Abstract
Background
The long‐term impact of fenestration at the time of Fontan operation remains unclear. We aimed to review the early and long‐term impact of Fontan fenestration in the Australia and New Zealand cohort.
Methods and Results
We reviewed 1443 patients (621 fenestrated, 822 nonfenestrated) from the Australia and New Zealand Fontan registry. Data were collected on preoperative demographics, operative details, and follow‐up. Propensity‐score matching was performed to account for the various preoperative and operative differences and risk factors. Primary outcomes were survival and freedom from failure. Median follow‐up was 10.6 years. After propensity‐score matching (407 matched pairs), there was no difference in survival (87% versus 90% at 20 years; P=0.16) or freedom from failure (73% versus 80% at 20 years; P=0.10) between patients with and without fenestration, respectively. Although patients with fenestration had longer bypass and cross‐clamp times (P<0.001), there was no difference in hospital length of stay or prolonged pleural effusions (P=0.80 and P=0.46, respectively). Freedom from systemic and Fontan circuit thromboembolism was higher in the nonfenestrated group (89%; 95% CI, 88%–95%) than the fenestrated group (84%; 95% CI, 77%–89%; P=0.03). There was no difference in incidence of plastic bronchitis, protein‐losing enteropathy, New York Heart Association Class III/IV symptoms, or Fontan takedown.
Conclusions
In the propensity score–matched analysis we have demonstrated no difference in long‐term survival or freedom from Fontan failure in patients with and without fenestration. There was a higher incidence of long‐term thromboembolic events in patients with fenestration. Overall, it appears that fenestration in Fontan circulation does not bring long‐term benefits.
Keywords: fenestration, risk factor, survival, thromboembolism, univentricular
Subject Categories: Mortality/Survival, Cardiovascular Surgery, Congenital Heart Disease
Nonstandard Abbreviations and Acronyms
- ANZ
Australia and New Zealand
- AVV
atrioventricular valve
Clinical Perspective
What Is New?
Fenestration of the Fontan circuit does not appear to convey long‐term benefits in propensity score–matched cohorts.
Fenestration is associated with a higher risk of thromboembolic events.
What Are the Clinical Implications?
It is important to precisely define the short‐term benefits of fenestration in Fontan circulation given that routine placement fenestration does not appear to confer long‐term benefits and is associated with an increased risk of thrombosis.
The addition of fenestration at the time of Fontan operation should be considered on a case‐by‐case basis.
The concept of fenestration between the systemic venous return and atrial chamber was developed to improve early outcomes after the Fontan procedure. 1 , 2 The proposed benefits of fenestration are to reduce the rise in post‐Fontan systemic venous pressure and to augment preload of the systemic ventricle. 3 These benefits are believed to minimize pleural drainage, hospital length of stay, and short‐term morbidity. 4 , 5 However, fenestration causes a degree of systemic arterial desaturation and exposes the patient to a risk of paradoxical thromboembolism. The overall long‐term effects of fenestration remain poorly defined. Although some advocate for routine fenestration of the Fontan pathway, there remains a debate as to its benefits in all patients. 6 , 7 , 8 We aimed to address this uncertainty through a propensity‐scored analysis of a large cohort of patients with Fontan circulation.
Methods
Because of the confidential nature of the data used, the study data will not be made available. The analytic methods used in this study are described in the statiscial analysis section. The Australian and New Zealand (ANZ) Fontan Registry is a binational registry that includes patients from the 2 countries who have survived to hospital discharge with an intact Fontan circulation. The design of the ANZ Fontan Registry has previously been described, and the ongoing approval for research using the contained patient data is maintained by all institutional review boards involved. 9 A review of the ANZ Fontan Registry was conducted. Patient demographics, pre‐Fontan hemodynamic data, operative details, and follow‐up data were collected from the registry. Fenestration was performed using a technique previously described. 10 The decision whether to perform a fenestration was variable across institutions, with some performing routine fenestration and others on a case‐by‐case basis. Thromboembolic prophylaxis as well as management of liver and renal dysfunction were also on a case‐by‐case basis.
A total of 1690 patients were identified from the registry who underwent the Fontan procedure between June 1975 and January 2020. Although the atriopulmonary Fontan operation was performed in the early era, following a brief period of lateral tunnel use, the extracardiac conduit has almost exclusively been performed since 1996 across ANZ. To make the results of this study applicable to contemporary practice, patients with atriopulmonary Fontan circulation (n=232) were excluded. Of the 1458 patients with a lateral tunnel or extracardiac conduit Fontan modification, a further 15 patients did not have data recorded on the presence of fenestration and were excluded. The remaining 1443 patients, who underwent Fontan operation between 1980 and 2020, constituted the cohort used in analysis.
