Abstract
Lateral extra-articular tenodesis (L.E.T.) have been proposed to reduce the tibia’s anterior translation and internal rotation in concomitant to Anterior cruciate ligament (A.C.L.) reconstruction. Recent studies show that the addition of L.E.T. to A.C.L. reconstruction results in a statistically significant reduction in graft failure. The purpose of the present study was to evaluate the clinical outcomes, complications, and rate of return to preinjury sports level in pediatric patients who underwent combined A.C.L. reconstruction with L.E.T. at a minimum 2-year follow-up. The authors retrospectively evaluated 42 pediatric patients at high risk of graft failure who experienced ACLR connected to L.E.T. IKDC and Tegner-Lysholm Knee Scores Scale were used to assess clinical outcomes, and the Tegner Activity Scale to evaluate the return to sport. No graft failure or subsequent surgery related to A.C.L. reconstruction occurred. Furthermore, 88% of patients returned to the sport. Satisfactory clinical results were obtained on a short and medium-term follow-up.
These findings help to consider this procedure for active adolescents at a high risk of graft failure to enhance A.C.L. reconstruction.
Keywords: Lateral Extra-articular tenodesis, ACL, LET, pediatric, young
Introduction
The incidence of Anterior Cruciate Ligament (A.C.L.) tears in younger patients (aged 6 to 18 years) has steadily increased by about 2.3% annually over the last 20 years,1 mainly because children participated in adolescents in competitive sports at a high level.2 The management of these injuries is still under debate. Indeed, surgical reconstruction of the ligament can lead to a growth disturbance of the open physis. On the other hand, the delay in surgery may increase the risk of subsequent intra-articular injury caused by the development of knee instability, or conversely may prevent patients from participating in sports activities with increased risk of juvenile obesity.3–5 For these reasons, the increase in A.C.L. reconstructions in younger aged patients outpaced the growth in these procedures in adults over the past decades.6 A.C.L. tears can create rotational and sagittal instability of the knee, and intra-articular reconstruction techniques of the ligament represent the gold standard in their management.7 However, the postoperative recovery of rotatory stability is challenging.8 Several studies pointed out that a persistent anterolateral rotatory instability of the knee after A.C.L. reconstruction is associated with worse functional outcomes and increased rate of graft failure.9,10 Biomechanical studies have indicated that peripheral anterolateral structures of the knee such as the iliotibial band and anterolateral ligament represent necessary restraints to the internal rotation of the tibia, and can effectively counteract the anterolateral rotatory instability.11 Consequently, different techniques of lateral extra-articular tenodesis (L.E.T.) have been proposed to reduce the tibia’s anterior translation and internal rotation.8,12 These procedures are of particular interest in the growing age when joint hypermobility along with participation in high-level contact sports can promote the re-injury.13 Indeed, it was recently reported that the addition of L.E.T. to A.C.L. reconstruction results in a statistically significant reduction in graft failure.14 However, there is a lack of data on the outcomes of these procedures in growing age patients involved in high-level contact sports. The present study’s purpose was to evaluate clinical outcomes, complications, and rate of return to preinjury sports level in young sports patients who underwent combined A.C.L. reconstruction with L.E.T. at a minimum 2-year follow-up.
