Med. 1996;156:799–805. doi: 10.1001/archinte.1996.00440070131015 [DOI] [PubMed] [Google Scholar]
- 31. Gu A, Yue Y, Desai RP, Argulian E. Racial and ethnic differences in antihypertensive medication use and blood pressure control among US adults with hypertension: the National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10:e003166. doi: 10.1161/CIRCOUTCOMES.116.003166 [DOI] [PubMed] [Google Scholar]
- 32. Ritchey M, Chang A, Powers C, Loustalot F, Schieb L, Ketcham M, Durthaler J, Hong Y. Vital signs: disparities in antihypertensive medication nonadherence among Medicare part D beneficiaries—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65:967–976. doi: 10.15585/mmwr.mm6536e1 [DOI] [PubMed] [Google Scholar]
- 33. Ferdinand KC, Yadav K, Nasser SA, Clayton‐Jeter HD, Lewin J, Cryer DR, Senatore FF. Disparities in hypertension and cardiovascular disease in blacks: the critical role of medication adherence. J Clin Hypertens. 2017;19:1015–1024. doi: 10.1111/jch.13089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. DeFilippis AP, Young R, Carrubba CJ, McEvoy JW, Budoff MJ, Blumenthal RS, Kronmal RA, McClelland RL, Nasir K, Blaha MJ. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med. 2015;162:266–275. doi: 10.7326/M14-1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, Cheng X, Mu L, Zhang H, Liu J, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population‐based screening study. Lancet. 2017;390:2549–2558. doi: 10.1016/S0140-6736(17)32478-9 [DOI] [PubMed] [Google Scholar]
- 36. Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. doi: 10.1056/NEJMoa010273 [DOI] [PubMed] [Google Scholar]
- 37. Chockalingam A. Impact of world hypertension day. Can J Cardiol. 2007;23:517–519. doi: 10.1016/S0828-282X(07)70795-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650 [DOI] [PubMed] [Google Scholar]
- 39. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, et al.; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4