Definitions
Thromboembolic events were defined as all systemic, intracardiac, and Fontan conduit thromboembolic events, with the exclusion of distal deep vein thromboses and pulmonary embolism. Prolonged pleural drainage was defined as chest drains in situ for >30 days postoperatively or reoperations for pleural effusions. Fontan failure was defined as death, Fontan takedown, transplantation, plastic bronchitis, protein‐losing enteropathy, or New York Heart Association Class III/IV symptoms during follow‐up. For patients who experienced >1 of these end points, the date of Fontan failure was the date of the earliest end point. In the absence of clear event dates, the time to event was determined to be the time until last seen well.
Statistical Analysis
All analyses were performed in Stata V.18 (StataCorp, College Station, TX). Values are given as mean±SD for normally distributed variables or median (interquartile range and range) for nonparametric continuous variables and count and percentages for categorical variables. Categorical variables were compared using the χ2 test unless group size was <10, in which case the Fisher exact test was used. Continuous variables were compared using the Kruskal–Wallis test.
Propensity‐score matching was performed using the following variables: sex, age at Fontan operation, era of Fontan operation, hypoplastic left heart syndrome, right ventricular dominance, pre‐Fontan moderate or great atrioventricular valve (AVV) regurgitation, pre‐Fontan pulmonary artery (PA) pressure, Fontan modification type, isomerism, concomitant AVV surgery at Fontan operation, and concomitant PA plasty at Fontan operation. Regarding the definition of propensity matching, we prospectively defined a well‐matched pair as a pair in which 1‐to‐1 matching had a fixed calliper width equal to 0.2 SDs of the logistic regression of the mean of propensity scores. An acceptable degree of balance was considered a standardized mean difference of <10%.
Time‐dependent end points were analyzed using the Kaplan–Meier method. A log‐rank test stratified on quintiles of the propensity score was used to compare Kaplan–Meier curves. The threshold for statistical significance was P<0.05.
Results
Overall Unmatched Cohort
Baseline patient demographics comparing patients with fenestrated and nonfenestrated Fontan circulations are shown in Table 1. The median follow‐up time was 10.6 years (range, 1 day–41.7 years). Importantly, the group who underwent fenestration had a significantly higher proportion with hypoplastic left heart syndrome, lateral tunnel Fontan modification, right ventricular dominance, significant preoperative AVV regurgitation, concomitant PA plasty, concomitant AVV surgery, and higher mean preoperative PA pressures.
Table 1.
Baseline Demographics of the Unmatched Cohort
| Fenestrated | Nonfenestrated | Standardized difference | P value | |
|---|---|---|---|---|
| N | 621 | 822 | ||
| Age, y | 4.7 (3.8–5.8) | 4.5 (3.7–5.5) | −9.3 | 0.55 |
| Male sex | 369 (59.4) | 480 (58.4) | 5.1 | 0.70 |
| HLHS | 151 (24.3) | 67 (8.2) | 50.6 | <0.001 |
| Fontan type | −19.0 | <0.001 | ||
| LT | 151 | 137 | ||
| ECC | 470 | 685 | ||
| RV dominance | 277 (44.6) | 246 (29.9) | −30.9 | <0.001 |
| Isomerism | 38 (6.1) | 66 (8.0) | −0.9 | 0.16 |
| Preoperative AVV regurgitation | 67/523 | 55/653 | 16.8 | 0.01 |
| PA pressure, mmHg | 11.7±2.8 | 10.9±3.6 | 13.0 | <0.001 |
| AVV surgery | 28 (4.5) | 14 (1.7) | 16.0 | 0.002 |
| PA plasty | 82 (13.2) | 48 (5.8) | 25.2 | <0.001 |
| Decade of surgery | 8.1 | 0.02 | ||
| 1980–1989 | 0 | 10 | ||
| 1990–1999 | 127 | 184 | ||
| 2000–2009 | 229 | 293 | ||
| 2010–2020 | 265 | 334 |
Fenestrated and nonfenestrated data are provided as number, number (percentage), mean±SD, or median (range). AVV indicates atrioventricular valve; ECC, extracardiac conduit; HLHS, hypoplastic left heart syndrome; LT, lateral tunnel; PA, pulmonary artery; and RV, right ventricular.