Materials and Methods
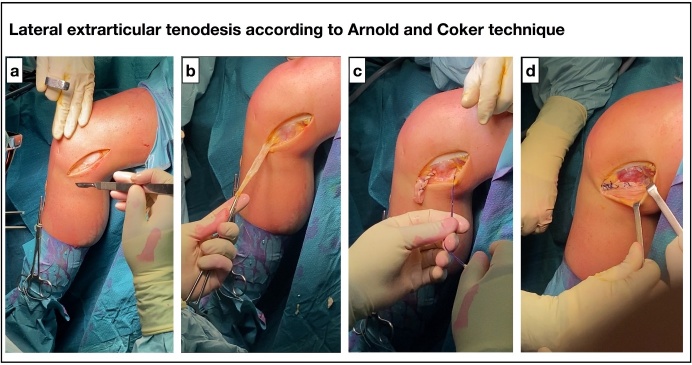
Forty-two young patients (18 years or younger) who had undergone A.C.L. reconstruction combined with L.E.T. were evaluated in this retrospective study at a minimum 2-year follow-up (mean 4.1 ± 2.6 years; range 2 - 9). Inclusion criteria included participation in contact sports, anterior cruciate ligament tear with pivot-shift test grade 2 or more, and knee hypermobility. All patients underwent surgery at IRCCS Sacro Cuore - Don Calabria in Negrar (VE), Italy, between 2016 and 2019. A.C.L. reconstruction was performed with autologous hamstring tendons using the Top Traction System (T.T.S. J-TECH Srl Padova, Italy) in the femur and BIORCI bioabsorbable interferential screw (Smith & Nephew, Memphis, TN, U.S.A.) in the tibia. Eight patients (19.0%) with failure of a previous A.C.L. reconstruction underwent A.C.L. revision with tibial tendon allograft combined with L.E.T. The Macintosh technique modified by Arnold and Coker15 was used for L.E.T. (Figure 1). Briefly, a strip of the iliotibial band was detached proximally, passed beneath the fibular collateral ligament and popliteus tendon, and finally sutured to the Gerdy tubercle with the knee flexed to 90-100°and foot in external rotation. Clinical outcome was assessed using the International Knee Documentation Committee (IKDC) score and the Tegner Lysholm Knee Scoring Scale. In addition, the return to sports activity was evaluated with the Tegner Activity.16,17 To assess the deterioration of clinical outcomes over time, patients with a follow-up of more minor than or more fantastic than four years were compared. Data from the two groups were compared using the Student t-test. Statistical analysis was carried out using SPSS software (version 21.0; I.B.M., Armonk, NY, U.S.A.). A p < 0.05 was considered as significant.
Figure 1. Lateral extra-articular tenodesis according to Arnold and Coker Technique.
Lateral view of the left knee. (a,b) The iliotibial band (ITB) is exposed and left attached distally to the Gerdy’s Tubercle. (c,d) the ITB is passed beneath the fibular collateral ligament and popliteus tendon and finally sutured to the Gerdy tubercle.
Results
Baseline data of the patients are summarized in Table 1. IKDC and Tegner-Lysholm Knee Scores Scale at follow-up indicated satisfactory and painless function of the knee in all the patients (Table 2). Analyzing the results by follow-up length, no difference was observed between patients with a follow-up of less than or greater than 4 years (Table 2). As shown in Table 3, most patients were satisfied with their postoperative results and resumed their pre-injury sports activity. The difference between the mean preoperative and postoperative Tegner activity scale was insignificant. There were no cases of re-rupture. Reoperation was necessary for one patient. This patient sustained a knee injury during a soccer match and underwent knee arthroscopy for a meniscal tear three years after the A.C.L. reconstruction. No graft failure or subsequent surgery related to the A.C.L. reconstruction occurred.
Table 1. Baseline characteristics of the patients.
| Patients data | Mean ± SD (range) or N (%) | |
| Sex, male | 28 (67) | |
| Age, years | 17 ± 1.18 (14 – 18) | |
| BMI, kg/m2 | 26 ± 2.34 | |
| Side of injury | ||
| Left | 18 (43) | |
| Right | 24 (57) | |
| Obvious knee instability (Pivot Shift grade 2 or more) | 42(100) | |
| Sport played at the time of injury | ||
| Soccer | 18 (43) | |
| Basketball | 5 (12) | |
| Rugby or Football | 6 (14) | |
| Skiing | 5 (12) | |
| Gymnastics | 2 (5) | |
| Other | 6 (14) | |
| Graft source | ||
| Autologous hamstrings tendon | 34 (81) | |
| Tibial tendon allograft | 8 (19) | |
| Arthroscopic procedures associated | ||
| Associated meniscal repair | ||
| Medial | 10 (24) | |
| Lateral | 14 (33) | |
| Associated meniscectomy | ||
| Medial | 4 (10) | |
| Lateral | 3 (7) | |
| Follow-up (years) | 4.07 ± 2.55 (2 - 9) | |
Table 2. Clinical results in the study group at follow-up.
| Score | Mean ± SD | P-value | ||
| All patients (N = 42) | FU < 4 years (N = 16) | FU > 4 years (N = 26) | ||
| Tegner-Lysholm Knee Scoring Scale | 92.0 ± 9.6 | 93.4 ± 7.5 | 89.8 ± 12.4 | 0.4 |
| IKDC score | 91.5 ± 8.0 | 92.5 ± 7.2 | 90.0 ± 9.8 | 0.5 |
Table 3. Level of satisfaction, reoperations and return to sport in the study group at the time of follow-up.
| Mean (range) or N (%) | |
| Satisfied with the result of surgery | |
| Yes | 39 (93) |
| No | 3 (7) |
| Reoperation | |
| Yes | 1 (2) |
| No | 41 (98) |
| Return to sport | |
| Yes | 37 (88) |
| No | 5 (12) |
| Resumption of preinjury levels of sports participation | 32 (76) |
| Preoperative Tegner activity scale | 8.1 (6 – 10) |
| Postoperative Tegner activity scale | 7.8 (6 – 10) |
Discussion
The most important finding of the present study is that the combination of L.E.T. to A.C.L. reconstruction is a safe and effective surgical option in young patients with A.C.L. rupture. Clinical scores at follow-up were satisfactory in the study group, and 86% of patients could return to their pre-injury sports level. Furthermore, in this study, no case of graft failure occurred. The most common complication of A.C.L. reconstruction in skeletally immature patients is graft failure, observed in up to 25% of patients undergoing A.C.L. reconstruction.18–22 Age-related joint hypermobility, the open physis, and the participation in high-level and contact sports make these patients at high risk for A.C.L. rupture.13 Recently, Pennock et al.18 reported that quadriceps tendon grafting is associated with a lower failure rate than hamstring grafting in skeletally immature patients. These authors hypothesized that preservation of the stabilizing effect of hamstrings combined with a reduction in extension force due to quadriceps tendon harvest might protect the graft during the ligamentization process.
In contrast, Cordasco et al.23 reported that the revision rate of A.C.L. reconstruction due to graft failure was significantly higher (20%) in transphyseal reconstruction compared with the all-epiphyseal technique (6%) in subjects younger than 20 years of age. The rupture rate may be even higher when allografts are used for A.C.L. reconstruction, probably because of the low-dose graft irradiation that occurs during the sterilization process. However, allograft failures have been reported in studies of all-epiphyseal or transphyseal A.C.L. reconstruction in the absence of lateral extra-articular augmentation.24,25 The reason for using an allograft instead of the autologous tendon in all revision cases was to avoid donor site morbidity due to harvest of the patellar tendon or contralateral hamstrings. The absence of graft failure cases in our series could be attributable to the combination of L.E.T. to A.C.L. reconstruction. Indeed, extra-articular augmentation between the tibia and femur on the lateral side of the knee could prevent internal rotation of the tibia, stabilize the knee, and protect the reconstructed ligament.26 Conversely, the use of L.E.T. procedures alone (without A.C.L. reconstruction) is not an option with an A.C.L. rupture, even in skeletally immature patients, as demonstrated by the lack of literature data. Therefore, we didn’t perform any L.E.T. without simultaneously performing the A.C.L. reconstruction.