Intraoperative and early postoperative outcomes are shown in Table 2. Patients with fenestration had longer bypass and cross‐clamp times; however, the length of stay and proportion with prolonged pleural drainage did not differ significantly.
Table 2.
Operative and Early Postoperative Details for the Unmatched Cohort
| Fenestrated | Nonfenestrated | P value | |
|---|---|---|---|
| N | 621 | 822 | |
| Cardiopulmonary bypass, min | 117 (94–155) | 93 (71–120) | <0.001 |
| Aortic cross‐clamp, min | 32 (20–51) | 0 (0–41) | <0.001 |
| Length of stay, d | 13 (10–20) | 13 (10–20) | 0.15 |
| Additional procedure during admission | 108 (17) | 64 (8) | <0.001 |
| Fontan revision | 11 | 4 | |
| Pleurodesis | 6 | 8 | |
| Fenestration intervention, dilation/creation | 14 | 4 | |
| Coiling of collaterals | 13 | 8 | |
| Early pacemaker insertion | 14 | 13 | |
| Intercostal catheter insertion, additional | 16 | 3 | |
| Re‐exploration for bleeding or tamponade | 34 | 20 | |
| Prolonged effusions, >30 d or requiring intervention | 40 (6) | 48 (6) | 0.72 |
Fenestrated and nonfenestrated data are provided as number, number (percentage), or median (range).
Survival
Survival at 10 and 20 years was 95.5% (95% CI, 93.1%–97.1%) and 88.9% (95% CI, 83.6%–92.6%) in the fenestrated group compared with 97.7% (95% CI, 96.0%–98.7%) and 92.5% (95% CI, 88.4%–95.1%) in the nonfenestrated group (P=0.04; Figure 1A).
Figure 1. Comparison of unmatched cohorts.
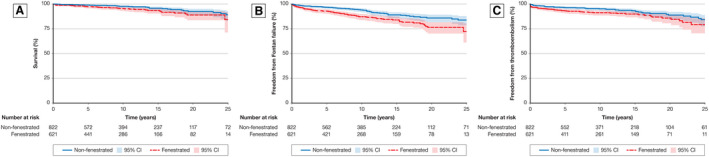
A, Survival in unmatched cohorts. Log‐rank analysis of the unmatched cohorts demonstrated better survival in the nonfenestrated cohort (P=0.04). This result may pertain to the higher preoperative risk factors in the fenestration group, influencing the decision to perform fenestration. B, Freedom from Fontan failure in unmatched cohorts. Log‐rank analysis of the unmatched cohorts demonstrated improved freedom from Fontan failure in the nonfenestrated group. Similarly, this is likely attributed to higher risk patients undergoing fenestration, which is unaccounted for in the unmatched analysis (P=0.01). C, Freedom from thromboembolic events in unmatched cohorts. Log‐rank analysis of the unmatched cohorts showed a higher incidence of thromboembolic events in the fenestrated group. Although this may be attributed to higher preoperative risk factors in the fenestration group, the presence of the fenestration may also predispose the group to thromboembolism (P=0.01).
Fontan Failure
Freedom from Fontan failure at 10 and 20 years was 87.2% (95% CI, 83.7%–90.0%) and 76.4% (95% CI, 70.2%–81.5%) in the fenestrated group compared with 94.0% (95% CI, 91.7%–95.7%) and 85.9% (95% CI, 81.6%–89.2%) in the nonfenestrated group (P=0.01; Figure 1B).
Thromboembolic Events
Freedom from Fontan thromboembolism at 10 and 20 years was 91.3% (95% CI, 88.4%–93.4%) and 85.8% (95% CI, 80.5%–89.7%) in the fenestrated group compared with 95.2% (95% CI, 93.2%–96.6%) and 88.8% (95% CI, 84.4%–92.1%) in the nonfenestrated group (P=0.01; Figure 2C).
Figure 2. Comparison of propensity score–matched cohorts.