It is important to note that the satisfactory clinical results in the current study were obtained on a short- and medium-term follow-up. Still, concerns exist about the late development of lateral compartment osteoarthritis in patients who had undergone L.E.T. many years earlier because of possible chronic overloading of the joint. Several recent studies have found no correlation between L.E.T. and osteoarthritis.27,28
In this study, Arnold and Coker’s L.E.T. technique was used because it involves only soft tissue and does not require any additional femoral tunneling, is easily reproducible, and requires a short surgical time. Unlike other L.E.T. techniques, there is no risk of damaging the distal femoral physis or femoral cavity of the A.C.L. reconstruction.29
In conclusion, the combination of L.E.T. with A.C.L. reconstruction in young patients at high risk of failure in the current study leads to satisfactory functional outcomes, high rates of return to sports activities, and no graft failure. Therefore, we recommend this procedure as a good complement of primary A.C.L. reconstruction in adolescent athletes.
Author Contribution
Dr. Massimo Mariconda and Dr. Claudio Zorzi participate in the conception and design of the study. Daniele Screpis, Gianluca Piovan and Maria Rizzo worked on acquisition, analysis and interpretation of data. Amedeo Guarino and Luca Farinelli draft the article. All Authors revise it critically for the crucial intellectual continent. All authors agree to be accountable for all aspects of the work if questions arise regarding its accuracy or integrity, especially the corresponding author.
Conflict of Interest
All authors declare that there is no conflict of interest.
References
- 1. Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3). doi:10.1542/peds.2016-1877 [DOI] [PubMed]
- 2. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med. 2014;42(3):675-680. doi:10.1177/0363546513518412 [DOI] [PubMed]
- 3. Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: Is there harm in delay of treatment? Am J Sports Med. 2011;39:2582-2587. [DOI] [PubMed]
- 4. Newman JT, Carry PM, Terhune EB, et al. Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med. 2015;43(2):282-288. doi:10.1177/0363546514562168 [DOI] [PubMed]
- 5. Shaw L, Finch C. Trends in Pediatric and Adolescent Anterior Cruciate Ligament Injuries in Victoria, Australia 2005–2015. Int J Environ Res Public Health. 2017;14(6):599. doi:10.3390/ijerph14060599 [DOI] [PMC free article] [PubMed]
- 6. Werner BC, Yang S, Looney AM, Gwathmey FW. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447-452. doi:10.1097/bpo.0000000000000482 [DOI] [PubMed]
- 7. Hughes JD, Rauer T, Gibbs CM, Musahl V. Diagnosis and treatment of rotatory knee instability. J Exp Orthop. 2019;6(1):48. doi:10.1186/s40634-019-0217-1 [DOI] [PMC free article] [PubMed]
- 8. Geeslin AG, Moatshe G, Chahla J, et al. Anterolateral knee extra-articular stabilizers: a robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46(3):607-616. doi:10.1177/0363546517745268 [DOI] [PubMed]
- 9. Devitt BM, Bell SW, Ardern CL, et al. The role of lateral extra-articular tenodesis in primary anterior cruciate ligament reconstruction: a systematic review with meta-analysis and best-evidence synthesis. Orthop J Sports Med. 2017;5(10):2325967117731767. doi:10.1177/2325967117731767 [DOI] [PMC free article] [PubMed]
- 10. Ayeni OR, Chahal M, Tran MN, Sprague S. Pivot shift as an outcome measure for ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):767-777. doi:10.1007/s00167-011-1860-y [DOI] [PubMed]
- 11. Kittl C, El-Daou H, Athwal KK, et al. The role of the anterolateral structures and the ACL in controlling laxity of the intact and acl-deficient knee. Am J Sports Med. 2016;44(2):345-354. doi:10.1177/0363546515614312 [DOI] [PubMed]
- 12. Inderhaug E, Stephen JM, Williams A, Amis AA. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(2):347-354. doi:10.1177/0363546516681555 [DOI] [PubMed]