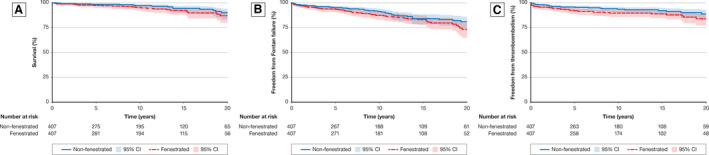
A, Survival in propensity score–matched cohorts. Log‐rank analysis of the propensity score–matched cohorts showed no difference in survival (P=0.16). The lack of difference demonstrates the influence of preoperative risk factors and the lack of impact of the fenestration on long‐term survival. B, Freedom from Fontan failure in propensity score–matched cohorts. Log‐rank analysis of the propensity score–matched cohorts showed no difference in freedom from Fontan failure (P=0.10). Similarly, the lack of difference demonstrates the influence of preoperative risk factors and the lack of impact of the fenestration on long‐term survival. C, Freedom from thromboembolic events in propensity score–matched cohorts. Log‐rank analysis of the propensity score–matched cohorts showed a higher incidence of thromboembolic events in the fenestrated group (P=0.03). Given this difference persists after propensity‐score matching, it demonstrates an association between fenestration and long‐term thromboembolic events that cannot be attributed to the cohort demographics.
Functional Status
Patients with fenestration had lower freedom from New York Heart Association Class III/IV symptoms (P<0.01) and freedom from protein‐losing enteropathy (P=0.001). However, there was no difference in the rate of Fontan takedown (P=0.10) or plastic bronchitis (P=0.15).
Propensity Score–Matched Cohort
After propensity‐score matching was performed, 407 well‐matched pairs of patients were identified. Baseline demographics of the matched cohort are presented in Table 3. Intraoperative and early postoperative outcomes are shown in Table 4. Patients with fenestration had longer bypass and cross‐clamp times; however, the length of stay and proportion with prolonged pleural drainage did not differ significantly between the groups.
Table 3.
Demographic Data of Matched Cohort
| Fenestrated | Nonfenestrated | Standardized difference | P value | |
|---|---|---|---|---|
| N | 407 | 407 | ||
| Age, y | 4.7 (3.8–5.8) | 4.5 (3.7–5.6) | 4.5 | 0.50 |
| Male sex | 249 (59.3) | 249 (59.3) | −2.0 | 1.0 |
| HLHS | 58 (14.3) | 59 (14.5) | −0.7 | 0.92 |
| Fontan type | −1.8 | 0.8 | ||
| LT | 91 (22.4) | 88 (21.6) | ||
| ECC | 316 (77.6) | 319 (78.4) | ||
| Dominant RV | 156 (38.3) | 148 (36.4) | 7.5 | 0.56 |
| Isomerism | 27 (6.6) | 32 (7.9) | 0.6 | 0.50 |
| Preoperative AVV regurgitation | 43 (10.5) | 46 (11.3) | −2.4 | 0.74 |
| PA pressure, mmHg | 11.7±2.7 | 11.7±3.1 | 1.6 | 0.81 |
| AVV surgery | 7 (1.7) | 11 (2.7) | −5.7 | 0.34 |
| PA plasty | 44 (10.8) | 35 (8.6) | 7.6 | 0.29 |
| Decade of surgery | 1.2 | 0.77 | ||
| 1980–1989 | 0 | 0 | ||
| 1990–1999 | 92 | 95 | ||
| 2000–2009 | 145 | 140 | ||
| 2010–2020 | 170 | 171 |
Fenestrated and nonfenestrated data are provided as number, number (percentage), mean±SD, or median (range). AVV indicates atrioventricular valve; ECC, extracardiac conduit; HLHS, hypoplastic left heart syndrome; LT, lateral tunnel; PA, pulmonary artery; and RV, right ventricular.
Table 4.
Operative and Early Postoperative Details for the Matched Cohort
| Fenestrated | Nonfenestrated | P value | |
|---|---|---|---|
| N | 407 | 407 | |
| Cardiopulmonary bypass, min | 117 (91–157) | 100 (77–127) | <0.001 |
| Aortic cross‐clamp, min | 32 (22–52) | 0 (0–49) | <0.001 |
| Length of stay, d | 14 (10–20) | 14 (10–21) | 0.80 |
| Additional procedure | 64 (15.7) | 31 (7.6) | <0.001 |
| Prolonged effusions, >30 d or requiring intervention | 27 (6) | 22 (6) | 0.46 |
Fenestrated and nonfenestrated data are provided as number, number (percentage), or median (range).
Survival
Survival at 10 and 20 years was 95.3% (95% CI, 92.2%–97.2%) and 87.0% (95% CI, 80.0%–91.7%) in the fenestrated group compared with 97.1% (95% CI, 94.3%–98.6%) and 90.0% (95% CI, 83.2%–94.2%) in the nonfenestrated group (P=0.16; Figure 2A).
Fontan Failure
Freedom from Fontan failure at 10 and 20 years was 87.3% (95% CI, 82.9%–90.6%) and 73.2% (95% CI, 64.9%–80.0%) in the fenestrated group compared with 91.2% (95% CI, 87.2%–94.0%) and 80.9% (95% CI, 74.0%–86.1%) in the nonfenestrated group (P=0.10; Figure 2B).
Thromboembolic Events
Freedom from Fontan thromboembolism at 10 and 20 years was 89.6% (95% CI, 85.7%–92.5%) and 84.1% (95% CI, 77.2%–89.0%) in the fenestrated group compared with 93.5% (95% CI, 90.0%–95.8%) and 88.8% (95% CI, 87.9%–94.9%) in the nonfenestrated group (P=0.03; Figure 2C).
Functional Status
There was no difference between groups in terms of freedom from New York Heart Association Class III/IV symptoms (P=0.06), plastic bronchitis (P=0.25), protein‐losing enteropathy (P=0.46), or Fontan takedown (P=0.73).
Discussion
Fenestration of the Fontan circuit was initially devised to address the sequelae of the immediate postoperative increase in systemic venous pressure and expand the eligibility for the Fontan operation. Since its conception, there have been numerous studies attempting to address the impact of fenestration, both short term and long term. 4 , 5 , 6 , 7 , 11 , 12 , 13 It has been demonstrated that Fontan fenestration may reduce the duration of postoperative pleural drainage. 7 , 11 , 13 , 14 Contrarily, a recent report noted excellent early outcomes with nonfenestrated Fontans for several decades. 15 Previous studies were predominantly limited by small numbers, short follow‐up, lack of randomization, or propensity‐score matching.
The only randomized control trial was conducted by Lemler et al in 49 patients and demonstrated that patients with fenestration (n=25) had less pleural drainage and shorter hospital stays. 5 This study, however, was also limited by a small cohort and lack of follow‐up beyond hospital discharge.
Two recent meta‐analyses were performed by Li et al and Bouhout et al in 2019 and 2020, respectively. 6 , 11 Both meta‐analyses describe inconsistent conclusions of various articles on the topic. Li et al reported a lower early postoperative arrhythmia burden in the fenestrated group at the expense of reduced early systemic oxygen saturation and longer bypass time. 6 In addition, Bouhout et al described the apparent benefit of fenestration in reducing PA pressures and minimizing pleural drainage. 11 These varying results could be attributable to the heterogeneity of patients’ preoperative conditions as patients undergoing fenestration often had more comorbidities and higher PA pressures. There was no difference in the incidence of stroke and thrombosis between the 2 groups in both meta‐analyses. 6 , 11 Both analyses noted the lack of significant impact of fenestration on the long‐term survival or Fontan failure. 6 , 11
Saiki et al attempted to identify the physiological benefits of persistent long‐term fenestration for chronic cardioprotection. They demonstrated that persistent fenestration allowed for more reserve in preload and reduction in afterload; however, these benefits disappeared with atrial tachycardia. 12
It is well documented that many fenestrations undergo spontaneous closure. The exact timing of spontaneous closure is unknown. However, it has been reported that high preoperative pulmonary vascular resistance and history of venous thromboembolism may prevent spontaneous closure. 16 A review by Atz et al of the effects of persistent Fontan fenestration demonstrated that the persistence of a patent fenestration did not have deleterious effects on long‐term morbidity or mortality. 13 However, they did report that persistent fenestration was associated with lower systemic oxygen saturations and more medications.
In the current study, we observed in the unmatched cohort lower survival, lower freedom from Fontan failure, and lower freedom from thromboembolic events in patients with fenestrated Fontan circulation. However, patients with fenestration had significantly high rates of hypoplastic left heart syndrome, right ventricular dominance, AVV regurgitation, PA plasty, and higher PA pressures. As such, the differences in these baseline characteristics may have influenced the outcomes. Thus, we performed a propensity‐match analysis to adjust for the aforementioned baseline characteristics.