- 13. Dean RS, DePhillipo NN, McGaver RS, LaPrade RF, Larson CM. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis in skeletally immature patients: surgical technique. Arthrosc Tech. 2020;9(7):e897-e903. doi:10.1016/j.eats.2020.03.005 [DOI] [PMC free article] [PubMed]
- 14. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020;48(2):285-297. doi:10.1177/0363546519896333 [DOI] [PubMed]
- 15. Slette EL, Mikula JD, Schon JM, et al. Biomechanical results of lateral extra-articular tenodesis procedures of the knee: a systematic review. Arthroscopy. 2016;32(12):2592-2611. doi:10.1016/j.arthro.2016.04.028 [DOI] [PubMed]
- 16. Ebrahimzadeh MH, Makhmalbaf H, Golhasani-Keshtan F, Rabani S, Birjandinejad A. The International Knee Documentation Committee (IKDC) Subjective Short Form: a validity and reliability study. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3163-3167. doi:10.1007/s00167-014-3107-1 [DOI] [PubMed]
- 17. Lysholm J, Tegner Y. Knee injury rating scales. Acta Orthop. 2007;78(4):445-453. doi:10.1080/17453670710014068 [DOI] [PubMed]
- 18. Pennock AT, Johnson KP, Turk RD, et al. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: quadriceps tendon autograft versus hamstring tendon autograft. Orthop J Sports Med. 2019;7(9):2325967119872450. doi:10.1177/2325967119872450 [DOI] [PMC free article] [PubMed]
- 19. Longo UG, Ciuffreda M, Casciaro C, et al. Anterior cruciate ligament reconstruction in skeletally immature patients. Bone Joint J. 2017;99-B:1053–60:1053-1060. [DOI] [PubMed]
- 20. Peterson DC, Ayeni OR. Pediatric anterior cruciate ligament reconstruction outcomes. Curr Rev Musculoskelet Med. 2016;9(4):339-347. doi:10.1007/s12178-016-9358-3 [DOI] [PMC free article] [PubMed]
- 21. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric Anterior Cruciate Ligament Reconstruction: A Systematic Review of Transphyseal Versus Physeal-Sparing Techniques. Am J Sports Med. 2017;45(2):488-494. doi:10.1177/0363546516638079 [DOI] [PubMed]
- 22. Wong SE, Feeley BT, Pandya NK. Complications after pediatric ACL Reconstruction: a meta-analysis. J Pediatr Orthop. 2019;39(8):566-571. doi:10.1097/bpo.0000000000001075 [DOI] [PubMed]
- 23. Cordasco FA, Black SR, Price M, et al. Return to sport and reoperation rates in patients under the age of 20 after primary anterior cruciate ligament reconstruction: risk profile comparing 3 patient groups predicated upon skeletal age. Am J Sports Med. 2019;47(3):628-639. doi:10.1177/0363546518819217 [DOI] [PubMed]
- 24. Larson CM, Heikes CS, Ellingson CI, et al. Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: Outcomes and complications. Arthroscopy. 2016;32(5):860-867. doi:10.1016/j.arthro.2015.10.014 [DOI] [PubMed]
- 25. Hulet C, Sonnery-Cottet B, Stevenson C, et al. The use of allograft tendons in primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:1754-1770. doi:10.1007/s00167-019-05440-3 [DOI] [PubMed]
- 26. Engebretsen L, Lew WD, Lewis JL, Hunter RE. The effect of an iliotibial tenodesis on intraarticular graft forces and knee joint motion. Am J Sports Med. 1990;18(2):169-176. doi:10.1177/036354659001800210 [DOI] [PubMed]
- 27. Devitt BM, Bouguennec N, Barfod KW, Porter T, Webster KE, Feller JA. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis does not result in an increased rate of osteoarthritis: a systematic review and best evidence synthesis. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1149-1160. doi:10.1007/s00167-017-4510-1 [DOI] [PubMed]
- 28. Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45(14):3233-3242. doi:10.1177/0363546517723013 [DOI] [PubMed]
- 29. Schlichte LM, Aitchison AH, Green DW, Cordasco FA. Modified Lemaire lateral extra-articular tenodesis in the pediatric patient: an adjunct to anterior cruciate ligament reconstruction. Arthrosc Tech. 2020;9(1):111-116. doi:10.1016/j.eats.2019.09.010 [DOI] [PMC free article] [PubMed]