The propensity‐match analysis demonstrated no difference in survival or Fontan failure between fenestrated and nonfenestrated groups. We did not observe a difference in the rate of prolonged postoperative pleural drainage (duration of >30 days). However, we demonstrated a long‐term increase in the rate of thromboembolic events in patients with fenestration. A meta‐analysis recently reported no difference in the incidence of stroke (with varying anticoagulation strategies). 11 By comparison, Fontan circuit thrombosis and intracardiac thrombosis were included in our definition of thromboembolic events rather than only stroke. Given the turbulent flow across the fenestration and altered atrial morphology and flow, it is unsurprising that atrial thromboses account for most of the intracardiac thrombosis in patients with a Fontan modification. 17 , 18
Because of the design of the ANZ Fontan Registry, we cannot make any inferences into the impact of fenestration on operative mortality or Fontan takedown that may have occurred before discharge from the hospital. However, because of low operative mortality and takedown of Fontan circulation, the impact of fenestration, if any, is expected to be minimal. 19 , 20 , 21 , 22 Similarly, because of the design of the registry, we were unable to determine the effects of fenestration on long‐term renal and hepatic function in this study.
Limitations
Our study is limited by the retrospective nature of the ANZ Fontan Registry. The study includes only hospital survivors with Fontan circulation. Thus, the impact of fenestration on operative mortality and takedown of Fontan circulation cannot be assessed. In addition, our definitions of variables are set by the recorded data within the registry. Although the groups were well matched, the propensity‐score matching may not account for all possible confounding variables. The study was performed as an intention‐to‐treat analysis and, as such, the long‐term patency of the fenestration was not accounted for.
Conclusions
In the propensity score–matched analysis, we demonstrated no difference in long‐term survival or freedom from Fontan failure in patients with and without fenestration. There was a higher incidence in long‐term thromboembolic events in patients with fenestration (Figure 3). Overall, it appears that fenestration in Fontan circulation does not bring long‐term benefits.
Figure 3. The impact of Fontan fenestration on long‐term outcomes.
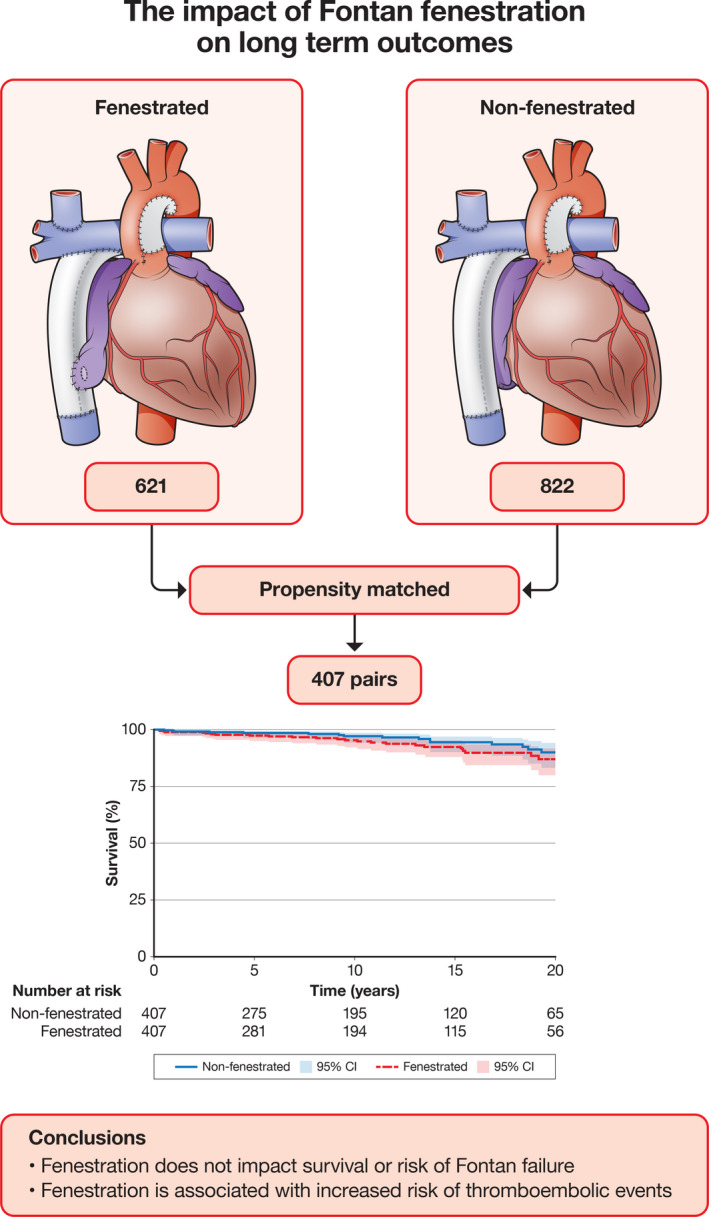
Propensity‐score matching was performed on 1443 patients, producing 407 matched pairs for an intention‐to‐treat analysis. Log‐rank tests were performed on time‐dependent variables to test the differences between groups. No difference in survival or freedom from failure was detected between the 2 groups. Patients undergoing fenestration did have an increased risk of thromboembolic events during follow‐up.
Sources of Funding
This work was supported by a National Health and Medical Research Council Partnership grant (1076849) and a grant from the Starship Foundation. The authors acknowledge support provided to the Murdoch Children’s Research Institute through the Victorian Government’s Operational Infrastructure Support Program.
Disclosures
Dr King is supported by a National Heart Foundation Health Professional Scholarship (102510). Dr d’Udekem has been a consultant for Merck Sharp and Dohme and Actelion. The remaining authors having no disclosures to report.
Acknowledgments
We thank our research assistants for their support in maintaining the Australian and New Zealand Fontan Registry.
For Sources of Funding and Disclosures, see page 8.
References
- 1. Bridges ND, Lock JE, Castaneda AR. Baffle fenestration with subsequent transcatheter closure. Modification of the Fontan operation for patients at increased risk. Circulation. 1990;82:1681–1689. doi: 10.1161/01.CIR.82.5.1681 [DOI] [PubMed] [Google Scholar]
- 2. Choussat A, Fontan F, Besse P, Vallot F, Chauve A, Bricaud H, Anderson R, Shinebourne E. Selection criteria for the Fontan procedure. Paediatr Cardiol. 1978;559–566. [Google Scholar]
- 3. Rychik J, Atz AM, Celermajer DS, Deal BJ, Gatzoulis MA, Gewillig MH, Hsia T‐Y, Hsu DT, Kovacs AH, McCrindle BW, et al. Evaluation and management of the child and adult with Fontan circulation: a scientific statement from the American Heart Association. Circulation. 2019;140. doi: 10.1161/CIR.0000000000000696 [DOI] [PubMed] [Google Scholar]
- 4. Bridges ND, Mayer JE Jr, Lock JE, Jonas RA, Hanley FL, Keane JF, Perry SB, Castaneda AR. Effect of baffle fenestration on outcome of the modified Fontan operation. Circulation. 1992;86:1762–1769. doi: 10.1161/01.CIR.86.6.1762 [DOI] [PubMed] [Google Scholar]
- 5. Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C. Fenestration improves clinical outcome of the Fontan procedure: a prospective, randomized study. Circulation. 2002;105:207–212. doi: 10.1161/hc0202.102237 [DOI] [PubMed] [Google Scholar]
- 6. Li D, Li M, Zhou X, An Q. Comparison of the fenestrated and non‐fenestrated Fontan procedures: a meta‐analysis. Medicine. 2019;98:e16554. doi: 10.1097/MD.0000000000016554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Airan B, Sharma R, Choudhary SK, Mohanty SR, Bhan A, Chowdhari UK, Juneja R, Kothari SS, Saxena A, Venugopal P. Univentricular repair: is routine fenestration justified? Ann Thorac Surg. 2000;69:1900–1906. doi: 10.1016/S0003-4975(00)01247-9 [DOI] [PubMed] [Google Scholar]
- 8. Schreiber C, Horer J, Vogt M, Cleuziou J, Prodan Z, Lange R. Nonfenestrated extracardiac total cavopulmonary connection in 132 consecutive patients. Ann Thorac Surg. 2007;84:894–899. doi: 10.1016/j.athoracsur.2007.04.034 [DOI] [PubMed] [Google Scholar]
- 9. Iyengar AJ, Winlaw DS, Galati JC, Gentles TL, Weintraub RG, Justo RN, Wheaton GR, Bullock A, Celermajer DS, d'Udekem Y. The Australia and New Zealand Fontan registry: description and initial results from the first population‐based Fontan registry. Intern Med J. 2014;44:148–155. doi: 10.1111/imj.12318 [DOI] [PubMed] [Google Scholar]
- 10. Ruiz E, Guerrero R, d'Udekem Y, Brizard C. A technique of fenestration for extracardiac Fontan with long‐term patency. Eur J Cardiothorac Surg. 2009;36:200–202; discussion 202. doi: 10.1016/j.ejcts.2009.03.037 [DOI] [PubMed] [Google Scholar]
- 11. Bouhout I, Ben‐Ali W, Khalaf D, Raboisson MJ, Poirier N. Effect of fenestration on Fontan procedure outcomes: a meta‐analysis and review. Ann Thorac Surg. 2020;109:1467–1474. doi: 10.1016/j.athoracsur.2019.12.020 [DOI] [PubMed] [Google Scholar]
- 12. Saiki H, Kuwata S, Iwamoto Y, Ishido H, Taketazu M, Masutani S, Nishida T, Senzaki H. Fenestration in the Fontan circulation as a strategy for chronic cardioprotection. Heart. 2019;105:1266. doi: 10.1136/heartjnl-2018-314183 [DOI] [PubMed] [Google Scholar]
- 13. Atz AM, Travison TG, McCrindle BW, Mahony L, Quartermain M, Williams RV, Breitbart RE, Lu M, Radojewski E, Margossian R, et al. Late status of Fontan patients with persistent surgical fenestration. J Am Coll Cardiol. 2011;57:2437–2443. doi: 10.1016/j.jacc.2011.01.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Luo Q, Zhao W, Su Z, Liu Y, Jia Y, Zhang L, Wang H, Li Y, Wu X, Li S, et al. Risk factors for prolonged pleural effusion following total cavopulmonary connection surgery: 9 years' experience at Fuwai hospital. Front Pediatr. 2019;7. doi: 10.3389/fped.2019.00456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stephens EH, Talwar AA, Devlin PJ, Eltayeb O, Mongé MC, Tsao S, Backer CL. 24‐year results of nonfenestrated extracardiac Fontan including Fontan conversions. Ann Thorac Surg. 2021;112:619–625. doi: 10.1016/j.athoracsur.2020.06.019 [DOI] [PubMed] [Google Scholar]
- 16. Gorla SR, Jhingoeri NK, Chakraborty A, Raja KR, Garg A, Sandhu S, Rosenkranz ER, Swaminathan S. Incidence and factors influencing the spontaneous closure of Fontan fenestration. Congenit Heart Dis. 2018;13:776–781. doi: 10.1111/chd.12652 [DOI] [PubMed] [Google Scholar]
- 17. Balling G, Vogt M, Kaemmerer H, Eicken A, Meisner H, Hess J. Intracardiac thrombus formation after the Fontan operation. J Thorac Cardiovasc Surg. 2000;119:745–752. doi: 10.1016/S0022-5223(00)70010-9 [DOI] [PubMed] [Google Scholar]
- 18. Zentner D, Celermajer DS, Gentles T, d’Udekem Y, Ayer J, Blue GM, Bridgman C, Burchill L, Cheung M, Cordina R, et al. Management of people with a Fontan circulation: a cardiac society of Australia and New Zealand position statement. Heart Lung Circ. 2020;29:5–39. doi: 10.1016/j.hlc.2019.09.010 [DOI] [PubMed] [Google Scholar]
- 19. Iyengar AJ, Winlaw DS, Galati JC, Wheaton GR, Gentles TL, Grigg LE, Justo RN, Radford DJ, Weintraub RG, Bullock A, et al. The extracardiac conduit Fontan procedure in Australia and New Zealand: hypoplastic left heart syndrome predicts worse early and late outcomes. Eur J Cardiothorac Surg. 2014;46:465–473. doi: 10.1093/ejcts/ezu015 [DOI] [PubMed] [Google Scholar]
- 20. d’Udekem Y, Iyengar AJ, Galati JC, Forsdick V, Weintraub RG, Wheaton GR, Bullock A, Justo RN, Grigg LE, Sholler GF, et al. Redefining expectations of long‐term survival after the Fontan procedure. Circulation. 2014;130:S32–S38. doi: 10.1161/CIRCULATIONAHA.113.007764 [DOI] [PubMed] [Google Scholar]
- 21. d'Udekem Y, Xu MY, Galati JC, Lu S, Iyengar AJ, Konstantinov IE, Wheaton GR, Ramsay JM, Grigg LE, Millar J, et al. Predictors of survival after single‐ventricle palliation. J Am Coll Cardiol. 2012;59:1178–1185. doi: 10.1016/j.jacc.2011.11.049 [DOI] [PubMed] [Google Scholar]
- 22. Iyengar AJ, Winlaw DS, Galati JC, Celermajer DS, Wheaton GR, Gentles TL, Grigg LE, Weintraub RG, Bullock A, Justo RN, et al. Trends in Fontan surgery and risk factors for early adverse outcomes after Fontan surgery: the Australia and New Zealand Fontan registry experience. J Thorac Cardiovasc Surg. 2014;148:566–575. doi: 10.1016/j.jtcvs.2013.09.074 [DOI] [PubMed] [Google Scholar]


